Abstract
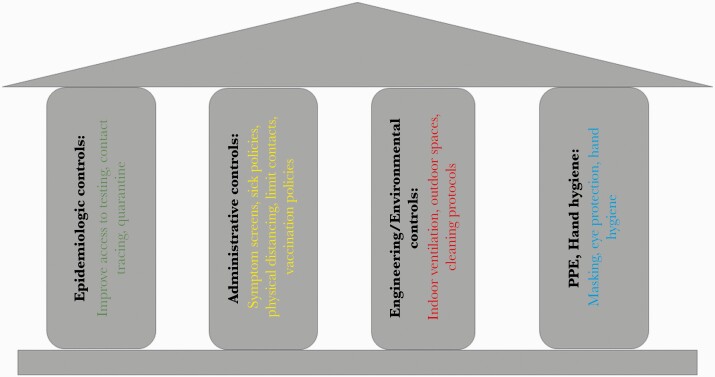
There are limited tools for adapting coronavirus disease 2019 (COVID-19) infection control plans to school settings. We present an infection prevention model for optimizing safe re-opening for elementary and secondary schools during the global COVID-19 pandemic and review the current evidence behind various infection prevention interventions in school settings. The model is adapted from the Centers for Disease Control and Prevention fundamental pillars for infection prevention and includes 4 categories of intervention: epidemiologic controls (town prevalence metrics, diagnostic testing, quarantine strategies), administrative controls (state vaccination policies, alternative school models, symptom screens, quarantine breaks), engineering/environmental controls (distancing, outdoor space, ventilation), and personal protective equipment (PPE)/hand hygiene (face coverings, hand sanitizing).
The adapted infection control pillars model utilizes implementation science–informed considerations to maximize pragmatism and adherence by leveraging evidence-based strategies. It highlights the necessity of redundant infection prevention interventions, acknowledges the importance of community buy-in to achieve real-world effectiveness, and addresses tactics to overcome implementation barriers. Recommendations are grounded in the Dynamic Sustainability Framework and include suggestions to maintain infection prevention effectiveness over time to ensure ongoing safety.
Keywords: COVID-19, infection prevention, implementation science
Due to time-sensitivity of the research, the editors ask that no embargo be placed on the accepted MS. Remove Editor's Choice and promotion if necessary to proceed with expedited publication. Editorial Office will try to get summary quickly and pass on later.
Schools are a critical part of societal infrastructure, with closures estimated to cost between $10 and $47 billion per month in 2009 dollars [1]. Since March 2020, coronavirus disease 2019 (COVID-19) has disrupted education across the United States. Primary and secondary schools were abruptly closed, and in 48/50 states they remained closed for the duration of the academic year [2]. At their peak, the closures affected at least 55.1 million students in 124 000 US public and private schools [3]. During the 2020/2021 academic year, many districts remain fully remote or in a hybrid model in which students are not fully in person for their education [4]. Women, particularly mothers of elementary school-aged children and women of color, are disproportionally impacted by school closing policies, due to a variety of factors, including lack of child care, the need to supervise remote education, and concerns about how they will be judged in the workplace [5]. These factors, among others, have led to women disproportionally exiting the workforce, furthering gender disparities [6].
Since the policy change was implemented in March 2020, negative impacts of school closures on children, particularly underprivileged students, have been increasingly reported, both in academic journals and in the lay press [7–10]. Primary and secondary students who are placed in remote models or partially in-person (hybrid) models are falling behind academically, as evidence increasingly demonstrates failure to achieve basic literacy and other key academic milestones [11, 12]. Rates of childhood obesity and psychiatric illness in children and adolescents are on the rise, and recent reports suggest a pandemic of mental health concerns, particularly among older students [13–17].
Initially, policies about opening schools in many districts appeared to be centered on the hope that a safe and effective vaccine would be rapidly identified, with schools remaining closed until herd immunity was achieved through a nationwide mass vaccination campaign. However, the vaccine-based strategy will not be sufficient for the 2020/2021 school year, and as children aged <16 years have not yet been part of large-scale studies, they will not be vaccinated by the start of the 2021/2022 year, rendering this strategy insufficient for next year as well [18]. Thus, it is critical that as we pursue a vaccination-based strategy to facilitate a safe return to school, we also consider the evidence supporting other infection prevention strategies in parallel to inform policy decisions about strategies to optimize the safety of school re-opening in a practical and feasible manner.
Several guideline-issuing bodies have published recommendations about optimizing COVID-19 prevention in school settings, including the World Health Organization [19], the Centers for Disease Control and Prevention (CDC) [20, 21], and the American Academy of Pediatrics [22]. Each of these sets of recommendations emphasizes the importance of in-person education and delineates general severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection control principles adapted for school settings. In December 2020, the CDC updated its recommendations and stated that schools should be the last to close and the first to open—a critical and important policy change, indicating the importance of in-person learning [23]. However, available guidelines lack detail about the specifics of how to implement infection prevention strategies [24], creating challenges for school districts that must individually develop their own policies and procedures, while accounting for local barriers that may be specific to their own district, or even school building.
Well-established infection control principles can be applied and adapted to nontraditional settings, including school buildings. Experiences in other countries and districts that developed strategies for opening classrooms to in-person learning during the pandemic can be used to inform best practices to support the safest possible elementary and secondary school re-opening.
Here, we present an adapted infection prevention model for optimizing a safe re-opening for in-person learning in the setting of the global SARS-CoV-2 pandemic for elementary and secondary schools, highlighting different infection prevention strategies and the evidence behind these strategies for implementation and adaption in school settings. The model is based on the CDC’s Fundamental Pillars for Infection Control Model [25], is grounded in the Dynamic Sustainability Framework [26], and leverages evidence-based implementation strategies (Figure 1) [27]. The Dynamic Sustainability Framework provides a foundation for research, policy, and practice that supports development and testing of falsifiable hypotheses and continued learning to advance the implementation, transportability, and impact of health services research [26]. The implementation science–informed model [28] includes consideration of acceptability, feasibility, and sustainability, and the proposed plans are designed to be pragmatic and adaptable as data about COVID-19 in school settings continue to evolve. In line with principles of implementation science, cost and feasibility at the local school district level are considered, and the evidence supporting different interventions is reviewed.
Figure 1.
The infection control pillars for elementary and secondary schools.
THE ROLE OF SCHOOLS IN THE COVID-19 PANDEMIC
In March 2020, based on information extrapolated from influenza transmission models, schools were closed as a strategy to reduce community transmission of COVID-19 [29]. Since that time, data increasingly support the finding that children are less likely to become critically ill from COVID-19 [30]. Additionally, although the magnitude of the role of children and schools in the spread of COVID-19 remains controversial, children and schools do not appear to be the primary driver of the pandemic [31]. Thus, the impact of school closing for controlling community COVID rates is likely not as great as the impact on closing schools for influenza control. Empiric data from regions in the United States and other countries that have subsequently re-opened schools suggest that, in regions and districts with low community prevalence, schools that implement mitigation measures do not have high rates of within-school COVID-19 transmission, although the risk is not 0 [32–36]. Surveillance testing in New York City suggests that in-school rates may in fact be lower than in surrounding communities [37]. In regions with high community prevalence, in-person schooling with mitigation measures still may be safer than the unregulated environment that results from lack of structured in-person education and lack of supervision. For example, a recent case–control study from Mississippi found that children who became infected with SARS-CoV-2 were more likely to have had attended gatherings with persons outside their household, including activities with other children, or to have had visitors in their home when compared with children who had not participated in these activities. Notably, attendance of in-person school 14 days before infection was not identified as a risk factor for SARS-CoV-2 infection [38]. The balance of evidence suggests that, with appropriate mitigation measures, transmission within school buildings can be minimized [39–41].
THE PILLARS OF INFECTION CONTROL
Within infection control, there are several different classes of infection prevention interventions, previously described in the CDC Pillars of Infection Control Model, developed to guide responses to the H1N1 influenza pandemic (URL no longer active); these include epidemiologic controls, administrative controls, engineering/environmental controls, and personal protective equipment (PPE) and hand hygiene. Ideally, infection control plans leverage interventions in each 1 of these categories and include redundancy, such that there is never reliance on only 1 infection control intervention to mitigate spread of infectious diseases.
