Summary
Grocery store is usually considered to be a healthy food outlet as it provides access to a variety of healthy food, such as fruits and vegetables, which may potentially improve overall dietary quality and protect against obesity. However, findings of the association between grocery store and childhood obesity are controversial. This study aimed to systematically review the evidence on the association between access to grocery stores and childhood obesity. A literature search was conducted in the PubMed, Embase, and Web of Science for articles published before January 1, 2019, using the combinations of three groups of keywords separately for grocery store, children and adolescents, and weight‐related behaviours and outcomes. A total of 27 cross‐sectional and eight longitudinal studies were identified. Controversial results existed among 24 studies, which examined the association between the access to grocery stores and weight‐related outcomes. A null association was observed in almost all meta‐analyses conducted by different measures of grocery stores and weight status, except the analysis between presence of grocery stores and overweight, which reached borderline significance. For weight‐related behaviours, mixed findings were reported between grocery stores and dietary behaviours, and no significant associations were found for physical activity. This systematic review and meta‐analysis suggested that access to grocery stores may have a rather small influence on child weight.
Keywords: adolescent, child, dietary behaviour, grocery store, obesity, overweight, physical activity
1. INTRODUCTION
The prevalence of overweight and obesity in children and adolescents has risen dramatically worldwide in the past few decades, from 4% in 1975 to over 18% in 2016. 1 Overweight and obesity in childhood and adolescence is strongly associated with overweight in adulthood, 2 and may cause a wide range of serious complications, such as type 2 diabetes and cardiovascular diseases, and increase the risk of premature illness and death later in life. 3 It may also lead to a negative body image and several adverse mental and psychosocial consequences, such as being more likely to be socially inept 4 , 5 and academically unsuccessful. 6 , 7
It is widely accepted that the neighbourhood environment may interact with personal characteristics to affect individual weight status. 8 , 9 , 10 Grocery store is one of such obesogenic environmental factors, defined in the North American Industry Classification System (NAICS) as “a type of food stores selling a general line of food, such as canned and frozen foods, fresh fruits and vegetables, and fresh and prepared meats, fish, and poultry,” usually with annual sales of less than $2 million and less than 50 employees. 11 It is usually assumed to be a healthy food outlet as it provides children access to a variety of healthy food, such as fruits and vegetables, which may potentially improve overall dietary quality and protect youth against obesity. 12 However, findings of the association between grocery stores and childhood obesity are mixed. For example, grocery store was found positively associated with obesity among school children in some studies, 13 , 14 but negatively associated with obesity in other studies. 15 , 16
There is only one review that examined the association between grocery stores and childhood obesity, where a null association between grocery store and childhood obesity was found in more than 90% of the associations reported in the included studies. 17 However, this review was restricted to studies conducted in United States and Canada, and it only focused on weight‐related outcomes, including body mass index (BMI), BMI percentile, BMI z score, or overweight and obesity, without summarizing the results on weight‐related behaviours. In addition, the majority of articles included were cross‐sectional studies, and only a few studies conducted subgroup analysis in the previous review, while more studies with longitudinal study design and/or subgroup analysis were published in recent years. 18 Over the past decade, a growing number of studies were conducted to analyse this topic in various countries, 19 and it is necessary to conduct a systematic review of studies conducted globally and re‐analyse the association between access to grocery stores and childhood obesity.
Our review contributes to the literature in the following aspects. First, we reviewed existing longitudinal studies, cross‐sectional studies, case‐control studies, ecological studies, and intervention studies on the associations between grocery stores and childhood obesity. Second, we expanded the concept of the access to grocery stores to a full range of measurements (eg, the number of grocery stores, the density of grocery stores, and the proximity to the nearest grocery store) around multiple sites (eg, home and school), for a comprehensive understanding of the influences of grocery stores on childhood obesity. Third, we examined both body‐weight status as well as weight‐related behaviours (eg, diet, physical activity, and sedentary behaviour). Fourth, we may conduct subgroup analyses by country, type of measures (subjectively reported or objectively measured), and targeted site (home or school).
By this review, we aimed to systematically examine the association between access to grocery stores and weight‐related behaviours/outcomes among children and adolescents. Furthermore, we conducted a meta‐analysis to quantify the influence of grocery stores on childhood obesity.
2. METHODS
A systematic review and meta‐analysis were conducted in accordance with the Cochrane handbook version 5.1.0 and results of this study were reported by following the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist. 20
2.1. Study selection criteria
Studies that met all of the following criteria were included in the review: (a) study designs: longitudinal studies including prospective and retrospective cohort studies, cross‐sectional studies, case‐control studies, ecological studies, and intervention studies; (b) study subjects: children and adolescents aged less than 18 years; (c) exposure: grocery stores in the neighbourhood; (d) study outcomes: weight‐related behaviours (eg, diet, physical activity, and sedentary behaviour) and/or outcomes (eg, overweight and obesity measured by BMI, waist circumference, waist‐to‐hip ratio, and body fat); (e) article types: peer‐reviewed original research; (f) time of publication: from the inception of an electronic bibliographic database to 1 January 2019; and (g) language: articles written in English.
2.2. Search strategy
A keyword search was performed for related studies published before 1 January 2019 in three electronic bibliographic databases: PubMed, Embase, and Web of Science. The search strategy included all possible combinations of keywords for grocery store, child, and weight‐related behaviours and outcomes in the title or abstract field. Detailed search terms are described in Appendix A in the Data S1.
Titles and abstracts of the articles identified through the keyword search were screened against the study selection criteria. Potentially relevant articles were retrieved for an evaluation of the full text. Two reviewers independently conducted the title and abstract screening and identified potentially relevant articles for the full‐text review. Interrater agreement was assessed by using the Cohen kappa (κ = .90). Discrepancies were compiled and screened by a third reviewer. Three reviewers jointly determined the list of articles for the full‐text review through a discussion. Then, two reviewers independently reviewed the full texts of all articles in the list and determined the final pool of articles included in the review. Interrater agreement was again assessed by the Cohen kappa (κ = .77). Figure 1 shows the search and screening process.
FIGURE 1.
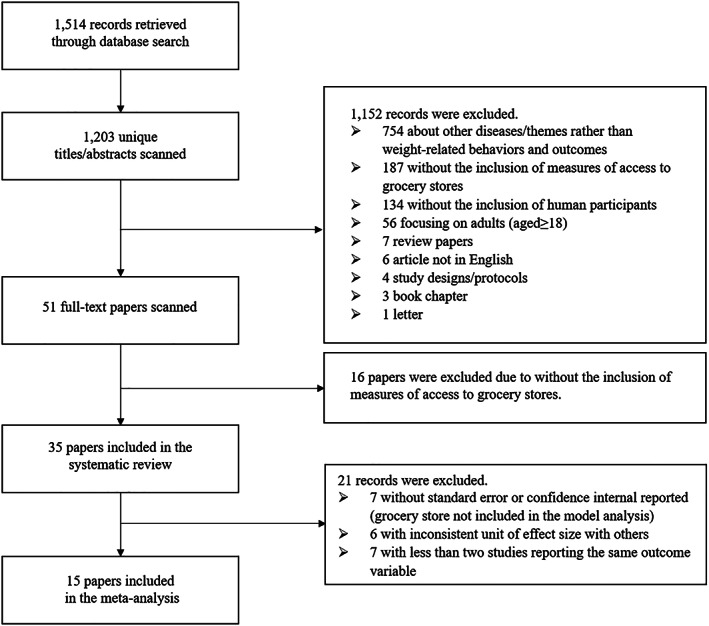
Study exclusion and inclusion flowchart
2.3. Data extraction and preparation
A standardized data extraction form was used to collect methodological and outcome variables from each selected study, including authors, year of publication, study area and country, sample size, age at baseline, follow‐up years, number of repeated measures, sample characteristics, statistical model, attrition rate, measures of the access to grocery stores, measures of weight‐related behaviours, measures of body‐weight status, and key findings on the association between grocery stores and weight‐related behaviours and/or outcomes. Two reviewers independently extracted data from each study included in the review, and discrepancies were resolved by a third reviewer.
2.4. Study quality assessment
We used the National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies to assess the quality of each included study. This assessment tool rates each study on the basis of 14 criteria (Appendix B). For each criterion, a score of 1 was assigned if yes was the response, whereas a score of 0 was assigned otherwise (ie, an answer of no, not applicable, not reported, or cannot determine). A study‐specific global score ranging from 0 to 14 was calculated by summing up scores across all criteria. The study quality assessment helped measure the strength of scientific evidence but was not used to determine the inclusion of studies.
