Summary
Urban sprawl is thought to be a risk factor for childhood obesity primarily because the physical environment it creates discourages children's physical activity while encouraging their sedentary behavior. However, there has not been any review on the association between urban sprawl and childhood obesity. This study filled this research gap by comprehensively reviewing literature focusing on associations between urban sprawl and weight‐related behaviors and outcomes among children and adolescents. Only two longitudinal and three cross‐sectional studies conducted in two countries were identified. Sample sizes ranged from 2324 to 129 781. Four studies used weight status, and only one study used both behaviors and weight status as outcome variables. All positive, negative, and non‐significant associations were reported. This review could not identify a clear association between urban sprawl and childhood obesity. More longitudinal studies are needed for in‐depth analyses on this important topic in more regions, which would be important not only for public health guidelines but also for research, practice, and policies in urban planning.
Keywords: built environment, obesity, physical activity, urban sprawl
1. INTRODUCTION
Obesity, a prolonged condition of being abnormally or excessively overweight, is a leading cause of morbidity and premature mortality worldwide. Not only is obesity a significant health problem in its own right, it is also one of the key risk factors for other non‐communicable diseases. 1 For instance, overweight/obesity has been linked to approximately 58% of all individuals with diabetes and 8–41% of people with different types of cancers 2 , 3 ; higher rates of deaths for a wide range of cancers have also been attributed to obesity. 4 As in adults, obesity in children also causes, among other serious health problems, hypertension, gallbladder disease, and various psychosocial distempers that impair their quality of life. 5 Moreover, childhood obesity has lifecourse effects as children and adolescents with obesity are more likely to persist with obesity into adulthood compared with their counterparts without obesity. 6 In 2016, about 39% of men and 39% of women suffered from obesity and overweight, and 18% of children and adolescents were overweight or obese; by 2035, the obesity (including overweight) share of the global population is predicted to reach 45% or nearly 4 billion people given population projections by the United Nations. 7
An increasingly obesogenic, or obesity‐inducing, environment may account for the growing prevalence of childhood obesity, which is mainly determined by the built and food environments. 8 , 9 , 10 , 11 , 12 Also, many reviews have been conducted to synthesize this evidence. 6 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 However, most, if not all, such reviews have focused on neighborhood environmental factors; environmental factors beyond the neighborhood level have been relatively understudied. Urban sprawl is one such obesogenic environmental factor. Urbanization has been most rapid in developing economies, but urban sprawl has become increasingly pronounced in developed economies such as the United States and European Union. 23 It can be generally defined as the expansion of built land cover with low population density, with change characterized by the speed of urban area growth outstripping the speed of population growth. This often leads to the inefficient use of land resources as well as higher energy use and material throughput, prompting scientists to characterize the phenomenon as being environmentally unsustainable. 24 , 25 , 26 , 27 In addition to its impacts on land and climate, urban sprawl can also generate public health challenges. Perhaps most significantly with relation to its effects on lifestyle choices, the physical environment it creates discourages residents from walking since different functional zones are separated by distances that are not walkable from the standpoint of practical, daily activities. 28 Furthermore, children living in urban sprawl may be discouraged from outdoor physical activity (PA) due to safety concerns.
This study attempts to examine how urban sprawl is associated with childhood obesity outcomes. To the best of our knowledge, there have been no systematic reviews focusing on the association between urban sprawl and weight‐related behaviors or outcomes among children and/or adolescents. This study fills this research gap by systematically reviewing all relevant existing studies on this important public health issue. We tested our hypothesis that urban sprawl is associated with lower PA levels but higher levels of sedentary behaviors and thereby weight gain. Furthermore, this review contributes to the existing literature by summarizing multiple types of measures of urban sprawl and demonstrating the heterogeneities in the associations between those measures and various measures of weight‐related behaviors and outcomes. Our findings provide a comprehensive and up‐to‐date summary and interpretation of the scientific evidence on how a key dimension of urbanization may affect childhood health. This, in turn, could serve as an important reference for aligning urban planning, a key goal of which is the control of urban sprawl, 23 , 29 with the imperatives of public health in which the curtailment of the childhood obesity epidemic is increasingly urgent. 30 , 31
2. METHODS
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses. 32
2.1. Study selection criteria
Inclusion in this review required studies to meet all of the following criteria: (1) article type: peer‐reviewed original research; (2) study design: longitudinal and cross‐sectional studies; (3) study subject: children and adolescents aged <18; (4) exposure of interest: urban sprawl; (5) study outcome: individual‐level weight‐related behaviors (e.g., exercise, diet and active transportation) or outcomes (e.g., body mass index, overweight and obesity); (6) time of publication: from the inception of the given electronic bibliographic database to 31 December 2018; and (7) article language: written in English.
2.2. Search strategy
A keyword search was performed in PubMed and Web of Science (Appendix A), following a search strategy that included all possible combinations of keywords from the three groups related to urban sprawl, children, and weight‐related behaviors or outcomes. Two reviewers independently screened the titles and abstracts of the articles identified through the keyword search and retrieved potentially relevant articles for the full‐text review; discrepancies were resolved by a third reviewer. Three reviewers independently reviewed the identified articles and jointly determined the final list of articles included in the review.
