Abstract
Introduction:
Intimate partner violence and food insecurity are both structural drivers of HIV acquisition, care, and treatment, but little is known about how the two conditions intersect in the lives of those already living with HIV.
Methods:
This study examined cross-sectional baseline data (collected January 2016–December 2017) from an ongoing trial in southwestern Kenya. Trained interviewers asked enrolled participants living with HIV aged 18–60 years about household food insecurity (using the Household Food Insecurity Access Scale), intimate partner violence (using an adapted WHO multi-country study instrument), and sociodemographics. Negative binomial regression was used to examine the association between food insecurity and partner violence victimization (among women) or perpetration (among men). This secondary analysis was analyzed in August 2019–March 2020.
Results:
Of 720 participants, more than half of women reported experiencing intimate partner violence (57.6%) and most men reported perpetrating it (58.4%). Participants reporting any partner violence had higher Household Food Insecurity Access Scale scores (21.8) compared with those reporting no violence (21.3, p=0.02). Each categorical change in food insecurity (mild, moderate, severe) was associated with 41% increased risk of an additional intimate partner violence episode. In models controlling for relationship status, wealth, season of interview (lean versus not), and baseline physical health, each 1-point increase in food insecurity was associated with 6% higher risk of violence victimization among women and 4% greater risk of men perpetrating partner violence.
Conclusions:
This study highlights the interconnected nature of intimate partner violence and food insecurity among women and men living with HIV. This relationship suggests that enhancing food security may be a useful intervention strategy to prevent intimate partner violence and improve HIV-related health outcomes.
INTRODUCTION
Syndemics are concurrent and mutually reinforcing social and health problems.1,2 The syndemic conditions of food insecurity and intimate partner violence (IPV) are associated with HIV acquisition,3–5 and poor health among HIV-positive populations.6,7 In sub-Saharan Africa, all 3 conditions are higher than elsewhere globally.8,9
Food insecurity is associated with doubled odds of IPV victimization among women in the general population,10–14 though quantitative work among HIV-positive women is limited. Qualitative research suggests IPV leads to food insecurity if it prompts HIV-positive women to leave violent partners and shoulder household financial needs alone.15
Among men in the general population, food insecurity is associated with higher odds of IPV perpetration.16,17 Little is known about this association among HIV-positive men, though IPV perpetration and food insecurity are both linked to men’s HIV risk.5,18
A theoretical framework underpins the relationship between food insecurity and IPV.16 Men may re-exert control through violence if unable to meet provider roles (gender resource theory)19,20 or deprivation could heighten acute stressors in the household (family stress theory)21 and deplete men’s ability to attain self-control (physiology of willpower).22 A bidirectional relationship could exist if IPV exposure lowers economic earnings,23 increases household financial burden due to injury or missing work,24 or makes relationships unstable—lowering the ability of single-earner households to obtain sufficient food.
This study examines the association between food insecurity severity and IPV among HIV-positive individuals in rural Kenya using cross-sectional data from an ongoing trial.
METHODS
This was a secondary analysis of baseline data from the Shamba Maisha cluster RCT. Shamba Maisha is a multisectoral agricultural intervention including: (1) low-cost irrigation water pump, (2) group agricultural training, and (3) loan ($150) for seeds/fertilizers.25,26
Study Sample
Eight matched pairs of health facilities in southwestern Kenya were randomized to intervention (n=360) or control arms (n=362). Inclusion criteria were being on antiretroviral treatment, aged 18–60 years, with access to surface water. Included participants had moderate-to-severe food insecurity, assessed using the Household Food Insecurity Access Scale (HFIAS), and were willing to save a down payment applied toward the agricultural loan. Trained researchers led structured interviews (January 2016–December 2017) and abstracted clinical data from medical records.
Measures
This study assessed IPV through 4 self-reported items on lifetime physical or sexual violence (adapted from the WHO instrument27). Investigators examined IPV experienced by female participants and perpetrated by male participants. Frequency of each violent act was assessed on a Likert-type scale (0, never; 1, once; 2, two or three times; 3, ≥4 times). The index was assessed as a dichotomous outcome (ever versus never) and continuous measure of IPV intensity (scores ranged from 0 to 12).
