Introduction
Irritability, defined as an increased proneness to anger relative to peers at the same developmental level [1], is linked to depression. In the current review we first distinguish between two types of irritability, namely episodic and chronic irritability. Then, we describe the two types of association between irritability and depression, namely cross-sectional, and longitudinal. Next, we provide possible explanations, propose mechanistic pathways that might explain the link between irritability and depression, and discuss treatment implications of such association. We finalize with future directions to investigate unanswered questions in the link between irritability and depression.
Duration matters: episodic vs chronic irritability
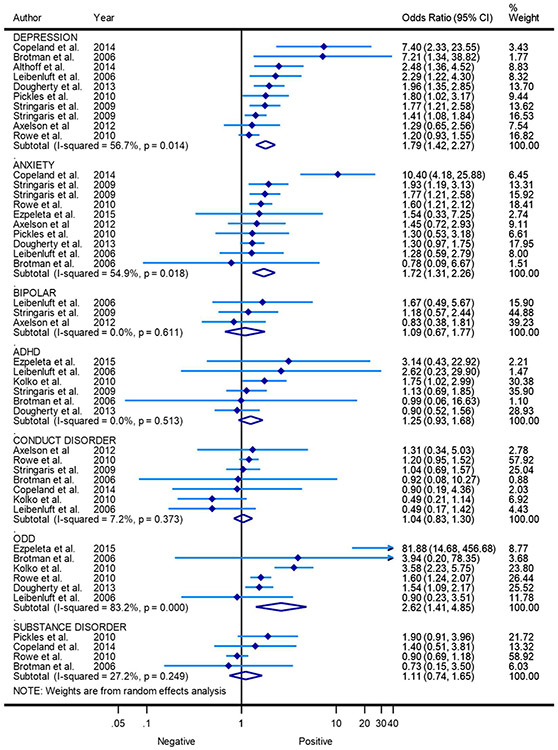
Current psychiatric nosology makes a distinction between chronic and episodic irritability [2] (Figure 1). Chronic irritability is persistent, does not constitute a change from the child’s baseline mood, refers to how the child usually appears and characterizes DMDD, and its precursor, severe mood dysregulation (SMD) [3], in which clinically significant irritability must have been present for at least 12 months. Chronic irritability is also seen in ODD, in which symptoms must have been present for at least 6 months [4]. By contrast, in depression or bipolar disorder (BD), irritability is episodic; it is a distinct change in relation to the child’s baseline mood, analogous to the manic elevation in mood or the depressive decline [4].
Figure 1.
Simplified depiction of types of irritability based on its course over time. Episodic irritability (solid line) constitutes a change from a child’s baseline mood and is present in depression and BD. Chronic irritability (dotted line) is persistent over time and is the hallmark of DMDD and ODD. Although phasic irritability (i.e., temper outbursts) and tonic irritability (i.e., irritable or angry mood between outbursts) have been usually studied in the context of chronic irritability, these also take place in the context of episodic irritability as long as the mood episode lasts.
DSM-5 also distinguishes between tonic and phasic irritability [5]. Tonic irritability refers to persistently angry, grumpy, or grouchy mood, usually lasting days and weeks. Phasic irritability refers to behavioral outbursts of intense anger, manifested by brief or protracted verbal or physical aggression. Irritable or angry mood (i.e., tonic irritability) and severe recurrent temper outbursts (i.e., phasic irritability) occurring frequently over this grumpy mood are the core symptoms of DMDD. However, these irritability components can also be seen during episodes of depression or mania coursing with irritability (Figure 1). We discuss the implications of tonic vs phasic irritability later in this review.
Cross-sectional links between episodic irritability and depression
The study of irritability as part of depression has existed for a long time. For example, anger was considered an important symptom in Burton’s concept of melancholia [6], and for Freud, melancholia involved self-directed hostility originally directed toward others, underlying what he described as “the undoubtedly pleasurable self-torture of melancholy.” [7].
Today, the DSM-5 considers irritability as a cardinal symptom of depression only in children and adolescents, but not in adults[4]. Since irritability is part of a depression episode, it is therefore considered episodic irritability; that is, it should be a change from the patient’s baseline mood noticeable by parents, teachers, or friends. That said, presenting only irritable mood - in contrast to low mood or anhedonia - as a cardinal symptom in pediatric depression seems rare [8].