EPIDEMIOLOGIC CONTROLS
Epidemiologic controls are interventions designed to decrease the likelihood of cases of COVID-19 entering the building by focusing on the community around the school, as well as improving detection and early quarantining of cases to limit disease spread. Various epidemiologic controls for elementary and secondary settings with in-person learning include testing, contact tracing, and quarantining strategies.
The first line of defense in preventing the spread of SARS-CoV-2 within school buildings is controlling the spread of SARS-CoV-2 in community settings. When community incidence is low, there is a correspondingly low probability that an infectious individual will enter a school building, thereby limiting transmission risk independent of any interventions adopted in school settings. In addition, when community case rates are low, few students and staff require quarantining, as they are less likely to be exposed to known cases, limiting the impact of infections on attendance and school staffing.
Since early in the pandemic, guidelines have utilized closing and re-opening metrics based on rates of positive tests in the community surrounding a school or total number of cases/10 000 persons in the past 7 days [21, 42, 43]. However, there is no consensus on which metrics should be used and what thresholds to set. As data have continued to evolve, scientific evidence suggests that the initially conservative metrics may be substantially relaxed, completely re-imagined, or removed entirely. Initially, the state of Massachusetts set a closure threshold of 5%, and New York City 3% [44, 45]. France kept schools open despite an 11% test positivity rate in the community [46]. Relaxation of closure thresholds is also supported by recent data from Italy, which found very low rates of transmission in day care settings and elementary schools; the only large cluster occurred in a secondary school setting [47].
From a practical standpoint, when the force of infection gets high due to community prevalence, it may be necessary for schools to close for in-person learning, due to either in-school transmission or inability to adequately staff a school building due to cases acquired outside of school, but impacting operations inside of schools.
Case ascertainment, with contact testing and quarantine if cases are identified, is a cornerstone of COVID-19 epidemiologic control [48]. Districts should develop plans to facilitate accessible and affordable COVID-19 diagnostic testing, with a rapid turnaround time, for students and staff members who require testing in order to guide decisions about quarantining and staffing [49]. Ideally, testing should be accessible to cohort members of positive index cases as well, and these data should drive decisions about cohort and school quarantines. These measures are most effective when supported by resources outside the school system.
Beyond diagnostic testing, surveillance testing to identify asymptomatic cases is also a consideration, particularly for teachers and adolescent students, though there is no evidence that surveillance testing is essential for safe re-opening. Models for surveillance testing within schools could include partnering with local health care facilities or public–private partnerships with outside vendors to provide testing, as was successfully piloted in Wellesley, Massachusetts, although the cost of this program limits its practicality for widespread dissemination if additional resources are not made available to public school districts [50]. Recently the state of Massachusetts made pooled surveillance testing available to all public school districts state-wide for students and staff, with significant financial and logistical support [51]. Unless state or federal governments provide funding for testing, the high costs associated with testing programs may disproportionately impact districts in poorer communities, already more impacted by the pandemic, without the means to support them.
ADMINISTRATIVE CONTROLS
Administrative controls are policies and procedures designed to minimize the risk of exposure. They include governmental and local-level mandates designed to reduce disease transmission.
State-Level
State-level policies are an important administrative control that can support the re-opening of elementary and secondary schools. Phased re-openings, with careful consideration of which services should open, are critical for reducing SARS-CoV-2 spread. In the United States, elementary and secondary schools were not prioritized during the phased re-opening, and other high-risk sectors of the economy, such as indoor restaurants, bars, and casinos, were permitted to open before schools; reconsideration of what is included in which phase is a critical aspect of supporting in-person learning. The CDC update from December changed earlier priority rankings; in this update schools were recommended to be the first to open and the last to close [20, 23]. Within the different school structures, consideration may be given to prioritizing elementary schools, because younger children may be less likely to transmit disease [52], they have the least observed risk of in-school transmission [53], they are least able to participate in self-directed learning, and there is usually only 1 homeroom teacher, resulting in reduced mixing of students and adults. However, although middle and high school models include more moving between classes and more mixing between students and adults, and thus potentially higher risk of COVID-19 transmission when compared with elementary school settings, consideration should also be given to the recent reports of increased mental health concerns, including increasing rates of suicidal behavior in adolescents, when making school opening policy decisions for older students [16, 54].
Mandatory influenza vaccination was implemented in health care settings several years ago as a cost-saving intervention [55]. Similar influenza vaccination policies can be mandated for children and school staff to limit co-infections and minimize testing and quarantining of individuals with symptoms that overlap with COVID-19. The Governor of Massachusetts announced a first-in-the-nation mandatory influenza vaccination policy for all students, with limited exceptions [56]; other states could consider similar mandatory vaccination policies. Those who did not or could not comply with recommended vaccinations were directed to a remote learning model, when available. Given minimal circulating influenza in the community (14 cases reported to the state as of 2/5/2021) [57], Massachusetts removed the influenza vaccine mandate for the 2020/2021 season, though it may require this vaccination again in future seasons.
Local (School District–Level)
To limit the number of potential person-to-person contacts and SARS-CoV-2 exposures, the first administrative control is that only students and essential staff should be permitted into school buildings. This low-cost intervention reduces the number of people entering and exiting and thus reduces the chances that an individual infected with COVID-19 will enter the building, potentially resulting in clusters of infections.
Duration and proximity of contacts impact SARS-CoV-2 transmission [58]; thus, early recommendations highlighted the importance of physical distancing policies. However, the evidence about the effectiveness of distancing as an infection control strategy when implemented in school settings remains unclear. The CDC currently recommends maintaining 6 feet of physical distancing to the extent possible [21], although the quality of evidence to support this recommendation is low. Conversely, the World Health Organization (WHO) recommends 1 meter (3.3 feet) of distance between students [19]. The American Academy of Pediatrics recommends 3–6 feet [59].
Because of the differences in policy recommendations, different countries and regions have adopted different distancing policies (Table 1) [19, 39, 60–64]. These data do not suggest a major difference between regions with 3 vs 6 feet of distance. A recent analysis of data gathered from school districts across Massachusetts found that districts that returned to school at a minimum of 3 feet of distance did not report more cases of COVID-19 among either students or staff than districts that returned to school at a minimum of 6 feet of distance [65]. Although additional direct comparative studies are needed to improve policy decisions, these data suggest that 3 feet of distancing can be adopted without negatively impacting student or staff safety, an important finding as 3 feet of distance is more feasible with existing school infrastructure. Evidence for relaxing distancing recommendations is strongest at the elementary school level. Based on the currently available evidence, it is reasonable to implement different distancing policies for elementary, middle, and high school if other mitigation measures, particularly universal masking, cannot be ensured.
Table 1.
