Summary
Excessive access to fast‐food restaurants (FFRs) in the neighbourhood is thought to be a risk factor for childhood obesity by discouraging healthful dietary behaviours while encouraging the exposure to unhealthful food venues and hence the compensatory intake of unhealthy food option. A literature search was conducted in the PubMed, Web of Science, and Embase for articles published until 1 January 2019 that analysed the association between access to FFRs and weight‐related behaviours and outcomes among children aged younger than 18. Sixteen cohort studies and 71 cross‐sectional studies conducted in 14 countries were identified. While higher FFR access was not associated with weight‐related behaviours (eg, dietary quality score and frequency of food consumption) in most studies, it was commonly associated with more fast‐food consumption. Despite that, insignificant results were observed for all meta‐analyses conducted by different measures of FFR access in the neighbourhood and weight‐related outcomes, although 17 of 39 studies reported positive associations when using overweight/obesity as the outcome. This systematic review and meta‐analysis revealed a rather mixed relationship between FFR access and weight‐related behaviours/outcomes among children and adolescents.
Keywords: dietary behaviour, fast food, food environment, obesity
1. INTRODUCTION
Obesity is a major risk factor for global mortality, with an estimated 2.8 million people died of obesity‐related causes each year. 1 Obesity can lead to a variety of health consequences, including heart disease, stroke, diabetes mellitus, hypertension, dyslipidaemia, breathing disorders, and certain types of cancer. 2 In 2016, the World Health Organization (WHO) reported that 39% of adults had obesity, whereas the obesity rate in 1975 was only around 3% in men and 6% in women. 1 However, a considerable proportion of adult obesity stem from childhood, which, therefore, is a critical period to prevent obesity. 3 , 4 Childhood obesity is one of the most serious global public health problems in the 21st century. The prevalence of overweight and obesity in children and adolescents has risen dramatically from 4% in 1975 to over 18% in 2016. 5 Childhood obesity can also lead to a range of health problems, including high blood pressure, high total cholesterol, and impaired glucose tolerance. Prevention of childhood obesity requires high priority in public health practices.
It is widely accepted that some environmental factors in the neighbourhood may interact with personal characteristics to affect individual weight status. 6 , 7 Fast‐food restaurants (FFRs) are one of such environmental factors, which are defined as food venues primarily engaged in providing food services (except snack and non‐alcoholic beverage bars) where patrons generally order or select items and pay before eating. They allow convenient consumption of fast food that typically contains high levels of calories, saturated fat, trans‐fat, sugar, simple carbohydrates, and sodium, sold at a relatively low price. FFRs can be categorized using Standard Industrial Classification (SIC) code (5812002) or North America Industry Classification System (NAICS) code (722513) under the category of limited‐service restaurants. 8 With the rapid development of international fast‐food chains, the consumption of fast food has risen dramatically over the past few decades along with the increasing obesity rates globally. 9 , 10 Moreover, fast food has been more popular among children and adolescents, partly due to easy availability, taste, and marketing strategies. 11 Some studies showed that FFR access may potentially lead to greater risk of being overweight and obesity, especially in children and adolescents. 12 However, compared with the evidence suggesting an association between fast‐food consumption and weight gain, 13 the association between FFR access and childhood obesity was less clear.
This systematic review comprehensively investigated the association between FFR access and weight‐related behaviours and weight status. We tested our hypothesis that the greater FFR access was associated with higher levels of unhealthful food intake and weight gains among children and adolescents. Studies that use a full range of measures of FFR access in the neighbourhood and examine multiple weight‐related behaviours and outcomes were included. Furthermore, meta‐analyses were conducted to quantify the association between FFR access and childhood obesity.
2. METHODS
A systematic review and meta‐analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses.
2.1. Study selection criteria
Studies that met all of the following criteria were included in the review: (a) study subjects (children and adolescents aged younger than 18); (b) study outcomes (weight‐related behaviours [eg, diet, physical activity, and sedentary behaviour] and/or outcomes [eg, overweight and obesity measured by body mass index (BMI, kg/m2), waist circumference, waist‐to‐hip ratio, and body fat]); (c) article types (peer‐reviewed original research); (d) time of publication (earlier than 1 January 2019); and (5) language (articles written in English).
Studies that met any of the following criteria were excluded from the review: (1) studies that incorporated no measures of FFR access or weight‐related behaviours/outcomes; (2) computer‐based simulation studies without the inclusion of human participants; (3) controlled experiments conducted in manipulated rather than naturalistic settings; (4) articles not written in English; or (5) letters, editorials, study/review protocols, or review articles.
2.2. Search strategy
A keyword search was performed in three electronic bibliographic databases: PubMed, Web of Science, and Embase. The search strategy included all possible combinations of keywords from the three groups related to fast‐food restaurant, children, and weight‐related behaviours or outcomes. The specific search strategy is provided in Appendix A.
Two reviewers (M.L. and Y.L.) independently conducted the title and abstract screening and identified potentially relevant articles for the full‐text review. Inter‐rater agreement was assessed by using the Cohen kappa (κ = 0.8). Discrepancies were compiled by M.L. and screened by a third reviewer (P.J.). M.L., Y.L., and PJ. jointly determined the list of articles for the full‐text review through discussion. Then M.L. and Y.L. independently reviewed the full texts of all articles in the list and determined the final pool of articles included in the review. Inter‐rater agreement was again assessed by the Cohen kappa (κ = 0.9). [Correction added on 14 January 2021, after first online publication: the title of Section 2.2 has been amended to ‘Search Strategy’.]
2.3. Data extraction
Two reviewers (M.L. and Y.L.) independently extracted data from each included study, and discrepancies were resolved by the third reviewer (P.J.). A standardized data extraction form was used to collect methodological and outcome variables from each selected study, including authors, year of publication, study area and scale, sample size and characteristics, statistical models, and age at baseline, follow‐up years, number of repeated measures, and attrition rate for cohort studies, as well as measures of FFR access, weight‐related behaviours/outcomes, and their association.
2.4. Meta‐analysis
A meta‐analysis was performed to estimate the pooled effect size of FFR access on each weight‐related behaviour and outcomes. Weight‐related outcomes included BMI, BMI percentile, BMI z‐score, overweight, and obesity. Overweight was defined as BMI at or above the 85th percentile, and obesity was defined as BMI at or above the 95th percentile based on references mentioned in each article. Several studies were excluded from the meta‐analysis due to the following reasons: neither standard error nor confidence interval (CI) was reported; effect size was unable to be transformed into a standardized coefficient (ie, beta coefficient) due to limited information reported; the unit of effect size was inconsistent with others; and less than two studies reported the same outcome variable.
Effect sizes were reported by mean differences for continuous outcomes (ie, BMI and BMI percentile) and odds ratios for categorical variables (ie, overweight and obesity). Study heterogeneity was assessed by using the I 2 index. The level of heterogeneity represented by I 2 was interpreted as modest (I 2 ≤ 25%), moderate (25% < I 2 ≤ 50%), substantial (50% < I 2 ≤ 75%), or considerable (I 2 > 75%). Q tests were also conducted, where P < .1 indicates the presence of heterogeneity across studies. A random‐effect model was used to pool the estimates from individual studies because of the varying population and criteria used to define outcomes. Publication bias was assessed by a visual inspection of the funnel plot and Begg's and Egger's tests. All meta‐analyses were performed by the “meta” and “metagen” packages using R version 4.3‐2. 14 All analyses used two‐sided tests, and P < .05 was considered statistically significant except for the evaluation of heterogeneity (P < .1).
2.5. Study quality assessment
The quality of included studies was assessed using the National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies. 15 This assessment tool rates each study based on 14 criteria (Table S2). For each criterion, a score of one was assigned if “yes” was the response, whereas a score of zero was assigned otherwise (ie, an answer of “no,” “not applicable,” “not reported,” or “cannot determine”). A study‐specific global score ranging from zero to 14 was calculated by summing up scores across all criteria. The study quality assessment helped measure the strength of scientific evidence but was not used to determine the inclusion of studies.
3. RESULTS
3.1. Study selection
A total of 1441 articles were identified through the keyword search, of which 66 were non‐duplicated articles (Figure 1). After title and abstract screening, 575 articles were excluded. The full texts of the remaining 111 articles were reviewed against the study selection criteria, and 24 articles were further excluded. The remaining 87 studies that examined the association between FFR access and children's weight‐related behaviours and/or outcomes were included in this review.
FIGURE 1.
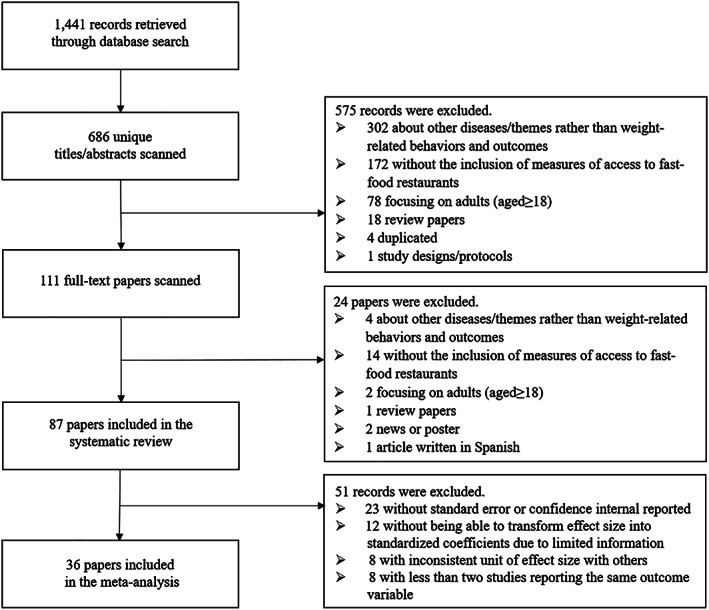
Flowchart of study inclusion and exclusion
3.2. Study characteristics
Eighty‐seven included studies consisted of 16 cohort studies and 71 cross‐sectional studies and were published during 2004 to 2018 (Table 1). Most of these studies were conducted in the United States (n = 45); one international comparison study was conducted in the United States, Canada, and Scotland; the remaining studies were conducted in Canada (n = 13), the United Kingdom (n = 10), China (n = 4), Australia (n = 3), South Korea (n = 3), Denmark (n = 2), Brazil (n = 1), France (n = 1), Germany (n = 1), Ireland (n = 1), New Zealand (n = 1), and Sweden (n = 1). Twenty of these studies were conducted at a national level, and 26, 32, and nine studies were conducted at state, city, and county levels, respectively. The sample size of included studies ranged widely from 78 to 3 003 288, and school children/adolescents were the most common study population (n = 54).
TABLE 1.
