Summary
Guidelines and evidence suggest primary care clinicians should give opportunistic interventions to motivate weight loss, but these rarely occur in practice. We sought to examine why by systematically reviewing qualitative research examining general practitioners' (‘GPs’) and nurses' views of discussing weight with patients. We systematically searched English language publications (1945‐2018) to identify qualitative interview and focus group studies. Thematic methods were used to synthesise the findings from these papers. We synthesised the studies by identifying second‐order themes (explanations offered by the original researchers) and third‐order constructs (new explanations which went beyond those in the original publications). Quality assessment using the Joanna Briggs checklist was undertaken. We identified 29 studies (>601 GPs, nurses and GP trainees) reporting views on discussing weight with patients. Key second‐order themes were lack of confidence in treatments and patients' ability to make changes, stigma, interactional difficulty of discussing the topic and a belief of a wider societal responsibility needed to deal with patients with overweight and obesity. The third‐order analytical theme was that discussions about weight were not a priority, and other behavioural interventions, including those relating to smoking, often took precedent. GPs and nurses reported that noting body mass index measurements at every consultation alongside a framework to deliver interventions would likely increase the frequency and perceived efficacy of behavioural weight interventions. GPs and nurses acknowledge the importance of obesity as a health issue, but this is insufficient, particularly amongst GPs, for them to construe this as a medical problem to address with patients in consultations. Strategies to implement clinical guidelines need to make tackling obesity a clinical priority. Training to overcome interactional difficulties, regular weighing of patients and changing expectations and understanding of weight loss interventions are also probably required.
Keywords: behavioural interventions, obesity, primary care, qualitative
1. INTRODUCTION
Several national guidelines recommend that primary care physicians should identify patients with obesity and provide treatment options, including brief opportunistic behavioural interventions. 1 , 2 , 3 A recent trial showed direct evidence for the effectiveness and acceptability of a primary care opportunistic 4 intervention which offered referral to a behavioural weight‐management programme. 5 If implemented at a population level, this could reduce the projected annual incidence of heart disease, hypertension and diabetes by 22%, 23% and 17% by 2035. 5 Despite such evidence and guidelines, primary care weight management interventions are rare and declining. In the United Kingdom, for example, only 3% of people with obesity are referred by general practitioners (GPs) for weight loss support despite obesity prevalence being 27% and the average person visiting their GP six times per year. 6 , 7 Survey data have shown that weight management counselling of patients with obesity visiting their GP in US primary care declined from 33% in 2008 to 2009 to 21% in 2012 to 2013 and the reported prevalence of obesity in primary care records is considerably underestimated. 8 In the United Kingdom, surveys suggest that a minority of patients with overweight (17%) or obesity (42%) recalled ever having been offered weight loss advice by primary care nurses and GPs. 9 Surveys suggest that GPs believe that obesity does not belong in the medical domain, 10 whilst qualitative evidence from interviews suggest that weight loss discussions are an inappropriate use of their time and also worry about damaging the relationship with the patient. 11 Conversely, patients with overweight report being open to receiving GP advice on weight loss, with less than 1% describing it as inappropriate. 5 , 12 A systematic review on this topic 13 uncovered largely quantitative studies, (11/13) (studies were surveys and questionnaires), describing GPs' and nurses' views, finding that weight is awkward to discuss. There have been two 14 , 15 exclusively qualitative reviews investigating this topic. One 14 focused on the issue of stigma, but because of the narrow search criteria (studies had to mention stigma), it did not examine other barriers to conversations (such as time, lack of skills and confidence) nor did it explore clinical implications—for example, it did not examine attitudes towards guidelines. This criterion also limited the breadth and number of studies, including two studies of GPs and five studies of primary care nurses. The other qualitative review by Dewhurst et al. 15 provided insights into GPs' reported views and experiences but missed key studies related to physicians' in training, nurses' experiences and studies related to communication with patients, perhaps because the electronic search was too narrow. We therefore aimed to provide a comprehensive overview of GPs' and nurses' views of treating obesity in primary care using broader selection criteria than either of the other published reviews. Effective strategies to implement obesity guidelines need to understand how GPs and nurses view treating obesity if they are to succeed. We undertook a systematic synthesis of research with GPs and nurses to understand (i) why conversations with patients with overweight are infrequent and (ii) to identify potential mechanisms to increase the frequency of discussions in practice.
2. METHODS
2.1. Terminology
This study included papers from many different countries with different terms for family doctors, GPs, family nurses and practice nurses. For consistency and clarity, we will call all types of family practitioners (GPs) and will call all primary care nurses, practice nurses and family nurses (nurses).
2.2. Search strategy
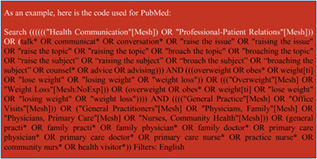
The search criteria used terms relating to (1) primary care, (2) overweight and obesity and (3) discussions and communications about weight (example of search code displayed in Box 1). During the development of the search, we trialled wider search terms, which included ‘cultural influences’ affecting the discussion of weight, but these did not yield additional studies. We also used forward and backward citation searches, which yielded two additional studies.
Box 1: Example of search code.
As an example, the following is the code used for PubMed:
Search (((((("Health Communication"[Mesh]) OR "Professional‐Patient Relations"[Mesh])) OR (talk* OR communicat* OR conversation* OR "raise the issue" OR "raising the issue" OR "raise the topic" OR "raising the topic" OR "broach the topic" OR "broaching the topic" OR “raise the subject” OR “raising the subject” OR “broach the subject” OR “broaching the subject” OR counsel* OR advice OR advising))) AND (((overweight OR obes* OR weight1 OR "lose weight" OR "losing weight" OR "weight loss")) OR ((("Overweight"[Mesh] OR "Weight Loss"[Mesh:NoExp])) OR (overweight OR obes* OR weight1 OR "lose weight" OR "losing weight" OR "weight loss")))) AND (((("General Practice"[Mesh] OR "Office Visits"[Mesh])) OR ("General Practitioners"[Mesh] OR "Physicians, Family"[Mesh] OR "Physicians, Primary Care"[Mesh] OR "Nurses, Community Health"[Mesh])) OR (general practi* OR family practi* OR family physician* OR family doctor* OR primary care physician* OR primary care doctor* OR primary care nurse* OR practice nurse* OR community nurs* OR health visitor*)) Filters: English
2.3. Information sources
Searches were carried out using an emergent rather than an exhaustive strategy, following an approach used to address other complex public health questions. 16 The reviewers identified relevant search terms, which were then further explored by an information specialist (Nia Roberts). Preliminary searches were conducted to check whether known relevant papers were identified. An initial search of the electronic databases PubMed, Embase, Cinahl, Web of Science and PsycINFO was undertaken. Searches were conducted for papers published in peer‐reviewed journals, written in English with publication date between 1945 and 8 October 2018 and supplemented with forward and backward citation searches. The information related to coverage dates of each source is detailed as follows in Box 2.
Box 2: Sources and coverage dates.
2.4. Study selection
We included studies which were carried out in primary care, reported the perspectives of primary care staff in discussing overweight and obesity with adults (18+ years) who were overweight and included qualitative studies based on interviews or focus groups in which GPs and nurses reported their views about discussing overweight.
We excluded studies carried out exclusively in specialist health care, studies that reported GPs' and nurses' views of discussing excess weight with children, parents or pregnant women, studies exclusively about the attitudes of patients rather than health‐care professionals, quantitative studies involving surveys or questionnaires and discussions exclusively concerning underweight or anorexia. Abstracts were excluded because they are too short for useful thematic analysis. Books and dissertations were excluded for practical reasons.
Title and abstract screening was conducted by two independent reviewers (WW and CA) using Covidence. In the event of disagreement, the article proceeded to the next phase. 17 Full text screening was done by WW, and two 10% samples were checked by other authors.
