Abstract
The inappropriate marketing and aggressive promotion of breastmilk substitutes (BMS) undermines breastfeeding and harms child and maternal health in all country contexts. Although a global milk formula ‘sales boom’ is reportedly underway, few studies have investigated its dynamics and determinants. This study takes two steps. First, it describes trends and patterns in global formula sales volumes (apparent consumption), by country income and region. Data are reported for 77 countries, for the years 2005–19, and for the standard (0–6 months), follow‐up (7‐12 m), toddler (13‐36 m), and special (0‐6 m) categories. Second, it draws from the literature to understand how transformations underway in first‐food systems – those that provision foods for children aged 0–36 months – explain the global transition to higher formula diets. Total world formula sales grew by 115% between 2005 and 2019, from 3.5 to 7.4 kg/child, led by highly‐populated middle‐income countries. Growth was rapid in South East and East Asia, especially in China, which now accounts for one third of world sales. This transition is linked with factors that generate demand for BMS, including rising incomes, urbanisation, the changing nature of woman's work, social norms, media influences and medicalisation. It also reflects the globalization of the baby food industry and its supply chains, including the increasing intensity and sophistication of its marketing practices. Policy and regulatory frameworks designed to protect, promote and support breastfeeding are partially or completely inadequate in the majority of countries, hence supporting industry expansion over child nutrition. The results raise serious concern for global child and maternal health.
Keywords: breastmilk substitutes, commercial determinants of health, infant and young child feeding, infant formula, marketing, nutrition transition
Key messages.
The aggressive and inappropriate marketing of breastmilk substitutes (BMS) harms child and maternal health. Despite this, a global milk formula ‘sales boom’ is underway. World milk formula sales grew by 121.5% between 2005‐19, from 3.5 to 7.4 kg/child, led by highly‐populated middle‐income countries.
This transition links with first‐food systems transformations, including rising incomes, urbanization, social norms, woman's work, medicalisation, and the globalization of the baby food industry.
Companies have used diverse marketing techniques to grow their markets, including product diversification, cross‐promotion, digital marketing, and health professional co‐optation.
Policies to protect, promote and support breastfeeding are partially or completely inadequate.
1. INTRODUCTION
Breastfeeding is the biological norm for feeding human infants and young children. Breastmilk is a personalized source of early‐life nutrition, providing optimal levels of nutrients in volumes regulated by the mother–child feeding dyad, and an array of biological factors crucial for normal physical, immunological and neurological development of the child (Victora et al., 2016). To achieve optimal growth, development and health the World Health Organization (WHO) recommends infants initiate breastfeeding in the first hour of life, are exclusively breastfed for the first six months, and thereafter receive nutritionally adequate and safe complementary foods, while breastfeeding continues for up to two years of age or beyond (World Health Organization & UNICEF, 2003). The WHO/UNICEF Global Strategy for Infant and Young Child Feeding calls on governments to protect, promote and support breastfeeding through policy and programming action, including the adoption of The International Code of Marketing of Breast‐Milk Substitutes and subsequent World Health Assembly resolutions (The Code) into national law (World Health Organization & UNICEF, 2003). Implementation and monitoring of The Code is supported by the United Nations Convention on the Rights of the Child, and its monitoring body the Committee on the Rights of the Child (United Nations Office of the High Commissioner on the Rights of the Child, 1989).
First adopted in 1981, The Code is a response to long‐standing concern that the marketing of commercial breastmilk substitutes (BMS) undermines breastfeeding and harms newborn, child and maternal health in all countries, irrespective of their development status (World Health Organization, 1981). Commercial BMS include any milks (or products that could be used to replace milk, such as fortified soy milk), in either liquid or powdered form, that are specifically marketed for feeding infants and young children up to the age of 3 years', including infant, follow‐up and toddler formulas (World Health Organization, 2016, 2017a). Various animal milks and other liquids are also often used as functional BMS in many (typically low‐income) settings, although not marketed as such (Victora et al., 2016). Commercial complementary foods can further displace breastmilk, when marketed or used inappropriately (World Health Organization, 2017a). In this paper we focus on milk formulas as the main type of commercial BMS consumed worldwide. These are ultra‐processed foods (Baker et al., 2020; Monteiro, Cannon, Lawrence, Costa Louzada, & Machado 2019), typically formulations of skimmed milk powder and milk proteins (from cows or other animals), vegetable oils, sweeteners, micronutrients and other additives. Milk formulas can be appropriate when breastfeeding is medically contraindicated, and when alternatives such as breastmilk expression, wet‐nursing or human donor milk are unavailable. However, these products are implicated in child malnutrition through several mechanisms, including inter aliaunder‐ and over‐dilution, under‐ and over‐feeding, pathogen and industrial contamination (e.g. China's 2008 melamine poisoning crisis), and the displacement of breastfeeding and breastmilk in the child's diet (Baker et al., 2016; Jelliffe & Jelliffe, 1978; Victora et al., 2016; Wells et al., 2020).
Evidence of the adverse health implications of formula‐feeding comes from studies comparing never and partially breast‐fed versus exclusively breast‐fed infants and young children. For the child, this includes significant increased risks of diarrhoea and respiratory infection, malocclusion, and all‐cause mortality, and probable increased risks of obesity and type‐2 diabetes (Victora et al., 2016). Delayed initiation of breastfeeding following birth (beyond 1‐hour), significantly increases the risk of newborn death (Edmond et al., 2016). For mothers, not breastfeeding increases the risk of breast cancer, and possibly ovarian cancer and type‐2 diabetes, and forgoes further benefits of breastfeeding for birth spacing and family planning (Kennedy, Rivera, & McNeilly, 1989; Victora et al., 2016). Not breastfeeding can be attributed to an estimate 595,379 child deaths (6 to 59 months) annually from diarrhoea and pneumonia, and 98,243 maternal deaths from breast and ovarian cancers, and type‐2 diabetes (Walters, Phan, & Mathisen, 2019). Not breastfeeding further generates economic losses of US$341.3 billion annually, resulting from higher health care costs, premature mortality and lost productivity (Walters et al., 2019). Dairy production linked with milk formula supply‐chains also generates significant environmental harm, including greenhouse gas emissions, water pollution and plastic waste (Joffe, Webster, & Shenker, 2019; Karlsson, Garnett, Rollins, & Röös, 2019).
In low and middle‐income countries, milk formula consumption is strongly and negatively associated with continued breastfeeding at 12–15 months (Neves et al., 2019). Although the global exclusive breastfeeding rate (<6 months) improved from 33% in 1995 to 42% in 2018 (UNICEF, 2019), this progress is insufficient to meet the World Health Assembly's global target of 50% by 2025 (Development Initiatives, 2020). Mirroring this slow progress is a global infant and young child feeding (IYCF) transition to diets higher in commercial milk formulas (Baker et al., 2016; Rollins et al., 2016). This transition reflects unprecedented changes in first‐food systems – the systems that provision foods for children aged 0–36 months – at national, regional and global levels. Such transitions and first‐food systems transformations are not a new phenomenon. Some countries (e.g. Australia, United States, Norway), experienced declines in breastfeeding and a normalisation of formula‐feeding during the mid‐20th century, linked with rising incomes, urbanization, the changing nature of women's work, the medicalization of pregnancy and birthing, more intensive BMS marketing, and the failure of policies to protect, promote and support breastfeeding in these new contexts (Liestøl, Rosenberg, & Walløe, 1988; Ryan, 1997a; Smith, 2007). Several countries have since experienced a reversal in these historical declines in breastfeeding. Such transitions are socially stratified, occurring first in higher‐income and then in lower‐income groups, as countries grow richer (Cattaneo, 2012; Neves et al., 2019; World Health Organization, 1982).
In this paper, we examine important features of the current transition in IYCF that differentiates it from the past. First, it is unprecedented in the scale of change, occurring mainly in middle‐income countries, home to the majority of the world's population. Second, it involves a wider range of child age groups and commercial milk formula categories, including not just standard (for ages 0–6 months) and follow‐up (6–12 months) milk formulas, but also toddler (13–36 months) and special (0‐6 m) categories. The WHO has long maintained that follow‐up and toddler milks are unnecessary and unsuitable as substitutes for continued breastfeeding (World Health Organization, 2013). Third, the transition is occurring in the context of ongoing economic globalization and rapid growth in the size, transnational reach and consolidation of the baby food industry. Market reports describe a global milk formula ‘sales boom’ underway, with the majority of sales accruing to a small number of ‘Big Formula’ corporations (Changing Markets Foundation, 2017; Save the Children, 2013a). Big Formula are reportedly using intensive and increasingly sophisticated marketing techniques to reach mothers and expand their markets, hence increasingly commodifying infant and young child feeding worldwide (Changing Markets Foundation, 2017; Choi, Ludwig, & Harris, 2019; Save the Children, 2013a).
These developments are important to understand, given the implications for global infant, child and maternal health. Yet few analyses describing the current IYCF transition and its determinants exist. In this paper, we provide new data on global trends and patterns in commercial milk formula sales, and describe the first‐food systems transformations linked with the IYCF transition to higher milk formula diets, including the marketing practices Big Formula is using to expand and sustain their markets worldwide. We also review the literature explaining the global rise in toddler and special milk formula consumption. We ask, has the IYCF transition to higher diets higher in milk formulas continued, accelerated or abated in recent decades, in which countries and regions? What first‐food systems factors and underlying drivers are likely to explain the observed changes in worldwide milk formula sales trends and patterns?
2. METHODS
Given the complex nature of the topic, we adopted a synthesis review method involving three steps. First, we elucidated the main components of first‐food systems to help guide the study. Second, using market sales data we quantified worldwide trends and patterns in the apparent consumption of commercial milk formulas. Third, we reviewed academic and grey literature to understand what first‐food system factors likely explain the observed results.
First‐food systems framework: Food systems are the inputs, actors and activities relating to the production, processing, distribution, preparation, consumption and disposal of food, the social, economic and environmental outcomes resulting from those activities, and the underlying biophysical, social, economic, technological, institutional, and political drivers (High Level Panel of Experts on Food Security and Nutrition, 2017). Breastfeeding has been described as a global food production system (Smith, 2015), and breastmilk the “original ready‐to‐serve 24‐hour convenience food” with output regulated by the mother–child dyad (Jelliffe & Jelliffe, 1978). More broadly, we define first‐food systems as those that provision foods for infants and young children aged 0–36 months, including breastmilk, commercial BMS, other non‐human milks, and home‐prepared or commercial complementary foods (Baker, 2020). To describe the main components of first‐food systems, we integrated several food systems and IYCF frameworks, shown in Table 1 (High Level Panel of Experts on Food Security and Nutrition, 2017; Pérez‐Escamilla, Curry, Minhas, Taylor, & Bradley, 2012; Piwoz & Huffman, 2015; Rollins et al., 2016; UNICEF & Global Alliance for Improved Nutrition, 2019).
TABLE 1.