2.3. Data extraction and preparation
A standardized data extraction form was used to collect methodological and outcome variables from each selected study, including the names of the authors, the year of publication, study design, period, area, scale and dataset, sample size, age and other characteristics, statistical model(s), measures of urban sprawl and weight‐related behaviors and/or outcomes and key findings on the association between urban sprawl and weight‐related behaviors and/or outcomes. Two reviewers independently extracted data from each included study, with discrepancies resolved by a third reviewer.
2.4. Study quality assessment
We used the National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies to assess the quality of each included study (Appendix B). This assessment tool rates each study based on 14 criteria; for each criterion, a score of 1 was assigned if ‘yes’ was the response, whereas a score of 0 was assigned otherwise (i.e., an answer of ‘no,’ ‘not applicable,’ ‘not reported’ or ‘cannot determine’). A study‐specific global score ranging from 0 to 14 was calculated by summing the scores across all criteria. The study quality assessment helped to measure the strength of the scientific evidence in each included study but was not used to determine whether or not a given study was included.
3. RESULTS
3.1. Study selection
Figure 1 shows the study selection flow chart. We identified a total of 286 articles through the keyword search. After undergoing title and abstract screening, 260 articles were excluded. The full texts of the remaining 26 articles were reviewed against the study selection criteria. Of these, 21 articles were further excluded. The remaining five studies that examined the association between urban sprawl and children's weight‐related behaviors and/or outcomes were included in this review.
FIGURE 1.
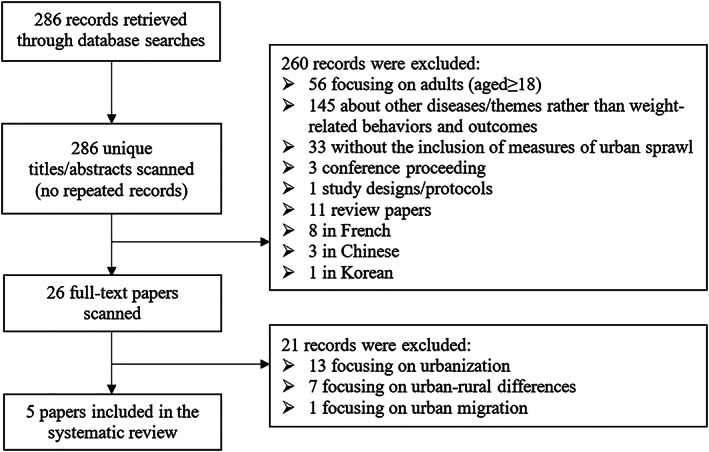
Study exclusion and inclusion flowchart
3.2. Study characteristics
Table 1 summarizes the basic characteristics of the five included studies, which were two longitudinal studies, both conducted in the United States, and three cross‐sectional studies, two in the United States and one in Canada. Sample sizes ranged from 2324 to 129 781, aged from 2 to 18. Samples were children in three studies and adolescents in four studies.
TABLE 1.
Basic characteristics of five included studies
| First author (year) | Study design a (period) | Study area b (scale) | Sample characteristics | Sample size | Sample age c | Dataset used | Statistical model |
|---|---|---|---|---|---|---|---|
| Ewing (2006) 33 | C (1997) | US (N) | Adolescents | 6760 | 12–17, 18–23 between 1997 and 2003 | • Round‐1 (1997) data of 1997 National Longitudinal Survey of Youth (NLSY97) | Multilevel logistic regression |
| C (2002) | Adolescents | 5815 | • Round‐6 (2002) data of 1997 National Longitudinal Survey of Youth (NLSY97) | ||||
| L (1997–2003) | Adolescents lived in the same county throughout survey | 3367 | • All consecutive rounds of NLSY97 from 1997 through 2003 | ||||
| L (1997–2003) | Adolescents moved | 3567 | • The intercounty movers of all consecutive rounds of NLSY97 from 1997 to 2003 | ||||
| Guarnizo‐Herreño (2019) 34 | C (2003) C (2007) C (2011–2012) | US (N) | Children and adolescents | 129 781 | 10–17 between 2003 and 2012 | National Surveys of Children's Health (NSCH) | Linear probability regression |
| Guettabi (2014) 35 | L (1988–2008) | US (N) | Children | 2324 | 2–17 between 1988 and 2008 | • 1979 National Longitudinal Survey of Youth (NLSY79)• The NLSY79 Child Survey |
• Linear regression • First difference estimation |
| Schwartz (2011) 36 | C (2001–2008) | 31‐county region of Pennsylvania, US (C31) | Children and adolescents | 47 769 | 5–18 between 2001 and 2008 | • Electronic health record (EHR): individual‐level data• Pennsylvania Spatial Data Access: (PASDA) place‐level data for Pennsylvania | Multilevel logistic regression |
| Seliske (2012) 37 | C (2007, 2008) | 33 census metropolitan areas (CMA), Canada (C33) | Adolescents | 7017 | 12–19 in 2007, 2008 | • Canadian Community Health Survey (CCHS) | Multilevel logistic regression |
Abbreviation: NA, not available.
