Abstract
Background
The initial focus of the US public health response to coronavirus disease 2019 (COVID-19) was the implementation of numerous social distancing policies. While COVID-19 was the impetus for imposing these policies, it is not the only respiratory disease affected by their implementation. This study aimed to assess the impact of social distancing policies on non–severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) respiratory pathogens typically circulating across multiple US states.
Methods
Linear mixed-effect models were implemented to explore the effects of 5 social distancing policies on non-SARS-CoV-2 respiratory pathogens across 9 states from January 1 through May 1, 2020. The observed 2020 pathogen detection rates were compared week by week with historical rates to determine when the detection rates were different.
Results
Model results indicate that several social distancing policies were associated with a reduction in total detection rate, by nearly 15%. Policies were associated with decreases in pathogen circulation of human rhinovirus/enterovirus and human metapneumovirus, as well as influenza A, which typically decrease after winter. Parainfluenza viruses failed to circulate at historical levels during the spring. The total detection rate in April 2020 was 35% less than the historical average. Many of the pathogens driving this difference fell below the historical detection rate ranges within 2 weeks of initial policy implementation.
Conclusions
This analysis investigated the effect of multiple social distancing policies implemented to reduce transmission of SARS-CoV-2 on non-SARS-CoV-2 respiratory pathogens. These findings suggest that social distancing policies may be used as an impactful public health tool to reduce communicable respiratory illness.
Keywords: coronavirus, COVID-19, intervention, respiratory, social distancing
Acute respiratory infections are associated with significant mortality and societal disruption. Influenza accounts for ~20 000 deaths annually in the United States and has been as high as 80 000 deaths in recent years [1, 2]. Noninfluenza respiratory infections lead to ~$40 billion annually in direct and indirect costs in the United States due to missed work and health care treatment [3]. The COVID-19 pandemic illustrates these negative impacts at epic proportions. As of March 2021, >515 000 US deaths are attributed to COVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [4]. In the second quarter of 2020, the US economy experienced a 31% decrease in real GDP [5].
To reduce transmission and population exposure to SARS-CoV-2, the initial focus of the US public health response was to implement numerous social distancing policies. While COVID-19 was the impetus for imposing these policies, it is not the only respiratory disease affected by their implementation. The wide-scale adoption of multiplex diagnostic tests and pathogen surveillance platforms, such as BioFire Syndromic Trends, enables the analysis of respiratory diseases throughout the pandemic [6, 7]. While there may be many contributing factors that affect respiratory disease incidence, the initial interventions to prevent the spread of SARS-CoV-2 provide a unique opportunity to evaluate their secondary effects on non-SARS-CoV-2 pathogens.
Previous studies examined the effects of social distancing policies on mobility within a population and the growth rates of COVID-19, concluding that the policies resulted in a measurable decrease for both outcomes [8–15]. Other studies have concluded that the implementation of social distancing policies reduced the incidence of non-SARS-CoV-2 respiratory pathogens such as influenza, respiratory syncytial virus, and Mycoplasma pneumoniae [16–21].
This study aimed to assess the impact of social distancing policies intended to limit the spread of SARS-CoV-2 on non-SARS-CoV-2 respiratory pathogens typically circulating at the time of implementation. This was achieved using current and historical detection rates from a large-scale epidemiological network that includes results from 21 respiratory pathogens across multiple states. Understanding the effects of the policies on non-SARS-CoV-2 respiratory pathogens may better inform future policies to reduce the incidence and societal impacts of respiratory infections.
METHODS
Data
Non-SARS-CoV-2 respiratory pathogen detection rates were acquired from BioFire Syndromic Trends, a cloud-based epidemiological network containing de-identified results from a multiplex diagnostic panel surveying 21 respiratory targets [6]. This diagnostic panel simultaneously tests for adenovirus (AdV), Bordetella pertussis, Bordetella parapertussis, Chlamydia pneumoniae, Mycoplasma pneumoniae, coronaviruses (CoVs) 229E, HKU1, NL63, and OC43, influenza A H1, H1-2009, H3, and influenza A (no subtype), influenza B, human metapneumovirus (hMPV), human rhinovirus/enterovirus (HRV/EV), parainfluenza viruses (PIVs) 1, 2, 3, and 4, and respiratory syncytial virus (RSV). Due to variance in pathogen subtype circulation each year, the bacterial and viral targets were categorized into 9 groups: AdV, bacteria, non-SARS-CoV-2 CoVs, influenza A, influenza B, hMPV, HRV/EV, PIVs, and RSV. Pathogen detection rate was defined as positive counts of a given pathogen group divided by the total number of tests. The total detection rate was calculated as the sum of all pathogen detection rates. Daily detection rates from January 2015 through May 2020 for 9 US states, including California, Colorado, Illinois, Kansas, Michigan, Missouri, Nebraska, New York, and Ohio, were included in these analyses. States chosen were those with 3 or more data-contributing institutions and at least 3 years of data for historical comparisons. National detection rates were calculated by aggregating data from all data-contributing US institutions. Supplementary Table 1 provides a breakdown of the tests per year by state and national totals that were available for this analysis.
