Abstract
Background:
Although everted bursal flaps of delaminated tears have been reported, few studies have reported radiologic images, arthroscopic findings, and clinical results after repair.
Purpose:
To compare the repair outcomes of everted delaminated tears with those of classic delaminated supraspinatus tears.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Among 153 patients who underwent arthroscopic rotator cuff repair for a delaminated supraspinatus tear, everted bursal flap tears were observed in 24 patients upon arthroscopy (group A). Another 24 patients with classic delaminated supraspinatus tears, matched for age and sex, were selected for group B. Magnetic resonance imaging (MRI) and ultrasonography were performed preoperatively and postoperatively. Patients were evaluated using a visual analog scale (VAS) for pain as well as functional scores (American Shoulder and Elbow Surgeons [ASES] score, Constant score, and University of California Los Angeles shoulder score). Scores were compared preoperatively and at final follow-up (mean follow-up, 32 months).
Results:
Patients in both groups A and B reported improved VAS and functional scores at the final follow-up. In group A, preoperative VAS scores were higher and functional scores were poorer than in group B. Subacromial effusions with tendon swelling on preoperative MRI were more common in group A. During follow-up ultrasonography, group A patients exhibited persistent subacromial effusion. However, VAS scores at final follow-up were significantly better in group A (0.4 ± 0.7) than in group B (1.6 ± 1.4) (P < .001), and ASES scores at final follow-up were better in group A (84.3 ± 4.3) than in group B (77.0 ± 10.2) (P = .005).
Conclusion:
Everted bursal flap delaminated tears were associated with higher VAS scores and poorer functional scores preoperatively. Although subacromial effusions were experienced by group A during the early postoperative period, clinical outcomes at final follow-up were significantly better for everted delaminated tears compared with classic delaminated tears.
Keywords: supraspinatus, everted, delamination, broccoli-like, arthroscopy
The term delamination is used when horizontal cleavage is seen in torn tendons.11 Previous studies have reported an incidence of delaminated rotator cuff tear ranging from 38% to 82%.3,8 Delamination is mostly observed as a retraction of intratendinous fiber and a horizontal intrasubstance tear. It is mainly found in chronic degenerative tears.9,24,26
Delamination is a concern because it is considered a negative prognostic factor after rotator cuff repair.16,25 In a histologic study by Sonnabend et al,27 synovium-like cells reportedly lined the delaminated layer, which could interrupt tendon-to-bone healing after repair. Boileau et al3 showed that tendon healing was negatively affected when the infraspinatus tendon was delaminated. However, Kim et al13 reported a higher retear rate in nondelaminated tears and proposed that delamination is not a negative prognostic factor. Thus, delamination as a prognostic factor cannot yet be determined.
Although the term delamination is commonly used, it has not been clearly defined.15 Various definitions are used, and there is no standard classification depending on radiologic images or arthroscopic findings.6,17 Recently, the “everted type,” bursal-sided, partial-thickness tear was reported as being associated with worse pain and range of motion (ROM) preoperatively than a simple bursal-sided tear.14 However, we did not find other studies on this topic.
The purpose of the current study was to compare everted bursal-sided delaminated tears to classic delaminated supraspinatus tears, from the preoperative period to early and final follow-up after surgical repair. We also compared the radiologic findings from diagnosis to follow-up. The study hypothesis was that the clinical results after repair of everted bursal flap delaminated tears would be better at final follow-up, with a retear rate that is similar to classic delaminated supraspinatus tears.
Methods
Patient Enrollment
We retrospectively reviewed data from 153 consecutive patients (from January 2012) with delaminated rotator cuff tears confirmed using arthroscopy among 466 patients who underwent arthroscopic cuff repair. All surgery was done at a single university hospital by a senior surgeon (H.S.S.). Among the included patients, we identified 24 patients (5.2% of the cuff repairs; 15.7% of delaminated tears) with an everted bursal flap delaminated tear observed upon arthroscopy (group A). Of the remaining 129 patients with classic delaminated rotator cuff tears, 24 patients matched by age and sex were selected (group B). Exclusion criteria were (1) combined proximal humeral fractures, (2) open repair cases, (3) cases with follow-up <2 years, and (4) Bankart lesions or superior and posterior labral repairs. Of note, in the everted bursal flap group, “broccoli head–like” torn surfaces were observed in 6 patients.
