Abstract
Background
Border closure is one of the policy changes implemented to mitigate against coronavirus disease 2019 (COVID-19). We evaluated the effect of border closure on the incidence rate of COVID-19 across nine African countries.
Methods
An interrupted time series analysis was used to assess COVID-19 incidence rates in Egypt, Tunisia, Democratic Republic of the Congo (DRC), Ethiopia, Kenya, Ghana, Nigeria, Senegal and South Africa (SA). Data were collected between 14 February and 19 July 2020 from online data repositories. The linear trend and magnitude of change were evaluated using the itsa function with ordinary least-squares regression in Stata with a 7-d deferred interruption point, which allows a period of diffusion post-border closure.
Results
Overall, the countries recorded an increase in the incidence rate of COVID-19 after border closure. However, when compared with matched control groups, SA, Nigeria, Ghana, Egypt and Kenya showed a higher incidence rate trend. In contrast, Ethiopia, DRC and Tunisia showed a lower trend compared with their controls.
Conclusions
The implementation of border closures within African countries had minimal effect on the incidence of COVID-19. The inclusion of other control measures such as enhanced testing capacity and improved surveillance activities will reveal the effectiveness of border closure measures.
Keywords: Africa, border closure, coronavirus, incidence
Introduction
Since the onset of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), named coronavirus disease 2019 (COVID-19), 29 155 581 confirmed cases and 926 544 deaths have been reported to the World Health Organization (WHO) as of 13 September 2020.1 On 11 March 2020, WHO declared COVID-19 a pandemic, affecting >100 countries.2 The countries with the current highest number of cases (>1 million) include the USA, India, Brazil and Russia.1 In Africa, there were >1.1 million confirmed cases in 47 countries as of 15 September 2020.1 The first cases in northern Africa were reported on 14 February 2020 in Egypt and 27 February 2020 in Nigeria.3 As of 15 September 2020, the southern region of the African Union (AU) had reported the greatest number of cases, reporting 51% (700 000) of the cases. South Africa (SA) bears the highest burden of the disease in the region, accounting for approximately 47% of the cases (650 000).4
In contrast to other continents, Africa appears to be the least affected, accounting for 4% of all cases.5 Against a backdrop of a high burden of communicable diseases,6 it was expected that a high mortality rate would be recorded in Africa.7 In addition, the fragile health systems, poorer access to healthcare, lower socio-economic status and a potentially vulnerable population are factors that were expected to drive the incidence rates (IRs) of COVID-19 within Africa.7 However, low levels of testing may be responsible in part for the apparent low infection rates.7
At the start of the pandemic, the AU endorsed a joint continental strategy with the WHO and Africa Centres for Disease Control that provided support to prepare the countries in the region.3 Public health institutes within the continent leveraged on the built-in surveillance and contact tracing systems that were developed during the 2013–2016 West African Ebola outbreak to control local transmission of the disease.3 In addition, in some countries, molecular testing for COVID-19 was scaled up using existing systems for other disease programs, such as drug-resistant tuberculosis, Lassa fever and human immunodeficiency virus.3
Furthermore, public health and social measures have been implemented across Africa to control and prevent the importation of COVID-19 and local transmission of the disease.3 Measures implemented included enforcing lockdowns and border closures across the region.3,8 While lockdown has been shown to be effective in reducing the transmission of COVID-19,9,10 the effect of cross-border measures and border closures on the transmission of COVID-19 are not well understood.11 The limited evidence on cross-border measures has focused primarily on the impact of travel restrictions, with mixed findings.11 Available evidence suggests that travel restrictions during the influenza outbreak had only limited effectiveness in the prevention of influenza spread.12 For example, the effectiveness of travel restrictions was limited unless combined with public health interventions and behavioural changes in China.13 In contrast, a current modelling study from Australia showed that a travel ban was effective in delaying transmission of COVID-19.14 However, there are economic impacts of border closures, such as a reduction in cross-border trade. Evidence suggests that cross-border and informal trade account for 40% of the gross domestic product (GDP) and 55.7% of employment in sub-Saharan Africa (SSA).6 Therefore a decrease in terms of trade may lower revenue and cause a decline in the economic growth of African countries.6 Other impacts of cross-border restrictions include a reduction in tourism and withdrawal of investors, which may also decrease revenue and affect the GDP.15
Given that China is Africa's leading commercial partner, the risk of importation of the virus was increased due to the high air traffic.16 Using the findings of a recent study, nine countries were selected based on the risk of importation of the virus.16 Egypt and SA were estimated to be at highest risk; Nigeria, Ethiopia, Ghana and Kenya had a moderate risk and Tunisia, Democratic Republic of Congo (DRC) and Senegal had a low–moderate risk of importation of COVID-19.16 As countries across Africa are currently opening up their borders for trade, travel and business, it is vital to investigate the effect of border closure on the incidence of COVID-19. Identifying the effect of border closure in containing COVID-19 will inform policy decisions on the use of border closure as a preventive and control measure for disease transmission.
In this exploratory analysis we examined the effectiveness of border closure in nine African countries as a public health intervention against COVID-19.