Social distancing policies included the following: federal guidelines, foreign travel bans, stay at home orders, bans on large gatherings, public school closures, dine-in restaurant closures, and gym closures. The Foreign Travel Ban occurred on March 11 and banned entry for non-US residents present in the Schengen Area of Europe within 14 days of travel [22]. Federal Guidelines, released on March 16, recommended avoiding social gatherings, halting discretionary travel, and following all local ordinances such as closures of public venues [23]. To combat the data’s highly correlated nature, similar local policies were aggregated into single policy variables describing the proportion of local social distancing policies in effect on a given day. Public school, dine-in restaurant, and gym closures were aggregated to create the single policy variable Public Closures. Bans on gatherings of more than 50 persons and 500 persons were aggregated to create the single policy variable Gatherings Ban. Stay at Home orders implemented by states and counties included shelter-in-place orders [24]. The dates of social distancing policies implemented from January through April 2020 were acquired at the county level for the 9 states [24]. County-level policy implementation dates were averaged to calculate a single state implementation date.
Historical Comparison
National and state-level historical mean detection rates and ranges (minimum rate and maximum rate) were calculated using detection rates from 2015 to 2019 for each epidemiological week. The observed 2020 detection rates were compared week by week with the historical rates to determine deviations from historical values. The Deviation Week was marked as the first of 3 consecutive weeks in which the 2020 rate fell below its respective historical range.
Additionally, to assess the impact of BioFire test utilization on pathogen detection rates, 2020 weekly test counts were calculated as a proportion of 2019 weekly test counts. The same 2020–2019 comparison was performed for weekly positive tests.
Model
Linear models have been previously used to assess the impact of policy effects on COVID-19 rates and mobility [8, 12–15]. Linear mixed-effect models were built for each pathogen group detection rate and total detection rate using state-level rates from January 1 through May 1, 2020. The 5 policy groupings were included as fixed effects: Foreign Travel Ban, Federal Guidelines, Public Closures, Gatherings Ban, and Stay at Home. States were included as a random intercept to control for variability between states and to assess the impact of the policies themselves. A linear temporal effect was included to account for nonpolicy effects across states, such as growing awareness of the emerging pandemic. For each pathogen group, and the total detection rate, the model is:
where is the daily (t) detection rate in a state (s), is the coefficient of a social distancing policy (p) for a state, is a proportion within a given policy grouping describing how many social distancing policies are in effect on a given day, is the coefficient of the temporal component, is the temporal component incrementing from 0 to 1 over the analysis time frame, is the random intercept of a state, and is the error. Models were implemented in Python using the statsmodel, version 0.10.1, package.
Due to the range of pathogen incubation periods and the potential delay for testing, the analysis investigated 1-week and 2-week lags [25]. Models were therefore built with no lag, a 1-week lag, and a 2-week lag.
Policy effects on detection rates were assessed by examining the policy coefficients from all models. Each coefficient represents the shift from the mean detection rate, given that everything else is held constant in the model. A policy grouping effect was considered statistically significant if the policy coefficient’s 95% CI did not overlap with 0. Model performance was evaluated using the coefficient of determination, R2.
RESULTS
Historical Comparison
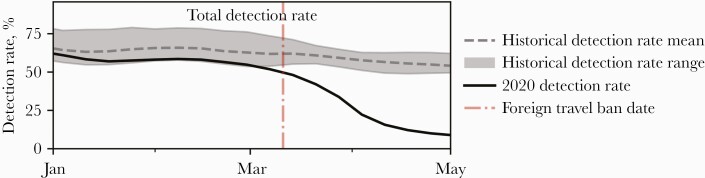
Decreases in national total detection rate and in many pathogen detection rates were seen in March and April 2020 (Supplementary Figure 1). Comparisons of national historical and 2020 total detection rate and pathogen group detection rates are shown in Figures 1 and 2, respectively. The national total detection rate was within the historical range in the weeks before the Foreign Travel Ban implementation on March 11, 2020, and exhibited a reduction in subsequent weeks (Figure 1). Both the national and state detection rates’ Deviation Weeks, compared with the Foreign Travel Ban, are outlined in Supplementary Table 2.