2.5. Meta‐analysis
A meta‐analysis was performed to estimate the pooled effect size of grocery stores on each weight‐related behaviours and outcomes. Weight‐related outcomes included BMI, BMI percentile, and overweight/obesity. Overweight and obesity were defined on the basis of the standards used in the original paper, including age‐sex‐specific Centers for Disease Control and Prevention (CDC) growth charts, World Health Organization (WHO) growth references, and International Obesity Task Force (IOTF) recommendations. Separate meta‐analyses were conducted on different measures of grocery stores, including presence of grocery stores, number of grocery stores, and density of grocery stores. We were not able to conduct a meta‐analysis on weight‐related behaviours because of insufficient number of articles with the same measures of grocery stores.
Effect sizes were reported using mean differences for continuous outcomes (ie, BMI and BMI percentile) or odds ratios for categorical variables (ie, overweight and obesity). Heterogeneity was assessed with the Q test. P value < .1 in the Q test indicates the presence of heterogeneity across studies. The level of heterogeneity measured by I 2 and was interpreted as modest (I 2 ≤ 25%), moderate (25% < I 2 ≤ 50%), substantial (50% < I 2 ≤ 75%), or considerable (I 2 > 75%). A random‐effect model was used to pool the estimates from individual studies because of the varying population and criteria used to define outcomes. All meta‐analyses were performed by the “meta” and “metagen” packages using R version 4.3‐2. 21 All analyses used two‐sided tests, and P < .05 were considered statistically significant except for the evaluation of heterogeneity (P < .1).
3. RESULTS
3.1. Study selection
Figure 1 shows the flow chart of study selection. We identified 1514 articles in the three databases, and 1203 non‐duplicated articles were included in the title and abstract screening. Articles were excluded for irrelevant themes (n = 754), no measures of access to grocery stores (n = 187), not human subjects (n = 134), adult population (n = 56), or other reasons (n = 21), and the remaining 51 articles were included in the full‐text review. In total, 35 studies were included in this systematic review, and 15 of them had sufficient data for meta‐analysis. Studies were excluded from the meta‐analysis because of the following reasons: neither standard error nor confidence interval (CI) was reported (n = 7); the unit of effect size was inconsistent with others (n = 6) and less than two studies reported the same outcome variable (n = 7).
3.2. Study characteristics
Table 1 summarizes the basic characteristics of the 35 included studies. All the studies were published between 2005 and 2018, with 27 cross‐sectional studies and eight prospective cohort studies. The sample size in these studies ranged widely from 78 to 529 367. The majority of the studies were conducted in the United States (n = 26), followed by Canada (n = 4) and the United Kingdom (n = 2), and one study in each of Brazil, Australia, and China. Twelve of these studies were conducted at a national level, and the rest were conducted in state (n = 7), city (n = 11), or county (n = 5) levels.
TABLE 1.
Basic characteristics of 35 studies included in this review
| Author (year)[ref] a | Study Area [scale] b | Sample Size | Sample Age (yrs, range, and/or mean ± SD) c | Sample Characteristics (Follow‐up Status for Longitudinal Studies) | Statistical Model |
|---|---|---|---|---|---|
| Cohort studies | |||||
| Chen (2016) 16 , d | US [N] | 7090 | 11 in 2004 | School children (followed up from 2004 to 2007 with two repeated measures) | Multilevel linear regression |
| Lee (2012) 22 | US [N] | 7710 | 6.2 ± 0.4 in 1999 | School children (follow up from 1999 to 2004 with four repeated measures and an attrition rate of 43.0%) | Multilevel linear regression |
| Leung (2011) 23 | California, US [CT4] | 353 | 6‐7 (7.4 ± 0.4) in 2005 | Girls (followed up from 2005 to 2008 with three repeated measures and an attrition rate of 20.5%) | Generalized linear and logistic regression |
| Miles (2018) 24 | Tallahassee, US [C] | 2770 | 5.6‐12.6 in 2010 | Low‐income elementary school children (followed up from spring to fall in 2010 with two repeated measures and an attrition rate of 17.2%) | Multilevel linear regression |
| Powell (2009) 25 , d | US [N] | 5215 | 12‐17 (15.5 ± 1.7) in 1997 | Adolescents living at home (followed up from 1997 to 2000 with four repeated measures) | Multilevel linear regression |
| Shier (2012) 25 | US [N] | 6260 | in 2004 | Grade 5 students in 2004 and Grade 8 students in 2007 | Multilevel linear regression |
| Sturm (2005) 26 | US [N] | 6918 | 6.2 ± 0.4 in 1999 | Followed up from 1999 to 2002 with three repeated measures and an attrition rate of 42.4% | Multilevel linear regression |
| Zhang (2016) 27 | China [S9] | 348 | 6‐17 (10.9 ± 2.8) in 2009 | Followed up from 2009 to 2011 with two repeated measures | Generalized Estimating Equation |
| Cross‐sectional studies | |||||
| An (2012)49, e | California, US [S] | 13 462 | 8226 aged 5‐11 (8.3 ± 2.0) and 5,236 aged | Measured in 2005 and 2007 | Negative binomial regression |
| 12‐17 (14.5 ± 1.7) in 2005 and 2007 | |||||
| Barrett (2017) 28 | Hampshire, UK [CT] | 1173 | 6 (6.7 ± 0.3) in 2007‐2014 | NA | Multilevel linear regression |
| Carroll‐Scott (2013) 29 | New Haven, US [C] | 1048 | 10.9 ± 0.8 in 2009 | School children at grades 5 and 6 | Multilevel linear regression |
| Correa (2018) 30 | Florianopolis, Brazil [C] | 2195 | 7‐14 in 2012‐2013 | School children | Multivariate logistic regression |
| Davis (2009) 31 | California, US [S] | 529 367 | in 2002‐2005 | Middle and high school students | Multivariate linear regression, and multivariate logistic regression |
| Galvez (2009) 32 | New York, US [C] | 323 | 6‐8 in 2004 | NA | Multivariate logistic regression |
| Grafova (2008) 33 | US [N] | 2482 | 5‐18 (11.8 ± 3.7) in 2002‐2003 | NA | Multivariate logistic regression |
| Harris (2011) 34 | Maine, US [S] | 552 | NA | Grades 9–12 students | Multivariate logistic regression |
| Harrison (2011) 35 | Norfolk, UK [CT] | 1995 | 9‐10 (10.3 ± 0.3) in 2007 | School children at grade 5 | Multilevel linear regression |
| Jago (2006) 36 | Houston, US [C] | 210 | 10‐14 (12.8 ± 1.1) in 2003 | Boy scouts | Multilevel linear regression |
| Jilcott (2011) 37 | Pitt County, US [CT] | 744 | 8‐18 (2.9 ± 2.5) in 2007‐2008 | Paediatric patients | Generalized linear regression |
| Kepper (2016) 38 | Louisiana, US [S] | 78 | 2‐5 (2.9 ± 0.7) | Pre‐school children | Multiple linear regression |
| Laska (2010) 39 | Minneapolis, US [C] | 349 | 11‐18 (15.4 ± 1.7) in 2006‐2007 | NA | Multilevel linear regression |
| Le (2016) 40 | Sasktoon, Canada [C] | 1221 | 10‐14 in 2011 | Elementary school children | Logistic regression |
| Leatherdale (2011) 14 | Ontario, Canada [S] | 2449 | Grades 5‐8 in 2007‐2008 | School children at grades 5–8 | Multilevel logistic regression |
| Liu (2007) 41 | Marion, Indiana, US [CT] | 7334 | 3‐18 in 2000 | Children for routine well‐child care | Cumulative logit models |
| Ohri‐Vachaspati (2015) 42 | New Jersey, US [S] | 560 | 3‐18 in 2009‐2010 | NA | Multivariate logistic regression |
| Pabayo (2012) 43 | Edmonton, Canada [C] | 1760 | 4‐5 in 2005‐2007 | Pre‐school children | Multivariate binomial regression |
| Powell (2007) 62 , e | US [N] | 73 079 | 14.7 ± 1.2 in 1997‐2003 | School children at grades 8–10 (seven annual repeated measures from 1997 to 2003) | Multilevel linear regression |
| Powell (2009) 32 , e | US [N] | 3797 | 6‐17 (12.0 ± 3.2) in 1998, 2000, and 2002 | (measured in 1998, 2000, and 2002) | Multilevel linear regression |
| Powell (2011) 27 , e | US [N] | 1134 | 12‐18 (14.8 ± 1.9) in 1997 and 2002‐2003 | (measured in 1997 and 2002–2003) | Multivariate linear regression |
| Salois (2016) 44 | US [N] | 2192 counties | 2‐4 in 2007‐2009 | Low‐income preschool children | Multivariate linear regression |
| Seliske (2009) 15 | Canada [N] | 7281 | 11‐16 in 2005‐2006 | Grades 6–10 school children | Multilevel logistic regression |
| Shier (2016) 45 | US [N] | 903 | 12‐13 in 2013 | Children in military families | Multivariate linear regression |
| Tang (2014) 46 | New Jersey, US [C4] | 12 954 | 13.5 ± 3.5 in 2008‐2009 | Middle and high school students in low‐income communities | Multilevel linear regression |
| Timperio (2008) 47 | Melbourne and Geelong, Australia [C2] | 801 | 340 aged 5‐6 and 461 aged 10‐12 in 2002‐2003 | School children | Logistic regression |
| Wasserman (2014) 13 | Kansas, US [C2] | 12118 | 4‐12 (8.2 ± 1.8) in 2008‐2009 | Elementary school children | Multilevel linear regression |
Abbreviation: NA, not available.