Methods
This is an interrupted time series analysis (ITSA) assessing COVID-19 IRs within nine countries across the geopolitical regions of Africa with clear border closure policies. We extracted data between 14 February (the first confirmed case of COVID-19 in Africa) and 19 July 2020 from online data repositories provided by the Oxford University Blavatnik School of Government17 and the Johns Hopkins University Center for Systems Science and Engineering.18 National government policy measures regarding border closures were obtained from the Blavatnik database, details of which have been previously described.17 We chose border closures as an intervention as most cases of COVID-19 were initially introduced by travellers returning from overseas. Population data used to calculate IRs were extracted online from the United Nations World Population Prospects 2019.19 Data from two North Africa (Egypt and Tunisia) and seven SSA (DRC, Ethiopia, Kenya, Ghana, Nigeria, Senegal and SA) countries were included.
At the aggregate level, we modelled the daily natural logarithm of IRs (per 10 000 inhabitants) plus one ln(IR+1) for COVID-19 within nine African countries that implemented border closure as a strategy to curtail the spread of the disease, using an interrupted time series design.20,21 First, we fit a linear segmented multiple regression model with the form
where Tt is the time since the start of the study, Yt is the aggregated expected outcome ln(IR+1) at equidistant time point t, β0 to β3 denote the control group and β4 to β7 denote the treatment group. Specifically, β4 is the difference in the level of the intercept of the outcome between the treatment and control group before the intervention, β5 is the slope/trend of the outcome between the treatment and control group prior to the intervention, β6 denotes the difference between the treatment and control group in the level of the outcome immediately following the intervention and β7 is the difference in slope/trend between the treatment and control group of the outcome after intervention (closure) compared with pre-intervention (before closure, i.e. the difference in differences of slope).22
The intervention (Xt) was set 7 d after the date closure was implemented for the various countries. This was to account for the time it takes the border closure policy to take effect23 and for the reported incubation period of COVID-19.24,25 Here, Xt=0 before closure and Xt=1 otherwise, Z is a dummy variable and represents the group allocation (treatment, country of interest or control, other countries, matched control country), XtTt, ZXt and ZXtTt are interaction terms and εt is the error term.
The data were analysed using Stata 16.1 (StataCorp, College Station, TX, USA) with the user-written commands actest for the Cumby–Huizinga test for autocorrelation and itsa and itsamatch for linear ITSA models.21,26 Unlike the single-group model, where the counterfactual estimates depend on the treatment group's pre-intervention trend estimates, the strength of the multigroup ITSA model lies in the fact that the control group serves as the counterfactual to the treatment group for all estimates.22 Controls for each country were selected using itsamatch, which identifies countries that will best serve as matched controls in the multigroup ITSA.26 The matched controls for DRC were Kenya and Nigeria; for Egypt they were Senegal, SA and Tunisia; for Ethiopia they were all other countries; for Ghana it was DRC; for Kenya they were DRC, Ethiopia and Nigeria; for Nigeria they were DRC and Kenya; for Senegal they were Egypt, SA and Tunisia; for SA they were Egypt, Senegal and Tunisia and for Tunisia they were (Egypt, Senegal and SA). We adjusted for autocorrelation by setting the lag to 7. We assumed there would be no seasonality because time points were relative to the start of the pandemic rather than calendar time.
Results
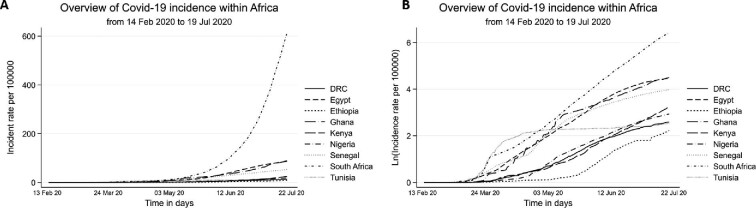
The COVID-19 IRs for all nine included countries (Egypt, Tunisia, DRC, Ghana, Nigeria, Senegal, Kenya, Ethiopia and South Africa) since 14 February 2020 are shown in Figure 1. SA had the highest IR of COVID-19, while Ethiopia had the lowest IR.
Figure 1.
Trends and daily observed incidence of Covid-19 in nine countries within Africa from 14 February to 19 July 2020. (A) Linear data and (B) ln(IR+1).
All ITSA models were of good fit. The country-specific segmented multiple regression data of ln(IR+1) are presented in Table 1 (Egypt and Tunisia), Table 2 (DRC, Ethiopia and Kenya) and Table 3 (Ghana, Nigeria, Senegal and SA).
Table 1.