2.5. Quality assessment and risk of bias
We appraised data quality using the Joanna Briggs checklist, which has been recommended as the most coherent and comprehensive tool to capture study quality. 18 Based on the results of this checklist, we assessed whether the ‘higher‐quality’ studies contributed richer data to the thematic analysis We found that there was no such relationship and therefore included all papers. 17
2.6. Methods for data extraction and a thematic synthesis
We included both the results and interpretations sections of papers, following the approach of Thomas and Harden. 19 , 20 Thematic synthesis involved three overlapping stages: (i) free line‐by‐line coding of the all findings and discussion sections of the primary studies using NVivo software (version 11) 21 ; (ii) the consolidation of these ‘free codes’ into related areas to develop overarching ‘descriptive themes’ which were completed by organising the results into a mind‐map (WW, CA and BN) 22 ; (iii) and the development of analytical themes, which directly addressed the aims of the review. In meta‐ethnography, the equivalent to this last stage of ‘analytical themes’ is ‘third‐order interpretations.’ 23
2.7. Protocol and registration
We wrote a protocol which was supplied to the editor of the journal.
3. RESULTS
The search identified 1,525 nonduplicated studies, of which 29 were included for final analysis after a screening process displayed in Figure 1. Qualitative data from the included studies provided data for 601 GPs and nurses. The earliest paper was published in 2001.
FIGURE 1.
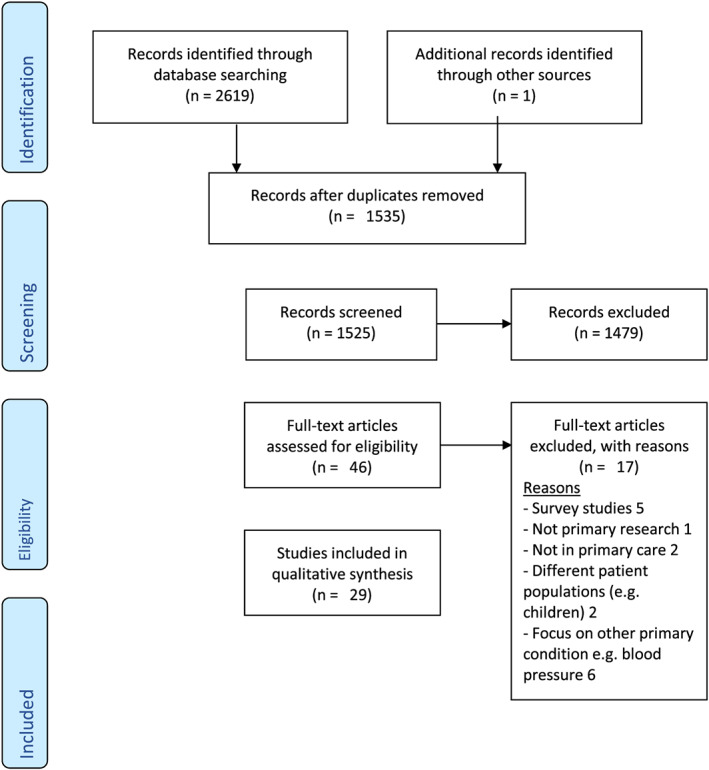
PRISMA flow chart of included studies
3.1. Study quality and risk of bias
There were some quality issues. Some studies did not report ethical approval 11 , 24 ; authors drew conclusions that did not flow from the data 25 or did not discuss reflexivity. 26 , 27 Recruitment to the study group was sometimes self‐selected from a subgroup with training in weight management 28 , 29 , 30 or recruitment was incentivised by offering educational obesity treatment training, 27 which perhaps meant that clinicians with greater interest were recruited.
3.2. Descriptive themes summary
Table 1 demonstrates the similarity of findings across different countries, between 2001 and 2017. The themes are the interactional difficulty of raising the topic in the consultation, a lack of confidence in treatments, a lack of confidence in patients to make changes, lack of knowledge and skills, insufficient time or resources, the suggestion that weight loss is not their clinical responsibility and stigma. Table 1 also illustrates that there has been little change in the number or types of themes discussed since 2001. In some instances in the following sections, descriptive themes are discussed together to save space.
TABLE 1.
Summary table of included studies with descriptive themes from thematic synthesis
| Study information | Descriptive themes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study name | Country | GP and/or nurse | Study type, e.g., focus groups | Lack of confidence in treatments | Lack of confidence in patients' ability to follow treatments | Awkward nature of discussing weight | Lack of knowledge/skills | Lack of resources/competition for resources | Not GPs' or nurses' responsibility | Stigma |
| Mercer and Tessier 11 | UK | 10 GPs 10 nurses | Interviews after survey | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Huang et al. 31 | US | 24 GPs | Focus groups | ✓ | ✓ | |||||
| Douglas et al. 32 | SCO | 10 nurses | Interviews after questionnaire | ✓ | ✓ | |||||
| Epstein and Ogden 33 | UK | 21 GPs | Interviews | ✓ | ✓ | ✓ | ✓ | |||
| Ribera et al. 24 | ESP | 33 GPs and Nurses | Interviews and focus groups | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Forman‐Hoffman et al. 34 | US | Seven GPs | Focus groups | ✓ | ✓ | ✓ | ✓ | |||
| Alexander et al. 35 | US | 17 GPs | Focus groups | ✓ | ✓ | ✓ | ✓ | |||
| Brown et al. 36 | UK | 15 GPs | Interviews after survey | ✓ | ✓ | ✓ | ||||
| Leverence et al. 37 | US | 14 GPs and nine nurses | Interviews | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Ampt et al. 28 | AUS | 15 GPs and one nurse | Interviews (after prevention trial) | ✓ | ✓ | ✓ | ||||
| Ali et al. 38 | UAE | 15 GP and five nurse | Interviews (new sample) | ✓ | ||||||
| Jochemsen‐van der Leeuw et al. 39 | NL | 13 GP trainees and 12 trainers | Focus groups (new sample) | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Hansson et al. 40 | SWE | 10 GPs and 10 nurses | Interviews | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Heintze et al. 41 | DEU | 15 GPs | Interviews | ✓ | ✓ | ✓ | ||||
| Derksen et al. 42 | NL | 12 GPs and three nurses | Interviews and focus groups | ✓ | ✓ | |||||
| Gudzune et al. 30 | US | 24 GPs and two nurses | Focus groups (after obesity trial) | ✓ | ‘✓ | ✓ | ✓ | ✓ | ||
| Gunther et al. 43 | UK | Seven GPs and seven nurses | Interviews | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Nolan et al. 26 | UK | 22 nurses | Interviews | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Sonntag et al. 44 | DEU | 15 GPs | Interviews | ✓ | ✓. | ✓ | ||||
| Phillips et al. 45 | UK | 18 nurses | Interviews | ✓ | ✓ | ✓ | ✓ | |||
| Claridge et al. 46 | NZ | 12 GPs | Interviews | ✓ | ✓ | ✓ | ✓ | |||
| Blackburn et al. 47 | UK | 17 GPs and 17 nurses | Interviews | ✓ | ✓ | ✓ | ✓ | |||
| Kim et al. 48 | AUS | 12 GPs | Interviews | ✓ | ✓ | ✓ | ||||
| Teixeira et al. 4 | PRT | 16 GPs | Interviews | ✓ | ✓ | ✓ | ||||
| Ashman et al. 29 | AUS | 12 GPs | Interviews | ✓ | ✓ | ✓ | ||||
| Antognoli et al. 27 | US | Nine GPs | Interviews with most knowledgeable GP trainers after survey | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Asselin et al. 49 | CAN | 15 nurses | Interviews (participants from obesity trial) | ✓ | ||||||
| Glenister et al. 50 | AUS | Seven GPs and seven patients | Interviews | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Lee et al. 25 | SGP | 50 GPs | Interviews and focus groups | ✓ | ✓ | |||||
| Total | 17 | 17 | 22 | 15 | 13 | 16 | 7 | |||
Abbreviation: GP, general practitioner.
3.3. Descriptive themes
3.3.1. The awkward nature of weight discussions
The interactional delicacy of the topics was a key theme addressed in 22 of 29 papers. It covered a number of subthemes described as follows.