The study protocol was approved by an institutional review board, which waived the requirement for informed consent due to the retrospective nature of this study.
Clinical Assessment
Preoperative and final follow-up data were collected, including information on duration of pain affecting sleep and daily activities, trauma history, ROM for forward flexion and internal rotation, and a visual analog scale (VAS) for pain. For internal rotation at the back, we converted the vertebral level to a number for convenience of statistical analysis of internal rotation as follows: levels above T12 were numbered 5, levels T12 to L1 as 4, L2 to L3 as 3, L4 to L5 as 2, and levels below sacrum as 1.16,21 Also, functional scores including American Shoulder and Elbow Surgeons (ASES) score, Constant shoulder score, and University of California Los Angeles (UCLA) scores were evaluated preoperatively and at final follow-up (minimum follow-up of 2 years, mean follow-up 32 months).
Radiologic Assessment
Using plain radiographs of the shoulder in true anteroposterior views and caudal 30° tilting views, we assessed acromial spurs and degenerative changes in the greater tuberosity. Acromial spurs were categorized as heel type, hat type, sclerotic, or minimal.1,14,23 The greater tuberosity was categorized as normal (grade 0), exhibiting sclerosis only (grade 1), exhibiting changes <2 mm (grade 2), or exhibiting changes >2 mm (grade 3).5
Magnetic resonance imaging (MRI) and ultrasonography were performed on all patients to assess the size and configuration of the tears before surgery. The variables analyzed on MRI were the presence of subacromial effusions and the thickness of the involved tendon. Subacromial effusion was assessed as focal or extending to the subdeltoid space (Figure 1). The thickness of the involved tendon was measured as per the method of Kim et al14 (Figure 2).
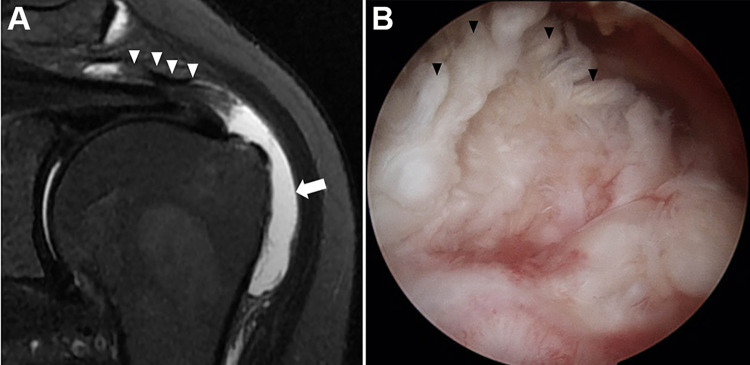
Figure 1.
(A) Magnetic resonance image of the left shoulder of a 65-year-old woman showing a subacromial effusion (arrow) extending into the subdeltoid space and the thickened torn edge (arrowheads) of an everted bursal flap tear. (B) Arthroscopic image showing the torn surface (arrowheads) of the everted bursal flap tear.
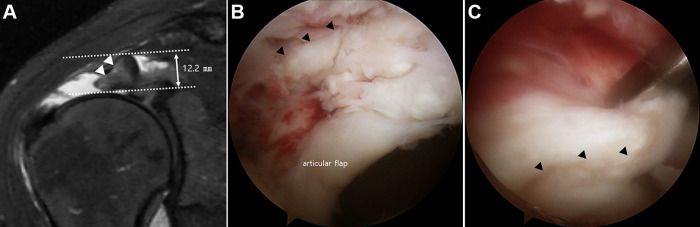
Figure 2.
(A) Magnetic resonance image of the right shoulder of a 52-year-old woman showing how the thickness of the medial torn edge (arrow heads) of an everted bursal flap tear is measured (arrow). See the online Supplemental Video showing the everted bursal flap of delaminated tear in this patient. (B) Arthroscopic image showing the torn surface (arrowheads) of the everted bursal flap tear. (C) Arthroscopic image showing the reduced bursal flap (arrowheads) to the footprint.