Longitudinal links between chronic irritability and depression
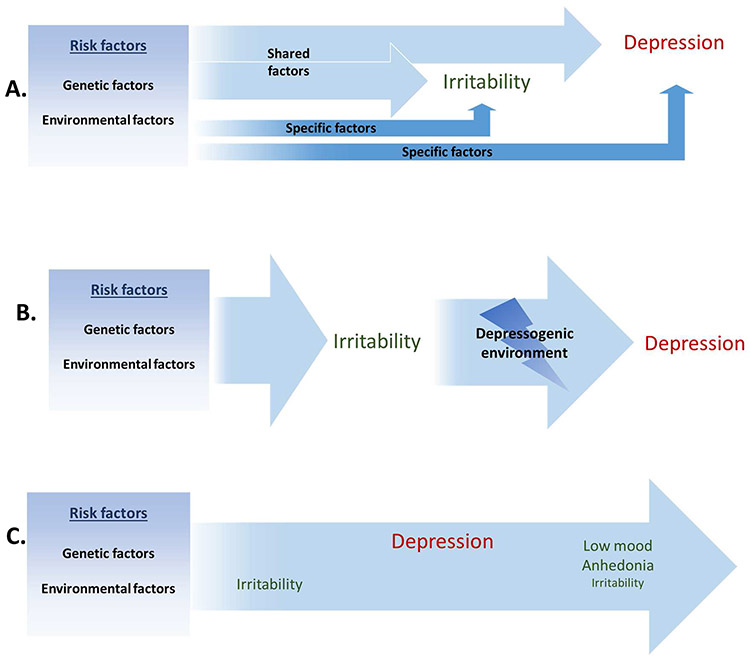
Besides depression, irritability is listed as a cardinal or associated symptom of several behavioral and emotional psychiatric disorders in the DSM-5, particularly in children and adolescents [4]. However, in a recent meta-analysis that included articles in which dimensional or categorical (i.e., DMDD) irritability was a predictor of any future psychiatric outcome, irritability was found to be a significant predictor of depression, anxiety, and ODD, but not of bipolar disorder, conduct disorder, ADHD, or substance abuse [9] (Figure 2). The association between chronic irritability and future depression has been demonstrated using the two main conceptualizations of chronic irritability, named the irritability dimension of ODD and DMDD.
Figure 2.
Forest plot of irritability as a predictor of future psychiatric disorders. Points represent the estimated odds ratio of each study; the lines bisecting the point correspond to the 95% confidence intervals (CI). Pooled effect sizes are represented by diamonds. Weights for each study are given in the right column. ADHD: Attention deficit hyperactivity disorder. ODD: Oppositional defiant disorder.
Adapted from Vidal-Ribas P, Brotman MA, Valdivieso I, et al. The Status of Irritability in Psychiatry: A Conceptual and Quantitative Review. J Am Acad Child Adolesc Psychiatry 2016;55(7):561; with permission.
According to the DSM-5, ODD is characterized by persistent irritable mood, and argumentative and defiant behaviors against authority figures such as parents or teachers (APA, 2013). In previous versions of the DSM, if ODD was accompanied by serious antisocial behaviors and violence, then the diagnosis of CD superseded that of ODD. However, research has shown that ODD is not only a precursor of CD [10], and ADHD [11], but also of emotional disorders such as depression and anxiety [10]. There are at least two distinct symptoms dimensions: irritability/negative affectivity dimension and headstrong/oppositional behavior dimension [12]. Stringaris and Goodman [13] showed that irritability in ODD – defined as touchiness, easy annoyance and anger was a significantly stronger predictor of depression and GAD than of conduct problems, whereas the headstrong dimension of ODD was predictive of ADHD and CD.
These distinct longitudinal associations across ODD dimensions have also been replicated in other samples and countries [14, 15] and by latent class analysis (LCA) [16].
Chronic irritability of the type seen in DMDD has also been associated with the development of depression and other emotional problems [2, 17, 18]. In the Children of the Community study in US, children and adolescents with chronic irritability followed up to late adolescence and young adulthood showed higher odds of developing depression and anxiety 10 and 20 years later, even when considering the presence of depression at baseline [2, 18]. In another prospective population-based study, children and adolescents with DMDD were more likely to suffer from depression and anxiety disorders in young adulthood than those without a psychiatric disorder or those with a psychiatric disorder other than DMDD. However, no differences were found in rates of antisocial behaviors or substance abuse disorders [17]. These findings have been also replicated in young children [19].
Three potential models to explain the link between irritability and depression
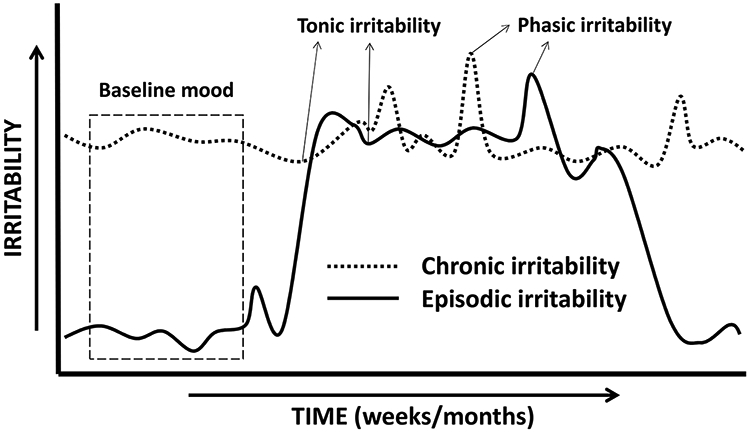
Three plausible models have been suggested to describe the potential mechanisms that explain the association between irritability and depression. The one with the most supportive evidence, discussed in the next section, is that irritability and depression are linked due to shared risk factors. (Figure 3A). Secondly, irritability in youth could cause depression through the environment that it elicits, such as school failure or relationship problems with family and peers (Figure 3B). However, other aspects of ODD such arguing and defying adults, and annoying and blaming peers, thought to be more associated with academic failure and with interpersonal problems within the family and peers [20] are less likely to be associated with depression than the ODD dimension of irritability [13, 14]. Finally, insofar as young children may have difficulties in articulating internalizing symptoms but demonstrate externalizing behaviors when depressed, their caregivers will observe only the latter in their child. Therefore, for some children, it is also possible that irritability may appear to be an early manifestation of depression. (Figure 3C). Although this model does not exclude a shared factor link, more studies and data from multiple informants on irritability and depressive symptoms are needed to support it.