ITSA of the effect of border closure on COVID-19 rates across Egypt and Tunisia
| Newey–West | ||||
|---|---|---|---|---|
| Variable | β | standard error | p-Value | 95% CI |
| Egypt | ||||
| β1 | 0.011 | 0.003 | <0.001 | 0.006 to 0.016 |
| β5+β1 | 0.008 | 0.002 | <0.001 | 0.004 to 0.012 |
| β4 | 0.043 | 0.055 | 0.432 | −0.065 to 0.151 |
| β5 | −0.003 | 0.003 | 0.294 | −0.009 to 0.003 |
| First day of closure | 0.741 | 0.185 | <0.001 | 0.378 to 1.103 |
| β3 | 0.019 | 0.005 | <0.001 | 0.001 to 0.029 |
| β3+β7 | 0.031 | 0.002 | <0.001 | 0.026 to 0.035 |
| β6 | −0.466 | 0.204 | 0.023 | −0.065 to 0.868 |
| β7 | 0.012 | 0.006 | 0.033 | 0.001 to 0.023 |
| Constant | −0.122 | 0.040 | 0.002 | 0.044 to 0.200 |
| Tunisia | ||||
| β1 | 0.006 | 0.011 | <0.001 | 0.004 to 0.008 |
| β5+β1 | 0.009 | 0.003 | 0.002 | 0.003 to 0.015 |
| β4 | −0.029 | 0.052 | 0.575 | −0.131 to 0.073 |
| β5 | 0.003 | 0.003 | 0.383 | −0.003 to 0.009 |
| First day of closure | 0.344 | 0.118 | 0.004 | 0.112 to 0.576 |
| β3 | 0.034 | 0.003 | <0.001 | 0.026 to 0.040 |
| β3+β7 | −0.000 | 0.003 | 0.926 | −0.006 to 0.005 |
| β6 | 1.068 | 0.243 | <0.001 | 0.592 to 1.544 |
| β7 | −0.035 | 0.004 | <0.001 | 0.027 to 0.043 |
| Constant | −0.062 | 0.019 | 0.001 | 0.024 to 0.099 |
β1: pre-closure trend, control; β3: difference pre-closure vs post-closure, control; β4: difference pre-closure level, treatment vs control; β5: difference pre-closure trend, treatment vs control; β6: difference immediately after closure, treatment vs control; β7: difference pre-closure vs post-closure, treatment vs control; β5+β1: pre-closure trend, treatment; β3+β7: difference pre-closure vs post-closure, treatment.
Table 2.
ITSA of the effect of border closure on COVID-19 rates across DRC, Ethiopia and Kenya
| Newey–West | ||||
|---|---|---|---|---|
| Variable | β | standard error | p-Value | 95% CI |
| DRC | ||||
| β1 | 0.001 | 0.000 | 0.005 | 0.000 to 0.001 |
| β5+β1 | 0.001 | 0.000 | 0.016 | 0.000 to 0.002 |
| β4 | −0.005 | 0.007 | 0.538 | −0.019 to 0.010 |
| β5 | 0.000 | 0.001 | 0.406 | −0.001 to 0.001 |
| First day of closure | −0.257 | 0.055 | <0.001 | 0.148 to 0.365 |
| β3 | 0.029 | 0.001 | <0.001 | 0.027 to 0.030 |
| β3+β7 | 0.024 | 0.001 | <0.001 | 0.022 to 0.025 |
| β6 | 0.128 | 0.071 | 0.072 | −0.012 to 0.267 |
| β7 | −0.007 | 0.003 | <0.001 | 0.002 to 0.008 |
| Constant | −0.007 | 0.003 | 0.029 | 0.001 to 0.0134 |
| Ethiopia | ||||
| β1 | 0.001 | 0.000 | 0.036 | 0.000 to 0.001 |
| β5+β1 | 0.001 | 0.001 | 0.016 | 0.000 to 0.002 |
| β4 | −0.008 | 0.009 | 0.409 | −0.026 to 0.011 |
| β5 | 0.001 | 0.001 | 0.246 | −0.001 to 0.002 |
| First day of closure | −0.171 | 0.048 | <0.001 | 0.077 to 0.265 |
| β3 | 0.024 | 0.001 | <0.001 | 0.023 to 0.026 |
| β3+β7 | 0.037 | 0.002 | <0.001 | 0.033 to 0.041 |
| β6 | 0.593 | 0.146 | <0.001 | 0.305 to 0.881 |
| β7 | 0.013 | 0.002 | <0.001 | 0.009 to 0.017 |
| Constant | −0.007 | 0.004 | 0.109 | −0.015 to 0.002 |
| Kenya | ||||
| β1 | 0.000 | 0.000 | 0.009 | 0.000 to 0.001 |
| β5+β1 | 0.000 | 0.000 | 0.021 | 0.000 to 0.001 |
| β4 | −0.001 | 0.003 | 0.785 | −0.006 to 0.004 |
| β5 | 0.000 | 0.000 | 0.732 | −0.000 to 0.000 |
| First day of closure | −0.321 | 0.073 | <0.001 | 0.179 to 0.464 |
| β3 | 0.025 | 0.001 | <0.001 | 0.022 to 0.027 |
| β3+β7 | 0.028 | 0.001 | <0.001 | 0.026 to 0.031 |
| β6 | −0.019 | 0.121 | 0.877 | −0.256 to 0.219 |
| β7 | 0.004 | 0.002 | 0.049 | 0.000 to 0.007 |
| Constant | −0.003 | 0.001 | 0.030 | 0.000 to 0.006 |
β1: pre-closure trend, control; β3: difference pre-closure vs post-closure, control; β4: difference pre-closure level, treatment vs control; β5: difference pre-closure trend, treatment vs control; β6: difference immediately after closure, treatment vs control; β7: difference pre-closure vs post-closure, treatment vs control; β5+β1: pre-closure trend, treatment; β3+β7: difference pre-closure vs post-closure, treatment.
