Lesson
We are reporting a case of thoracic outlet syndrome and the value of duplex in the diagnosis of this syndrome.
Keywords: cardiovascular medicine, clinical diagnostic tests, radiology and imaging
Introduction
Thoracic outlet syndrome is a constellation of symptoms in the shoulder and upper extremity that may present as pain, dysesthesia, weakness, oedema and pallor resulting from total or partial compression of the neurovascular bundle exiting the thoracic outlet. Thoracic outlet syndrome is classified into three subgroups according to its pathophysiology: neurogenic thoracic outlet syndrome, arterial thoracic outlet syndrome and venous thoracic outlet syndrome. Among them, neurogenic thoracic outlet syndrome accounts for more than 90% of the cases, followed by venous thoracic outlet syndrome accounting for 3–5%, and arterial thoracic outlet syndrome accounting for 1–2%.1 Venous thoracic outlet syndrome occurs as a result of extrinsic compression and subsequent stenosis of the subclavian vein. Anomalous anatomy, repetitive movement-induced swelling with microhaemorrhage and subsequent fibrosis, compressive soft tissue masses, deep-venous thrombosis can be initiators of venous thoracic outlet syndrome.2–5
Case illustration
A 37-year-old man presented with recurrent pressure-quality left chest discomfort with radiation to neck and shoulder, accompanied by left arm numbness and tingling, intermittently aggravated by shoulder movement. Physical examination revealed tenderness along the medial scapula, reduced abduction of the left shoulder, minimal pain with impingement testing including Neer and Hawkins exam, positive Adson’s test, negative cross-body and O’Brien’s exams. Cardiac work up was negative, including electrocardiogram and stress echocardiogram. Regular computed topography and magnetic resonance imaging were negative. His symptoms failed to improve with physical therapy.
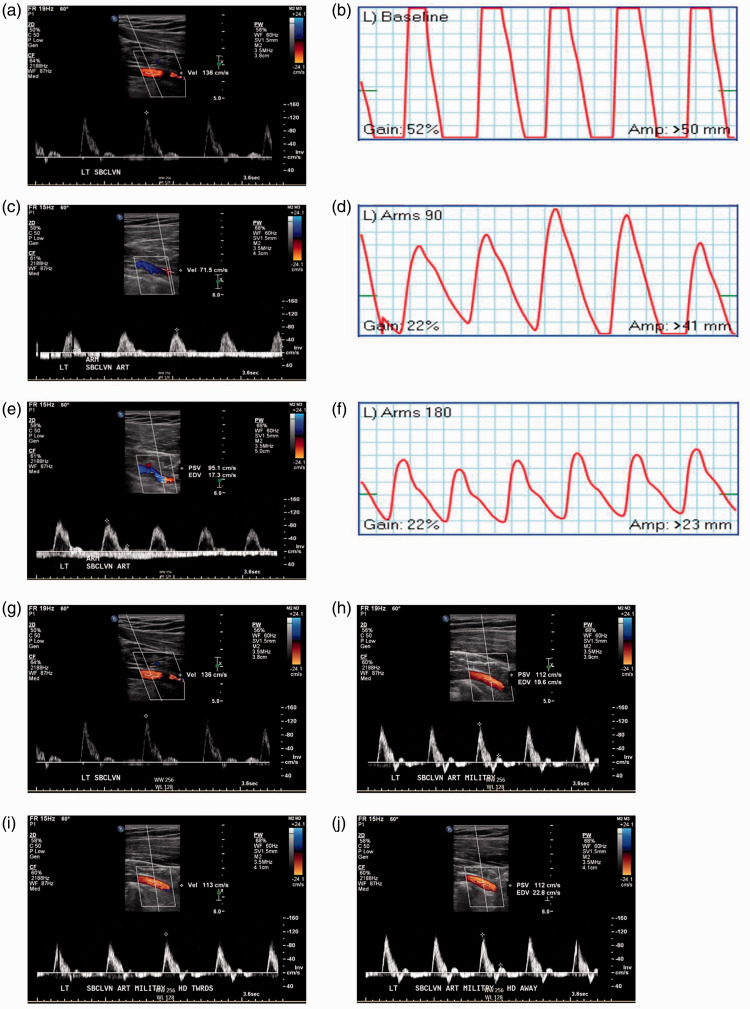
A vascular duplex of left upper extremity showed compression of both the subclavian vein and artery. The subclavian vein was assessed with color and spectral Doppler in the neutral position, at 90° and 180° abduction. At both 90° and 180° abduction, there was loss of cardiac pulsatility and respiratory phasicity, but continuous flow remained, indicating compression without obstruction (Figure 1). Halstead manoeuvre was also performed to illicit obstruction. There was complete flow obstruction provoked by this manoeuvre (Figure 1). Interrogation of the subclavian artery was performed with shoulder abduction and Halstead manoeuvre. Diminished peak systolic velocities and pulse volume recordings with provocation indicate arterial compression (Figures 2). Repeated computed topography with three-dimensional reconstruction suggested vascular compression from first rib. The patient underwent left scalenectomy and first rib resection for thoracic outlet syndrome decompression. His symptoms of left arm and chest discomfort were significantly improved post operation.