Studies included in meta‐analyses are in bold.
Study area: [N] – National; [S] – State (e.g., in the US) or equivalent unit (e.g., province in China, Canada); [Sn] – n states or equivalent units; [CT] – County or equivalent unit; [CTn] – n counties or equivalent units; [C] – City; [Cn] – n cities.
Sample age: Age in baseline year for cohort studies or mean age in survey year for cross‐sectional studies.
Including cross‐sectional analysis.
Repeated cross‐sectional study.
[Correction added on 14 January 2021, after first online publication: under ‘Cross‐sectional studies’ column, the reference citat ion of An (2012) has been amended to ‘49’.]
Table S1 reports criterion‐specific and global ratings from the National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies. The 35 studies scored between 7 and 14 with an average of 10.3.
3.3. Measures of access to grocery stores
The access to grocery stores was measured by Geographic Information Systems (GIS) as number of grocery stores (n = 17), density of grocery stores (n = 11), distance to the nearest grocery stores (n = 8), and presence of grocery stores (n = 7) (Table 2). Home neighbourhood was more commonly (n = 23) studied, while fewer studies analysed school neighbourhood (n = 7) or both neighbourhoods (n = 5). Neighbourhood area was commonly measured using individual's home‐ or school‐centred buffer zones with varying radii (from 0.1 to 8.0 km), calculated using straight‐line or, more precisely, road‐network distance. The most commonly used buffer zone was a 0.8‐km road‐network one (n = 6), followed by a 0.4‐km road‐network (n = 4) and a 1.6‐km straight‐line buffer zone (n = 4). The density of grocery stores was usually calculated as the number of grocery stores per 10 000 persons (n = 6) or per 1000 persons (n = 4) within the neighbourhood area. Different from other measures, the most commonly used measure for neighbourhood area when calculating density of grocery stores included ZIP codes area (n = 4), census tract area (n = 3), and county (n = 4).
TABLE 2.
Measures of the access to grocery stores (GSs), weight‐related behaviours and body‐weight status in the included studies
| Author (year)[ref] a | Measures of Access to GS | Other Environmental Factors Adjusted for in the Model | Measures of Weight‐Related Behaviour | Detailed Measures of Weight‐Related Outcomes | Results of Weight‐Related Behaviour | Results of Weight‐Related Outcomes |
|---|---|---|---|---|---|---|
| Longitudinal studies | ||||||
| Chen (2016) 16 | ● Number of GS in home postal zone (in categories of 0, 1, 2, or ≥3) |
● SES features: poverty rate, urbanity, and total business size ● Demographic features: population size, and % of Hispanics, blacks, and foreign‐born population |
NA |
● Measured BMI ● Obesity (BMI ≥ 95th percentile on the 2000 US CDC growth charts) |
NA |
● Exposure to decreased GS was associated with girls' lower BMI after 3 y (β = −0.37, SE = 0.14, p < .05). ● Exposure to increased GS was associated with girls' less obesity status after 3 y (OR = 0.64; 95% CI, 0.42‐0.97). ● The newly opened GS in neighbourhoods without GS was associated with girls' lower BMI 3 y later (β = −0.51, SE = 0.24, p = .04). |
| Lee (2012) 22 |
● Density of GS (supermarkets, large‐scale grocers) per square mile in home census tract ● Density of GS per 1000 persons in home census tract |
● Density of convenience stores, full‐service restaurants, and FF chain restaurants ● Population density, poverty rate, and racial/ethnic composition |
NA | ● Measured BMI percentile (on the basis of the 2000 US CDC growth charts) | NA | ● No association was found between density of GS and change in BMI percentile. |
| Leung (2011) 23 | ● Density of GS per 1000 persons in 0.4/1.6‐km home road‐network buffer (in tertiles and quintiles) | NA | NA |
● Measured BMI z score (on the basis of the 2000 US CDC growth charts) ● Overweight (BMI ≥ 85th percentile on the 2000 US CDC growth charts) |
NA | ● No association was found between density of GS and change in BMI z score or overweight/obesity. |
| Miles (2018) 24 |
● Presence of large GS in 1.6‐km home straight‐line buffer ● Number of small GS in 1.6‐km home straight‐line buffer |
● Presence of park with play equipment in 1.6‐km home straight‐line buffer, presence of green space in 0.4‐km home straight‐line buffer, number of FF restaurants or convenience stores in 0.4‐km home straight‐line buffer, and mean % of roads with high traffic volume in 1.6‐km home straight‐line buffer ● SES features: % of housing units in large multi‐family buildings, low‐income households, college‐educated residents, single‐parent households, black residents, and residents who lived in the same house as 5 y ago. |
NA |
● Measured BMI ● BMI percentile (on the basis of the 2000 US CDC growth charts) ● Overweight (BMI ≥ 85th percentile on the 2000 US CDC growth charts) |
NA |
● Number of GS was negatively associated with BMI change (ref ≥2 GS, β 0GS = 0.06, p = .039; β 1GS = 0.10, p = .004), and was insignificantly associated with BMI percentile change. ● When stratified by weight, this association remained significant only in overweight participants (BMI change: β 0GS = 0.15, p = .021; β 1GS = 0.22, p = .003), not in normal participants. |
| Powell (2009) 48 | ● Density of GS per 10 000 persons in home county |
● Density of FF restaurants, full‐service restaurants, supermarkets, convenience stores, and PA facilities. ● Price of FF. ● Price of food at home (derived from prices of 13 general grocery food consumed at home). |
NA | ● Self‐reported BMI | NA | ● No association was found between density of GS and BMI. |
| Shier (2012) 25 |
● Presence of GS in home census tract. ● Number of GS per 1000 persons in home census tract. |
● Street connectivity index. ● SES features: median household income, and % of non‐Hispanic white |
NA | ● Measured BMI percentile (on the basis of the 2000 US CDC growth charts) | NA | ● No association was found between GS availability and change in BMI percentile. |
| Sturm (2005) 26 | ● Density of GS per 1000 persons in home/school postal zone | NA | NA | ● Measured BMI | NA | ● No association was found between density of GSs and BMI change. |
| Zhang (2016) 27 | ● Straight‐line distance from home to the nearest GS (in quartiles). | ● Distance from home to the nearest free market, Chinese restaurant, and outdoor food stall | NA | ● Measured BMI | NA | ● Boys living in the second quartile of proximity to GSs showed increased BMI (β = 1.66; 95% CI, 0.07‐3.24), while girls showed decreased BMI (β = −1.78; 95% CI, −3.38 to −0.18), compared with those in the first quartile. |
| Cross‐sectional studies | ||||||
| An (2012) 49 |
● Number of GS in 0.16/0.8/1.6/2.4‐km home/school straight‐line buffer. ● Number of GS in joint area by home and school straight‐line buffers. |
● Population density, median household income, and % of non‐Hispanic whites in home and school census tract | ● Daily servings of fruits, vegetables, 100% juice, milk (only for children), soda, high sugar foods, and FF on the day before the interview (parent‐reported for children and self‐reported for adolescents). | ● Parent/self‐reported BMI percentile (on the basis of the 2000 US CDC growth charts; parent‐reported for children and self‐reported by adolescents). | ● No association was found between number of GS and food consumption. | ● The association of GS counts in almost all buffer zones was not associated with BMI percentile, except 0.8‐km straight‐line buffer around adolescent home (β = −0.02, p < .05). |
| Barrett (2017) 28 |
● Number of healthy specialty stores (greengrocers, healthy food stores, farm shops, and butchers) in 0.8‐km home/school straight‐line buffer. ● Number of healthy specialty stores in joint area by home and school straight‐line buffers. |
● Level of neighbourhood deprivation. | ● Standardized diet quality score (indicating dietary quality along with dietary recommendations calculated from consumption frequency of each type of food in FFQ). | NA |
● Better diet score was associated with number of healthy specialty stores (β = 0.03 SD/store; 95% CI, 0.01‐0.04) and greater exposure to healthy outlets relative to all outlets (β = 0.07 SD/10% increase in HSS as a proportion of total outlets; 95% CI, 0.02‐0.12). |
NA |
| Carroll‐Scott (2013) 29 |
● Presence of GS in 0.8‐km home road‐network buffer. ● Road‐network distance from home to the nearest GS. |
● Number of FF restaurants in home census tract. ● Road‐network distance from home to the nearest FF restaurant. ● Perceived access to parks, playgrounds, or gyms (1 = little access, 5 = good access). ● SES features: ethnicity, concentrated affluence, and concentrated disadvantage in home census tract. ● Social environment: social ties scale, safety scale, and property crimes in home census tract. |
● Healthy eating scales (calculated from self‐reported frequency of consumption of vegetables, fruits, whole grains, and nuts/beans per week). ● Unhealthy eating scales (calculated from self‐reported frequency of consumption of FF, foods high in salt and fat, sweets, and sugar‐sweetened beverages per week). ● Days of exercise more than or equal to 30 min per week (self‐reported). ● Hours of screen time on each school day (self‐reported) |