Table 3.
ITSA of the effect of border closure on COVID-19 rates across Ghana, Nigeria, Senegal and South Africa
| Newey–West | ||||
|---|---|---|---|---|
| Variable | β | standard error | p-Value | 95% CI |
| Ghana | ||||
| β1 | 0.001 | 0.000 | 0.036 | 0.000 to 0.001 |
| β5+β1 | 0.001 | 0.001 | 0.016 | 0.000 to 0.002 |
| β4 | −0.008 | 0.010 | 0.409 | −0.026 to 0.011 |
| β5 | 0.001 | 0.001 | 0.246 | −0.001 to 0.002 |
| First day of closure | −0.171 | 0.048 | <0.001 | 0.077 to 0.265 |
| β3 | 0.024 | 0.001 | <0.001 | 0.023 to 0.026 |
| β3+β7 | 0.037 | 0.002 | <0.001 | 0.033 to 0.041 |
| β6 | 0.593 | 0.146 | <0.001 | 0.305 to 0.881 |
| β7 | 0.013 | 0.002 | <0.001 | 0.009 to 0.017 |
| Constant | −0.007 | 0.004 | 0.109 | −0.015 to 0.002 |
| Nigeria | ||||
| β1 | 0.001 | 0.000 | <0.001 | 0.001 to 0.002 |
| β5+β1 | 0.001 | 0.000 | 0.013 | 0.000 to 0.001 |
| β4 | 0.007 | 0.008 | 0.329 | −0.007 to 0.022 |
| β5 | −0.001 | 0.000 | 0.162 | −0.001 to 0.000 |
| First day of closure | −0.166 | 0.052 | 0.002 | 0.063 to 0.269 |
| β3 | 0.026 | 0.001 | <0.001 | 0.024 to 0.028 |
| β3+β7 | 0.029 | 0.001 | <0.001 | 0.027 to 0.031 |
| β6 | −0.005 | 0.080 | 0.953 | −0.162 to 0.153 |
| β7 | 0.003 | 0.002 | 0.054 | −0.000 to 0.006 |
| Constant | −0.016 | 0.006 | 0.008 | 0.004 to 0.027 |
| Senegal | ||||
| β1 | 0.009 | 0.002 | <0.001 | 0.006 to 0.013 |
| β5+β1 | 0.007 | 0.002 | 0.001 | 0.003 to 0.012 |
| β4 | 0.022 | 0.051 | 0.663 | −0.079 to 0.124 |
| β5 | −0.002 | 0.003 | 0.535 | −0.008 to 0.004 |
| First day of closure | 0.696 | 0.177 | <0.001 | 0.349 to 1.043 |
| β3 | 0.023 | 0.005 | <0.001 | 0.013 to 0.032 |
| β3+β7 | 0.025 | 0.003 | <0.001 | 0.020 to 0.031 |
| β6 | −0.271 | 0.223 | 0.224 | −0.708 to 0.166 |
| β7 | 0.003 | 0.006 | 0.615 | −0.008 to 0.014 |
| Constant | −0.100 | 0.032 | 0.002 | 0.036 to 0.164 |
| South Africa | ||||
| β1 | 0.010 | 0.002 | <0.001 | 0.006 to 0.0139 |
| β5+β1 | 0.011 | 0.004 | 0.011 | 0.003 to 0.020 |
| β4 | −0.023 | 0.080 | 0.776 | −0.180 to 0.135 |
| β5 | 0.001 | 0.005 | 0.789 | −0.008 to 0.011 |
| First day of closure | 0.696 | 0.149 | <0.001 | 0.403 to 0.988 |
| β3 | 0.016 | 0.004 | <0.001 | 0.010 to 0.023 |
| β3+β7 | 0.039 | 0.005 | <0.001 | 0.030 to 0.048 |
| β6 | −0.286 | 0.189 | 0.131 | −0.657 to 0.085 |
| β7 | 0.022 | 0.006 | <0.001 | 0.011 to 0.034 |
| Constant | −0.106 | 0.035 | 0.002 | 0.038 to 0.174 |
β1: pre-closure trend, control; β3: difference pre-closure vs post-closure, control; β4: difference pre-closure level, treatment vs control; β5: difference pre-closure trend, treatment vs control; β6: difference immediately after closure, treatment vs control; β7: difference pre-closure vs post-closure, treatment vs control; β5+β1: pre-closure trend, treatment; β3+β7: difference pre-closure vs post-closure, treatment.
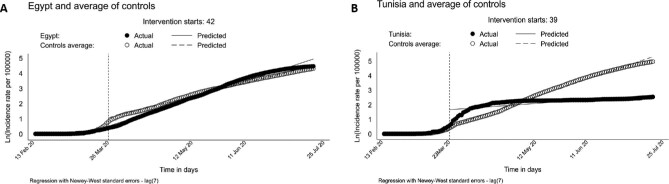
For Egypt, the mean difference in COVID-19 ln(IR+1) level between Egypt and controls/counterfactuals before border closure was 0.043 (95% confidence interval [CI] −0.065 to 0.151) and the mean difference in the COVID-19 ln(IR+1) trend was −0.003 (95% CI −0.009 to 0.003). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.741 (95% CI 0.378 to 1.103). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within Egypt after border closure of 0.031 (95% CI 0.026 to 0.035). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Egypt and controls was −0.012 (95% CI −0.001 to 0.023). We see that ln(IR+1) in Egypt increased after border closure by 0.039 and in the controls/counterfactuals by 0.030, a difference of 0.009 (95% CI −0.001 to 0.018) (see Figure 2, panel A and Table 1).