Summary of Evidence of Impact of Physical Distancing in School Settings
| Study/Country | Setting | Study Type | Distancing Intervention | Simultaneous Interventions | Results | Data Source |
|---|---|---|---|---|---|---|
| Netherlands [61, 64] | Primary schools & child care facilities | European Centre for Disease Prevention and Control (ECDC) report, nationwide surveillance | Children ≤12 y did not have to distance 1.5 m from each other or adults; children 13–18 y did not have to distance from each other but had to distance from adults | Masking not recommended | After schools re-opened May 11, 2020, no increase in reproductive number or significant outbreaks, with moderately high notification rates. Children ≤17 y represent 7.3% of cases between Jun 1 and Aug 23, though they comprise 20.7% of the population. No deaths. | National Institute for Public Health and the Environment (RIVM), The European Surveillance System (TESSy) |
| Iceland [61] | Child care institutions & primary care schools | ECDC report, nationwide surveillance | No physical distancing rules; no limitations in activities including sports & music; schools kept open during pandemic | Masking not recommended | Rates of infection in children <15 y remained low compared with rates in older age groups throughout spring term as of Jul 2020. | TESSy |
| Ludvigsson et al. [63, 100], Sweden | Schools & preschools (ages 1–16) | Cohort study, followed all children admitted to ICUs in Sweden, Mar 1–Jun 30, 2020 | Physical distancing was recommended (unclear distance); schools kept open during pandemic | Masking not recommended | Low incidence of severe COVID-19 among school children. Among 1.95 million children, 15 had severe COVID-19 requiring ICU admission (1 per 130K). | Swedish Intensive Care Registry |
| Zimmerman et al. [39], USA | North Carolina K-12 school districts | Cohort study, investigated COVID-19 infection in districts with >90K students & staff open for 9 wk of in-person instruction, Aug 15–Oct 23, 2020 | 6-ft distancing | Mandatory masking for children ≥5 y | 773 community-acquired infections documented. Via contact tracing, health department staff determined 32 school-acquired infections. Within-school infections were rare, with no child-to-adult transmission. | North Carolina Department of Health and Human Services |
| Yung et al. [101], Singapore [62] | Educational settings in Singapore | Cohort study, nationwide surveillance, Feb–Mar 2020 | Students spaced 3–6 ft apart | K-2 children in clusters | Identified only 3 potential transmission incidents in 3 separate educational settings. | Ministry of Health Singapore |
| Macartney et al. [35], Australia New South Wales [102] | 25 schools & early childhood care settings (ECEC) | Cohort study, evaluated SARS-CoV-2 transmission, Jan 25–Apr 9, 2020; schools encouraged distanced learning Mar 23 | Physical distancing unspecified | Advised to consider reduction in class size | In 15 schools & 10 ECEC settings, 12 children & 15 adults attended while infectious with 1448 contacts. 18 secondary cases were identified (attack rate 1.2%). Transmission rates were low. | New South Wales Department of Health |
Society guidance: Centers for Disease Control [20]: space seating/desks ≥6 feet apart when possible; World Health Organization [19]: physical distance ≥1 m; American Academy of Pediatrics [22]: desks should be placed ≥3 feet apart and ideally 6 feet apart.
Abbreviations: AAP, American Academy of Pediatrics; CDC, Centers for Disease Control and Prevention; COVID-19, coronavirus disease 2019; ECEC, early childhood care settings; ECDC, European Centre for Disease Prevention and Control; ICU, intensive care unit; RIVM, National Institute for Public Health and the Environment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TESSy, The European Surveillance System; WHO, World Health Organization.
Multiple countries began to require 3 feet or 1 meter of distance between students [19, 60]. When evidence showed that the distancing policy intervention did not significantly alter in-school spread or risk of transmission to teachers and school staff, some countries eliminated distance requirements completely [61, 64] or transitioned to a “bubble” or cohorting model [60, 62, 66], with small groups of students interacting but keeping the number of different contacts to a minimum. Before fall school re-opening, Northern Ireland changed its distancing guidance of 2 meters to 1 meter between school children, combined with using bubbles to minimize student interaction [67]. Cohorting students in educational settings to minimize interaction may be an effective way to limit disease transmission, and the current evidence for this is displayed in Table 2.
Table 2.
Summary of Evidence of Impact of Cohorting/“Bubble” Formation to Minimize Student Interaction in School Settings
| Study/Country | Setting | Study Type | Cohorting Intervention | Simultaneous Interventions | Results | Data Source |
|---|---|---|---|---|---|---|
| Brandal et al. [103], Norway [60, 62] | Primary schools in Oslo & Viken, grades 1–7 | Cohort study, examined transmission in students who attended school within 48 h with tracing/testing of contacts twice during quarantine period, Aug–Nov 2020 | Established small, fixed groups (15 & 20 maximum class size in primary & middle schools, respectively) | Masks not recommended | Minimal child-to-child (0.9%, 2/234) and child-to-adult (1.7%, 1/58) transmission | Department of Virology at the Norwegian Institute of Public Health, Norwegian Surveillance System for Communicable Diseases |
| Denmark [61, 62] | Child care & primary education settings | European Centre for Disease Prevention and Control (ECDC) report, nationwide surveillance | Split classes into small groups (bubbles) of 10–11 students [7]; first phase re-opening, children ≤12 y, Apr 15, 2020 | Physical distancing 2 m; masks not recommended | Did not report an increase in the reproductive number or detect important school outbreaks after re-opening; published Aug 6, 2020 | The European Surveillance System (TESSy) |
| Ismail et al. [104], England [66] | Early years settings, primary schools, & secondary schools | Cross-sectional analysis, estimated rate of infection & outbreaks during summer half-term, Jun–Jul 2020 | Classes small & separated into distinct social bubbles that perform all activities together and do not mix with other bubbles | Maintain distance as able between children and 2 m between adults | Median daily student attendance 928K. Median of 38K early year settings (age <5), 15.6K primary schools (age 5–11), and 4K secondary schools (age 11–18) open daily. Infections & outbreaks low. 113 single cases of infection, 9 coprimary cases, and 55 outbreaks. | Public Health England |
| Isphording et al. [105], Germany | Schools in all German states | Event study analysis, evaluated effect of end of summer break and school re-opening on pandemic spread, Aug–Sep 2020 | Fixed groups were assigned on classroom or cohort basis, remaining physically separated, often with staggered school start times | Masks mandatory | Three weeks after end of summer breaks, relative numbers of new cases gradually decreased (0.55 cases per 100K inhabitants) in re-opening states relative to those not yet re-opening. | Robert-Koch-Institute |
| Link-Gelles et al. [32], USA | Child care programs in Rhode Island | Cohort study, investigated COVID-19 cases at child care programs, Jun 1–Jul 31, 2020 | Initially maximum 12 persons including staff members in stable groups; increased to 20 persons on Jun 29 | Masks mandatory for adults | 666 of 891 programs re-opened. 33 confirmed child care–associated cases & 19 probable child care–associated cases. 30 cases in children with median age 5 y. 39 cases occurred from mid- to late July when state incidence was increasing. Cases occurred in 29 programs, 20 (69%) of which had a single case without secondary transmission. | Rhode Island Department of Health |
Abbreviations: COVID-19, coronavirus disease 2019; ECDC, European Centre for Disease Prevention and Control; TESSy, The European Surveillance System.
Although data remain limited, it is reasonable to implement physical distancing requirements for higher-risk activities that take place during the course of the school day, such as during mealtimes or mask breaks [22, 68]. For older students inherently at higher risk of transmitting disease and also of severe illness, greater distances for high-risk activities are a consideration until more evidence emerges. To keep school staff safe and limit spread to adults, who are at higher risk of severe complications of infection, adults should maintain at least 6 feet of distance from both students and other school staff at all times, including during breaktimes. Additionally, the impact of a distancing policy needs to be weighed against the negative impacts of the policy, which may preclude many districts from providing full, in-person education.
In early school planning, many US districts implemented hybrid learning structures [69, 70] in order to maintain maximal physical distance between students, as well as to decrease a cohort size that might be considered contact if 1 member is identified as a case. There remains a theoretical concern that hybrid models may paradoxically lead to the highest transmission among school-aged children [71]. This elevated transmission rate may result from the reality that on “off” days, students comingle with students outside of their cohort and that infection control measures implemented outside of the controlled school setting may be less rigorous than those implemented inside of school buildings. As data continue to emerge, it is critical that communities and districts maintain the ability to adapt their plans and to change models to optimize safety.
In-school activities may also have to be adjusted to support education. Choral singing has the potential to spread COVID-19 [72,73], and many school-based clusters have been reported secondary to sports practice and games [74]. Consideration should be given to moving these higher-risk activities outside, where natural airflow provides an additional layer of protection, or to canceling them entirely until additional prevention measures are available.
Presenteeism, or attending work/school when sick, is a major cause of clusters in health care settings [75]. Strategies to reduce presenteeism are critical for maintaining a safe school environment. Policy modifications could include increasing sick pay, providing more robust backup/substitute capabilities so educators do not fear overburdening their colleagues when they call out, or not deducting COVID-19-related absences from the individual’s bank of acquired sick days. Reconsideration of sick-leave policies has been demonstrated in hospital settings to reduce workplace clusters [76].
Symptom screens are a low-cost intervention that may limit presenteeism and therefore transmission [76]. To prevent infected individuals from entering school, before entry, a daily symptom, exposure, and travel screen should be completed by both school staff and students. Leveraging evidence-based implementation strategies [27] to enhance ease of use and promote adoption of this intervention, the screening platform should ideally be integrated into existing school technologic infrastructure. The screening tool should include an evaluation for symptoms potentially consistent with COVID-19, exposure to individuals who have recently tested positive, and out-of-state travel. Individuals who do not pass the screener should be instructed not to participate in in-person education that day and be referred for additional evaluation, either by school nursing services or their personal physician, until cleared to return, which should be in line with current guidelines for clearance from isolation or quarantine [77].
Mandatory “COVID-19 quarantine breaks” built into the school schedule are another consideration. Districts can consider eliminating in-person education for 7–10 days (1 full SARS-CoV-2 quarantine period) after a high-risk period, such as after major holidays. Schedule changes such as these might limit the potential for school-based clusters resulting in unplanned closures, but also must be balanced against the concern that students outside of schools may engage in high-risk activities, jeopardizing the intervention’s utility.
Engineering/Environmental Controls
Engineering and environmental controls, such as leveraging outdoor spaces and opening windows to improve ventilation, are another pillar of COVID-19 risk mitigation. Research suggests that the risk of SARS-CoV-2 transmission in outdoor spaces is substantially lower than in indoor settings, particularly those with poor ventilation [78]. Thus, outdoors spaces should be used, flexibly and to the extent feasible, particularly during warmer parts of the school year. Higher-risk activities, such as those that require mask removal, including eating and instrument or vocal practice, should take place outside whenever possible, to leverage the increased air exchanges inherently provided by outdoor ventilation. To extend the amount of time spent in outdoor spaces, additional infrastructure, such as tents with heating elements, may also be pursued. Although building additional infrastructure is costly in the short run, if outdoor spaces are expanded enough, this might allow many schools to greatly expand in-person learning options, even if distancing requirements are maintained.
Inside the buildings, identifying ways to optimize ventilation by increasing the number of air exchanges in classrooms and considering the use of air purifiers are important considerations. Based on modeling and engineering studies, windows should remain open to the extent feasible during the day, particularly during higher-risk activities, such as during indoor mask breaks and during indoor mealtimes [79, 80]. In colder weather, opening windows even a small amount may provide sufficient air exchanges to reduce viral presence [42]. If windows cannot be opened or there are no windows in a classroom, then air purifiers, such as HEPA filters, are another consideration. However, it is crucial to recognize that these interventions are based on rational—but theoretical—evidence. Some studies have demonstrated reduced viral particles in the air after use of HEPA filters or improved ventilation in other settings; however, real-world data demonstrating a reduction in viral transmission are lacking [81–83]. Thus, inability to adopt ventilation interventions should not automatically preclude schools from opening.
As the epidemiologic role of fomite-based transmission of SARS-CoV-2 appears to be substantially less important than initially suspected [84], enhanced cleaning and disinfection interventions should be discontinued, in favor of standard cleaning policies. Further, strategies implemented early in the pandemic to reduce environmental spread, such as closing school playgrounds [85], which are an outdoor shared space that is inherently safer than indoor spaces, should be discontinued.
PERSONAL PROTECTIVE EQUIPMENT/HAND HYGIENE
PPE and hand hygiene strategies reduce the risk of infection in the event of exposure to SARS-CoV-2. Within health care and community settings, these strategies are critical for preventing spread. Further, modeling data and data from regions around the world about COVID-19 transmission in school settings suggest that universal masking is an important intervention for preventing in-school spread and keeping schools open (Table 3) [86].
Table 3.
Summary of Evidence of Impact of Masking in School Settings
| Study/Country | Setting | Study Type | Mask Intervention | Simultaneous Interventions | Results | Data Source |
|---|---|---|---|---|---|---|
| Falk et al. [40], USA | 17 K-12 in-person schools, Wisconsin | Cohort, investigated COVID-19 cases and compliance with mask use, Aug 31–Nov 29, 2020 | Masking required for students & staff | Students in cohorts | Reported rate of student mask wearing was >92%. Case rates among students & staff (191 cases among 5530 persons or 3453/100K) were lower than in the county overall (5466/100K). 1 in 20 cases among students linked to in-school transmission. No infections among staff were school acquired. | Wood County COVID-19 dashboard, weekly surveys to calculate school masking compliance |
| Stein-Zaimer et al. [106], Israel | Israel Regional Public High School, grades 7–12 | Outbreak investigation | On May 19–21, 2020, during an extreme heatwave, the Ministry of Health exempted pupils from wearing masks. Windows were closed with 35–38 students per class. | 10 days later, a major outbreak occurred, with student attack rate 13% vs staff 17%. | Israel Ministry of Health | |
| Panovska-Griffiths et al. [107], UK (preprint) | UK secondary schools (ages ≥12 y) | Modeling study, simulated mask effective coverage in schools & community settings, estimated as the product of the mask efficacy (per-contact risk reduction) and coverage (proportion of contacts in which they are worn) | Mandatory masking in secondary schools (re-opened Sept 1). Mandatory masking in community started Jul 24, 2020. | Assuming current test-and-trace isolate levels, adoption of masks in secondary schools in addition to community settings will reduce size of a second wave as compared with no adoption of masks. Greater benefit of mandatory masks in secondary schools if effective coverage of masks is high (30%) under current testing and tracing levels. | UK COVID-19 dashboard, NHS Test and Trace |
Society guidance: Centers for Disease Control and Prevention [108]: masks recommended when students are <6 feet apart and should be considered when students are >6 feet apart. Wearing masks may not be possible for younger students and those with mental/physical health conditions. World Health Organization [109]: masks recommended for children >5 years. Apply a risk-based approach for children 6–11 years. Children ≥12 years should follow WHO guidance for adult mask use. American Academy of Pediatrics [22]: strongly recommends universal use of masks for children ≥2 years.
Abbreviations: COVID-19, coronavirus disease 2019; NHS, National Health Service; WHO, World Health Organization.
The grade of mask necessary outside of hospital settings continues to be an area of debate. The effectiveness of masking for the prevention of SARS-CoV-2 transmission is a complex interplay of many factors and depends on the quality of filtration, the quality of fit, and fidelity (adherence) to the intervention. Consideration of all 3 factors must be taken into account when crafting sustainable and effective PPE policy.
Ideally, teachers and school staff should be provided with high-quality masks, such as medical/surgical masks. Eye protection is an important aspect of the infection control response in health care and community settings, with some estimates suggesting that eye protection is associated with an 80% reduction in the odds of contracting COVID-19 [87]. Another time-series analysis found a rapid and substantial reduction in in-hospital transmission after universal eye protection was added to universal masking [88]. Thus, devices that provide eye protection, such as face shields or goggles/safety glasses, should also be available for wear during in-person instruction. This level of protection is similar to what is provided for effective control in health care settings, including for interactions with COVID-19-positive patients not undergoing aerosol-generating procedures.
The PPE plan should consider practical, evidence-based considerations to optimize real-world effectiveness. Prior work in prevention of influenza demonstrates the importance of sustained compliance when leveraging PPE as an infection control strategy: In community settings, lower rates of self-adherence are associated with higher rates of infection [89]. Thus, to optimize effectiveness of the masking approach, districts should use an implementation science–informed approach to masking to maximize adherence [27]. Considering the critical need to sustain compliance, students should be able to choose from a variety of options including cloth masks, surgical masks, and masks/face shields and may switch throughout the day to promote adherence [90]. Consideration of factors such as fit, comfort, training, and devices to support compliance (such as button headbands) are critical factors for promoting fidelity to the intervention and ultimately achieving and sustaining the benefits of PPE. In the real world, a choice that appears less than perfect in experimental and mannequin settings may be more effective due to improved compliance. To improve adherence at the level of an individual student, systems interventions such as the use of outside spaces for facilitation of safer and more frequent mask breaks may increase mask adherence in indoor classrooms, where the intervention is most critical for controlling spread.
Hand hygiene campaigns are also fundamental to school re-opening infection control plans. Although current CDC guidance suggests that soap and water are preferred to hand sanitizer, cluster randomized controlled trials in school settings suggest that hand sanitizer is at least equivalent to, if not superior to, soap and water, likely because hand sanitizer is faster and easier [91, 92]. Considering this evidence, both hand sanitizer and soap and water should be considered acceptable alternatives, and education on both types of hand hygiene should be provided to students and staff. Sinks should be made available for soap and water use, for situations when hands are visibly soiled and hand sanitizer would not be appropriate.
Hand sanitizing stations should be present throughout the buildings. Frequent sanitizing breaks should be encouraged, and the time required for sanitizing needs to be built into high-risk activities, such as before and after eating.
BEYOND THE 4 PILLARS: POLITICS, IMPLEMENTATION, AND EMERGING SCIENCE
Critical to the success of any school re-opening plan is a consideration of evidence-based implementation strategies and outcomes in order to ensure appropriate adoption of infection prevention interventions. Powell et al. highlight 73 evidence-based implementation strategies [27], many of which can be considered and leveraged to promote best infection control practices in school settings; evidence-based implementation strategies include educational programs, support, and engagement of local leaders and stakeholders, among many others. Recent data suggest that implementation plans that leverage multiple strategies simultaneously are associated with higher rates of a successful implementation [89]. Thus, development of any infection control plan for safe re-opening of schools should be coupled with a comprehensive and multifaceted implementation plan, leveraging as many implementation strategies as is feasible. Implementation strategies may include stakeholder, physician, and community engagement, educational campaigns, fundraising drives, and novel public–private partnerships, among others, to optimize the chances of a safe re-opening.
Implementation Barriers and Challenges
Although science and the basics of infection control can be used to develop safe school re-opening policies, underlying evidence about COVID-19 mitigation is not the only factor driving the current school policy debate. Recently published data suggest that the strongest predictors of decisions about school opening are the political lean of a district and the strength of the local teachers union, with schools in Republican-leaning areas and with weaker unions far more likely to open than in Democratic-leaning areas with stronger unions, regardless of rates of community prevalence or mitigation measures implemented in school settings [93]. A critical implementation barrier that has faced districts nationwide has been a lack of trust, partly driven by the politicization of the debate, between parents advocating to re-open schools and teachers’ unions that may prefer to stay remote until both students and school staff are fully vaccinated against COVID-19. Medical professionals and scientific experts may have a role in bridging that mistrust. Medical and scientific professionals wishing to become involved may do so in many capacities, including advising the district on implementation and adoption of evidence-based infection control policies, volunteering to answer questions/address concerns from teachers/staff members, and providing education on proper use of PPE and other mitigation strategies. By offering up their expertise, involved physicians have the ability to change the conversation from “whether to open schools” to “how to open schools safely.” However, in volunteering, it is critical that medical and scientific experts recognize the limits of their expertise and consider feedback from local stakeholders when assisting in the development of evidence-based plans. The scientific community can provide critical feedback about evidence-based practices, but are not experts on education and must recognize the limits of their own knowledge base when providing infection control advice and support.
Addressing Implementation Barriers and Challenges With Evidence-Informed Strategies
In addition to relying on medical and scientific experts, schools could develop an educational campaign with identification of local thought leaders about the importance of masking and a guide for parents to use with their children who are struggling. Within the school, teachers and nurses should be engaged to encourage ongoing education and interactive campaigns to assist students and school staff in order to maintain effectiveness. In addition, specific interventions designed to promote compliance in high-risk settings, such as break rooms, should also be integrated into school re-opening plans.
The Dynamic Sustainability Framework highlights a perennial challenge in implementation science work: The need for mechanisms to avoid “voltage drop” that may occur over time [26]. Some of the pillars of infection control, such as engineering controls, do not require day-to-day compliance, which is part of what makes them attractive. Vaccination programs are similarly attractive because they provide long-term protection without the need for sustainment on a day-to day-basis. However, others, such as hygiene protocols, PPE, and recommendations to maintain distancing at all times, particularly during break and mealtimes, are at high risk for “voltage drop,” or decreasing rates of compliance—and therefore effectiveness—over time.
Due to this risk, inherent in any safe re-opening plan is a consideration of strategies to maintain sustainability throughout the school year. Ongoing educational initiatives and use of evidence-based implementation strategies on a continual or intermittent basis may be necessary to sustain necessary levels of compliance to provide protection. Creation of eating areas with limited seating, tape to delineate spaces, signage, or other strategies may be necessary to maintain compliance in the highest-risk settings [75]. Community-wide public health messaging from the school district must be ongoing in the town and the community, emphasizing the importance of community-level safe practices, such as continued masking and social distancing both, in order to keep the prevalence low in the town.
In addition to considerations about sustainability, we must also recognize that evidence about SARS-CoV-2 continues to evolve, and infection control strategies for school settings will require updates and adaptations as data continue to emerge. Epidemiologists, public health experts, and physicians may assist district administrators, who may have limited expertise in this area, with this ongoing process.
The Evolving Science About COVID-19 Vaccines and Considerations for School Re-opening Policies
Much of the early school re-opening debate was based on hope of a vaccine. However, although vaccination and herd immunity are an important tool for supporting school re-opening, this strategy has many limitations. In late 2020, the Advisory Committee on Immunization Practices provided recommendations for allocation of vaccine that prioritized those who work in the education sector (teachers and support staff members) to Phase 1B [94].
As of March 2021, 3 vaccines have received Emergency Use Authorization within the United States (2 different 2-dose mRNA vaccines and 1 single-dose, live adenovirus vaccine), with additional vaccine possibilities on the horizon [95–97]. However, manufacturing and distribution continue to be a challenge in many regions.
Vaccine availability has raised questions about when and how to open schools. Several different milestones have been discussed, including vaccination of teachers and vaccination of students, among others. Although teachers are prioritized in many vaccination schemes, children are very low on the priority list [94]. Further confounding the question of how vaccine availability impacts school opening policy decisions, studies on vaccine efficacy in children have been delayed by limited enrollment; thus, it is unclear when children will be vaccinated [98]. Because children will be among the last to be vaccinated, even if school staff are prioritized, concerns about children becoming infected at school, and potentially bringing the virus home, will continue to be present for the foreseeable future. This challenge is particularly acute for children who live with high-risk family members and those who live in multigenerational homes. Beyond questions about who can get vaccinated when, recent reports about the lack of effectiveness of 1 of the vaccines against an emerging strain in South Africa raise concerns that the virus may evade many of the currently developed vaccines, limiting the long-term viability of this “single-intervention” strategy as a tool to facilitate re-opening schools [99]. Thus, even with school staff vaccinated, mitigation measures will continue to be necessary in school settings for the foreseeable future.
CONCLUSIONS
School re-opening presents risks and promise for students, parents, and school staff. Maximizing the chances of successful opening requires leveraging every tool at our disposal and considering the impact of policies on in-school and out-of-school transmission and risk. Data regarding COVID-19 are constantly changing. Thus, school infection control plans must be flexible and adaptable, with the potential for revisions as additional research becomes available. This may mean relaxing some standards or strengthening others as we continue to learn more about this novel pathogen.
All of these risk mitigation strategies require strong support from parents, teachers, local communities, and all levels of the state and federal government. Schools must be recognized as an essential service, and treated as such. Additionally, incidence of COVID-19 is not the only relevant outcome—we must think more broadly about negative impacts that are both seen and unseen. If the critical importance of in-person learning is not recognized, children may be committed to remote learning for the foreseeable future, and although long-term data on the impacts of school closures will not be available immediately, early data suggest that the harms are dire and may take years to reverse.
Acknowledgments
Potential conflicts of interest. Elissa M. Schechter-Perkins: no conflicts. Polly van den Berg: no conflicts. Westyn Branch-Elliman: W.B.E. is the site PI of a Gilead-funded study (funds to institution). All other authors have no conflicts of interest to declare. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Patient consent. Not applicable; not human subjects research.
References
- 1. Lempel H, Epstein JM, Hammond RA. Economic cost and health care workforce effects of school closures in the U.S. PLoS Curr 2009; 1:RRN1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ballotpedia. School responses to the coronavirus (COVID-19) pandemic during the 2020–2021 academic year. Available at: https://ballotpedia.org/School_responses_to_the_coronavirus_(COVID-19)_pandemic_during_the_2020-2021_academic_year. Accessed 14 February 2021.
- 3. Map: coronavirus and school closure. Education Week. 6; March 2020. Available at: https://www.edweek.org/ew/section/multimedia/map-coronavirus-and-school-closures.html. Accessed 23 August 2020. [Google Scholar]
- 4. School districts’ reopening plans: a snapshot. Education Week. 15 July 2020. Available at: https://www.edweek.org/leadership/school-districts-reopening-plans-a-snapshot/2020/07. Accessed 13 February 2021.
- 5.LeanIn.Org and McKinsey. Women in the workplace 2020. 2020. Available at: https://wiw-report.s3.amazonaws.com/Women_in_the_Workplace_2020.pdf. Accessed 13 February 2021.
- 6. Ewing-Nelson C; National Women’s Law Center.. Another 275 000 women left the labor force in January. 2021. Available at: https://nwlc.org/wp-content/uploads/2021/02/January-Jobs-Day-FS.pdf. Accessed 9 February 2021.
- 7. Meckler L, Natanson H. ‘A lost generation’: surge of research reveals students sliding backward, most vulnerable worst affected.Washington Post. 6 December 2020. Available at: https://www.washingtonpost.com/education/students-falling-behind/2020/12/06/88d7157a-3665-11eb-8d38-6aea1adb3839_story.html. Accessed 8 December 2020. [Google Scholar]
- 8.Curriculum Associates. I-Ready: understanding student needs: early results from fall assessments. 2020. Available at: https://www.curriculumassociates.com/-/media/mainsite/files/i-ready/iready-diagnostic-results-understanding-student-needs-paper-2020.pdf. Accessed 9 February 2021.
- 9. Chetty R, Friedman J, Hendren N, et al. The economic impacts of COVID-19: evidence from a new public database built using private sector data. National Bureau of Economic Resesearch Working Paper w27431. Available at: https://www.nber.org/papers/w27431. Accessed 13 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peterson PE. The price students pay when schools are closed. Education Next. 31 July 2020. Available at: https://www.educationnext.org/price-students-pay-when-schools-are-closed/. Accessed 9 February 2021. [Google Scholar]
- 11. Dorn E, Hancock B, Sarakatsannis J, Viruleg E;McKinsey & Company. COVID-19 and learning loss—disparities grow and students need help.2020. Available at: https://www.mckinsey.com/~/media/McKinsey/Industries/Public%20and%20Social%20Sector/Our%20Insights/COVID%2019%20and%20learning%20loss%20disparities%20grow%20and%20students%20need%20help/COVID-19-and-learning-loss-disparities-grow-and-students-need-help-V2.pdf?shouldIndex=false. Accessed 9 February 2021.
- 12.Fairfax County Public Schools, Office of Research and Strategic Improvement. Study of teaching and learning during the COVID-19 pandemic: analyses of Q1 secondary marks. 2020. Available at: https://go.boarddocs.com/vsba/fairfax/Board.nsf/files/BVJV847F7247/$file/Q1%20Marks%20Rpt%20-%20v6%20lzh.pdf. Accessed 9 February 2021.
- 13. Haripersad YV, Kannegiesser-Bailey M, Morton K, et al. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child 2021; 106:e15. [DOI] [PubMed] [Google Scholar]
- 14. Rundle AG, Park Y, Herbstman JB, et al. COVID-19–related school closings and risk of weight gain among children. Obesity 2020; 28:1008–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics 2020; 146:e2020016824. [DOI] [PubMed] [Google Scholar]
- 16. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry 2020; 59:1218–39.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thakur A. Mental health in high school students at the time of COVID-19: a student’s perspective. J Am Acad Child Adolesc Psychiatry 2020; 59:1309–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bahrampour T. Parents grapple with reality that young children won’t be vaccinated soon.Washington Post. 8 February 2021. Available at: https://www.washingtonpost.com/local/social-issues/parents-grapple-with-reality-that-young-children-wont-be-vaccinated-soon/2021/02/08/e5851334-67ee-11eb-8468-21bc48f07fe5_story.html. Accessed 9 February 2021. [Google Scholar]
- 19.World Health Organization. Checklist to support schools re-opening and preparation for COVID-19 resurgences or similar public health crises. Available at: https://www.who.int/publications-detail-redirect/9789240017467. Accessed 5 February 2021.
- 20.Centers for Disease Control and Prevention. Operating schools during COVID-19: CDC’s considerations. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/schools.html. Accessed 5 February 2021.
- 21.Centers for Disease Control and Prevention. Community, work, and school.2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/operation-strategy.html. Accessed 13 February 2021.
- 22.American Academy of Pediatrics. COVID-19 guidance for safe schools. Available at: http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/. Accessed 6 January 2021.
- 23. Honein MA, Christie A, Rose DA, et al. ; CDC COVID-19 response team. summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1860–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ranney M, Kass D, Choo E. Trump rejected the CDC’s first coronavirus reopening America guide. The second is useless. NBC News. 19 March 2020. Available at: https://www.nbcnews.com/think/opinion/trump-rejected-cdc-s-first-coronavirus-reopening-america-guide-second-ncna1209626. Accessed 25 August 2020. [Google Scholar]
- 25.Centers for Disease Control and Prevention. Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings (2007). Available at: https://www.cdc.gov/infectioncontrol/guidelines/isolation/recommendations.html. Accessed 23 August 2020.
- 26. Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci 2013; 8:117–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Powell BJ, Waltz TJ, Chinman MJ, et al. et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci 2015; 10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011; 38:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cauchemez S, Valleron AJ, Boëlle PY, et al. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature 2008; 452:750–4. [DOI] [PubMed] [Google Scholar]
- 30. Castagnoli R, Votto M, Licari A, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr 2020; 174:882–9. [DOI] [PubMed] [Google Scholar]
- 31. Lewis D. Why schools probably aren’t COVID hotspots. Nature 2020; 587:117. [DOI] [PubMed] [Google Scholar]
- 32. Link-Gelles R. Limited secondary transmission of SARS-CoV-2 in child care programs — Rhode Island, June 1–July 31, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1170–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.gov.uk. SARS-CoV-2 infection and transmission in educational settings. Available at: https://www.gov.uk/government/publications/sars-cov-2-infection-and-transmission-in-educational-settings. Accessed 29 August 2020.
- 34. Ismail SA, Saliba V, Lopez Bernal J, et al. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis. 2021; 21:344–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Macartney K, Quinn HE, Pillsbury AJ, et al. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health 2020; 4:P807–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Heavey L, Casey G, Kelly C, et al. No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020. Eurosurveillance 2020; 25:2000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.NYC DOE Health Screening. School based testing report. NYC DOE health screening. Available at: https://testingresults.schools.nyc/. Accessed 9 February 2021.
- 38. Hobbs CV, Martin LM, Kim SS, et al. ; CDC COVID-19 Response Team . Factors associated with positive SARS-CoV-2 test results in outpatient health facilities and emergency departments among children and adolescents aged <18 years–Mississippi, September-November 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1925–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zimmerman KO, Akinboyo IC, Brookhart MA, et al. Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021; 147:e2020048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Falk A, Benda A, Falk P, et al. COVID-19 cases and transmission in 17 k–12 schools — Wood County, Wisconsin, August 31–November 29, 2020. MMWR Morb Mortal Wkly Rep 2021; 70:136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fricchione MJ, Seo JY, Arwady MA. Data-driven reopening of urban public education through Chicago’s tracking of COVID-19 school transmission. J Public Health Manag Pract. 2021; 27:229–32. [DOI] [PubMed] [Google Scholar]
- 42. Jones E, Young A, Clevenger K, et al. Harvard T.H. Chan School of Public Health Healthy Buildings program. Healthy schools: risk reduction strategies for reopening schools.2020. Available at: https://schools.forhealth.org/wp-content/uploads/sites/19/2020/06/Harvard-Healthy-Buildings-Program-Schools-For-Health-Reopening-Covid19-June2020.pdf. Accessed 13 February 2021.
- 43.Rubin D, Matone M, Marshall D, Gerber J, Coffin S, Fisher B. Policy review: evidence and guidance for in-person schooling during the COVID-19 pandemic. 21 October 2020. Available at: https://policylab.chop.edu/reports-and-tools/policy-review-evidence-and-guidance-in-person-schooling-during-covid-19-pandemic. Accessed 6 February 2021.
- 44. Shapiro E, Rubinstein D. Did it hit 3%? Why parents and teachers are fixated on one number.The New York Times. 15 November 2020. Available at: https://www.nytimes.com/2020/11/15/nyregion/coronavirus-nyc-schools-shutdown.html. Accessed 6 February 2021. [Google Scholar]
- 45.DeCosta-Klipa N. Charlie Baker says he could roll back reopening if COVID-19 uptick continues. Boston.com. 4 August 2020. Available at: https://www.boston.com/news/coronavirus/2020/08/04/charlie-baker-coronavirus-uptick-massachusetts. Accessed 6 February 2021.
- 46. Onishi N, Méheut C, Francini A. Positive test rate of 11%? France’s schools remain open. The Chicago Tribune. 1 December 2020. Available at: https://www.chicagotribune.com/coronavirus/sns-nyt-france-covid-schools-20201201-wnqtlc3t3nft3l2d24qzmyvgj4-story.html. Accessed 8 December 2020. [Google Scholar]
- 47. Buonsenso D, De Rose C, Moroni R, Valentini P. SARS-CoV-2 infections in italian schools: preliminary findings after 1 month of school opening during the second wave of the pandemic. Front Pediatr. 2020; 8:615894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Salathé M, Althaus CL, Neher R, et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Med Wkly 2020; 150:w20225. [DOI] [PubMed] [Google Scholar]
- 49. Wellesley Public Schools. COVID-19 pool surveillance testing plan FAQs. 2020. Available at: https://wellesleyps.org/viral-testing/wps-covid-19-pool-surveillance-testing-plan-faqs/. Accessed 10 February 2021.
- 50. Wellesley Education Foundation. Back to school testing program. Available at: https://www.wellesleyeducationfoundation.org/testing-collaborative. Accessed 10 February 2021.
- 51.Massachusetts Department of Elementary and Secondary Education. COVID-19 guidance/on the desktop messages. 2021. Available at: https://www.doe.mass.edu/covid19/on-desktop.html. Accessed 10 March 2021.
- 52. Lee B, Raszka WV. COVID-19 transmission and children: the child is not to blame. Pediatrics. 2020; 146:e2020004879. [DOI] [PubMed] [Google Scholar]
- 53. Levinson M, Cevik M, Lipsitch M. Reopening primary schools during the pandemic. N Engl J Med 2020; 383:981–5. [DOI] [PubMed] [Google Scholar]
- 54. Hill RM, Rufino K, Kurian S, et al. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021; 147:e2020029280. [DOI] [PubMed] [Google Scholar]
- 55. Branch-Elliman W, Safdar N, Nelson R. Economic considerations in infectious diseases emergency response preparedness: it’s all about the point of view. Clin Infect Dis 2021; 72:148–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lazar K, Gans F, Stoico N. Most Mass. students will be required to get the flu vaccine this year.The Boston Globe. 19 August 2020. Available at: https://www.bostonglobe.com/2020/08/19/metro/mass-students-will-be-required-get-flu-vaccine-this-year/. Accessed 29 August 2020. [Google Scholar]
- 57.Mass.gov. Weekly flu report, February 5, 2021. 2021. Available at: https://www.mass.gov/info-details/weekly-flu-report-february-5-2021. Accessed 6 February 2021. [Google Scholar]
- 58. Hu M, Lin H, Wang J, et al. The risk of COVID-19 transmission in train passengers: an epidemiological and modelling study. Clin Infect Dis. 2021; 72:604-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.American Academy of Pediatrics. American Academy of Pediatrics updates guidance on school safety amid pandemic. 2021. Available at: http://services.aap.org/en/news-room/news-releases/aap/2021/american-academy-of-pediatrics-updates-guidance-on-school-safety-amid-pandemic/. Accessed 6 January 2021.
- 60. Johansen TB, Astrup E, Jore S, et al. Infection prevention guidelines and considerations for paediatric risk groups when reopening primary schools during COVID-19 pandemic, Norway, April 2020. Eurosurveillance. 2020; 22:2000921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.European Centre for Disease Prevention and Control. COVID-19 in children and the role of school settings in COVID-19 transmission. Published 6 August 2020. Available at: https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission. Accessed 28 August 2020.
- 62. Melnick H, Darling-Hammon L, Leung M, et al. Reopening schools in the context of COVID-19: health and safety guidelines from other countries. Learning Policy Institute. 15 May 2020. Available at: https://learningpolicyinstitute.org/product/reopening-schools-covid-19-brief. Accessed 13 February 2021. [Google Scholar]
- 63. Ludvigsson JF. The first eight months of Sweden’s COVID-19 strategy and the key actions and actors that were involved. Acta Paediatr 2020; 109:2459–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.RIVM. Children, school and COVID-19. Available at: https://www.rivm.nl/en/novel-coronavirus-covid-19/children-and-covid-19?fbclid=IwAR08cCg84RmbR7oKzgasZG46QX3TWT8VLWarRFk5-sT0xa7_PTLtJ1bVKWI. Accessed 4 November 2020. [Google Scholar]
- 65. van den Berg P, Schechter-Perkins EM, Jack RS, et al. Effectiveness of 3 Versus 6 ft of Physical Distancing for Controlling Spread of Coronavirus Disease 2019 Among Primary and Secondary Students and Staff: A Retrospective, Statewide Cohort Study. Clin Infect Dis. 2021; 73:1871–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.gov.uk. Actions for schools during the coronavirus outbreak. Available at: https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak. Accessed 5 February 2021.
- 67.Meredith R. Coronavirus: NI schoolchildren to follow 1m social distancing. BBC News. 18 June 2020. Available at: https://www.bbc.com/news/uk-northern-ireland-53098017. Accessed 6 February 2021. [Google Scholar]
- 68.Washington State Department of Health. K-12 schools guidance 2020–2021. 2021. Available at: https://www.doh.wa.gov/Portals/1/Documents/1600/coronavirus/FallGuidanceK-12.pdf. Accessed 13 February 2021. [Google Scholar]
- 69. Buckle J. What will return to school look like this fall? A look inside hybrid learning plans. Panorama Education. 27 October 2020. Available at: https://www.panoramaed.com/blog/hybrid-learning-return-to-school. Accessed 6 February 2021. [Google Scholar]
- 70. Superville DR. Hybrid school schedules: more flexibility; big logistical challenges.Education Week. 24 June 2020. Available at: https://www.edweek.org/leadership/hybrid-school-schedules-more-flexibility-big-logistical-challenges/2020/06. Accessed 6 February 2021. [Google Scholar]
- 71.North A. Hybrid school might be the worst of both worlds.Vox. 19 October 2020. Available at: https://www.vox.com/21515864/covid-hybrid-school-learning-remote-plan-pandemic. Accessed 8 December 2020. [Google Scholar]
- 72. Hamner L, Dubbel P, Capron I, et al. High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 2020; 69:606–10. [DOI] [PubMed] [Google Scholar]
- 73. Bahl P, de Silva C, Bhattacharjee S, et al. Droplets and aerosols generated by singing and the risk of coronavirus disease 2019 for choirs. Clin Infect Dis. 2021; 72:e639–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lazar K. Mounting clusters in youth sports, pandemic fatigue complicate fight against coronavirus in Mass.The Boston Globe. 4 November 2020. Available at: https://www.bostonglobe.com/2020/11/04/metro/mounting-clusters-youth-sports-pandemic-fatigue-complicate-fight-against-coronavirus-mass/. Accessed 9 February 2021. [Google Scholar]
- 75. Haessler S. COVID-19 town hall round 17: anatomy of a Covid-19 outbreak. Presented at the: SHEA Webinar; 2 August 2020. [Google Scholar]
- 76. Branch-Elliman W, Araujo-Castillo RV, Snyder GM, et al. Identification of a norovirus outbreak on a hematopoietic stem cell transplant unit and development and implementation of a novel infection prevention algorithm for controlling transmission. Infect Control Hosp Epidemiol 2020; 41:472–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Centers for Disease Control and Prevention. Options to reduce quarantine for contacts of persons with SARS-CoV-2 infection using symptom monitoring and diagnostic testing. 2 December 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-options-to-reduce-quarantine.html. Accessed 17 December 2020.
- 78. Qian H, Miao T, liu L, et al. Indoor transmission of SARS-CoV-2. Indoor Air. 2021; 31:639–45. [DOI] [PubMed] [Google Scholar]
- 79.The MITRE Corporation. Face masks, open windows on buses reduce potentially infectious particles in the air. MITRE News. 9 December 2020. Available at: https://www.mitre.org/news/press-releases/face-masks-open-windows-on-buses-reduce-potentially-infectious-particles. Accessed 10 February 2021.
- 80. Mathai V, Das A, Bailey JA, Breuer K. Airflows inside passenger cars and implications for airborne disease transmission. Sci Adv 2021; 7:eabe0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Centers for Disease Control and Prevention. Ventilation in buildings. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html. Accessed 13 February 2021.
- 82. Mousavi ES, Kananizadeh N, Martinello RA, Sherman JD. COVID-19 outbreak and hospital air quality: a systematic review of evidence on air filtration and recirculation. Environ Sci Technol. 2020; 55:4134–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Christopherson DA, Yao WC, Lu M, et al. High-efficiency particulate air filters in the era of COVID-19: function and efficacy. Otolaryngol Head Neck Surg 2020; 163:1153–5. [DOI] [PubMed] [Google Scholar]
- 84. Meyerowitz EA, Richterman A, Gandhi RT, Sax PE. Transmission of SARS-CoV-2: a review of viral, host, and environmental factors. Ann Intern Med. 2021; 174:69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.National Recreation and Park Association. NRPA statement on playgrounds and play structures during COVID-19 pandemic. Available at: https://www.nrpa.org/about-national-recreation-and-park-association/press-room/nrpa-statement-on-playgrounds-and-play-structures-during-covid-19-pandemic/. Accessed 6 February 2021.
- 86. Head JR, Andrejko K, Cheng Q, et al. The effect of school closures and reopening strategies on COVID-19 infection dynamics in the San Francisco Bay Area: a cross-sectional survey and modeling analysis. medRxiv 2020.08.06.20169797 [Preprint]. 7 August 2020. Available at: https://doi.org/10.1101/2020.08.06.20169797. Accessed 13 February 2021. [Google Scholar]
- 87. Chu DK, Akl EA, Duda S, et al. ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors . Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020; 395:1973–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Hemmige V, Winterer B, Lasco T, Lembcke B. LB-16. Association between universal face shield in a quaternary care center and reduction of SARS-COV2 infections among healthcare personnel and hospitalized patients. Open Forum Infect Dis 2020; 7:XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Rogal SS, Yakovchenko V, Waltz TJ, et al. The association between implementation strategy use and the uptake of hepatitis C treatment in a national sample. Implement Sci 2017; 12:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Prevent Epidemics. Mask guidance playbook. Available at: https://preventepidemics.org/covid19/resources/mask-playbook/. Accessed 29 August 2020.
- 91. Hammond B, Ali Y, Fendler E, et al. Effect of hand sanitizer use on elementary school absenteeism. Am J Infect Control 2000; 28:340–6. [DOI] [PubMed] [Google Scholar]
- 92. Sandora TJ, Shih MC, Goldmann DA. Reducing absenteeism from gastrointestinal and respiratory illness in elementary school students: a randomized, controlled trial of an infection-control intervention. Pediatrics 2008; 121:e1555–62. [DOI] [PubMed] [Google Scholar]
- 93. Hartney MT, Finger LK. Politics, markets, and pandemics: public education’s response to COVID-19. EdWorkingPaper No. 20-301. 2020. Available at: https://www.edworkingpapers.com/sites/default/files/ai20-304.pdf. Accessed 13 February 2021.
- 94. Dooling K. The Advisory Committee on Immunization Practices’ updated interim recommendation for allocation of COVID-19 vaccine — United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.US Food and Drug Administration. FDA takes key action in fight against COVID-19 by issuing Emergency Use Authorization for first COVID-19 vaccine. 11 December 2020. Available at: https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19. Accessed 9 February 2021.
- 96.US Food and Drug Administration. FDA takes additional action in fight against COVID-19 by issuing Emergency Use Authorization for second COVID-19 vaccine. Published 18 December 2020. Available at: https://www.fda.gov/news-events/press-announcements/fda-takes-additional-action-fight-against-covid-19-issuing-emergency-use-authorization-second-covid. Accessed 9 February 2021.
- 97.Johnson & Johnson. Johnson & Johnson announces submission of application to the U.S. FDA for Emergency Use Authorization of its investigational single-shot Janssen COVID-19 vaccine candidate. Available at: https://www.jnj.com/johnson-johnson-announces-submission-of-application-to-the-u-s-fda-for-emergency-use-authorization-of-its-investigational-single-shot-janssen-covid-19-vaccine-candidate. Accessed 9 February 2021.
- 98. Weintraub K. Moderna struggles to find 3000 adolescent volunteers needed for COVID-19 vaccine trial.USA Today. 13 January 2021. Available at: https://www.usatoday.com/story/news/health/2021/01/13/moderna-covid-19-vaccine-trial-adolescent-volunteers-coronavirus/6646795002/. Accessed 10 February 2021. [Google Scholar]
- 99. Cohen J. South Africa suspends use of AstraZeneca’s COVID-19 vaccine after it fails to clearly stop virus variant. Science. 8 February 2021. Available at: https://www.sciencemag.org/news/2021/02/south-africa-suspends-use-astrazenecas-covid-19-vaccine-after-it-fails-clearly-stop. Accessed 10 February 2021.
- 100. Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E. Open schools, COVID-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021; 384:669–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Yung CF, Kam K-Q, Nadua KD, et al. Novel coronavirus 2019 transmission risk in educational settings. Clin Infect Dis. 2021; 72:1055–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Australian Government Department of Health. Australian Health Protection Principal Committee (AHPPC) coronavirus (COVID-19) statement on 17 March 2020.2020. Available at: https://www.health.gov.au/news/australian-health-protection-principal-committee-ahppc-coronavirus-covid-19-statement-on-17-march-2020-0. Accessed 5 February 2021.
- 103. Brandal LT, Ofitserova TS, Meijerink H, et al. Minimal transmission of SARS-CoV-2 from paediatric COVID-19 cases in primary schools, Norway, August to November 2020. Eurosurveillance. 2021; 26:2002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Ismail SA, Saliba V, Bernal JL, et al. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis. 2021; 21:344–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Isphording IE, Lipfert M, Pestel N;Institute of Labor Economics (IZA). School re-openings after summer breaks in Germany did not increase SARS-CoV-2 cases.2020. Available at: http://hdl.handle.net/10419/227317. Accessed 13 February 2021.
- 106. Stein-Zamir C, Abramson N, Shoob H, et al. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Euro Surveill. 2020; 25:2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Panovska-Griffiths J, Kerr CC, Waites W, et al. Modelling the potential impact of mask use in schools and society on COVID -19 control in the UK. medRxiv 2020.09.28.20202937 [Preprint]. 8 October 2020. Available at: https://doi.org/10.1101/2020.09.28.20202937. Accessed 13 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Centers for Disease Control and Prevention. Guidance for wearing masks. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/cloth-face-cover.html. Accessed 5 February 2021.
- 109.World Health Organization. Advice on the use of masks for children in the community in the context of COVID-19. Available at: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-IPC_Masks-Children-2020.1. Accessed 5 February 2021.