First‐food systems components
| Components | Description |
|---|---|
| Underlying drivers | Factors linked with social, economic, technological and political change, including changing birth‐rates, income growth, urbanization, the nature of women's work within and outside of the home, shifts in socio‐cultural norms, and globalization. |
| First‐food supply chains | Breastmilk supplied by the mother–child breastfeeding dyad; also by wet nurses, milk banks, informal sharing networks or commercial sources; BMS and other baby food supply chains, involving the inputs, actors and activities relating to the production of ingredients through to processing, manufacturing, distribution and disposal. |
| First‐food environments | The contexts in which mothers and care‐givers make feeding decisions, including health care, retail, workplace, community and household settings, and the extent to which these promote, support or undermine breastfeeding; and/or the feeding of BMS and other foods in relation to availability, price, convenience, safety and quality, and exposure to marketing. |
| Maternal and infant attributes | The mother's age, weight, education, socio‐economic status and confidence, and her baby's sex, wellbeing, and temperament influence feeding decisions; this includes moment‐by‐moment interactions and perceptions (e.g. if her baby is satisfied and content), and the internalisation of other first‐food system influences and structural forces. |
| Governance, policy and regulatory frameworks | The degree to which governance arrangements, policies, regulations and knowledge systems support, promote and protect breastfeeding at all levels; this includes the degree to which breastfeeding is prioritised, and to which laws, policies and programmes are developed, resourced, implemented, monitored and enforced, and sustained over time. |
Data sources: To quantify trends we sourced milk formula sales volume data (kg) from Euromonitor for the years 2005–2019 with projections to 2024, for 77 countries for the standard (0–6 months), follow‐up (6‐12 m), toddler (13‐36 m) and special (0‐6 m) milk formula categories. We define these categories, and provide examples of leading brands, in Supplemental Table S1. This data was sourced from Euromonitor by the lead author, through an institutional license with Deakin University. We used sales volume rather than value data, as milk formula prices used to calculate the latter can vary markedly across countries and regions (Changing Markets Foundation, 2017). Countries were grouped by UNICEF region and World Bank income level, outlined in Supplemental Table S2. These included 37 (48.1% of total) high‐income countries (HICs), 25 (32.5%) upper‐middle income countries (UMICs), and 15 (19.5%) lower‐middle income countries (LMICs). The milk formula categories are those defined by Euromonitor (Euromonitor International, 2019). Euromonitor collects this data from trade associations, industry bodies, business press, company financial reports, company filings, and official government statistics. People working within industry validate the estimates (Euromonitor International, 2019). We controlled for population growth by converting sales volume data to per child using age‐specific population estimates and projections sourced from the World Bank for the same years (World Bank, 2019). To illustrate trends in supply chain ingredients, we sourced production volume data (tonnes) from FAOSTAT (Food and Agriculture Organization of the United Nations, 2019).
Data analysis: We generated descriptive statistics of milk formula category sales volumes per child for the period 2005–2019 with projections to 2024, and growth rates for the period 2005–2019, by country income and region, using R version 3.6.2 (Foundation for Statistical Computing). Growth rate measures included the percentage change for the time periods listed above, and the compounding annual growth rate (CAGR), representing the mean annual growth rate for the 2005–19 period. Due to insufficient data availability, we did not correct the per child estimates for the proportion of infants/children exclusively breastfed or mixed‐fed within each country. Hence our estimates are likely to be underestimates in countries with higher breastfeeding rates.
Literature search and synthesis: To understand what first‐food system components and dynamics might explain the observed milk formula sales trends and patterns, we searched academic and grey literature, extracted key findings and synthesised results. This involved a search of the Google Scholar, Web of Science and Econlit databases using combinations of the terms ‘breastmilk substitutes’, ‘formula’, ‘infant feeding’ and ‘infant and young child feeding’ with terms from the first‐food systems framework, with no time‐constraints. Grey literature sources included the websites of lead UN nutrition agencies (WHO, UNICEF, FAO, World Bank), and international civil society organizations (Save the Children, 1,000 Days, FHI Solutions/Alive & Thrive, International Baby Food Action Network, Helen Keller International, World Vision). Given the topic's complexity and diverse literature sources, further reference list searches and branching searches using Google Scholar were also used. Studies were included if published in English, relevant to the study aim, with described objectives, a clear method (if relevant), and conclusions substantiated by the results. All documents were uploaded to NVivo (QSR International) and coded. The quantitative data and findings from the literature were then synthesised into the final results.
3. RESULTS
3.1. Global trends and patterns in commercial milk formula sales
Figure 1 and Figure 2 present historic and projected data on milk formula category sales per child by country income and region respectively. Supplemental Figure 1 presents data on total milk formula sales volumes by category for all countries combined. Figure 3 shows country‐level category sales per child in 2019 versus 2005–19 compounding annual growth rates. Table 2 provides a summary of category sales volumes and growth rates by country income and region, and for all countries combined.
FIGURE 1.

Commercial milk formula category sales volumes (kg) per child by World Bank country income‐level, 2005–2019, with projections to 2024
FIGURE 2.
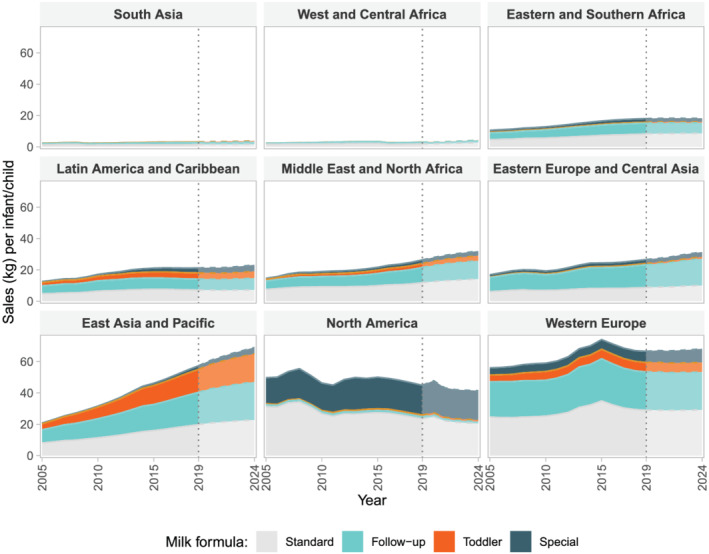
Commercial milk formula category sales volumes (kg) per child by UNICEF region, 2005–2019, with projections to 2024
FIGURE 3.

Country milk formula category sales volumes (kg) per child in 2019 v. 14‐year compounding annual growth rate (CAGR; %) for 2005–2019; weighted markers represent infant/child population sizes
TABLE 2.
Commercial milk formula category sales volumes (kg) per child (c) in 2019, with 2005–19 compounding annual growth rates (CAGR; %), and historical and projected period growth rates (%), by country income group, region, and all countries combined
| Markets | Standard (0–6 months) | Follow‐up (7–12 months) | Toddler (12–36 months) | Special (0–6 months) | Total (0–36 months) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 (kg/c) | CAGR 2005–2019 (%) | Δ2005–2019 (%) | Δ2019–2024 (%) | 2019 (kg/c) | CAGR 2005–2019 (%) | Δ2005–2019 (%) | Δ2019–2024 (%) | 2019 (kg/c) | CAGR 2005–2019 (%) | Δ2005–2019 (%) | Δ2019–2024 (%) | 2019 (kg/c) | CAGR 2005–2019 (%) | Δ2005–2019 (%) | Δ2019–2024 (%) | 2019 (kg/c) | CAGR 2005–2019 (%) | Δ2005–2019 (%) | Δ2019–2024 (%) | ||
| Income | HICs (n = 37) | 29.0 | −0.1 | 4.5 | −2.1 | 16.7 | 1.0 | 21.4 | 0.8 | 7.0 | 6.6 | 147.7 | 10.6 | 11.8 | 1.7 | 33.8 | 9.9 | 14.2 | 2.1 | 36.1 | 5.0 |
| UMICs (n = 25) | 15.7 | 7.6 | 172.5 | 18.3 | 17.2 | 7.4 | 166.2 | 21.3 | 7.6 | 9.6 | 248.9 | 21.3 | 2.7 | 12.5 | 406.3 | 70.4 | 10.9 | 8.6 | 206.9 | 22.2 | |
| LMICs (n = 15) | 3.6 | 2.7 | 41.0 | 10.1 | 3.8 | 3.4 | 54.3 | 11.3 | 3.6 | 8.6 | 203.9 | 13.9 | 0.3 | 4.5 | 80.8 | 21.8 | 3.7 | 6.1 | 122.3 | 12.9 | |
| Region | East Asia & Pacific | 19.7 | 6.6 | 143.1 | 15.0 | 20.6 | 6.7 | 145.5 | 17.5 | 14.7 | 10.3 | 287.8 | 22.0 | 2.3 | 11.2 | 342.8 | 78.6 | 16.9 | 8.7 | 215.2 | 21.1 |
| Eastern & Southern Africa | 8.2 | 4.9 | 79.9 | 4.6 | 6.9 | 4.0 | 59.5 | −1.9 | 0.6 | 3.2 | 37.5 | −2.5 | 2.4 | 5.1 | 83.3 | −3.1 | 3.3 | 4.4 | 63.0 | 2.7 | |
| Eastern Europe & Central Asia | 8.7 | 3.3 | 42.7 | 14.7 | 14.5 | 4.2 | 61.6 | 17.8 | 0.9 | 9.5 | 199.1 | 34.8 | 2.5 | 4.2 | 62.6 | 22.1 | 4.8 | 4.4 | 57.0 | 19.3 | |
| Latin America & Caribbean | 7.1 | 2.6 | 50.3 | 1.1 | 7.0 | 2.0 | 37.5 | 6.6 | 4.0 | 4.2 | 87.9 | 8.8 | 3.2 | 11.8 | 396.7 | 33.3 | 5.5 | 3.7 | 75.6 | 8.6 | |
| Middle East & North Africa | 11.8 | 5.1 | 56.9 | 19.5 | 9.7 | 6.1 | 80.8 | 19.9 | 2.6 | 9.2 | 149.5 | 27.6 | 2.3 | 10.8 | 231.8 | 28.6 | 5.6 | 6.8 | 86.8 | 23.5 | |
| North America | 23.5 | −2.6 | −24.8 | −13.1 | 1.3 | 0.3 | 12.4 | −1.1 | 1.1 | 3.6 | 67.7 | −12.2 | 19.0 | 0.4 | 14.0 | −1.1 | 8.1 | −1.0 | −10.0 | −7.2 | |
| South Asia | 1.5 | 0.3 | 9.1 | 6.6 | 1.3 | 3.4 | 66.9 | 24.5 | 0.4 | 3.4 | 67.6 | 27.4 | 0.0 | 5.1 | 108.1 | 53.6 | 0.7 | 2.2 | 42.3 | 18.7 | |
| West & Central Africa | 1.9 | 2.6 | 8.8 | 43.1 | 1.1 | 5.3 | 56.5 | 39.2 | 0.1 | 5.1 | 47.3 | 38.7 | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 3.5 | 21.1 | 41.8 | |
| Western Europe | 29.0 | 0.9 | 17.8 | 0.6 | 24.4 | 0.3 | 8.2 | −1.1 | 6.0 | 2.5 | 40.8 | 1.4 | 7.2 | 3.0 | 56.2 | 22.0 | 14.0 | 1.3 | 21.0 | 2.5 | |
| All countries (n = 77) | 10.8 | 3.3 | 54.5 | 8.0 | 9.9 | 4.7 | 86.5 | 11.8 | 5.4 | 8.7 | 210.0 | 15.4 | 2.5 | 4.2 | 75.0 | 30.4 | 7.4 | 5.8 | 115.5 | 13.6 | |
Abbreviations: HICs – high‐income countries; UMICs – upper‐middle income countries; LMICs – lower‐middle income countries; CAGR – or compounding annual growth rate, represents the mean annual growth rate over the period; Δ – or delta, represents the total percentage change over the period.