Figure 2.
Trends and observed and predicted IRs of COVID-19 within (A) Egypt and (B) Tunisia from 14 February to 19 July 2020.
For Tunisia, the mean difference in the COVID-19 ln(IR+1) level between Tunisia and controls before border closure was 0.029 (95% CI −0.131 0.073) and the mean difference in the COVID-19 ln(IR+1) trend was −0.003 (95% CI −0.003 to 0.009). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.344 (95% CI 0.112 to 0.576). This was followed by no change in the mean difference in the COVID-19 ln(IR+1) trend within Tunisia after border closure of −0.000 (95% CI −0.006, 0.005). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Tunisia and controls was −0.035 (95% CI 0.027 to 0.043). The ln(IR+1) in Tunisia increased after border closure by 0.009 and in the controls/counterfactuals by 0.041, a difference of −0.032 (95% CI 0.025, 0.039) (see Figure 2, panel B and Table 1).
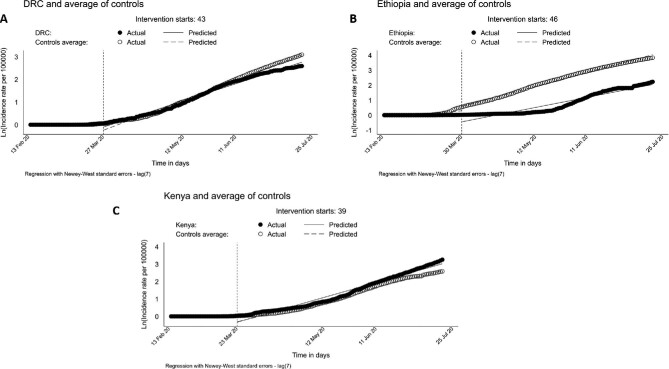
For the SSA countries, the mean difference in the COVID-19 ln(IR+1) level between DRC and controls before border closure was −0.005 (95% CI −0.019 to 0.010) and the mean difference in the COVID-19 ln(IR+1) trend was 0.000 (95% CI −0.001 to 0.001). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.257 (95% CI 0.148, 0.365). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within DRC after border closure of 0.024 (95% CI 0.022 to 0.025). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between DRC and controls was −0.007 (95% CI 0.002 to 0.008). The ln(IR+1) in DRC increased during border closure by 0.025 and in the controls by 0.029, a difference of −0.004 (95% CI 0.002 to 0.006) (see Figure 3, panel A and Table 2).
Figure 3.
Trends and observed and predicted IRs of COVID-19 within (A) DRC, (B) Ethiopia and (C) Kenya from 14 February to 19 July 2020.
In Ethiopia, the mean difference in the COVID-19 ln(IR+1) level between Ethiopia and controls before border closure was 0.008 (95% CI −0.026 to 0.011) and the mean difference in the COVID-19 ln(IR+1) trend was 0.001 (95% CI −0.001 to 0.002). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.171 (95% CI 0.077 to 0.265). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within Ethiopia after border closure of 0.037 (95% CI 0.033 to 0.041). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Ethiopia and the controls was 0.013 (95% CI 0.009 to 0.017). The ln(IR+1) in Ethiopia increased after border closure by 0.022 and in the controls by 0.031, a difference of −0.009 (95% CI 0.003 to 0.015) (see Figure 3, panel B and Table 2).
In Kenya, the mean difference in the COVID-19 ln(IR+1) level between Kenya and controls before border closure was −0.001 (95% CI −0.006 to 0.004) and the mean difference in the COVID-19 ln(IR+1) trend was 0.000 (95% CI −0.000 to 0.000). On the first day of the intervention we saw a decrease in ln(IR+1) of 0 (95% CI 0.179 to 0.464). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within Kenya after border closure of 0.028 (95% CI 0.026 to 0.031). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Kenya and the controls was 0.004 (95% CI 0.000 to 0.007). The ln(IR+1) in Kenya increased after border closure by 0.028 and in the controls by 0.025, a difference of 0.004 (95% CI 0.000 to 0.007) (see Figure 3, panel C and Table 2).
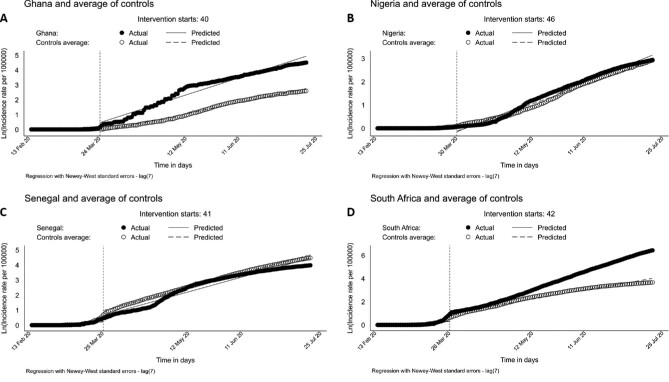
In Ghana, the mean difference in the COVID-19 ln(IR+1) level between Ghana and controls before border closure was −0.008 (95% CI −0.026 to 0.011) and the mean difference in the COVID-19 ln(IR+1) trend was 0.001 (95% CI −0.001, 0.002). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.171 (95% CI 0.077, 0.265). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within Ghana after border closure of 0.037 (95% CI 0.033, 0.041). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Ghana and the controls was 0.013 (95% CI 0.009 to 0.017). The ln(IR+1) in Ghana increased after border closure by 0.038 and in the controls by 0.025, a difference of 0.013 (95% CI 0.010, 0.017) (see Figure 4 panel A and Table 3).