Study design: C, cross‐sectional; L, longitudinal.
Study scale: (N), National; (Nn), n countries; (C), city; (Cn), n cities.
Sample age: age in baseline year for cohort studies or mean age in survey year for cross‐sectional studies.
3.3. Measures of urban sprawl
Urban sprawl in the included studies was directly measured as the proportion of state population living in the central cities of a given metropolitan statistical area (a higher proportion reflects lower urban sprawl) and the distance to the nearest micro/metropolitan area (Table 2). It was also measured by the sprawl index at different scales: the urban sprawl index in a Canadian study was constructed through principal components analysis (PCA) on the basis of the three urban sprawl components related to population distribution and dwelling density (i.e., dwelling density, percentage of single or detached dwellings and percentage of the population living in the urban core) and standardized (with a mean of 0 and a standard deviation of 1) 37 ; the county sprawl index and the metropolitan index of sprawl, used by three US studies, was constructed through PCA by combining gross population density, percentage of population living at low population densities, percentage of population living at high population densities, county population divided by the amount of urban land, average block size and percentage of blocks with small block sizes. 33 , 35 , 36
TABLE 2.
Measures of urban sprawl and weight‐related behaviors and outcomes in five included studies
| First author (year) | Measures of urban sprawl | Weight‐related outcomes | Weight‐related behaviours | Other factors adjusted for |
|---|---|---|---|---|
| Ewing (2006) 33 | • County sprawl index, calculated based on the six variables through PCA: gross population density, % of population living at low population densities, % of population living at high population densities, county population divided by the amount of urban land, average block size and % of blocks with small block sizes |
• Reported BMI • Overweight (BMI ≥ 85th percentile on the CDC growth charts) |
NA |
• Individual variables: age, gender, race/ethnicity, smoking, hours worked, TV watching, exercise and fruit and vegetable consumption • SES features: highest grade completed by respondent, highest grade attained by a household member, household income, • Crime rates • Climate variables |
| Guarnizo‐Herreño (2019) 34 | • % of the state population living in the central cities of the metropolitan statistical areas |
• Obesity (reported BMI ≥ 95th percentile on the age and gender specific BMI distribution in the NSCH datasets) • Overweight or obesity (BMI ≥ 85th percentile on the age and gender specific BMI distribution in the NSCH datasets) |
NA | • Household income |
| Guettabi (2014) 35 |
• Metropolitan index of sprawl, calculated based on the six variables through PCA: gross population density, % of population living at low population densities, % of population living at high population densities, county population divided by the amount of urban land, average block size and % of blocks with small block sizes • Distance to the nearest micro/metropolitan area |
• Measured BMI | NA |
• SES features: mother education, family income • County personal income • County government transfer • Incremental distances from urban centers of different hierarchy |
| Schwartz (2011) 36 | • County sprawl index, calculated by the six variables through PCA: gross population density, % of population living at low population densities, % of population living at high population densities, county population divided by the amount of urban land, average block size and % of blocks with small block sizes | • Measured BMI | NA | NA |
| Seliske (2012) 37 | • Urban sprawl index was calculated by the following three variables through PCA: dwelling density, % of single or detached dwellings and % of the population living in the urban core | • Reported BMI• Overweight and obesity (based on age‐ and sex‐specific International Obesity Task Force pediatric BMI thresholds) |
• MVPA (≥60 min per day or <60 min per day) • Active transportation (≥30 min per day or <30 min per day) |
• Season of survey interview • Climate: daily temperature, annual rainfall, annual snowfall • SES features: household education, household income, community size |
Abbreviations: BMI, body mass index; CDC, Center for Disease Control and Prevention; MVPA, moderate‐to‐vigorous physical activity; NSCH, National Surveys of Children's Health; PCA, principal component analysis; SES, socio‐economic status.
3.4. Measures of weight‐related behaviors and outcomes
One study with weight‐related behaviors as outcome variables of interest measured moderate‐to‐vigorous PA and the use of active transportation 37 (Table 3). Body mass index (BMI), calculated by dividing weight (kg) by squared height (m2), was used as a weight outcome in all five studies, self‐reported in three studies and measured in two studies. Overweight/obesity status was used in three studies but defined by different references: the US Center for Disease Control and Prevention (CDC) growth charts, the International Obesity Task Force pediatric BMI thresholds and BMI distribution in the National Surveys of Children's Health (NSCH) datasets.
TABLE 3.