● Measured BMI | ● The distance to the nearest GS was not associated with healthy eating scale, unhealthy eating scale, physical activity, and sedentary behaviour. | ● Higher BMI was significantly associated with living more than a half mile from the nearest GS (β = 1.48, p < .01). |
| Correa (2018) 30 | ● Presence of greengrocers or public markets in 0.4‐km home straight‐line buffer. |
● Presence of restaurants, snack bars/FF outlets, street vendors, supermarkets, minimarkets, butchers, and bakeries. ● Income for home weighting area, which are defined by the government for the purpose of surveys. |
NA | ● Overweight (measured BMI z score > +1SD, equivalent to a BMI ≥ 25 kg/m2 in adults, on the basis of the 2007 WHO growth reference). | NA | ● No association was found between presence of greengrocers/public markets and overweight. |
| Davis (2009) 31 | ● Presence of GS in 0.8‐km school road‐network buffer. |
● Presence of FF restaurants, gas stations, and motels. ● School location type. |
NA |
● Measured BMI ● Overweight (BMI ≥ 85th percentile) and obesity (BMI ≥ 95th percentile on the US CDC growth charts) |
NA | ● No association was found between presence of GS and BMI or overweight or obesity. |
| Galvez (2009) 32 | ● Number of GS in home census tract | NA | NA | ● Measured BMI percentile (on the basis of the 2000 US CDC growth charts; categorized into tertiles) | NA | ● No association was found between presence of GS and BMI percentile. |
| Grafova (2008) 33 | ● Density of GS (supermarkets and other groceries) per 10 000 persons in home county. | NA | NA | ● Overweight (measured BMI ≥ 95th percentile on the 2000 US CDC growth charts). | NA | ● No association was found between density of GS and overweight. |
| Harris (2011) 34 |
● Number of GS in 2‐km school road‐network buffer. ● Road‐network distance from school to the nearest GS. |
NA | NA | ● Underweight (self‐reported BMI < 5th percentile), normal weight (5th ≤ BMI < 85th percentile), overweight (85th ≤ BMI < 95th percentile) and obesity (BMI ≥ 95th percentile on the 2000 US CDC growth charts). | NA | ● No association was found between availability of GS and overweight/obesity. |
| Harrison (2011) 35 |
● Number of healthy food outlets (supermarkets and greengrocers) in 0.8‐km pedestrian‐network buffer around the route from home to school, divided by route length. ● The weighted sum of the pedestrian‐network distance to every healthy food outlet in 6‐km home/school buffer. |
● Access to convenience stores, takeaways, PA facilities, and open land area. ● Road safety variables: density of serious and fatal road traffic accidents, proportion of roads that are major roads and density of verges. ● Street connectivity variables: effective walk‐able area & route length ratio, connected node ratio. ● Land use mix. |
NA | ● Fat Mass Index (= fat mass (kg)/height(m)2; fat mass was measured as foot‐to‐foot bioelectrical impedance). | NA | ● Better access to healthy food outlets around home is associated with lower FMI among girls (β walk or cycle = −0.149, p < .01), but the association is insignificant for GS around school and for all environments among boys. |
| Jago (2006) 36 | ● Number of GS in 1.6‐km home straight‐line buffer. | NA | ● Minutes of sedentary, light, and moderate to vigorous activity per day (measured by accelerometry). | NA | ● No association was found between number of GS and physical activity. | NA |
| Jilcott (2011) 37 |
● Number of GS in 0.4/0.8/1.6/8.0‐km home road‐network buffer ● Straight‐line distance from home to the nearest GS. |
NA | NA |
● Measured BMI percentile (on the basis of the 2000 US CDC growth charts; BMI was extracted from medical records) |
NA | ● No association was found between proximity or number of GS and BMI percentile. |
| Kepper (2016) 38 | ● Number of GS in 1.6/3.2/6.4‐km home straight‐line buffer | NA | ● Servings of fruit and vegetable intake per week (perceived by parents or guardians). | ● Measured BMI z score | ● Fruit intake was associated with increased number of GS within 3.2 km (p = .041) and 6.4 km buffer (p = .028). | ● The ratio of FF outlets to GS was not significantly associated with BMI z score. |
| Laska (2010) 39 |
● Presence of GS in 0.8/1.6/3.0‐km home/school road‐network buffer. ● Road‐network distance from home/school to the nearest GS. |
● Median household income in census tracts. | ● Average daily dietary intake of total energy, fat, fruit and vegetables, vegetables only, and sweetened soft drinks (assessed using 24‐h dietary recalls). |
● Measured BMI z score (on the basis of the 2000 US CDC growth charts). ● Measured body fat percentage. |
● Sugar‐sweetened beverage intake was associated with presence of GS within 1.6‐km buffer (β = 0.31; 95% CI, 0.11‐0.51), and was negatively associated with distance to the nearest GS (β = −0.01; 95% CI, −0.01 to ‐−0.001). | ● No associations were found between presence/density of GS and BMI z score or percentage body fat. |
| Le (2016) 40 |
● Number of GS (smaller GS, large supermarkets) in 0.5/0.8‐km home road‐network buffer. ● Road‐network distance from home to the nearest GS. |
NA | NA | ● Overweight and obesity (measured BMI > +1 SD and > +2 SD of the age‐sex‐specific mean, respectively, on the basis of the 2007 WHO growth reference). | NA | ● No association was found between number/distance of GS and overweight/obesity. |
| Leatherdale (2011) 14 | ● Number of GSs (supermarkets, minimarkets) in 1‐km school straight‐line buffer. | ● Number of gas stations, FF retailers, bakeries/doughnut shops, variety stores and recreation facilities (includes dance studios, fitness/gym facilities, and sport and recreation clubs). | NA | ● Overweight (self‐reported BMI ≥ 95th percentile on the 2000 US CDC growth charts). | NA |
● No association was found between number of GS and overweight in total population. ● Number of GS was positively associated with overweight when stratified by grades, and the increased risk is largest among students in grade 5 relative to students in grades 6‐8. |
| Liu (2007) 41 | ● Road‐network distance from home to the nearest GS. | ● Neighbourhood median family income | NA |
● At risk for overweight (measured BMI ≥ 85th percentile) and overweight (BMI ≥ 95th percentile on the 2000 US CDC growth charts). ● Overweight index (=1 if BMI ≤ 85th percentile; =2 if 85th < BMI ≤ 95th percentile; =3 if 95th < BMI ≤98th percentile; =4 if BMI > 98th percentile). |
NA | ● No association was found between proximity to GS and overweight. |
| Ohri‐Vachaspati (2015) 42 | ● Presence of healthy food outlets (small GS, specialty stores) in 0.4‐km home road‐network buffer. |
● Presence of large parks, PA facility, supermarkets, convenience stores, and limited‐service restaurants. ● Parental perceptions of neighbourhood about PA, traffic safety, crime safety, sidewalk condition, fruit and vegetable shopping, and low‐fat food shopping. ● Neighbourhood income and race. ● Household economic status, language speaking, and car for food shopping. |
NA | ● Overweight (measured BMI ≥ 85th percentile on the 2000 US CDC growth charts). | NA | ● No association was found between presence of GS and overweight/obesity. |
| Pabayo (2012) 43 | ● Number of GS in 1‐km home straight‐line buffer (in categories of 0, 1‐3, and ≥4). | ● Number of FF restaurants and convenience stores. |
● Average servings of soft drink per week. ●Average servings of fruit juice per day (assessed by questionnaire). |
NA | ● Greater number of GS was significantly associated with less regular soft drinks consumption (ref 0GS, RR1–3GS = 0.84; 95% CI, 0.73‐0.96; RR≥ 4GS = 0.64; 95% CI, 0.42‐0.98]), while the association was insignificant for fruit juice consumption. | NA |
| Powell (2007) 50 | ● Density of GS per 10 000 persons in school postal zone. |
● Density of chain supermarkets, non‐chain supermarkets, convenience stores, restaurants, and FF restaurants. ● Price of FF and fruit/vegetable. ● Neighbourhood per capita income. |
NA |
● Self‐reported BMI ● Overweight (BMI ≥ 95th percentile on the 2000 US CDC growth charts). |
NA |
● No association was found between density of GS and BMI. ● Density of GSs had a very small positive and statistically weak association with overweight (β = 0.001, p < .1). |
| Powell (2009) 51 | ● Density of GS per 10 000 persons in home county. |
● Density of FF restaurants, full‐service restaurants, supermarkets, and convenience stores. ● Price of FF and fruit/vegetable. ● Median household income. |
NA | ● Self‐reported BMI. | NA | ● No association was found between density of GS and BMI. |
| Powell (2011) 52 | ● Density of GS (GS, supermarkets) per 10 000 persons per 10 mi2 in home postal zone. |
● Density of FF restaurant, full‐service restaurants, and convenience stores. ● Price of FF and price of food at home. ● Median household income. |
● Number of days food items were consumed in the last week, including fruit and fruit juice, vegetables, meat, nonmeat protein, dairy, grains, and sweets (collected by audio computer‐assisted self‐interview). | NA |