A HFIAS score assessed food insecurity as a continuous variable. Scores ranged from 11 to 36 and the scale had acceptable internal consistency (Cronbach’s α=0.81). Scores were categorized as mild (<14), moderate (14–21), or severe (≥22) food insecurity.28
Sociodemographic covariates included: season of interview (lean versus not), age, marital status (married versus widowed/separated/single), number of children, education level, baseline CD4 count, and a wealth index.29
Statistical Analysis
These secondary analyses were not pre-registered (conducted August 2019–May 2020) and were led using Stata, version16. Bivariate analyses for normally distributed and categorical variables (t-test, chi-square test) and non-normally distributed variables (Wilcoxon) were conducted by IPV status.
The authors fitted negative binomial regressions by sex to account for participants with no experience of IPV (resulting in a large number of 0s). Negative binomial models assume each individual has their own Poisson distribution, thus allowing individuals to vary in propensity of reporting IPV. Authors adjusted for covariates of theoretical significance: season of interview, age, wealth index, marital status, education, and health status (CD4 count). Past research suggests the similar sociodemographic covariates predict IPV victimization and IPV perpetration,30,31 so similar covariates were used in models for women and men. Analyses accounted for clustering by clinic using a sandwich estimator.
Written informed consent was obtained from study participants. Ethical approval for the study was granted by Kenya Medical Research Institute and University of California, San Francisco. As data are part of an ongoing trial, they are not yet publicly available.
RESULTS
Of 720 baseline participants, 396 (55.0%) were female. The mean HFIAS score was 21 for men and 22 for women (p=0.008), with 569 (78.9%) reporting severe food insecurity (Table 1).
Table 1.
Descriptive Data and Bivariate Associations of Sociodemographics and IPV, by sex (n=720)
| Total | IPV experience among women | IPV perpetration by men | |||||
|---|---|---|---|---|---|---|---|
| Sociodemographics | Median (IQR) or n (%) | None | Ever IPV | p-value | None | Ever IPV | P-value |
| Age (years) | 40 (34–47) | 43.3 | 42.3 | 0.53 | 38.5 | 37.9 | 0.38 |
| Children (number) | 4 (2–5) | 3.5 | 3.7 | 0.29 | 4.1 | 4.3 | 0.80 |
| Primary school education (vs not) | 415 (57.6%) | 52.1% | 47.6% | 0.38 | 64.9% | 70.2% | 0.32 |
| Widowed, separated, or single (vs married) | 198 (27.5%) | 46.1% | 37.9% | 0.10 | 14.2% | 8.0% | 0.07 |
| Polygynous marriage | 173 (29.5%) | 21.1% | 35.9% | 0.01 | 30.6% | 27.3% | 0.53 |
| Lowest wealth quintile | 142 (19.5%) | 18.9% | 24.1% | 0.54 | 23.5% | 14.0% | 0.13 |
| Baseline CD4 (count) | 560 (397–745) | 636 | 649 | 0.68 | 506 | 512 | 0.86 |
| Interview season (lean vs not) | 165 (22.8%) | 22.8% | 22.5% | 0.95 | 17.9% | 27.1% | 0.05 |
IPV, intimate partner violence.
A majority of women (57.6%) reported IPV victimization and a majority of men (58.4%) reported perpetrating IPV. Participants reporting any IPV had higher HFIAS scores (21.8) compared with those reporting no IPV (21.3, p=0.02), though this bivariate analysis was not significant by sex (men: p=0.07, women: p=0.05, data not shown). A scatterplot with fitted line (Figure 1) illustrates how HFIAS was associated with IPV perpetration (p=0.029) and victimization (p=0.002).
Figure 1.