Word choice
Clinicians reported word choice as a barrier, with concern particularly that their patients might be offended and rapport damaged if terms such as ‘overweight’ or ‘obesity’ were used. 25 , 27 , 36 , 44 , 45 , 47 , 48 , 50
This experience was similar across many different countries in both public and private settings: a UK GP reported that using these terms was not ‘very PC (politically correct)’ and could cause patients to get ‘very hurt’ 47 ; another Singapore GP in a private practice reported patients being offended by such terms. 25
It's a very sensitive subject you cannot tell the patient ‘Oh by the way, I think you are obese’ because you'll end up offending them, they'll never come to your clinic again [laughs]. GP, Singapore (who ran several private clinics) 25
Clinicians reported softening of terms and generally avoiding the term obesity because of its negative connotations. 51 Instead clinicians reported asking more general questions about whether the patient had ever tried to lose weight. The word choice at the start of the conversation when broaching the topic was deemed most difficult.
I find it quite difficult because I do not want to offend someone, I do not wanna start off by putting them on sort of the back foot. Nurse UK 51
Difficulty making progress on a complex problem in time constraints
Weight and obesity were reported as too complex to deal with in a 10‐min appointment, 50 especially if a patient was presenting for another reason. 27 , 34 , 47 The complexity of the subject was attributed to the belief that obesity was related to many other aspects of a patient's life 46 , 50 and that behaviour change was a long‐term process requiring long‐term management. 42 The personal and societal roots of the issue made clinicians feel disempowered to properly address within the time constrains of their consultations. 46
Comparative difficulty of assessing obesity
Some GPs, nurses and GP trainees suggested that obesity was more difficult to discuss than smoking 39 because smoking was seen as a more accepted risk factor 47 and more straightforward to assess 28 and treat. 39 There was a perception that smoking was a clear choice in behaviour whereas obesity was a consequence of a long‐term aggregation of several behaviours.
Smoking is more a choice while becoming overweight just happens. GP, New Zealand 46
These behaviours (such as diet and physical activity) were often inferred by appearance, only being assessed if the patient was visibly overweight. 28
Reported mechanisms used to broach the awkward topic
A long‐term trusting relationship between the patient and clinician 30 , 39 , 40 , 41 , 45 , 50 eased discussion. Clinicians also found that objective ‘medicalised’ body mass index (BMI) measurements, or reading guidance from the computer, helped them feel more comfortable. 25 , 30 , 33 , 37 , 40 , 46 , 51
I actually, sort of, put it sideways and say, ‘Well the computer's saying that, in fact, you are overweight or obese’ Nurse, UK 51
Clinicians described linking discussions of weight to relevant medical concerns. 25 , 30 , 33 , 37 , 40 , 46 , 51 The topic was also seen as less interactionally difficult when they positioned the issue as more ‘doctorable’ (e.g., if there was severe obesity 28 , 33 and bariatric surgery 48 was a treatment option.
For those seriously overweight … who are either encountering medical problems, or at a high risk of medical problems, and actually probably what we should be taking is a more medical medicalised approach. UK, GP 33
Some GPs and nurses said they felt more comfortable reframing weight loss discussions as recommendations about maintaining health. 30 , 51 GPs and nurses also speculated that if they were ‘forced’ to intervene by some mechanism, they would be more likely to discuss weight. 28
3.3.2. Lack of confidence in treatments and patients' ability to follow treatments, and lack of knowledge and skills
Three themes widely developed across studies: a lack of confidence in the treatments (reported in 17 studies), clinicians' lack of knowledge and skills to support weight loss (cited in 15 studies) and lack of confidence in patients' abilities to make changes and sustain weight loss (cited in 17 studies).
Lack of confidence in treatment
Clinicians' lack of confidence in treatment was a key theme addressed in 17 of 29 papers. It covered a number of subthemes described as follows.
Lack of previous success
Past experience of treatments' lack of success often made clinicians doubtful about offering them,
I just have not seen it be very successful with very many people. … I mean the reality is [that] you know from everywhere you look weight loss does not work very well for most people. GP, USA 37
Clinicians also worried about recommending a treatment they had little faith in because this could damage their credibility with the patient. 33
Lack of confidence in skills
Lack of specialist skills to talk about what was believed to be a very complex topic gave physicians reservations about broaching the subject,
I do not feel confident to really get into the nitty gritty of… patients' questions about this diet, this food and that food, and I think, oh, I'll leave that to somebody else to do. GP Australia 29
The lack of confidence in skills was in some instances blamed on lack of a standardised approach to raising the issue. 47 Despite this, some clinicians attempted interventions drawing from personal experience and media sources. 47
Lack of confidence in patients' ability to make changes
Clinicians doubted that patients had the ability to make changes with some suggesting that the prevalence of obesity in society was proof that individuals' weight loss strategies did not work. 37 They expressed these thoughts sometimes in pejorative terms.
You can lead a horse to water but you cannot stop it eating cream cakes. GP, UK 43
This pessimism was sometimes presented as borne of experience, but some acknowledged their own lack of skills 29 and knowledge of effective treatment, 37 which contributed to a reported feeling of powerlessness. 33 Some GPs said that they wanted to encourage patients to lose weight but did not know how to do so, 29 whilst others spoke pejoratively about patients who were reluctant to change. 46
Lack of confidence in existing guidelines and metrics of success
Some GPs believed that following guidelines which encouraged clinicians to use weight metrics and to judge success by weight or BMI ‘as yardsticks of success’ was the wrong approach. Furthermore, this damaged their self‐efficacy since they knew they did not believe what they were being told to recommend and track would help people lose weight.
I do not want to be falsely saying… ‘I really believe if you do this this would be effective’… GP Australia 29
Authenticity was also felt more challenging by those clinicians with a lower personal BMI. 51
National guidelines were judged by some as needing to be localised, taking into account local needs and variances in obesity service provision. 43 Others were reluctant to follow national guidelines, 35 preferring to draw on and adapt personal experience about what techniques had been successful interventions. 45
Mechanisms to improve clinicians' confidence in prospect of change
Across several studies, clinicians reported that tracking patients' weight had made them less pessimistic. 25 , 30 , 33 , 37 , 40 , 46 , 51 Even where this system was not in place, some GPs reflected that they thought it would help. 29
Gudzune describes clinicians' belief that by acknowledging any degree of weight loss success provided positive reinforcement.
‘You've lost six pounds since you were here last.’ [Patients] really need that positive feedback that we are paying attention to what they are doing. GP, Singapore 30
Nurses in a UK study said they found it effective to link weight loss to a future social event in patients' lives (e.g., wedding) to incentivise change. 45 Similarly linking patients' weight to wider objective health measurements was perceived to keep patients motivated. 30 Another approach was to moderate GPs' and nurses' expectations so that modest weight loss, or no weight gain, could be seen as an achievement. This approach of encouraging either moderate weight loss or preventing weight gain was observed to ameliorate GPs' sense of frustration. 11 , 29
3.3.3. Responsibility
Another highly developed descriptive theme, reported in 20 studies, was that it was not GPs' and nurses' responsibility to intervene. These papers discussed subthemes, including the boundaries of medical responsibility, patients' responsibility, differences in role perceptions between GP and nurses and the role of the clinician in society.
Medical responsibility does not include treating obesity unless severe
There was concern about medicalising what many viewed as a nonmedical problem 4 , 26 , 42 , 47 for which society, the patient or the family should take responsibility. 35
I do not think you should take it for granted that we are the ones to intervene. We're trained in medical care. Overweight and obesity are more of a societal problem. GP, Sweden 40
However, if obesity was deemed to be ‘severe’ (sometimes 45 defined by clinicians as BMI ≥ 35), clinicians did acknowledge the necessity to intervene. 4 , 33 , 45
Patients' responsibility
GP participants in a study exploring the delivery of a lifestyle behavioural risk factor screening and management health check often discussed a patient's motivation as if it was immoveable. 28 Some said that once the patient had been educated regarding risk factors, the responsibility whether to act lay with the patient. 28 In studies examining GP training, GP trainers and trainees noted that how discussing obesity with patients or in general was not prioritised in the curriculum. 27 , 39
Different responsibility between GPs and nurses
There were differences between nurses and GPs attitudes towards discussing weight. Some GPs suggested that dealing with overweight and obesity was an inappropriate use of their time or that responsibility for this task should be shifted to nurses. 11 , 40 Both nurses and GPs reported that talking about weight could damage their patient relationship, but nevertheless, nurses reported feeling responsible for raising the topic. 47 No studies reported nurses saying that treating patients with obesity was not their responsibility (0/10), whereas GPs in 11/20 studies did report this.