All patients underwent ultrasonography preoperatively, at 2, 3, and 6 months postoperatively, and at final follow-up; real-time images were obtained with a linear 1- to 15-MHz transducer (Philips HD11 XE; Philips Medical Systems). All ultrasound examinations were performed by the same senior shoulder surgeon. Examinations were performed with the patient sitting on a chair and the examiner standing behind the patient. To examine the repaired supraspinatus tendon, the patient’s shoulder was extended, the elbow flexed, and the hand placed on the iliac wing (a modified Crass position), thus maximally exposing the supraspinatus tendon under the acromion.
The presence of subacromial effusions and retear of the involved tendon were assessed at 2, 3, and 6 months postoperatively and at final follow-up. The presence of subacromial effusions and any gap in the repaired tendon was also assessed. All radiologic measurements were assessed by 2 orthopaedic surgeons (H.S.K. and H.S.S.) and repeated at a 1-month interval. The intra- and interobserver reliabilities were evaluated by calculating intraclass correlation coefficients (ICCs).
Surgical Procedure and Postoperative Protocol
All surgical procedures were performed with the patient under general anesthesia and placed in the beach-chair position. Through a standard arthroscopic portal, the glenohumeral joint was examined. Proper management such as debridement or repair was performed for any subscapularis and labral lesions. For biceps pathology, tenotomy or tenodesis was performed, depending on the age and daily activities of the patient. After articular lesions of the supraspinatus were examined, the arthroscope was moved to the subacromial space. Acromioplasty was performed if a large or sharp bony spur was observed after bursectomy.
Full inspection to the edge of the infraspinatus and removal of the synovial lining were performed. In bursal flap delaminated tears, the bursal-sided flap was found to be everted and retracted in a superomedial direction. Severely ragged margins were debrided. Particularly, bursal flaps with multiple, round, pedunculated lesions resembling broccoli heads were noted as a “broccoli-like sign” (Figure 3). During debridement, we preserved as much remnant cuff tendon as possible, to avoid the possibility of leaving a defect after repair.
Figure 3.

Arthroscopic image of the left shoulder of a 56-year-old man showing a broccoli head–like torn surface (black arrow) of the supraspinatus tendon.
The footprint of the greater tuberosity was debrided using a shaver, and light decortication was performed. In the full-thickness tears, both layers were repaired. Double-row repair (suture bridge technique) was performed. We tried to repair the cuffs with minimal tension.
All patients were immobilized for 6 weeks in a shoulder abduction brace. Intermittent wrist and hand exercises were encouraged immediately after surgery, and elbow motion was permitted on the second day after the operation. Pendulum exercises and passive forward flexion were allowed at 4 weeks after surgery, and active-assisted ROM exercises were allowed at 6 weeks after surgery with weaning of the abduction brace. Strengthening exercises were begun after 3 months postoperatively.
Statistical Analysis
Wilcoxon signed rank-sum tests were used to assess pre- to postoperative functional scores and ROM within groups A and B, and the Mann-Whitney U test was used to compare differences in functional scores, ROM, and tendon thickness between groups A and B. The chi-square test with linear-by-linear association was used to assess the severity and persistence of subacromial effusions on preoperative MRI, ultrasonography, and follow-up ultrasonography scans. The Spearman correlation analysis was used to assess the correlation between the VAS preoperatively and postoperatively. SPSS software (Version 24.0; IBM Corp) was used for all statistical analyses. The significance level for all analyses was set at P < .05.
Results
Patient Demographics
The mean follow-up for the 48 study patients was 32 months. Mean symptom duration before surgery was 3.8 months in group A and 10.9 months in group B (Table 1). The duration of aggravated pain before surgery differed significantly between the 2 groups: 1.3 months in group A and 6.0 months in group B (P = .001).
Table 1.