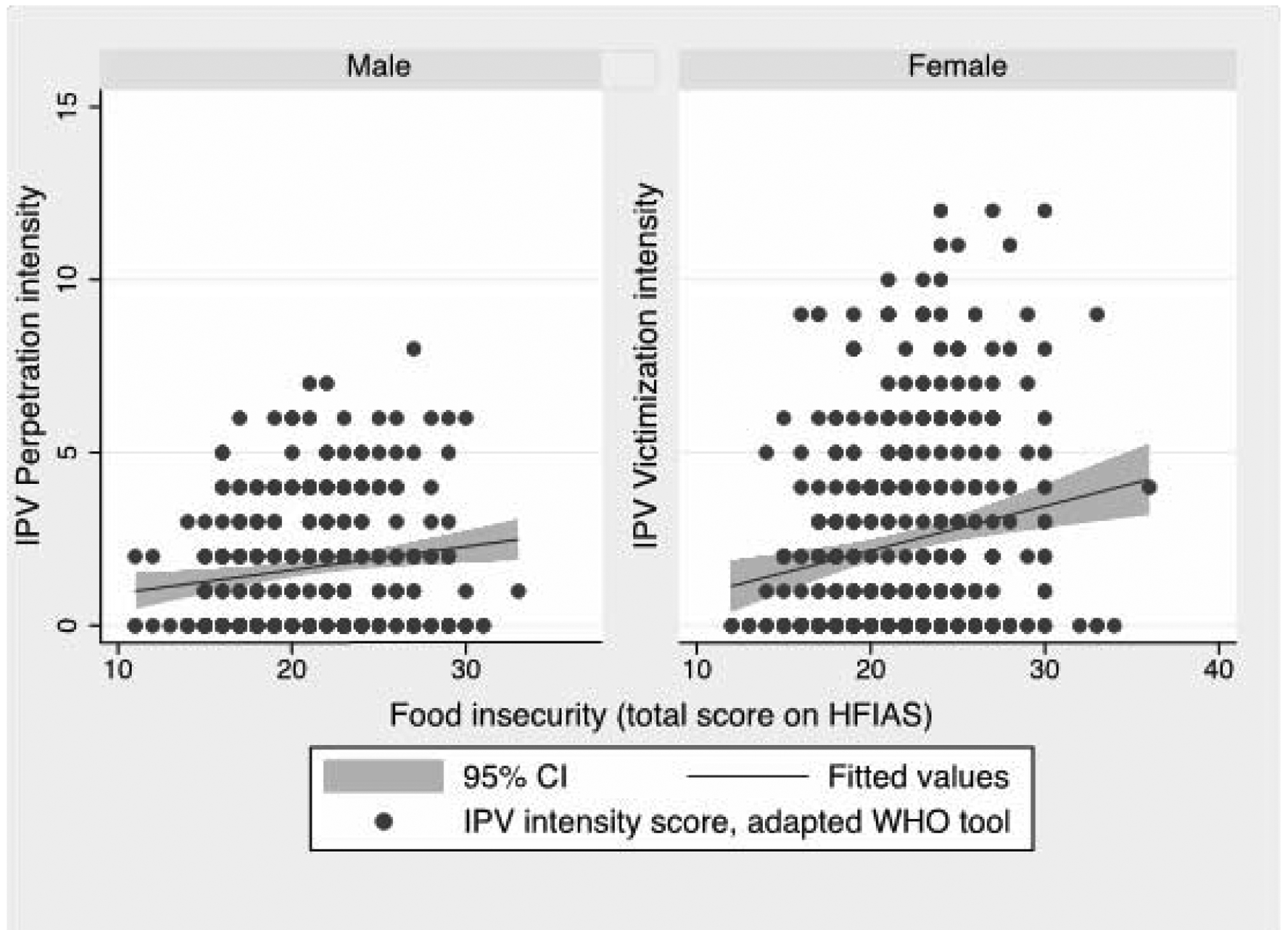
Scatterplot and fitted line of food insecurity and IPV intensity, by sex. IPV, intimate partner violence.
Each 1-point increase on HFIAS was associated with higher adjusted risk of IPV victimization among women (adjusted incident rate=1.06, 95% CI=1.01, 1.10) (Table 2). Among men, HFIAS was associated with greater risk of IPV perpetration (adjusted incident rate ratio=1.04, 95% CI=1.01, 1.07). Each change in food insecurity category (mild, moderate, severe) was associated with 41% increased risk of an additional IPV episode (95% CI=1.10, 1.82, p=0.007) (Appendix Table 1). Categorical interpretation did not reach statistical significance among women (p=0.068) or men (p=0.097).
Table 2.