Between 2005 and 19, the total milk formula retail sales volume for all countries increased 121.5% from 0.97 to 2.15 million tonnes, with further projected growth of 10.8% to 2.38 million tonnes by 2024 (Figure S1). Historic growth was mostly attributed to the toddler category, which grew by 220% over the period, compared with 57.2%, 89.7% and 78.1% growth in the standard, follow‐up and special categories respectively. The toddler category made up 48% of total sales by volume for all countries in 2019, followed by 24%, 22% and 5.6% for the standard, follow‐up and special categories respectively. On a per child basis, total sales for all countries combined grew by 115.5% from 3.5 to 7.5 kg. This figure is projected to increase by 13.6% to 8.5 kg by 2024, with growth led by middle‐income countries. The standard category had the highest per child volume in HICs, follow‐up in UMICs, with little difference between standard, follow‐up and toddler in LMICs. In 2019, per child volumes of standard formula in HICs were double those in UMICs, and 8‐fold higher thanin LMICs. Follow‐up and toddler formula volumes per child in UMICs exceeded those in HICs (Table 2).
There was wide variation in category sales and growth rates between regions and country income categories, and between countries at the same income level. Much of the recent growth was attributed to UMICs, where total volumes per child increased by 206.9% in 2005–19 (Figure 1 and Table 2). This growth was led by China, Brazil, Turkey, South Africa and Russia (Figure 3). Growth was also strong in LMICs at 122.3% over the same period, although with some exceptions (e.g. Indonesia) total per child volumes were 3‐ to 4‐fold lower than in UMICs and HICs respectively.
By region, the UMICs and HICs of the Middle East & North Africa region had comparatively high volumes and growth rates, notably Saudi Arabia and Turkey. In Latin America & the Caribbean, Peru and Brazil had high growth rates across nearly all categories. Growth was especially rapid in several highly‐populated middle‐income countries of East and South East Asia, namely China, Indonesia and Vietnam, and weaker growth but higherper child volumesin Thailand and Malaysia. Of all countries China stands‐out, as home to the world's second largest infant and young child population. In 2005, it represented 14.1% of the total sales volume for all countries combined. By 2019 this figure was 32.5%, equivalent to 698 million kg of total formula, 2.3‐fold more than the US and Western Europe markets combined. This was equivalent to 2.8 kg per child in 2005, increasing by 79.9% to 13.9 kg by 2019.
Overall, growth was much lower in HIC countries, where total milk formula per child sales volumes grew by 36.1% in 2005–19. This figure reflected weak growth in the standard category at 4.5% over the period, but masks strong growth in the follow‐up, toddler and special categories which grew by 21.4%, 147.7% and 33.8% respectively (Table 2). Certain HICs including New Zealand, Australia, Ireland and the Netherlands had remarkably high volumes and/or growth rates across all milk formula categories. Mexico stands‐out as a middle‐income country experiencing declines or stagnant growth across categories. As home to the world's largest infant and young child population, India has remarkably low per child volumes across all categories and negative growth in the standard category.
Special formula had the highest growth rates and projected growth across most regions (Table 2), in particular East Asia & Pacific, Latin America & Caribbean and Middle East & North Africa, which grew by 342.8%, 396.7% and 231.8% respectively over the period. Highly populated UMICs including China and Mexico were experiencing the highest growth rates in special formula sales, whereas HICs such as Australia, New Zealand and the United States had remarkably high sales volumes. While the US is expected to remain the largest global special formula market, strong growth is forecasted in the East Asia & Pacific region, especially in China.
3.2. First‐food system transformations explaining worldwide milk formula sales trends and variations
Guided by the first‐food systems framework, we reviewed the literature to understand how the trends and patterns in worldwide milk formula sales observed in the previous section, reflect transformations underway in first‐food systems across different country contexts. It is important to acknowledge that much of this literature is sourced from high‐income and middle‐income country studies.
3.2.1. Underlying economic, demographic and socio‐cultural drivers
At the most basic level, the observed changes reflect factors that drive demand for BMS. As economies grow consumer incomes rise, although unequally, resulting in the increased affordability and expenditure on higher‐value products, including processed and animal‐sourced foods (Grigg, 1999; Popkin & Reardon, 2018; Reardon et al., 2014). Milk formula consumption is positively associated with income across countries, and with wealth quintiles within countries (Baker et al., 2016; Neves et al., 2019). Hence, rapid sales growth in East and South East Asia, and in particular China, at least partly reflects the emergence of that reigon's increasingly affluent middle‐class (Baker, Kay, & Walls, 2014). Urbanization also likely explains the observed growth in UMICs and LMICs – the movement of people from rural to urban areas, and societal adaptations to this change (Baker et al., 2014; Reardon et al., 2014). This can increase physical proximity to BMS and exposure to marketing, associates with more work outside of the home, shrinking family sizes (from larger kin‐dominated to smaller nuclear units), and the adoption of ‘modernity’ values and lifestyles more conducive to formula‐feeding (Haddad et al., 2016; Jelliffe & Jelliffe, 1978).
Another driver is the changing nature of women's work and its compatibility with breastfeeding. Rising workforce participation in the absence of maternity protection and workplace entitlements, and without the gendered redistribution of work within the home, increases the opportunity cost of breastfeeding and reduces duration and intensity (Jelliffe & Jelliffe, 1978; Roe, Whittington, Fein, & Teisl, 1999; Rollins et al., 2016). Growing BMS demand across Asia, may partly reflect the rise of large labour‐intensive manufacturing industries in the regions special economic and export processing zones (where women can comprise 70–90% of the workforce), and large informal economies where maternity protection is often absent (Baker et al., 2016; International Labor Organization & Asia Development Bank, 2011). Changing social beliefs and norms can also drive demand (Grant, 2016; Grayson, 2016; Stuart‐Macadam, 2017). The de‐normalisation of breastfeeding relative to formula‐feeding has been linked with rising stigma about breastfeeding in public, the hyper‐sexualisation (or defunctionalisation) of breasts, changing beliefs about gender roles and motherhood, and the degree to which IYCF knowledge and skills are transferred inter‐generationally (Hannan, Li, Benton‐Davis, & Grummer‐Strawn, 2005; Jelliffe & Jelliffe, 1978; Scott & Mostyn, 2003). These can be propagated and reinforced by commercial marketing practices and media portrayals of IYCF (see first food environments).
3.2.2. First‐food supply chain transformations
Understanding the observed growth in global milk formula sales also requires consideration of evolving commercial supply chains. The mother–child breastfeeding dyad is arguably the shortest food supply chain on earth. In contrast, commercial milk formula supply chains are highly complex, involving many production inputs, and are typically ‘long‐chains’ comprising national and global sourcing and distribution networks (Coriolis, 2014).
The evolution and global expansion of milk formula supply chains, is closely linked with the timing and depth of trade liberalization – i.e. systematic reductions in barriers to cross‐border trade and investment. This accelerated following the establishment of the World Trade Organization (WTO) in 1995, and since then an explosion in regional and bilateral trade agreements, as well as unilateral actions by governments to liberalize their economies (Baker et al., 2014; Smith, Galtry, & Salmon, 2014). This has facilitated global supply chain expansion, by reducing barriers to the movement of production inputs, final products and investments across borders. This enables companies to enter or more vigorously expand into new markets, which can in‐turn stimulate market competition and greater marketing intensity (Baker et al., 2014; Baker & Friel, 2016).
Milk formula supply chains begin with the production, processing and trade of raw ingredients used in manufacturing. World production of dry milk powder, grew 7‐fold between 1961 and 2014 from 491,000 to 3,444,000 tonnes (Figure S2), providing a cheap and readily‐available production input. Europe produced the majority of this commodity until the 1990s, with New Zealand, Australia, and South America then intensifying their dairy sectors and increasing output. Such production is highly concentrated in some countries, with a few firms dominating – for example, Dairy Farmers of America in the United States, Groupe Lactalis in France, and Fonterra in New Zealand (Clay, Garnett, & Lorimer, 2019). These firms supply BMS manufacturers with raw or processed ingredients, or even package final products (Coriolis, 2014), integrated into global supply chains. For example, New Zealand dry milk powder exports rapidly expanded following its 2008 bilateral trade agreement with China, which by 2012 comprised 30% of all exports to that country (Galtry, 2013; Gao, 2016). World production of vegetable oils, another key milk formula ingredient, has also massively expanded in recent decades (Hawkes, 2010).
The baby food manufacturing sector has also evolved in important ways to drive global supply. A small number of transnational corporations, originating in either the food or pharmaceutical sectors of Europe and the United States, dominate milk formula manufacturing and own the major brands. According to Euromonitor data, just five controlled 57% of global market share in 2018: Nestlé (Switzerland), Danone (France), Reckitt Benckiser (UK; recently acquired Mead Johnson Nutrition), Abbott Laboratories (US) and Royal FreislandCampina (Netherlands). These ‘Big Formula’ companies are the end result of intensive merger and acquisition activity over recent decades, with most markets controlled by a small number of these players. A small number of ‘residual’ firms have important market shares at regional or country levels, for example Hipp in Germany and Eastern Europe, Meiji and Morinaga in Japan, and Vinamilk in Vietnam. China is the exception, where intense competition between a mix of many transnational and home‐grown companies is underway (Coriolis, 2014).
Although Big Formula companies have long‐established global operations, they expanded into emerging middle‐income country markets with renewed vigour from the early‐2000s onwards in pursuit of new growth opportunities, in the context of declining sales in their home HIC markets and enabled by trade liberalization. The expansion and growth of the industry is reflected in rapid global sales growth from ~US$1.5 billion in 1978, rising to ~US$4 billion in 1983 (Post, 1985), US$22.9 billion in 2005 and US$55.6 billion in 2019. This represents a ~ 36‐fold increase over a 40‐year period, and a doubling since 2005. Prior to the adoption of The Code in 1981, an ‘infant formula’ category marketed for birth onwards dominated the market. Almost immediately following The Code's adoption, companies expanded their product range to include follow‐up, toddler and other categories marketed for infants/children beyond 6 months (Changing Markets Foundation, 2017). Since then these categories have become crucial to industry revenues to the extent that in 2017, toddler formula was the highest value category with $US19 billion in sales, followed by standard (US$14 billion), follow‐up ($US10 billion), and special formula (US$4 billion) (Passport Global Market Information Database, 2019).