Patient Demographics by Group
| Variable | Group A (n = 24) | Group B (n = 24) | P Value |
|---|---|---|---|
| Mean age, y | 62.0 | 62.3 | .877 |
| Sex | >.99 | ||
| Male | 11 (45) | 11 (45) | |
| Female | 13 (55) | 13 (55) | |
| Dominant arm involved | 16 (67) | 18 (75) | .525 |
| Mean symptom duration, mo | |||
| Total | 3.8 | 10.9 | .257 |
| Aggravated | 1.3 | 6.0 | .001 |
| Thickness | .551 | ||
| Partial | 10 (42) | 8 (33) | |
| Full | 14 (58) | 16 (67) | |
| Trauma history | .871 | ||
| Major | 7 (29) | 6 (25) | |
| Minor | 2 (8) | 3 (12) | |
| None | 15 (63) | 15 (63) | |
| Sports | .806 | ||
| Contact, throwing | 2 (8) | 1 (4) | |
| Swimming, fitness | 4 (17) | 5 (21) | |
| Never | 18 (75) | 18 (75) | |
| Other pathologies | .812 | ||
| Subscapularis tears | 2 (8) | 2 (8) | |
| Tenodesis of biceps | 3 (12) | 2 (8) |
aValues are reported as n (%) unless otherwise indicated. Bolded P value indicates statistically significant difference between groups (P < .05).
In group A, partial-thickness tears were confirmed using arthroscopy in 10 patients and full-thickness tears in 14 patients. In group B, partial-thickness tears were confirmed in 8 patients and full-thickness tears in 16 patients. There were no statistical differences between the 2 groups regarding repair of the subscapularis tendon and tenodesis of the biceps tendon.
Clinical Assessment
A clinically and statistically significant improvement in pain after surgery was seen in both groups. ASES, Constant, and UCLA scores improved significantly after surgical repair in both groups (P < .001 for all). However, preoperative pain and all functional scores were significantly worse in group A; at final follow-up, VAS and all functional scores were significantly better in group A (Table 2). A subgroup analysis of patients with partial-thickness tears showed no significant difference between groups for postoperative VAS (P = .702) or functional scores (P > .05). We found no significant difference in postoperative ROM between the groups.
Table 2.
Functional Scores by Groupa
| Variable | Group A (n = 24) | Group B (n = 24) | P Value |
|---|---|---|---|
| Preoperative | |||
| VAS pain | 7.1 ± 1.6 | 4.6 ± 1.7 | <.001 |
| ASES | 39.5 ± 13.9 | 61.0 ± 15.4 | <.001 |
| Constant | 56.1 ± 14.4 | 67.5 ± 15.3 | .014 |
| UCLA | 17.7 ± 5.1 | 21.5 ± 6.1 | .032 |
| Postoperative | |||
| VAS pain | 0.4 ± 0.7 | 1.6 ± 1.4 | <.001 |
| ASES | 84.3 ± 4.3 | 77.0 ± 10.2 | .005 |
| Constant | 82.6 ± 5.0 | 75.5 ± 6.3 | <.001 |
| UCLA | 29.9 ± 2.1 | 27.8 ± 2.0 | .002 |
aValues are reported as mean ± SD. Bolded P values indicate statistically significant difference between groups (P < .05). ASES, American Shoulder and Elbow Surgeons; Constant, Constant shoulder score; UCLA, University of California Los Angeles; VAS, visual analog scale.
Radiologic Assessment
We observed 2 cases of retear in group A and 2 cases in group B. On plain radiographs, heel-type acromial spurs were observed in 10 patients in group A and 12 patients in group B. Hat-type spurs were observed in 4 patients in group A and 2 patients in group B. In all patients, there was degeneration at a minimum level of sclerosis in the greater tuberosity. The acromial spur type and degenerative grade of the greater tuberosity associated with each patient were categorized. There was no difference between 2 groups.
The ICC for intra- and interobserver reliabilities was 0.825, which indicated good reliability.
On preoperative MRI, the thickness of the supraspinatus tendon was significantly greater in group A (P < .001) (Table 3). Additionally, significantly more group A patients experienced subacromial effusions compared with group B patients (P = .004). On preoperative ultrasonography, a higher incidence of subacromial effusions was observed in group A (P = .002). In both groups, regression of subacromial effusions was observed during the follow-up period (Table 4). Although not significant at 2 months postoperatively, group A had a significantly higher incidence of subacromial effusions at 3 and 6 months postoperatively (P = .026 and P = .013, respectively).