Figure 1.
Left subclavian vein with adduction and military position. (a) In the neutral shoulder position, there is normal respiratory phasicity and normal cardiac pulsatility (arrow heads). (b) At 90° adduction, there is loss of phasicity and pulsatility due to subclavian compression, illustrated by the continuous Doppler flow signal. The negative pulsatile signal represents contamination signal from the subclavian artery. (c) At 180° adduction, continuous flow once again represents compression without obstruction. (d) Normal venous flow Doppler signal. (e) Abrupt cessation of flow when military position is assumed (arrow). (f) Military posture + left head turn shows ongoing obstruction to flow. (g) Military posture + right head turn relieved the obstruction, but compression remained, shown by continuous flow with loss of pulsatility and passivity.
Figure 2.
Left subclavian artery with Adson’s manoeuvre and military position. (a) Baseline peak systolic velocity in neutral position, 136 cm/s. (b) Baseline pulse volume recording, amplitude > 50 mm. (c) 90° abduction shows interval decreased in peak systolic velocity 71.5 cm/s, indicating compression. (d) 90° abduction pulse volume recording shows corresponding dampened amplitude. (e) 180° abduction shows a decrescendo decrease in peak systolic velocity, indicating dynamic compression. Nadir peak systolic velocity, ∼70 cm/s. (f) 180° abduction pulse volume recording with progressive decrease in amplitude. (g) Neutral position, decremental peak systolic velocity 136 cm/s. (h) Military, decremental peak systolic velocity 112 cm/s. (i) Military, head towards, decremental peak systolic velocity 113 cm/s. (j) Military, head away, decremental peak systolic velocity 112 cm/s.
Discussion
Thoracic outlet syndrome is usually caused by extrinsic compression and subsequent stenosis of the neurovascular structure. An anatomical abnormality is the typically fundamental prerequisite, including a cervical rib, anomalous first rib or anomalous scalene muscle.6 Additionally, injuries such as hyperextension/flexion injury of neck and bony fracture have been described.7,8 Thrombosis and tumour are also potential etiologies. Venous thoracic outlet syndrome composed of 3–5% cases of thoracic outlet syndrome. It is more common in younger (aged 14–45), able-bodies individuals, and most often affects the dominant upper extremity.9 Venous thoracic outlet syndrome is also grouped into three categories: intermittent positional stenosis/obstruction, secondary subclavian vein thrombosis due to catheter placement and effort thrombosis.3
The symptoms of neurogenic thoracic outlet syndrome include pain, dysesthesia, numbness and weakness involving the distribution area of C5 through T1 brachial plexus nerves. The arterial thoracic outlet syndrome can present with hand ischemic symptoms like pain, pallor, paresthesia and coldness. The venous thoracic outlet syndrome presents with upper extremity edema, accompanied by pain and cyanosis.