Transformations in the distribution of BMS are also relevant. Besides health systems, the main milk formula distribution channels are pharmacies, supermarkets, discounters and online stores. The liberalization of trade in retail services has spurred the ‘supermarketization’ of developing countries since the late 1990s, creating new opportunities to market baby food products to urban consumers with rising incomes (Baker et al., 2016). Supermarketisation links with a product differentiation and line extension marketing strategy, because by expanding product ranges in these ways, companies can acquire more shelf space in supermarkets and pharmacies, further promoting product visibility and sales (Piwoz & Huffman, 2015). Online and in‐store retailers often violate The Code, by price‐discounting or running in‐store promotions to move stock. Large supermarket chains, for example Walmart in the United States, have developed their own formula brands under ‘home’ labels manufactured by contracted suppliers.
Another key distribution channel in some countries and especially in China, is the black market, which may explain the remarkably high per capita volumes we observed in some countries. For example, sophisticated Daigou (meaning ‘grey channel’) operations have been established in Australia, New Zealand, the UK and Germany whereby shoppers purchase well known branded products for export (usually in small shipments or in suitcases) to China. This channel has become so significant that Daigou sales were equivalent to half of what foreign companies were selling in the formal Chinese market in 2014 (Changing Markets Foundation, 2017). A final but important distribution channel are the large volumes of BMS donated by companies during emergencies, often to humanitarian relief organizations and well in excess of actual need (Carothers, & Gribble, 2014). This raises serious concern, given the high morbidity and mortality rates reported in formula‐fed infants during emergencies (Adhisivam, Srinivasan, Soudarssanane, Deepak Amalnath, & Nirmal Kumar, 2006; Binns et al., 2012; Hipgrave, Assefa, Winoto, & Sukotjo, 2012). It is especially relevant to South East Asia, as the most disaster‐prone region in the world (Baker et al., 2016; Binns et al., 2012).
3.2.3. First‐food environment transformations
First‐food environments are the contexts in which mothers and caregivers make IYCF decisions, including healthcare, retail, workplace, community and household settings, and the extent to which these promote, support or undermine breastfeeding relative to BMS and other foods.
Healthcare settings are a key feature of first‐food environments. Here, the medicalisation of pregnancy, birthing and post‐natal care is highly relevant, as these practices have become increasingly managed in clinical settings by healthcare specialists trained under a biomedical paradigm (Benyamini, Molcho, Dan, Gozlan, & Preis, 2017). Multiple studies report IYCF knowledge and skills deficits among healthcare professionals, limited consideration in medical curricula, and apathy towards breastfeeding in hospital settings (Dykes, 2006; Gavine et al., 2017; World Health Organization, 2017b). In‐hospital feeding of infant formula, including the use of pre‐lacteal feeds, appears to be widely practiced, associating with early cessation of breastfeeding and subsequent formula feeding (Nguyen, Withers, Hajeebhoy, & Frongillo, 2016). Medicalization also involves pathologising normal biological processes and medical intervention. Delivery of births by caesarean‐section is a form of medicalisation, associated with reduced breastfeeding initiation (Prior et al., 2012). A background caesarean‐section delivery rate of 10–15% is considered acceptable for obstetric complications; yet rates of >25% are common in HICs, and have increased to higher levels elsewhere, especially in Latin America and East Asia. The rate among urban mothers in China, for example, rose from 10% in 1988 to 64% in 2008 (Feng, Xu, Guo, & Ronsmans, 2012). Hospitals and other clinical settings are also a key BMS marketing channel, with formula marketed directly to health professionals for many decades (see marketing).
Portrayals of IYCF in traditional and digital media is also a feature of first‐food environments, which can undermine breastfeeding and promote BMS. In UK television and newspaper media, for example, bottle‐feeding has featured more often and as less problematic than breastfeeding (Henderson, Kitzinger, & Green, 2000). In US parenting magazines, bottle‐feeding and breastfeeding were portrayed with near equal frequency. Messages placed responsibility for infant feeding with mothers, and much less with partners and societal responsibility (Frerichs, Andsager, Campo, Aquilino, & Dyer, 2006). In contrast, civil society groups and movements have fostered pro‐breastfeeding beliefs and norms (Boyer, 2011; Jelliffe & Jelliffe, 1978). From the 1960s onwards, the growth of the La Leche League and kindred organizations providing breastfeeding information, peer‐support and advocacy, is attributed to improved breastfeeding rates in (mostly) high‐income countries (Jelliffe & Jelliffe, 1978; Ryan, 1997b). Since the 1970s, the International Baby Food Action Network (IBFAN) has raised the social salience of commerciogenic malnutrition, and conducted crucial corporate accountability functions including Code monitoring, training, publishing model laws and implementation guidance (Arendt & Allain, 2019; International Baby Food Action Network & International Code Documentation Center, 2017; Richter, 2001). Newer civil society initiatives (Michaud‐Létourneau et al., 2019; Michaud‐Létourneau, Gayard, & Pelletier, 2019; Zehner, 2016), and the Global Breastfeeding Collective, & Code monitoring efforts led by WHO and UNICEF (Bégin et al., 2019), also provide these norm‐promotion functions. Mothers breastfeeding movements have emerged in some countries, involving public acts of breastfeeding and other forms of ‘care‐work activism’ (Boyer, 2011).
Intensive and increasingly sophisticated BMS marketing is a dominant feature of first‐food environments, especially in the absence of legislated marketing restrictions. Marketing helps companies to shift social norms and attitudes about what IYCF practices are considered normal, acceptable and socially desirable (Piwoz & Huffman, 2015), while differentiating their products in competitive markets (Changing Markets Foundation, 2017). Long‐standing evidence shows that exposure to BMS marketing undermines breastfeeding initiation, duration and exclusivity, and diminishes the confidence of mothers in their ability to breastfeed (Bergevin, Dougherty, & Kramer, 1983; Rosenberg, Eastham, Kasehagen, & Sandoval, 2008; Sobel et al., 2011). Studies on global BMS marketing expenditures are unavailable. However, we make a conservative estimate of ~3–10% of sales (Changing Markets Foundation, 2017; Coriolis, 2014), equivalent to a global BMS marketing spend of between US$1.68 and US$5.56 billion in 2019. These amounts likely far outweigh expenditures on breastfeeding promotion by governments and international organizations (Piwoz & Huffman, 2015). The baby food industry has pursued a range of strategies across the entire marketing mix to grow and sustain their markets – product design, pricing, promotion and advertising, placement and public relations.
A foundational strategy is marketing through health systems. Strong evidence implicates BMS marketing targeted at health professionals and mothers during and after the perinatal period with reduced breastfeeding initiation, duration and exclusivity (Rollins et al., 2016). Health professionals – paediatricians, obstetricians, gynaecologists, allergists, nurses, midwives, dietitians, lactation consultants and nutritionists – are often trusted sources of IYCF advice (The Nielsen Company, 2015). Hence, companies make large investments in their capabilities to engage them in clinical settings. For example, Mead Johnson (now RB Mead Johnson) had a global salesforce of 1,900 employees in 2010, of which 1,350 (71%) were dedicated to selling to health professionals, and the remaining 550 (29%) to pharmacy and supermarket retailers (Coriolis, 2014). Sales techniques used across the industry have included direct engagement in clinical settings and hospital procurement offices; funding new neonatal wards and equipment in return for branding privileges; providing free or low‐cost samples for maternity discharge packs; providing branded gifts (e.g. lanyards, notepads); paid advertising in professional journals; sponsoring professional associations (e.g. scholarships, grants and other awards); and ‘educational interfaces’ including sponsoring professional education programmes, publications and conferences (Coriolis, 2014; Grummer‐Strawn, Holliday, Tabea Jungo, & Rollins, 2019; Piwoz & Huffman, 2015).
The provision of free samples for inclusion in maternity discharge packs is a key strategy (Piwoz & Huffman, 2015). This implies hospital and health professional endorsement (Rosenberg et al., 2008; Thorley, 2015), associates with reduced in‐hospital exclusive breastfeeding and out‐of‐hospital breastfeeding duration (Rosenberg et al., 2008; Sadacharan, Grossman, Matlak, & Merewood, 2014; Tarrant et al., 2015). It appears to be extensively practiced in the United States especially (Merewood et al., 2010; Save the Children, 2013b). For example, one 2010 study found that of 3,209 hospitals surveyed 91% had distributed infant formula in sponsored discharge packs (Merewood et al., 2010). Studies in other countries are limited. However, one 2012 evaluation in China found 40% of new mothers had received free samples, of which 61% were provided directly by company sales representatives and one third by health professionals (Save the Children, 2013b).
Health care professionals also play a key role in the marketing of special formulas (therapeutic milks), sold over the counter or by prescription for medically diagnosed conditions affecting a small proportion of the infant population (van Tulleken, 2018). Among others, these include formulas for premature babies, anti‐regurgitation, anti‐diarrhoea, allergy treatment and prevention, and impaired renal function (Changing Markets Foundation, 2017; Martin, Ling, & Blackburn, 2016). Prescribing behaviours are in‐turn shaped by research activities, clinical guideline development, medical education and public awareness – all activities which companies influence. Hence, industry‐driven over‐diagnosis at least partly explains our observation of high special formula sales growth in certain countries. For example, in the UK prescriptions of special formula for infants with cows‐milk protein allergy (CMPA) increased 500% from 105,029 in 2006 to over 600,000 in 2016, a rate greatly exceeding any credible change in prevalence. This occurred alongside a ~ 700% increase in expenditure on these products by the National Health Service from £8.1 million to >£60 million. In this context it is noteworthy that the baby food industry funded the first international guidelines on CMPA in 2007 and revisions in 2010, with most authors involved in developing these and other guidelines declaring prior industry funding (van Tulleken, 2018).
A second key strategy is direct‐to‐consumer marketing. This has occurred through traditional channels including advertisements in parenting magazines, television, and in‐store retail displays (Choi et al., 2019; Piwoz & Huffman, 2015), and increasingly through digital channels including social media platforms, online parenting forums, mobile apps for new and expecting parents, reward programmes and sponsored parenting blogs (Abrahams, 2012; Harris, Fleming‐Milici, & Frazier, 2016; Piwoz & Huffman, 2015). Marketing messages often portray BMS as a symbol of modernity, as equivalent with or superior to breast milk, and formula‐feeding as extensively practised and as an appropriate lifestyle choice (Mejia, Seklir, Gardin, & Nixon, 2016; Piwoz & Huffman, 2015). Evidence suggests this is highly effective in shaping beliefs. For example, one recent United States survey found 52% of infant caregivers agreed with the statement that infant formula can be better for babies' digestion and brain development than breastmilk; 62% that it can provide nutrition not present in breastmilk (Romo‐Palafox, Pomeranz, & Harris, 2020). Messaging also interacts with the socio‐cultural factors mentioned earlier, for example, by promoting positive values such as ‘freedom from judgement’ and by appealing to the emotional and psychological aspects of parenting and parental aspirations, such as scholastic achievement (Mejia et al., 2016).
Another key feature of direct‐to‐consumer marketing are product strategies, reflected in the marked increase in the variety of product types available on markets worldwide (Changing Markets Foundation, 2017). These strategies are intended to drive new sales growth by inventing entirely new product categories, differentiating products in competitive markets, and raising prices through premiumisation.