Basic characteristics of 87 included studies
| Author (Year)[ref] a | Study Area [Scale] b | Sample Size | Sample Age (Years, range, and/or mean ± SD) c | Sample Characteristics | Statistical Models |
|---|---|---|---|---|---|
| Longitudinal studies | |||||
| Chen (2016) 27 | Arkansas, USA [S] | 21 639 | in 2003–2004 | School children (followed up from academic year 2003/2004 to 2009/2010 with seven repeated measures) | Growth curve model and cox regression |
| Chen (2016) 28 | USA [N] | 7090 | 11 in 2004 | School children (followed up from 2004 to 2007 with two repeated measures) | Multilevel linear regression |
| Fraser (2012) 29 | Avon, UK [CT] | 4022 | 13 y | Adolescents (followed up from 13 to 15 y with two repeated measures and an attrition rate of 21.2%) | Linear and logistic regression |
| Ghenadenik (2018) 30 | Montreal, Canada [C] | 391 | 8‐10 in 2005‐2008 | Children with a parental history of obesity (followed up from 2005‐2008 to 2008‐2011 with two repeated measures and an attrition rate of 37.9%) | Multivariate linear regression |
| Green (2018) 31 | Leeds, UK [C] | 746 | 11‐12 in 2005 | Secondary school students (followed up from 2005 to 2010 with three repeated measures) | Multilevel linear regression |
| Hamano (2017) 32 | Sweden [N] | 944 487 | 0‐14 in 2005 | Entire Swedish population (followed up from 2005 to 2010 with two repeated measures) | Multilevel logistic regression |
| Khan (2012) 33 | USA [N] | 11 700 | in 2004 | School children (followed up from 2004 to 2007 with two repeated measures) | Multilevel linear regression |
| Lee (2012) 34 | USA [N] | 7710 | 6.2 ± 0.4 in 1999 | School children (follow up from 1999 to 2004 with four repeated measures and an attrition rate of 43.0%) | Multilevel linear regression |
| Leung (2011) 35 | California, USA [CT4] | 353 | 6‐7 in 2005 | Girls (followed up from 2005 to 2008 with three repeated measures and an attrition rate of 20.5%) | Generalized linear and logistic regression |
| Pearce (2018) 36 | Gloucestershire, UK [CT] | 1577 | in 2006‐2007 | School children (followed up from 2006/2007 to 2012/2013 with two repeated measures and an attrition rate of 34.4%) | Multivariate logistic regression |
| Powell (2009) 37 | USA [N] | 5215 | 12‐17 (15.5 ± 1.7) in 1997 | Adolescents living at home (followed up from 1997 to 2000 with four repeated measures) | Multilevel linear regression |
| Shier (2012) 38 | USA [N] | 6260 | in 2004 | School children (followed up from 2004 to 2007 with two repeated measures) | Multilevel linear regression |
| Smith (2013) 39 | London, UK [C] | 757 | 11‐12 in 2001 | Secondary school students (followed up from 2001 to 2005 with two repeated measures and an attrition rate of 45.2%) | Generalized linear regression |
| Sturm (2005) 40 | USA [N] | 6918 | 6.2 ± 0.4 in 1999 | Elementary school children (followed up from 1999 to 2002 with three repeated measures and an attrition rate of 42.4%) | Multilevel linear regression |
| Van Hulst (2015) 41 | Quebec, Canada [S] | 512 | 8‐10 in 2005‐2008 | Children with a parental history of obesity (followed up from 2005‐2008 to 2008‐2011 with two repeated measures and an attrition rate of 9.8%) | Multivariate linear regression |
| Wang (2012) 42 | China [N] | 185 | 6‐18 in 2004 | School‐age children (followed up from 2004 to 2006 with two repeated measures and an attrition rate of 19%) | Multilevel linear regression |
| Cross‐sectional studies | |||||
| Alviola (2014) 43 | Arkansas, USA [S] | 942 public schools | in 2008‐2009 | Children in kindergarten, grades 2, 4, 6, 8, and 10 | Multivariate linear regression |
| An (2012) 44 | California, USA [S] | 13 462 | 8226 aged 5‐11 and 5236 aged 12‐17 in 2005 and 2007 | Measured in 2005 and 2007 | Negative binomial regression |
| Bader (2013) 45 | New York City, USA [C] | 94 348 | ≥13 y in 2007‐2008 | Public high school students | Generalized multilevel linear regression |
| Baek (2014) 46 | California, USA [S] | 926 018 | in 2007 | Grades 5, 7, and 9 students | Multilevel linear regression |
| Barrett (2017) 47 | Hampshire, UK [CT] | 1173 | 6 y between 2007 and 2014 | NA | Multilevel linear regression |
| Burdette (2004) 48 | Cincinnati, Ohio, USA [C] | 7020 | 36‐59 months in 1998‐2001 | Low‐income preschool children | Multivariate logistic regression |
| Carroll‐Scott (2013) 49 | New Haven, USA [C] | 1048 | 10.9 ± 0.8 in 2009 | Grades 5 and 6 students | Multilevel linear regression |
| Casey (2012) 50 | Bas‐Rhin, France [S] | 3327 | 12.0 ± 0.6 in 2001 | Middle‐school first‐level students | Multilevel logistic regression |
| Cetateanu (2014) 51 | UK [N] | 3 003 288 | 4‐5 and 10‐11 in 2007‐2010 | School Reception and Grade 6 children | Multivariate linear regression |
| Chiang (2011) 52 | Taiwan [S] | 2283 | 6‐13 in 2001‐2002 | Elementary school children |
Multivariate linear regression |
| Choo (2017) 20 | Seoul, South Korea [C] | 126 | 9‐12 in 2015 | Elementary school children at Grades 4 to 6 |
Multivariate logistic regression |
| Clark (2014) 53 | Otago, New Zealand [S] | 664 | 15‐18 in 2011 | Grades 11‐13 adolescents | Generalized estimating equation |
| Correa (2018) 54 | Florianopolis, Brazil [C] | 2195 | 7‐14 in 2012‐2013 | School children | Multivariate logistic regression |
| Crawford (2008) 55 | Melbourne, Australia [C] | 380 | 137 aged 8‐9 and 243 aged 13‐15 in 2004 | Schoolchildren | Linear and logistic regression |
| Cutumisu (2017) 56 | Quebec, Canada [S] | 26 655 | in 2010‐2011 | Secondary school children | Multilevel logistic regression |
| Davis (2009) 57 | California, USA [S] | 529 367 | in 2002‐2005 | Middle and high school students | Linear and logistic regression |
| Dwicaksono (2018) 58 | New York, USA [S] | 680 school districts | in 2010‐2012 | School‐aged children | Multivariate linear regression |
| Fiechtner (2013) 59 | Massachusetts, USA [S] | 438 | 2‐6.9 in 2006‐2009 | Overweight and obese preschool‐age children | Multivariate linear regression |
| Fiechtner (2015) 60 | Massachusetts, USA [S] | 49 770 | 4‐18 in 2011‐2012 | Paediatric patients | Multivariate linear regression |
| Forsyth (2012) 61 |
Minneapolis/St. Paul, USA [C] |
2724 | 14.5 ± 2.0 in 2009‐2010 | Adolescents in secondary schools | Multilevel linear regression |
| Fraser (2010) 62 | Leeds, West Yorkshire, UK [C] | 33 594 | 3‐14 in 1998‐2006 | NA | Generalized estimating equation |
| Galvez (2009) 63 | New York, USA [C] | 323 | 6‐8 in 2004 | NA | Multivariate logistic regression |
| Gilliland (2012) 64 | London, UK [C] | 891 | 10‐14 y | Grades 6‐8 students | Multilevel linear regression |
| Gorski Findling (2018) 65 | USA [N] | 3748 | 2‐18 in 2012‐2013 | NA | Logistic regression |
| He (2012) 66 | London, Ontario, Canada [C] | 782 | 11‐13 in 2006‐2007 | Grades 7 and 8 students |
Multilevel logistic regression |
| He (2012) 67 | London, Ontario, Canada [C] | 632 | 11‐14 in 2006‐2007 | Grades 7 and 8 students | Multilevel linear regression |
| Hearst (2012) 68 | Minneapolis and St Paul, MN, USA [C2] | 634 | 10.8‐17.7 in 2007‐2008 | Adolescents |
Multilevel linear regression |
| Heroux (2012) 69 | Canada, Scotland, and the USA [N3] | 26 778 | 13‐15 in 2009‐2010 | Students |
Multilevel logistic regression |
| Ho (2010) 70 | Hong Kong, China [S] | 24 796 | 14.5 ± 0.11 in 2006‐2007 | Secondary school students | Logistic regression |
| Hobin (2013) 71 | Ontario, Canada [S] | 21 754 | in 2005‐2006 | Grades 9 to 12 students in secondary schools |
Multilevel linear regression |
| Howard (2011) 72 | California, USA [S] | 879 public schools | in 2007 | Grade 9 students in public schools | Multivariate linear regression |
| Jago (2007) 73 | Houston, USA [C] | 204 | 10‐14 in 2003 | Boy scouts | Multivariate linear regression |
| Jilcott (2011) 74 | Pitt County, USA [CT] | 744 | 8‐18 (12.9 ± 2.5) in 2007‐2008 | Paediatric patients | Generalized linear regression |
| Joo (2015) 75 | Suwon, Hwaseong, and Osan, Korea [C3] | 243 | in 2012 | Grades 6 and 8 students | Chi‐square test and t test |
| Kelly (2018) 76 | Ireland [N] | 5344 | in 2010 | Post‐primary school students | Logistic regression |
| Kepper (2016) 77 | Louisiana, USA [S] | 78 | 2‐5 (2.9 ± 0.7) y | Pre‐school children | Multivariate linear regression |
| Koleilat (2012) 78 | Los Angeles, USA [CT] | 266 ZIP codes | 3‐4 in 2008 | Children who participated in the WIC programme | ANOVA |
| Lakes (2016) 79 | Berlin, Germany [C] | 28 159 | 5‐6 in 2012 | Preschool children | Multivariate linear regression |
| Lamichhane (2012) 80 | South Carolina, USA [S] | 359 | 14.5 ± 2.9 in 2001‐2005 | Youth with diabetes | Generalized estimating equation |
| Lamichhane (2012) 81 | South Carolina, USA [S] | 845 | 11.7 ± 4.7 in 2001‐2006 | Youth with diabetes | Generalized estimating equation |
| Langellier (2012) 82 | Los Angeles, USA [CT] | 1694 schools | in 2008‐2009 | Grades 5, 7, and 9 students | Multilevel linear regression |
| Larsen (2015) 83 | Toronto, Canada [C] | 943 | 11.02 ± 9.63 in 2010‐2011 | Grades 5 and 6 students | Logistic regression |
| Laska (2010) 84 | Minneapolis, USA [C] | 349 | 11‐18 (15.4 ± 1.7) in 2006‐2007 | Adolescents | Multilevel linear regression |
| Laxer (2014) 85 | Canada [N] | 6099 | 11‐15 in 2009‐2010 | Grades 6‐10 students |
Multilevel logistic regression |
| Le (2016) 86 | Saskatoon, Canada [C] | 1221 | 10‐14 in 2011 | Elementary school students | Logistic regression |
| Leatherdale (2011) 87 | Ontario, Canada [S] | 1207 | Grades 5‐8 in 2007‐2008 | School children at grades 5‐8 | Multilevel logistic regression |
| Li (2011) 88 | Xi'an, China [C] | 1792 | 11‐17 in 2004 | Junior high students | Multilevel linear regression |
| Liu (2007) 89 | Marion, Indiana, USA [CT] | 7334 | 3‐18 in 2000 | Children for routine well‐child care | Logistic regression |
| Longacre (2012) 90 | New Hampshire and Vermont, USA [S2] | 1547 | 12‐18 in 2007‐2008 | Grades 7‐11 students | Poisson regression |
| Mellor (2011) 91 | Virginia, USA [S] | 2023 | 11.4 ± 1.7 in 2006 | Grades 3, 6, and 7 students | Linear and logistic regression |
| Miller (2014) 92 | Perth, Australia [C] | 1850 | 5‐15 in 2005‐2010 | NA | Logistic regression |
| Ohri‐Vachaspati (2015) 93 | New Jersey, USA [S] | 560 | 3‐18 years in 2009‐2010 | NA | Multivariate logistic regression |
| Oreskovic (2009) 94 | Massachusetts, USA [S] | 6680 | 2‐18 in 2006 |
Children from a Partners HealthCare outpatient affiliate |
Multilevel logistic regression |
| Oreskovic (2009) 95 | Massachusetts, USA [S] | 21 008 | 2‐18 in 2006 |
Children from a Partners HealthCare outpatient affiliate |
Multilevel logistic regression |
| Pabayo (2012) 96 | Edmonton, Canada [C] | 1760 | 4‐5 in 2005‐2007 | Pre‐school children | Multivariate logistic regression |
| Park (2013) 97 | Seoul, South Korea [C] | 939 | 12.1 ± 1.8 in 2011 | Grades 4‐9 students | Generalized estimating equation |
| Powell (2009) 98 | USA [N] | 6594 | 6‐17 (12.0 ± 3.2) in 1998, 2000, and 2002 | NA | Multilevel linear regression |
| Powell (2011) 99 | USA [N] | 1134 | 12‐18 (14.8 ± 1.9) in 1997 and 2002‐2003 | (measured in 1997 and 2002‐2003) | Multivariate linear regression |
| Salois (2012) 100 | USA [N] | 2192 counties | 2‐4 in 2007‐2009 | Low‐income preschool children | Multivariate linear regression |
| Sanchez (2012) 101 | California, USA [S] | 926 018 | in 2007 | Grades 5, 7, and 9 students | Multilevel logistic regression |
| Seliske (2009) 102 | Canada [N] | 7281 | 11‐16 in 2005‐2006 | Grades 6‐10 students | Multilevel logistic regression |
| Shareck (2018) 103 | London, UK [C] | 3089 | 13‐15 in 2014 | Year 9 students in secondary schools | Poisson regression |
| Shier (2016) 104 | USA [N] | 903 | 12‐13 in 2013 | Children in military families | Multivariate linear regression |
| Svastisalee (2012) 105 | Denmark [N] | 6034 | 11‐15 in 2006 | Grades 5, 7, and 9 students | Multilevel logistic regression |
| Svastisalee (2016) 106 | Denmark [N] | 4642 | 11‐15 in 2010 | Grades 5, 7, and 9 students | Multilevel logistic regression |
| Tang (2014) 107 | New Jersey, USA [C4] | 12 954 | 13.5 ± 3.5 in 2008‐2009 | Middle and high school students in low‐income communities | Multilevel linear regression |
| Timperio (2008) 108 | Melbourne and Geelong, Australia [C2] | 801 | 340 aged 5‐6 and 461 aged 10‐12 in 2002‐2003 | School children | Logistic regression |
| Van Hulst (2012) 109 | Quebec, Canada [C] | 512 | 8‐10 in 2005‐2008 | Grades 2‐5 students | Logistic regression and generalized estimating equation |
| Wall (2012) 110 | Minneapolis/St. Paul, USA [C] | 2682 | 14.5 ± 2.0 in 2009‐2010 | Public middle and high school students | Multivariate linear regression |
| Wasserman (2014) 111 | Kansas, USA [C2] | 12 118 | 4‐12 in 2008‐2009 | Elementary school children | Multilevel linear regression |
| Williams (2015) 112 | Berkshire, UK [CT] | 16 956 | 4‐5 y and 10‐11 y in 2010‐2011 | Primary school children | Multilevel linear and logistic regression |
Abbreviation: NA, not available.