Unadjusted and Adjusted Negative Binomial Regressions of IPV, by Sex (n=720)
| Bivariate associations | Model 1: IPV experience among women (n=396) | Model 2: IPV perpetration by men (n=324) | ||||
|---|---|---|---|---|---|---|
| Variable | IRR (95% CI) | p-value | aIRR (95% CI) | p-value | aIRR (95% CI) | p-value |
| Food insecurity | 1.06 (1.02, 1.09) | <0.001 | 1.06 (1.01, 1.10) | 0.012 | 1.04 (1.01, 1.07) | 0.043 |
| Sociodemographics | ||||||
| Age (years) | 0.99 (0.98, 1.01) | 0.521 | 0.99 (0.97, 1.01) | 0.350 | 0.99 (0.98, 1.02) | 0.616 |
| Children | 1.01 (0.67, 1.04) | 0.615 | 0.99 (0.93, 1.05) | 0.340 | 1.01 (0.95, 1.06) | 0.819 |
| Primary school education | 0.87 (0.75, 1.02) | 0.095 | 0.78 (0.61, 1.04) | 0.097 | 1.17 (0.98, 1.63) | 0.171 |
| Wealth index quintiles | 0.95 (0.86, 1.05) | 0.306 | 0.91 (0.83, 1.04) | 0.537 | 1.02 (0.92, 1.07) | 0.632 |
| Widowed, separated, or single | 0.99 (0.80, 1.19) | 0.834 | 0.98 (0.68–1.45) | 0.891 | 0.80 (0.43, 1.47) | 0.475 |
| Polygynous household | 1.18 (0.97, 1.44) | 0.079 | 1.41 (1.15, 1.72) | 0.001 | 0.99 (0.60, 1.39) | 0.946 |
| Baseline CD4 | 1.00 (1.00, 1.00) | 0.188 | 1.00 (1.00, 1.00) | 0.589 | 1.00 (1.00, 1.00) | 0.594 |
| Interview Season (lean vs not) | 1.24 (0.90, 1.72) | 0.184 | 0.08 (0.59, 1.24) | 0.412 | 1.34 (0.96, 1.86) | 0.085 |
Note: Boldface indicates statistical significance (p<0.05).
IRR, incident risk ratio; aIRR, adjusted incident risk ratio; IPV, intimate partner violence.
DISCUSSION
In a sample of men and women living with HIV, food insecurity was independently associated with IPV. In this predominately food-insecure sample, increased severity of food insecurity was linearly associated with greater IPV intensity. Each change in food insecurity category (mild, moderate, severe) was associated with 41% increased risk of an additional IPV episode.
These findings are consistent with extant studies among the general population, where food insecurity is associated with between 2-fold and 6-fold increased odds of any IPV perpetration16,17,32 or victimization.33–36 This is the first analysis, to the authors’ knowledge, to examine food insecurity and IPV among an HIV-positive cohort in sub-Saharan Africa. Further research may suggest these conditions in HIV-positive samples are unique from or similar to the general population.
More than half of women (58%) reported experiencing IPV, which is higher than among HIV-positive women in Uganda (44%).37 Among men, 58% reported IPV perpetration, which is higher than among HIV-positive men in Vietnam (38%).38 High IPV exposure has clinical implications, as it leads to incident HIV infection,3 lowers women’s antiretroviral treatment adherence and viral control,6 and has health effects for men themselves.39
These findings suggest that even when programs are unable to fully ameliorate food insecurity, slight improvements around food may be accompanied by safer relationships. Adding food security programming to clinical care could reach HIV-positive patients who experience or perpetrate IPV. By focusing on food security as an “upstream determinant” of health, programs may ultimately reduce IPV and improve HIV-related health.
Limitations
There are several limitations of this analysis. The small sample limits analysis of variables as categorical. Cross-sectional data limit causal conclusions, in particular given timing of past-month food insecurity and lifetime IPV. The study controlled for potential seasonality of food security by including season of interview as a covariate, but this does not fully ameliorate the temporality of food reporting. Self-reported measures for food insecurity or IPV may be limited by social desirability bias. Asking about women’s experience and men’s perpetration of IPV precludes exploring bidirectional relationship violence. Though the measure of IPV asks behaviorally-specific items, there are noted limitations to IPV measures,40 and the 4-item scale was not validated.
CONCLUSIONS
This report highlights the interconnected nature of IPV and food insecurity in an HIV-positive sample in Kenya. High prevalence of IPV in this region, alongside the declines in adherence and HIV-related health associated with IPV6,41 and food insecurity,7 make this a crucial intersection for future work. Enhancing food security may be a useful intervention strategy to address nutrition, IPV, and HIV going forward.