Figure 3.
Potential models to explain the association between irritability and depression. A. Model of shared factors between irritability and depression. B. Model of irritability as a cause of depression. C. Model of irritability as an early manifestation of depression
Shared developmental risks between irritability and depression
The evidence that suggests that the association between irritability and depression is mostly explained by shared risk factors includes studies examining genetic risk, family history of depression, shared temperamental and personality characteristics, and negative parenting styles.
Genetic risk
The stronger evidence for shared risks factors between irritability and depression comes from genetically-informative studies. The association between irritability and depression is mostly explained by shared genetic factors both cross-sectionally [15] and longitudinally [15]. In a sample of adolescent twins followed, on average, for two years, Stringaris et al. [15] found that irritability was genetically associated with future depression more strongly than headstrong/hurtful behaviors were. In contrast, headstrong/hurtful behaviors shared more genetic variance with delinquent behavior at follow-up than with depression. The remaining variance between irritability and depression was explained by non-shared environmental factors. Similar results were found in more recent studies [21, 22]. Interestingly, the impact of irritability on future emotional symptoms seems to be larger than the impact of emotional symptoms on subsequent irritability[21].
It has been suggested that the genetic covariance between irritability and emotional symptoms varies over time and is especially evident from early to middle puberty (ages 13–14). Recent studies have adopted a developmental approach to examine more in depth the genetic covariance of irritability with distinct psychiatric correlates across time, including ADHD and depression. Irritability in children with ADHD, which is often referred to as emotional or mood lability or dysregulation in the literature, is common both in epidemiological and clinical samples [23]. More than 35% of children with ADHD in a population-based study showed marked irritability [24]. Chronic irritability in ADHD is also associated with higher rates of depressive symptoms, cross-sectionally [25] and longitudinally [26], as well as family history of depression [25]. Moreover, as it happens with depression, the overlap between irritability and ADHD is mostly accounted for by shared genetic risks, rather than environmental factors [27]. Using a longitudinal design, a recent study found higher levels of irritability in males than females in childhood, whereas females presented higher irritability than males in adolescence [28]. In addition, irritability with a childhood onset was higher in males and associated with ADHD genetic risk, and higher rates of ADHD and depression. In contrast, irritability with and adolescent onset, was more common in females and associated with genetic risk of both depression and ADHD, and higher rates of depression [29]. These findings suggest that there might be distinct types of irritability (e.g. ADHD-like and depression-like irritability) that could be distinguished if a development perspective is considered.
Family history of depression
Family studies can also be used to examine how phenotypes aggregate across generations which can be suggestive of genetic overlap between distinct phenotypes. It is well known that children with depression are more likely to have parents with a history of depression themselves [30]. Studies examining parents and children suggest that a family history of depression is also associated with irritability in the offspring [31, 32]. In addition, the relation between maternal history of depression and adolescent depression is partly mediated by the presence of irritability in childhood [33]. These findings are also supported by studies examining categorical diagnoses of irritability (DMDD/SMD) in offspring. In one study, parents of youth with narrow BD were more likely to be diagnosed with BD than parents of youth with SMD [34], results that have been replicated also in youth with DMDD [35]. Youth with DMDD, instead, have more parents with a history of depression [36].
Early temperament and personality
Irritability can be viewed as a temperamental or personality characteristic. Indeed, proneness to anger, as we define irritability, is a dimensional trait that can be found in the population [37] and shows to be stable over time [38] ranging from normality to pathology. Anger is thought to develop at around 6 months of age out of a broader emotion of distress [39]. According to the model of emotions by Buss and Plomin [40], anger is considered under the early-temperament of “emotionality”, with the other two being “activity” and “sociability”. Taking this model of temperamental dimensions, Stringaris, Maughan, and Goodman [41] used data from the community-based sample of the Avon Longitudinal Study of Parents and Children (ALSPAC) to examine the relation between early-temperaments of emotionality -characterized by emotion dysregulation- and activity at 38 months, and later psychiatric outcomes at 91 months. The authors found that both temperaments predicted ODD; however, whereas temperamental activity predicted comorbidity between ODD and ADHD, emotionality predicted comorbidity with internalizing psychopathology. This replicated previous studies in which irritable-like temperament was associated with internalizing symptoms [42].
In adults, irritability is subsumed under the higher order personality trait of neuroticism. In a longitudinal twin study, Kendler et al. [43], found a strong relationship between neuroticism and the liability to suffer an episode of major depression. Moreover, close to 55% of the genetic liability to major depression appeared to be shared with neuroticism. The extent to which irritability (as part of neuroticism) may be linked to depression due to such genetic factors remains to be established.