● Density of GS was not significantly associated with food consumption categories in total population. ● Density of GS was significantly associated with vegetable consumption in the low family income group (β = 0.31, p < .05) and meat consumption in high family income group (β = 0.02, p < .01). |
NA |
| Salois (2012) 44 | ● Density of GS (GS, supermarkets) per person per square mile in home county. |
● Density of FF restaurant, full‐service restaurant, supercenters and club stores, convenience store, specialty store, farmers’ market, SNAP‐authorized store, and WIC‐authorized store. ● PA environment: recreational/fitness facilities density, natural amenity index, nonattainment air quality county, criminal activity rate. ● Neighbourhood economic status. ● Household composition: ethnicity, education, percent foreign‐born, average household size, percent female headed population density. |
NA | ● Prevalence of low‐income preschool obesity (measured BMI ≥ 95th percentile on the 2000 US CDC growth charts). | NA | ● Density of GS was associated with childhood obesity in metropolitan counties (β = 3.33, p < .01), but the association was not found in all counties and nonmetropolitan counties. |
| Seliske (2009) 15 | ● Density of GS per 10 000 persons in 5‐km school straight‐line buffer (in categories of none, low, medium, and high exposures). |
● Density of full‐service restaurants, FF restaurants, sub/sandwich retailers, doughnut/coffee shops, and convenience stores. ● Total food retailer index (calculated as total number of food retailers). |
NA |
● Self‐reported BMI. ● Overweight (on the basis of IOTF cut‐offs, equivalent to BMI ≥ 25 kg/m2 in adults). |
NA | ● Density of GS in medium exposure categories were negatively associated with overweight (ref none, OR = 0.70; 95% CI, 0.54‐0.92). |
| Shier (2016) 45 |
● Number of GS in 3.2‐km home straight‐line buffer. |
● Residential region. |
● Frequency of fruit, vegetable, soda, sweet snack, salty snack, and ready‐made dinner consumption per week. |
● Measured BMI z score (on the basis of the 2000 US CDC growth charts). ● Overweight (BMI ≥ 85th percentile on the 2000 US CDC growth charts). |
● No associations were found between number of GS and food consumption frequencies. | ● No associations were found between number of GS and BMI z score or overweight/obesity. |
| Tang (2014) 46 | ● Number of GS in 0.4‐km school road‐network buffer. | ● Number of supermarkets, convenience stores, and limited‐service restaurants. | NA |
● Measured BMI z score (on the basis of the 2000 US CDC growth charts). ● Overweight (BMI ≥ 85th percentile on the 2000 US CDC growth charts). |
NA |
● Number of GS and an additional GS was associated with significantly lower BMI z scores (β = −0.12; 95% CI, −0.24 to −0.01; β = −0.1; 95% CI, −0.17 to 0.003). ● No association was found between number of GS and overweight/obesity. |
| Timperio (2008) 47 |
● Number of GS in 0.8‐km home road‐network buffer. ● Road‐network distance from home to the nearest GS. |
NA | ● Frequency of fruit and vegetable consumption (collected by parents' answered questionnaires). | NA | ● No associations were found between access to GSs and fruit and vegetable intake. | NA |
| Wasserman (2014) 13 | ● Number of GS in 0.8‐km school straight‐line buffer. | ● Number of convenience stores, FF restaurants, fitness facilities, and parks. | NA |
● BMI percentile (on the basis of the 2000 US CDC growth charts). ● At risk of overweight (BMI ≥ 85th percentile) and overweight (BMI ≥ 95th percentile on the 2000 US CDC growth charts). |
NA |
● Number of GS was associated with higher BMI percentile (β = 0.66, p < .01). ● Number of GS was associated with higher odds of overweight (OR = 1.06; 95% CI, 0.99‐1.12) and at risk of overweight (OR = 1.06; 95% CI, 1.00, 1.12). |
Note. Straight‐line buffer—a regular (e.g., circular) zone with a certain radius around a given address/location or a street to represent a catchment or influential area of that address/location or street; Road‐network buffer—an irregular zone around a given address/location where it covers the same distance (or takes the same time) to travel from any point on the boundary of the zone to that address/location along the shortest road network path. The buffer zone area for adjusted environmental variables was the same as access to grocery stores, unless indicated otherwise.
Abbreviations: BMI, body mass index; CDC, Center for Disease Control and Prevention; FF, fast food; FFQ, food frequency questionnaire; GIS, Geographic Information Systems; GS, grocery store; IOTF, International Obesity Task Force; NEMS‐S, Nutrition Environment Measures Survey for Stores; NA, not available; PA, physical activity; SES, socioeconomic status; WHO, World Health Organization.
Studies included in meta‐analyses are in bold.
3.4. Association between access to grocery stores and weight‐related behaviours
Ten cross‐sectional studies examined the association between the access to grocery stores and weight‐related behaviours, including dietary behaviours (n = 9), physical activity (n = 2), and sedentary behaviour (n = 1), where mixed findings were reported (Table 2). In terms of dietary behaviours, five studies reported null associations between access to grocery stores and food consumption frequency of fruit (12 out of 14 associations), vegetables (18 out of 18 associations), and beverages (9 out of 12 associations), one study reported a negative association on soft drink consumption, and three studies reported positive associations, including one on overall dietary quality, one on fruit intake, and one on sugar sweated beverage intake. No significant association was found between the access to grocery stores and physical activity or sedentary behaviours.
3.5. Association between access to grocery stores and weight‐related outcomes
Twenty‐one studies examined the association between the access to grocery stores and weight‐related outcomes, including overweight/obesity (n = 17), BMI (n = 10), BMI z score (n = 5), BMI percentile (n = 7), body fat percentage (n = 1), and fat mass index (FMI) (n = 1).
In eight cohort studies, five studies reported insignificant associations between access to grocery stores and change in weight‐related outcomes. Two studies conducted stratified analysis on gender and reported significant results. One found the exposure to a decrement in grocery stores was associated with girls' lower BMI 3 years later, while the analysis of boys was insignificant 16 ; the other reported that living farther from a grocery store was associated with higher BMI in boys but lower BMI in girls. 27 One study reported a negative association between number of grocery stores and BMI change, and when stratified by weight, this significant association only persisted in overweight participants, not in normal weight participants.
In cross‐sectional analyses, the majority of associations (12 out of 17 in BMI, 28 out of 30 in BMI percentile, five out of seven in BMI z score, and 24 out of 29 in overweight/obesity) reported between access to grocery stores and weight‐related outcomes were insignificant. Significant findings with mixed results were also reported. Two studies reported a negative association between number or density of grocery stores and weight‐related outcomes, while one reported a positive association. Also, one study reported a negative association between distance to the nearest grocery store and BMI. Despite reporting null associations in the overall population, some studies reported significant findings when conducting stratified analysis by gender, grades, or location. One study reported better access to grocery stores were associated with lower FMI in girls while insignificant association was found in boys; one study reported that a positive association between number of grocery stores and overweight was only observed when stratified by grades, and the increased risk of overweight was largest among students in grade 5, relative to students in grades 6 to 8 14 ; one study found that density of grocery stores was associated with obesity in metropolitan counties, while the association was not found in non‐metropolitan counties.
Table 3 summarizes the modelling results from the meta‐analysis. Four meta‐analyses were conducted to estimate the pooled effect size between measures of grocery stores and weight‐related outcomes. We observed insignificant pooled effects in three meta‐analyses, with one between density of grocery stores and BMI (β = 0.006; 95%CI, −0.022 to 0.033), one between number of grocery stores and BMI percentile (β = 0.001; 95%CI, −0.041 to 0.043), and one between number of grocery stores and overweight/obesity (OR = 1.01; 95%CI, 0.99‐1.03). The analysis between presence of grocery stores and overweight reached borderline significance (OR = 0.98; 95%CI, 0.96‐1.00) in seven eligible studies. Stratified meta‐analysis was conducted on these seven studies by study design (Figure 2), where we found this significant association was only found in cross‐sectional studies (OR = 0.98; 95%CI, 0.95‐1.00) not cohort studies (OR = 1.23; 95%CI, 0.89‐1.70).