Studies included in meta‐analyses are in bold.
Study area: [N], national; [S], state (eg, in the United States) or equivalent unit (eg, province in China and Canada); [Sn], n states or equivalent units; [CT], county or equivalent unit; [CTn], n counties or equivalent units; [C], city; [Cn], n cities.
Sample age: age in baseline year for longitudinal studies or mean age in survey year for cross‐sectional studies.
3.3. Measures of FFR access
Access to FFRs was usually measured by the presence (n = 20), number (n = 50), and density (n = 23) of FFRs within various types of buffer zones and the distance to the nearest FFR (n = 28; Table S1). Other measures included the proportion of FFRs over all restaurants or food venues (n = 4) and weighted accessibility score (n = 3), which was calculated from measures of number and distance in the neighbourhood. Most of these measures used road‐network (n = 36) or straight‐line distance (n = 34) around the centroid of home (n = 56) and/or school (n = 34). Some studies also focused on home‐school travel route (n = 4) and community child centre (n = 1). Among studies that used measures within road‐network–based buffer zones, the radii of buffer zones ranged from 0.16 to 3.0 km, and the most commonly used ones were 0.8 (n = 13), 0.4 (n = 9), and 1.6 km (n = 7). In contrast, among studies that measured FFR access within straight‐line buffer zones, a greater range of radii, from 0.16 to 8.0 km, was observed, and the commonly used ones included 1.0 (n = 13), 0.8 (n = 8), and 1.6 km (n = 6). Other measures of buffer zones included 5 to 20 minutes' walking time (n = 3), postal zone (n = 4), and census tract (n = 5).
3.4. Measures of weight‐related behaviours and outcomes
Of the 87 included studies, 35 studies have used weight‐related behaviours as outcome variables, which were usually measured by food consumption (n = 33) and physical activity (n = 3). Measures of food consumption varied a lot across studies, including food consumption frequency (n = 23), dietary quality scores calculated based on food frequency questionnaire (n = 8), average daily nutrition intake (n = 2), food purchasing frequency (n = 2), and place having lunch (n = 1). Measures of physical activity included the time of exercise and time of sedentary behaviours.
Weight‐related outcomes were used in 61 studies, where measures included overweight/obesity (n = 37), BMI z‐score (n = 15), BMI (n = 10), BMI percentile (n = 6), BMI standard deviation score (SDS) (n = 2), waist circumference SDS (n = 1), height z‐score (n = 1), weight z‐score (n = 1), waist circumference z‐score (n = 1), waist circumference (n = 1), triceps skinfold thickness (TSF) z‐score (n = 1), waist‐height ratio (n = 1), weight gain (n = 1), and body fat percentage (n = 1). The BMI references used included the US Centers for Disease Control and Prevention (CDC) growth charts (n = 32), WHO growth reference (n = 3), UK BMI reference (n = 2), 2012 guidelines of Korea CDC (n = 1), and reference values of Kromeyer‐Haushild (n = 1). Most of weight‐related outcomes were objectively measured (n = 49), while some were self‐ or parent‐reported (n = 12).
3.5. FFR access and weight‐related behaviours
In terms of dietary behaviours related to FFR access, the most commonly studied types of food included fast food, fruit and vegetable, juice, and sugar‐sweetened beverages. Of the 14 studies analysing the frequency of fast‐food consumption, 11 studies reported a positive association between FFR access and fast‐food consumption, with this association observed only among boys in two studies; such association varied in rural (positive) and urban (negative) areas in one study, and the other two studies reported a null association. Nine of 14 studies examining FFR access and fruit/vegetable consumption reported a null association between them, while three reported a negative association and two reported a positive association. Two of five studies focusing on FFR access and juice consumption reported a negative association and the other three studies reported a null association. For the consumption of sugar‐sweetened beverages, five of eight studies reported null associations while three reported a positive association. Seven studies using a dietary quality score as the outcome variable reported positive (n = 2), negative (n = 3), and null (n = 2) associations with FFR access. No associations were found between FFR access and nutritional intake. In terms of physical (in)activity, most associations were not significant for both exercise (n = 2) and sedentary behaviours (n = 2), whereas one study reported a positive association for exercise.
3.6. FFR access and weight status
When using continuous weight measures as outcome variables (ie, BMI and BMI percentile/z‐score/SDS), the majority of the included cohort studies reported non‐significant associations with FFR access and weight‐related outcomes (n = 9), with only one study reporting a positive association. Half of the cohort studies using overweight/obesity as outcome variables reported a positive association (n = 3), while the other half reported non‐significant associations (n = 3). Twenty‐four cross‐sectional studies used BMI‐related continuous measures as weight‐related outcomes, where 19 studies reported null associations, nine studies reported a positive association, and two studies reported a negative association. Overweight/obesity was used as outcome variables in 33 cross‐sectional studies, where 26 studies reported null associations, and positive and negative associations were reported in 11 and four studies, respectively. In addition, the majority of the studies (n = 8) conducting stratified analyses showed different associations with FFR access among stratified subgroups, including gender (n = 5), age (n = 4), income (n = 1), ethnicity (n = 1), and grades (n = 1).
3.7. Meta‐analyses between FFR access and weight status
We conducted separate meta‐analyses for different measures of FFR access (i.e., presence of FFRs, density of FFRs, and distance to the nearest FFR) and outcomes (i.e., overweight/obesity, obesity, BMI, BMI percentile, and BMI z‐score) (Table 2). Although most studies suggested a positive association between FFR access and weight‐related outcomes, none of the meta‐analyses demonstrated significant results. For instance, the pooled odds ratio for the presence of FFRs and overweight/obesity was 1.01 (95% CI, 0.97‐1.05) based on 13 included studies (Figure 2). The pooled odds ratio for the number of FFRs and overweight/obesity was 1.00 (95%CI, 0.99‐1.01) based on 15 included studies (Figure 3). The pooled beta coefficient for the density of FFRs and BMI z‐score was 0.0006 (95% CI, −0.0015 to 0.0027) based on eight included studies. The meta‐analysis for the density of FFRs and BMI showed a negative but not significant association (β = −0.0275; 95% CI, −0.3132 to 0.2582)3.
TABLE 2.