First, is a combined product line extension and cross‐promotion strategy. From the mid‐1980s onwards, companies extended their BMS product ranges beyond standard formula to include follow‐up, toddler and other age‐specific categories beyond six months (Changing Markets Foundation, 2017; Pereira, Ford, & Feeley, 2016). These latter products are often branded, packaged and labelled in similar ways, and are thereby frequently mistaken by parents and caregivers for standard formula (Pereira et al., 2016). In Australia and Italy, for example, 67% and 81% of mothers surveyed reported having seen an infant formula advertisement respectively, despite the legal non‐existence of such advertisements (Berry, Jones, & Iverson, 2010; Berry, Jones, & Iverson, 2012; Cattaneo et al., 2015). Many specialised formulas also have similar branding and packaging, which can cause health professional and consumer confusion, thereby increasing the risk of feeding unsuitable or unsafe products (Changing Markets Foundation, 2017; Crawley, Westland, & Weston, 2017). By using cross‐promotion, companies can boost brand loyalty across the entire BMS product range, and indirectly promote standard formula in countries where legislation prohibits this (Changing Markets Foundation, 2017; Coriolis, 2014). Companies have gone even further with ‘womb‐to‐tomb’ cross‐promotion, by developing formula products for pregnant and lactating mothers, adolescents, and the elderly. The latter often play a key role in infant and child care as grandparents, and hence influence BMS purchasing decisions (Changing Markets Foundation, 2017).
Another strategy is product differentiation through the development of novel products with content claims and implied or direct health claims, often on premium or specialised products that sell for markedly higher prices (Changing Markets Foundation, 2017). Although such products have existed since the 1950s, the range of products has expanded markedly in recent decades. Claims made on product labels include those relating to brain, eye and immune system development, reduced allergies, and common infant behaviours such as spitting‐up, gas, fussiness, crying and sleeplessness (Belamarich, Bochner, & Racine, 2016; Stang, Hoss, & Story, 2010). Many of these claims are not supported by scientific evidence (Pomeranz, Romo Palafox, & Harris, 2018). Most are related to added functional ingredients claimed to mimic breastmilk (e.g. DHA, probiotics or prebiotics) or as linked to specific outcomes (e.g. hydrolysed protein to prevent milk protein allergy), or by reformulating existing ingredients (e.g. reduced lactose) (Belamarich et al., 2016). Companies have also developed novel delivery products that appeal to convenience and life‐style aspirations, such as Nestlé's BabyNes capsule machine, which dispenses ready‐to‐drink milk in age‐specific servings that sell for markedly higher per unit prices than regular formula (Changing Markets Foundation, 2017).
3.2.4. Policy and regulatory drivers
Wide variations in worldwide milk formula sales also reflect differences in the strength of IYCF policy and regulatory frameworks across countries. Multiple synergistic actions are needed to promote, support and protect breastfeeding (Pérez‐Escamilla et al., 2012; Robinson, Buccini, Curry, & Perez‐Escamilla, 2019; Rollins et al., 2016). We focus on several crucial policy and regulatory frameworks shaping first‐food systems,and most relevant to BMS.
First, is the regulation of BMS marketing. The Code sets out provisions for adoption by WHO member countries into national law, as a minimum requirement for preventing inappropriate marketing (World Health Organization, 1981). Manufacturers and distributors are also requested to monitor their marketing practices and comply with these provisions (World Health Organization, 1981). The latest monitoring report found 136 (70%) of 194 reporting countries had adopted at least some provisions of The Code into national law. However, just 25 (13%) were substantially aligned with The Code, 42 (22%) moderately aligned, 69 (36%) had included at least some provisions, and 58 (30%) had adopted no provisions whatsoever (World Health Organization, UNICEF,, & IBFAN, 2020). Major dairy and baby food producing nations, such as the United States, Australia and New Zealand, have adopted no provisions into law. There are major gaps in coverage. Of countries with legal measures in place, 79 (41%) prohibited promotion in health facilities, 51 (26%) the provision of free or low‐cost supplies, and 19 (10%) health professional or scientific meeting sponsorship; 114 (59%) restricted advertising to the general public, 112 (58%) pictures or text idealizing formula‐feeding, and 50 (26%) nutrition and health claims (World Health Organization et al., 2020). Compliance with The Code is highest in Europe and the Eastern Mediterranean, and lowest in the Western Pacific and Americas (World Health Organization, UNICEF, & IBFAN, 2018).
The World Health Assembly adopted Resolution 69.9 in 2016, welcoming new WHO technical guidance clarifying the definition of BMS covers any milk products marketed for ages 6–36 months, including follow‐up and toddler milks (World Health Organization, 2016). As of 2018, however, only 76 countries restricted the marketing of BMS up to or beyond the first year of life, and just 31 covered products up to 36 months of age (World Health Organization et al., 2020). Subsequently, the promotion of follow‐up and toddler milks is allowed in the large majority of countries, and manufacturers have exploited this legislative gap. In Australia, for example, print advertisements for infant formula nearly disappeared in the late 1970s (just prior to adoption of The Code), while those for toddler milks have increased significantly (Smith & Blake, 2013). In the United States, advertising expenditures on toddler milks increased four‐fold between 2006 and 2015, and the sales volume increased 2.6‐fold, while advertising spending and sales of standard formula declined (Choi et al., 2019).
Even where legal restrictions are in place, violations of The Code are common in all country contexts (Changing Markets Foundation, 2017; International Baby Food Action Network & International Code Documentation Center, 2017; Zehner, 2016). Internet marketing channels, including social media, are new areas of non‐compliance (International Baby Food Action Network & International Code Documentation Center, 2017; Save the Children, 2013a). Compliance is undermined by weak or non‐existent monitoring and compliance mechanisms; just 82 (42%) countries with any provisions of The Code in place define sanctions for violators (World Health Organization et al., 2020). Companies such as Danone and Nestlé have policies in place to comply with some provisions of The Code. However, these can be misapplied or ignored by company subsidiaries operating at national and regional levels, where violations are often reported. In terms of the products covered by the companies' own policies, none comply with the WHA Resolution 69.9 product scope of 0–36 months (Access to Nutrition Foundation, 2018).
Second, compatibility of breastfeeding with maternal employment likely explains some of the differences in milk formula sales across countries. A 2015 systematic review involving 25 studies across 19 countries, found maternal employment was the most frequently reported barrier to exclusive breastfeeding (Balogun, Dagvadorj, Anigo, Ota, & Sasaki, 2015). Length of maternity leave post‐partum and time of return to work is associated with longer duration of exclusive breastfeeding in countries with high formal employment (Baker & Milligan, 2008; Ogbuanu, Glover, Probst, Liu, & Hussey, 2011). In the context of absent or ineffective maternity protection policies and workplace entitlements, formula‐feeding can be the only choice if the alternative results in loss of employment and income. In countries where women comprise a high share of the informal workforce, maternity protection is often lacking or laws unenforced. This is especially applicable to China, Latin America and Sub‐Saharan Africa where almost half of all informal workers are women (Bhan et al., 2020). Among all working women worldwide 830 million (68%) do not have adequate maternity protection, of whom 80% live in Africa and Asia (International Labour Organization, 2014).
The Maternity Protection Convention (MPC) of the International Labour Organization (ILO) protects against maternity discrimination and provides for paid maternity leave for a minimum of 14 but preferably 18 weeks at two‐thirds of earnings. This is below the 24 weeks (6 months) WHO recommended duration for exclusive breastfeeding, hence representing an area of international policy incoherence. The MPC provides for the right to continue breastfeeding on return to work, paid nursing breaks, and access to appropriate and hygienic nursing facilities. A 2014 ILO report found most countries in Asia (81%), the Middle East (92%), and Latin America (79%) fail to meet the minimum leave and earnings standards. Just 31% of countries have legislated the mandatory provision of nursing facilities (International Labour Organization, 2014). The United States stands out as the only HIC without any national maternity protection scheme in place. Worldwide, only 41% of women with newborns received a cash benefit providing them with income security after childbirth, ranging from 81% in Europe and Central Asia, to 69% in the Americas, 33% in the Asia Pacific and just 16% in Africa (International Labour Organization, 2017).
Third, policies in hospitals and other clinical settings are crucial. The UNICEF/WHO Baby Friendly Hospitals Initiative (BFHI) was launched in 1991 to promote, protect and support breastfeeding in maternity facilities worldwide. This enables national breastfeeding authorities to designate maternity facilities as ‘baby friendly’ when the facility does not accept free or low‐cost BMS, feeding bottles or teats, and has implemented the Ten Steps to Successful Breastfeeding (Ten Steps). It represents a key initiative resisting inappropriate BMS marketing to health professionals. Evidence shows the BFHI has had a significant positive effect on exclusive breastfeeding rates at national and global levels, including a dose–response relationship between the number of Ten Steps women are exposed to and breastfeeding initiation and duration (Pérez‐Escamilla, Martinez, & Segura‐Pérez, 2016; Spaeth, Zemp, Merten, & Dratva, 2018). Worldwide as of 2016, just 10% of newborns were born in ‘baby‐friendly’ designated facilities. This varies markedly from 36% in Europe to 17% in the Eastern Mediterranean, 13% in the Americas, 11% in the Western Pacific, 4% in Africa and 3% in South East Asia. Weak BFHI implementation is hampered by funding constraints, lack of buy‐in and apathy about breastfeeding among health professionals, and limited national implementation of The Code (World Health Organization, 2017b).
3.3. Limitations
Our analysis has several limitations. First, the milk formula categories used are Euromonitor definitions and do not capture the wider range of product categories that exist in reality. For example, RB Mead Johnson's Enfamil brand also includes products for newborns (0‐3 m), all infants (0‐12 m) and for a narrower toddler age band (9‐18 m). Furthermore, we have not captured teats, bottles and other feeding apparatus, which are also captured in The Code, and can undermine breastfeeding when marketed inappropriately. Second, the Euromonitor data has similar limitations to official government statistics and is not a scholarly database. Sales data do not capture products sold through informal channels or wastage. From a nutritional standpoint, the data have not been validated, for example, by comparison to survey data. However, it does have some advantages. Unlike survey data, it is not subject to recall bias, and is consistently reported across all countries over time using standardized measures (Baker et al., 2020).
Third, we reported very high special formula sales in the US, but low toddler milk sales, a possible inaccuracy. This may reflect the lack of a regulatory definition for toddler milks in the US, and weak regulations allowing a wide range of health and nutrition claims to be made on product labels (Harris & Pomeranz, 2020), and hence the designation of many toddler milks as special formulas. Finally, this analysis does not provide a complete picture of first‐food systems transformations and IYCF transitions. We have not reported other key IYCF indicators, including global breastfeeding trends and dynamics. Furthermore, we have omitted a crucial topic – the power of Big Formula to shape first‐food systems in their entirety – including the political practices (e.g. lobbying, political financing and policy substitution) used to undermine implementation of The Code (Baker, 2020). This requires further analysis.
4. CONCLUSION
We find that an infant and young child feeding transition to diets higher in commercial milk formulas is underway, and expected to continue apace. This transition is occurring in all country‐contexts, but growth is most rapid in lower‐ and upper‐middle income countries, home to the world's largest infant and child populations. There have been substantial increases in total and per child sales volumes in the follow‐up, toddler and special milk formula categories especially. The transition is therefore affecting an unprecedented number of infants and young children, spanning a wider range of age groups and product categories. These findings raise major concern and identify barriers for improving newborn, child and maternal health, given the known health promoting effects of breastfeeding, and evidence of the adverse health, economic and environmental outcomes associated with not breastfeeding. This also indicates that infant and young child diets are becoming increasingly commodified and more highly processed, a trend mirrored by the growing worldwide consumption of ultra‐processed foods (Baker et al., 2020).