Associations between urban sprawl and weighted‐related behaviors and outcomes in five included studies
| First author (year) | Main findings on the association between urban sprawl and: | |
|---|---|---|
| Weight‐related behavior | Weight‐related outcome | |
| Ewing (2006) 33 (including two longitudinal and two cross‐sectional analyses) | NA |
(Cross‐Sectional Analysis Based on Round‐1 [1997] Data) • The county sprawl index was related to overweight in the expected direction at a significant level (β = −.0045, p = .014), after controlling for individual household characteristics and TV watching. |
|
(Cross‐Sectional Analysis Based on Round‐6 [2002] Data) • The association between the county sprawl index and obesity was statistically significant after controlling for exercise, diet and TV watching (β = −.0026, p = .048). | ||
|
(Longitudinal Analysis Based on all Consecutive Rounds) • Neither BMI at the mean age nor BMI growth with age was related to county sprawl, although both had the expected signs (β = −.00082, p = .78), after controlling for other predictors. | ||
|
(Longitudinal Analysis Based on the intercounty movers of all Consecutive Rounds) • The difference in degree of sprawl between counties was not associated with weight gain as measured by BMI after move (β = −.00022, p = .88), after controlling for other predictors. | ||
| Guarnizo‐Herreño (2019) 34 | NA |
• Overall, the proportion of population living in central cities was negatively associated with overweight/obesity (β = −.126, p < .05). • Among children from low‐income households, the proportion of population living in central cities was negatively associated with overweight/obesity (β = −.229, p < .01). • Among children from higher‐income households, the proportion of population living in central cities was positively associated with overweight/obesity (β = .114, p < .05). |
| Guettabi (2014) 35 | NA | • The association between the metropolitan index of sprawl and BMI was statistically significant (β = −.0352, p < .05). |
| Schwartz (2011) 36 | NA | • County sprawl index was associated with BMI in older children aged 10–18 (β = .009, p = .002). |
| Seliske (2012) 37 | • Urban sprawl was associated with active transportation among 12‐ to 15‐year‐old (OR per SD increase = 1.24; 95% CI, 1.10–1.39).• For the entire sample aged 12–19, higher urban sprawl was associated with higher MVPA (OR per SD increase = 1.10; 95% CI, 1.01–1.20). | • No association between urban sprawl and overweight/obesity was found (OR per SD increase = 1.06; 95% CI, 0.94–1.18). |
Abbreviations: BMI, body mass index; MVPA, moderate‐to‐vigorous physical activity; OR, odds ratio; SD, standard deviation.
3.5. Associations between urban sprawl and weight‐related behaviors and outcomes
One study in Canada reported a significant association between urban sprawl and engagement in at least 30 min of active transportation per day (OR = 1.24; 95% CI, 1.10–1.39) and moderate‐to‐vigorous PA (OR = 1.10; 95% CI, 1.01–1.20). 37 All five studies investigated the association between urban sprawl and weight‐related outcomes. Two studies conducted longitudinal analyses of which one study reported a non‐significant association between the county sprawl index and BMI, 33 and one study reported a negative association between the Metropolitan index of sprawl and BMI (β = −.0352, p < .05). 35 Four studies conducted cross‐sectional analyses. Two of them did not observe a significant association between the county sprawl index and BMI 33 and between the urban sprawl index and overweight/obesity status. 37 One study reported a negative association between the county sprawl index and overweight (β = −.0045, p = .014). 33 Two studies found a positive association between the proportion of state population living in the central cities of the metropolitan areas and overweight/obesity (β = −.126, p < .05) 34 and between the county sprawl index and BMI (β = .009, p = .002). 36 Also, one study reported opposite results in stratified analyses by income level, finding that urban sprawl, measured by the proportion of state population living in the central cities of the metropolitan areas, was associated with increased overweight/obesity among lower income households and with decreased overweight/obesity among higher income households. 34
3.6. Study quality assessment
Table 4 reports criterion‐specific and global ratings from the study quality assessment of the included articles. Five studies scored 9.8 out of 14 on average, with a range from 8 to 12.
TABLE 4.
Study quality assessment (see 14 questions in Appendix B)
| First author (year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ewing (2006) 33 | Y | Y | Y | Y | N | Y | Y | Y | NA | Y | Y | Y | Y | Y | 12 |
| Guarnizo‐Herreño (2019) 34 | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | NA | Y | 10 |
| Guettabi (2014) 35 | Y | Y | N | Y | N | Y | Y | Y | Y | NA | Y | Y | NA | Y | 10 |
| Schwartz (2011) 36 | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | NA | N | 9 |
| Seliske (2012) 37 | Y | Y | N | Y | N | N | N | Y | Y | N | Y | Y | NA | Y | 8 |
Abbreviation: NA, not available.
4. DISCUSSION
This study systematically reviewed existing research on the association between urban sprawl and obesity among children and adolescents. We included five eligible studies, and their findings were not consistent with one another. The association between urban sprawl and obesity was found to be negative in two studies, positive in two studies and not significant in one study. Given the limited number of included studies and inconsistencies of their conclusions, we could not conclusively report a scientifically credible consensus on the association between childhood/adolescent obesity and urban sprawl.