Parenting styles
Early temperaments can also have an impact on parenting styles, and vice versa, leading to the development of irritability [44-46] and depression [42, 47]. Using a longitudinal monozygotic (MZ) twins difference design, Oliver [48] examined the non-shared environmental links between negative parenting behavior, conduct problems and irritability. The author found that the cross-sectional association between negative parenting and irritability explained by non-shared environment in early and late childhood was larger than the association between negative parenting and conduct problems. Most importantly, while irritability in early childhood predicted negative parenting in middle childhood, the latter predicted higher levels of irritability in late childhood. In other words, the association between irritability and negative parenting styles seems to be bidirectional. From other studies, not involving irritability, we also know that negative parenting has also been associated with an increased risk of depression in children [44, 47], with irritable temperament increasing the depressogenic effect of overprotection and lack of emotional warmth [47].
Treatment implications of the link between irritability and depression
The most supported psychological approaches to treat irritability are parent management training (PMT) and cognitive behavioral therapy (CBT). Evidence for the efficacy of these interventions comes from studies focusing on disorders in which irritability is a common symptom, such as ODD or ADHD [49-51]. In the last years, modified psychological therapies have been tested for DMDD. For example, there is encouraging preliminary evidence of efficacy of Dialectical Behavior Therapy (DBT) [52] and Interpersonal Psychotherapy (IPT) [53] against treatment as usual (TAU) in adolescents with DMDD. Of note, IPT is, along CBT, the treatment of choice for adolescent depression [54].
In terms of pharmacological approaches to irritability, until recently, there was only one pharmacological randomized controlled trial with lithium specifically designed for the treatment of severe chronic irritability [55], which emerged within the context of the controversy around paediatric bipolar disorder (BD) [56]. However, this small trial [55] showed that lithium was ineffective for the treatment of chronic severe irritability in children and adolescents. Given the link between irritability and depression, the logical next step was to test whether a serotonin reuptake inhibitor (SRI) would be effective in treating severe chronic irritability in youth.
Evidence derived from adult samples indicates that SRIs might be efficacious in the treatment of irritability in depression [57], as well as in patients with intermittent explosive disorder [58] and those with premenstrual dysphoria [59]. In a systematic review on the effect of antidepressants on irritability in young people, Kim and Boylan [60] identified two uncontrolled studies of SRIs that reported on irritability as an outcome [61, 62]; both studies indicated substantial improvement of irritability with SRI treatment.
Using a double-blind randomized controlled design, we examined the effect of adding citalopram, an SRI, to open-label treatment with stimulant medication, compared to adding placebo, in children with DMDD. The decision of treating first with stimulant medication was based on the high rates of ADHD in clinical samples of children with DMDD [63] as well as the evidence of stimulant on decreased irritability in the context of ADHD [64]. We found that add-on citalopram was effective in reducing irritability compared to placebo, though this was not translated to decreases in functional impairment [65].
It remains to properly test what would be the effect of an antidepressant alone in treating irritability. A case series suggest that atomoxetine, a presynaptic inhibitor of norepinephrine considered a second-line treatment for ADHD when comorbid with emotional disorders, might be effective in reducing irritability in those with DMDD without ADHD [66]. Further research is needed to address the treatment of irritability in children, not only in the context of DMDD but also in its episodic form in the context of depression.
Summary and future research directions
The association between pediatric irritability and depression can be explained by several shared risk factors including genetic and environmental risks. Both conditions are associated with higher rates of family history of depression, specific childhood temperaments and personality styles and, negative parenting styles. However, there are still more paths to be explored to fully elucidate why irritability and depression are linked.
For instance, pathophysiological models conceptualize irritability in two ways, namely, an aberrant response to threat and an aberrant response to reward [1]. In terms of the former, it is hypothesized that youth with severe irritability show attentional bias towards threatening angry faces [67] and are more likely to interpret ambiguous or neutral faces as more threatening [68] Youth with severe irritability also present a generalized deficit in emotion recognition, both in faces [69, 70] and voices [70, 71]. However, these deficits are not specific to irritability; attentional biases towards negative stimuli and deficits in emotion recognition are also evident in people with depression [72-74]. Therefore, emotion processing deficits might represent an increased risk for both irritability and depression. There is some evidence to suggest that deficits in emotion processing in non-referred samples might predict the development of depressive symptomatology [75, 76], and that this could be also the case in youth with chronic severe irritability [70].
In terms of aberrant response to reward, irritability and anger are considered a response to frustration, which occurs when an individual continues to do an action in the expectation of a reward but does not actually receive that reward [77]. Similarly, there is a large body of literature supporting the notion that alterations in reward processing are a central mechanism in the development and maintenance of depression [78, 79]. In a recent neuroimaging meta-analysis, we found that reduced striatal activation was evident in depressed participants during reward feedback and reward anticipation, and the latter was particularly strong in young people [80]. Paradoxically, though, depression is typically associated with low reward approaches [81], whereas irritability is associated with behavioral approach tendencies and the seeking of rewards [82]. That is, both irritability and depression have an impact on the motivation to obtain rewards, though in opposite directions. Therefore, it still unclear how altered reward as seen in irritability is associated with that seen in depression, and even whether both types of reward deficits are related.