Figure 1.
National historical and 2020 total detection rates. The range surrounding the historical rates is from 2015 through 2019.
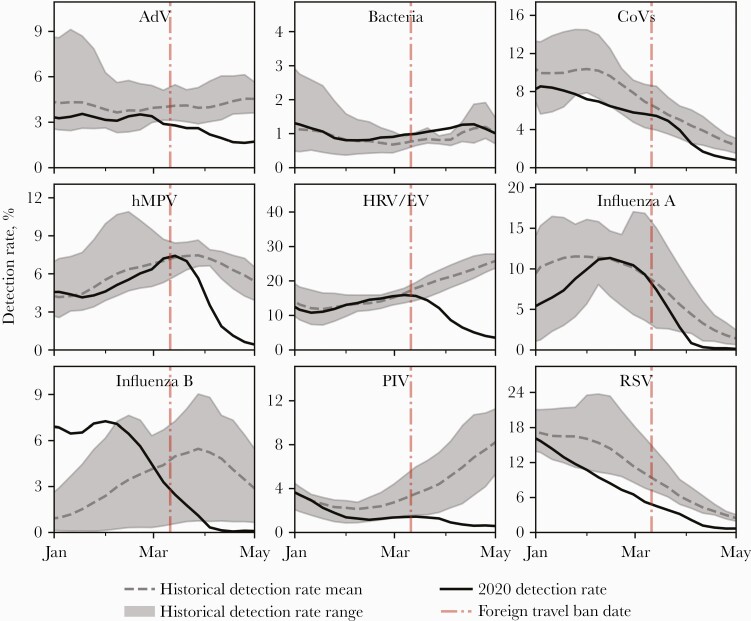
Figure 2.
National historical and 2020 detection rates between January and May for non-SARS-CoV-2 pathogens. The ranges surrounding the historical rates are from 2015 through 2019. Abbreviations: AdV, adenovirus; CoVs, coronaviruses; hMPV, human metapneumovirus; HRV/EV, human rhinovirus/enterovirus; PIV, parainfluenza virus; RSV, respiratory syncytial virus; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Based on observed Deviation Weeks, the decrease in the national total detection rate may be attributed to decreases in AdV, hMPV, and HRV/EV, as well as the lack of an increase in PIV (Figure 2). The detection rates for AdV and PIV decreased nationally during the week preceding the Foreign Travel Ban’s implementation. Conversely, HRV/EV and hMPV detection rates both deviated within 2 weeks after the policy implementation.
Non-SARS-CoV-2 CoVs, influenza A, and RSV had detection rates that fell outside their historical range during the time of the analysis. Influenza B also fell outside its historical range but had increased detection rates earlier than in past years. Bacteria was the only group with consistent national detection rates through the time frame of the analysis (Figure 2).
During the time frame investigated, all 9 states included in the model had total detection rate decreases. Mean state-level mobility also decreased in all states during this time. State total detection rates, mean state population mobility, and policy implementation dates can be found in Supplementary Figure 2. As reported by Deviation Weeks, the departures of California, Kansas, Nebraska, and New York from the state historical total detection rate range occurred within a week of the Foreign Travel Ban. Both Colorado’s and Ohio’s Deviation Week for state total detection rate was many weeks earlier than the Foreign Travel Ban, due in part to reduced overall total detection rates for the 2019–2020 season.
State-level Deviation Weeks for many pathogen detection rates were also observed. HRV/EV decreased within 3 weeks of the Foreign Travel Ban in all investigated states except Colorado. Further, hMPV’s and PIV’s Deviation Weeks occurred within a month of the Foreign Travel Ban in many states.