TABLE 3.
Meta‐analysis of associations between the access to grocery stores (GSs) and body‐weight status
| Author (year)[ref] | Study Design | Study Area | Sample Size | GS Measures | Weight‐Related Outcomes | Estimated Effect | Pooled Effect Size [95% CI] | I 2 Index |
|---|---|---|---|---|---|---|---|---|
| Overweight/obesity | ||||||||
| Chen (2016) 16 | CO | US | 7090 | Presence of GSs in home postal zone | Obesity(i) | OR(95%CI) | OR(95%CI) | 0 |
| 1.19(0.85‐1.66) | 0.98(0.96‐1.00) | |||||||
| Leung (2011) 23 | CO | US | 353 | Presence of GSs per 1000 persons in 0.4‐km home road‐network buffer | Overweight(i) | OR(95%CI) | ||
| 1.90(0.57, 6.37) | ||||||||
| Correa (2018) 30 | CS | Brazil | 2195 | Presence of GSs in 0.4‐km home straight‐line buffer | Overweight (ii) | OR(95%CI) | ||
| 0.92(0.71‐1.19) | ||||||||
| Davis (2009) 31 | CS | US | 529 367 | Presence of GSs in 0.8‐km school road‐network buffer | Overweight(i) | OR(95%CI) | ||
| 0.98(0.95‐1.01) | ||||||||
| Ohri‐Vachaspati (2015) 42 | CS | US | 560 | Presence of healthy food outlets (small grocery stores and specialty stores) in 0.4‐km home road‐network buffer | Overweight(i) | OR(95%CI) | ||
| 1.03(0.58‐1.83) | ||||||||
| Seliske (2009) 15 | CS | Canada | 7281 | Presence of GSs per 10 000 persons in 5‐km school straight‐line buffer | Overweight (iii) | OR(95%CI) | ||
| 0.90(0.70‐1.15) | ||||||||
| Tang (2014) 46 | CS | US | 12 954 | Presence of GSs in 0.4‐km school road‐network buffer | Overweight(i) | OR(95%CI) | ||
| 0.98(0.94‐1.02) | ||||||||
| Overweight/obesity | ||||||||
| Leatherdale (2011) 14 | CS | Canada | 2449 | Number of GSs in 1‐km school straight‐line buffer | Obesity(i) | OR(95%CI) | OR(95%CI) | 33% |
| 1.10(0.86‐1.42) | 1.01(0.99, 1.03) | |||||||
| Shier (2016) 45 | CS | US | 903 | Number of GSs in 3.2‐km home straight‐line buffer | Overweight(i) | OR(95%CI) | ||
| 1.00(0.99‐1.01) | ||||||||
| Tang (2014) 46 | CS | US | 12 954 | Number of GSs in 0.4‐km school road‐network buffer | Overweight(i) | OR(95%CI) | ||
| 1.00(0.97‐1.02) | ||||||||
| Wasserman (2014) 13 | CS | US | 12 118 | Number of GSs in 0.8‐km school straight‐line buffer | Overweight(i) | OR(95%CI) | ||
| 1.06(1.00‐1.12) | ||||||||
| Obesity | ||||||||
| Grafova (2008) 33 | CS | US | 2482 | Density of GSs per 10 000 persons in home county | Obesity(i) | OR(95%CI) | OR(95%CI) | 68% |
| 1.10 (0.99‐1.3) | 1.03(0.95‐1.13) | |||||||
| Powell (2007) 50 | CS | US | 73 079 | Density of GSs per 10 000 persons in school postal zone | Obesity(i) | OR(95%CI) | ||
| 1.00(1.00‐1.00) | ||||||||
| BMI percentile | ||||||||
| An (2012) 49 | CS | US | 13 462 | Number of GSs in 0.8‐km school straight‐line buffer | Parent‐reported/self‐reported BMI percentile |
β (SE) For child 0.0097(0.0111) For adolescent −0.0164(0.0070) |
β(95%CI) 0.0013(−0.0406 to 0.0432) |
83% |
| Wasserman (2014) 13 | CS | US | 12,118 | Number of GSs in 0.8‐km school straight‐line buffer | Measured BMI percentile | β (SE) | ||
| 0.66(0.24) | ||||||||
| BMI | ||||||||
| Powell (2007) 50 | CS | US | 73 079 | Density of GSs per 10 000 persons in school postal zone | Self‐reported BMI | β (SE) | β(95%CI) | 10% |
| 0.012(0.009) | 0.006(−0.022 to 0.033) | |||||||
| Powell (2009) 48 | CS | US | 5215 | Density of GSs per 10 000 persons in home county | Self‐reported BMI | β (SE) | ||
| −0.007(0.047) | ||||||||
| Powell (2009) 51 | CS | US | 3797 | Density of GSs per 10 000 persons in home county | Self‐reported BMI | β (SE) | ||
| −0.068(0.055) | ||||||||
Note. Overweight is defined as (i)BMI percentile higher than or equal to the 85th on the 2000 US CDC growth charts; (ii)BMI z score > 1 or age‐sex‐specific BMI > +1SD, equivalent to a BMI ≥25 kg/m2 in adults, on the basis of the 2007 WHO growth reference; (iii)BMI > age‐sex‐specific cut‐off points, equivalent to a BMI greater than or equal to 25 kg/m2 in adults, on the basis of the 2000 IOTF recommendations. Obesity is defined as (i)BMI percentile higher than or equal to the 95th on the 2000 US CDC growth charts; (ii)BMI z score > 1 or age‐sex‐specific BMI > +1SD, on the basis of the 2007 WHO growth reference; (iii)BMI > age‐sex‐specific cut‐off points, equivalent to a BMI ≥ 30 kg/m2 in adults, on the basis of the 2000 IOTF recommendations.
Abbreviations: BMI, body mass index; CDC, Centers for Disease Control and Prevention; CI, confidence interval; GS, grocery store; SD, standard deviation; WHO, World Health Organization.
FIGURE 2.
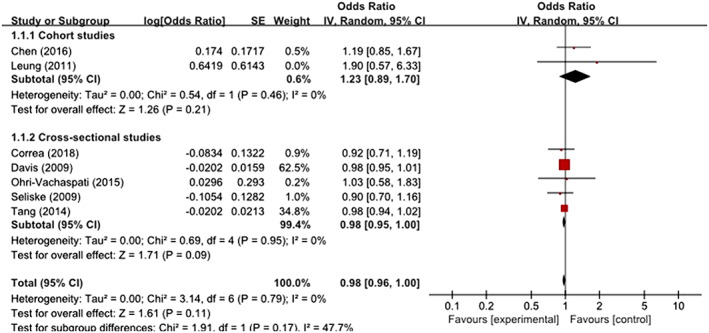
Meta‐analyses of the associations between presence of grocery stores in neighbourhood and child overweight/obesity [Colour figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
We systematically reviewed and identified 35 studies that assessed the association between the access to grocery stores and weight‐related behaviours and outcomes in children and adolescents. We included 27 cross‐sectional studies and eight cohort studies, where most of the studies were conducted in the United States. The majority of studies measured the access to grocery stores using GIS‐based measures, and overweight/obesity was the most commonly studied outcome variable. Mixed results were observed for this association for studies both conducted in and outside the United States. While only a few studies reported protective effects for children's weight‐related behaviour/outcomes with increased access to grocery stores, most of the studies reported null associations and some studies observed obesogenic effects with increased access to grocery stores. The meta‐analysis found insignificant associations between access to grocery stores and weight‐related outcomes in eligible studies, though the association between presence of grocery store and decreased odds of overweight/obesity reached borderline significance.
In this review, we identified 10 studies that analysed the association between access to grocery stores and weight‐related behaviours, however, there are large variations in outcome measures among these studies. The consumption of food categories including fruits, vegetables, and beverages was most commonly analysed, but it is difficult to make conclusions on the position of association because of inconsistency of existing results and limited number of studies available. Physical activity was consistently reported to have null associations with access to grocery stores in two included studies. 29 , 36 Other different aspects of dietary behaviours analysed included overall dietary quality score and eating habits.
The findings of the association between access to grocery stores and weight‐related outcomes were consistent with the systematic review by Cobb et al (2015), which reported no indication of association between grocery stores availability and childhood obesity. 17 In this review, we also found that the majority of associations were insignificant both in cross‐sectional and longitudinal analysis, suggesting that access to grocery stores in the home or school neighbourhood may have little influence on childhood obesity.