This study is the first to systematically review the existing scientific literature on the association between urban sprawl and childhood obesity. However, some previous studies, although not specifically reviewing the association between urban sprawl and childhood obesity, have also reported relevant findings. For instance, urban sprawl, together with access to equipment and facilities and neighborhood pattern (e.g., suburban or urban), was found to contribute to the physical environment in which childhood obesity was prevalent. 38 Also, a review on the association between the urban built environment and childhood obesity reported the potential influence of urban sprawl on PA levels. 39
We found that the association between urban sprawl and childhood obesity varied by family socio‐economic status. For example, the association between urban sprawl and obesity was negative among children from high‐income families and positive among their counterparts from low‐income families. 34 Several explanations may underlie these associations. Compared with high‐income families, children from low‐income families may experience greater commuting time and less PA opportunities. On the other hand, high‐income families often have higher educational attainment and health literacy, so the arrangement of calorie intake and output and leisure‐time PA may be more reasonable. 40 Ewing et al. showed that children living in sprawling counties in the United States were more likely to have overweight than those living in compact counties. 33 A possible reason may be that, compared with counties with large populations, children living in compact counties tended to exercise less and engage in more sedentary activities, such as television‐watching and other indoor leisure. However, Seliske et al. found that a high degree of urban sprawl was associated with higher odds of PA and more use of active transportation, although no associations between urban sprawl and childhood obesity were found. 37
There are several aspects of the current research on this topic that can be improved or further explored. More objective measures of obesity and related health outcomes or behaviors should be adopted, such as waist circumference, waist‐to‐hip ratio, body fat, PA intensity and TV‐watching duration and frequency. However, studies on urban sprawl also need a large sample size. Variables such as the duration of video game playing, TV watching, and other sedentary activities are difficult to accurately measure across large populations. For example, Ewing et al. 33 and Seliske et al. 37 used subjective measures (i.e., reported BMI and PA), which may underestimate actual BMI values 41 and overestimate the actual PA levels, 42 affecting the strength of the observed associations. Also, results might vary across outcome variables. For example, Ewing et al. showed that the county sprawl index was negatively associated with overweight in cross‐sectional analyses, 33 which, however, was not significant in longitudinal analyses for all subjects and intercounty movers 33 ; by contrast, a negative association was found in another longitudinal study. 14 In addition, the built environment was measured at county level in some studies 33 , 35 , 36 , 37 and at state level in other studies, 34 which could be better measured at a daily spatial extent of activity for most children and adolescents. 43
Our study has several limitations. First, we did not undertake meta‐analyses. This was due to the small sample size and the different methods used across the included studies, which meant that we were unable to calculate the standardized effect sizes of the predictor variables. Second, various outcome variables were used in the included studies, such as BMI, overweight and obesity (defined differently in various studies). These different measures should be interpreted separately. Third, there were also differences in the measurements of urban sprawl. Urban sprawl is often defined in terms of land use diversity (or lack thereof) and the centering (or lack thereof) of the resident population. 44 Therefore, we suggest that future studies should use consistent urban sprawl indicators or a fixed set of indices in the same study (e.g., multiscale studies), facilitating comparability across studies. Lastly, most of the studies in this review were cross‐sectional designs. More longitudinal studies should be conducted in the future to reveal a causal relationship between urban sprawl and obesity and/or related behaviors.
This study has important implications for future research and practice. First, more research is needed to determine the association between urban sprawl and childhood/adolescent obesity and relevant behaviors. A recent systematic review showed that multicomponent behavior‐changing interventions incorporating diet, PA and behavioral changes may contribute to achieving small, short‐term reductions in BMI, BMI z‐scores and weight levels in children aged 6–11 years. 45 However, relatively few studies have explored the association between urban sprawl and these health‐related behaviors. Note that urbanization is a commonly used variable, which should be differentiated from urban sprawl. 46 , 47 , 48 , 49 , 50 A more explicit distinction needs to be made between urban sprawl and urbanization in future research: Sprawl is not urbanization or suburbanization generally but rather a specific form of urban and suburban development; urbanization on the basis of population density, transportation and infrastructure measures may be more likely to capture the impact of urban sprawl on built environments than simply calculating the level of urbanization based on population density. 49 Also, urban sprawl in most of the included studies has been measured by indices related to residential density, which may not be able to fully capture the effects of urban sprawl. Earth observation technologies should be used for this purpose, so urban sprawl can be more accurately measured and consistently defined in future studies. 51 , 52 Doing so would also lead to better quality reporting of such obesogenic environmental research, which could enhance the comparability among studies and hence form stronger, more consistent and more actionable evidence. 53 , 54 In addition, included studies were conducted in only the United States and Canada, but urban sprawl also occurs in many other countries, while the prevalence of childhood obesity is increasing worldwide. In‐depth studies of Europe and Asia, 55 , 56 , 57 , 58 for instance, could provide a more comprehensive and balanced picture of the association between urban sprawl and childhood/adolescent obesity.
5. CONCLUSIONS
This systematic review of the existing literature found a mixed association between urban sprawl and weight‐related behaviors/outcomes among children and adolescents, with relevant results insufficiently consistent to yield a consensus conclusion. However, longitudinal studies were limited, and measures of urban sprawl were diverse. More longitudinal research using a set of standard measures of urban sprawl at multiple scales should be conducted in more regions, especially outside the United States and Canada, to confirm their association with childhood/adolescent obesity and weight‐related behaviors. Future studies and further reviews could provide important insights into the association between the urban environment and children's health, thereby providing evidence and guidance for urban and public transport policies.