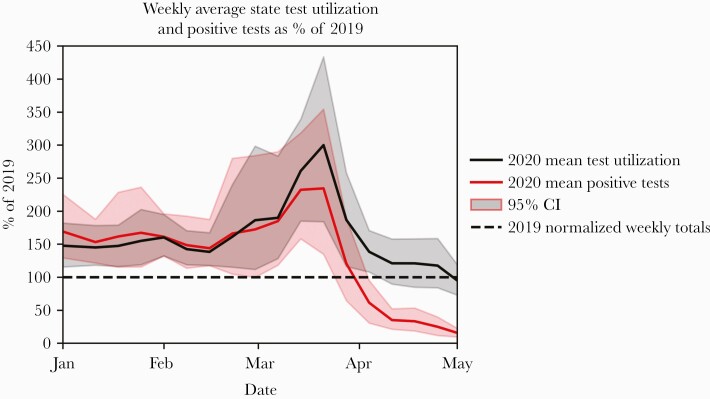
National test utilization in early 2020 was nearly 150% of 2019 test utilization until reaching 300% in March (Figure 3). By May 2020, test utilization had returned to 2019 levels. Weekly positive test counts in 2020 were ~150% of 2019 until reaching close to 250% in March. By May 2020, weekly positive test counts dropped to ~15% of 2019 values.
Figure 3.
The proportion of 2020 weekly BioFire test counts compared with 2019 for all tests run and positive tests. The average weekly rate of all states is plotted, with a 95% CI.
Model
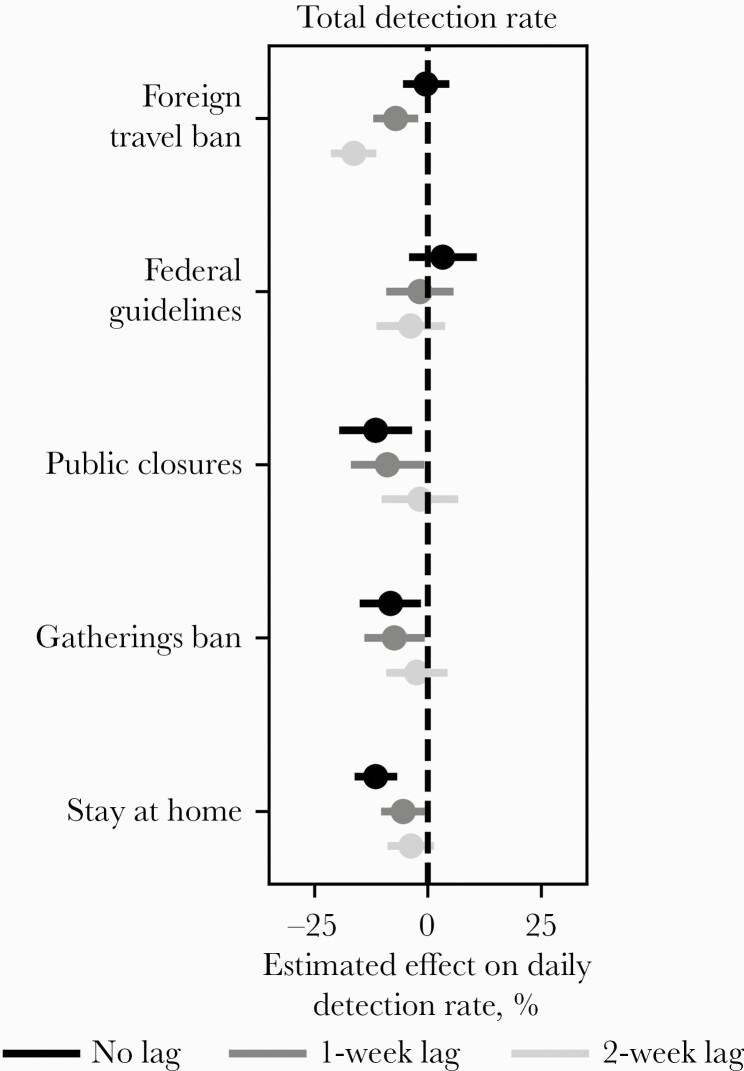
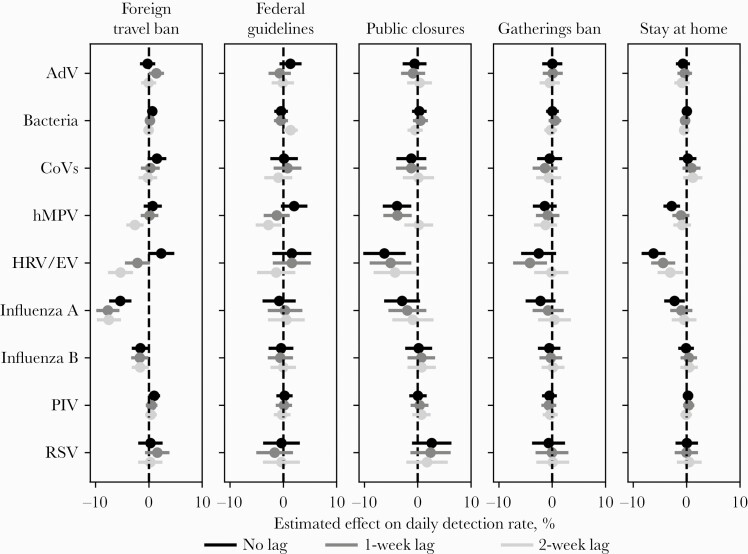
The effects of social distancing policies on non-SARS-CoV-2 respiratory pathogen detection rates were estimated using linear mixed-effect models. Figure 4 outlines the policies’ mean effect sizes on total detection rate and 95% CI. By including the temporal effect, policy effect sizes are measures of the change in the slope of the pathogen rate. Positive effects suggest an increase in total detection rate potentially associated with a given policy, while negative effects indicate decreases. Individual social distancing policies decreased the total detection rate, in some cases by nearly 15%. The 1-week lag yielded the best model fit, with the highest R2 value, for total detection rate. Supplementary Table 3 presents R2 values for all models and pathogens. Except for the Federal Guidelines, all policies had a statistically significant negative effect for the 1-week lag model. The temporal effect on the total detection rate for all 3 models was statistically significant; however, the effect size is largely dependent upon the scaling. Therefore, it is not meaningful to compare the temporal effect size with the policy effects. Model results for all pathogen groups may be found in Figure 5, while results for individual pathogens may be found in Supplementary Figure 3. HRV/EV and hMPV were both negatively affected by Stay at Home orders and Public Closures. Policies were not significantly associated with a change in the detection rate of PIV, a pathogen normally circulating in the spring and the fall. The Foreign Travel Ban did have a statistically significant effect on pathogens typically circulating in winter months, specifically influenza A.
Figure 4.
Effects of the social distancing policies on total detection rate without a lag (black) and with a 1-week and 2-week lag (dark gray and light gray, respectively). Center points with 95% CIs represent the mean estimated effect on total detection rate. CIs were Bonferroni-corrected to account for multiple comparisons across models.
Figure 5.