We are not the friendly neighbour, we are health care professionals. I do see it as my professional task to tell patients about the risks of their weight …. Nurse, Netherlands 42
Society's responsibility
Some GPs believed that their responsibility to intervene was somewhat undermined by a belief that the bigger actions lay with society. 35 Some nurses said that causes of obesity, including childbirth and media influences, were too complex to resolve through a general discussion and therefore focused on patients taking greater personal responsibility. As one author 51 summarises,
It was evident that this was a difficult course to steer, and eventually some participants would return to the importance of personal lifestyle in obesity: ‘So it is lifestyle, it is, you know, them’ Nurse UK.
Some 35 , 37 saw the family as responsible for a family member's weight.
‘If the family was not onboard, it would be “very hard, if not nearly impossible” to achieve a weight loss.’ GP, US. 35
Contexts where GPs and nurses took responsibility for weight loss discussions
Participants in several studies reportedly felt responsible to intervene. 30 , 35 , 37 , 41 , 42 , 46 These examples were from the Netherlands, the United States of America, New Zealand Sweden and the United Kingdom which all have different health systems, with different payment models and consultation lengths. (Consultation lengths in the United States and New Zealand are 3‐5 min longer than in the United Kingdom or the Netherlands 52 , 53 ). If the GP saw their role as treating disease, rather than attending to risk factors, then obesity in the absence of an associated health problem was out of their sphere 27 as this author notes ‘[Staff] considered that their main task was to treat diseases, and overweight and obesity were seen more as conditions that might involve a risk of diabetes or some other disease.’ 40
However, if a disease associated with obesity was present, then intervention could be justified as it ‘lifted the negativity and ambiguity that existed about managing obesity,’ 11 though even in such a scenario, one GP reported that it would still be a task better suited to a nurse. 40
A final mechanism which GPs reported making them feel responsible was having a system of long‐term follow up in order to achieve sustained weight loss as this Dutch GP suggests,
There is a neat reporting system, but after the last treatment no one feels responsible. 42
3.3.4. Lack of resources and competition for resources
Doctors and nurses reported that they did not have sufficient time to address overweight 40 and that other activities took priority. 47
That's the trouble is not it, it's the conflict of time for all the other things that we are supposed to do in a ten‐minute consultation, of which probably smoking cessation comes quite high on the sort of health promotion thing … and alcohol, of course, that's another. Nurse, UK 47
Contexts when time and resources were allocated to obesity
When there was a formalised framework, GPs and nurses reported feeling a sense of duty to make weight interventions. 4 , 24 , 28 These frameworks were reported to have positively affected nurses' role adequacy and legitimacy 26 and helped make practitioners feel supported. 43
It is part of our functions and our workload … to engage a preventative approach, advising patients to lose weight or do … Measuring weight is now a mandatory procedure for all of us in all consultations. We do it on a daily basis for every patient, regardless if he or she is overweight or not. GP, Portugal 4
3.3.5. Stigma
Stigma was a descriptive theme that was apparent in the tone of many clinicians' responses to statements and cited by many of the primary authors. 27 , 40 , 41 , 43 , 47 , 50 , 51 It can be seen in a number of themes.
Difficulty negotiating the stigma when advocating weight loss
Clinicians reported a worry that patients would think they were stigmatising them by talking about weight and imply they were lazy or greedy, 46 which sometimes led them to avoid the topic. 50 The stigmatised nature of obesity in society more generally made some clinicians avoid the topic even if they themselves did not report a stigmatised attitude towards patients. 36 Other clinicians noted the associated psychological problems with obesity as stigmatising and sometimes assumed they had associated conditions which made conversations difficult.
Depending on their mental health, so if somebody's a bit um, if they are fragile you certainly would not be bringing up about their weight. GP, Australia 50
A stigmatised attitude towards patients with obesity, especially those from poorer or certain ethnic backgrounds
Others had a stigmatised attitude towards those with obesity, describing patients as lazy and lacking in energy or indifferent to their situation. 40 Even those who were motivated to lose weight were thought to be reluctant to make the necessary changes. And those who did seek help did so for the wrong reasons, such as wanting to wear smaller clothes.
Patients want to lose weight but they do not want to change. Start walking instead of taking the bus, and eat less, that's all there is to it. Or the motivation might be there but they do not really want to do it, only if they think it's important. GP, Sweden. 40
This stigmatised attitude towards patients was especially apparent in papers which focused on patients on low incomes 37 or those from certain ethnic backgrounds, 40 with these groups reported to be less frequently counselled.
Contexts when stigma was overcome
Some clinicians believed that the stigma could be overcome by focusing on health‐focused approaches rather than purely weight focused approaches. 29 These included the ‘Health at Every Size’ movement which aims to reduce weight‐related stigma by focussing on other potential health‐related benefits of interventions, by focusing more on medical endpoints such as fasting glucose or blood pressure, aiming for a maintenance of current weight (over or otherwise) or aiming for lifestyle changes such as increased physical activity which have recognised health benefits independent of weight. 29 Others believed that stigma could be reduced by not using terms such as ‘obese’ or talking around the topic.
I just talk in terms, you know, ‘Have you ever thought, you know, trying to lose weight?’ or this sort of thing, not just saying, ‘You're obese.’ I think that they must know they are overweight—you do not want to rub it in. Nurse, UK 36
3.4. Analytical theme summary
Although the papers reported different clinical perspectives across different settings, there were clear similarities connecting clinicians' views towards discussing weight (Figure 2). Each of these themes contributed to clinicians affording low priority to intervening with patients on obesity. Clinicians often spoke about patients with obesity in a way that reflected society's underlying stigma about obesity.
FIGURE 2.
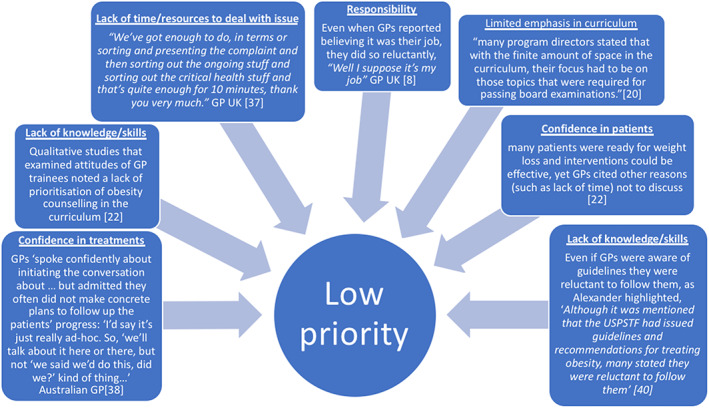
Themes contributing to the lower priority afforded to weight management discussions
3.5. Analytical theme: Low priority of weight discussions
The main overarching theme that binds the first‐ and second‐order themes was the low priority given to obesity interventions. This was remarkably consistent across studies over decades of research. This sense of low priority was shared by doctors, nurses, doctors in training and across different health‐care systems (both public and private).
3.5.1. Low priority of weight discussions
Many of the descriptive themes listed in Table 1 can be viewed through the lens of priorities (Figure 2). Discussing weight was not a priority for GPs and nurses at all levels of seniority. This higher‐order latent theme was present even amongst those GPs and nurses who said they had confidence in their patients and in the treatments. Even those who saw discussing weight as their responsibility often did it reluctantly. 26 , 40
Prevention activities perceived as a second division of optional approaches … the doctor in general is more concerned with whether the patient smokes or has high cholesterol … Spanish study of GPs and nurses 24
Stigma
Stigma fed into the low‐priority theme. In some clinicians' responses, their tone hinted that recipients of their care are unworthy or make themselves unworthy of their time and constructed obesity as an individual behavioural problem. 33 Obesity was constructed by some clinicians as both a fault of individuals' behaviours whilst also noting that it was a social problem for wider society to deal with rather than be medicalised in their clinic 33 , 34 , 37 , 40 (Tables 2 and 3).