CONFLICT OF INTEREST
We declare no conflicts of interest.
ACKNOWLEDGEMENTS
We thank the International Institute of Spatial Lifecourse Epidemiology (ISLE) and the State Key Laboratory of Urban and Regional Ecology of China (SKLURE2018‐2‐5) for research support.
APPENDIX A. SEARCH STRATEGY
The search strategy includes all possible combinations of keywords in the title/abstract from the following three groups:
‘urban sprawl*,’ ‘urban growth*,’ ‘urban expansion*,’; ‘metropolitan sprawl*,’ ‘metropolitan growth*,’ ‘metropolitan expansion*,’ ‘suburban sprawl*,’ ‘suburban growth *,’ ‘suburban expansion*,’ ‘sub‐urban sprawl*,’ ‘sub‐urban growth*,’ ‘sub‐urban expansion*,’ ‘urban/suburban sprawl*,’ ‘urban/sub‐urban sprawl*,’ ‘urban‐suburban sprawl*,’ ‘urban/suburban growth*,’ ‘urban/sub‐urban growth*,’ ‘urban‐suburban growth*,’ ‘urban/suburban expansion*,’ ‘urban/sub‐urban expansion*,’ ‘urban‐suburban expansion*,’ ‘county sprawl*,’ ‘county growth*,’ ‘county expansion*’;
‘child*,’ ‘juvenile*,’ ‘pubescent*,’ ‘pubert*,’ ‘adolescen*,’ ‘youth*,’ ‘teen*,’ ‘kid*,’ ‘young*,’ ‘youngster*,’ ‘minor*,’ ‘student*,’ ‘pupil*,’ ‘pediatric*,’ ‘preschooler*,’ ‘pre‐schooler*,’ ‘schoolchild*,’ ‘school‐child*,’ ‘school child*,’ ‘schoolage*,’ ‘school‐age*,’ ‘school age*’;
‘diet*,’ ‘diet behavio*,’ ‘dietary behavio*,’ ‘eating*,’ ‘eating behavio*,’ ‘food*,’ ‘food intak*,’ ‘food consum*,’ ‘energy intak*,’ ‘energy consum*,’ ‘energy balance,’ ‘calorie*,’ ‘caloric intak*,’ ‘physical activit*,’ ‘physical exercis*,’ ‘exercis*,’ ‘body activit*,’ ‘body mass index,’ ‘BMI,’ ‘weight,’ ‘weight status,’ ‘weight‐related behavio*,’ ‘weight‐related health,’ ‘overweight,’ ‘obese,’ ‘obesity,’ ‘adiposity,’ ‘abdominal overweight,’ ‘abdominal obesity,’ ‘central overweight,’ ‘central obesity,’ ‘central adiposity,’ ‘waist circumference,’ ‘waist to hip,’ ‘waist‐to‐hip,’ ‘waist to height,’ ‘waist‐to‐height,’ ‘waist to stature,’ ‘waist‐to‐stature,’ ‘fatness,’ ‘body fat,’ ‘excess fat,’ ‘excess weight,’ ‘overnutrition,’ ‘over‐nutrition,’ ‘over nutrition.’
APPENDIX B. THE US NATIONAL INSTITUTES OF HEALTH (NIH)'S QUALITY ASSESSMENT TOOL FOR OBSERVATIONAL COHORT AND CROSS‐SECTIONAL STUDIES (AVAILABLE FROM https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools)
Was the research question or objective in this paper clearly stated?
Was the study population clearly specified and defined?
Was the participation rate of eligible persons at least 50%?
Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?
Was a sample size justification, power description or variance and effect estimates provided?
For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?
Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?
For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure or exposure measured as continuous variable)?
Were the exposure measures (independent variables) clearly defined, valid, reliable and implemented consistently across all study participants?
Was the exposure(s) assessed more than once over time?
Were the outcome measures (dependent variables) clearly defined, valid, reliable and implemented consistently across all study participants?
Were the outcome assessors blinded to the exposure status of participants?
Was loss to follow‐up after baseline 20% or less?
Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
Wu T, Yang S, Liu M, et al. Urban sprawl and childhood obesity. Obesity Reviews. 2021;22(S1):e13091. 10.1111/obr.13091
Tong Wu and Shujuan Yang contributed equally.
[Correction added on 3 February 2021, after first online publication: Peng Jia's correspondence details have been updated. Also, affiliations 7 and 8 were interchanged.]
Contributor Information
Miyang Luo, Email: lmy4300@gmail.com.
Peng Jia, Email: jiapengff@hotmail.com.