Infant and young child feeding is often portrayed as an individual behaviour, as a matter of free parental choice, and the responsibility of mothers and parents alone. Our findings present a counter‐view – feeding decisions are powerfully shaped by transformations underway in first‐food systems, associated with the globalization of the baby food industry and its marketing practices, processes of medicalisation and limited support for breastfeeding among healthcare professionals, and the shift of labour and production out of the home, in the context of weak or absent maternity protection and breastfeeding support. Existing regulations intended to protect the health of children and mothers and to prevent unethical formula marketing are inadequate or not working effectively in these new contexts – renewed efforts towards the implementation, monitoring and enforcement of The Code, including stronger accountability mechanisms for governments and industry are urgently needed.
More specifically, actions are needed to broaden the coverage of BMS marketing regulations in many countries – to include products marketed for consumption between the ages of 0–36 months, end cross‐promotion, limit marketing via health systems through implementation of the Baby Friendly Hospital Initiative, and by restricting direct‐to‐consumer advertising. Actions are also needed to curtail interactions between baby food companies and health professionals, including conflicts of interest in IYFC guideline development (World Health Organization, 2016). Other key actions include expanding maternity protection and workplace entitlements, mainstreaming IYCF training for health professionals, and scaling‐up breastfeeding support and counselling services (Pérez‐Escamilla et al., 2012; World Health Organization & UNICEF, 2003). These and other actions to promote, support and protect breastfeeding can only come about through greater political priority and investments in the health of children and mothers. This includes mobilizing civil society coalitions, strategic advocacy, and other society‐wide efforts to fulfil the rights and entitlements of mothers and children (Arendt & Allain, 2019; Bégin et al., 2019; Clark et al., 2020; Michaud‐Létourneau, Gayard, Mathisen, et al., 2019).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
PB conceived the study with co‐authors, developed the method, and wrote the first draft of the manuscript; TMS, PAN, PM and PB conducted the data analysis; all authors contributed input into draft iterations, and approved the final version of the manuscript.
Supporting information
Table S1. Commercial milk formula category definitions*
Table S2. Included countries by World Bank income level and UNICEF region
Figure S1. Total commercial BMS sales volumes for all countries combined, 2005–19 with projections to 2024
Figure S2. World dry milk production by region, 1961–2014
ACKNOWLEDGMENTS
This work was supported by funding from the Department of Maternal, Newborn, Child and Adolescent Health, World Health Organization (WHO). The views expressed in this articles are those of the authors, and do not necessarily reflect those of the funder (WHO). We kindly thank David Clark (UNICEF) and Roger Mathisen (FHI 360) for their helpful suggestions for improving this manuscript.
Baker P, Santos T, Neves PA, et al. First‐food systems transformations and the ultra‐processing of infant and young child diets: The determinants, dynamics and consequences of the global rise in commercial milk formula consumption. Matern Child Nutr. 2021;17:e13097. 10.1111/mcn.13097
[Correction added on 13 November 2020 after its first online publication. The affiliations of the two authors have been amended in this version.]
REFERENCES
- Abrahams, S. W. (2012). Milk and social media: online communities and the International Code of Marketing of Breast‐milk Substitutes. Journal of Human Lactation, 28(3), 400–406. 10.1177/0890334412447080 [DOI] [PubMed] [Google Scholar]
- Access to Nutrition Foundation . (2018). Access to Nutrition Index Global Index 2018. Retrieved from https://accesstonutrition.org/index/global-index-2018/
- Adhisivam, B. , Srinivasan, S. , Soudarssanane, M. , Deepak Amalnath, S. , & Nirmal Kumar, A. (2006). Feeding of infants and young children in tsunami affected villages in Pondicherry. Indian Pediatrics, 43(8), 724–727. [PubMed] [Google Scholar]
- Arendt, M. , & Allain, A. (2019). Annelies Allain: Pioneer of the International Code of Marketing of Breastmilk Substitutes. Journal of Human Lactation, 35(1), 15–20. 10.1177/0890334418812075 [DOI] [PubMed] [Google Scholar]
- Baker, M. , & Milligan, K. (2008). Maternal employment, breastfeeding, and health: Evidence from maternity leave mandates. Journal of Health Economics, 27(4), 871–887. 10.1016/j.jhealeco.2008.02.006 [DOI] [PubMed] [Google Scholar]
- Baker, P. (2020). Breastfeeding, first food systems and corporate power. Breastfeeding Review, 28(2), 33. [Google Scholar]
- Baker, P. , & Friel, S. (2016). Food systems transformations, ultra‐processed food markets and the nutrition transition in Asia. Globalization and Health, 12(1), 80. 10.1186/s12992-016-0223-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, P. , Kay, A. , & Walls, H. (2014). Trade and investment liberalization and Asia's noncommunicable disease epidemic: a synthesis of data and existing literature. Globalization and Health, 10(1), 66. 10.1186/s12992-014-0066-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, P. , Machado, P. , Santos, T. , Sievert, K. , Backholer, K. , Hadjikakou, M. , … Lawrence, M. (2020). Ultra‐processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obesity Reviews, n/a–n/a. 10.1111/obr.13126 [DOI] [PubMed] [Google Scholar]
- Baker, P. , Smith, J. , Salmon, L. , Friel, S. , Kent, G. , Iellamo, A. , … Renfrew, M. J. (2016). Global trends and patterns of commercial milk‐based formula sales: is an unprecedented infant and young child feeding transition underway? Public Health Nutrition, 19(14), 2540–2550. 10.1017/s1368980016001117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balogun, O. O. , Dagvadorj, A. , Anigo, K. M. , Ota, E. , & Sasaki, S. (2015). Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Maternal & Child Nutrition, 11(4), 433–451. 10.1111/mcn.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bégin, F. , Lapping, K. , Clark, D. , Taqi, I. , Rudert, C. , Mathisen, R. , & Stathopoulos, Z. (2019). Real‐time evaluation can inform global and regional efforts to improve breastfeeding policies and programmes. Maternal & Child Nutrition, 15(S2), e12774. 10.1111/mcn.12774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belamarich, P. F. , Bochner, R. E. , & Racine, A. D. (2016). A critical review of the marketing claims of infant formula products in the United States. Clinical Pediatrics, 55(5), 437–442. 10.1177/0009922815589913 [DOI] [PubMed] [Google Scholar]
- Benyamini, Y. , Molcho, M. L. , Dan, U. , Gozlan, M. , & Preis, H. (2017). Women's attitudes towards the medicalization of childbirth and their associations with planned and actual modes of birth. Women and Birth, 30(5), 424–430. 10.1016/j.wombi.2017.03.007 [DOI] [PubMed] [Google Scholar]
- Bergevin, Y. , Dougherty, C. , & Kramer, M. S. (1983). Do infant formula samples shorten the duration of breast‐feeding? Lancet, 1(8334), 1148–1151. 10.1016/s0140-6736(83)92878-7 [DOI] [PubMed] [Google Scholar]
- Berry, N. J. , Jones, S. , & Iverson, D. (2010). It's all formula to me: women's understandings of toddler milk ads. Breastfeeding Review, 18(1), 21–30. [PubMed] [Google Scholar]
- Berry, N. J. , Jones, S. C. , & Iverson, D. (2012). Toddler milk advertising in Australia: Infant formula advertising in disguise? Australasian Marketing Journal, 20(1), 24–27. 10.1016/j.ausmj.2011.10.011 [DOI] [Google Scholar]
- Bhan, G. , Surie, A. , Horwood, C. , Dobson, R. , Alfers, L. , Portela, A. , & Rollins, N. (2020). Informal work and maternal and child health: a blind spot in public health and research. Bulletin of the World Health Organization, 98(3), 219–221. https://dx.doi.org/10.2471%2FBLT.19.231258, 10.2471/BLT.19.231258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binns, C. W. , Lee, M. K. , Tang, L. , Yu, C. , Hokama, T. , & Lee, A. (2012). Ethical issues in infant feeding after disasters. Asia‐Pacific Journal of Public Health, 24(4), 672–680. 10.1177/1010539512453253 [DOI] [PubMed] [Google Scholar]
- Boyer, K. (2011). "The way to break the taboo is to do the taboo thing" breastfeeding in public and citizen‐activism in the UK. Health & Place, 17(2), 430–437. 10.1016/j.healthplace.2010.06.013 [DOI] [PubMed] [Google Scholar]
- Carothers, C. , & Gribble, K. (2014). Infant and young child feeding in emergencies. Journal of Human Lactation, 30(3), 272–275. 10.1177/0890334414537118 [DOI] [PubMed] [Google Scholar]
- Cattaneo, A. (2012). Academy of breastfeeding medicine founder's lecture 2011: inequalities and inequities in breastfeeding: an international perspective. Breastfeeding Medicine, 7(1), 3–9. 10.1089/bfm.2012.9999 [DOI] [PubMed] [Google Scholar]
- Cattaneo, A. , Pani, P. , Carletti, C. , Guidetti, M. , Mutti, V. , Guidetti, C. , & Knowles, A. (2015). Advertisements of follow‐on formula and their perception by pregnant women and mothers in Italy. Archives of Disease in Childhood, 100(4), 323–328. 10.1136/archdischild-2014-306996 [DOI] [PubMed] [Google Scholar]
- Changing Markets Foundation . (2017). How milk formula companies are putting profits before science. In. Brussels, New York.