Symptoms may be atypical and elusive, as illustrated in our patient with recurrent chest pressure, masquerading as angina pectoris. A clue to diagnosis was the precipitant of symptoms triggered by arm movement. As such, he was referred for an upper extremity venous duplex with examination manoeuvres to temporarily occlude the neurovascular structure. Electrodiagnostic testing via nerve conduction and electromyography are indicated for suspected neurogenic thoracic outlet syndrome. For venous thoracic outlet syndrome and arterial thoracic outlet syndrome, Doppler ultrasound is the primary test of choice due to the real-time assessment of dynamic Doppler signals associated with compressive manoeuvres, yielding a high sensitivity and specificity.10 Secondary tests include computed tomography or magnetic resonance imaging to define anatomical defects, such as prominent cervical rib or compressive tumours and their anatomical relationship to the thoracic outlet.10
Treatment strategy of thoracic outlet syndrome depends on the underlying etiology, and can involve conservative or surgical measures. Cervical rib or anomalous rib without symptoms only need observation. Therapeutic strategies for neurogenic thoracic outlet syndrome include physical therapy with option for interscalene injection, corticosteroids and botulinum toxin type A. Anticoagulation can be given for thrombosis complicating venous thoracic outlet syndrome or arterial thoracic outlet syndrome. Surgical intervention such as thoracic outlet decompression remains the final method conservative management fails. Surgical intervention is often the initial approach for venous thoracic outlet syndrome and arterial thoracic outlet syndrome in current practice, with the first rib being resected to decompress the brachial plexus. The procedure is usually performed by transaxillary, supraclavicular or infraclavicular techniques. Blocking the scalene muscle or pectoralis minor may be done to predict the effect of surgery.
Conclusion
Duplex ultrasound is efficient, easily performed diagnostic tool in the evaluation of thoracic outlet syndrome.
Acknowledgements
None.
Declarations:
Competing Interests: None declared.
Funding: None declared.
Ethics approval: Not applicable.
Guarantor: Vinh Nguyen.
Contributorship: JH contributed to patient care, chart review and data collection, discussion, and article writing and revision. RB, KK, JW, VF, TF contributed equally on patient care, discussion, article revision. VN contributed patient care, discussion, supervision of article writing and revision.
Provenance: Not commissioned. Externally peer reviewed.
ORCID iD: Jian Hu https://orcid.org/0000-0002-0465-8307
References
- 1.Freischlag J and Orion K. Understanding thoracic outlet syndrome. Scientifica (Cairo) 2014: 248163. [DOI] [PMC free article] [PubMed]
- 2.Ibrahim R, Dashkova I, Williams M, Kozikowski A, Abrol N, Gandhi A, et al. Paget-Schroetter syndrome in the absence of common predisposing factors: a case report. Thromb J 2017; 15: 20–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirza AK, Barrett IJ, Rathore A, Rose PS, Shives T, Bower TC, et al. Soft tissue neoplasms causing apparent venous thoracic outlet syndrome. Ann Vasc Surg 2017; 42: 306 e1–306 e4. [DOI] [PubMed] [Google Scholar]
- 4.Yuschak E, Haq F, Chase S. A case of venous thoracic outlet syndrome: primary care review of physical exam provocative tests and osteopathic manipulative technique considerations. Cureus 2019; 11: e4921–e4921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther 2019; 8: 5–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halsted WS. An experimental study of circumscribed dilation of an artery immediately distal to a partially occluding band, and its bearing on the dilation of the subclavian artery observed in certain cases of cervical rib. J Exp Med 1916; 24: 271–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Almeida DF, Meyer RD, Oh SJ. True neurogenic thoracic outlet syndrome in a competitive swimmer: a case report of this rare association. Arq Neuropsiquiatr 2007; 65: 1245–1248. [DOI] [PubMed] [Google Scholar]
- 8.Katirji B, Hardy RW, Jr. Classic neurogenic thoracic outlet syndrome in a competitive swimmer: a true scalenus anticus syndrome. Muscle Nerve 1995; 18: 229–233. [DOI] [PubMed] [Google Scholar]
- 9.Maru S, Dosluoglu H, Dryjski M, Cherr G, Curl GR, Harris LM. Thoracic outlet syndrome in children and young adults. Eur J Vasc Endovasc Surg 2009; 38: 560–564. [DOI] [PubMed] [Google Scholar]
- 10.Demondion X, Herbinet P, Jan SVS, Boutry N, Chantelot C, Cotten A. Imaging assessment of thoracic outlet syndrome. Radiographics 2006; 26: 1735–1750. [DOI] [PubMed] [Google Scholar]