Meta‐analyses of associations between access to fast‐food restaurants (FFRs) and weight status
| Author (Year)[ref] | Study Design 1 | Study Area [Scale] 2 | Sample Size | FFR Measures | Weight‐related Outcomes | Estimated Effect | Pooled Effect Size (95% CI) | I 2 Index |
|---|---|---|---|---|---|---|---|---|
| Presence of FFRs and overweight/obesity (N = 13) | ||||||||
| Hamano (2017) 32 | LO | Sweden [N] | 944 487 | Presence of FFRs within 1‐km straight‐line buffer around home | Hospital or out‐patient diagnosis of childhood obesity |
OR (95% CI) 0.99 (0.94‐1.05) |
OR (95% CI) 1.01 (0.97‐1.05) random |
50% |
| Leung (2011) 35 | LO | California, USA [CT4] | 353 | Presence of FFRs within 0.4‐km road‐network buffers around home | Overweight/obesity (BMI percentile ≥85th on the 2000 US CDC growth charts) |
OR (95% CI) 0.82 (0.28‐2.44) |
||
| Correa (2018) 54 | CS | Florianopolis, Brazil [C] | 2195 | Presence of FFRs within 0.4‐km straight‐line buffer around home | Overweight/Obesity (BMI z‐score > +1SD based on the 2007 WHO growth reference, equivalent to BMI ≥25 kg/m2 in adults) |
OR (95% CI) 1.00 (0.75‐1.34) |
||
| Crawford (2008) 55 | CS | Melbourne, Australia [C] | 380 | Presence of FFRs within 2‐km straight‐line buffer around home | Overweight/obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) 8‐ to 9‐year‐old boys: 1.52 (0.84‐2.76); 8‐ to 9‐year‐old girls: 0.48 (0.06‐3.60); 13‐ to 15‐year‐old boys: 0.63 (0.19‐2.10); 13‐ to 15‐year‐old girls: 0.19 (0.09‐0.41) 0.56 (0.17‐1.84) random |
||
| Davis (2009) 57 | CS | California, USA [S] | 529 367 | Presence of FFRs within 0.8 km from school | Overweight/obesity (BMI ≥85th percentile) based on the US CDC growth charts |
OR (95% CI) 1.06 (1.02‐1.10) |
||
| Heroux (2012) 69 | CS | Canada, Scotland, and the USA [N3] | 26 778 | Presence of FFRs within 1‐km straight‐line buffer around school | Overweight/obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) Canadian youth (n = 11 945): 0.92 (0.83‐1.03); Scottish youth (n = 4697): 0.94 (0.74‐1.20); US youth (n = 4928): 1.08 (0.96‐1.21) 0.98 (0.88‐1.10) random |
||
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Presence of FFRs within 0.16‐/0.4‐/0.8‐/1.6‐km road‐network buffers around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.16‐km buffer zone: 3.83 (0.94‐15.63); 0.4‐km buffer zone: 1.05 (0.67‐1.65); 0.8‐km buffer zone: 1.19 (0.80‐1.77); 1.6‐km buffer zone: 0.94 (0.64‐1.39) 1.09 (0.86‐1.38) fixed |
||
| Miller (2014) 92 | CS | Perth, Australia [C] | 1850 | Presence of FFRs within 0.8‐km road‐network buffer around home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.691 (0.529‐0.903) |
||
| Ohri‐Vachaspati (2015) 93 | CS | New Jersey, USA [S] | 560 | Presence of FFRs within 0.4‐km road‐network buffer around home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.67 (0.38‐1.20) |
||
| Oreskovic (2009) 95 | CS | Massachusetts, USA [S] | 21 008 | Presence of FFRs within 0.4‐km road‐network buffer around home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 1.05 (0.98‐1.12) |
||
| Seliske (2009) 102 | CS | Canada [N] | 7281 | Presence of FFRs within 1‐km straight‐line buffer around school | Overweight/obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) 0.83 (0.70‐0.98) |
||
| Shier (2016) 104 | CS | USA [N] | 903 | Parent‐perceived presence of FFRs within 20‐min walk from home | Overweight/obesity (BMI ≥85th percentile) |
β (SE) 0.020 (0.030) OR (95% CI) 1.02 (0.96‐1.08) |
||
| Tang (2014) 107 | CS | New Jersey, USA [C4] | 12 954 | Presence of FFRs within 0.4‐km road‐network buffer around school | Overweight/obesity (BMI percentile ≥85th) |
β (95% CI) 0.03 (−0.004 to 0.06) OR (95% CI) 1.03 (1.00‐1.07) |
||
| Presence of FFRs and obesity (N = 4) | ||||||||
| Hamano (2017) 32 | LO | Sweden [N] | 944 487 | Presence of FFRs within 1‐km straight‐line buffer around home | Hospital or out‐patient diagnosis of childhood obesity |
OR (95% CI) 0.99 (0.94‐1.05) |
OR (95% CI) 1.04 (0.99‐1.09) random |
42% |
| Davis (2009) 57 | CS | California, USA [S] | 529 367 | Presence of FFRs within 0.8 km from school | Obesity (BMI ≥95th percentile) based on the US CDC growth charts |
OR (95% CI) 1.07 (1.02‐1.12) |
||
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Presence of FFRs within 0.16/0.4/0.8/1.6‐km road‐network buffers around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.16‐km buffer zone: 3.83 (0.94‐15.63); 0.4‐km buffer zone: 1.05 (0.67‐1.65); 0.8‐km buffer zone: 1.19 (0.80‐1.77); 1.6‐km buffer zone: 0.94 (0.64‐1.39) 1.09 (0.86‐1.38) fixed |
||
| Oreskovic (2009) 95 | CS | Massachusetts, USA [S] | 21 008 | Presence of FFRs within 0.4‐km road‐network buffer around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 1.06 (0.98‐1.14) |
||
| Number of FFRs and overweight/obesity (N = 15) | ||||||||
| Bader (2013) 45 | CS | New York, USA [C] | 94 348 | Number of FFRs in the residential census tract | Overweight/obesity (BMI ≥85th percentile) based on the 2011 US CDC growth charts |
OR (95% CI) 0.972 (0.957‐0.988) |
OR (95% CI) 1.00 (0.99‐1.01) random |
89% |
| Choo (2017) 20 | CS | Seoul, South Korea [C] | 126 | Number of Western FFRs within 0.2‐km straight‐line buffer around community child centre | Obesity (BMI ≥95th percentile or BMI >25 kg/m2) based on the 2012 guidelines of Korea Centers for Disease Control and Prevention |
OR (95% CI) 0.87 (0.608‐1.245) |
||
| Crawford (2008) 55 | CS | Melbourne, Australia [C] | 380 | Number of FFRs within 2‐km straight‐line buffer around home | Overweight/obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) 8‐ to 9‐year‐old boys: 0.96 (0.84‐1.10); 8‐ to 9‐year‐old girls: 0.82 (0.63‐1.08); 13‐ to 15‐year‐old boys: 0.91 (0.78‐1.06); 13‐ to 15‐year‐old girls: 0.86 (0.74‐0.99) 0.90 (0.83‐0.98) fixed |
||
| Fraser (2010) 62 | CS | Leeds, West Yorkshire, UK [C] | 33 594 | Number of FFRs in residential super‐output area (SOA) | Overweight/obesity (BMI ≥85th percentile) |
OR (95% CI) 1.01 (1.002‐1.02) |
||
| Gorski Findling (2018) 65 | CS | USA [N] | 3748 | Number of FFRs within 1.6‐km straight‐line buffer around home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.99 (0.96‐1.02) |
||
| Larsen (2015) 83 | CS | Toronto, Canada [C] | 943 | Number of FFRs within 1‐km road‐network buffer around home | Overweight and obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) 0.978 (0.953‐1.003) |
||
| Leatherdale (2011) 87 | CS | Ontario, Canada [S] | 1207 | Number of FFRs within 1‐km straight‐line buffer around school | Obesity (BMI percentile ≥95th based on the 2000 US CDC growth charts) |
OR (95% CI) 0.96 (0.82‐1.13) |
||
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Number of FFRs within 0.16‐/0.4‐/0.8‐/1.6‐km road‐network buffer around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.16‐km buffer zone: 3.07 (0.75‐12.59); 0.4‐km buffer zone: 1.04 (0.92‐1.19); 0.8‐km buffer zone: 0.97 (0.89‐1.06); 1.6‐km buffer zone: 0.98 (0.94‐1.03) 0.98 (0.95‐1.02) fixed |
||
| Miller (2014) 92 | CS | Perth, Australia [C] | 1850 | Number of FFRs within 0.8‐/3‐km road‐network buffer around home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.8‐km buffer zone: 0.961 (0.919‐1.006); 3‐km buffer zone: 0.993 (0.988‐0.999) 0.98 (0.96‐1.01) random |
||
| Oreskovic (2009) 94 | CS | Massachusetts, USA [S] | 6680 | Number of FFRs within 0.4‐km road‐network buffer around home | Overweight (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) high‐income towns: 1.09 (0.82‐1.26) low‐income towns: 1.09 (1.07‐1.11) 1.09 (1.07‐1.11) fixed |
||
| Oreskovic (2009) 95 | CS | Massachusetts, USA [S] | 21 008 | Number of FFRs within 0.4‐km road‐network buffer around home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.98 (0.96‐1.01) |
||
| Park (2013) 97 | CS | Seoul, South Korea [C] | 939 | Number of FFRs within 0.5‐km straight‐line buffer around school | Overweight/obesity (BMI ≥85th percentile) based on the 2007 Korean National Growth Charts |
OR (95% CI) 0.83 (0.72‐0.96) |
||
| Shier (2016) 104 | CS | USA [N] | 903 | Number of FFRs within 3.2‐km straight‐line buffer around home | Overweight/obesity (BMI ≥85th percentile) |
β (SE) 0.000 (0.002) OR (95% CI) 1.00 (0.9961‐1.0039) |
||
| Tang (2014) 107 | CS | New Jersey, USA [C4] | 12 954 | Number of FFRs within 0.4‐km straight‐line buffer around school | Overweight/obesity (BMI percentile ≥85th) |
β (95% CI) 0.0001 (−0.004 to 0.005) OR (95% CI) 1.0001 (0.9960‐1.0042) |
||
| Wasserman (2014) 111 | CS | Kansas, USA [C2] | 12 118 | Number of FFRs within 0.8‐km straight‐line buffer around school | Overweight (BMI ≥85th percentile) |
OR (95% CI) 1.02 (0.98‐1.08) |
||
| Number of FFRs and obesity (N = 8) | ||||||||
| Choo (2017) 20 | CS | Seoul, South Korea [C] | 126 | Number of Western FFRs within 0.2‐km straight‐line buffer around community child centre | Obesity (BMI ≥95th percentile or BMI >25 kg/m2) based on the 2012 guidelines of Korea Centers for Disease Control and Prevention |
OR (95% CI) 0.87 (0.608‐1.245) |
OR (95% CI) 1.02 (0.98‐1.07) random |
90% |
| Fraser (2010) 62 | CS | Leeds, West Yorkshire, UK [C] | 33 594 | Number of FFRs in residential super‐output area (SOA) | Obesity (BMI ≥95th percentile) |
OR (95% CI) 1.01 (1.002‐1.02) |
||
| Leatherdale (2011) 87 | CS | Ontario, Canada [S] | 1207 | Number of FFRs within 1‐km straight‐line buffer around school | Obesity (BMI percentile ≥95th based on the 2000 US CDC growth charts) |
OR (95% CI) 0.96 (0.82‐1.13) |
||
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Number of FFRs within 0.16‐/0.4‐/0.8‐/1.6‐km road‐network buffer around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.16‐km buffer zone: 3.07 (0.75‐12.59); 0.4‐km buffer zone: 1.04 (0.92‐1.19); 0.8‐km buffer zone: 0.97 (0.89‐1.06); 1.6‐km buffer zone: 0.98 (0.94‐1.03) 0.98 (0.95‐1.02) fixed |
||
| Oreskovic (2009) 94 | CS | Massachusetts, USA [S] | 6680 | Number of FFRs within 0.4‐km road‐network buffer around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) high‐income towns: 0.95 (0.72‐1.25); low‐income towns: 1.13 (1.10‐1.16) 1.13 (1.10‐1.16) fixed |
||
| Oreskovic (2009) 95 | CS | Massachusetts, USA [S] | 21 008 | Number of FFRs within 0.4‐km road‐network buffer around home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.99 (0.96‐1.02) |
||
| Park (2013) 97 | CS | Seoul, South Korea [C] | 939 | Number of FFRs within 0.5‐km straight‐line buffer around school | Obesity (BMI ≥95th percentile) based on the 2007 Korean National Growth Charts |
OR (95% CI) 1.15 (0.94‐1.39) |
||
| Wasserman (2014) 111 | CS | Kansas, USA [C2] | 12 118 | Number of FFRs within 0.8‐km straight‐line buffer around school | Obesity (BMI ≥95th percentile) |