TABLE 2.
Summary table for quality assessment using the Joanna Briggs checklist
| Paper congruity | Alexander et al. 35 | Ali et al. 38 | Ampt et al. 28 | Antognoli et al. 27 | Ashman et al. 54 | Asselin et al. 49 | Blackburn et al. 47 | Brown et al. 36 | Claridge et al. 46 | Derksen et al. 42 | Douglas et al. 32 | Epstein et al. 33 | Glenister et al. 50 | Gudzune et al. 30 | Gunther et al. 43 | Hansson et al. 40 | Forman‐Hoffman et al. 34 | Heintz et al. 41 | Huang et al. 31 | Jochemsen et al. 39 | Kim et al. 48 | Leverence et al. 37 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Theoretical framework | + | + | + | − | + | + | + | + | + | + | − | + | + | − | + | + | − | + | + | − | + | + |
| Appropriateness of research design | + | + | ‐ | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Data collection | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | + | + | + |
| Data analysis | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | + | + | + | + |
| Findings | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Context | + | + | + | + | + | − | + | + | − | − | − | + | + | ‐ | + | + | − | + | + | + | + | + |
| Impact of investigator | ‐ | − | ‐ | − | + | − | ‐ | − | ‐ | ‐ | − | ‐ | + | − | + | + | ‐ | − | − | − | + | − |
| Believability | + | + | ‐ | ‐ | + | + | + | + | + | − | + | + | + | + | + | + | + | + | + | + | + | + |
| Ethics | + | + | + | + | + | + | + | + | + | − | + | + | + | − | + | + | − | + | − | − | + | − |
| Evaluation/outcome | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Paper congruity | Lee et al. 25 | Mercer and Tessier 11 | Nolan et al. 26 | Phillips et al. 45 | Ribera et al. 24 | Sonntag et al. 44 | Teixeira et al. 4 |
|---|---|---|---|---|---|---|---|
| Theoretical framework | + | + | + | + | + | + | + |
| Appropriateness of research design | − | + | + | + | + | + | + |
| Data collection | + | + | + | + | + | + | + |
| Data analysis | + | + | + | + | + | + | + |
| Findings | + | + | + | + | + | + | + |
| Context | + | + | + | + | + | + | + |
| Impact of investigator | − | − | + | − | − | − | + |
| Believability | − | + | + | ‐ | + | + | + |
| Ethics | + | − | + | + | − | + | + |
| Evaluation/outcome | − | + | + | + | + | + | + |
TABLE 3.
Study characteristics
| Author, year | Sample size | % (f) | % nurses | Country | BMI | Methodological and theoretical approach | Method/places of recruitment | Age range |
|---|---|---|---|---|---|---|---|---|
| Alexander, 2006 | 17 | 65 | 0 | US | 18 to 33 (mean 23.7; SD, 4.0) | Grounded theory | Emailed colleagues in medical Centre | 29–61 |
| Ali, 2009 | 29 | 100 | 34 | UAE | Not given | Grounded theory | Not given. | Not given |
| Ampt, 2009 | 15 | 54 | 0 | AUS | Not given | The theory of planned behaviour | Through involvement in recent similar study. | Not given |
| Antognoli, 2017 | 38 | Not given | 0 | US | Not given | Not given | Letter (but incentivised through training for obesity and nutrition counselling) | Not given |
| Ashman, 2015 | 12 | 66 | 0 | AUS | Not given | Social cognitive theory | Snowball recruitment of GPs who had agreed to deliver a pilot of an obesity management programme. | 31–60 |
| Asselin, 2016 | 29 | 97 | 100 | CAN | Not given | Theoretical domains framework | Family practices who were randomised to the intervention of an obesity management tool. | 26–68 |
| Blackburn, 2015 | 34 | 82% combined (64% GPs 100% nurses) | 50 | UK | 18–30 + (52% healthy weight, 32% overweight, 11% obese, 2% not specified). | Theoretical domains framework | Email to GP surgeries, thereafter snowball recruitment, practice level reimbursement for their time. | 30–49 |
| Brown, 2007 | 15 | 100 | 100 | UK | 40% healthy weight, 33% obese, 26% healthy range | Pragmatic qualitative methodology | Postal survey response about obesity management | 28–57 |
| Claridge, 2014 | 12 | 42 | 0 | NZ | Not given | Inductive thematic analysis | 33% existing connection, 67% random calling of GP clinics. | 31–60+ |
| Derksen, 2012 | 11 | 66 | 72 | NL | Not detailed, only given in vague language e.g. ‘about one‐third seemed to be overweight’ | Not detailed | Members of research team asked their colleagues. | Not detailed. |
| Douglas, 2005 | 10 | 100 | 100 | SCO | Not given | Not detailed other than ‘mixed methods approach’ | Recruited by virtue of them returning a questionnaire | Not given |
| Epstein, 2005 | 21 | 52 | 0 | UK | Not given | Interpretative phenomenological approach | All GPs in one trust were invited but not detailed by what method. | 30–60+ |
| Glenister, 2017 | 7 | Not given | 0 | AUS | Not given | Thematic analysis | Email sent to two general practice in two towns. | Not given |
| Gudzune, 2012 | 26 | 58 | 8 | US | Not given | Not detailed | Recruited as a substudy from an obesity reduction trial, only practitioners who had enrolled 4 or more patients in the trial were eligible. | Mean (SD) 46.4 (10.7) |
| Gunther, 2012 | 14 | 85.5 combined (43% female amongst GPs, 100% amongst nurses) | 100 | UK | Not given | Interviews used but no theory detailed | ‘Obesity leads' in trusts were aksed to identify practices with different levels of obesity | 31–64 |
| Hansson, 2011 | 20 | 65 | 50 | SWE | Not given. | Phenomenographic | Mail/phone to medical heads of primary care centres in well‐defined area in Sweden who then referred staff. | 34–60 |
| Hoffman, 2006 | 6 | Not given | Not given | US | Not given | Focus groups but theory not mentioned | Not detailed | Not detailed |
| Heintz 2011 | 15 | 60 | 0 | DEU | None had elevated BMI (mean 22.4) | Free associated narrative method, MAYRING's qualitative content analysis and theoretical sampling | Written letter sent to 70 GPs who which 15 participated in the study | Mean age 51 |
| Huang, 2004 | 24 | 22 | 0 | US | Not given | Focus groups with scripted probes and encouraged participants to clarify answers | Not detailed but participants compensated between $50–100 depending on seniority | 27–52 |
| Jochemsen, 2011 | 25 | 60 | Unclear because GP teachers are both GP's and behavioural scientists | NL | Not given | Focus groups with probing questions, no theory detailed | Prospective sampling by selecting every third name on an alphabetical list from GP training Centre | 29–36 for trainees, trainers not detailed |
| Kim, 2015 | 24 | 54 | 0 | AUS | Not given | Semistructured interviews, not wider theory detailed | Invited via email sent by primary care organisations' local liaison officers. | Not given in full detail |
| Leverence, 2007 | 23 (paediatricians not included) | 43 total (but not detailed when paediatricians removed) | 39 | US | Not given | In depth semistructured interviews and focus groups designed to elicit encounter‐based narratives | Not detailed other than a researcher directly contacted prospective interviewers in sample taken from research in outpatient settings network | Not given |
| Lee, 2017 | 50 | 42 | 0 | SGP | Not given | Grounded theory. Focus groups and in‐depth interviews. | Email and telephone contact, but no further detail | 25–56 |
| Nolan, 2012 | 22 | 95 | 100 | UK | Not given | Semistructured face‐to‐face interviews. Interviewer worked locally for primacy care trust as an obesity lead and had organised local obesity training, and some participants were aware of this. | Invited by letter to nurses, contacted subsequently via telephone. During recruitment, potential participants were told study was about take‐up and use of NICE guidance on obesity. | Not detailed |
| Phillips, 2013 | 18 | 100 | 100 | UK | Not given | F2F interviews with a thematic analysis of results. | Via email sent to lead nurses for local health board who were asked to send to all practice nurses in their area. Interested nurses contacted the research team via email or phone. 78% declared specific interest in obesity management | Not detailed |
| Ribera, 2005 | 33 | Not detailed for focus groups | 45 | ESP | Not given | Semistructured interviews corroborated data and focus groups provided ‘in‐depth personalised information’. Stages of change theory and decisional balance concept was used. Theoretical sampling strategy was used. | Not detailed for focus groups, but overall sample was selected from seven regions of Catalan health system, it does not detail how they were contacted. | Not detailed |
| Sonntag, 2011 | 15 | 60 | 0 | DEU | None had elevated BMI (mean 22.4 kg/m2) | Semistructured interviews with open‐ended questions, transcribed and subjected to Mayring's technique for qualitative analysis. | GPs were contacted by the local board of health in Berlin and not incentivised. | Average age 51 |
| Teixeira, 2014 | 16 | 56 | 0 | PRT | Average BMI 25.55/m2 (range 20.83–30.48 kg/m2). | Semistructure face to face interviews with an inductive thematic analysis of results. | GPs invited via telephone and/or after approval of heads of GP centres. After first contact, snowball sampling employed | 32–57 |
Abbreviations: BMI, body mass index; GP, general practitioner.
