Abstract
Purpose of review
The optimal approach to screening young people to decrease the risk of sudden death remains unknown. It deserves the passionate attention that researchers, clinicians and families have given it. The new data from January 2018 to July 2019 are reviewed here.
Recent findings
Cardiac findings associated with a risk of sudden death were reported in 0.4% of screened athletes. Well-run programs continue report varying sensitivity for screening ECGs (between 86–100%). One major paper reported a higher incidence of sudden death in young people than has been previously published (6.8/100,000 athletes).
Summary
The rate of important findings in sophisticated screening programs is approximately 0.4%, suggesting that this is near the population rate of detectable disease in most athletic groups. ECGs are unquestionably capable of detecting disease that can be missed by history and physical, but the performance characteristics of ECGs continue to vary from study to study. In addition, the underlying cost and infrastructure of ECG and echocardiographic screening remains unaddressed by the recent literature. A few small studies have started to look at alternative technology approaches to ECG screening.
Keywords: Pediatrics, Sudden Death, Primary Prevention, Review
Introduction
Sudden death in the young due to cardiovascular diseases remains a focus of the public health system. When victims under 40 years of age, they forfeit decades of potentially healthy life. In addition, several of the diseases that cause sudden death in the young can be diagnosed and treated prior to the first lethal event.
While sudden death from cardiovascular causes is a small percentage of sudden death in young people (Figure 1), it is an appealing target for screening. The goal is to identify people at risk using a relatively limited intervention, such as a history and physical and/or ECG. SCD is also important because the emotional toll is devastating. Sudden cardiac death deeply affects families and communities; the stories are often dramatic and receive extensive media coverage. One of the most inspirational examples of locally-driven healthcare initiatives during the last two decades has been the blossoming of support networks and local screening programs, often with local fundraising support and extensive volunteerism.
Figure 1.
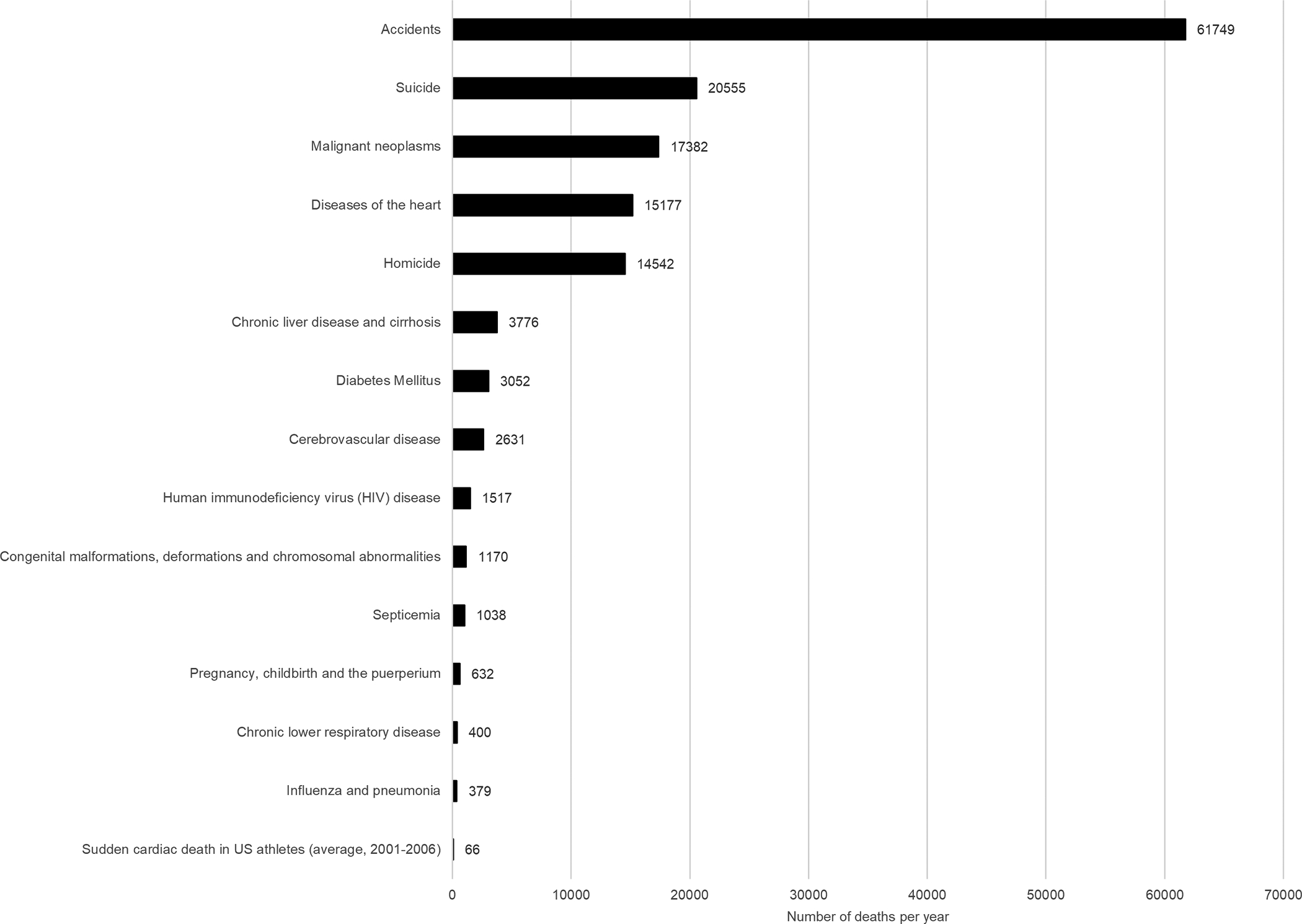
Causes of Death in the United States
Causes of death in the United States, as reported by the National Center for Health Statistics[42] and compared to prior publication of deaths in young, competitive athletes in the United States.[18]