Table 3.
Comparison of Preoperative Radiologic Findingsa
| Variable | Group A (n = 24) | Group B (n = 24) | P Value |
|---|---|---|---|
| MRI | |||
| SA effusion | .004 | ||
| None | 1 (4) | 8 (33) | |
| Focal | 12 (50) | 12 (50) | |
| Subdeltoid | 11 (46) | 4 (17) | |
| Tendon thickness, mm, mean ± SD | 9.1 ± 2.3 | 6.6 ± 1.5 | <.001 |
| Ultrasonography | |||
| SA effusion | .002 | ||
| None | 4 (17) | 15 (63) | |
| Focal | 13 (54) | 7 (29) | |
| Subdeltoid | 7 (29) | 2 (8) |
aValues are reported as n (%) unless otherwise indicated. Bolded P values indicate statistically significant difference between groups (P < .05). MRI, magnetic resonance imaging; SA, subacromial.
Table 4.
Subacromial Effusion Observed During Follow-up Ultrasonographya
| Variable | Group A (n = 24) | Group B (n = 24) | P Value |
|---|---|---|---|
| 2 months | .084 | ||
| None | 7 (29) | 11 (46) | |
| Focal | 12 (50) | 12 (50) | |
| Subdeltoid | 5 (21) | 1 (4) | |
| 3 months | .026 | ||
| None | 9 (37) | 15 (63) | |
| Focal | 11 (46) | 9 (37) | |
| Subdeltoid | 4 (17) | 0 (0) | |
| 6 months | .013 | ||
| None | 12 (50) | 20 (83) | |
| Focal | 11 (46) | 4 (17) | |
| Subdeltoid | 1 (4) | 0 (0) |
aValues are reported as n (%). Bolded P values indicate statistically significant difference between groups (P < .05).
Discussion
The major finding of this study that was patients with everted bursal flap delaminated tears had better outcomes at final follow-up than patients with classic delaminated tears. There was no difference in the retear rate. During the follow-up ultrasound, persistent subacromial effusions were observed in group A.
The patients with everted bursal flap delaminated tears (group A) had worse clinical symptoms preoperatively compared with those with classic delaminated tears (group B). This result was consistent with that reported by Kim et al,14 although that study analyzed only partial-thickness rotator cuff tears. Contrary to the study by Kim et al,14 which reported no significant differences in the final clinical outcomes between everted and simple (classic delaminated) tears, the current study included the full-thickness tears and showed that functional scores at final follow-up were better in group A. Although we can not explain the reason why the functional scores at final follow-up were better in group A, we hypothesize that the preserved folded flap could make it easy to perform a repair with less tension in group A.
The total duration of symptoms was not significantly different between the study groups. However, the duration of aggravated symptoms was significantly shorter in group A. Preoperative VAS scores were worse in group A. We hypothesize that when the delaminated flap becomes everted, the pain worsens, resulting in patients deciding to undergo surgery earlier. Many studies have revealed that early repair of acutely aggravated tears is associated with significantly improved clinical outcomes.4,7,12,19 In this study, symptom duration of group A was only 1.3 months, which was significantly shorter than that of group B (average, 6.0 months; P = .001) (Table 1).
More severe subacromial effusions were observed in group A on preoperative MRI and follow-up ultrasound performed at 2, 3, and 6 months postoperatively. A subacromial effusion is a clinical finding representative of inflammation of the bursal tissue and rotator cuff tendons.20 It is also related to subacromial mechanical impingement and irritation, resulting in bursal-sided tears.30,31 However, in the radiologic images at final follow-up, we saw few incidences of subacromial effusions in cases with no retears (Figure 4). We hypothesize that as degenerated tendon healed, inflammation decreased and subacromial effusions decreased.