Effects of the social distancing policies on pathogen group detection rates without a lag (black) and with 1-week and 2-week lags (dark gray and light gray, respectively). Center points with 95% CIs represent the mean estimated effect on total detection rate. CIs were Bonferroni-corrected to account for multiple comparisons across models. Abbreviations: AdV, adenovirus; CoVs, coronaviruses; hMPV, human metapneumovirus; HRV/EV, human rhinovirus/enterovirus; PIV, parainfluenza virus; RSV, respiratory syncytial virus; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
DISCUSSION
During March and April 2020, the detection rates of many respiratory pathogens dropped below historical ranges. Linear mixed-effect models were implemented to explore the effects of social distancing policies on these non-SARS-CoV-2 respiratory pathogen detection rates. Policy groupings included Foreign Travel Ban, Federal Guidelines, Public Closures, Gatherings Ban, and Stay at Home orders. The models were limited to January through April 2020. A temporal effect was included to account for societal changes during this time frame, such as increasing awareness of the pandemic, media coverage, and public health messaging. After accounting for temporal effects, significant policy effects were observed. Model results indicated that social distancing policies may have decreased the total detection rate and the detection rates of many springtime viruses such as HRV/EV and hMPV. Other seasonal viruses such as influenza A exhibit accelerated decreases at the end of winter.
The decreases may be due to the policies’ secondary effects on population mobility. All investigated states experienced decreases in mobility during the time frame in which the social distancing policies were implemented (Supplementary Figure 2), suggesting population adherence to the policies. Previous studies have shown that social distancing policies led to voluntary social distancing that reduced mobility [14]. Voluntary social distancing may also explain the Foreign Travel Ban’s significant effect on pathogens endemic within the United States as the number of domestic US passengers decreased by 51% in March 2020 compared with March 2019, while the number of US international passengers decreased by 53% during the same time frame [26]. Media coverage of SARS-CoV-2 may have been an additional factor contributing to increases in voluntary social distancing [27]. Distinguishing between the effects of Federal Guidelines, the Gatherings Ban, and Public Closures was difficult as they were implemented within a narrow time frame and had some overlap in recommendation components. Additionally, New York and Michigan implemented state-wide mask mandates on April 15 and 26, respectively [28, 29]. Because these were implemented toward the end of the study period, mask mandates were excluded from the analysis. These nonpolicy effects, such as voluntary social distancing, social awareness, and early mask usage, are accounted for in the model with the inclusion of the temporal effect.