The consideration of ECGs as a component of a national screening initiative – or as a standalone screening methodology – has been the subject of intense focus for over 25 years.[1] While the European Society of Cardiology “recommends the implementation of a common European screening protocol essentially based on 12-lead ECG” [pp. 517],[2] Italy and Israel remain the only countries to have incorporated ECGs in their national screening programs. In addition, several major organizations in the United States have published comprehensive position statements which do not recommend a pre-participation ECG program in either athletes or the unselected young population in the United States.[3–7]
Given the ongoing controversies, we reviewed new data that have been published within the last 18 months (January, 2018 – July, 2019) and put those data within the context of existing knowledge within the field.
Performance of ECG screening
The positive and negative predictive values of screening ECGs remain the central scientific question that determines their use in population screening. The largest study to evaluate this question in the last 18 months was published by Malhotra et al.[8] In this study, 0.38% of athletes had cardiac disorders associated with SCD. This prevalence is the same as earlier studies and other studies published this year (Figure 2).[5, 9, 10] It is important to establish scientific consensus around this rate; it is a major pivot point in cost effectiveness analyses.[11–15] These authors also performed longitudinal follow-up of their screening cohort. The incidence of sudden death was 6.8/100,000 athletes. This rate of death is higher than has been reported in other populations. Importantly, it is higher than the rate of death in the Veneto region of Italy in 1979–1981, which was 4.2/100,000.[16] Prior to the Malhotra publication, no previous large systematic study had documented rates >4. In contrast, most reports have shown rates <1/100,000 patients.[17–20] The low rate of sudden death elsewhere and the question of whether Veneto had achieved real death reduction with an ECG screening program is among the most common criticisms of the Italian effort. It remains unclear whether the rate in Malhotra’s work represents something unique about the English soccer cohort, a statistical blip, or whether it is an improved tabulation of a large population. The NIH-funded Sudden Death in the Young network, coordinated with the Centers for Disease Control, was funded several years ago in part to report accurate incidence data. While the data are not yet available, the network reported their initial methodology in 2017 and further data should be forthcoming.[21] These data may put the Malhotra rate in context of a U.S. population-based effort. The other important feature of the Malhotra data was the lack of efficacy in a one-time ECG screening, a point that has been made on several previous occasions. Seven of eight sudden cardiac deaths in their cohort were secondary to cardiomyopathy, plus one sudden arrhythmia death. Among those eight deaths, 75% had undergone a normal screening evaluation, including ECG, suggesting that they were screened in a pre-clinical phase of the disease.
Figure 2.