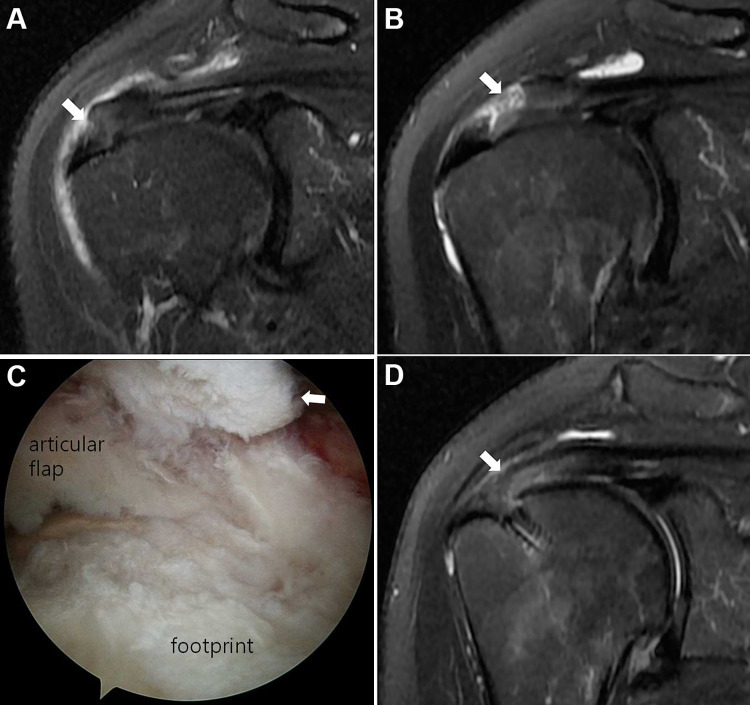
Figure 4.
Serial follow-up MRI scans of the right shoulder of a 58-year-old woman. (A) Preoperative MRI scan taken at 10 months earlier showing a mild grade partial-thickness tear (arrow). (B) Preoperative MRI scan taken on the day before surgery showing a progressed everted tear (arrow). (C) Arthroscopic image showing the everted bursal flap of the supraspinatus (arrow). (D) MRI scan taken at 10 months postoperatively showing little subacromial effusion over the repaired tendon.
In the only previous report about everted delaminated tears, Kim et al14 concluded that these type of tears are associated with a hat-type (52%) and a heel-type acromial spur (48%). In this study, we did not find significant differences between groups with respect to presence of acromial spurs and degeneration in the greater tuberosity. Subacromial spurs are related to impingement, and their association with rotator cuff tears has been reported in many studies.2,18,28 Ogawa et al22 emphasized that large spurs (>5 mm) have a diagnostic value for bursal-sided and full-thickness tears. Tucker and Snyder29 described an “acromial keel spur,” which is a downward-sloping spur on the acromial undersurface. They reported that keel spurs were related to bursal-sided and full-thickness tears. The progression of degeneration and the enlargement of spur size are related to the degree and size of the torn rotator cuff.5,10 To our knowledge, there are few studies on the relationship between acromial spurs and delaminated rotator cuff tears.
The torn tendon was observed to be significantly thicker in group A on preoperative MRI, because the everted torn flap was folded medially. This is in agreement with Kim et al,14 who reported that the folded tendons in everted bursal-sided partial-thickness tears were thickened compared with those in simple tears (classic delaminated tears). Therefore, the swollen edge of the everted bursal flap of the supraspinatus tendon and marked subacromial effusion observed on preoperative MRI are diagnostic clues for an everted bursal flap delaminated tear. Although the everted bursal flap can be visualized on preoperative ultrasound, the identifiable portion of the supraspinatus would be limited in some cases in spite of the modified Crass position.
We suggest that the broccoli head–like tear is a variant of the everted bursal flap delaminated tear. Although the broccoli head tear looks worse, we found no significant differences in preoperative radiologic findings and postoperative functional scores in patients with these tears as observed using arthroscopy. The tears did not seem to be associated with symptom severity or repair outcomes; however, only a small number of cases were observed. Nevertheless, this broccoli head–like torn surface can be indicative of an everted bursal flap. When this type of surface is seen, we recommend that less extensive debridement of the torn edge be performed so as not to leave a defect in the repaired tendon.