- Choi, Y. , Ludwig, A. , & Harris, J. (2019). US toddler milk sales and associations with marketing practices. Public Health Nutrition, 23(6), 1127–1135. 10.1017/S1368980019003756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, H. , Coll‐Seck, A. M. , Banerjee, A. , Peterson, S. , Dalglish, S. L. , Ameratunga, S. , … Claeson, M. (2020). A future for the world's children? A WHO–UNICEF–Lancet Commission. The Lancet, 395(10224), 605–658. 10.1016/S0140-6736(19)32540-1 [DOI] [PubMed] [Google Scholar]
- Clay, N. , Garnett, T. , & Lorimer, J. (2019). Dairy intensification: Drivers, impacts and alternatives. Ambio, 49, 1–14. 10.1007/s13280-019-01177-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coriolis . (2014). Understanding the infant formula value chain. Retrieved from https://coriolisresearch.com/pdfs/coriolis_dairy_infant_formula_value_chain.pdf
- Crawley, H. , Westland, S. , & Weston, S. (2017). Specialised infant milks in the UK: infants 0–6 months – Information for health professionals. Retrieved from http://www.firststepsnutrition.org/pdfs/Specialised_infant_milks_March2017.pdf
- Development Initiatives . (2020). Global Nutrition Report 2020. Bristol: Development Initiatives Poverty Research. [Google Scholar]
- Dykes, F. (2006). The education of health practitioners supporting breastfeeding women: time for critical reflection. Maternal & Child Nutrition, 2(4), 204–216. 10.1111/j.1740-8709.2006.00071.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmond, K. , Newton, S. , Hurt, L. , Shannon, C. S. , Kirkwood, B. R. , Taneja, S. , … Bahl, R. (2016). Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. The Lancet Global Health, 4(4), e266–e275. 10.1016/s2214-109x(16)00040-1 [DOI] [PubMed] [Google Scholar]
- Euromonitor International . (2013). Baby Food: Unveiling global growth drivers and premiumisation strategies. Retrieved from https://www.euromonitor.com/baby-food-unveiling-global-growth-drivers-and-premiumisation-strategies/report
- Feng, X. L. , Xu, L. , Guo, Y. , & Ronsmans, C. (2012). Factors influencing rising caesarean section rates in China between 1988 and 2008. Bulletin of the World Health Organization, 90(1), 30–39, 39a. 10.2471/blt.11.090399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Agriculture Organization of the United Nations . (2019). FAOSTAT. Retrieved from http://www.fao.org/faostat/en/
- Frerichs, L. , Andsager, J. L. , Campo, S. , Aquilino, M. , & Dyer, C. S. (2006). Framing breastfeeding and formula‐feeding messages in popular US magazines. Women & Health, 44(1), 95–118. 10.1300/j013v44n01_06 [DOI] [PubMed] [Google Scholar]
- Galtry, J. A. (2013). Improving the New Zealand dairy industry's contribution to local and global wellbeing: the case of infant formula exports. The New Zealand Medical Journal, 126(1386), 82–89. https://pubmed.ncbi.nlm.nih.gov/24316995/ [PubMed] [Google Scholar]
- Gao, H. S. (2016). China‐New Zealand free trade agreement. In Lester S. & Mercurio B. (Eds.), Bilateral and Regional Trade Agreements: Case Studies (pp. 79–96). Cambridge: Cambridge University Press. Retrieved from. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2728863 [Google Scholar]
- Gavine, A. , MacGillivray, S. , Renfrew, M. J. , Siebelt, L. , Haggi, H. , & McFadden, A. (2017). Education and training of healthcare staff in the knowledge, attitudes and skills needed to work effectively with breastfeeding women: a systematic review. International Breastfeeding Journal, 12(1), 6–10. 10.1186/s13006-016-0097-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, A. (2016). “I … don't want to see you flashing your bits around”: Exhibitionism, othering and good motherhood in perceptions of public breastfeeding. Geoforum, 71, 52–61. 10.1016/j.geoforum.2016.03.004 [DOI] [Google Scholar]
- Grayson, J. (2016). Unlatched: The evolution of breastfeeding and the making of a controversy. New York: Harper Collins. [Google Scholar]
- Grigg, D. (1999). The changing geography of world food consumption in the second half of the twentieth century. Geographical Journal, 165, 1–11. https://pubmed.ncbi.nlm.nih.gov/20662185/. 10.2307/3060507 [DOI] [PubMed] [Google Scholar]
- Grummer‐Strawn, L. , Holliday, F. , Tabea Jungo, K. , & Rollins, N. (2019). Sponsorship of national and regional professional paediatrics associations by companies that make breast‐milk substitutes: evidence from a review of official websites. BMJ Open, 9, e029035. 10.1136/bmjopen-2019-029035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad, L. , Hawkes, C. , Waage, J. , Webb, P. , Godfray, C. , & Toulmin, C. (2016). Food systems and diets: Facing the challenges of the 21st century. Retrieved from https://glopan.org/sites/default/files/ForesightReport.pdf
- Hannan, A. , Li, R. , Benton‐Davis, S. , & Grummer‐Strawn, L. (2005). Regional variation in public opinion about breastfeeding in the United States. Journal of Human Lactation, 21(3), 284–288. 10.1177/0890334405278490 [DOI] [PubMed] [Google Scholar]
- Harris, J. , Fleming‐Milici, F. , & Frazier, W. (2016). Baby food FACTS: Nutrition and marketing of baby and toddler food and drinks. Retrieved from http://www.uconnruddcenter.org/files/Pdfs/BabyFoodFACTS_FINAL.pdf
- Harris, J. L. , & Pomeranz, J. L. (2020). Infant formula and toddler milk marketing: opportunities to address harmful practices and improve young children's diets. Nutrition Reviews, 78, 866–883. 10.1093/nutrit/nuz095 [DOI] [PubMed] [Google Scholar]
- Hawkes, C. (2010). The influence of trade liberalization and global dietary change: The case of vegetable oils, meat and highly processed foods. In Hawkes C., Blouin C., Henson S., Drager N., & Dube L. (Eds.), Trade, Food, Diet and Health: Perspectives and Policy Options (pp. 35–59). Chichester: John Wiley & Sons. [Google Scholar]
- Henderson, L. , Kitzinger, J. , & Green, J. (2000). Representing infant feeding: content analysis of British media portrayals of bottle feeding and breast feeding. British Medical Journal, 321(7270), 1196–1198. 10.1136/bmj.321.7270.1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- High Level Panel of Experts on Food Security and Nutrition (Ed.) . (2017). Nutrition and food systems: A report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. Rome: Committee on World Food Security. [Google Scholar]
- Hipgrave, D. B. , Assefa, F. , Winoto, A. , & Sukotjo, S. (2012). Donated breast milk substitutes and incidence of diarrhoea among infants and young children after the May 2006 earthquake in Yogyakarta and Central Java. Public Health Nutrition, 15(2), 307–315. 10.1017/s1368980010003423 [DOI] [PubMed] [Google Scholar]
- International Baby Food Action Network, & International Code Documentation Center . (2017). Breaking the Rules. Penang: Stretching the Rules. [Google Scholar]
- International Labor Organization, & Asia Development Bank . (2011). Women and Labour Markets in Asia: Rebalancing for Gender Equality. Retrieved from https://www.adb.org/sites/default/files/publication/28620/women-labor-markets.pdf
- International Labour Organization . (2014). Maternity and Paternity at Work Law and Practice across the World. Retrieved from https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms:242615.pdf
- International Labour Organization . (2017). World Social Protection Report 2017–19: Universal social protection to achieve the Sustainable Development Goals. Retrieved from https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms:604882.pdf
- Jelliffe, D. B. , & Jelliffe, E. P. (1978). Human milk in the modern world. Oxford: Oxford University Press. [Google Scholar]
- Joffe, N. , Webster, F. , & Shenker, N. (2019). Support for breastfeeding is an environmental imperative. British Medical Journal, 367, l5646. 10.1136/bmj.l5646 [DOI] [PubMed] [Google Scholar]
- Karlsson, J. O. , Garnett, T. , Rollins, N. C. , & Röös, E. (2019). The carbon footprint of breastmilk substitutes in comparison with breastfeeding. Journal of Cleaner Production, 222, 436–445. 10.1016/j.jclepro.2019.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy, K. I. , Rivera, R. , & McNeilly, A. S. (1989). Consensus statement on the use of breastfeeding as a family planning method. Contraception, 39(5), 477–496. 10.1016/0010-7824(89)90103-0 [DOI] [PubMed] [Google Scholar]
- Liestøl, K. , Rosenberg, M. , & Walløe, L. (1988). Breast‐feeding practice in Norway 1860–1984. Journal of Biosocial Science, 20(1), 45–58. [PubMed] [Google Scholar]
- Martin, C. R. , Ling, P.‐R. , & Blackburn, G. L. (2016). Review of infant feeding: key features of breast milk and infant formula. Nutrients, 8(5), 279. https://dx.doi.org/10.3390%2Fnu8050279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejia, P. , Seklir, L. , Gardin, K. , & Nixon, L. (2016). Mother and child promotion: A preliminary analysis of social media marketing of infant formula. Retrieved from http://www.bmsg.org/wp-content/uploads/2016/10/bmsg_infant_formula_marketing_social_media_analysis.pdf
- Merewood, A. , Grossman, X. , Cook, J. , Sadacharan, R. , Singleton, M. , Peters, K. , & Navidi, T. (2010). US hospitals violate WHO policy on the distribution of formula sample packs: results of a national survey. Journal of Human Lactation, 26(4), 363–367. 10.1177/0890334410376947 [DOI] [PubMed] [Google Scholar]
- Michaud‐Létourneau, I. , Gayard, M. , Mathisen, R. , Phan, L. T. H. , Weissman, A. , & Pelletier, D. L. (2019). Enhancing governance and strengthening advocacy for policy change of large Collective Impact initiatives. Maternal & Child Nutrition, 15, e12728. 10.1111/mcn.12728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaud‐Létourneau, I. , Gayard, M. , & Pelletier, D. L. (2019). Translating the International Code of Marketing of Breast‐milk Substitutes into national measures in nine countries. Maternal & Child Nutrition, 15(S2), e12730. 10.1111/mcn.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro, C. A. , Cannon, G. , Lawrence, M. , Costa Louzada, M. L. , & Machado, P. P. (2019). Ultra‐processed foods, diet quality, and health using the NOVA classification system. Food and Agriculture Organization of the United Nations: Rome. Retrieved from http://www.fao.org/3/ca5644en/ca5644en.pdf [Google Scholar]
- Neves, P. A. , Gatica‐Domínguez, G. , Rollins, N. C. , Piwoz, E. , Baker, P. , Barros, A. J. , & Victora, C. G. (2019). Infant Formula Consumption Is Positively Correlated with Wealth, Within and Between Countries: A Multi‐Country Study. The Journal of Nutrition, 150(4), 910–917. 10.1093/jn/nxz327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, T. T. , Withers, M. , Hajeebhoy, N. , & Frongillo, E. A. (2016). Infant Formula Feeding at Birth Is Common and Inversely Associated with Subsequent Breastfeeding Behavior in Vietnam. The Journal of Nutrition, 146(10), 2102–2108. 10.3945/jn.116.235077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogbuanu, C. , Glover, S. , Probst, J. , Liu, J. , & Hussey, J. (2011). The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics, 127(6), e1414–e1427. 10.1542/peds.2010-0459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passport Global Market Information Database (2019). London: Euromonitor International.
- Pereira, C. , Ford, R. , & Feeley, A. (2016). Cross‐sectional survey shows that follow‐up formula and growing‐up milks are labelled similarly to infant formula in four low and middle income countries. Maternal & Child Nutrition, 12, 91–105. 10.1111/mcn.12269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez‐Escamilla, R. , Curry, L. , Minhas, D. , Taylor, L. , & Bradley, E. (2012). Scaling up of breastfeeding promotion programs in low‐ and middle‐income countries: the "breastfeeding gear" model. Advances in Nutrition, 3(6), 790–800. 10.3945/an.112.002873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez‐Escamilla, R. , Martinez, J. L. , & Segura‐Pérez, S. (2016). Impact of the Baby‐friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Maternal & Child Nutrition, 12(3), 402–417. 10.1111/mcn.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piwoz, E. G. , & Huffman, S. L. (2015). The impact of marketing of breast‐milk substitutes on WHO‐recommended breastfeeding practices. Food and Nutrition Bulletin, 36(4), 373–386. 10.1177/0379572115602174 [DOI] [PubMed] [Google Scholar]
- Pomeranz, J. , Romo Palafox, M. , & Harris, J. (2018). Toddler drinks, formulas, and milks: labeling practices and policy implications. Preventive Medicine, 109, 11–16. 10.1016/j.ypmed.2018.01.009 [DOI] [PubMed] [Google Scholar]
- Popkin, B. M. , & Reardon, T. (2018). Obesity and the food system transformation in Latin America. Obesity Reviews, 19(8), 1028–1064. 10.1111/obr.12694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post, J. E. (1985). Assessing the Nestlé boycott: Corporate accountability and human rights. California Management Review, 27(2), 113–131. 10.2307/41165133 [DOI] [Google Scholar]
- Prior, E. , Santhakumaran, S. , Gale, C. , Philipps, L. H. , Modi, N. , & Hyde, M. J. (2012). Breastfeeding after cesarean delivery: a systematic review and meta‐analysis of world literature. The American Journal of Clinical Nutrition, 95(5), 1113–1135. 10.3945/ajcn.111.030254 [DOI] [PubMed] [Google Scholar]
- Reardon, T. , Tschirley, D. , Dolislager, M. , Snyder, J. , Hu, C. , & White, S. (2014). Urbanization, diet change, and transformation of food supply chains in Asia. Retrieved from http://www.fao.org/fileadmin/templates/ags/docs/MUFN/DOCUMENTS/MUS_Reardon_2014.pdf
- Richter, J. (2001). Holding corporations accountable: Corporate conduct, international codes, and citizen action: Palgrave Macmillan.