REFERENCES
- 1. World Health Organization . International statistical classification of diseases and related health problems. 1 World Health Organization; 2004. [Google Scholar]
- 2. Chen D‐R, Truong K. Using multilevel modeling and geographically weighted regression to identify spatial variations in the relationship between place‐level disadvantages and obesity in Taiwan. Applied Geography. 2012;32(2):737‐745. [Google Scholar]
- 3. Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body‐mass index and incidence of cancer: a systematic review and meta‐analysis of prospective observational studies. Lancet (London, England). 2008;371(9612):569‐578. [DOI] [PubMed] [Google Scholar]
- 4. Calle EE, Rodriguez C, Walker‐Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625‐1638. [DOI] [PubMed] [Google Scholar]
- 5. Pouliou T, Elliott SJ. An exploratory spatial analysis of overweight and obesity in Canada. Prev Med. 2009;48(4):362‐367. [DOI] [PubMed] [Google Scholar]
- 6. Xin J, Zhao L, Wu T, et al. Association between access to convenience stores and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Revels S, Kumar SA, Ben‐Assuli O. Predicting obesity rate and obesity‐related healthcare costs using data analytics. Health Policy and Technology. 2017;6(2):198‐207. [Google Scholar]
- 8. Jia P, Xue H, Cheng X, Wang Y, Wang Y. Association of neighborhood built environments with childhood obesity: evidence from a 9‐year longitudinal, nationally representative survey in the US. Environ Int. 2019;128:158‐164. [DOI] [PubMed] [Google Scholar]
- 9. Wang Y, Jia P, Cheng X, Xue H. Improvement in food environments may help prevent childhood obesity: evidence from a 9‐year cohort study. Pediatr Obes. 2019;14(10):e12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang X, Zhang M, Zhao Z, et al. Obesogenic environmental factors of adult obesity in China: a nationally representative cross‐sectional study. Environ Res Lett. 2020;15(4):044009. [Google Scholar]
- 11. Pereira M, Nogueira H, Padez C. Association between childhood obesity and environmental characteristics: testing a multidimensional environment index using census data. Applied Geography. 2018;92:104‐111. [Google Scholar]
- 12. Jia P, Xue H, Cheng X, Wang Y. Effects of school neighborhood food environments on childhood obesity at multiple scales: a longitudinal kindergarten cohort study in the USA. BMC Med. 2019;17(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jia P, Cheng X, Xue H, Wang Y. Applications of geographic information systems (GIS) data and methods in obesity‐related research. Obes Rev. 2017;18(4):400‐411. [DOI] [PubMed] [Google Scholar]
- 14. Jia P, Luo M, Li Y, Zheng JS, Xiao Q, Luo J. Fast‐food restaurant, unhealthy eating, and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jia P, Zou Y, Wu Z, et al. Street connectivity, physical activity, and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhou Q, Zhao L, Zhang L, et al. Neighborhood supermarket access and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xu F, Jin L, Qin Z, et al. Access to public transport and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang Z, Zhao L, Huang Q, et al. Traffic‐related environmental factors and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li Y, Luo M, Wu X, Xiao Q, Luo J, Jia P. Grocery store access and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yang S, Zhang X, Feng P, et al. Access to fruit and vegetable markets and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zou Y, Ma Y, Wu Z, et al. Neighbourhood residential density and childhood obesity. Obes Rev. 2021;22(Suppl 1):e13037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pan X, Zhao L, Luo J, et al. Access to bike lanes and childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2021;22(Suppl 1):e13042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fertner C, Jørgensen G, Sick Nielsen TA, Bernhard Nilsson KS. Urban sprawl and growth management – drivers, impacts and responses in selected European and US cities. Future Cities Environ. 2016;2(0):9. [Google Scholar]
- 24. Li G, Li F. Urban sprawl in China: differences and socioeconomic drivers. Sci Total Environ. 2019;673:367‐377. [DOI] [PubMed] [Google Scholar]
- 25. Bhatta B, Saraswati S, Bandyopadhyay D. Urban sprawl measurement from remote sensing data. Appl Geography. 2010;30(4):731‐740. [Google Scholar]
- 26. Grimm NB, Faeth SH, Golubiewski NE, et al. Global change and the ecology of cities. Science. 2008;319(5864):756‐760. [DOI] [PubMed] [Google Scholar]
- 27. Jaeger JAG, Bertiller R, Schwick C, Kienast F. Suitability criteria for measures of urban sprawl. Ecol Indic. 2010;10(2):397‐406. [Google Scholar]
- 28. Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. A J Health Promotion: AJHP. 2003;18(1):47‐57. [DOI] [PubMed] [Google Scholar]
- 29. Wei YD, Ewing R. Urban expansion, sprawl and inequality. Landscape Urban Plan. 2018;177:259‐265. [Google Scholar]
- 30. Apovian CM. The obesity epidemic—understanding the disease and the treatment. N Engl J Med. 2016;374(2):177‐179. [DOI] [PubMed] [Google Scholar]
- 31. Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet (London, England). 2010;375(9727):1737‐1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Int J Surg. 2010;8(5):336‐341. [DOI] [PubMed] [Google Scholar]