Limitations
This study has some limitations. First, it was a retrospective study with a relatively small sample size. Second, only age and sex were matched between groups. Other variables (eg, full vs partial-thickness tear, associated pathologies) were not matched, which may have caused selection bias. Third, the final follow-up period was relatively short (mean follow-up, 32 months).
We believe that this study contains meaningful clinical information on everted bursal-sided flap delaminated tears. To our knowledge, this was the first study to focus on clinical and structural outcomes of the repair of everted bursal-sided flap delamination compared with those of classic delaminated tears. Additionally, we present a diagnostic clue: the presence or absence of a broccoli head–like surface, with its presence being indicative of everted bursal-sided flap delamination.
Conclusion
Everted bursal flap delaminated tears were associated with higher VAS scores and poorer functional scores preoperatively compared with classic delaminated tears. Although subacromial effusion occurred during the early postoperative period, clinical outcomes were better in repaired everted delaminated tears at final follow-up.
A Video Supplement for this article is available at https://journals.sagepub.com/doi/suppl/10.1177/2325967121990423
Footnotes
Final revision submitted September 25, 2020; accepted November 3, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Institutional Review Board of Eunpyeong St. Mary's Hospital (PIRB-00146-1-002).
References
- 1. Bassett RW, Cofield RH. Acute tears of the rotator cuff: the timing of surgical repair. Clin Orthop Relat Res. 1983;175:18–24. [PubMed] [Google Scholar]
- 2. Bigliani LU. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:228. [Google Scholar]
- 3. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. [DOI] [PubMed] [Google Scholar]
- 4. Butler BR, Byrne AN, Higgins LD, Shah A, Fowler RL. Results of the repair of acute rotator cuff tears is not influenced by tear retraction. Int J Shoulder Surg. 2013;7(3):91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Choi JY, Yum JK, Song MC. Correlation between degree of torn rotator cuff in MRI and degenerative change of acromion and greater tuberosity in simple radiography. Clin Shoulder Elbow. 2013;16(1):1–9. [Google Scholar]
- 6. Choo HJ, Lee SJ, Kim JH, et al. Delaminated tears of the rotator cuff: prevalence, characteristics, and diagnostic accuracy using indirect MR arthrography. AJR Am J Roentgenol. 2015;204(2):360–366. [DOI] [PubMed] [Google Scholar]
- 7. Duncan NS, Booker SJ, Gooding BWT, Geoghegan J, Wallace WA, Manning PA. Surgery within 6 months of an acute rotator cuff tear significantly improves outcome. J Shoulder Elbow Surg. 2015;24(12):1876–1880. [DOI] [PubMed] [Google Scholar]
- 8. Flurin PH, Landreau P, Gregory T, et al. Arthroscopic repair of full-thickness cuff tears: a multicentric retrospective study of 576 cases with anatomical assessment [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(suppl_8):31–42. [DOI] [PubMed] [Google Scholar]
- 9. Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85(1):3–11. [DOI] [PubMed] [Google Scholar]
- 10. Ghandour TM, Elghazaly SA, Ghandour AM. Greater tuberosity sclerosis: a radiographic sign of rotator cuff tear? Acta Orthop Belg. 2017;83(3):416–420. [PubMed] [Google Scholar]
- 11. Han Y, Shin JH, Seok CW, Lee CH, Kim SH. Is posterior delamination in arthroscopic rotator cuff repair hidden to the posterior viewing portal? Arthroscopy. 2013;29(11):1740–1747. [DOI] [PubMed] [Google Scholar]
- 12. Hantes ME, Karidakis GK, Vlychou M, Varitimidis S, Dailiana Z, Malizos KN. A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1766–1770. [DOI] [PubMed] [Google Scholar]
- 13. Kim CW, Kim JH, Gwak HC, Park JH. The comparison of outcomes between delaminated and nondelaminated rotator cuff tear repair: is delamination a negative prognostic factor? J Shoulder Elbow Surg. 2017;26(2):216–224. [Google Scholar]