While the impact of the social distancing policies can be seen in both the historical comparison and model results for HRV/EV and hMPV, the relationship between the 2 analyses is more nuanced for other pathogens. The models showed negative effects of the Foreign Travel Ban on influenza A, a pathogen expected to decline in the spring. RSV and CoVs, however, did not have strong evidence of policy effects because the slope of the detection rate remained consistent during the time frame. Compared with historical rates, influenza A, influenza B, RSV, and CoV detection rates started near the average levels and dropped below the historical minimum, suggesting a practical impact of the policies. PIV, which frequently circulates in the spring, remained consistently low after policies were implemented. While this suggests that the policies may have practically impacted the PIV detection rate, the model results did not have strong evidence of policy effects.
A number of factors may affect pathogen prevalence, including normal seasonal variations and pathogen interactions. Although some respiratory pathogens, such as AdV, tend to circulate consistently throughout the year, many circulate annually or semiannually, with the prevalence and dominant strains varying from year to year [6]. These effects can be seen in the model results of all 21 pathogens (Supplementary Figure 3), where significant policy effects are noted for influenza A H1-2009, the influenza A subtype primarily circulating in the 2019–2020 season. Further, influenza B circulated earlier than expected in the 2019–2020 respiratory season, peaking in January rather than April as in previous years.
Several studies have suggested that the presence of 1 pathogen may deter a secondary pathogen infection, as was observed with the disappearance of seasonal influenza and delayed onset of RSV during the 2009 influenza A H1N1 pandemic [30–33]. Another study found that the presence of HRV interfered with influenza A infections by stimulating an immune response [34]. Conversely, studies have suggested that infection with 1 pathogen may also encourage opportunistic secondary infections [32, 35, 36]. During this study period, the BioFire System did not contain a SARS-CoV-2 assay, which made it challenging to assess pathogen interactions. However, the HRV/EV detection rate and the COVID-19 incidence rate began increasing nationally in August 2020 while COVID-19 positivity decreased. The increase in both HRV/EV and COVID-19 cases may have been more related to increased social mobility/re-opening and less suggestive of pathogen interactions (Supplementary Figure 4). Additional research is needed to determine if and to what extent SARS-CoV-2 interferes with seasonal respiratory viruses after data are available from the 2020–2021 respiratory season.
A limitation of this investigation was the restricted resolution into institutions’ testing procedures and testing algorithms. To rule out the use of testing as a confounder, the proportions of 2020 weekly tests run as well as 2020 weekly positive tests compared with 2019 were evaluated. The increase in early 2020 national test utilization from 150% to nearly 300% may have been due to BioFire test use as a rule-out diagnostic for COVID-19 while the availability of COVID-19 tests was still limited [37, 38]. However, the change in test utilization was not proportional to the rapid decrease in detection rates. Additionally, weekly positive tests increased between January and March of 2020 before drastically decreasing in April, suggesting that the decreases in detection rates may be due to declining pathogen circulation rather than solely an increase in testing.
An additional limitation of this analysis is the time frame over which pathogen detection rates were being investigated. A prior study suggests that M. pneumoniae may be affected by social distancing policies [21]. However, when looking at individual bacteria (Supplementary Figure 5), no detection rate decline was seen during the time frame investigated. B. pertussis, C. pneumoniae, and M. pneumoniae detection rates did decrease in the second half of 2020. The decreases’ potential connections to social distancing policies will be investigated in a further analysis.
A similar decrease in detection rates was apparent for communicable gastrointestinal viruses (Supplementary Figure 6). Between the beginning of March and the end of April, there was an 82% decrease in combined detection rates of adenovirus, astrovirus, norovirus, rotavirus, and sapovirus. Gastrointestinal bacterial pathogen detection rates did not decrease. This suggests that the social distancing policies during the COVID-19 pandemic may be associated with declines in viral pathogens of nonrespiratory syndromes.
While social distancing policies were implemented to reduce transmission of SARS-CoV-2, their implementation was effective at decreasing detection rates for non-SARS-CoV-2 respiratory pathogens. This analysis investigated the effects of social distancing policies on respiratory pathogens in 9 US states and identified multiple policies that may have resulted in a decrease in pathogen circulation. When spring 2020 rates were compared against the historical averages, there was a significant decline in detection rates. These findings suggest that social distancing measures may be an impactful public health tool for reducing the incidence and burden of communicable respiratory illness. Further research should evaluate the effects of social distancing fatigue, states re-opening, and the long-term effects of the COVID-19 pandemic on respiratory disease.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
Potential conflicts of interest. J.N., K.O., J.H., L.M., C.C., M.P., C.V.C., J.J., T.R., A.H., and C.C.G. are present or former employees of bioMérieux, Inc., or its subsidiaries. bioMérieux markets the BioFire System and Syndromic Trends. M.C.H. is a paid consultant of BioFire Diagnostics, LLC. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Patient consent. The data from Syndromic Trends used in this study are de-identified according to HIPAA standards. Additionally, BioFire enters into a Data Use Agreement with each institution to protect against re-identification of any individual and to control the use of the data. Therefore, patient consent was neither required nor applicable due to the nature of this study.
Data access. The data used in this study have been aggregated to further protect both the privacy of the patient for publication and the identity of the contributing institutions. Access to the data used in the study may be made available upon request, subject to applicable privacy restrictions.
References
- 1. Thompson MG, Shay DK, Zhou H, et al. Estimates of deaths associated with seasonal influenza united states, 1976–2007. Morb Mortal Wkly Rep 2010; 59:1057–62. [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Estimated Influenza Illnesses, Medical visits, Hospitalizations, and Deaths in the United States—2017–2018 Influenza Season. Atlanta: Centers for Disease Control and Prevention; 2018.
- 3. Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non–influenza-related viral respiratory tract infection in the United States. Arch Intern Med 2003; 163:487–94. [DOI] [PubMed] [Google Scholar]
- 4. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020; 20:533–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bureau of Economic Analysis. Gross domestic product (third estimate), corporate profits (revised), and GDP by industry, second quarter 2020. 2020. Available at: https://www.bea.gov/news/2020/gross-domestic-product-third-estimate-corporate-profits-revised-and-gdp-industry-annual. Accessed 9 July 2020.
- 6. Meyers L, Ginocchio CC, Faucett AN, et al. Automated real-time collection of pathogen-specific diagnostic data: syndromic infectious disease epidemiology. JMIR Public Heal Surveill 2018; 4:e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meyers L, Dien Bard J, Galvin B, et al. Enterovirus D68 outbreak detection through a syndromic disease epidemiology network. J Clin Virol 2020; 124:104262. [DOI] [PubMed] [Google Scholar]
- 8. McCafferty S, Ashley S. Covid-19 social distancing interventions by state mandate and their correlation to mortality in the United States. medRxiv 2020.08.26.20182758v1 [Preprint]. 1 September 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.08.26.20182758v1. Accessed 9 July 2020. [Google Scholar]
- 9. Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020; 584:262–7. [DOI] [PubMed] [Google Scholar]
- 10. Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis 2020; 26:1740–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang X, Pasco RF, Du Z, et al. Impact of social distancing measures on coronavirus disease healthcare demand, Central Texas, USA. Emerg Infect Dis 2020; 26:2361–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Courtemanche C, Garuccio J, Le A, et al. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff 2020; 39:1237–46. [DOI] [PubMed] [Google Scholar]
- 13. Canning D, Karra M, Dayalu R, Guo M, Bloom DE. The association between age, COVID-19 symptoms, and social distancing behavior in the United States. medRxiv 2020.04.19.20065219 [Preprint]. 23 April 2020. Available at: http://medrxiv.org/content/early/2020/04/23/2020.04.19.20065219.abstract. Accessed 9 July 2020.
- 14. Abouk R, Heydari B. The immediate effect of COVID-19 policies on social-distancing behavior in the United States. Public Health Rep 2021; 136:245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wellenius GA, Vispute S, Espinosa V, et al. Impacts of US state-level social distancing policies on population mobility and COVID-19 case growth during the first wave of the pandemic. arXiv 2004.10172 [Preprint]. 21 April 2020. Available at: http://arxiv.org/abs/2004.10172. Accessed 1 December 2020.
- 16. Kuo S-C, Shih S-M, Chien L-H, Hsiung CA. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg Infect Dis 2020; 26:1928–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wu D, Lu J, Liu Y, Zhang Z, Luo L. Positive effects of COVID-19 control measures on influenza prevention. Int J Infect Dis 2020; 95:345–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yeoh DK, Foley DA, Minney-Smith CA, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian Winter. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nolen LD, Seeman S, Bruden D, et al. Impact of social distancing and travel restrictions on non–coronavirus disease 2019 (non–COVID-19) respiratory hospital admissions in young children in Rural Alaska. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Friedrich F, Ongaratto R, Scotta MC, et al. Early impact of social distancing in response to COVID-19 on hospitalizations for acute bronchiolitis in infants in Brazil. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa1458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oster Y, Michael-Gayego A, Rivkin M, et al. Decreased prevalence rate of respiratory pathogens in hospitalized patients during the COVID-19 pandemic: possible role for public health containment measures? Clin Microbiol Infect 2021; 27:811–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Trumph D. Presidential proclamations on novel coronavirus. Proclamation No. 9993, 85 FR 15045. 2020. Available at: https://travel.state.gov/content/travel/en/News/visas-news/presidential-proclamation-coronavirus.html. Accessed 15 October 2020.
- 23. Trumph D. The President’s coronavirus guidelines for America. 2020. Available at: https://trumpwhitehouse.archives.gov/briefings-statements/coronavirus-guidelines-america/. Accessed 15 October 2020.
- 24. Killeen BD, Wu JY, Shah K, et al. A county-level dataset for informing the United States’ Response to COVID-19. arXiv 2004.00756 [Preprint]. 1 April 2020. Available at: http://arxiv.org/abs/2004.00756.
- 25. Lessler J, Reich NG, Brookmeyer R, et al. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis 2009; 9:291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bureau of Transportation Studies. Preliminary Air Traffic Data, April 2020: 96% reduction in U.S. airline passengers from 2019. 2020. Available at: https://www.bts.gov/newsroom/preliminary-air-traffic-data-april-2020-96-reduction-us-airline-passengers-2019. Accessed 1 March 2020.
- 27. Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Heal Psychol 2020; 39:355–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weixel N. New York to require all people to wear masks when in public. The Hill. 15 April 2020. Available at: https://thehill.com/policy/healthcare/492967-new-york-to-require-all-people-to-wear-masks-when-in-public. Accessed 9 July 2020. [Google Scholar]
- 29.FOX59 Web. Face mask orders, eased restrictions: here’s where stay-at-home orders stand in Indiana’s surrounding states. FOX 59. 24 April 2020. Available at: https://fox59.com/news/coronavirus/face-mask-orders-eased-restrictions-heres-where-stay-at-home-orders-stand-in-indianas-surrounding-states/. Accessed 9 July 2020.
- 30. Greer RM, McErlean P, Arden KE, et al. Do rhinoviruses reduce the probability of viral co-detection during acute respiratory tract infections? J Clin Virol 2009; 45:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schultz-Cherry S. Viral interference: the case of influenza viruses. J Infect Dis 2015; 212:1690–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kumar N, Sharma S, Barua S, et al. Virological and immunological outcomes of coinfections. Clin Microbiol 2018; 31:e00111-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Casalegno JS, Ottmann M, Bouscambert-Duchamp M, et al. Impact of the 2009 influenza A(H1N1) pandemic wave on the pattern of hibernal respiratory virus epidemics, France, 2009. Euro Surveill 2010; 15:19485. [PubMed] [Google Scholar]
- 34. Wu A, Mihaylova VT, Landry ML, Foxman EF. Interference between rhinovirus and influenza A virus: a clinical data analysis and experimental infection study. The Lancet Microbe 2020; 1:e254–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McNamee LA, Harmsen AG. Both influenza-induced neutrophil dysfunction and neutrophil-independent mechanisms contribute to increased susceptibility to a secondary Streptococcus pneumoniae infection. Infect Immun 2006; 74:6707–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Goto H, Ihira H, Morishita K, et al. Enhanced growth of influenza A virus by coinfection with human parainfluenza virus type 2. Med Microbiol Immunol 2016; 205:209–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Johnson M. Commercial coronavirus test developers tweak timelines, EUA plans in light of loosened FDA guidance. genomeweb. 20 March 2020. Available at: https://www.genomeweb.com/pcr/commercial-coronavirus-test-developers-tweak-timelines-eua-plans-light-loosened-fda-guidance#.XwdYvChKjQA. Accessed 28 September 2020.
- 38. LabCorp. LabCorp launches test for coronavirus disease 2019 (COVID-19). 2020. Available at: ir.labcorp.com. Accessed 9 July 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.