Quantitative genetic studies will be needed to test the genetic and environmental contributions to the relationship between irritability, depression, and deficits in emotion and reward processing. We know that irritability and depression [15], as well as depression and reward sensitivity [83], share genetic risk. However, it is unknown whether irritability and reward sensitivity share genetic and/or environmental factors. Similarly, preliminary data suggest genetic correlations between deficits in emotion recognition and irritability [84]. However, to our knowledge, no data from quantitative genetic studies exist that examine associations between emotion processing and depression. Longitudinal twin designs could help us to estimate the direction of effects between irritability, emotion/reward processing deficits, and depression, and the genetic contributions to these effects.
Several studies have examined current and future correlates of irritability; yet few studies have examined early predictors of chronic severe irritability [85]. Early stress is a strong predictor of depression [86], and it has been hypothesized that this is partly caused by the impact that stress has on the neural reward circuit, according to the reward mediation hypothesis [87]. In addition, it has been suggested that aberrant reward processing can generate interpersonal stress in its own right, which in turn would increase the risk of depression, based on the stress generation hypothesis [87, 88]. We have shown that stress can be both, precursor and consequence of aberrant neural response to rewarding stimuli [89]. It would be interesting to test whether early stress also impacts on the development of irritability, perhaps also by altering the reward circuit, and whether irritability can be a generator of interpersonal stress as well. If this was the case, that could be another pathway by which irritability increases the risk of depression.
Finally, further investigation is needed in parsing distinct components of irritability and their correlates. At the beginning of this review, we introduced the reader to tonic (i.e., persistent irritable mood) and phasic irritability (i.e., temper outbursts). Both irritability components have been found to be moderately heritable (54%–61%); yet, only half of the genetic variance of tonic irritability is shared with phasic irritability [90]. This opens the door to investigate whether they also have differential psychopathological correlates, both cross-sectionally and longitudinally. Preliminary unpublished data from a population-based sample of children suggest that irritable mood would be more associated with internalizing disorders like depression and anxiety, whereas temper outbursts would be more linked to externalizing disorders like ADHD and CD.
In conclusion, irritability and depression are closely linked, mostly due to shared genetic variance. Other factors, related to this genetic variance or not, also play a role in this association. However, there is still many gaps that need to be examined to fully understand the links between irritability and depression, and consequently, improve the lives of those children with these emotional problems.
Key points:
Based on its time course and the baseline mood of the child, current psychiatric nosology differentiates between episodic and chronic irritability.
Episodic irritability is cross-sectionally linked to depression as a cardinal symptom in young people, but the manifestation of irritability alone is rare.
Chronic irritability is longitudinally linked to depression rather than other disorders such as BD, ADHD or CD.
The association between irritability and depression can be explained by shared genetic and environmental risk factors, including higher rates of family history of depression, specific childhood temperaments and personality styles, and negative parenting styles.
Synopsis:
Based on its course over time, irritability is linked to depression cross-sectionally and longitudinally. Cross-sectionally, irritability takes an episodic form as a symptom in pediatric depression; yet, the manifestation of irritability in the absence of depressed mood or anhedonia is rare. Longitudinally, chronic irritability has been shown to predict depression rather than bipolar disorder or externalizing disorders. Evidence suggest that the link between irritability and depression is mostly explained by shared genetic risk. Both conditions are also associated with higher rates of family history of depression, specific childhood temperaments and personality styles, and negative parenting styles. The treatment implications of this association are discussed. Future research should examine the roles played by emotion and reward processing, early stress exposures, and phasic vs tonic irritability in the links between irritability and depression.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure statement:
The Authors have nothing to disclose.
References
- 1.Brotman MA, et al. , Irritability in Youths: A Translational Model. Am J Psychiatry, 2017: p. appiajp201616070839. [DOI] [PubMed] [Google Scholar]
- 2.Leibenluft E, et al. , Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol, 2006. 16(4): p. 456–66. [DOI] [PubMed] [Google Scholar]
- 3.Leibenluft E, et al. , Defining clinical phenotypes of juvenile mania. Am J Psychiatry, 2003. 160(3): p. 430–7. [DOI] [PubMed] [Google Scholar]
- 4.APA, Diagnostic and Statistical Manual of Mental Disorders (5th ed.). 5th ed. 2013, Washington, DC. [Google Scholar]
- 5.Avenevoli S, Blader JC, and Leibenluft E, Irritability in Youth: An Update. J Am Acad Child Adolesc Psychiatry, 2015. 54(11): p. 881–3. [DOI] [PubMed] [Google Scholar]
- 6.Burton R, The anatomy of melancholy. 1857, London: JW Moore. [Google Scholar]
- 7.Freud S, Trauer und Melancholie. 1915, Frankfurt a.m.: Fischer Taschenbuch Verlag. [Google Scholar]
- 8.Stringaris A, et al. , Irritable mood as a symptom of depression in youth: prevalence, developmental, and clinical correlates in the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry, 2013. 52(8): p. 831–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vidal-Ribas P, et al. , The Status of Irritability in Psychiatry: A Conceptual and Quantitative Review. J Am Acad Child Adolesc Psychiatry, 2016. 55(7): p. 556–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burke JD, et al. , Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry, 2005. 46(11): p. 1200–10. [DOI] [PubMed] [Google Scholar]
- 11.Angold A, Costello EJ, and Erkanli A, Comorbidity. J Child Psychol Psychiatry, 1999. 40(1): p. 57–87. [PubMed] [Google Scholar]
- 12.Stringaris A and Goodman R, Three dimensions of oppositionality in youth. J Child Psychol Psychiatry, 2009. 50(3): p. 216–23. [DOI] [PubMed] [Google Scholar]
- 13.Stringaris A and Goodman R, Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry, 2009. 48(4): p. 404–12. [DOI] [PubMed] [Google Scholar]
- 14.Burke JD, An affective dimension within oppositional defiant disorder symptoms among boys: personality and psychopathology outcomes into early adulthood. J Child Psychol Psychiatry, 2012. 53(11): p. 1176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stringaris A, et al. , Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry, 2012. 169(1): p. 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Althoff RR, et al. , Classes of oppositional-defiant behavior: concurrent and predictive validity. J Child Psychol Psychiatry, 2014. 55(10): p. 1162–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Copeland WE, et al. , Adult diagnostic and functional outcomes of DSM-5 disruptive mood dysregulation disorder. Am J Psychiatry, 2014. 171(6): p. 668–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stringaris A, et al. , Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry, 2009. 166(9): p. 1048–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dougherty LR, et al. , Preschool irritability: longitudinal associations with psychiatric disorders at age 6 and parental psychopathology. J Am Acad Child Adolesc Psychiatry, 2013. 52(12): p. 1304–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greene RW, et al. , Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am J Psychiatry, 2002. 159(7): p. 1214–24. [DOI] [PubMed] [Google Scholar]
- 21.Savage J, et al. , A genetically informed study of the longitudinal relation between irritability and anxious/depressed symptoms. J Am Acad Child Adolesc Psychiatry, 2015. 54(5): p. 377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mikolajewski AJ, Taylor J, and Iacono WG, Oppositional defiant disorder dimensions: genetic influences and risk for later psychopathology. J Child Psychol Psychiatry, 2017. 58(6): p. 702–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaw P, et al. , Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry, 2014. 171(3): p. 276–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stringaris A and Goodman R, Mood lability and psychopathology in youth. Psychol Med, 2009. 39(8): p. 1237–45. [DOI] [PubMed] [Google Scholar]
- 25.Eyre O, et al. , Irritability in ADHD: Associations with depression liability. J Affect Disord, 2017. 215: p. 281–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eyre O, et al. , Irritability in ADHD: association with later depression symptoms. Eur Child Adolesc Psychiatry, 2019. 28(10): p. 1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Merwood A, et al. , Genetic associations between the symptoms of attention-deficit/hyperactivity disorder and emotional lability in child and adolescent twins. J Am Acad Child Adolesc Psychiatry, 2014. 53(2): p. 209–220 e4. [DOI] [PubMed] [Google Scholar]
- 28.Riglin L, et al. , Investigating the genetic underpinnings of early-life irritability. Transl Psychiatry, 2017. 7(9): p. e1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riglin L, et al. , Identifying Novel Types of Irritability Using a Developmental Genetic Approach. Am J Psychiatry, 2019. 176(8): p. 635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klein DN, et al. , Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychol Med, 2005. 35(3): p. 353–65. [DOI] [PubMed] [Google Scholar]
- 31.Krieger FV, et al. , Dimensions of oppositionality in a Brazilian community sample: testing the DSM-5 proposal and etiological links. J Am Acad Child Adolesc Psychiatry, 2013. 52(4): p. 389–400 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiggins JL, et al. , Developmental trajectories of irritability and bidirectional associations with maternal depression. J Am Acad Child Adolesc Psychiatry, 2014. 53(11): p. 1191–205, 1205 e1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whelan YM, et al. , Pathways from maternal depressive symptoms to adolescent depressive symptoms: the unique contribution of irritability symptoms. J Child Psychol Psychiatry, 2015. 56(10): p. 1092–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brotman MA, et al. , Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry, 2007. 164(8): p. 1238–1241. [DOI] [PubMed] [Google Scholar]
- 35.Fristad MA, et al. , Disruptive Mood Dysregulation Disorder and Bipolar Disorder Not Otherwise Specified: Fraternal or Identical Twins? J Child Adolesc Psychopharmacol, 2016. 26(2): p. 138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Propper L, et al. , Disruptive mood dysregulation disorder in offspring of parents with depression and bipolar disorder. The British Journal of Psychiatry, 2017. [DOI] [PubMed] [Google Scholar]
- 37.Copeland WE, Brotman MA, and Costello EJ, Normative Irritability in Youth: Developmental Findings From the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry, 2015. 54(8): p. 635–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caprara GV, et al. , Individual differences conducive to aggression and violence: trajectories and correlates of irritability and hostile rumination through adolescence. Aggress Behav, 2007. 33(4): p. 359–74. [DOI] [PubMed] [Google Scholar]
- 39.Katharine MBB, Emotional Development in Early Infancy. Child Development, 1932. 3(4): p. 324–341. [Google Scholar]
- 40.Buss AH and Plomin R, Temperament: Early developing personality traits. 1984, Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- 41.Stringaris A, Maughan B, and Goodman R, What's in a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: findings from the Avon longitudinal study. J Am Acad Child Adolesc Psychiatry, 2010. 49(5): p. 474–83. [DOI] [PubMed] [Google Scholar]
- 42.Kiff CJ, Lengua LJ, and Bush NR, Temperament variation in sensitivity to parenting: predicting changes in depression and anxiety. J Abnorm Child Psychol, 2011. 39(8): p. 1199–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kendler KS, et al. , A longitudinal twin study of personality and major depression in women. Arch Gen Psychiatry, 1993. 50(11): p. 853–62. [DOI] [PubMed] [Google Scholar]
- 44.Kiff CJ, Lengua LJ, and Zalewski M, Nature and nurturing: parenting in the context of child temperament. Clin Child Fam Psychol Rev, 2011. 14(3): p. 251–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lengua LJ and Kovacs EA, Bidirectional associations between temperament and parenting and the prediction of adjustment problems in middle childhood. Journal of Applied Developmental Psychology, 2005. 26(1): p. 21–38. [Google Scholar]
- 46.Lipscomb ST, et al. , Trajectories of parenting and child negative emotionality during infancy and toddlerhood: a longitudinal analysis. Child development, 2011. 82(5): p. 1661–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oldehinkel AJ, et al. , Temperament, parenting, and depressive symptoms in a population sample of preadolescents. J Child Psychol Psychiatry, 2006. 47(7): p. 684–95. [DOI] [PubMed] [Google Scholar]
- 48.Oliver BR, Unpacking externalising problems: negative parenting associations for conduct problems and irritability. BJPsych Open, 2015. 1(1): p. 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barkley RA, Taking charge of ADHD: The complete, authoritative guide for parents. 2013, New York, NY: Guildford press. [Google Scholar]
- 50.Comer JS, et al. , Psychosocial treatment efficacy for disruptive behavior problems in very young children: a meta-analytic examination. J Am Acad Child Adolesc Psychiatry, 2013. 52(1): p. 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sukhodolsky DG and Scahill L, Cognitive-Behavioral Therapy for Anger and Aggression in Children. 2012, New York, NY: Guildford press. [Google Scholar]
- 52.Perepletchikova F, et al. , Randomized Clinical Trial of Dialectical Behavior Therapy for Preadolescent Children With Disruptive Mood Dysregulation Disorder: Feasibility and Outcomes. J Am Acad Child Adolesc Psychiatry, 2017. 56(10): p. 832–840. [DOI] [PubMed] [Google Scholar]
- 53.Miller L, et al. , Interpersonal psychotherapy for mood and behavior dysregulation: Pilot randomized trial. Depress Anxiety, 2018. 35(6): p. 574–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhou X, et al. , Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: A systematic review and network meta-analysis. World psychiatry : official journal of the World Psychiatric Association (WPA), 2015. 14(2): p. 207–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dickstein DP, et al. , Randomized double-blind placebo-controlled trial of lithium in youths with severe mood dysregulation. J Child Adolesc Psychopharmacol, 2009. 19(1): p. 61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wozniak J, et al. , Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry, 1995. 34(7): p. 867–76. [DOI] [PubMed] [Google Scholar]
- 57.Fava M and Rosenbaum JF, Anger attacks in patients with depression. Journal of clinical psychiatry, 1999. 60(15): p. 21–4. [PubMed] [Google Scholar]
- 58.Coccaro EF, Lee RJ, and Kavoussi RJ, A double-blind, randomized, placebo-controlled trial of fluoxetine in patients with intermittent explosive disorder. J Clin Psychiatry, 2009. 70(5): p. 653–662. [DOI] [PubMed] [Google Scholar]
- 59.Dimmock PW, et al. , Efficacy of selective serotonin-reuptake inhibitors in premenstrual syndrome: a systematic review. The Lancet, 2000. 356(9236): p. 1131–1136. [DOI] [PubMed] [Google Scholar]
- 60.Kim S and Boylan K, Effectiveness of Antidepressant Medications for Symptoms of Irritability and Disruptive Behaviors in Children and Adolescents. J Child Adolesc Psychopharmacol, 2016. 26(8): p. 694–704. [DOI] [PubMed] [Google Scholar]
- 61.Garland EJ and Weiss M, Case study: obsessive difficult temperament and its response to serotonergic medication. J Am Acad Child Adolesc Psychiatry, 1996. 35(7): p. 916–20. [DOI] [PubMed] [Google Scholar]
- 62.Armenteros JL and Lewis JE, Citalopram treatment for impulsive aggression in children and adolescents: an open pilot study. J Am Acad Child Adolesc Psychiatry, 2002. 41(5): p. 522–9. [DOI] [PubMed] [Google Scholar]
- 63.Deveney CM, et al. , A prospective study of severe irritability in youths: 2- and 4-year follow-up. Depress Anxiety, 2015. 32(5): p. 364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fernandez de la Cruz L, et al. , Treatment of children with attention-deficit/hyperactivity disorder (ADHD) and irritability: results from the multimodal treatment study of children with ADHD (MTA). J Am Acad Child Adolesc Psychiatry, 2015. 54(1): p. 62–70 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Towbin K, et al. , A Double-Blind Randomized Placebo-Controlled Trial of Citalopram Adjunctive to Stimulant Medication in Youth With Chronic Severe Irritability. J Am Acad Child Adolesc Psychiatry, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Benarous X, et al. , Effective use of atomoxetine to treat six inpatient youths with disruptive mood dysregulation disorder without attention deficit disorder. CNS Spectr, 2019: p. 1–3. [DOI] [PubMed] [Google Scholar]
- 67.Hommer RE, et al. , Attention bias to threat faces in severe mood dysregulation. Depress Anxiety, 2014. 31(7): p. 559–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brotman MA, et al. , Amygdala activation during emotion processing of neutral faces in children with severe mood dysregulation versus ADHD or bipolar disorder. Am J Psychiatry, 2010. 167(1): p. 61–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rich BA, et al. , Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Dev Psychopathol, 2008. 20(2): p. 529–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vidal-Ribas P, et al. , Deficits in emotion recognition are associated with depressive symptoms in youth with disruptive mood dysregulation disorder. Depress Anxiety, 2018. 35(12): p. 1207–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Deveney CM, et al. , Affective prosody labeling in youths with bipolar disorder or severe mood dysregulation. J Child Psychol Psychiatry, 2012. 53(3): p. 262–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Peckham AD, McHugh RK, and Otto MW, A meta-analysis of the magnitude of biased attention in depression. Depress Anxiety, 2010. 27(12): p. 1135–42. [DOI] [PubMed] [Google Scholar]
- 73.Dalili MN, et al. , Meta-analysis of emotion recognition deficits in major depressive disorder. Psychol Med, 2015. 45(6): p. 1135–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Naranjo C, et al. , Major depression is associated with impaired processing of emotion in music as well as in facial and vocal stimuli. J Affect Disord, 2011. 128(3): p. 243–51. [DOI] [PubMed] [Google Scholar]
- 75.Beevers CG and Carver CS, Attentional bias and mood persistence as prospective predictors of dysphoria. Cognitive Therapy and Research, 2003. 27(6): p. 619–637. [Google Scholar]
- 76.Vrijen C, Hartman CA, and Oldehinkel AJ, Slow identification of facial happiness in early adolescence predicts onset of depression during 8 years of follow-up. Eur Child Adolesc Psychiatry, 2016. 25(11): p. 1255–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Berkowitz L, Frustration-aggression hypothesis: examination and reformulation. Psychol Bull, 1989. 106(1): p. 59. [DOI] [PubMed] [Google Scholar]
- 78.Admon R and Pizzagalli DA, Dysfunctional Reward Processing in Depression. Curr Opin Psychol, 2015. 4: p. 114–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Forbes EE and Dahl RE, Research Review: altered reward function in adolescent depression: what, when and how? J Child Psychol Psychiatry, 2012. 53(1): p. 3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Keren H, et al. , Reward Processing in Depression: A Conceptual and Meta-Analytic Review Across fMRI and EEG Studies. Am J Psychiatry, 2018. 175(11): p. 1111–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Treadway MT and Zald DH, Reconsidering anhedonia in depression: lessons from translational neuroscience. Neuroscience & Biobehavioral Reviews, 2011. 35(3): p. 537–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Carver CS and Harmon-Jones E, Anger is an approach-related affect: evidence and implications. Psychol Bull, 2009. 135(2): p. 183. [DOI] [PubMed] [Google Scholar]
- 83.Bogdan R and Pizzagalli DA, The heritability of hedonic capacity and perceived stress: a twin study evaluation of candidate depressive phenotypes. Psychol Med, 2009. 39(2): p. 211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rappaport LM, et al. , A Population-Based Twin Study of Childhood Irritability and Internalizing Syndromes. J Clin Child Adolesc Psychol, 2018: p. 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Munhoz TN, et al. , Perinatal and postnatal risk factors for disruptive mood dysregulation disorder at age 11: 2004 Pelotas Birth Cohort Study. J Affect Disord, 2017. 215: p. 263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pizzagalli DA, Depression, Stress, and Anhedonia: Toward a Synthesis and Integrated Model. 2014. 10(1): p. 393–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Auerbach RP, Admon R, and Pizzagalli DA, Adolescent depression: stress and reward dysfunction. Harv Rev Psychiatry, 2014. 22(3): p. 139–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hammen C, Generation of stress in the course of unipolar depression. J Abnorm Psychol, 1991. 100(4): p. 555–61. [DOI] [PubMed] [Google Scholar]
- 89.Vidal-Ribas P, et al. , Bidirectional Associations Between Stress and Reward Processing in Children and Adolescents: A Longitudinal Neuroimaging Study. Biol Psychiatry Cogn Neurosci Neuroimaging, 2019. 4(10): p. 893–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Moore AA, et al. , Heritability, stability, and prevalence of tonic and phasic irritability as indicators of disruptive mood dysregulation disorder. 2019. 60(9): p. 1032–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]