I do not think you should take it for granted that we are the ones to intervene. We're trained in medical care. Overweight and obesity are more of a societal problem. GP, UK 40
There's also the other side of what that patient is doing, or not doing, … so there's just so far that we as providers can go. You can educate but then it's on the other side, in the other party's hands. GP, America 37
Financial incentives
Financial incentives were reported as making weight management a higher priority.
With the introduction of QoF, we are increasingly aware of certain things we need to address … obesity interacts with other co‐morbidities … So, you cannot ignore it. GP UK 43
4. DISCUSSION
4.1. Statement of principal findings
Discussing weight was found consistently as not a priority for primary care GPs, GP trainees or nurses. This consistency demonstrates the imperative for policymakers to take action to improve the implementation and perceived value in obesity guidelines. The reasons clinicians gave for not intervening on obesity were as follows: that discussing weight was interactionally difficult; it was not seen as the GPs' responsibility to treat people with obesity, although nurses felt more that this was their responsibility; nurses and GPs lacked knowledge about interventions and it had not been prioritised in the GPs' curriculum; a lack of confidence in patients' ability to make changes; and a lack of confidence in the efficacy of treatments. Clinicians reflected stigmatised views of people with obesity.
4.2. Strengths and weaknesses of the study
A strength of this study was the qualitative thematic synthesis method, which was chosen because it has been used successfully to address questions relating to intervention need, appropriateness and acceptability. 55 It draws on relevant elements of grounded theory (taking an inductive approach using constant comparison) and meta‐ethnography (using third order interpretations). Another strength was its focus on primary care. Brief opportunistic interventions are arguably more relevant in primary care than in other contexts, 1 particularly in view of the long‐term regular contact, 56 which is important given individuals' difficulties in sustaining long‐term weight loss and the impact of trust and ongoing relationships in enabling clinicians to raise this topic.
Our review was limited by the quality of available of studies as well as the quality assessment tool. The Joanna Briggs checklist was used in accordance with good practice, but there was a mismatch between the richness of the data in the studies and the score they received in the checklist, which raises questions of the usefulness of such checklists. Additionally, every study in this review asked clinicians directly about why they do not intervene to help patients who are overweight. Studies repeatedly elicited responses such as lack of time or that it is awkward to discuss. This approach is likely to be subject to social desirability bias, 57 which encourages interviewees to present a justification for their lack of engagement with the official standard of care. Investigators appeared not to have gone beyond reporting these reasons to probe more deeply to uncover the cause of this reluctance.
4.3. Findings in relation to the existing literature
We identified four existing reviews in this domain, two of which were either exclusively 58 quantitative or predominantly quantitative studies. 13 Regarding the two remaining qualitative reviews, one 14 was useful to contextualise health‐care workers' thoughts on obesity stigma, but it did not explore the relevant clinical implications—for example, it did not examine attitudes towards obesity guidelines. Moreover, the breadth of this previous review was limited: it only included two studies with GPs and five studies with nurses, whereas we included 23 with GPs and seven with nurses. The other qualitative review by 15 provided insights into GPs' reported views and experiences but did not include studies related to physicians' in training, nurses' experiences and studies related to communication with patients perhaps because the electronic search was too narrow. Although the review of Dewhurst et al. included 16 studies, we included 14 of the same studies and an additional 15. By using different search terms, our review uncovered further studies, which gave a unique insight. For example, Ashman et al. 29 explored GPs' self‐efficacy towards obesity treatments and discovered that GPs did not feel ‘authentic’ giving advice related to BMI targets, which they felt were unlikely to work, and instead reported preferring to give interventions related to positive lifestyle changes, such as exercise which may have health benefits independent of weight.
Stigma was a theme that was raised in a number of different guises by clinicians in our study, building on a wide body of work on this topic. 59 , 60 There was an apparent contradiction in clinicians' attitudes who could simultaneously think it was both individual's responsibility to lose weight but also caused by a wider social problems, and both these perceived causes meant that intervening was not worth the clinicians time. This mindset has been previously highlighted in analysis of moral discourse in clinicians accounts about weight counselling, 61 which they noted contributed to a feeling of both tension and powerlessness amongst clinicians. Our study built on this individual versus society analysis and found that this attitude became more acute towards patients from poorer backgrounds, who they deemed lazier, 37 and towards groups from certain ethnic backgrounds, whose cultures did not prioritise weight loss interventions. 46
We also built on existing literature that had highlighted that clinicians may not always stigmatise individuals but find it hard to negotiate stigma when advocating weight loss. 61 Our study also complemented literature 62 which noted the impact of weight stigma on patients' care, finding that experiences of perceived substandard care may cause avoidance of care, poor adherence to weight management interventions and distrust of clinicians. This was reflected in our own findings of perceived physicians' frustrations in patients' adherence with interventions.
4.4. Meaning of the study: Possible mechanisms and implications for GPs, nurses and policymakers
The findings suggest that GPs see intervening on obesity as a low priority. This feeling was not so marked for nurses. The lack of confidence in the patients and treatments sometimes gave the impression that it was not that GPs did not have sufficient time, but treating obesity was not worth their time [1], sometimes related to an underlying stigma towards those with obesity. 50 What little time they did have should be used to treat priorities such as disease and more important prevention activities. 24 It appears therefore that GPs do not want to intervene or do not like intervening, and some of the reasons proffered may mask this underlying sense of dislike. Why might this be so? Anthropological studies of medical training show the emphasis placed on diseases, technical procedures and technological medicine and less on the behavioural aspects of medicine, such as prevention especially areas such as obesity where there are no easily prescribed medicines. 63 , 64 GPs in training believe that disciplines of medicine that involve highly technical procedures or experiments, such as surgery or laboratory medicine, are more prestigious than primary care. 65 Normalisation Process Theory proposes that interventions are adopted if clinicians value them. 66 Nursing places less emphasis on the technological aspects, and thus nurses seem to feel more duty to act on what both groups consider to be an important risk factor for ill health. Thus, interventions to support physicians need to grapple with this cultural block and find a way to make clinicians, particularly doctors, feel that intervening on obesity is valuable work. In addition, clinicians were highly sceptical of their ability to intervene for patients and patients' ability to respond, but such beliefs can be countered with evidence, but they also need the skills and confidence to enact brief interventions. When GPs did decide to intervene, they did so in a way which evidence has shown to be unhelpful. To navigate the perceived interactionally difficult and stigmatised topic, GPs and nurses talked around the issue 50 or linked weight to a corresponding health issue, believing they were on ‘safer ground’ and this would cause less offence to a patient. 46 , 50 , 67 However, there is evidence that GPs' and nurses' attempts to link discussions of weight to the patients' own health issues can result in resistance. 56 Other previous studies have noted the interactional delicacy and suggested that training is needed to make clinicians far more confident in navigating this delicacy. 68
4.5. Summary and future perspectives
Clinicians offer a variety of explanations as to why they do not offer support to their patients to lose weight, despite national guidelines that urge them to do so. These relate to the awkward and potentially stigmatising nature of the conversation, the lack of faith that patients will change and their own lack of a clear intervention to offer. However, underlying all this is a sense that such conversations are not valued, especially by doctors, and that this relates to unspoken value systems in medicine that prize technological fixes over behavioural interventions. Addressing nonadherence with guidelines will require attention to these underlying values.