OR (95% CI) 1.02 (0.97‐1.08) |
||
| Distance (km) to the nearest FFR and overweight/obesity (N = 6) | ||||||||
| Choo (2017) 20 | CS | Seoul, South Korea [C] | 126 | Road‐network distance (m) to the closest Western FFR around community child centre | Obesity (BMI ≥95th percentile or BMI >25 kg/m2) based on the 2012 guidelines of Korea Centers for Disease Control and Prevention |
OR (95% CI) 1.00 (0.984‐1.008) |
OR (95% CI) 0.98 (0.95‐1.01) random |
19% |
| Crawford (2008) 55 | CS | Melbourne, Australia [C] | 380 | Road‐network distance (km) to the nearest FFR from home | Overweight/obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) 8‐ to 9‐year‐old boys: 0.99 (0.86‐1.15); 8‐ to 9‐year‐old girls: 1.02 (0.83‐1.25); 13‐ to 15‐year‐old boys: 1.08 (0.89‐1.30); 13‐ to 15‐year‐old girls: 1.18 (0.96‐1.45) 1.05 (0.96‐1.15) fixed |
||
| Larsen (2015) 83 | CS | Toronto, Canada [C] | 943 | Road‐network distance (km) to the nearest FFR from home | Overweight and obesity based on IOTF cut‐offs, equivalent to BMI ≥25 kg/m2 in adults |
OR (95% CI) 1.261 (0.871‐1.825) |
||
| Miller (2014) 92 | CS | Perth, Australia [C] | 1850 | Road‐network distance (m) to the nearest FFR from home | Overweight/obesity (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 1.000 (1.000‐1.000) |
||
| Oreskovic (2009) 94 | CS | Massachusetts, USA [S] | 6680 | Road‐network distance (km) to the nearest FFR from home | Overweight (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) high‐income towns: 0.93 (0.86‐1.00); low‐income towns: 0.97 (0.92‐1.03) 0.96 (0.92‐1.00) fixed |
||
| Oreskovic (2009) 95 | CS | Massachusetts, USA [S] | 21 008 | Road‐network distance (km) to the nearest FFR from home | Overweight (BMI ≥85th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.98 (0.95‐1.00) |
||
| Distance (km) to the nearest FFR and obesity (N = 3) | ||||||||
| Choo (2017) 20 | CS | Seoul, South Korea [C] | 126 | Road‐network distance (m) to the closest Western FFR around community child centre | Obesity (BMI ≥95th percentile or BMI >25 kg/m2) based on the 2012 guidelines of Korea Centers for Disease Control and Prevention |
OR (95% CI) 1.00 (0.984‐1.008) |
OR (95% CI) 0.93 (0.84‐1.02) random |
65% |
| Oreskovic (2009) 94 | CS | Massachusetts, USA [S] | 6680 | Road‐network distance (km) to the nearest FFR from home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) high‐income towns: 0.93 (0.82‐1.04); low‐income towns: 0.83 (0.75‐0.91) 0.87 (0.80‐0.94) fixed |
||
| Oreskovic (2009) 95 | CS | Massachusetts, USA [S] | 21 008 | Road‐network distance (km) to the nearest FFR from home | Obesity (BMI ≥95th percentile) based on the 2000 US CDC growth charts |
OR (95% CI) 0.97 (0.94‐1.01) |
||
| Number of FFRs and BMI percentile (N = 2) | ||||||||
| An (2012) 44 | CS | California, USA [S] | 13 462 | Number of FFRs within 0.8‐km straight‐line buffer around school | Parent‐reported BMI percentile based on the 2000 US CDC growth charts |
β (SE) 5‐11 y: −0.0009 (0.0019); 12‐17 y: −0.0025 (0.0022) −0.0016 (0.0014) fixed |
β (95% CI) 0.0990 (‐0.2124, 0.4104) Random | 57% |
| Wasserman (2014) 111 | CS | Kansas, USA [C2] | 12 118 | Number of FFRs within 0.8‐km straight‐line buffer around school | Measured BMI percentile based on the 2000 US CDC growth charts |
β (SE) 0.35 (0.23) |
||
| Distance to nearest FFR and BMI z‐score (N = 2) | ||||||||
| Crawford (2008) 55 | CS | Melbourne, Australia [C] | 380 | Road‐network distance (km) to the nearest FFR from home | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 8‐ to 9‐year‐old boys: 0.05 (0.00‐0.10); 8‐ to 9‐year‐old girls: −0.04 (−0.13 to 0.05); 13‐ to 15‐year‐old boys: 0.04 (−0.06 to 0.13); 13‐ to 15‐year‐old girls: 0.03 (−0.03 to 0.09) 0.0304 (−0.0029 to 0.0637) fixed |
β (95% CI) 0.0316 (0.0098‐0.0534) fixed/random | 0 |
| Lamichhane (2012) 81 | CS | South Carolina, USA [S] | 845 | Road‐network distance (mile) to the nearest FFR from home | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 0.052 (0.007‐0.098) km: 0.0325 (0.0044‐0.0613) |
||
| Presence of FFRs and BMI z‐score (N = 6) | ||||||||
| Ghenadenik (2018) 30 | LO | Montreal, Canada [C] | 391 | Presence of FFRs in residential street segment | Measured BMI z‐score based on the 2010 US CDC growth charts |
β (SE) 0.105 (0.185) |
β (95% CI) 0.0276 (−0.0205 to 0.0757) random |
27% |
| Crawford (2008) 55 | CS | Melbourne, Australia [C] | 380 | Presence of FFRs within 2‐km straight‐line buffer around home | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 8‐ to 9‐year‐old boys: −0.02 (−0.23 to 0.25); 8‐ to 9‐year‐old girls: −0.01 (−1.11 to 1.09); 13‐ to 15‐year‐old boys: −0.49 (−0.95 to −0.03); 13‐ to 15‐year‐old girls: −0.35 (−0.69 to −0.02) −0.1573 (−0.3220 to 0.0073) fixed |
||
| Gilliland (2012) 64 | CS | London, UK [C] | 891 | Presence of FFRs within 0.5‐km road‐network buffer around home | Self‐reported BMI z‐score based on the WHO growth charts |
β (SE) 0.012 (0.121) |
||
| Tang (2014) 107 | CS | New Jersey, USA [C4] | 12 954 | Presence of FFRs within 0.4‐km road‐network buffer around school | BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 0.07 (−0.01 to 0.15) |
||
| Wall (2012) 110 | CS | Minneapolis/St Paul, USA [C] | 2682 | Presence of FFRs within 1.2‐km road‐network buffer around home | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (SE) boys: 0.095 (0.078); girls: 0.045 (0.060) 0.0636 (0.0476) fixed |
||
| Williams (2015) 112 | CS | Berkshire, UK [CT] | 16 956 | Presence of FFRs within 0.8‐km road‐network buffer around school | Measured BMI z‐score based on the IOTF reference curves |
β (95% CI) 0.02 (−0.02 to 0.06) |
||
| Number of FFRs and BMI z‐score (N = 8) | ||||||||
| Chen (2016) 27 | LO | Arkansas, USA [S] | 21 639 | Number of FFRs along the most direct street route from home to school within 50‐m buffer on either side of the street | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 0.0001 (−0.0004 to 0.0007) |
β (95% CI) 0.0006 (−0.0015 to 0.0027) random |
41% |
| Green (2018) 31 | LO | Leeds, UK [C] | 746 | Number of FFRs within 1‐km straight‐line buffer around home | Measured BMI SDS based on the UK 1990 growth charts |
β (95% CI) −0.017 (−0.035 to 0.002) |
||
| Baek (2014) 46 | CS | California, USA [S] | 926 018 | Number of FFRs within 0.4‐/0.8‐/1.2‐km straight‐line buffer around school | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (SE) 0.4‐km buffer zone: 1.14 × 10−3 (3.73 × 10−3); 0.8‐km buffer zone: 1.12 × 10−3 (1.97 × 10−3); 1.2‐km buffer zone: 1.72 × 10−3 (1.15 × 10−3) 0.0015 (0.0010) fixed |
||
| Crawford (2008) 55 | CS | Melbourne, Australia [C] | 380 | Number of FFRs within 2‐km straight‐line buffer around home | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 8‐ to 9‐year‐old boys: −0.01 (−0.05 to 0.04); 8‐ to 9‐year‐old girls: −0.02 (−0.15 to 0.11); 13‐ to 15‐year‐old boys: −0.07 (−0.14 to 0.01); 13‐ to 15‐year‐old girls: −0.03 (−0.08 to 0.02) −0.0262 (−0.0540 to 0.0017) fixed |
||
| Fraser (2010) 62 | CS | Leeds, West Yorkshire, UK [C] | 33 594 | Number of FFRs in residential super‐output area (SOA) | Measured BMI SDS based on the UK1990 BMI reference |
β (95% CI) 0.004 (−0.007 to 0.01) |
||
| Lamichhane (2012) 81 | CS | South Carolina, USA [S] | 845 | Number of FFRs within 1.6‐km road‐network buffer around home | Measured BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 0.002 (−0.027 to 0.031) |
||
| Shier (2016) 104 | CS | USA [N] | 903 | Number of FFRs within 3.2‐km straight‐line buffer around home | BMI z‐score based on the 2000 US CDC growth charts |
β (SE) −0.001 (0.004) |
||
| Tang (2014) 107 | CS | New Jersey, USA [C4] | 12 954 | Number of FFRs within 0.4‐km straight‐line buffer around school | BMI z‐score based on the 2000 US CDC growth charts |
β (95% CI) 0.01 (−0.002 to 0.02) |
||
| Presence of FFRs and BMI (N = 3) | ||||||||
| Davis (2009) 57 | CS | California, USA [S] | 529 367 | Presence of FFRs within 0.8 km from school | BMI |
β (95% CI) 0.10 (0.03‐0.16) |
β (95% CI) 0.2888 (−0.0942 to 0.6719) random |
52% |
| Li (2011) 88 | CS | Xi'an, China [C] | 1792 | Presence of FFRs within 10‐min walk around school reported by school doctors | Measured BMI |
β (95% CI) 0.7 (0.1‐1.2) |
||
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Presence of FFRs within 0.8‐km road‐network buffer around home | Measured BMI |
β (95% CI) 0.35 (−0.42 to 1.13) |
||
| Presence of FFRs and BMI (N = 2) | ||||||||
| Davis (2009) 57 | CS | California, USA [S] | 529 367 | Presence of FFRs within 0.4 km from school | BMI |
β (95% CI) 0.12 (0.04‐0.20) |
β (95% CI) 0.2420 (−0.2555 to 0.7395) random |
37% |
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Presence of FFRs within 0.4‐km road‐network buffer around home | Measured BMI |
β (95% CI) 0.77 (−0.24 to 1.78) |
||
| Density of FFRs and BMI (N = 2) | ||||||||
| Powell (2009) 37 | LO | USA [N] | 5215 | Density of FFRs per 10 000 capita | Self‐reported BMI |
β (SE) 0.1215 (0.1164) |
β (95% CI) −0.0275 (−0.3132 to 0.2582) random |
70% |
| Powell (2009) 98 | CS | USA [N] | 6594 | Density of FFRs per 10 000 capita | Mother‐reported BMI |
β (SE) −0.1701 (0.1081) |
||
| Number of FFRs and BMI (N = 2) | ||||||||
| Davis (2009) 57 | CS | California, USA [S] | 529 367 | Number of FFRs within 0.8‐km road‐network buffer around school | BMI |
β (95% CI) 0.00 (0.00‐0.00) |
β (95% CI) 0.004 (−0.15 to 0.16) |
NA |
| Mellor (2011) 91 | CS | Virginia, USA [S] | 2023 | Number of FFRs within 0.8‐km road‐network buffer around home | Measured BMI |
β (95% CI) 0.004 (−0.15 to 0.16) |
||
| Presence of FFRs and school overweight rates (N = 2) | ||||||||
| Howard (2011) 72 | CS | California, USA [S] | 879 public schools | Presence of FFRs within 0.8‐km road‐network buffer around school | School overweight rates based on criterion‐referenced gender‐, age‐, and test‐specific cut‐offs established by a national advisory panel |
β (95% CI) −0.04 (−1.18 to 1.10) |
β (95% CI) 0.1767 (−0.5830 to 0.9365) fixed/random |
0 |
| Langellier (2012) 82 | CS | Los Angeles, USA [CT] | 1694 schools | Presence of FFRs within 0.8‐km road‐network buffer around school | School overweight rates based on the sex‐ and age‐specific cut‐offs defined by the Physical Fitness Testing programme in 2009 |
β (SE) 0.35 (0.52) |
||
Study design: LO, longitudinal; CS, cross‐sectional;
Study area: [N], national; [S], state (eg, in the United States) or equivalent unit (eg, province in China and Canada); [Sn], n states or equivalent units; [CT], county or equivalent unit; [CTn], n counties or equivalent units; [C], city; [Cn], n cities.