Figure 4.
Trends and observed and predicted IRs of COVID-19 within (A) Ghana, (B) Nigeria, (C) Senegal and (D) South Africa from 14 February to 19 July 2020.
For Nigeria, the mean difference in the COVID-19 ln(IR+1) level between Nigeria and controls before border closure was 0.007 (95% CI −0.007 to 0.022) and the mean difference in the COVID-19 ln(IR+1) trend was −0.001 (95% CI −0.001 to 0.000). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.166 (95% CI 0.063 to 0.269). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within Nigeria after border closure of 0.029 (95% CI 0.027 to 0.031). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Nigeria and the controls was 0.003 (95% CI −0.000 to 0.006). The ln(IR+1) in Nigeria increased during border closure by 0.030 and in the controls by 0.027, a difference of 0.002 (95% CI −0.000 to 0.005) (see Figure 4, panel B and Table 3).
For Senegal, the mean difference in the COVID-19 ln(IR+1) level between Senegal and controls before border closure was 0.022 (95% CI −0.079 to 0.124) and the mean difference in the COVID-19 ln(IR+1) trend was 0.002 (95% CI −0.008 to 0.004). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.696 (95% CI 0.349 to 1.043). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within Senegal after border closure of 0.025 (95% CI 0.020 to 0.031). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between Senegal and the controls was 0.003 (95% CI −0.008 to 0.014). The ln(IR+1) in Senegal increased after border closure by 0.033 and in the controls by 0.032, a difference of 0.001 (95% CI −0.008 to 0.010) (see Figure 4, panel C and Table 3).
In SA, the mean difference in the COVID-19 ln(IR+1) level between SA and controls before border closure was 0.023 (95% CI −0.180 to 0.135) and the mean difference in the COVID-19 ln(IR+1) trend was 0.001 (95% CI −0.008 to 0.011). On the first day of the intervention we saw a decrease in ln(IR+1) of 0.696 (95% CI 0.403 to 0.988). This was followed by a significant increase in the mean difference in the COVID-19 ln(IR+1) trend within SA after border closure of 0.039 (95% CI 0.030 to 0.048). Overall, after border closure, the mean difference in the COVID-19 ln(IR+1) trend between SA and the controls was 0.022 (95% CI 0.011 to 0.034). The ln(IR+1) in SA increased after border closure by 0.050 and in the controls by 0.026, a difference of 0.024 (95% CI 0.018, 0.029) (see Figure 4, panel D and Table 3).
Discussion
Overall, the countries recorded an increase in the IR trend for COVID-19 after border closure. However, the ln(IR+1) trend after border closure varied across the nine countries, with SA showing a significantly higher ln(IR+1) trend compared with the control group. Similarly, Nigeria, Ghana, Egypt and Kenya had higher ln(IR+1) trends compared with their control groups, while Ethiopia, DRC and Tunisia showed a lower ln(IR+1) trend compared with their control groups. These findings suggest that border closure alone was not effective in decreasing the incidence of COVID-19 in African countries.