- Robinson, H. , Buccini, G. , Curry, L. , & Perez‐Escamilla, R. (2019). The World Health Organization Code and exclusive breastfeeding in China, India, and Vietnam. Maternal & Child Nutrition, 15(1), e12685. 10.1111/mcn.12685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roe, B. , Whittington, L. A. , Fein, S. B. , & Teisl, M. F. (1999). Is there competition between breast‐feeding and maternal employment? Demography, 36(2), 157–171. https://pubmed.ncbi.nlm.nih.gov/10332608/. 10.2307/2648105 [DOI] [PubMed] [Google Scholar]
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , … Group, T. L. B. S . (2016). Why invest, and what it will take to improve breastfeeding practices? The Lancet, 387(10017), 491–504. 10.1016/s0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Romo‐Palafox, M. J. , Pomeranz, J. L. , & Harris, J. L. (2020). Infant formula and toddler milk marketing and caregiver's provision to young children. Maternal & Child Nutrition, 16, e12962. 10.1111/mcn.12962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, K. D. , Eastham, C. A. , Kasehagen, L. J. , & Sandoval, A. P. (2008). Marketing infant formula through hospitals: the impact of commercial hospital discharge packs on breastfeeding. American Journal of Public Health, 98(2), 290–295. 10.2105/ajph.2006.103218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan, A. S. (1997a). The resurgence of breastfeeding in the United States. Pediatrics, 99(4), e12–e12. 10.1542/peds.99.4.e12 [DOI] [PubMed] [Google Scholar]
- Ryan, K. (1997b). The power of support groups: influence on infant feeding trends in New Zealand. Journal of Human Lactation, 13(3), 183–190. 10.1177/089033449701300302 [DOI] [PubMed] [Google Scholar]
- Sadacharan, R. , Grossman, X. , Matlak, S. , & Merewood, A. (2014). Hospital discharge bags and breastfeeding at 6 months: Data from the Infant Feeding Practices Study II. Journal of Human Lactation, 30(1), 73–79. 10.1177/0890334413513653 [DOI] [PubMed] [Google Scholar]
- Save the Children . (2013a). Don't Push It: Why the Formula Milk Industry Must Clean Up Its Act. Retrieved from https://resourcecentre.savethechildren.net/node/13218/pdf/dont-push-it.pdf
- Save the Children . (2013b). Superfood for babies: How overcoming barriers to breastfeeding will save children's lives. Retrieved from https://www.savethechildren.org/content/dam/global/reports/health-and-nutrition/baby-superfood-asia.pdf?vanityurl=BF-Report
- Scott, J. A. , & Mostyn, T. (2003). Women's experiences of breastfeeding in a bottle‐feeding culture. Journal of Human Lactation, 19(3), 270–277. 10.1177/0890334403255225 [DOI] [PubMed] [Google Scholar]
- Smith, J. (2007). The contribution of infant food marketing to the obesogenic environment in Australia. Breastfeeding Review, 15(1), 23–35. https://pubmed.ncbi.nlm.nih.gov/17424655/ [PubMed] [Google Scholar]
- Smith, J. , & Blake, M. (2013). Infant food marketing strategies undermine effective regulation of breast‐milk substitutes: trends in print advertising in Australia, 1950–2010. Australian and New Zealand Journal of Public Health, 37(4), 337–344. 10.1111/1753-6405.12081 [DOI] [PubMed] [Google Scholar]
- Smith, J. , Galtry, J. , & Salmon, L. (2014). Confronting the formula feeding epidemic in a new era of trade and investment liberalisation. The Journal of Australian Political Economy, 73, 132. [Google Scholar]
- Smith, J. P. (2015). Markets, breastfeeding and trade in mothers' milk. International Breastfeeding Journal, 10(1), 1–7. 10.1186/s13006-015-0034-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel, H. L. , Iellamo, A. , Raya, R. R. , Padilla, A. A. , Olivé, J.‐M. , & Nyunt‐U, S. (2011). Is unimpeded marketing for breast milk substitutes responsible for the decline in breastfeeding in the Philippines? An exploratory survey and focus group analysis. Social Science & Medicine, 73(10), 1445–1448. 10.1016/j.socscimed.2011.08.029 [DOI] [PubMed] [Google Scholar]
- Spaeth, A. , Zemp, E. , Merten, S. , & Dratva, J. (2018). Baby‐Friendly Hospital designation has a sustained impact on continued breastfeeding. Maternal & Child Nutrition, 14(1), e12497. 10.1111/mcn.12497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stang, J. , Hoss, K. , & Story, M. (2010). Health statements made in infant formula advertisements in pregnancy and early parenting magazines: a content analysis. Childhood Obesity and Nutrition, 2(1), 16–25. 10.1177/1941406409359806 [DOI] [Google Scholar]
- Stuart‐Macadam, P. (2017). Breastfeeding: Bicultural Perspectives. Oxford, New York: Routledge. [Google Scholar]
- Tarrant, M. , Lok, K. Y. , Fong, D. Y. , Lee, I. L. , Sham, A. , Lam, C. , … Chan, N. P. (2015). Effect of a hospital policy of not accepting free infant formula on in‐hospital formula supplementation rates and breast‐feeding duration. Public Health Nutrition, 18(14), 2689–2699. 10.1017/s1368980015000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Nielsen Company . (2015). Oh, Baby! Trends in the global baby food and diaper markets. Retrieved from https://www.nielsen.com/us/en/insights/report/2015/oh-baby-trends-in-the-global-baby-food-and-diaper-markets-august-2015/
- Thorley, V. (2015). Free supplies and the appearance of endorsement: Distribution of tobacco to soldiers and artificial infant formula to new mothers. Journal of Human Lactation, 31(2), 213–215. 10.1177/0890334414567776 [DOI] [PubMed] [Google Scholar]
- UNICEF . (2019). State of the World's Children 2019. Children, Food and Nutrition: Growing well in a changing world. Retrieved from https://www.unicef.org/media/60806/file/SOWC-2019.pdf
- UNICEF, & Global Alliance for Improved Nutrition . (2019). Food systems for children and adolescents. Working together to secure nutritious diets. Retrieved from https://www.unicef.org/nutrition/files/UNICEF_GAIN_Food_Systems_Children_Adolescents.pdf
- United Nations Office of the High Commissioner on the Rights of the Child . (1989). Conventions on the Rights of the Child. Retrieved from https://www.ohchr.org/EN/ProfessionalInterest/Pages/CRC.aspx
- van Tulleken, C. (2018). Overdiagnosis and industry influence: how cow's milk protein allergy is extending the reach of infant formula manufacturers. British Medical Journal, 363, k5056. 10.1136/bmj.k5056 [DOI] [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. , França, G. V. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. 10.1016/s0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Walters, D. D. , Phan, L. T. , & Mathisen, R. (2019). The cost of not breastfeeding: global results from a new tool. Health Policy and Planning, 34(6), 407–417. 10.1093/heapol/czz050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells, J. C. , Sawaya, A. L. , Wibaek, R. , Mwangome, M. , Poullas, M. S. , Yajnik, C. S. , & Demaio, A. (2020). The double burden of malnutrition: aetiological pathways and consequences for health. The Lancet, 395(10217), 75–88. 10.1016/S0140-6736(19)32472-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank . (2019). DataBank—population estimates and projections. Vol. 2019. Retrieved from https://databank.worldbank.org/data/reports.aspx?source=health‐nutrition‐and‐population‐statistics:‐population‐estimates‐and‐projections#
- World Health Organization . (1981). International Code of Marketing of Breastmilk Substitutes. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/40382/9241541601.pdf;jsessionid=8279E1AC2FC5A5F6F78B1D3D4AEE8036?sequence=1
- World Health Organization . (1982). The prevalence and duration of breast‐feeding: a critical review of available information. Division of Family Health World Health Organization. World Health Statistics Quarterly, 35(2), 92–116. [PubMed] [Google Scholar]
- World Health Organization . (2013). Information concerning the use and marketing of follow‐up formula. Retrieved from http://www.who.int/nutrition/topics/WHO_brief_fufandcode_post_17July.pdf
- World Health Organization . (2016). Maternal, infant and young child nutrition: Guidance on ending the inappropriate promotion of foods for infants and young children. Sixty‐Ninth World Health Assembly A69/7 Add.1. Retrieved from https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_7Add1-en.pdf?ua=1
- World Health Organization . (2017a). Guidance on ending the inappropriate promotion of foods for infants and young children: implementation manual. Sixty‐Ninth World Health Assembly A69/7 Add.1. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/260137/9789241513470-eng.pdf?sequence=1
- World Health Organization . (2017b). National Implementation of the Baby‐friendly Hospital Initiative 2017 . Retrieved from http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_7Add1-en.pdf?ua=1
- World Health Organization, & UNICEF . (2003). Global Strategy for Infant and Young Child Feeding. Retrieved from http://apps.who.int/iris/bitstream/10665/42590/1/9241562218.pdf?ua=1&ua=1
- World Health Organization, UNICEF, & IBFAN . (2018). Marketing of Breast‐Milk Substitutes: National Implementation of the International Code Status Report 2018. Retrieved from http://apps.who.int/iris/bitstream/handle/10665/272649/9789241565592-eng.pdf?ua=1
- World Health Organization, UNICEF, & IBFAN . (2020). Marketing of Breast‐Milk Substitutes: National Implementation of the International Code Status Report 2020. Retrieved from https://apps.who.int/iris/rest/bitstreams/1278635/retrieve
- Zehner, E. (2016). Promotion and consumption of breastmilk substitutes and infant foods in Cambodia, Nepal, Senegal and Tanzania. Maternal & Child Nutrition, 12(S2), 3–7. 10.1111/mcn.12308 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Commercial milk formula category definitions*
Table S2. Included countries by World Bank income level and UNICEF region
Figure S1. Total commercial BMS sales volumes for all countries combined, 2005–19 with projections to 2024
Figure S2. World dry milk production by region, 1961–2014