- 14. Kim HJ, Kim JY, Kee YM, Rhee YG. Bursal-sided rotator cuff tears: simple versus everted type. Am J Sports Med. 2018;46(2):441–448. [DOI] [PubMed] [Google Scholar]
- 15. Kim JH, Jung SH. Delaminated rotator cuff tear: concurrent concept and treatment. Clin Shoulder Elbow. 2019;22(3):159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kim YK, Jung KH, Kwon HM. Comparison of structural integrity and functional outcome between delaminated and nondelaminated rotator cuff tears after en masse arthroscopic repair: a retrospective cohort study with propensity score matching. Am J Sports Med. 2019;47(6):1411–1419. [DOI] [PubMed] [Google Scholar]
- 17. Kim YS, Kim JM, Bigliani LU, Kim HJ, Jung HW. In vivo strain analysis of the intact supraspinatus tendon by ultrasound speckles tracking imaging. J Orthop Res. 2011;29(12):1931–1937. [DOI] [PubMed] [Google Scholar]
- 18. Kum DH, Kim JH, Park KM, Lee ES, Park YB, Yoo JC. Acromion index in Korean population and its relationship with rotator cuff tears. Clin Orthop Surg. 2017;9(2):218–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lahteenmaki HE, Virolainen P, Hiltunen A, Heikkila J, Nelimarkka OI. Results of early operative treatment of rotator cuff tears with acute symptoms. J Shoulder Elbow Surg. 2006;15(2):148–153. [DOI] [PubMed] [Google Scholar]
- 20. Lee YB, Yang CJ, Li CZ, Zhuan Z, Kwon SC, Noh KC. Can a single sagittal magnetic resonance imaging slice represent whole fatty infiltration in chronic rotator cuff tears at the supraspinatus? Clin Orthop Surg. 2018;10(1):55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mori D, Funakoshi N, Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: patch autograft procedure versus partial repair procedure. Arthroscopy. 2013;29(12):1911–1921. [DOI] [PubMed] [Google Scholar]
- 22. Ogawa K, Yoshida A, Inokuchi W, Naniwa T. Acromial spur: relationship to aging and morphologic changes in the rotator cuff. J Shoulder Elbow Surg. 2005;14(6):591–598. [DOI] [PubMed] [Google Scholar]
- 23. Oh JH, Kim JY, Lee HK, Choi JA. Classification and clinical significance of acromial spur in rotator cuff tear: heel-type spur and rotator cuff tear. Clin Orthop Relat Res. 2010;468(6):1542–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Oh JH, Park MS, Rhee SM. Treatment strategy for irreparable rotator cuff tears. Clin Orthop Surg. 2018;10(2):119–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Park JW, Moon SH, Lee JH. Comparison of clinical and anatomical outcomes between delaminated rotator cuff tear and single layer rotator cuff tear. Clin Shoulder Elbow. 2018;21(4):207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sonnabend DH, Watson EM. Structural factors affecting the outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002;11(3):212–218. [DOI] [PubMed] [Google Scholar]
- 27. Sonnabend DH, Yu Y, Howlett CR, Harper GD, Walsh WR. Laminated tears of the human rotator cuff: a histologic and immunochemical study. J Shoulder Elbow Surg. 2001;10(2):109–115. [DOI] [PubMed] [Google Scholar]
- 28. Toivonen DA, Tuite MJ, Orwin JF. Acromial structure and tears of the rotator cuff. J Shoulder Elbow Surg. 1995;4(5):376–383. [DOI] [PubMed] [Google Scholar]
- 29. Tucker TJ, Snyder SJ. The keeled acromion: an aggressive acromial variant-a series of 20 patients with associated rotator cuff tears. Arthroscopy. 2004;20(7):744–753. [DOI] [PubMed] [Google Scholar]
- 30. van Holsbeeck M, Strouse PJ. Sonography of the shoulder: evaluation of the subacromial-subdeltoid bursa. AJR Am J Roentgenol. 1993;160(3):561–564. [DOI] [PubMed] [Google Scholar]
- 31. Voloshin I, Gelinas J, Maloney MD, O’Keefe RJ, Bigliani LU, Blaine TA. Proinflammatory cytokines and metalloproteases are expressed in the subacromial bursa in patients with rotator cuff disease. Arthroscopy. 2005;21(9):1076. [DOI] [PubMed] [Google Scholar]