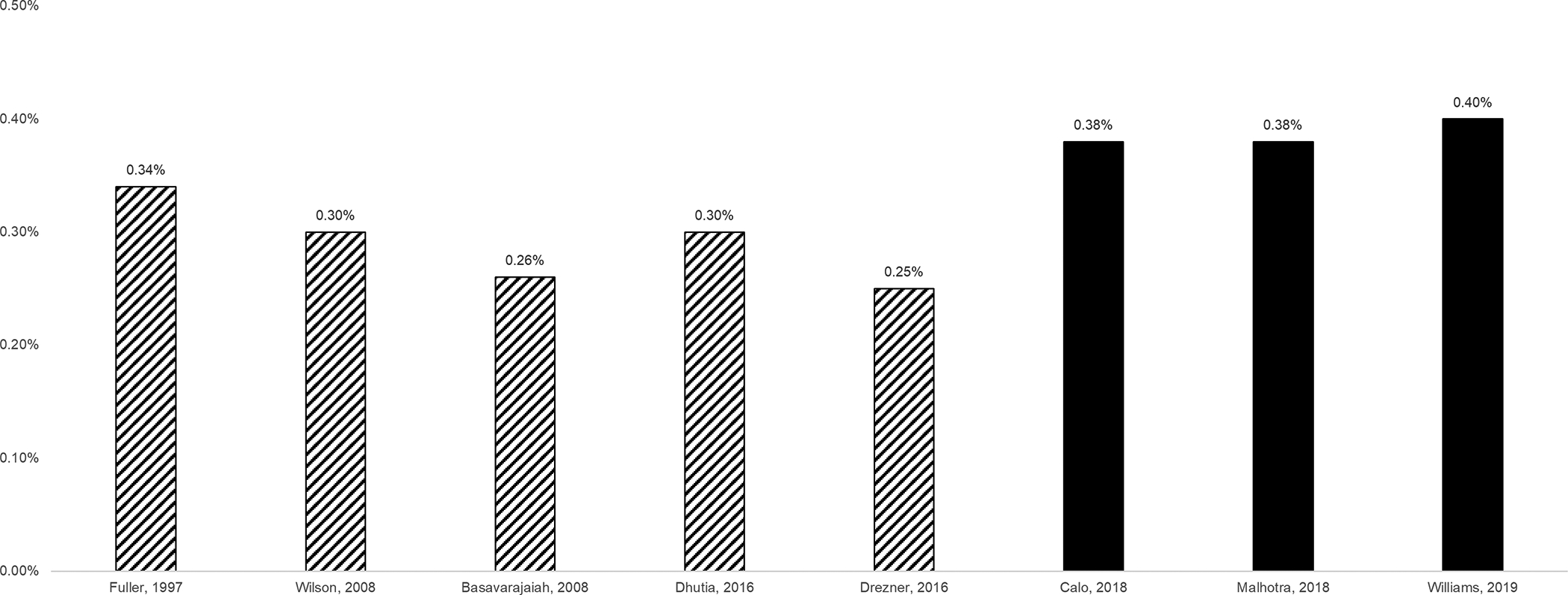
Discovery Rates for Previously Undiagnosed Cardiac Disease Associated with an Elevated Risk of Sudden Death
Data from prior studies (hatched)[43–47] are compared against papers published in the last 18 months (solid).[8–10] The range of the ordinate axis is a narrow band, between 0 and 0.5%, demonstrating a strong agreement between studies that the rate of undiagnosed disease is under 0.5%.
In a separate study[22], the Malhotra group analyzed ECGs using four methods: the 2010 European Society of Cardiology recommendations;[23] the Seattle criteria;[24] refined criteria;[25] and the international recommendations for ECG interpretation in young athletes.[26] All four methods identified the same cohort of 36 athletes with serious pathology, although ECGs missed 6 patients identified by other means. However, like the Williams paper below, Malhotra et al conclude that history and physical alone is insufficiently sensitive. They continue to recommend ECGs.
Williams et al, an experienced group from Washington State, also reported on abnormal screening rates using ECG.[9] In 5,003 high school students, the authors performed a prospective evaluation that included both the AHA 14-point screening evaluation and a resting ECG for cardiovascular screening, using the Seattle criteria for ECG evaluation. The authors report that 2.8% of students had an abnormal ECG, consistent with other recent rates in the field. At the end of the prospective screening algorithm, 0.4% of students were diagnosed with a condition associated with sudden cardiac death. This is congruent with the 0.38% reported by Malhotra et al, thus demonstrating that two well-designed studies in different populations of young athletes have the same yield of abnormal cardiac conditions when screening is performed in expert hands (Figure 2). Williams et al provided exceptional detail on the performance of the AHA screening tool versus the ECG and concluded that the ECG out-performed the AHA screening tool in this setting. The manuscript was the subject of an editorial that re-interpreted the data to emphasize the utility of the AHA tool.[27] The editorial re-interpretation had weaknesses, but in anyone’s hands, the data emphasize that the AHA tool and ECGs are testing a different expression of disease.
Finally, Calo et al extended the data from the Italian national screening program using the 2017 international recommendations, the Seattle criteria and the ESC criteria.[10] Abnormal ECGs were present in 2.9% of screened patients. The authors report that the sensitivity of ECG for critical disease was 100% (versus 93% in the Williams study and 86% in the Malhotra study, all three with small numbers of positive findings). Calo et al note that echocardiography uncovered additional cardiac disease; however, even with addition of echocardiography; they continue to report similar rates of critical disease to the Malhotra and Williams study (0.38%), emphasizing the stability of this estimate.