Supplementary Material
ACKNOWLEDGMENTS
This study was funded by National Institutes of Mental Health (R01 MH107330 05) and National Institutes of Mental Health (K01 MH12118501).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423‒441. 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 2.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941‒950. 10.1016/s0140-6736(17)30003-x. [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17(1):18845. 10.7448/ias.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiser SD, Palar K, Hatcher AM, Young SL, Frongillo EA. Food insecurity and health: a conceptual framework. In: Ivers L, ed. Food insecurity and public health. CRC Press; 2015:23‒50. 10.1201/b18451-3. [DOI] [Google Scholar]
- 5.Palar K, Laraia B, Tsai AC, Johnson M, Weiser SD. Food insecurity is associated with HIV, sexually transmitted infections and drug use among men in the United States. AIDS. 2016;30(9):1457‒1465. 10.1097/qad.0000000000001095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hatcher AM, Smout EM, Turan JM, Christofides N, Stoeckl H. Intimate partner violence and engagement in HIV care and treatment among women: a systematic review and meta-analysis. AIDS. 2015;29(16):2183‒2194. 10.1097/qad.0000000000000842. [DOI] [PubMed] [Google Scholar]
- 7.Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S‒1739S. 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Devries KM, Mak JY, Garcia-Moreno C, et al. The global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527‒1528. 10.1126/science.1240937. [DOI] [PubMed] [Google Scholar]
- 9.FAO, IFAD, UNICEF, WFP, WHO. The State of Food Security and Nutrition in the World 2019. Safeguarding against economic slowdowns and downturns. Rome: FAO; 2019. http://www.fao.org/3/ca5162en/ca5162en.pdf. Accessed July 20, 2020. [Google Scholar]
- 10.Breiding MJ, Basile KC, Klevens J, Smith SG. Economic insecurity and intimate partner and sexual violence victimization. Am J Prev Med. 2017;53(4):457‒464. 10.1016/j.amepre.2017.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melchior H, Hergert A, Hofreuter-Gatgens K, et al. [Predictors of treatment duration for inpatients with mental disorders--a systematic literature review]. Z Psychosom Med Psychother. 2010;56(4):399‒418. 10.13109/zptm.2010.56.4.399. [DOI] [PubMed] [Google Scholar]
- 12.Ricks JL, Cochran SD, Arah OA, Williams JK, Seeman TE. Food insecurity and intimate partner violence against women: results from the California Women’s Health Survey. Public Health Nutr. 2016;19(5):914‒923. 10.1017/s1368980015001986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diamond-Smith N, Conroy AA, Tsai AC, Nekkanti M, Weiser SD. Food insecurity and intimate partner violence among married women in Nepal. J Glob Health. 2019;9(1):010412. 10.7189/jogh.09.010412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conroy AA, Cohen MH, Frongillo EA, et al. Food insecurity and violence in a prospective cohort of women at risk for or living with HIV in the US. PLoS One. 2019;14(3):e0213365. 10.1371/journal.pone.0213365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Derose KP, Payan DD, Fulcar MA, et al. Factors contributing to food insecurity among women living with HIV in the Dominican Republic: a qualitative study. PLoS One. 2017;12(7):e0181568. 10.1371/journal.pone.0181568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatcher AM, Stockl H, McBride RS, Khumalo M, Christofides N. Pathways from food insecurity to intimate partner violence perpetration among peri-urban men in South Africa. Am J Prev Med. 2019;56(5):765‒772. 10.1016/j.amepre.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 17.Chirwa ED, Sikweyiya Y, Addo-Lartey AA, et al. Prevalence and risk factors of physical or sexual intimate violence perpetration amongst men in four districts in the central region of Ghana: baseline findings from a cluster randomised controlled trial. PLoS One. 2018;13(3):e0191663. 10.1371/journal.pone.0191663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatcher AM, Gibbs A, McBride R, Rebombo D, Khumalo M, Christofides N. Gendered syndemic of intimate partner violence, alcohol misuse, and HIV risk among peri-urban, heterosexual men in South Africa. Soc Sci Med. In press. Online October 22, 2019. 10.1016/j.socscimed.2019.112637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Connell RW, Messerschmidt JW. Hegemonic masculinity - rethinking the concept. Gend Soc. 2005;19(6):829‒859. 10.1177/0891243205278639. [DOI] [Google Scholar]
- 20.Stets JE. Job autonomy and control over one’s spouse: a compensatory process. J Health Soc Behav. 1995;36(3):244‒258. 10.2307/2137341. [DOI] [PubMed] [Google Scholar]
- 21.Fox GL, Benson ML, DeMaris AA, Wyk J. Economic distress and intimate violence: testing family stress and resources theories. J Marriage Fam. 2002;64(3):793‒807. 10.1111/j.1741-3737.2002.00793.x. [DOI] [Google Scholar]