- 33. Ewing R, Brownson RC, Berrigan D. Relationship between urban sprawl and weight of United States youth. Am J Prev Med. 2006;31(6):464‐474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Guarnizo‐Herreno CC, Courtemanche C, Wehby GL. Effects of contextual economic factors on childhood obesity. Matern Child Health J. 2019;23(10):1317‐1326. [DOI] [PubMed] [Google Scholar]
- 35. Guettabi M, Munasib A. Urban sprawl, obesogenic environment, and child weight. Journal of Regional Science. 2014;54(3):378–401. [Google Scholar]
- 36. Schwartz BS, Stewart WF, Godby S, et al. Body mass index and the built and social environments in children and adolescents using electronic health records. Am J Prev Med. 2011;41(4):e17‐e28. [DOI] [PubMed] [Google Scholar]
- 37. Seliske L, Pickett W, Janssen I. Urban sprawl and its relationship with active transportation, physical activity and obesity in Canadian youth. Health Rep. 2012;23(2):17‐25. [PubMed] [Google Scholar]
- 38. Dunton GF, Kaplan J, Wolch J, Jerrett M, Reynolds KD. Physical environmental correlates of childhood obesity: a systematic review. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity. 2009;10(4):393‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rahman T, Cushing RA, Jackson RJ. Contributions of built environment to childhood obesity. Mt Sinai J Med. 2011;78(1):49‐57. [DOI] [PubMed] [Google Scholar]
- 40. Cutilli CC, Bennett IM. Understanding the health literacy of America: results of the national assessment of adult literacy. Orthop Nurs. 2009;28(1):27‐32. quiz 33‐24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shields M, Connor Gorber S, Tremblay MS. Estimates of obesity based on self‐report versus direct measures. Health Rep. 2008;19(2):61‐76. [PubMed] [Google Scholar]
- 42. Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181‐188. [DOI] [PubMed] [Google Scholar]
- 43. Jia P. Spatial lifecourse epidemiology. The Lancet Planetary Health. 2019;3 (2):e57–e59. 10.1016/s2542-5196(18)30245-6. [DOI] [PubMed] [Google Scholar]
- 44. Ewing R, Meakins G, Hamidi S, Nelson AC. Relationship between urban sprawl and physical activity, obesity, and morbidity—update and refinement. Health Place. 2014;26:118‐126. [DOI] [PubMed] [Google Scholar]
- 45. Mead E, Brown T, Rees K, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6:CD012651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Inoue Y, Howard AG, Thompson AL, Gordon‐Larsen P. Secular change in the association between urbanisation and abdominal adiposity in China (1993‐2011). J Epidemiol Community Health. 2018;72(6):484‐490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013‐2016. JAMA. 2018;319(23):2410‐2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Klatka M, Zienkiewicz E, Kollataj W, Zienkiewicz T, Kollataj B. Socio‐economic development, level of urbanization and consumption of selected food products as factors in the prevalence of overweight and obesity among youths and young adults in Poland. Ann Agr Env Med AAEM. 2020;27(1):139‐145. [DOI] [PubMed] [Google Scholar]
- 49. Yang RJ, Sheu JJ, Chen HS, Lin KC, Huang HL. Morbidity at elementary school entry differs by sex and level of residence urbanization: a comparative cross‐sectional study. BMC Public Health. 2007;7(1):358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Protano C, Valeriani F, Macedonio A, et al. Family‐based social determinants and child health: cross‐sectional study. Pediatr Int. 2017;59(2):201‐208. [DOI] [PubMed] [Google Scholar]
- 51. Jia P, Stein A, James P, et al. Earth observation: investigating noncommunicable diseases from space. Annu Rev Public Health. 2019;40(1):85‐104. [DOI] [PubMed] [Google Scholar]
- 52. Jia P, Xue H, Yin L, Stein A, Wang M, Wang Y. Spatial technologies in obesity research: current applications and future promise. Trends Endocrinol Metab. 2019;30(3):211‐223. [DOI] [PubMed] [Google Scholar]
- 53. Jia P, Yu C, Remais JV, et al. Spatial Lifecourse epidemiology reporting standards (ISLE‐ReSt) statement. Health Place. 2020;61:102243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jia P, Lakerveld J, Wu J, et al. Top 10 research priorities in spatial lifecourse epidemiology. Environ Health Perspect. 2019;127(7):74501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jones RE, Jewell J, Saksena R, Ramos Salas X, Breda J. Overweight and obesity in children under 5 years: surveillance opportunities and challenges for the WHO European region. Front Public Health. 2017;5:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang X, Zhang M, Zhao Z, et al. Geographic variation in prevalence of adult obesity in China: results from the 2013‐2014 National Chronic Disease and Risk Factor Surveillance. Ann Intern Med. 2020;172(4):291‐293. [DOI] [PubMed] [Google Scholar]
- 57. Jia P, Ma S, Qi X, Wang Y. Spatial and Temporal Changes in Prevalence of Obesity Among Chinese Children and Adolescents, 1985‐2005. Prev Chronic Dis. 2019;16:190290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pineda E, Sanchez‐Romero LM, Brown M, et al. Forecasting future trends in obesity across Europe: the value of improving surveillance. Obes Facts. 2018;11(5):360‐371. [DOI] [PMC free article] [PubMed] [Google Scholar]