Given the risk of importation of COVID-19 through cross-border movement, many African countries implemented international guidelines to limit the importation of COVID-19 cases.6 Border closure was one of the strategies implemented, in addition to other mitigation measures such as school closures, workplace closures, cancellation of public events, restriction of gatherings and social distancing.27 Given that border closures were not singly implemented for the containment and control of COVID-19 in Africa, it is expected that there should be a reduction in the IRs of COVID-19 across the included countries. Based on the findings of this study, it is evident that there may be multifactorial reasons for the continued increase in the IRs of COVID-19 in Africa. Economic, political and sociocultural factors that differ between Africa and other continents need to be taken into account when adopting COVID-19 prevention measures.6 While measures such as personal hygiene, social distancing and stay-home lockdowns have proven to be successful in limiting the spread of COVID-19, this is not the case in Africa.28 These measures may be effective in the short term, however, they are unsustainable in the long term due to limited infrastructure, including piped water, sewage and adequate landfills.6 In addition, overcrowding and food security may also make these measures ineffective in Africa.29
Furthermore, high-income nations in Europe, the Americas, Asia and the Pacific have implemented economic stimulus packages to support businesses and individuals.6 However, countries in Africa could not afford such economic stimuli due to limited fiscal capacity.6 In addition, most economies are informal and contribute 60–80% of employment in Africa.6 Informal cross-border trade is considered an important source of employment, contributing to a large share of self-employment among women in the region.6 In many African countries, many families survive on daily earnings made from these ventures. The border closures may have had untold effects and affected the majority of livelihoods due to disruptions in trade and the supply chain.6,29 The effect is an increasing rate of unemployment that will have a profound negative effect on household welfare and health.6 As a result, a significant economic burden has been placed on many individuals and families. This economic insufficiency on individuals and families and the need to survive may prompt citizens to ignore the social distancing directive, which may contribute to the rising incidence of COVID-19 in many African countries.30 Therefore there is a need for African governments to consider other flexible and sustainable alternatives to facilitate informal trade.6 African leaders need to also focus on strengthening cross-border infrastructure that can manage cross-border heath threats, including developing an effective contact tracing and testing system.6
Limitations
This article has provided evidence on the effect of border closures on COVID-19 IRs in nine African countries with border closure measures. However, these findings should be interpreted with caution. First, ITSA does not consider data at the subject level and hence cannot predict the likelihood of the effectiveness of the intervention at the individual level. Second, the estimates of the overall effect of the intervention involved extrapolation, which is inevitably associated with uncertainty. Third, the regression method assumes linear trends over time that may not be the case for infectious disease dynamics; however, to avoid under predictions, each treatment country was measured against a modelled counterfactual/control, which strengthens the conclusions derived from this study. Although the Blavatnik database provided information about the presence or absence of a border closure policy, it did not offer information on policy adherence or the effective implementation of the policy. Given that informal cross-border trading is a source of income and is a poorly regulated market,31 it is unknown if the border closure policies were effectively implemented in the countries in this study. Furthermore, while airports are a relatively manageable point of entry, the same cannot be said of land borders between countries in Africa. Some land borders in the region may not be fenced and are only identified by an isolated concrete pillar.32 Also, people who reside close to borders between countries may have long-established cross-border economic and sociocultural relationships.32 To these people, borders do not exist and they continue to cross the border at unofficial points.32 Thus, beyond the designation of formal points of entry, border control is limited and borders are porous.32 Finally, the findings may be considered generalizable within the continent, however, it is important to consider the spread of the disease, testing capabilities within countries and culturally associated adherence to rules within countries and variations in the time from testing to diagnosis across the different countries in Africa. Support mechanisms need to be strengthened to ensure reduced COVID-19 IRs while border closures and other COVID-19 mitigation measures are being implemented.
Conclusions
The COVID-19 pandemic has swept across the entire globe, necessitating an unprecedented public health response, including lockdowns and border closures. The implementation of border closures within African countries has had minimal effect on the incidence of COVID-19, as shown by our study. A one-size-fits-all strategy using solely border closure measures does not seem adequate for the containment of COVID-19. The inclusion of other control measures such as enhanced testing capacities and improved surveillance activities alongside border closures will reveal the effectiveness of border closure measures. Prompt implementation of all COVID-19 mitigation measures needs to be well coordinated at the national level to ensure that residents of African countries do not live oblivious to the true state of COVID-19 infection.
Acknowledgements
None.
Contributor Information
Theophilus I Emeto, Discipline of Public Health and Tropical Medicine, College of Public Health, Medical and Veterinary Sciences, James Cook University, Douglas, Townsville 4811, Australia; Australian Institute of Tropical Health and Medicine, James Cook University, Douglas, Townsville 4811, Australia.
Faith O Alele, Discipline of Public Health and Tropical Medicine, College of Public Health, Medical and Veterinary Sciences, James Cook University, Douglas, Townsville 4811, Australia; Australian Institute of Tropical Health and Medicine, James Cook University, Douglas, Townsville 4811, Australia.
Olayinka S Ilesanmi, Department of Community Medicine, College of Medicine, University of Ibadan, Ibadan, Oyo State, Nigeria; Department of Community Medicine, University College Hospital, Ibadan, Oyo State, Nigeria.
Authors’ contributions
TIE, FOA and OSI conceptualised and designed the study. FOA extracted the data and wrote the Introduction section. TIE extracted the data, wrote the Methods section, conducted the statistical analysis, and wrote the results section. OSI, FOA, TIE wrote the Discussion section. All authors contributed to the initial draft and reviewed and approved the final version of the manuscript.
Funding
None.
Competing interests
None declared.
Ethical approval
Not required.
Data availability
The data underlying this article were derived from sources in public domains: the Oxford University Blavatnik School of Government (https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker#data) and the Johns Hopkins University Center for Systems Science and Engineering (https://github.com/CSSEGISandData/COVID-19).