SUMMARY BOX OF REPORTED MECHANISMS COVERED IN TEXT THAT ENABLED WEIGHT CONVERSATIONS.
When GPs and nurses allocate their time and resources to dealing with obesity.
-
When weight measurement becomes mandatory.
-
When there is a formalised template/framework.
-
Reported mechanisms to address GPs' and nurses' perceived feeling of lack of responsibility.
- Create a system of permanent follow‐up.
- Raising awareness about obesity associated diseases.
- Emphasise how interventions are part of a broader societal effort to tackle the multiple and complex causes of obesity.
-
Reported mechanisms to improve GPs' and nurses' confidence in patients and treatments:
- Linking weight loss to an upcoming event;
- Seeking wider objective health changes, like blood pressure, to keep patients motivated;
- Having a system of follow up.
- Moderate GPs' and nurses' expectations to seek only modest weight loss or no weight gain.
-
Reported contexts and mechanisms to make discussing weight less interactionally difficult:
- Using computer prompts.
- Routinely recording the patients' BMI.
- Linking the patient's weight to comorbidities and medicalizable conditions.*
- Having a long‐term trusting relationship.
- When there is severe obesity and the issue becomes more doctorable, particularly if bariatric surgery is a treatment option.
- Referring to broader ‘health’ changes rather than ‘weight’ changes.
CONFLICTS OF INTEREST
PA obtained funding from Cambridge Weight Plan for an investigator‐initiated clinical trial. PA spoke at a symposium at the Royal College of General Practitioners of the UK National Conference that was funded by Novo Nordisk. PA and CA did half a day's consultancy for Weight Watchers. None of these activities resulted in personal payments.
ACKNOWLEDGEMENTS
PA is a National Institute for Health Research (NIHR) senior investigator and is funded by the NIHR Oxford Biomedical Research Centre (BRC) Obesity, Diet and Lifestyle Theme and NIHR Applied Research Collaboration (ARC) Oxford and Thames Valley. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. [Correction added on January 20, 2021 after first online publication: The Acknowledgments section was added.]
Warr W, Aveyard P, Albury C, et al. A systematic review and thematic synthesis of qualitative studies exploring GPs' and nurses' perspectives on discussing weight with patients with overweight and obesity in primary care. Obesity Reviews. 2021;22:e13151. 10.1111/obr.13151
REFERENCES
- 1. NICE . Weight management: lifestyle services for overweight or obese adults. https://www.nice.org.uk/guidance/ph53/chapter/1-recommendations. Published 2014. Accessed 4th March 2018.
- 2. Ministry of Health CTRU . Clinical Guidelines for Weight Management in New Zealand Adults. Ministry of Health Wellington; 2017. [Google Scholar]
- 3. Moyer VA. Screening for and management of obesity in adults: US preventive services task force recommendation statement. Ann Intern Med. 2012;157(5):373‐378. [DOI] [PubMed] [Google Scholar]
- 4. Teixeira FV, Pais‐Ribeiro JL, Maia A. A qualitative study of GPs' views towards obesity: are they fighting or giving up? Public Health. 2015;129(3):218‐225. [DOI] [PubMed] [Google Scholar]
- 5. Aveyard P, Lewis A, Tearne S, et al. Screening and brief intervention for obesity in primary care: a parallel, two‐arm, randomised trial. The Lancet. 2016;388(10059):2492‐2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Booth HP, Prevost AT, Gulliford MC. Access to weight reduction interventions for overweight and obese patients in UK primary care: population‐based cohort study. BMJ Open. 2015;5(1):e006642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Digital N. Trends in Consultation Rates in General Practice ‐ 1995–2009. In: 2009.
- 8. Fitzpatrick SL, Stevens VJ. Adult obesity management in primary care, 2008–2013. Prev Med. 2017;99:128‐133. [DOI] [PubMed] [Google Scholar]
- 9. Jackson SE, Wardle J, Johnson F, Finer N, Beeken RJ. The impact of a health professional recommendation on weight loss attempts in overweight and obese British adults: a cross‐sectional analysis. BMJ Open. 2013;3(11):e003693. https://bmjopen.bmj.com/content/bmjopen/3/11/e003693.full.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ogden J, Flanagan Z. Beliefs about the causes and solutions to obesity: a comparison of GPs and lay people. Patient Educ Couns. 2008;71(1):72‐78. [DOI] [PubMed] [Google Scholar]
- 11. Mercer SW, Tessier S. a qualitative study of general practitioners' and practice nurses' attitudes to obesity management in primary care. Health Bull. 2001;59(4):248‐253. [PubMed] [Google Scholar]
- 12. Potter MB, Vu JD, Croughan‐Minihane M. Weight management: what patients want from their primary care physicians. J Fam Pract. 2001;50(6):513‐518. [PubMed] [Google Scholar]
- 13. Teixeira FV, Pais‐Ribeiro JL, Maia AR. Beliefs and practices of healthcare providers regarding obesity: a systematic review. Rev Assoc Med Bras (1992). 2012;58(2):254‐262. [PubMed] [Google Scholar]
- 14. Malterud K, Ulriksen K. Obesity, stigma, and responsibility in health care: a synthesis of qualitative studies. Int J Qual Stud Health Well Being. 2011;6(4):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dewhurst A, Peters S, Devereux‐Fitzgerald A, Hart J. Physicians’ views and experiences of discussing weight management within routine clinical consultations: a thematic synthesis. Patient Educ Couns. 2017;100(5):897‐908. [DOI] [PubMed] [Google Scholar]
- 16. Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health. 2010;33(3):412‐421. [DOI] [PubMed] [Google Scholar]
- 17. Noblit GW, Hare RD, Hare RD. Meta‐ethnography: Synthesizing Qualitative Studies. 11 sage; 1988. [Google Scholar]
- 18. Hannes K, Lockwood C, Pearson A. A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qual Health Res. 2010;20(12):1736‐1743. [DOI] [PubMed] [Google Scholar]
- 19. Sandelowski M, Barroso J. Handbook for Synthesizing Qualitative Research. Springer Publishing Company; 2006. [Google Scholar]
- 20. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Smyth R, NVivo (software) . The SAGE Encyclopedia of Qualitative Research Methods; 2008:564‐566. [Google Scholar]
- 22. Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ. 2006;40(5):405‐414. [DOI] [PubMed] [Google Scholar]
- 23. Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy. 2002;7(4):209‐215. [DOI] [PubMed] [Google Scholar]
- 24. Ribera AP, McKenna J, Riddoch C. Attitudes and practices of physicians and nurses regarding physical activity promotion in the Catalan primary health‐care system. Eur J Public Health. 2005;15(6):569‐575. [DOI] [PubMed] [Google Scholar]
- 25. Lee J‐JM‐L, Tung YC, Tai KP, et al. Do primary care physicians use the 5As in counselling obese patients? A qualitative study. Proc Singapore Healthcare. 2017;26(3):144‐149. [Google Scholar]
- 26. Nolan C, Deehan A, Wylie A, Jones R. Practice nurses and obesity: professional and practice‐based factors affecting role adequacy and role legitimacy. Prim Health Care Res Dev. 2012;13(4):353‐363. [DOI] [PubMed] [Google Scholar]
- 27. Antognoli EL, Seeholzer EL, Gullett H, Jackson B, Smith S, Flocke SA. Primary care resident training for obesity, nutrition, and physical activity counseling: a mixed‐methods study. Health Promot Pract. 2017;18(5):672‐680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ampt AJ, Amoroso C, Harris MF, McKenzie SH, Rose VK, Taggart JR. Attitudes, norms and controls influencing lifestyle risk factor management in general practice. BMC Fam Pract. 2009;10(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ashman F, Sturgiss E, Haesler E. Exploring self‐efficacy in Australian general practitioners managing patient obesity: a qualitative survey study. Int J Family Med. 2016;2016:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gudzune KA, Clark JM, Appel LJ, Bennett WL. Primary care providers’ communication with patients during weight counseling: a focus group study. Patient Educ Couns. 2012;89(1):152‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Huang J, Yu H, Estela M, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79(2):156‐161. https://journals.lww.com/academicmedicine/Fulltext/2004/02000/Physicians__Weight_Loss_Counseling_in_Two_Public.12.aspx [DOI] [PubMed] [Google Scholar]