- 22.Baumeister RF, Heatherton TF, Tice DM. Losing control: how and why people fail at self-regulation. Cambridge, MA: Academic Press; 1994. [Google Scholar]
- 23.Lindhorst T, Oxford M, Gillmore MR. Longitudinal effects of domestic violence on employment and welfare outcomes. J Interpers Violence. 2007;22(7):812‒828. 10.1177/0886260507301477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peterson C, Kearns MC, McIntosh WL, et al. Lifetime economic burden of intimate partner violence among U.S. adults. Am J Prev Med. 2018;55(4):433‒444. 10.1016/j.amepre.2018.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weiser SD, Bukusi EA, Steinfeld RL, et al. Shamba maisha: randomized controlled trial of an agricultural and finance intervention to improve HIV health outcomes in Kenya. AIDS. 2015;29(14):1889‒1894. 10.1097/qad.0000000000000781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen CR, Steinfeld RL, Weke E, et al. Shamba Maisha: pilot agricultural intervention for food security and HIV health outcomes in Kenya: design, methods, baseline results and process evaluation of a cluster-randomized controlled trial. Springerplus. 2015;4(1):122. 10.1186/s40064-015-0886-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368(9543):1260‒1269. 10.1016/s0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 28.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2006. 10.1037/e576842013-001. [DOI] [Google Scholar]
- 29.Measure DHS. DHS Wealth Index. Calverton, MD: ORC Macro; 2004. [Google Scholar]
- 30.Fulu E, Jewkes R, Roselli T, Garcia-Moreno C. Prevalence of and factors associated with male perpetration of intimate partner violence: findings from the UN Multi-country Cross-sectional Study on Men and Violence in Asia and the Pacific. Lancet Glob Health. 2013;1(4):e187‒207. 10.1016/s2214-109x(13)70074-3. [DOI] [PubMed] [Google Scholar]
- 31.Costa BM, Kaestle CE, Walker A, et al. Longitudinal predictors of domestic violence perpetration and victimization: a systematic review. Aggress Violent Behav. 2015;24:261‒272. 10.1016/j.avb.2015.06.001. [DOI] [Google Scholar]
- 32.Gilbert L, Michalopoulos L, Ma X, et al. How do risk environment factors influence perpetration of partner violence among male migrant and non-migrant market workers in Central Asia? J Urban Health. 2019;96(1):83‒95. 10.1007/s11524-018-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Field S, Onah M, van Heyningen T, Honikman S. Domestic and intimate partner violence among pregnant women in a low resource setting in South Africa: a facility-based, mixed methods study. Bmc Womens Health. 2018;18:119. 10.1186/s12905-018-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gibbs A, Jewkes R, Willan S, Washington L. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18‒30) women and men in urban informal settlements in South Africa: a cross-sectional study and structural equation model. PLoS One. 2018;13(10):e0204956. 10.1371/journal.pone.0204956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Swahn MH, Dill LJ, Palmier JB, Kasirye R. Girls and young women living in the slums of Kampala: prevalence and correlates of physical and sexual violence victimization. Sage Open. 2015;5(2). 10.1177/2158244015580853. [DOI] [Google Scholar]
- 36.Willie TC, Kershaw TS, Callands TA. Examining relationships of intimate partner violence and food insecurity with HIV-related risk factors among young pregnant Liberian women. AIDS Care. 2018;30(9):1156‒1160. 10.1080/09540121.2018.1466983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kabwama SN, Bukenya J, Matovu JK, et al. Intimate partner violence among HIV positive women in care-results from a national survey, Uganda 2016. BMC Womens Health. 2019;19(1):130. 10.1186/s12905-019-0831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hershow RB, Ha TV, Sripaipan T, et al. Perpetration of intimate partner violence among men living with HIV in Northern Vietnam. AIDS Behav . In press. Online February 20, 2020. 10.1007/s10461-020-02813-5. [DOI] [PubMed] [Google Scholar]
- 39.Courtenay WH. Constructions of masculinity and their influence on men’s well-being: a theory of gender and health. Soc Sci Med. 2000;50(10):1385‒1401. 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 40.Follingstad DR, Bush HM. Measurement of intimate partner violence: a model for developing the gold standard. Psychol Violence. 2014;4(4):369‒383. 10.1037/a0037515. [DOI] [Google Scholar]
- 41.Leddy AM, Weiss E, Yam E, Pulerwitz J. Gender-based violence and engagement in biomedical HIV prevention, care and treatment: a scoping review. BMC Public Health. 2019;19:897. 10.1186/s12889-019-7192-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