FIGURE 2.
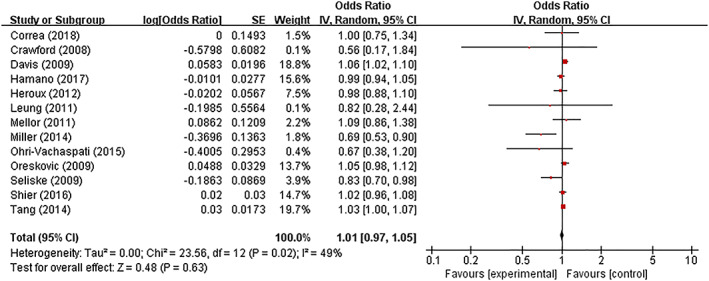
Meta‐analysis of associations between presence of fast‐food restaurants in the neighbourhood and childhood overweight/obesity [Colour figure can be viewed at wileyonlinelibrary.com]
FIGURE 3.
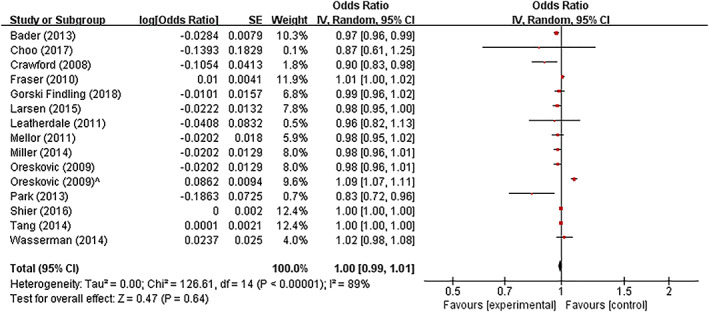
Meta‐analysis of associations between density of fast‐food restaurants in the neighbourhood and childhood overweight/obesity [Colour figure can be viewed at wileyonlinelibrary.com]
3.8. Study quality assessment
Table S2 reported criterion‐specific and global ratings from the study quality assessment. The included studies scored 10.1 of 14 on average, with a range from seven to 14.
4. DISCUSSION
In this review, 87 studies focusing on FFR access and childhood obesity were selected and based on which meta‐analyses were conducted. This pool was composed of studies with various study designs (ie, 16 cohort studies and 71 cross‐sectional studies) and study locations (ie, 14 different countries). Weight‐related behaviours and outcomes were used as outcome variables in 35 and 61 studies, respectively. Although FFR access was positively associated with fast‐food consumption in the majority of studies focusing on that relationship, its associations with other weight‐related behaviours, including frequency of food consumption, dietary quality score, and physical activity, were either mixed or not significant. For the association between FFR access and weight‐related outcomes, no associations were reported in most studies when using BMI‐related continuous measures; when using overweight/obesity measures, about half of cohort studies and one‐third of cross‐sectional studies reported a positive association. No significant results were observed in separate meta‐analyses between various measures of FFR access and body weight.
One previous review on local food environment and obesity in North America has covered the association between FFR access and childhood obesity, where the majority of studies found no associations, with half of the remaining studies reporting a positive association and the other half reporting a negative association. 16 Also, the availability of fast food was more consistently associated with higher risk of obesity in low‐income populations. Likewise, with mixed findings from the included studies (some evidence supporting a positive association but others suggesting a null association), this review also cannot provide a clear‐cut answer for the association between FFR access and childhood obesity. 16 Some parts of our hypothesis on the association between FFR access, unhealthy food consumption, and childhood obesity have been supported. For example, 10 of 14 included studies supported the link between FFR access and increased fast‐food consumption; a systematic review also supported the association between fast‐food consumption and increased caloric intake. 13 However, the association between fast‐food consumption and childhood obesity may be subject to many confounding factors, especially at the population level, as childhood obesity may be attributed to other factors including genetic susceptibility, prenatal and early life factors, consumption of other unhealthy or healthy food, physical activity, and family factors. 17 Therefore, the association between fast‐food consumption and childhood obesity is less easier to access without careful control for confounders. 18 More modern technologies used in spatial lifecourse epidemiologic research, such as location‐based mobile services, ecological momentary assessment, and things of Internet, need to be applied to collect more data on food acquisition and consumption and other behaviours that may result in and prevent obesity. 6 , 19 In addition, many studies have reported different associations when stratified by factors including age, gender, ethnicity, and income. Thus, it is also possible that the association between FFR access and childhood obesity only applies to certain subgroups and is not significant at the population level.
The results of the included studies may be influenced by several factors. First, the variation of food served in different FFRs may to some extent affect study results. For instance, one study analysed both Korean and western FFRs and reported that fast‐food consumption was significantly associated with access to Korean FFRs instead of access to western FFRs, which may be explained by the higher density of Korean FFRs than of western FFRs in the study area. 20 It is also important to note that many FFRs have started to change its unhealthy public image by providing relatively healthy food choices, like salad and sugar‐free beverages. Furthermore, some countries have taken measures to control excessive fast‐food eating by providing nutrition information (ie, calorie intake) on the menu. The actual effects of these measures on obesity prevention among children and adolescents are expected to be examined and adjusted in future studies. This also implies that definitions of the FFR and the fast food sold in those venues need to be made clear in each specific context. Second, variations in measures of FFR access were observed among the included studies. Although the measures used were either the number of FFRs or the distance to the nearest FFR, the definition of the neighbourhood area based on which measures were taken can be quite different, where the radii of buffer zones could range from 0.16 to 8 km. The administrative or postal zone boundaries were used where individual addresses were not available. 21 We suggested that the measurement in one study should be conducted at multiple scales for better comparability with other studies, 8 also to better present the results with the Modifiable Areal Unit Problem overcome. 22 , 23 Moreover, measuring the access to FFRs has been more challenging and complicated with the development of transportation and communication. Nowadays, it becomes increasingly convenient to commute in different parts of a city, and an increasing number of people, especially the young, have started to choose ordering food online. Thus, the definition and delineation of the area in which people have convenient access to certain food venues may need to change accordingly. 24 The advanced spatial and location‐based applications may aid in measuring the realistic access to fast food. 25 Third, different from most types of food venues, FFRs appear more frequently along the highways (eg, in rest areas and near gas stations), so fast‐food purchasing may happen in neither residential areas nor school neighbourhoods. Therefore, to comprehensively examine the effects of FFRs on childhood obesity needs the coordination of multiple stakeholders in the real world to track movement patterns of patrons and flows of fast food.
This systematic review, especially meta‐analyses, was limited by the number of studies available. We need to analyse separately for different combinations of exposure and outcomes, as it is not feasible to seamlessly synthesize different measures of access to FFR, as well as different measures of weight‐related behaviours and outcomes. Also, it is not feasible to conduct meta‐analyses for combinations with insufficient studies. We also noticed that the majority of the included studies were cross‐sectional studies, which has prevented us from examining effects of FFR access on individual weight status over time. Future studies were needed to focus on longitudinal associations to investigate their causality. 26
5. CONCLUSIONS
This systematic review revealed a rather mixed association between FFR access and weight‐related behaviours/outcomes among children and adolescents. Methods of defining and measuring FFR access need to be improved to better estimate individuals' exposure to FFRs. Also, research on pathways from FFR access to childhood obesity is needed to allow multiple stakeholders to design effective interventions and policies for prevention of childhood obesity.
CONFLICT OF INTEREST
No conflict of interest was declared.
Supporting information
Figure S1. Funnel plot for meta‐analysis of associations between presence of fast‐food restaurants in the neighborhood and childhood overweight/obesity
Figure S2. Funnel plot for meta‐analysis of associations between density of fast‐food restaurants in the neighborhood and childhood overweight/obesity
Table S1. Measures of access to fast‐food restaurants (FFRs), weight‐related behaviors, and body‐weight status in the included studies (see [ref] in the main text)
Table S2. Study quality assessment (see [ref] in the main text)
ACKNOWLEDGEMENTS
We thank the International Institute of Spatial Lifecourse Epidemiology (ISLE) and the National Natural Science Foundation of China (81872641) for research support. [Correction added on 8 February 2021, after first online publication: Acknowledgements have been revised.]
APPENDIX A. SEARCH STRATEGY
The search strategy includes all possible combinations of keywords in the title/abstract from the following three groups:
“fast‐food restaurant*,” “fast‐food restaurant*,” “fastfood restaurant*,” “fast food outlet*,” “fast‐food outlet*,” “fastfood outlet*,” “takeaway restaurant*,” “take‐away restaurant*,” “take away restaurant*,” “takeaway outlet*,” “take‐away outlet*,” “take away outlet*,” “takeout restaurant*,” “take‐out restaurant*,” “take out restaurant*,” “takeout outlet*,” “take‐out outlet*,” “take out outlet*,” “limited‐service restaurant*,” “limited service restaurant,” “quick‐service restaurant,” “quick service restaurant*”;
“child*,” “juvenile*,” “pubescent*,” “pubert*,” “adolescen*,” “youth*,” “teen*,” “kid*,” “young*,” “youngster*,” “minor*,” “student*,” “pupil*,” “pediatric*,” “preschooler*,” “pre‐schooler*,” “schoolchild*,” “school‐child*,” “school child*,” “schoolage*,” “school‐age*,” “school age*”;
“diet*,” “diet behavio*,” “dietary behavio*,” “eating*,” “eating behavio*,” “food*,” “food intak*,” “food consum*,” “energy intak*,” “energy consum*,” “energy balance,” “calorie*,” “caloric intak*,” “physical activit*,” “physical exercis*,” “exercis*,” “body activit*,” “body mass index,” “BMI,” “weight,” “weight status,” “weight‐related behavio*,” “weight‐related health,” “overweight,” “obese,” “obesity,” “adiposity,” “abdominal overweight,” “abdominal obesity,” “central overweight,” “central obesity,” “central adiposity,” “waist circumference,” “waist to hip,” “waist‐to‐hip,” “waist to height,” “waist‐to‐height,” “waist to stature,” “waist‐to‐stature,” “fatness,” “body fat,” “excess fat,” “excess weight,” “overnutrition,” “over‐nutrition,” “over nutrition.”
Jia P, Luo M, Li Y, Zheng J‐S, Xiao Q, Luo J. Fast‐food restaurant, unhealthy eating, and childhood obesity: A systematic review and meta‐analysis. Obesity Reviews. 2021;22(S1):e12944. 10.1111/obr.12944
Peng Jia and Miyang Luo have equal contribution.
[Correction added on 14 January 2021, after first online publication: Peng Jia's affiliations have been updated.]
[Correction added on 8 February 2021, after first online publication: Funding Information has been revised.]
Contributor Information
Peng Jia, Email: jiapengff@hotmail.com.
Jiayou Luo, Email: jiayouluo@csu.edu.cn.
REFERENCES
- 1. Curran PJ. The semivariogram in remote sensing: an introduction. Remote Sens Environ. 1988;24:15. [Google Scholar]
- 2. Lenz M, Richter T, Mühlhauser I. The morbidity and mortality associated with overweight and obesity in adulthood: a systematic review. Dtsch Arztebl Int. 2009;106(40):641‐648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403‐411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kelsey MM, Zaepfel A, Bjornstad P, Nadeau KJ. Age‐related consequences of childhood obesity. Gerontology. 2014;60(3):222‐228. [DOI] [PubMed] [Google Scholar]
- 5. Report of the commission on ending childhood obesity. World Health Organization ;2016.