References
- 1.World Health Organization . Coronavirus disease (COVID-19): weekly epidemiological update. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200914-weekly-epi-update-5.pdf?sfvrsn=cf929d04_2 [accessed 15 September 2020]. [Google Scholar]
- 2.World Health Organization . Coronavirus disease 2019 (COVID-19) situation report – 51. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 [accessed 30 April 2020]. [Google Scholar]
- 3.Ihekweazu C, Agogo E.. Africa's response to COVID-19. BMC Med. 2020;18(1):151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Regional Office for Africa . COVID-19: situation update for the WHO African Region. Available from: https://apps.who.int/iris/bitstream/handle/10665/334234/SITREP_COVID-19_WHOAFRO_20200909-eng.pdf [accessed 15 September 2020]. [Google Scholar]
- 5.World Health Organization . WHO coronavirus disease (COVID-19) dashboard. Available from: https://covid19.who.int/ [accessed 16 September 2020]. [Google Scholar]
- 6.Renzaho AMN.The need for the right socio-economic and cultural fit in the COVID-19 response in sub-Saharan Africa: examining demographic, economic political, health, and socio-cultural differentials in COVID-19 morbidity and mortality. Int J Environ Res Public Health. 2020;17(10):3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Lancet . COVID-19 in Africa: no room for complacency. Lancet. 2020;395(10238):1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Regional Office for Africa . Weekly bulletin on outbreaks and other emergencies. Available from: https://apps.who.int/iris/bitstream/handle/10665/331892/OEW17-2026042020.pdf [accessed 15 September 2020]. [Google Scholar]
- 9.Vinceti M, Filippini T, Rothman KJet al. Lockdown timing and efficacy in controlling COVID-19 using mobile phone tracking. EClinicalMedicine. 2020;25:100457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alfano V, Ercolano S.. The efficacy of lockdown against COVID-19: a cross-country panel analysis. Appl Health Econ Health Policy. 2020;18(4):509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee K, Worsnop CZ, Grépin KAet al. Global coordination on cross-border travel and trade measures crucial to COVID-19 response. Lancet. 2020;395(10237):1593–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Errett NA, Sauer LM, Rutkow L.. An integrative review of the limited evidence on international travel bans as an emerging infectious disease disaster control measure. J Emerg Manag. 2020;18(1):7–14. [DOI] [PubMed] [Google Scholar]
- 13.Chinazzi M, Davis JT, Ajelli Met al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adekunle A, Meehan M, Rojas-Alvarez Det al. Delaying the COVID-19 epidemic in Australia: evaluating the effectiveness of international travel bans. Aust N Zeal J Public Health. 2020;44(4):257–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lone SA, Ahmad A.. COVID-19 pandemic – an African perspective. Emerg Microbes Infect. 2020;9(1):1300–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilbert M, Pullano G, Pinotti Fet al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395(10227):871–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hale T, Petherick A, Phillips Tet al. Variation in government responses to COVID-19. Working paper BSG-WP-2020/032, Blavatnik School of Government, 20 December 2020. [Google Scholar]
- 18.Hopkins J. GitHub–CSSEGISandData/COVID-19: Data repository. Available from: https://github.com/CSSEGISandData/COVID-19 [accessed 25 February 2021]. [Google Scholar]
- 19.United Nations Department of Economic and Social Affairs . World population prospects 2019. Available from: https://population.un.org/wpp/Download/Standard/CSV/ [accessed 20 August 2020]. [Google Scholar]
- 20.Simonton DK.Cross-sectional time-series experiments: some suggested statistical analyses. Psychol Bull. 1977;84(3):489–502. [Google Scholar]
- 21.Linden A.Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15(2):480–500. [Google Scholar]
- 22.Linden A.A comprehensive set of postestimation measures to enrich interrupted time-series analysis. Stata J. 2017;17(1):73–88. [Google Scholar]
- 23.Bernal JL, Cummins S, Gasparrini A.. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lauer SA, Grantz KH, Bi Qet al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Figueiredo A, Daponte Codina A, Figueiredo Met al. Impact of lockdown on COVID-19 incidence and mortality in China: an interrupted time series study. Bull World Health Org. 2020; doi:http://dx.doi.org/10.2471/BLT.20.256701. [Google Scholar]
- 26.Linden A.A matching framework to improve causal inference in interrupted time-series analysis. J Eval Clin Pract. 2018;24(2):408–15. [DOI] [PubMed] [Google Scholar]
- 27.Senghore M, Savi MK, Gnangnon Bet al. Leveraging Africa's preparedness towards the next phase of the COVID-19 pandemic. Lancet Glob Health. 2020;8(7):e884–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau H, Khosrawipour V, Kocbach Pet al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020;27(3):taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dzinamarira T, Dzobo M, Chitungo I.. COVID-19: a perspective on Africa's capacity and response. J Med Virol. 2020;92(11):2465–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chirisa I, Mutambisi T, Chivenge Met al. The urban penalty of COVID-19 lockdowns across the globe: manifestations and lessons for Anglophone sub-Saharan Africa. GeoJournal. 2020; 10.1007/s10708-020-10281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouët A, Laborde Debucquet D. COVID-19 border policies create problems for African trade and economic pain for communities. In COVID-19 and global food security, eds. Johan Swinnen and John McDermott. Part Four: Food trade, Chapter 15, Washington, DC: International Food Policy Research Institute (IFPRI), 2020; 69–72. Available from: 10.2499/p15738coll2.133762_15. [DOI] [Google Scholar]
- 32.Moyo I. Southern Africa's porous borders pose a problem for containing the coronavirus. The Conversation, 19 April2020. Available from: https://theconversation.com/southern-africas-porous-borders-pose-a-problem-for-containing-the-coronavirus-135386 [accessed 8 January 2021]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article were derived from sources in public domains: the Oxford University Blavatnik School of Government (https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker#data) and the Johns Hopkins University Center for Systems Science and Engineering (https://github.com/CSSEGISandData/COVID-19).