- 32. Douglas F, van Teijlingen E, Torrance N, Fearn P, Kerr A, Meloni S. Promoting physical activity in primary care settings: health visitors' and practice nurses' views and experiences. J Adv Nurs. 2006;55(2):159‐168. 10.1111/j.1365-2648.2006.03903.x [DOI] [PubMed] [Google Scholar]
- 33. Epstein L, Ogden J. A qualitative study of GPs' views of treating obesity. Br J Gen Pract: J Royal College Gen Practitioners. 2005;55(519):750‐754. [PMC free article] [PubMed] [Google Scholar]
- 34. Forman‐Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Alexander SC, Østbye T, Pollak KI, Gradison M, Bastian LA, Brouwer RJN. Physicians' beliefs about discussing obesity: results from focus groups. Am J Health Promot. 2007;21(6):498‐500. [DOI] [PubMed] [Google Scholar]
- 36. Brown I, Stride C, Psarou A, Brewins L, Thompson J. Management of obesity in primary care: nurses’ practices, beliefs and attitudes. J Adv Nurs. 2007;59(4):329‐341. [DOI] [PubMed] [Google Scholar]
- 37. Leverence RR, Williams RL, Sussman A, Crabtree BF. Obesity counseling and guidelines in primary care: a qualitative study. Am J Prev Med. 2007;32(4):334‐339. [DOI] [PubMed] [Google Scholar]
- 38. Ali HI, Bernsen RM, Baynouna LM. Barriers to weight management among Emirati women: A qualitative investigation of health professionals' perspectives. Int Q Community Health Educ. 2009;29(2):143‐159. 10.2190/iq.29.2.d [DOI] [PubMed] [Google Scholar]
- 39. Jochemsen‐van der Leeuw HGA, van Dijk N, Wieringa‐de Waard M. Attitudes towards obesity treatment in GP training practices: a focus group study. Fam Pract. 2011;28(4):422‐429. 10.1093/fampra/cmq110 [DOI] [PubMed] [Google Scholar]
- 40. Hansson LM, Rasmussen F, Ahlstrom GI. General practitioners' and district nurses' conceptions of the encounter with obese patients in primary health care. BMC Fam Pract. 2011;12:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Heintze C, Sonntag U, Brinck A, et al. A qualitative study on patients’ and physicians’ visions for the future management of overweight or obesity. Fam Pract. 2011;29(1):103‐109. [DOI] [PubMed] [Google Scholar]
- 42. Derksen RE, Brink‐Melis WJ, Westerman MJ, Dam JJMT, Seidell JC, Visscher TLS. A local consensus process making use of focus groups to enhance the implementation of a national integrated health care standard on obesity care. Fam Pract. 2012;29(suppl_1):i177‐i184. [DOI] [PubMed] [Google Scholar]
- 43. Gunther S, Guo F, Sinfield P, Rogers S, Baker R. Barriers and enablers to managing obesity in general practice: a practical approach for use in implementation activities. Qual Prim Care. 2012;20(2):93‐103. [PubMed] [Google Scholar]
- 44. Sonntag U, Brink A, Renneberg B, Braun V, Heintze C. GPs’ attitudes, objectives and barriers in counselling for obesity—a qualitative study. Eur J Gen Pract. 2012;18(1):9‐14. [DOI] [PubMed] [Google Scholar]
- 45. Phillips K, Wood F, Kinnersley P. Tackling obesity: the challenge of obesity management for practice nurses in primary care. Fam Pract. 2014;31(1):51‐59. 10.1093/fampra/cmt054 [DOI] [PubMed] [Google Scholar]
- 46. Claridge R, Gray L, Stubbe M, Macdonald L, Tester R, Dowell AC. General practitioner opinion of weight management interventions in New Zealand. J Prim Health Care. 2014;6(3):212‐220. [PubMed] [Google Scholar]
- 47. Blackburn M, Stathi A, Keogh E, Eccleston C. Raising the topic of weight in general practice: perspectives of GPs and primary care nurses. BMJ Open. 2015;5(8):e008546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kim KK, Yeong L‐L, Caterson ID, Harris MF. Analysis of factors influencing general practitioners’ decision to refer obese patients in Australia: a qualitative study. BMC Fam Pract. 2015;16(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Asselin J, Osunlana AM, Ogunleye AA, Sharma AM, Campbell‐Scherer D. Challenges in interdisciplinary weight management in primary care: lessons learned from the 5As Team study As Team study. Clin Obes. 2016;6(2):124‐132. 10.1111/cob.12133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Glenister KM, Malatzky CA, Wright J. Barriers to effective conversations regarding overweight and obesity in regional Victoria. Aust Fam Physician. 2017;46(10):769‐773. [PubMed] [Google Scholar]
- 51. Brown I, Thompson J. Primary care nurses’ attitudes, beliefs and own body size in relation to obesity management. J Adv Nurs. 2007;60(5):535‐543. [DOI] [PubMed] [Google Scholar]
- 52. Bensing JM, Roter DL, Hulsman RL. Communication patterns of primary care physicians in the United States and the Netherlands. J Gen Intern Med. 2003;18(5):335‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Irving G, Neves AL, Dambha‐Miller H, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7(10):e017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ashman F, Sturgiss E, Haesler E. Exploring self‐efficacy in Australian general practitioners managing patient obesity: A aualitative survey study. Int J Fam Med. 2016;2016:1‐8. 10.1155/2016/8212837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Barnett‐Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Michie S. Talking to primary care patients about weight: a study of GPs and practice nurses in the UK. Psychol Health Med. 2007;12(5):521‐525. [DOI] [PubMed] [Google Scholar]
- 57. Bertrand M, Mullainathan S. Do people mean what they say? Implications for subjective survey data. Am Econ Rev. 2001;91(2):67‐72. [Google Scholar]
- 58. Budd GM, Mariotti M, Graff D, Falkenstein K. Health care professionals' attitudes about obesity: an integrative review. Appl Nurs Res. 2011;24(3):127‐137. [DOI] [PubMed] [Google Scholar]
- 59. Teachman BA, Brownell KD. Implicit anti‐fat bias among health professionals: is anyone immune? Int J Obes (Lond). 2001;25(10):1525‐1531. [DOI] [PubMed] [Google Scholar]
- 60. Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168‐1177. [DOI] [PubMed] [Google Scholar]
- 61. Blackburn M, Stathi A. Moral discourse in general practitioners’ accounts of obesity communication. Soc Sci Med. 2019;230:166‐173. [DOI] [PubMed] [Google Scholar]
- 62. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Conrad P. Learning to doctor: reflections on recent accounts of the medical school years. J Health Soc Behav. 1988;29(4):323‐332. [PubMed] [Google Scholar]
- 64. Mirand AL, Beehler GP, Kuo CL, Mahoney MC. Explaining the de‐prioritization of primary prevention: physicians' perceptions of their role in the delivery of primary care. BMC Public Health. 2003;3(1):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Aasland OG, Røvik JO, Wiers‐Jenssen J. Motives for choice of specialty during and after medical school. Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, Ny Raekke. 2008;128(16):1833‐1837. [PubMed] [Google Scholar]
- 66. Murray E, Treweek S, Pope C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Phillips K, Wood F, Spanou C, Kinnersley P, Simpson SA, Butler CC. Counselling patients about behaviour change: the challenge of talking about diet. Br J Gen Pract: J Royal College Gen Practitioners. 2012;62(594):e13‐e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Gray L, Stubbe M, Macdonald L, Tester R, Hilder J, Dowell AC. A taboo topic? How general practitioners talk about overweight and obesity in New Zealand. J Prim Health Care. 2018;10(2):150‐158. [DOI] [PubMed] [Google Scholar]