- 6. Jia P. Spatial lifecourse epidemiology. Lancet Planet Health. 2019;3(2):e57‐e59. [DOI] [PubMed] [Google Scholar]
- 7. Jia P, Xue H, Cheng X, Wang Y, Wang Y. Association of neighborhood built environments with childhood obesity: evidence from a 9‐year longitudinal, nationally representative survey in the US. Environ Int. 2019;128:158‐164. [DOI] [PubMed] [Google Scholar]
- 8. Jia P, Xue H, Cheng X, Wang Y. Effects of school neighborhood food environments on childhood obesity at multiple scales: a longitudinal kindergarten cohort study in the USA. BMC Med. 2019;17(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abdullah NN, Mokhtar MM, Bakar MHA, Al‐Kubaisy W. Trend on fast food consumption in relation to obesity among Selangor urban community. Procedia Soc Behav Sci. 2015;202:505‐513. [Google Scholar]
- 10. Xue H, Wu Y, Wang X, Wang Y. Time trends in fast food consumption and its association with obesity among children in China. PLoS ONE. 2016;11(3):e0151141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Demory‐Luce D. Fast food and children and adolescents: implications for practitioners. Clin Pediatr. 2005;44(4):279‐288. [DOI] [PubMed] [Google Scholar]
- 12. Jia P, Cheng X, Xue H, Wang Y. Applications of geographic information systems (GIS) data and methods in obesity‐related research. Obes Rev. 2017;18(4):400‐411. [DOI] [PubMed] [Google Scholar]
- 13. Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9(6):535‐547. [DOI] [PubMed] [Google Scholar]
- 14. Schwarzer G. meta: An R Package for Meta‐Analysis. R news. 2007;7. [Google Scholar]
- 15. National Heart L, Institute B . Quality assessment tool for observational cohort and cross‐sectional studies. Bethesda: National Institutes of Health, Department of Health and Human Services. 2014.
- 16. Cobb LK, Appel LJ, Franco M, Jones‐Smith JC, Nur A, Anderson CAM. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity. 2015;23(7):1331‐1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public‐health crisis, common sense cure. Lancet. 2002;360(9331):473‐482. [DOI] [PubMed] [Google Scholar]
- 18. Zhao Y, Wang L, Xue H, Wang H, Wang Y. Fast food consumption and its associations with obesity and hypertension among children: results from the baseline data of the Childhood Obesity Study in China Mega‐cities. BMC Public Health. 2017;17(1):933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jia P, Lakerveld J, Wu J, et al. Top 10 Research priorities in spatial lifecourse epidemiology. Environ Health Perspect. 2019;127(7):74501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Choo J, Kim HJ, Park S. Neighborhood environments: links to health behaviors and obesity status in vulnerable children. West J Nurs Res. 2017;39(8):1169‐1191. [DOI] [PubMed] [Google Scholar]
- 21. Wang Y, Jia P, Cheng X, Xue H. Improvement in food environments may help prevent childhood obesity: evidence from a 9‐year cohort study. Pediatr Obes. 2019;e12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Openshaw S. The Modifiable Areal Unit Problem. Norwick [Norfolk]: Geo Books; 1983. [Google Scholar]
- 23. Jia P, Wang F, Xierali IM. Using a Huff‐based model to delineate hospital service areas. Prof Geogr. 2017;69(4):522‐530. [Google Scholar]
- 24. Jia P. Developing a Flow‐based Spatial Algorithm to Delineate Hospital Service Areas. Appl Geogr. 2016;75:137‐143. [Google Scholar]
- 25. Jia P. Integrating kindergartener‐specific questionnaires with citizen science to improve child health. Frontiers in public health. 2018; 6:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jia P, Xue H, Yin L, Stein A, Wang M, Wang Y. Spatial technologies in obesity research: current applications and future promise. Trends Endocrinol Metab. 2019;30(3):211‐223. [DOI] [PubMed] [Google Scholar]
- 27. Chen D, Thomsen MR, Nayga RM Jr, Bennett JL. Persistent disparities in obesity risk among public schoolchildren from childhood through adolescence. Prev Med. 2016;89:207‐210. [DOI] [PubMed] [Google Scholar]
- 28. Chen HJ, Wang Y. Changes in the neighborhood food store environment and children's body mass index at peripuberty in the United States. J Adolesc Health. 2016;58(1):111‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fraser LK, Clarke GP, Cade JE, Edwards KL. Fast food and obesity: a spatial analysis in a large United Kingdom population of children aged 13‐15. Am J Prev Med. 2012;42(5):e77‐e85. [DOI] [PubMed] [Google Scholar]
- 30. Ghenadenik AE, Kakinami L, Van Hulst A, Henderson M, Barnett TA. Neighbourhoods and obesity: a prospective study of characteristics of the built environment and their association with adiposity outcomes in children in Montreal, Canada. Prev Med. 2018;111:35‐40. [DOI] [PubMed] [Google Scholar]
- 31. Green MA, Radley D, Lomax N, Morris MA, Griffiths C. Is adolescent body mass index and waist circumference associated with the food environments surrounding schools and homes? A longitudinal analysis. BMC Public Health. 2018;18(1):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hamano T, Li X, Sundquist J, Sundquist K. Association between childhood obesity and neighbourhood accessibility to fast‐food outlets: a nationwide 6‐year follow‐up study of 944,487 children. Obes Facts. 2017;10(6):559‐568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khan T, Powell LM, Wada R. Fast food consumption and food prices: evidence from panel data on 5th and 8th grade children. J Obes. 2012;2012:857697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee H. The role of local food availability in explaining obesity risk among young school‐aged children. Soc Sci Med. 2012;74:1193‐1203. [DOI] [PubMed] [Google Scholar]
- 35. Leung CW, Laraia BA, Kelly M, et al. The influence of neighborhood food stores on change in young girls' body mass index. Am J Prev Med. 2011;41(1):43‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pearce M, Bray I, Horswell M. Weight gain in mid‐childhood and its relationship with the fast food environment. J Public Health (Oxf). 2018;40:237‐244. [DOI] [PubMed] [Google Scholar]
- 37. Powell LM. Fast food costs and adolescent body mass index: evidence from panel data. J Health Econ. 2009;28(5):963‐970. [DOI] [PubMed] [Google Scholar]
- 38. Shier V, An R, Sturm R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public Health. 2012;126(9):723‐730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Smith D, Cummins S, Clark C, Stansfeld S. Does the local food environment around schools affect diet? Longitudinal associations in adolescents attending secondary schools in East London. BMC Public Health. 2013;13:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059‐1068. [DOI] [PubMed] [Google Scholar]
- 41. Van Hulst A, Roy‐Gagnon MH, Gauvin L, Kestens Y, Henderson M, Barnett TA. Identifying risk profiles for childhood obesity using recursive partitioning based on individual, familial, and neighborhood environment factors. Int J Behav Nutr Phys Act. 2015;12(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang R, Shi L. Access to food outlets and children's nutritional intake in urban China: a difference‐in‐difference analysis. Ital J Pediatr. 2012;38(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Alviola PA, Nayga RM Jr, Thomsen MR, Danforth D, Smartt J. The effect of fast‐food restaurants on childhood obesity: a school level analysis. Econ Hum Biol. 2014;12:110‐119. [DOI] [PubMed] [Google Scholar]
- 44. An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med. 2012;42(2):129‐135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bader MD, Schwartz‐Soicher O, Jack D, et al. More neighborhood retail associated with lower obesity among New York City public high school students. Health Place. 2013;23:104‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Baek J, Sanchez BN, Sanchez‐Vaznaugh EV. Hierarchical multiple informants models: examining food environment contributions to the childhood obesity epidemic. Stat Med. 2014;33(4):662‐674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Barrett M, Crozier S, Lewis D, et al. Greater access to healthy food outlets in the home and school environment is associated with better dietary quality in young children. Public Health Nutr. 2017;20(18):3316‐3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low‐income preschool children. Prev Med. 2004;38(1):57‐63. [DOI] [PubMed] [Google Scholar]
- 49. Carroll‐Scott A, Gilstad‐Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Casey R, Chaix B, Weber C, et al. Spatial accessibility to physical activity facilities and to food outlets and overweight in French youth. Int J Obes. 2012;36(7):914‐919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cetateanu A, Jones A. Understanding the relationship between food environments, deprivation and childhood overweight and obesity: evidence from a cross sectional England‐wide study. Health Place. 2014;27:68‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chiang PH, Wahlqvist ML, Lee MS, Huang LY, Chen HH, Huang ST. Fast‐food outlets and walkability in school neighbourhoods predict fatness in boys and height in girls: a Taiwanese population study. Public Health Nutr. 2011;14(9):1601‐1609. [DOI] [PubMed] [Google Scholar]
- 53. Clark EM, Quigg R, Wong JE, Richards R, Black KE, Skidmore PM. Is the food environment surrounding schools associated with the diet quality of adolescents in Otago, New Zealand? Health Place. 2014;30:78‐85. [DOI] [PubMed] [Google Scholar]
- 54. Correa EN, Rossi CE, das Neves J, Silva DAS, de Vasconcelos FAG. Utilization and environmental availability of food outlets and overweight/obesity among schoolchildren in a city in the south of Brazil. J Public Health (Oxf). 2018;40(1):106‐113. [DOI] [PubMed] [Google Scholar]
- 55. Crawford DA, Timperio AF, Salmon JA, et al. Neighbourhood fast food outlets and obesity in children and adults: the CLAN Study. Int J Pediatr Obes. 2008;3(4):249‐256. [DOI] [PubMed] [Google Scholar]
- 56. Cutumisu N, Traore I, Paquette MC, et al. Association between junk food consumption and fast‐food outlet access near school among Quebec secondary‐school children: findings from the Quebec Health Survey of High School Students (QHSHSS) 2010‐11. Public Health Nutr. 2017;20(5):927‐937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Davis B, Carpenter C. Proximity of fast‐food restaurants to schools and adolescent obesity. Am J Public Health. 2009;99(3):505‐510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Dwicaksono A, Brissette I, Birkhead GS, Bozlak CT, Martin EG. Evaluating the contribution of the built environment on obesity among New York State students. Health Educ Behav. 2018;45(4):480‐491. [DOI] [PubMed] [Google Scholar]
- 59. Fiechtner L, Block J, Duncan DT, et al. Proximity to supermarkets associated with higher body mass index among overweight and obese preschool‐age children. Prev Med. 2013;56(3‐4):218‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fiechtner L, Sharifi M, Sequist T, et al. Food environments and childhood weight status: effects of neighborhood median income. Child Obes. 2015;11(3):260‐268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Forsyth A, Wall M, Larson N, Story M, Neumark‐Sztainer D. Do adolescents who live or go to school near fast‐food restaurants eat more frequently from fast‐food restaurants? Health Place. 2012;18(6):1261‐1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Fraser LK, Edwards KL. The association between the geography of fast food outlets and childhood obesity rates in Leeds, UK. Health Place. 2010;16(6):1124‐1128. [DOI] [PubMed] [Google Scholar]