It is also worth noting that despite the non‐significant associations observed in the overall population, many studies reported significant findings in stratified analysis, where opposite associations were observed when stratified by gender, weight, and economic status. These results may suggest that the true association between access to childhood obesity was masked or diluted when analysing the overall population. Unfortunately, we were not able to conduct stratification in meta‐analysis because of insufficient data available, though some evidence may support these opposite associations between different subgroups. For instance, gender differences in age of puberty, physical activity, and eating habits may, to some extent, help to explain the opposite associations reported among boys and girls 16 , 53 ; weight and economic status may influence an individual's eating and shopping habits, thus change the direction of association. 24 , 52 Future studies would be needed to specifically examine whether these factors influence the true relationship between access to grocery store and childhood obesity.
Several possible reasons may also help to explain this null association. First, different definitions and classification systems for grocery store in different countries may influence the association. In the United States and Canada, where most studies were conducted, grocery store was more consistently defined using the 6‐digit NAICS code or Standard Industry Classification (SIC) codes, 54 plus the restriction on store size or annual sales. Though some studies in the United States or Canada (six out of 30 studies) has categorized grocery stores together with supermarkets, this definition system allows a rather clear separation among grocery stores and other similar types of food stores as compared with the definition in other countries. For instance, grocery store was categorized as health specialty stores together with healthy food stores, farm shops, and butchers in both of the two studies conducted in the United Kingdom, where both studies reported a protective effect on childhood obesity. Also, the study conducted in Brazil included both greengrocer and public market together, and the study conducted in China categorized indoor stores selling all types of food as one category, regardless of store size, which may possibly include supermarkets, grocery store, and convenience store. Second, the method of measuring the access to grocery stores varied, in terms of choosing the buffer radius and measuring the radius/distance (straight‐line or road‐network), which may influence the results. More importantly, according to the commonly used conceptual framework, how children could actually interact with their surrounding grocery stores may be determined by not only the access to grocery stores (ie, availability and accessibility), but also the affordability, acceptability, and accommodation. 55 In this review, four studies considered the affordability by taking into account food price 22 , 48 , 51 , 52 and 14 studies has considered the economic status of the family or the neighbourhood, while only one study has measured the acceptability (ie, people's attitudes) towards food shopping, and no study measured the features about accommodation (ie, the adaptation of stores to resident's needs). We should be aware that measuring different dimensions of the access to grocery stores may yield different results. For instance, Caitlin et al found that studies examining acceptability and accommodation generally showed a significant relationship between food quality or opening hours and fruit and vegetable consumption. 19 Third, most studies only considered walkable distance for children and their parents, and few studies have taken into account the role of transportation. Children might reach grocery stores beyond their buffer zones in other ways, eg, taking public transportation and being taken there by parents. 56 , 57
This review and especially the meta‐analysis were influenced by study quality and data availability of the included studies, while we found insufficient studies for high‐quality meta‐analysis. One reason for this insufficient data availability was the inconsistency in measures of exposure variables, where it is infeasible to pool together distinct measures, such as number of grocery stores and distance to the nearest grocery stores. Also, we observed that 10 included studies categorized grocery stores and supermarkets together, and one study categorized grocery stores together with fast‐food outlet. We have tried to conduct multiple meta‐analyses with similar measures, though some of these studies may truly have different underlying associations between the access to grocery store and childhood obesity under distinct study settings. The other possible limitations included nondetectable effect size, confounding issue, and insufficient food environment analysed. 58 , 59 , 60
To advance research on the association between the access to grocery stores and child weight‐related behaviours and outcomes, future studies are warranted to improve several aspects. First, objective measurement should be conducted in a more precise and consistent way, eg, using GIS‐based road‐network distance and a set of radii a priori for better comparability. More advanced spatial approaches, such as remote sensing and citizen science, are alternative methods to obtain such environmental measures where GIS‐based road‐network are not available. 61 , 62 , 63 Second, some novel objective measures and subjective measures should be added to measure all dimensions of the access to grocery stores, such as affordability, acceptability, and accommodation. 64 Third, more pathway‐based analyses need to be conducted to elucidate underlying mechanisms from grocery stores in individual's home and/or school neighbourhoods to child weight‐related behaviours and outcomes. Fourth, in addition to healthy food, most grocery stores also sell unhealthy food choices, eg, sweetened beverages and preserved food, 65 and the effect of grocery store on childhood obesity may depend on actual food catalogs sold and purchased in each store. It is also necessary to take into consideration a list of children‐specific factors, including children's pocket money, whether meal and/or snacks are provided at school, and mode of transportation between home and school. 66
5. CONCLUSIONS
This systematic review of both cross‐sectional and longitudinal studies revealed a rather weak relationship between grocery stores and weight‐related behaviours/outcomes among children and adolescents.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
Supporting information
Data S1. Appendix A. Additional tables
Table S1. Study quality assessment (see 14 questions in Appendix C)
Appendix B. Search strategy
Appendix C. National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies
ACKNOWLEDGEMENTS
We thank the International Institute of Spatial Lifecourse Epidemiology (ISLE), Hunan Provincial Natural Science Foundation of China (2018J J2553), the National Natural Science Foundation of China (81872641), and the National Science & Technology Basic Resource Investigation Program of China (2017FY101100) for research support. [Correction added on 14 January 2021, after first online publication: Acknowledgements have been revised.]
Li Y, Luo M, Wu X, Xiao Q, Luo J, Jia P. Grocery store access and childhood obesity: A systematic review and meta‐analysis. Obesity Reviews. 2021;22(S1):e12945. 10.1111/obr.12945
Yamei Li and Miyang Luo contributed equally to this work.
[Correction added on 14 January 2021, after first online publication: Peng Jia's affiliation and correspondence details have been updated.]
[Correction added on 8 February 2021, after first online publication: Funding Information has been revised.]
Contributor Information
Jiayou Luo, Email: jiayouluo@csu.edu.cn.
Peng Jia, Email: p.jia@utwente.nl.
REFERENCES
- 1. Commission on Ending Childhood Obesity WHO . Report of the Commission on Ending Childhood Obesity. 2016.
- 2. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474‐488. [DOI] [PubMed] [Google Scholar]
- 3. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public‐health crisis, common sense cure. The Lancet. 2002;360(9331):473‐482. [DOI] [PubMed] [Google Scholar]
- 4. Davison KK, Birch LL. Predictors of fat stereotypes among 9‐year‐old girls and their parents. Obes Res. 2004;12(1):86‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hill AJ, Silver EK. Fat, friendless and unhealthy: 9‐year old children's perception of body shape stereotypes. Int J Obes Relat Metab Disord: J Int Assoc Study Obes. 1995;19:423‐430. [PubMed] [Google Scholar]
- 6. Caird J, Kavanagh J, O'Mara‐Eves A, et al. Does being overweight impede academic attainment? A systematic review. Health Educ J. 2014;73(5):497‐521. [Google Scholar]
- 7. Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta‐analysis. Obes Rev. 2017;18(7):742‐754. [DOI] [PubMed] [Google Scholar]
- 8. Jia P, Cheng X, Xue H, Wang Y. Applications of geographic information systems (GIS) data and methods in obesity‐related research. Obes Rev. 2017;18:400‐411. [DOI] [PubMed] [Google Scholar]
- 9. Xin J, Zhao L, Wu T, et al. Association between access to convenience stores and childhood obesity: a systematic review. Obes Rev. 2021;22(Suppl 1):e12908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jia P, Xue H, Cheng X, Wang Y, Wang Y. Association of neighborhood built environments with childhood obesity: evidence from a 9‐year longitudinal, nationally representative survey in the US. Environ Int. 2019;128:158‐164. [DOI] [PubMed] [Google Scholar]
- 11. Horder J, Browning M, Simplicio M, Cowen PJ, Harmer CJ. Effects of 7 days of treatment with the cannabinoid type 1 receptor antagonist, rimonabant, on emotional processing. J Psychopha (oxford, england). 2012;26:125‐132. [DOI] [PubMed] [Google Scholar]
- 12. Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333‐339. [DOI] [PubMed] [Google Scholar]
- 13. Wasserman JA, Suminski R, Xi J, Mayfield C, Glaros A, Magie R. A multi‐level analysis showing associations between school neighborhood and child body mass index. Int J Obes (2005). 2014;38:912‐918. [DOI] [PubMed] [Google Scholar]
- 14. Leatherdale ST, Pouliou T, Church D, Hobin E. The association between overweight and opportunity structures in the built environment: a multi‐level analysis among elementary school youth in the PLAY‐ON study. Int J Public Health. 2011;56(3):237‐246. [DOI] [PubMed] [Google Scholar]
- 15. Seliske LM, Pickett W, Boyce WF, Janssen I. Association between the food retail environment surrounding schools and overweight in Canadian youth. Public Health Nutr. 2009;12(9):1384‐1391. [DOI] [PubMed] [Google Scholar]
- 16. Chen HJ, Wang Y. Changes in the neighborhood food store environment and children's body mass index at peripuberty in the United States. J Adolesc Health. 2016;58(1):111‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cobb LK, Appel LJ, Franco M, Jones‐Smith JC, Nur A, Anderson CAM. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity. 2015;23(7):1331‐1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang Y, Jia P, Cheng X, Xue H. Improvement in food environments may help prevent childhood obesity: evidence from a 9‐year cohort study. Pediatr Obes. 2019;e12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172‐1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schwarzer G. meta: An R Package for Meta‐Analysis 2007.