Racial Disparity
Most of the validation of ECG screening has continued to occur in predominantly white populations, with some recent exceptions.[28] Both the Malhotra data and the Williams data are drawn from populations of mostly white participants (79% and 91%, respectively). One purpose of a second Malhotra paper was to perform subgroup analysis.[22] Abnormal ECGs were 120–225% more likely to occur in black athletes in their study. The elevated rate of ECGs flagged as abnormal in African-Americans and black athletes was reinforced by Movahed et al in a separate study.[29] The authors evaluated a mostly-teenaged cohort of 636 people who were assembled through a volunteer-based organization, the Anthony Bates Foundation. The authors separated results by African-American identification (8%), compared to all other racial groups (92%). An abnormal ECG was reported in 21% of the African-American sub-group and 23% of the teenaged African-Americans. Both of these numbers were significantly higher than patients reporting other racial identification (7% and 8%, respectively for the overall cohort and teenagers). However, there are two critical gaps in this study. First, ECGs were “interpreted by a board-certified cardiologist” [pp. 86], without any apparent reference to existing ECG screening methodologies. The four ECG screening methods mentioned above have been subject to rigorous evaluation; whereas, unspecified evaluation by a participating physician is outside the current best practices of tabulating abnormal ECGs. Perhaps of greater concern, the authors report, “We have no follow-up to evaluate long-term outcome in participants with abnormal ECG” [pp. 88], meaning they report no data on whether abnormal ECGs were associated with disease. While the lack of follow-up may be due to understandable privacy limitations in a volunteer-based screening organization, the combination of no defined method of evaluating ECGs and no outcome data prevent this study from being generalizable.
Novel Technology
New ECG technologies have been introduced in the last several years. A Turkish group, collaborating with their Canadian counterparts, evaluated QTc intervals in both 12-lead ECGs and AliveCor devices, finding a Pearson’s correlation of 0.57 between the two.[30] This remains well below the correlation that would be required to substitute an AliveCor device for 12-lead ECG screening. In addition, the manuscript does not address findings other than long QT syndrome, such as ventricular pre-excitation and ventricular hypertrophy. However, since one of the major limitations to ECG screening is the availability of time, infrastructure, and qualified personnel to interpret the tracings across a large population, this effort represents an early attempt to understand the strengths and limitations of alternative approaches.
Another new technology that could affect the cost and feasibility of ECG screening programs is machine learning. In a 2019 study by Hannun et al, a deep neural network outperformed cardiologists in single-lead ambulatory ECG interpretation of 12 different rhythms.[31] This follow on the heels of other similar work.[32] If this technology reaches a point where it can reliably interpret 12 lead ECGs, then it could have a profound effect on the feasibility of a large population screening program.
ECG Summary
The data from 2018 and 2019 largely confirm existing data that the rate of critical disease in screened young athletes is less than 1%, with all three major studies this year having a consensus of 0.4%. Abnormal ECGs occur at a rate of approximately 2–3% in most studies. While current criteria have considered racial differences, there remains a higher rate of screen-positive ECGs among black or African-American populations. The most important new data are the high rate of subsequent sudden deaths in the Malhotra article (6.8/100,000), which will require further validation since it is substantially above the incidence established outside of the Veneto region of Italy.
Echocardiography
A growing body of literature has evaluated whether point-of-access echocardiography improves specificity. Since all comprehensive screening methods eventually involve echocardiography in the process of additional evaluation, there is intuitive value to including it at the point of access. For example, hypertrophic cardiomyopathy is an important cause of potentially preventable SCD in the United States.[18] While ECG may suggest hypertrophy, echocardiography remains the gold standard for diagnosis. The initial identification of echocardiographic cardiac hypertrophy may improve the sensitivity and specificity of the screening evaluation. Contemporaneous assessment of LV size and volume may decrease anxiety, decrease the use of temporary exercise restriction, and lessen the burden of additional referrals. In 2019, Modaff et al reported results from a 5-minute echocardiogram screening protocol in a university athletic screening setting in 2,898 athletes. Three athletes received restrictions on the basis of abnormal screening echocardiograms (0.1%).[33] The results of this study are consistent with other preliminary studies on echocardiographic screening.[34–36] Another study from Germany focused only on coronary arteries.[37] The sample size of 1,045 was small, but this represents another focused approach to echocardiographic screening. Many questions remain unanswered about the process of integrating echocardiography into screening, including structural findings that need to be communicated to families, but do not lead to life-saving interventions.[38] However, the most important hurdles of integrating echocardiography are the daunting operational, logistical and financial problems that would be required for population screening.
Laboratory screening
An interesting study from the last 18 months was from the University of Kansas. Darche et al reported a retrospective analysis of annual pre-participation screening results for a professional United States sports team, including blood serum results, which they specifically place into the context of their ECG screening effort.[39] While the laboratory panel varied slightly from year to year, the consistent tests were complete blood count, complete metabolic panel, lipid panel, thyroid-stimulating hormone, urinalysis, iron, purified protein derivative (tuberculosis skin test), and electrocardiogram (ECG). In 142 players with 3,148 tests, 10% of all tests were abnormal and 40% of those required additional testing; none were life-saving. In summary, the authors conclude that there was no mortality advantage to serum laboratory testing in a major professional sports team. While this conclusion has previously been assumed in the conversation surrounding sports screening for sudden death, this manuscript represents a unique report supporting this empiric decision in elite athletes.
Secondary Prevention
The relationship between exercise, athletics and sudden death has been extensively studied. In the 2006 paper from Italy, which triggered much interest in screening for sudden death in the young, the mortality rate among athletes was 4.2/100,000 person-years, decreasing to 2.4/100,000 person-years by the end of the observation period; whereas, in non-athletes, the rate was a stable 0.8/100,000 person-years. The article also notes that “in 91% [of cases], sudden death occurred during sports activity or immediately afterward.” [pp. 1596][16] From this anchor point, most of the data concerning sudden death prevention has focused on screening young, competitive athletes. Even the strongest guidelines to date from the European Society of Cardiology limited recommendations to athletes.[2] However, the pool of non-athletes is larger than athletes, and an editorial from Maron et al in 2018 explicitly makes the case that non-athletes, as a group, will account for more sudden unexplained deaths than athletes.[27] All of these arguments about exercise versus non-exercise occur with the background that for most people, lifelong exercise has been shown overwhelmingly to be cardioprotective.
Into this mix, Pechmajou et al reported from an ongoing, prospective registry that includes all sudden cardiac arrest in Paris and its suburbs.[40] They identified 13,400 cardiac arrests in a broad age group (mean age 51), of which 154 occurred during sports. An event during sports was associated with a corrected odds ratio of survival that was 1.8 times higher than the survival rate when sudden death occurred in a non-sports environment. The authors conclude that access to rapid interventions, especially cardiopulmonary resuscitation (CPR) and an automated external defibrillator (AED), saves lives. These data are complementary to data from Tsuda et al who documented the added diagnostic value available to physicians by downloading event tracings from children successfully treated by AEDs.[41] While these manuscripts do not resolve the underlying question of the relationship between sports and sudden cardiac death, they continue to suggest that the worldwide efforts toward teaching CPR, use of AEDs, and excellent secondary prevention continue to bear fruit. They also provide an example of the positive cultural gains that the CPR and AED community have made in the sporting world.
CLINICAL PERSPECTIVE
While the argument for screening for diseases that cause SCD has been ongoing for decades, we are now at the fifteenth anniversary of the Corrado paper, originally published in 2006, which kicked the argument into high gear. No optimal approach has yet been established to screen for risk of sudden cardiac death, either among athletes or in the broader population. Opinions continue to vary, with core positions held strongly on both sides, occasionally gaining adherents or splintering off into subgroups. This paper reviews nearly all of the novel data published in the last 18 months, consisting of 12 published manuscripts. By comparison, a structured search for “screening sudden death”, restricted to populations under 40, includes over 30 opinion papers in the same time period.
Population screening to decrease the incidence of sudden death in young people remains an important question that deserves the attention of researchers and clinicians. We are fortunate to practice in an era where new data become available at a rapid pace allowing us to better frame our local and national efforts.
CONCLUSION
The contributions in the last 18 months suggest that the rate of critical findings when screening athletes is 0.4%. ECGs detect pathology that a history-and-physical approach fails to identify, but consensus around the positive and negative predictive values remains elusive. In addition, the higher rate of sudden death found in the Malhotra study should continue to be tested in other populations. This is likely to be determined by future long-term, population-based studies, not by a re-evaluation of the data available now.
The underlying cost and infrastructure problem that ECG and echocardiographic screening programs produce remains unaddressed by the recent literature, except for a few small studies that have started to look at alternative technology approaches to ECG screening. These technologies are not yet ready for prime-time.
KEY POINTS.
The rate of previously undiagnosed cardiac disease carrying an elevated risk of sudden death in young athletes is approximately 0.4%.
ECGs detect pathology that a history-and-physical approach fails to identify, but data continue to show variability in the estimate of the incremental or replacement value compared to history and physical. Barriers to practical implementation remain unsolved in the United States.
Novel hardware and software technologies for ECG screenings continue to be developed, but are not yet ready for widespread adoption.
FINANCIAL SUPPORT AND SPONSORSHIP
This work was supported in part by the National Institutes of Health, National Heart, Lung and Blood Institute, grant number K23HL130554 and the American Heart Association, grant number 17MCPRP33660457.
Footnotes
CONFLICTS OF INTEREST
Dr. Webster is the recipient of research grants from the National Institutes of Health, National Heart, Lung and Blood Institute and the American Heart Association. The other authors have no conflicts of interest to report.
REFERENCES
- 1.Maron BJ. Sudden death in young athletes. Lessons from the Hank Gathers affair. N Engl J Med. 1993;329(1):55–7. [DOI] [PubMed] [Google Scholar]
- 2.Corrado D, Pelliccia A, Bjornstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(5):516–24. [DOI] [PubMed] [Google Scholar]
- 3.Jonas DE, Reddy S, Middleton JC, et al. Screening for Cardiovascular Disease Risk With Resting or Exercise Electrocardiography: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;319(22):2315–28. [DOI] [PubMed] [Google Scholar]
- 4.Aziz PF, Berger S, Kowey P, et al. The Second Annual Think Tank on Prevention of Sudden Cardiac Death in the Young: Developing a rational, reliable, and sustainable national health care resource. A report from the Cardiac Safety Research Consortium. Am Heart J. 2018;202:104–8. [DOI] [PubMed] [Google Scholar]
- 5.Maron BJ, Friedman RA, Kligfield P, et al. Assessment of the 12-Lead Electrocardiogram as a Screening Test for Detection of Cardiovascular Disease in Healthy General Populations of Young People (12–25 Years of Age): A Scientific Statement From the American Heart Association and the American College of Cardiology. JACC. 2014;64(14):1479–514. [DOI] [PubMed] [Google Scholar]
- 6.Kaltman JR, Thompson PD, Lantos J, et al. Screening for sudden cardiac death in the young: report from a national heart, lung, and blood institute working group. Circulation. 2011;123(17):1911–8. [DOI] [PubMed] [Google Scholar]
- 7.Mahle WT, Sable CA, Matherne PG, et al. Key concepts in the evaluation of screening approaches for heart disease in children and adolescents: a science advisory from the American Heart Association. Circulation. 2012;125(22):2796–801. [DOI] [PubMed] [Google Scholar]
- 8.Malhotra A, Dhutia H, Finocchiaro G, et al. Outcomes of Cardiac Screening in Adolescent Soccer Players. N Engl J Med. 2018;379(6):524–34. [DOI] [PubMed] [Google Scholar]; ** This comprehensive report from a large screening program reported an unusually high rate of sudden death (6.8/100,000 athletes).
- 9.Williams EA, Pelto HF, Toresdahl BG, et al. Performance of the American Heart Association ( AHA ) 14-Point Evaluation Versus Electrocardiography for the Cardiovascular Screening of High School Athletes: A Prospective Study. Am Heart J. 2019;8(14):e012235. [DOI] [PMC free article] [PubMed] [Google Scholar]; ** This comparison of ECG versus the AHA screening program is from an experienced program and attempts to illustrate the differences between the two controversal approaches in the United States.
- 10.Calo L, Martino A, Tranchita E, et al. Electrocardiographic and echocardiographic evaluation of a large cohort of peri-pubertal soccer players during pre-participation screening. Eur J Prev Cardiol. 2019:0(00) 1–12. [DOI] [PubMed] [Google Scholar]; * This European assessment was most notable for its attempt to incorporate echocardiographic screening.
- 11.Assanelli D, Levaggi R, Carre F, et al. Cost-effectiveness of pre-participation screening of athletes with ECG in Europe and Algeria. Intern Emerg Med. 2015;10(2):143–50. [DOI] [PubMed] [Google Scholar]
- 12.Leslie LK, Cohen JT, Newburger JW, et al. Costs and benefits of targeted screening for causes of sudden cardiac death in children and adolescents. Circulation. 2012;125(21):2621–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halkin A, Steinvil A, Rosso R, et al. Preventing sudden death of athletes with electrocardiographic screening: what is the absolute benefit and how much will it cost? JACC. 2012;60(22):2271–6. [DOI] [PubMed] [Google Scholar]
- 14.Malhotra R, West JJ, Dent J, et al. Cost and yield of adding electrocardiography to history and physical in screening Division I intercollegiate athletes: a 5-year experience. Heart rhythm. 2011;8(5):721–7. [DOI] [PubMed] [Google Scholar]
- 15.Wheeler MT, Heidenreich PA, Froelicher VF, et al. Cost-effectiveness of preparticipation screening for prevention of sudden cardiac death in young athletes. Ann Intern Med. 2010;152(5):276–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corrado D, Basso C, Pavei A, et al. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296(13):1593–601. [DOI] [PubMed] [Google Scholar]
- 17.Steinvil A, Chundadze T, Zeltser D, et al. Mandatory electrocardiographic screening of athletes to reduce their risk for sudden death proven fact or wishful thinking? JACC. 2011;57(11):1291–6. [DOI] [PubMed] [Google Scholar]
- 18.Maron BJ, Doerer JJ, Haas TS, et al. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119(8):1085–92. [DOI] [PubMed] [Google Scholar]
- 19.Berger S, Utech L, Fran Hazinski M. Sudden death in children and adolescents. Pediatr Clin North Am. 2004;51(6):1653–77, ix-x. [DOI] [PubMed] [Google Scholar]
- 20.Waller BF, Hawley DA, Clark MA, Pless JE. Incidence of sudden athletic deaths between 1985 and 1990 in Marion County, Indiana. Clin Cardiol. 1992;15(11):851–8. [DOI] [PubMed] [Google Scholar]
- 21.Burns KM, Bienemann L, Camperlengo L, et al. The Sudden Death in the Young Case Registry: Collaborating to Understand and Reduce Mortality. Pediatrics. 2017;139(3). [DOI] [PMC free article] [PubMed] [Google Scholar]; * This paper provides a description of the methods that are being used to compile a population incidence for sudden death in the young in the United States, supervised by the National Institutes of Heath and the Centers for Disease Control.
- 22.Malhotra A, Dhutia H, Yeo TJ, et al. Accuracy of the 2017 international recommendations for clinicians who interpret adolescent athletes’ ECGs: a cohort study of 11 168 British white and black soccer players. Br J Sports Med. 2019;0:1–8. [DOI] [PubMed] [Google Scholar]; ** This study is a follow-up to the 2018 New England Journal of Medicine article and provides extensive subgroup analysis as well as a comparison between the four most prevalent tools for reading ECGs in the screening setting.
- 23.Corrado D, Pelliccia A, Heidbuchel H, et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J. 2010;31(2):243–59. [DOI] [PubMed] [Google Scholar]
- 24.Drezner JA, Ackerman MJ, Anderson J, et al. Electrocardiographic interpretation in athletes: the ‘Seattle criteria’. Br J Sports Med. 2013;47(3):122–4. [DOI] [PubMed] [Google Scholar]
- 25.Sheikh N, Papadakis M, Ghani S, et al. Comparison of electrocardiographic criteria for the detection of cardiac abnormalities in elite black and white athletes. Circulation. 2014;129(16):1637–49. [DOI] [PubMed] [Google Scholar]
- 26.Sharma S, Drezner JA, Baggish A, et al. International recommendations for electrocardiographic interpretation in athletes. Eur Heart J. 2018;39(16):1466–80. [DOI] [PubMed] [Google Scholar]; ** This is the newest revision of ECG screening guidelines and represents an attempt to combine the strengths of the various methods in both the United States (the Seattle Criteria) and Europe (the ESC guidelines).
- 27.Maron BJ, Thompson PD, Maron MS. There is No Reason to Adopt ECG s and Abandon American Heart Association/American College of Cardiology History and Physical Screening for Detection of Cardiovascular Disease in the Young. Am Heart J. 2019;8(14):e013007. [DOI] [PMC free article] [PubMed] [Google Scholar]; * This editorial provides a counterpoint to the Williams study above, but does not provide novel data.
- 28.Sia CH, Dalakoti M, Tan BYQ, et al. A Population-wide study of electrocardiographic (ECG) norms and the effect of demographic and anthropometric factors on selected ECG characteristics in young, Southeast Asian males-results from the Singapore Armed Forces ECG (SAFE) study. Ann Noninvasive Electrocardiol. 2019;24(3):e12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Movahed MR, Sattur S, Bates S. Higher Prevalence of Abnormal Electrocardigrams (ECG) in African Americans Undergoing Screening ECG and Echocardiography. Crit Pathw Cardiol. 2019;18(2):86–8. [DOI] [PubMed] [Google Scholar]; * This report from a volunteer-based organization provides community-derived data on screening ECGs.
- 30.Karacan M, Celik N, Gul EE, et al. Validation of a smartphone-based electrocardiography in the screening of QT intervals in children. North Clin Istanb. 2019;6(1):48–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hannun AY, Rajpurkar P, Haghpanahi M, et al. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat Med. 2019;25(1):65–9. [DOI] [PMC free article] [PubMed] [Google Scholar]; ** This is a sophisticated extension of prior work in deep neural netowrks and continues to attempt to separate the work of interpreting ECGs from the hands of individual cardiologists.
- 32.Campbell M, Zhou X, Han C, et al. Pilot study analyzing automated ECG screening of hypertrophic cardiomyopathy. Heart rhythm. 2017. [DOI] [PubMed] [Google Scholar]
- 33.Modaff DS, Hegde SM, Wyman RA, Rahko PS. Usefulness of Focused Screening Echocardiography for Collegiate Athletes. Am J Cardiol. 2019;123(1):169–74. [DOI] [PubMed] [Google Scholar]; * This is a report of an echocardiographic screening effort used in nearly 3,000 athletes using a well-designed 5-minute echocardiogram protocol.
- 34.Grazioli G, Merino B, Montserrat S, et al. Usefulness of echocardiography in preparticipation screening of competitive athletes. Rev Esp Cardiol (English ed). 2014;67(9):701–5. [DOI] [PubMed] [Google Scholar]
- 35.Rizzo M, Spataro A, Cecchetelli C, et al. Structural cardiac disease diagnosed by echocardiography in asymptomatic young male soccer players: implications for pre-participation screening. Br J Sports Med. 2012;46(5):371–3. [DOI] [PubMed] [Google Scholar]
- 36.Baggish AL, Hutter AM Jr., Wang F, et al. Cardiovascular screening in college athletes with and without electrocardiography: A cross-sectional study. Ann Intern Med. 2010;152(5):269–75. [DOI] [PubMed] [Google Scholar]
- 37.Gerling S, Loose O, Zant R, et al. Echocardiographic diagnosis of congenital coronary artery abnormalities in a continuous series of adolescent football players. Eur J Prev Cardiol. 2019;26(9):988–94. [DOI] [PubMed] [Google Scholar]; * This is a report of an echocardiographic screening effort, focused on coronary abnormalities.
- 38.Nalliah CJ, Mahajan R, Elliott AD, et al. Mitral valve prolapse and sudden cardiac death: a systematic review and meta-analysis. Heart. 2019;105(2):144–51. [DOI] [PubMed] [Google Scholar]
- 39.Darche JP, Murray MJ, Bridges KM, et al. Assessing the utility of yearly pre-season laboratory screening for athletes on a major professional sports team. J Sci Med Sport. 2019;22(4):484–7. [DOI] [PubMed] [Google Scholar]; * This report from a major sports team provides quantitative evidence that laboratory screening does not identify an elevated risk of sudden death.
- 40.Pechmajou L, Sharifzadehgan A, Bougouin W, et al. Does occurrence during sports affect sudden cardiac arrest survival? Resuscitation. 2019;141:121–7. [DOI] [PubMed] [Google Scholar]; ** This article reports outcomes in a large, community-based secondary prevention effort in France.
- 41.Tsuda T, Geary EM, Temple J. Significance of automated external defibrillator in identifying lethal ventricular arrhythmias. Eur J Pediatr. 2019. Published online 11 July 2019 [DOI] [PubMed] [Google Scholar]; * This article reinforces the need to obtain tracings from automated external defibrillators after a successful secondary prevention intervention.
- 42.Heron M Deaths: Leading Causes for 2016. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2018;67(6):1–77. [PubMed] [Google Scholar]
- 43.Drezner JA, Owens DS, Prutkin JM, et al. Electrocardiographic Screening in National Collegiate Athletic Association Athletes. Am J Cardiol. 2016;118(5):754–9. [DOI] [PubMed] [Google Scholar]
- 44.Dhutia H, Malhotra A, Gabus V, et al. Cost Implications of Using Different ECG Criteria for Screening Young Athletes in the United Kingdom. JACC. 2016;68(7):702–11. [DOI] [PubMed] [Google Scholar]
- 45.Basavarajaiah S, Wilson M, Whyte G, et al. Prevalence of hypertrophic cardiomyopathy in highly trained athletes: relevance to pre-participation screening. JACC. 2008;51(10):1033–9. [DOI] [PubMed] [Google Scholar]
- 46.Wilson MG, Basavarajaiah S, Whyte GP, et al. Efficacy of personal symptom and family history questionnaires when screening for inherited cardiac pathologies: the role of electrocardiography. Br J Sports Med. 2008;42(3):207–11. [DOI] [PubMed] [Google Scholar]
- 47.Fuller CM, McNulty CM, Spring DA, et al. Prospective screening of 5,615 high school athletes for risk of sudden cardiac death. Med Sci Sports Exerc.1997;29(9):1131–8. [DOI] [PubMed] [Google Scholar]