- 63. Galvez MP, Hong L, Choi E, Liao L, Godbold J, Brenner B. Childhood obesity and neighborhood food‐store availability in an inner‐city community. Acad Pediatr. 2009;9(5):339‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gilliland JA, Rangel CY, Healy MA, et al. Linking childhood obesity to the built environment: a multi‐level analysis of home and school neighbourhood factors associated with body mass index. Can J Public Health. 2012;103(9 Suppl 3):eS15‐eS21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gorski Findling MT, Wolfson JA, Rimm EB, Bleich SN. Differences in the neighborhood retail food environment and obesity among US children and adolescents by SNAP participation. Obesity (Silver Spring). 2018;26(6):1063‐1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. He M, Tucker P, Gilliland J, Irwin JD, Larsen K, Hess P. The influence of local food environments on adolescents' food purchasing behaviors. Int J Environ Res Public Health. 2012;9(4):1458‐1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. He M, Tucker P, Irwin JD, Gilliland J, Larsen K, Hess P. Obesogenic neighbourhoods: the impact of neighbourhood restaurants and convenience stores on adolescents' food consumption behaviours. Public Health Nutr. 2012;15:2331‐2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hearst MO, Pasch KE, Laska MN. Urban v. suburban perceptions of the neighbourhood food environment as correlates of adolescent food purchasing. Public Health Nutr. 2012;15:299‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Heroux M, Iannotti RJ, Currie D, Pickett W, Janssen I. The food retail environment in school neighborhoods and its relation to lunchtime eating behaviors in youth from three countries. Health Place. 2012;18(6):1240‐1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ho SY, Wong BY, Lo WS, Mak KK, Thomas GN, Lam TH. Neighbourhood food environment and dietary intakes in adolescents: sex and perceived family affluence as moderators. Int J Pediatr Obes. 2010;5(5):420‐427. [DOI] [PubMed] [Google Scholar]
- 71. Hobin EP, Leatherdale S, Manske S, Dubin JA, Elliott S, Veugelers P. Are environmental influences on physical activity distinct for urban, suburban, and rural schools? A multilevel study among secondary school students in Ontario, Canada. J Sch Health. 2013;83(5):357‐367. [DOI] [PubMed] [Google Scholar]
- 72. Howard PH, Fitzpatrick M, Fulfrost B. Proximity of food retailers to schools and rates of overweight ninth grade students: an ecological study in California. BMC Public Health. 2011;11(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Jago R, Baranowski T, Baranowski JC, Cullen KW, Thompson D. Distance to food stores & adolescent male fruit and vegetable consumption: mediation effects. Int J Behav Nutr Phys Act. 2007;4(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Jilcott SB, Wade S, McGuirt JT, Wu Q, Lazorick S, Moore JB. The association between the food environment and weight status among eastern North Carolina youth. Public Health Nutr. 2011;14:1610‐1617. [DOI] [PubMed] [Google Scholar]
- 75. Joo S, Ju S, Chang H. Comparison of fast food consumption and dietary guideline practices for children and adolescents by clustering of fast food outlets around schools in the Gyeonggi area of Korea. Asia Pac J Clin Nutr. 2015;24:299‐307. [DOI] [PubMed] [Google Scholar]
- 76. Kelly C, Callaghan M, Molcho M, Nic Gabhainn S, Alforque TA. Food environments in and around post‐primary schools in Ireland: associations with youth dietary habits. Appetite. 2019;132:182‐189. [DOI] [PubMed] [Google Scholar]
- 77. Kepper M, Tseng TS, Volaufova J, Scribner R, Nuss H, Sothern M. Pre‐school obesity is inversely associated with vegetable intake, grocery stores and outdoor play. Pediatr Obes. 2016;11(5):e6‐e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Koleilat M, Whaley SE, Afifi AA, Estrada L, Harrison GG. Understanding the relationship between the retail food environment index and early childhood obesity among WIC participants in Los Angeles County using GeoDa. Online J Public Health Inform. 2012;4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Lakes T, Burkart K. Childhood overweight in Berlin: intra‐urban differences and underlying influencing factors. Int J Health Geogr. 2016;15(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Lamichhane AP, Mayer‐Davis EJ, Puett R, Bottai M, Porter DE, Liese AD. Associations of built food environment with dietary intake among youth with diabetes. J Nutr Educ Behav. 2012;44(3):217‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Lamichhane AP, Puett R, Porter DE, Bottai M, Mayer‐Davis EJ, Liese AD. Associations of built food environment with body mass index and waist circumference among youth with diabetes. Int J Behav Nutr Phys Act. 2012;9(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Langellier BA. The food environment and student weight status, Los Angeles County, 2008‐2009. Prev Chronic Dis. 2012;9:E61. [PMC free article] [PubMed] [Google Scholar]
- 83. Larsen K, Cook B, Stone MR, Faulkner GE. Food access and children's BMI in Toronto, Ontario: assessing how the food environment relates to overweight and obesity. Int J Public Health. 2015;60(1):69‐77. [DOI] [PubMed] [Google Scholar]
- 84. Laska MN, Hearst MO, Forsyth A, Pasch KE, Lytle L. Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr. 2010;13(11):1757‐1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Laxer RE, Janssen I. The proportion of excessive fast‐food consumption attributable to the neighbourhood food environment among youth living within 1 km of their school. Appl Physiol Nutr Metab. 2014;39:480‐486. [DOI] [PubMed] [Google Scholar]
- 86. Le H, Engler‐Stringer R, Muhajarine N. Walkable home neighbourhood food environment and children's overweight and obesity: proximity, density or price? Can J Public Health. 2016;107:5347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Leatherdale ST, Pouliou T, Church D, Hobin E. The association between overweight and opportunity structures in the built environment: a multi‐level analysis among elementary school youth in the PLAY‐ON study. Int J Public Health. 2011;56(3):237‐246. [DOI] [PubMed] [Google Scholar]
- 88. Li M, Dibley MJ, Yan H. School environment factors were associated with BMI among adolescents in Xi'an City, China. BMC Publ Health. 2011;11(1):792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: differences by population density. Am J Health Promot. 2007;21(4_suppl):317‐325. [DOI] [PubMed] [Google Scholar]
- 90. Longacre MR, Drake KM, MacKenzie TA, et al. Fast‐food environments and family fast‐food intake in nonmetropolitan areas. Am J Prev Med. 2012;42(6):579‐587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Mellor JM, Dolan CB, Rapoport RB. Child body mass index, obesity, and proximity to fast food restaurants. Int J Pediatr Obes. 2011;6(1):60‐68. [DOI] [PubMed] [Google Scholar]
- 92. Miller LJ, Joyce S, Carter S, Yun G. Associations between childhood obesity and the availability of food outlets in the local environment: a retrospective cross‐sectional study. Am J Health Promot. 2014;28(6):e137‐e145. [DOI] [PubMed] [Google Scholar]
- 93. Ohri‐Vachaspati P, DeLia D, DeWeese RS, Crespo NC, Todd M, Yedidia MJ. The relative contribution of layers of the Social Ecological Model to childhood obesity. Public Health Nutr. 2015;18:2055‐2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Oreskovic NM, Kuhlthau KA, Romm D, Perrin JM. Built environment and weight disparities among children in high‐ and low‐income towns. Acad Pediatr. 2009;9(5):315‐321. [DOI] [PubMed] [Google Scholar]
- 95. Oreskovic NM, Winickoff JP, Kuhlthau KA, Romm D, Perrin JM. Obesity and the built environment among Massachusetts children. Clin Pediatr. 2009;48(9):904‐912. [DOI] [PubMed] [Google Scholar]
- 96. Pabayo R, Spence JC, Cutumisu N, Casey L, Storey K. Sociodemographic, behavioural and environmental correlates of sweetened beverage consumption among pre‐school children. Public Health Nutr. 2012;15(8):1338‐1346. [DOI] [PubMed] [Google Scholar]
- 97. Park S, Choi BY, Wang Y, Colantuoni E, Gittelsohn J. School and neighborhood nutrition environment and their association with students' nutrition behaviors and weight status in Seoul, South Korea. J Adolesc Health. 2013;53:655‐662.e12. [DOI] [PubMed] [Google Scholar]
- 98. Powell LM, Bao Y. Food prices, access to food outlets and child weight. Econ Hum Biol. 2009;7(1):64‐72. [DOI] [PubMed] [Google Scholar]
- 99. Powell LM, Han E. The costs of food at home and away from home and consumption patterns among U.S. adolescents. J Adolesc Health. 2011;48:20‐26. [DOI] [PubMed] [Google Scholar]
- 100. Salois MJ. The built environment and obesity among low‐income preschool children. Health Place. 2012;18(3):520‐527. [DOI] [PubMed] [Google Scholar]
- 101. Sanchez BN, Sanchez‐Vaznaugh EV, Uscilka A, Baek J, Zhang L. Differential associations between the food environment near schools and childhood overweight across race/ethnicity, gender, and grade. Am J Epidemiol. 2012;175(12):1284‐1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Seliske LM, Pickett W, Boyce WF, Janssen I. Association between the food retail environment surrounding schools and overweight in Canadian youth. Public Health Nutr. 2009;12:1384‐1391. [DOI] [PubMed] [Google Scholar]
- 103. Shareck M, Lewis D, Smith NR, Clary C, Cummins S. Associations between home and school neighbourhood food environments and adolescents' fast‐food and sugar‐sweetened beverage intakes: findings from the Olympic Regeneration in East London (ORiEL) Study. Public Health Nutr. 2018;21:2842‐2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Shier V, Nicosia N, Datar A. Neighborhood and home food environment and children's diet and obesity: evidence from military personnel's installation assignment. Soc Sci Med. 2016;158:122‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Svastisalee CM, Holstein BE, Due P. Fruit and vegetable intake in adolescents: association with socioeconomic status and exposure to supermarkets and fast food outlets. J Nutr Metab. 2012;2012:185484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Svastisalee C, Pagh Pedersen T, Schipperijn J. Fast‐food intake and perceived and objective measures of the local fast‐food environment in adolescents. Public Health Nutr. 2016;19(3):446‐455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Tang X, Ohri‐Vachaspati P, Abbott JK, et al. Associations between food environment around schools and professionally measured weight status for middle and high school students. Child Obes. 2014;10(6):511‐517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Timperio A, Ball K, Roberts R, Campbell K, Andrianopoulos N, Crawford D. Children's fruit and vegetable intake: associations with the neighbourhood food environment. Prev Med. 2008;46(4):331‐335. [DOI] [PubMed] [Google Scholar]
- 109. Van Hulst A, Barnett TA, Gauvin L, et al. Associations between children's diets and features of their residential and school neighbourhood food environments. Can J Public Health. 2012;103:eS48‐eS54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Wall MM, Larson NI, Forsyth A, et al. Patterns of obesogenic neighborhood features and adolescent weight: a comparison of statistical approaches. Am J Prev Med. 2012;42(5):e65‐e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Wasserman JA, Suminski R, Xi J, Mayfield C, Glaros A, Magie R. A multi‐level analysis showing associations between school neighborhood and child body mass index. Int J Obes. 2014;38:912‐918. [DOI] [PubMed] [Google Scholar]
- 112. Williams J, Scarborough P, Townsend N, et al. Associations between food outlets around schools and BMI among primary students in England: a cross‐classified multi‐level analysis. PLoS ONE. 2015;10(7):e0132930‐e0132930. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Funnel plot for meta‐analysis of associations between presence of fast‐food restaurants in the neighborhood and childhood overweight/obesity
Figure S2. Funnel plot for meta‐analysis of associations between density of fast‐food restaurants in the neighborhood and childhood overweight/obesity
Table S1. Measures of access to fast‐food restaurants (FFRs), weight‐related behaviors, and body‐weight status in the included studies (see [ref] in the main text)
Table S2. Study quality assessment (see [ref] in the main text)