- 22. Lee H. The role of local food availability in explaining obesity risk among young school‐aged children. Soc Sci Med. 2012;74:1193‐1203. [DOI] [PubMed] [Google Scholar]
- 23. Leung CW, Laraia BA, Kelly M, et al. The influence of neighborhood food stores on change in young girls' body mass index. Am J Prev Med. 2011;41(1):43‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miles R, Wang Y, Johnson SB. Neighborhood built and social environments and change in weight status over the summer in low‐income elementary school children. Int J Environ Res Public Health. 2018;15(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shier V, An R, Sturm R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public Health. 2012;126(9):723‐730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059‐1068. [DOI] [PubMed] [Google Scholar]
- 27. Zhang J, Xue H, Cheng X, et al. Influence of proximities to food establishments on body mass index among children in China. Asia Pac J Clin Nutr. 2016;25:134‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Barrett M, Crozier S, Lewis D, et al. Greater access to healthy food outlets in the home and school environment is associated with better dietary quality in young children. Public Health Nutr. 2017;20(18):3316‐3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carroll‐Scott A, Gilstad‐Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Correa EN, Rossi CE, das Neves J, Silva DAS, de Vasconcelos FDG. Utilization and environmental availability of food outlets and overweight/obesity among schoolchildren in a city in the south of Brazil. J Public Health 2018; 40: 106‐113, 1. [DOI] [PubMed] [Google Scholar]
- 31. Davis B, Carpenter C. Proximity of fast‐food restaurants to schools and adolescent obesity. Am J Public Health. 2009;99(3):505‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Galvez MP, Hong L, Choi E, Liao L, Godbold J, Brenner B. Childhood obesity and neighborhood food‐store availability in an inner‐city community. Acad Pediatr. 2009;9(5):339‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Grafova IB. Overweight children: assessing the contribution of the built environment. Prev Med. 2008;47(3):304‐308. [DOI] [PubMed] [Google Scholar]
- 34. Harris DE, Blum JW, Bampton M, et al. Location of food stores near schools does not predict the weight status of Maine high school students. J Nutr Educ Behav. 2011;43(4):274‐278. [DOI] [PubMed] [Google Scholar]
- 35. Harrison F, Jones AP, van Sluijs EM, Cassidy A, Bentham G, Griffin SJ. Environmental correlates of adiposity in 9‐10 year old children: considering home and school neighbourhoods and routes to school. Soc Sci Med. 2011;72:1411‐1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jago R, Baranowski T, Baranowski JC. Observed, GIS, and self‐reported environmental features and adolescent physical activity. Am J Health Promot. 2006;20(6):422‐428. [DOI] [PubMed] [Google Scholar]
- 37. Jilcott SB, Wade S, McGuirt JT, Wu Q, Lazorick S, Moore JB. The association between the food environment and weight status among eastern North Carolina youth. Public Health Nutr. 2011;14(9):1610‐1617. [DOI] [PubMed] [Google Scholar]
- 38. Kepper M, Tseng TS, Volaufova J, Scribner R, Nuss H, Sothern M. Pre‐school obesity is inversely associated with vegetable intake, grocery stores and outdoor play. Pediatr Obes. 2016;11(5):E6‐E8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Laska MN, Hearst MO, Forsyth A, Pasch KE, Lytle L. Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr. 2010;13(11):1757‐1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Le H, Engler‐Stringer R, Muhajarine N. Walkable home neighbourhood food environment and children's overweight and obesity: Proximity, density or price? Can J Public Health‐Revue Canadienne De Sante Publique. 2016;107(S1):ES42‐ES47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: differences by population density. Am J Health Promot. 2007;21(4_suppl):317‐325. [DOI] [PubMed] [Google Scholar]
- 42. Ohri‐Vachaspati P, DeLia D, DeWeese RS, Crespo NC, Todd M, Yedidia MJ. The relative contribution of layers of the Social Ecological Model to childhood obesity. Public Health Nutr. 2015;18(11):2055‐2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pabayo R, Spence JC, Cutumisu N, Casey L, Storey K. Sociodemographic, behavioural and environmental correlates of sweetened beverage consumption among pre‐school children. Public Health Nutr. 2012;15(8):1338‐1346. [DOI] [PubMed] [Google Scholar]
- 44. Salois MJ. The built environment and obesity among low‐income preschool children. Health Place. 2012;18(3):520‐527. [DOI] [PubMed] [Google Scholar]
- 45. Shier V, Nicosia N, Datar A. Neighborhood and home food environment and children's diet and obesity: Evidence from military personnel's installation assignment. Soc Sci Med. 2016;158:122‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tang XY, Ohri‐Vachaspati P, Abbott JK, et al. Associations between food environment around schools and professionally measured weight status for middle and high school students. Child Obes. 2014;10(6):511‐517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Timperio A, Ball K, Roberts R, Campbell K, Andrianopoulos N, Crawford D. Children's fruit and vegetable intake: associations with the neighbourhood food environment. Prev Med. 2008;46(4):331‐335. [DOI] [PubMed] [Google Scholar]
- 48. Powell LM. Fast food costs and adolescent body mass index: evidence from panel data. J Health Econ. 2009;28(5):963‐970. [DOI] [PubMed] [Google Scholar]
- 49. An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med. 2012;42(2):129‐135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Powell LM, Auld MC, Chaloupka FJ, O'Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. Am J Prev Med. 2007;33(4):S301‐S307. [DOI] [PubMed] [Google Scholar]
- 51. Powell LM, Bao Y. Food prices, access to food outlets and child weight. Econ Hum Biol. 2009;7(1):64‐72. [DOI] [PubMed] [Google Scholar]
- 52. Powell LM, Han E. The costs of food at home and away from home and consumption patterns among U.S. adolescents. J Adolesc Health: Official Publication of the Society for Adolescent Medicine. 2011;48:20‐26. [DOI] [PubMed] [Google Scholar]
- 53. Larson NI, Wall MM, Story MT, Neumark‐Sztainer DR. Home/family, peer, school, and neighborhood correlates of obesity in adolescents. Obesity. 2013;21(9):1858‐1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jia P, Xue H, Cheng X, Wang Y. Effects of school neighborhood food environments on childhood obesity at multiple scales: a longitudinal kindergarten cohort study in the USA. BMC Med. 2019;17(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127‐140. [DOI] [PubMed] [Google Scholar]
- 56. White M. Food access and obesity. Obes Rev. 2007;8(Suppl 1):99‐107. [DOI] [PubMed] [Google Scholar]
- 57. Ver Ploeg M, Breneman V, Farrigan T, et al. Access to Affordable and Nutritious Food—Measuring and Understanding Food Deserts and Their Consequences: Report to Congress 2009.
- 58. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011‐2012. JAMA. 2014;311(8):806‐814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ogden C, Carroll M. Prevalence of overweight, obesity, and extreme obesity among adults: United States, trends 1960‐1962 through 2007‐2008 2010.
- 60. Bleich S, Cutler D, Murray C, Adams A. Why is the developed world obese? Annu Rev Public Health. 2008;29(1):273‐295. [DOI] [PubMed] [Google Scholar]
- 61. Jia P, Stein A, James P, et al. Earth observation: investigating noncommunicable diseases from space. Annu Rev Public Health. 2019;40(1):85‐104. [DOI] [PubMed] [Google Scholar]
- 62. Jia P. Spatial lifecourse epidemiology. Lancet Plan health. 2019;3(2):e57‐e59. [DOI] [PubMed] [Google Scholar]
- 63. Jia P, Stein A. Using remote sensing technology to measure environmental determinants of non‐communicable diseases. Int J Epidemiol. 2017;46(4):1343‐1344. [DOI] [PubMed] [Google Scholar]
- 64. Jia P, Xue H, Yin L, Stein A, Wang M, Wang Y. Spatial technologies in obesity research: current applications and future promise. Trends Endocrinol Metab. 2019;30(3):211‐223. [DOI] [PubMed] [Google Scholar]
- 65. Powell LM, Chaloupka FJ. Food prices and obesity: evidence and policy implications for taxes and subsidies. Milbank Q. 2009;87(1):229‐257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Jia P, Li M, Xue H, Lu L, Xu F, Wang Y. School environment and policies, child eating behaviour and overweight/obesity in urban China: the childhood obesity study in China megacities. Int J Obes (Lond). 2017;41(8):1310. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Appendix A. Additional tables
Table S1. Study quality assessment (see 14 questions in Appendix C)
Appendix B. Search strategy
Appendix C. National Institutes of Health's Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies


