Abstract
In this study, we aimed to determine the prevalence and factors associated with overweight and obesity among nonpregnant and nonlactating (NPNL) women of reproductive age with iron deficiency anaemia (IDA) in urban Bangladesh. We obtained data from the baseline assessment of a randomized control trial conducted among 525 women of reproductive age (18–49 years) with IDA (Hb < 12 gdl−1 and serum ferritin <30 μg L−1). The study was carried out in Mirpur, Dhaka, Bangladesh, between December 2017 and January 2019. We collected information on women's socio‐demographic characteristics and anthropometry. Body mass index (BMI) was calculated using the following formula: weight in kilograms per height in square metres. BMI ≥ 25–29.9 kg m−2 was considered as overweight, whereas BMI ≥ 30 kg m−2 as obese. A multivariable logistic regression model was used to ascertain the risk factors of overweight and obesity. The prevalence of overweight and obesity was 29.9% (95% CI: 26.0–34.0) and 13.1% (95% CI: 10.4–16.3), respectively. The combined prevalence of overweight and obesity was 43.0% (95% CI: 38.7–47.4). The multivariable analysis showed married women (aOR: 4.4; CI: 1.8–11.1), women aged 30–49 years (aOR: 7.6; CI: 2.4–24.1), unemployed women (aOR 1.5; CI: 1.0–2.4) and women from the wealthier households (aOR 3.9; CI: 2.3–6.8) had the highest risk of being overweight and obese compared with their counterparts. Both age and household wealth statuses showed dose–response relationships. Combination of overweight and obesity with IDA poses a particular challenge for public health interventions. The policymakers should consider what new interventions and policy initiatives are needed to address this combination of overweight and obesity with IDA.
Keywords: Bangladesh, iron deficiency anaemia, obesity, overweight, urban area, women of reproductive age
Key Messages.
The prevalence of overweight and obesity among women of reproductive age with iron deficiency anaemia (IDA) was 43.0% (95% CI: 38.7–47.4).
Combination of overweight and obesity with IDA poses a particular challenge for public health interventions.
Policymakers need to understand what new interventions and policy initiatives are needed to address the combination of overweight and obesity with IDA.
1. INTRODUCTION
Mounting national incomes along with significant alteration in food habits and physical activity are resulting in an accelerating prevalence of overweight and obesity across the globe (Bhurosy & Jeewon, 2014; Harding, Aguayo, & Webb, 2019). In recent years, most developing countries are experiencing a nutrition transition during the process of socio‐economic developments (Popkin, 1994). Persistent high burden of undernutrition along with the increasing prevalence of overweight and obesity is creating another type of public health challenge for the developing countries: “the double burden of malnutrition” (Abdullah, 2015). Countries with a high prevalence of undernutrition today and high projected growth in overweight and obesity could suffer a considerable epidemic of noncommunicable diseases over the next 30 years (Schmidhuber & Shetty, 2005).
Overweight and obesity pose special health risks for women of reproductive age. It not only increases the risk of gestational diabetes, Type 2 diabetes, preeclampsia, premature labour, caesarean delivery and cardiovascular disease (Cnattingius et al., 2013; Leddy, Power, & Schulkin, 2008; Thrift & Callaway, 2014) but also increases the likelihood of adverse perinatal, neonatal, infant and child health outcomes (Catalano et al., 2012). Similarly, women of reproductive age suffering from iron deficiency anaemia (IDA) had a higher risk of miscarriage, preterm labour, abruption placenta and low birth weight (Kamruzzaman, Rabbani, Saw, Sayem, & Hossain, 2015; Rasmussen, 2001; Scholl, Hediger, Fischer, & Shearer, 1992). Evidence suggests that overweight and obesity increase the risk of IDA (Zhao et al., 2015). Because of the interrelationships between overweight and obesity with IDA, globally the research interests are diverting towards the examination of coexistence of overweight and obesity with IDA (Chang et al., 2014; Jones et al., 2016; Rhodes et al., 2020; Wirth et al., 2017).
Over the last two decades, Bangladesh is observing an alarming rise in the prevalence of overweight and obesity among women of reproductive age (Balarajan & Villamor, 2009; Biswas, Uddin, Al Mamun, Pervin, & Garnett, 2017; Tanwi, Chakrabarty, & Hasanuzzaman, 2019). Secondary analysis of Bangladesh Demographic and Health Survey (BDHS) Data 2014 showed that around 34% women of reproductive age in urban Bangladesh were overweight and obese (Tanwi, Chakrabarty, Hasanuzzaman, Saltmarsh, & Winn, 2019). On the other hand, the prevalence of anaemia among nonpregnant ever‐married women living in urban areas was 37.2%. According to Bangladesh National Micronutrient Survey 2011, around 7% of nonpregnant and nonlactating (NPNL) women of reproductive age suffered from IDA (International Centre for Diarrheal Disease Research Bangladesh, icddr,b, 2013; Mamun & Mascie‐Taylor, 2019). Although several studies in this context already examined the prevalence and correlates of overweight and obesity and anaemia among women of reproductive age independently, none of the studies examined the coexistence of overweight and obesity with IDA.
Our study aimed to determine the prevalence and factors associated with overweight and obesity among NPNL women of reproductive age with IDA. Coexistence of overweight and obesity among women of reproductive age with IDA poses a particular challenge for public health interventions. Finding from this study will help policymakers design context‐specific solutions targeting population having a combination of overweight and obesity with IDA.
2. METHODS
2.1. Parent trial and sample size
A community based double‐blind, randomized control study was conducted among women of reproductive age (18–49 years) with IDA in Mirpur Dhaka, Bangladesh. The objective of the study was to test the efficacy and appropriate dose of bovine lactoferrin for correction and prevention of IDA among NPNL women of reproductive age. As part of the study, screening for anaemia was done in the community. We screened 3722 NPNL women of reproductive age for IDA. The prevalence of IDA was 19.1% (n = 710). We enrolled women who were aged between 18 and 49 years, were NPNL at the time of enrolment, had serum haemoglobin between 7 and 12 g dl−1, serum ferritin level below 30 μg L−1 and provided informed consent for participation in the trial. A total of 555 women with IDA were enrolled in the study. A baseline assessment of socio‐economic status and anthropometric measurements was done. We included 525 women in the analysis of this paper who participated in the baseline assessments (30 participants did not participate in baseline assessment after enrolment).
2.2. Study site
We conducted the study in the Mirpur area of Dhaka, the capital city of Bangladesh (Figure 1). Mirpur is one of the 42 thanas of Dhaka City with a population of about 1 million in an area of 39 km2. The area is densely populated and divided into 16 sections/wards for administrative purposes. Mirpur has both slum and nonslum areas. The majority of the population belongs to low socio‐economic conditions. The average income of the slum areas of Mirpur was Tk 4,200 (about USD 55) per month per family.
FIGURE 1.
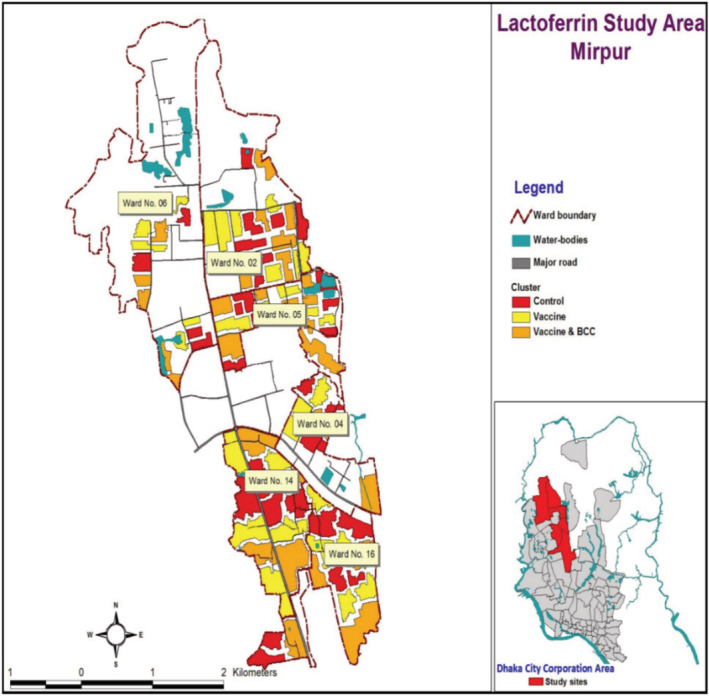
Study area map
2.2.1. Data collection and quality assurance measures
Baseline data collection was done between March 2018 and September 2018. We used CommCare for data collection. Commcare is a tab‐based data collection system with range checks and skips options inbuilt to minimize error during data collection. The tab‐based system also enabled us to monitor data quality in real time. We recruited data collectors who had prior experience in survey data collection and anthropometric measurements. Data collectors received 10‐day in‐house training by expert trainers, including 2‐days field practice. An expert nurse collected the blood samples under supervision of a study physician. All the biomarker assessments were done in icddr,b lab following standard procedures for biomarker analysis. icddr,b lab has ISO certification (ISO 15189:2012 and ISO 15190:2003).
2.3. Socio‐economic characteristics
We collected socio‐economic information using a structured questionnaire adopted from the BDHS 2014(National Institute of Population Research and Training (Bangladesh), Mitra and Associates (Firm), & MEASURE DHS (Program), 2019). In order to understand the respondent background, information regarding age of the respondent, marital status, parity, educational attainment and current employment status were explored. For household characteristics, we examined the household size and household wealth status (Chowdhury, Adnan, & Hassan, 2018). We used principle component analysis (PCA) to generate household wealth indexes using variables types of dwelling, source of drinking water, access to sanitary latrine, household's ownership of land, domestics animals, transports (autobike, rickshaw, van, bicycle, motorcycle, scooter, tempo and CN0) and 14‐item household affects. Household wealth indexes were classified into three (low, medium and high) (Islam et al., 2018; Kamruzzaman et al., 2015).
2.4. Anthropometry
Anthropometric information was collected using standard tools following the WHO guideline. We used stadiometer with a precision level of 0.1 cm for height measurement. We measured the weight of our study participants using a digital bathroom scale (Tanita) with a precision level of 0.1 lb/50 g. We also assessed the mid‐upper arm circumference using a MUAC tape. All the scales were calibrated daily before data collection. Body mass index (BMI) was calculated using formula (weight [kg]/height [m2]; BMI ≥ 25–29.9 kg m−2 was classified as overweight, whereas BMI ≥ 30 kg m−2 was defined as obesity. Participants having BMI ≤ 18.5 kg m−2 were defined as underweight).
2.5. Haemoglobin and iron status
We measured serum haemoglobin and serum ferritin of all our participants. The study nurse collected 5 ml of blood at the field clinic by study nurse following aseptic precautions. One millilitre of blood was stored in EDTA tube, and the rest of the 4 ml was centrifuged for aliquots formation. All samples were then transferred to icddr,b lab for testing of serum haemoglobin and serum ferritin. Participants who had serum haemoglobin <12 g dl−1 and serum ferritin level <30 μg L−1 were classified as IDA.
2.6. Ethical approval
The study was approved by the Institutional Review Boards (IRBs) and Independent Ethics Committees (IECs) in Bangladesh and Australia.
2.7. Informed consents
We took written informed consents from the study participants before the screening and during enrolment into the study. During the consent process, trained data collectors read out the consent form in the local language (Bangla). They explained the purpose of the study, voluntary nature of participation, possible risk, benefits and use of information to the participants before obtaining signature/thumb impression (for illiterate participants).
2.8. Data analysis
Our primary outcome of interest was the prevalence and factors associated with overweight and obesity among women of reproductive age (18–49 years) with IDA. For the descriptive statistics, we reported the mean and standard deviations for continuous variables and proportions with 95% confidence intervals for categorical variables. We did multivariable logistic regression to understand the factors associated with overweight and obesity among women of reproductive age with IDA. We selected the explanatory variables based on prior literature review. Variables found to have significant associations in bivariate analysis were included in the multivariable logistics regression model in a stepwise fashion. During the modelling exercise, we tested possible interactions among explanatory variables using interaction terms in multivariable logistics regression. We found no significant interaction effect among the possible explanatory variables. All analysis was done using STATA 14.
3. RESULTS
3.1. Socio‐demographic and socio‐economic characteristics of study participants
About two thirds of the study participants were aged between 30 and 49 years. Eighty‐seven percent of the women were married. One in 10 married women had no children. Around one third of women did not receive any formal schooling. More than two thirds of women were unemployed at the time of the survey. The average household size was 4.3. Households were equally distributed across three wealth indexes (low, medium and high) (Table 1).
TABLE 1.
Socio‐demographic characteristics of nonpregnant and nonlactating (NPNL) women of reproductive age (18–49 years) with iron deficiency anaemia (IDA) in Mirpur, Dhaka, Bangladesh, 2018
| Background characteristics | n = 525 | Percentage (%) |
|---|---|---|
| Women's characteristics | ||
| Age in years | ||
| 18–19 | 54 | 10.3 |
| 20–29 | 157 | 29.9 |
| 30–49 | 336 | 60.5 |
| Marital status | ||
| Unmarried | 69 | 13.1 |
| Married | 456 | 86.9 |
| Parity (n = 456) | ||
| None | 51 | 11.2 |
| 1 or more children | 405 | 88.8 |
| Women's education | ||
| No schooling | 155 | 29.5 |
| Primary (1–5 years) | 153 | 29.1 |
| Secondary and higher (+6 years) | 217 | 41.3 |
| Women's employment | ||
| Unemployed | 336 | 64.0 |
| Employed | 189 | 36.0 |
| Household characteristics | ||
| Household wealth index | ||
| Low | 175 | 33.3 |
| Medium | 175 | 33.3 |
| High | 175 | 33.3 |
| Household size | ||
| Mean household size | 525 | 4.3 |
| 1–4 persons | 308 | 58.7 |
| ≥5 persons | 217 | 41.3 |
3.2. Prevalence of overweight and obesity
The prevalence of overweight and obesity was 29.9% (95% CI: 26.0–34.0) and 13.1% (95% CI: 10.4–16.3), respectively, among our study participants (Table 2). The combined prevalence of overweight and obesity was 43.0% (95% CI: 38.7–47.4).
TABLE 2.
Nutritional characteristics of NPNL women of reproductive age (18–49 years) with IDA in Mirpur, Dhaka, Bangladesh, 2018
| Underweight (BMI ≤ 18.4 kg m−2) n = 58 | Normal weight (BMI 18.5–24.9 kg m−2) n = 241 | Overweight (BMI 25–29.9 kg m−2) n = 157 | Obesity (BMI ≥ 30 kg m−2) n = 69 | |
|---|---|---|---|---|
| Prevalence's (% with 95% CI) | 11.0 (8.5–14.0) | 45.9(41.6–50.3) | 29.9 (26.0–34.0) | 13.1(10.4–16.3) |
| Anthropometric measurement (mean ± sd) | ||||
| Height in cm | 150.9 ± 6.3 | 150.0 ± 5.9 | 149.9 ± 5.9 | 149.7 ± 7.1 |
| Weight in kg | 38.9 ± 4.2 | 48.8 ± 5.1 | 61.6 ± 5.6 | 73.8 ± 7.5 |
| MUAC in cm | 22.2 ± 1.7 | 26.1 ± 2.0 | 30.1 ± 3.2 | 33.5 ± 2.7 |
| BMI in kg m−2 | 17.0 ± 1.1 | 21.7 ± 1.8 | 27.4 ± 1.5 | 32.9 ± 2.9 |
| Biomarkers of IDA (mean ± sd) a | ||||
| Haemoglobin in g dl−1 | 11.2 ± 1.5 | 11.2 ± 1.3 | 11.4 ± 1.3 | 11.4 ± 1.3 |
| Serum ferritin in μg L−1 | 26.7 ± 22.6 | 24.9 ± 19.5 | 23.7 ± 15.7 | 27.1 ± 26.5 |
Anaemia is defined as serum haemoglobin concentration <12 g dl−1; iron deficiency is defined as serum ferritin concentration <30 μg L−1.
Abbreviations: BMI, body mass index; IDA, iron deficiency anaemia; NPNL, nonpregnant and nonlactating.
3.3. Prevalence of overweight and obesity by socio‐economic factors
Table 3 shows the prevalence of overweight and obesity among NPNL women of reproductive age with IDA by socio‐economic categories. The prevalence of overweight and obesity was more than 50% among women above 30 years of age compared to the younger women. Around half of the married women were overweight or obese. The prevalence of overweight and obesity was higher among women who accomplished secondary or higher level education compared to the women with no education. The burden of overweight and obesity increased with increasing wealth status of the households (25% in low wealth group vs. 61% in high wealth group).
TABLE 3.
Prevalence of overweight and obesity among nonpregnant and nonlactating (NPNL) women of reproductive age (18–49 years) with iron deficiency anaemia (IDA) by socio‐economic characteristics in Mirpur, Dhaka, Bangladesh, 2018
| Background characteristics | Total number of participants N = 525 | Number of participants with overweight and obesity N = 226 | Proportion of participants with overweight and obesity % (95% CI) |
|---|---|---|---|
| Women's characteristics | |||
| Age in years | |||
| 15–19 | 54 | 4 | 7.4(2.1–17.9) |
| 20–29 | 157 | 54 | 34.4(27.0–42.4) |
| 30–49 | 314 | 168 | 53.5(47.8–59.1) |
| Marital status | |||
| Unmarried | 69 | 8 | 11.6(5.1–21.6) |
| Married | 456 | 218 | 47.8(43.1–52.5) |
| Parity (n = 456) | |||
| None | 51 | 19 | 37.3(24.1–51.9) |
| 1 or more children | 405 | 199 | 49.1(44.2–54.1) |
| Women's education | |||
| No schooling | 155 | 56 | 36.1(28.6–44.2) |
| Primary (1–5 years) | 153 | 63 | 41.2(33.3–49.4) |
| Secondary and higher (+6 years) | 217 | 107 | 49.3(42.5–56.1) |
| Women's employment | |||
| Unemployed | 336 | 163 | 48.5(43.1–54.0) |
| Employed | 189 | 63 | 33.3(26.7–40.5) |
| Household characteristics | |||
| Household wealth index | |||
| Low | 175 | 44 | 25.1(18.9–32.2) |
| Medium | 175 | 76 | 43.4(35.9–51.1) |
| High | 175 | 106 | 60.6(52.9–67.9) |
| Household size | |||
| 1–4 persons | 308 | 140 | 45.5(39.7–51.2) |
| ≥5 persons | 217 | 86 | 39.6(33.1–46.5) |
3.4. Factors associated with overweight and obesity among NPNL women of reproductive age with IDA
Table 4 describes the adjusted and unadjusted associations of different socio‐economic factors with overweight and obesity among NPNL women of reproductive age with IDA. After adjustment, dose–response relationships were observed between overweight and obesity with the age of the women and household wealth indexes. Married women were more likely to be overweight or obese compared with unmarried women (adjusted odds ratio: 4.4; 95% CI: 1.8–11.1). The risk of being overweight or obese was higher among women having secondary and higher educational attainment compared with the women having no schooling (adjusted odds ratio: 1.9; 95% CI: 1.1–3.3). Unemployed women were more likely to be overweight or obese (adjusted odds ratio: 1.5; 95% CI: 1.0–2.4). We did not observe any association between overweight and obesity with household size.
TABLE 4.
Factors associated with overweight and obesity among NPNL women of reproductive age (18–49 years) with IDA in Mirpur, Dhaka, Bangladesh, 2018
| Background characteristics | Unadjusted a | Adjusted b | ||
|---|---|---|---|---|
| Odd ratios | 95% CI | Odd ratios | 95% CI | |
| Women's characteristics | ||||
| Age in years | ||||
| 18–19 | Ref | Ref | ||
| 20–29 | 5.0** | (1.7–15.1) | 4.1* | (1.3–12.9) |
| 30–49 | 10.3*** | (3.5–29.8) | 7.6*** | (2.4–24.1) |
| Marital status | ||||
| Unmarried | Ref | Ref | ||
| Married | 6.4*** | (2.9–13.9) | 4.4 ** | (1.7–11.1) |
| Parity c | ||||
| None | Ref | |||
| 1 or more children | 1.3 | (0.7–2.4) | ||
| Women's education | ||||
| No schooling | Ref | Ref | ||
| Primary (1–5 years) | 1.1 | (0.7–1.7) | 1.1 | (0.6–1.8) |
| Secondary and higher (+6 years) | 1.6* | (1.0–2.5) | 1.9* | (1.1–3.3) |
| Women's employment | ||||
| Employed | Ref | Ref | ||
| Unemployed | 2.1*** | (1.4–3.1) | 1.5* | (1.0–2.4) |
| Household characteristics | ||||
| Household wealth index | ||||
| Low | Ref | Ref | ||
| Medium | 2.3** | (1.4–3.7) | 2.3** | (1.4–3.9) |
| High | 4.6*** | (2.9–7.5) | 3.9*** | (2.3–6.8) |
| Household size c | ||||
| 1–4 persons | Ref | |||
| ≥5 persons | 0.9 | (0.6–1.3) | ||
Unadjusted odds are reported from bivariate logistic regression.
Adjusted odds are reported from multivariable logistic regression.
Parity and household size were omitted from multivariable logistic regression as the variables were not found significant in bivariate logistic regression.
P value < 0.05.
P value < 0.001.
P value < 0.000.
4. DISCUSSION
Our study has reported a high burden of overweight and obesity among NPNL women of reproductive age with IDA. Our findings suggest that the prevalence of overweight and obesity among NPNL women with IDA is 43% (95% CI: 39–47) higher than the prevalence of overweight and obesity among any women of reproductive age at 34% (95% CI: 30–38) in urban Bangladesh (Tanwi, Chakrabarty, & Hasanuzzaman, 2019). According to National Micronutrient Survey Bangladesh 2013, around 7% of nonpregnant nonlactating women of reproductive age suffered from IDA (International Centre for Diarrheal Disease Research Bangladesh, icddr,b, 2013). Similar to our findings, studies conducted in other settings like India, United States, Malawi, Taiwan, Morocco and Tunisia also confirmed the coexistence of overweight and obesity with IDA (Adib Rad et al., 2019; Chang et al., 2014; Fongar, Godecke, & Qaim, 2019; Gartner et al., 2014; Keding, 2016; Neymotin & Sen, 2011; Rhodes et al., 2020).
Overweight and obesity is a risk factor for IDA (Cepeda‐Lopez et al., 2011; Chang et al., 2014; Zhao et al., 2015). Findings from a meta‐analysis including data from 26 cross‐sectional and case–control studies (13,393 overweight/obese vs. 26,621 nonoverweight individuals) reported that overweight and obese individuals had 31% higher odds of developing iron deficiency (OR: 1.31; 95% CI: 1.01–1.68) (Zhao et al., 2015). Another study looking at the interaction effect of diet, BMI and IDA among Taiwanese women showed that overweight and obese women having high fat/low CHO diet had 10.11 (1.267–80.797) times higher risk of developing IDA (Chang et al., 2014). Despite having similar iron intake, obese women in Mexico had lower serum iron level (62.6 ± 29.5 vs. 72.4 ± 34.6 μg dl−1; P = 0.014) and iron binding capacity (399 ± 51 vs. 360 ± 48 μg dl−1; P < 0.001) compared with normal weight women (Cepeda‐Lopez et al., 2011). Potential explanations of increased risk of IDA among obese individuals include higher iron requirement, increased intake of energy‐dense food, dilutional hypoferremia and/or impaired iron absorption because of obesity‐induced inflammation (Cepeda‐Lopez, Aeberli, & Zimmermann, 2010; Cepeda‐Lopez et al., 2011; Chang et al., 2014). Biologically, obese individuals have a high level of obesity‐induced inflammatory biomarkers: serum hepcidin, interleukin‐1 (IL‐1), IL‐6 and tumour necrosis factor α (TNF‐α) (Aigner, Feldman, & Datz, 2014). These inflammatory biomarkers are strong modulators of iron availability. Elevated serum hepcidin level reduces dietary iron absorption as well as decreases systematic iron bioavailability (Camaschella, Nai, & Silvestri, 2020; Sanad, Osman, & Gharib, 2011; Tussing‐Humphreys, Pusatcioglu, Nemeth, & Braunschweig, 2012).
While looking at the socio‐economic factors associated with overweight and obesity among NPNL women of reproductive age with IDA, we found that household wealth status had a positive dose–response relationship with overweight or obesity. Several other studies reported similar associations (Ahirwar & Mondal, 2019; Khan & Kraemer, 2009; Neupane, Prakash, & Doku, 2016; Sarma et al., 2016; Tanwi, Chakrabarty, Hasanuzzaman, Saltmarsh, et al., 2019). Bangladesh is observing a fast‐paced economic growth along with a shift towards western culture of food intake, especially processed foods or diets containing more fats and refined sugars (Drewnowski & Popkin, 1997; Naicker, Venter, MacIntyre, & Ellis, 2015). Increased consumption of calorie‐dense fast food and a sedentary lifestyle among the richest in urban areas may result in an increased prevalence of overweight and obesity (Das et al., 2019; Morgan & Sonnino, 2010; Rahman, 2013).
Our study found a significant positive association between overweight and obesity with higher educational attainment among women with IDA. Studies looking at the association of education with overweight and obesity found a positive relationship between education and obesity in developing countries, whereas an inverse association was mostly found in developed countries (Ball & Crawford, 2005; Cohen, Rai, Rehkopf, & Abrams, 2013; Kim, Roesler, & von dem Knesebeck, 2017). One possible explanation could be that education may be linked with better access to food in developing countries.
Married women with IDA have five times higher risk of being overweight or obese compared with unmarried women. Our result is consistent with findings from other studies (Mkuu, Epnere, & Chowdhury, 2018; Sarma et al., 2016; Subramanian, Perkins, & Khan, 2009; Tanwi, Chakrabarty, & Hasanuzzaman, 2019; Tanwi, Chakrabarty, Hasanuzzaman, Saltmarsh, et al., 2019). The use of hormonal contraceptives could be one of the reasons for the higher risk of overweight and obesity among married women (Mkuu et al., 2018; Morotti et al., 2017). Hormonal contraceptives increase fluid retention that may lead to increase weight gain (Morotti et al., 2017).
Unlike other studies, we found unemployment as a risk factor for overweight or obese. Several studies conducted in similar settings refute this association (Mkuu et al., 2018; Tanwi, Chakrabarty, & Hasanuzzaman, 2019; Tanwi, Chakrabarty, Hasanuzzaman, Saltmarsh, et al., 2019). One possible explanation could be that majority of our study population are from the lower socio‐economic group and are involved in unskilled work, such as housekeeping and construction work, which requires lots of physical labour resulting in a low level of overweight and obesity among employed women.
A combination of overweight and obesity with IDA poses major challenges for public health interventions. One particular challenge is the lower efficacy of standard oral IDA treatment in presence of overweight or obesity (Camaschella et al., 2020). Although we were unable to find any study among adult women showing the efficacy of standard IDA treatment in presence of overweight or obesity, a randomized controlled trial conducted among South African children with IDA reported that children with high BMI for age had a twofold higher risk of remaining iron deficient after standard iron supplementation compared to children with normal weight (Baumgartner et al., 2013; Li, Dai, Jackson, & Zhang, 2008). A recent systematic review of literatures exploring genetic and molecular biology of iron metabolism and IDA recommends to revisit the standard treatment options of IDA (oral iron treatment and the choice of oral vs. intravenous iron) and suggested development of targeted therapies in presence of inflammation (Camaschella et al., 2020). In countries like Bangladesh where the prevalence of IDA is moderate to severe, our findings will help design context‐specific solutions for national health programming targeting anaemia and overweight or obesity.
4.1. Limitations
One limitation of the study is the use of cross‐sectional data, which limits the ability to draw causal inferences among observed associations. Moreover, there was no comparison group with overweight and obese NPNL women without IDA, which is recommended for future exploration. Also, we were unable to examine dietary patterns, level of physical activity, food security and use of hormonal contraceptives among the study participants that are intermediate in the causal pathways. Future studies looking at the association of dietary intake, physical activity, food security and the use of hormonal contraceptives with overweight and obesity are suggested.
5. CONCLUSION
Bangladesh is undergoing an epidemiologic transition with an increasing burden of overweight and obesity in the presence of a high level of micronutrient deficiencies. The growth in the prevalence of overweight and obesity outweighs the reduction in the prevalence of undernutrition in the country. In countries like Bangladesh where the prevalence of IDA is moderate to severe for public health significance, our findings illuminate the high burden of overweight and obesity among NPNL women with IDA and socio‐economic factors associated with this. Findings from this study will help design context‐specific solutions for national health programming targeting anaemia in presence of overweight and obesity.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
TMH and MJD designed the study and sought funding. NBA and TMH conceptualized the manuscript and prepared the first draft. NBA, MJD, SI, MMR, SR, SET, QSR, MHR, SEA and TMH contributed to the revisions.
ACKNOWLEDGMENT
This research protocol was funded by Medical Research Counsel, UK and Saving Lives at birth consortium. We acknowledge with gratitude the commitment of Medical Research Counsel, UK and Saving Lives at birth consortium to their research efforts. We are also grateful to the Governments of Bangladesh, Canada, Sweden and the United Kingdom for providing core/unrestricted support.
Ali NB, Dibley MJ, Islam S, et al. Overweight and obesity among urban women with iron deficiency anaemia in Bangladesh. Matern Child Nutr. 2021;17:e13102. 10.1111/mcn.13102
REFERENCES
- Abdullah, A. (2015). The double burden of undernutrition and overnutrition in developing countries: an update. Current Obesity Reports, 4(3), 337–349. 10.1007/s13679-015-0170-y [DOI] [PubMed] [Google Scholar]
- Adib Rad, H. , Sefidgar, S. A. A. , Tamadoni, A. , Sedaghat, S. , Bakouei, F. , Bijani, A. , & Omidvar, S. (2019). Obesity and iron‐deficiency anemia in women of reproductive age in northern Iran. Journal of Education Health Promotion, 8, 115. 10.4103/jehp.jehp_371_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahirwar, R. , & Mondal, P. R. (2019). Prevalence of obesity in India: A systematic review. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 13(1), 318–321. 10.1016/j.dsx.2018.08.032 [DOI] [PubMed] [Google Scholar]
- Aigner, E. , Feldman, A. , & Datz, C. (2014). Obesity as an emerging risk factor for iron deficiency. Nutrients, 6(9), 3587–3600. 10.3390/nu6093587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balarajan, Y. , & Villamor, E. (2009). Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. The Journal of Nutrition, 139(11), 2139–2144. 10.3945/jn.109.112029 [DOI] [PubMed] [Google Scholar]
- Ball, K. , & Crawford, D. (2005). Socioeconomic status and weight change in adults: A review. Social Science & Medicine, 60(9), 1987–2010. 10.1016/j.socscimed.2004.08.056 [DOI] [PubMed] [Google Scholar]
- Baumgartner, J. , Smuts, C. M. , Aeberli, I. , Malan, L. , Tjalsma, H. , & Zimmermann, M. B. (2013). Overweight impairs efficacy of iron supplementation in iron‐deficient South African children: A randomized controlled intervention. International Journal of Obesity, 37(1), 24–30. 10.1038/ijo.2012.145 [DOI] [PubMed] [Google Scholar]
- Bhurosy, T. , & Jeewon, R. (2014). Overweight and obesity epidemic in developing countries: A problem with diet, physical activity, or socioeconomic status? The Scientific World Journal. 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas, T. , Uddin, M. J. , Al Mamun, A. , Pervin, S. , & Garnett, S. P. (2017). Increasing prevalence of overweight and obesity in Bangladeshi women of reproductive age: Findings from 2004 to 2014. PLoS ONE, 12(7), e0181080. 10.1371/journal.pone.0181080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camaschella, C. , Nai, A. , & Silvestri, L. (2020). Iron metabolism and iron disorders revisited in the hepcidin era. Haematologica, 105(2), 260–272. 10.3324/haematol.2019.232124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano, P. M. , McIntyre, H. D. , Cruickshank, J. K. , McCance, D. R. , Dyer, A. R. , Metzger, B. E. , … Hadden, D. R. (2012). The hyperglycemia and adverse pregnancy outcome study: Associations of GDM and obesity with pregnancy outcomes. Diabetes Care, 35(4), 780–786. 10.2337/dc11-1790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda‐Lopez, A. C. , Aeberli, I. , & Zimmermann, M. B. (2010). Does obesity increase risk for iron deficiency? A review of the literature and the potential mechanisms. International Journal for Vitamin and Nutrition Research, 80(4–5), 263–270. 10.1024/0300-9831/a000033 [DOI] [PubMed] [Google Scholar]
- Cepeda‐Lopez, A. C. , Osendarp, S. J. , Melse‐Boonstra, A. , Aeberli, I. , Gonzalez‐Salazar, F. , Feskens, E. , … Zimmermann, M. B. (2011). Sharply higher rates of iron deficiency in obese Mexican women and children are predicted by obesity‐related inflammation rather than by differences in dietary iron intake. The American Journal of Clinical Nutrition, 93(5), 975–983. 10.3945/ajcn.110.005439 [DOI] [PubMed] [Google Scholar]
- Chang, J.‐S. , Chen, Y.‐C. , Owaga, E. , Palupi, K. C. , Pan, W.‐H. , & Bai, C.‐H. (2014). Interactive effects of dietary fat/carbohydrate ratio and body mass index on iron deficiency anemia among Taiwanese women. Nutrients, 6(9), 3929–3941. 10.3390/nu6093929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury, M. A. B. , Adnan, M. M. , & Hassan, M. Z. (2018). Trends, prevalence and risk factors of overweight and obesity among women of reproductive age in Bangladesh: A pooled analysis of five national cross‐sectional surveys. BMJ Open, 8(7), e018468–e018468. 10.1136/bmjopen-2017-018468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cnattingius, S. , Villamor, E. , Johansson, S. , Bonamy, A.‐K. E. , Persson, M. , Wikström, A.‐K. , & Granath, F. (2013). Maternal obesity and risk of preterm delivery. JAMA, 309(22), 2362–2370. 10.1001/jama.2013.6295 [DOI] [PubMed] [Google Scholar]
- Cohen, A. K. , Rai, M. , Rehkopf, D. H. , & Abrams, B. (2013). Educational attainment and obesity: A systematic review. Obesity Reviews, 14(12), 989–1005. 10.1111/obr.12062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das, S. , Fahim, S. M. , Islam, M. S. , Biswas, T. , Mahfuz, M. , & Ahmed, T. (2019). Prevalence and sociodemographic determinants of household‐level double burden of malnutrition in Bangladesh. Public Health Nutrition, 22(8), 1425–1432. 10.1017/S1368980018003580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski, A. , & Popkin, B. M. (1997). The nutrition transition: New trends in the global diet. Nutrition Reviews, 55(2), 31–43. 10.1111/j.1753-4887.1997.tb01593.x [DOI] [PubMed] [Google Scholar]
- Fongar, A. , Godecke, T. , & Qaim, M. (2019). Various forms of double burden of malnutrition problems exist in rural Kenya. BMC Public Health, 19(1), 1543. 10.1186/s12889-019-7882-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gartner, A. , El Ati, J. , Traissac, P. , Bour, A. , Berger, J. , Landais, E. , … Delpeuch, F. (2014). A double burden of overall or central adiposity and anemia or iron deficiency is prevalent but with little socioeconomic patterning among Moroccan and Tunisian urban women. The Journal of Nutrition, 144(1), 87–97. 10.3945/jn.113.178285 [DOI] [PubMed] [Google Scholar]
- Harding, K. L. , Aguayo, V. M. , & Webb, P. (2019). Trends and correlates of overweight among pre‐school age children, adolescent girls, and adult women in South Asia: An analysis of data from twelve national surveys in six countries over twenty years. Nutrients, 11(8). 10.3390/nu11081899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Centre for Diarrheal Disease Research Bangladesh,icddr,b , (United Nations Children's Fund (UNICEF), Global Alliance for Improved Nutrition (GAIN), and Institute of Public Nutrition. (2013). National Micronutrients Status Survey 2011–12: Final Report. Retrieved from Dhaka, Bangladesh: Centre for Nutrition and Food Security, icddr,b:
- Islam, M. , Ercumen, A. , Ashraf, S. , Rahman, M. , Shoab, A. K. , Luby, S. P. , & Unicomb, L. (2018). Unsafe disposal of feces of children <3 years among households with latrine access in rural Bangladesh: Association with household characteristics, fly presence and child diarrhea. PLoS ONE, 13(4), e0195218. 10.1371/journal.pone.0195218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, A. D. , Hayter, A. K. M. , Baker, C. P. , Prabhakaran, P. , Gupta, V. , Kulkarni, B. , … Kinra, S. (2016). The co‐occurrence of anemia and cardiometabolic disease risk demonstrates sex‐specific sociodemographic patterning in an urbanizing rural region of southern India. European Journal of Clinical Nutrition, 70(3), 364–372. 10.1038/ejcn.2015.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamruzzaman, M. , Rabbani, M. G. , Saw, A. , Sayem, M. A. , & Hossain, M. G. (2015). Differentials in the prevalence of anemia among non‐pregnant, ever‐married women in Bangladesh: Multilevel logistic regression analysis of data from the 2011 Bangladesh Demographic and Health Survey. BMC Womens Health, 15, 54–54. 10.1186/s12905-015-0211-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keding, G. (2016). Nutrition Transition in Rural Tanzania and Kenya. World Review of Nutrition and Dietetics, 115, 68–81. 10.1159/000442073 [DOI] [PubMed] [Google Scholar]
- Khan, M. M. , & Kraemer, A. (2009). Factors associated with being underweight, overweight and obese among ever‐married non‐pregnant urban women in Bangladesh. Singapore Medical Journal, 50(8), 804–813. [PubMed] [Google Scholar]
- Kim, T. J. , Roesler, N. M. , & von dem Knesebeck, O. (2017). Causation or selection ‐ examining the relation between education and overweight/obesity in prospective observational studies: A meta‐analysis. Obesity Reviews, 18(6), 660–672. 10.1111/obr.12537 [DOI] [PubMed] [Google Scholar]
- Leddy, M. A. , Power, M. L. , & Schulkin, J. (2008). The impact of maternal obesity on maternal and fetal health. Reviews in Obstetrics and Gynecology, 1(4), 170–178. [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Dai, Q. , Jackson, J. C. , & Zhang, J. (2008). Overweight is associated with decreased cognitive functioning among school‐age children and adolescents. Obesity (Silver Spring), 16(8), 1809–1815. 10.1038/oby.2008.296 [DOI] [PubMed] [Google Scholar]
- Mamun, S. , & Mascie‐Taylor, C. G. N. (2019). Double burden of malnutrition (DBM) and anaemia under the same roof: A Bangladesh perspective. Medical Science, 7(2), 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mkuu, R. S. , Epnere, K. , & Chowdhury, M. A. B. (2018). Prevalence and predictors of overweight and obesity among Kenyan women. Preventing Chronic Disease, 15, E44. 10.5888/pcd15.170401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan, K. , & Sonnino, R. (2010). The urban foodscape: World cities and the new food equation. Cambridge Journal of Regions, Economy and Society, 3(2), 209–224. [Google Scholar]
- Morotti, E. , Casadio, P. , Guasina, F. , Battaglia, B. , Mattioli, M. , & Battaglia, C. (2017). Weight gain, body image and sexual function in young patients treated with contraceptive vaginal ring. A prospective pilot study. Gynecological Endocrinology, 33(8), 660–664. 10.1080/09513590.2017.1306850 [DOI] [PubMed] [Google Scholar]
- Naicker, A. , Venter, C. , MacIntyre, U. E. , & Ellis, S. (2015). Dietary quality and patterns and non‐communicable disease risk of an Indian community in KwaZulu‐Natal, South Africa. Journal of Health, Population and Nutrition, 33(1), 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Population Research and Training (Bangladesh), Mitra and Associates (Firm), & MEASURE DHS (Program) . (2019). Bangladesh demographic and health survey, 2017: Key indicators. Dhaka: National Institute of Population Research and Training, Ministry of Health and Family Welfare. [Google Scholar]
- Neupane, S. , Prakash, K. C. , & Doku, D. T. (2016). Overweight and obesity among women: Analysis of demographic and health survey data from 32 Sub‐Saharan African Countries. BMC Public Health, 16, 30. 10.1186/s12889-016-2698-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neymotin, F. , & Sen, U. (2011). Iron and obesity in females in the United States. Obesity (Silver Spring), 19(1), 191–199. 10.1038/oby.2010.112 [DOI] [PubMed] [Google Scholar]
- Popkin, B. M. (1994). The nutrition transition in low‐income countries: An emerging crisis. Nutrition Reviews, 52(9), 285–298. 10.1111/j.1753-4887.1994.tb01460.x [DOI] [PubMed] [Google Scholar]
- Rahman, S. (2013). Obesity in junk food generation in Asia: A health time bomb that needs early defusing! South East Asia . Journal of Public Health, 3(1), 1–2. [Google Scholar]
- Rasmussen, K. (2001). Is there a causal relationship between iron deficiency or iron‐deficiency anemia and weight at birth, length of gestation and perinatal mortality? Journal of Nutrition, 131(2s‐2), 590S–601S; discussion 601S–603S. 10.1093/jn/131.2.590S [DOI] [PubMed] [Google Scholar]
- Rhodes, E. C. , Suchdev, P. S. , Narayan, K. M. V. , Cunningham, S. , Weber, M. B. , Tripp, K. , … Williams, A. M. (2020). The co‐occurrence of overweight and micronutrient deficiencies or anemia among women of reproductive age in Malawi. The Journal of Nutrition, 150(6), 1554–1565. 10.1093/jn/nxaa076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanad, M. , Osman, M. , & Gharib, A. (2011). Obesity modulate serum hepcidin and treatment outcome of iron deficiency anemia in children: A case control study. Italian Journal of Pediatrics, 37, 34. 10.1186/1824-7288-37-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarma, H. , Saquib, N. , Hasan, M. M. , Saquib, J. , Rahman, A. S. , Khan, J. R. , … Ahmed, T. (2016). Determinants of overweight or obesity among ever‐married adult women in Bangladesh. BMC Obesity, 3, 13. 10.1186/s40608-016-0093-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidhuber, J. , & Shetty, P. (2005). The nutrition transition to 2030. Why developing countries are likely to bear the major burden. Acta Agriculturae Scand Section c, 2(3–4), 150–166. [Google Scholar]
- Scholl, T. O. , Hediger, M. L. , Fischer, R. L. , & Shearer, J. W. (1992). Anemia vs iron deficiency: increased risk of preterm delivery in a prospective study. The American Journal of Clinical Nutrition, 55(5), 985–988. 10.1093/ajcn/55.5.985 [DOI] [PubMed] [Google Scholar]
- Subramanian, S. V. , Perkins, J. M. , & Khan, K. T. (2009). Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? The American Journal of Clinical Nutrition, 90(2), 369–376. 10.3945/ajcn.2009.27487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanwi, T. S. , Chakrabarty, S. , & Hasanuzzaman, S. (2019). Double burden of malnutrition among ever‐married women in Bangladesh: A pooled analysis. BMC Womens Health, 19(1), 24. 10.1186/s12905-019-0725-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanwi, T. S. , Chakrabarty, S. , Hasanuzzaman, S. , Saltmarsh, S. , & Winn, S. (2019). Socioeconomic correlates of overweight and obesity among ever‐married urban women in Bangladesh. BMC Public Health, 19(1), 842. 10.1186/s12889-019-7221-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrift, A. P. , & Callaway, L. K. (2014). The effect of obesity on pregnancy outcomes among Australian Indigenous and non‐Indigenous women. Medical Journal of Australia, 201(10), 592–595. 10.5694/mja13.11170 [DOI] [PubMed] [Google Scholar]
- Tussing‐Humphreys, L. , Pusatcioglu, C. , Nemeth, E. , & Braunschweig, C. (2012). Rethinking iron regulation and assessment in iron deficiency, anemia of chronic disease, and obesity: Introducing hepcidin. Journal of the Academy of Nutrition and Dietetics, 112(3), 391–400. 10.1016/j.jada.2011.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirth, J. P. , Woodruff, B. A. , Engle‐Stone, R. , Namaste, S. M. , Temple, V. J. , Petry, N. , … Aaron, G. J. (2017). Predictors of anemia in women of reproductive age: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. The American Journal of Clinical Nutrition, 106(Suppl 1), 416S–427S. 10.3945/ajcn.116.143073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, L. , Zhang, X. , Shen, Y. , Fang, X. , Wang, Y. , & Wang, F. (2015). Obesity and iron deficiency: A quantitative meta‐analysis. Obesity Reviews, 16(12), 1081–1093. 10.1111/obr.12323 [DOI] [PubMed] [Google Scholar]


