Abstract
Coronavirus disease 2019 (COVID-19), a respiratory viral infection, has affected more than 78 million individuals worldwide as of the end of December 2020. Previous studies reported that severe acute respiratory syndrome coronavirus 1 and Middle East respiratory syndrome–related coronavirus infections may affect the gastrointestinal (GI) system. In this review we outline the important GI manifestations of COVID-19 and discuss the possible underlying pathophysiological mechanisms and their diagnosis and management. GI manifestations are reported in 11.4–61.1% of individuals with COVID-19, with variable onset and severity. The majority of COVID-19-associated GI symptoms are mild and self-limiting and include anorexia, diarrhoea, nausea, vomiting and abdominal pain/discomfort. A minority of patients present with an acute abdomen with aetiologies such as acute pancreatitis, acute appendicitis, intestinal obstruction, bowel ischaemia, haemoperitoneum or abdominal compartment syndrome. Severe acute respiratory syndrome coronavirus 2 RNA has been found in biopsies from all parts of the alimentary canal. Involvement of the GI tract may be due to direct viral injury and/or an inflammatory immune response and may lead to malabsorption, an imbalance in intestinal secretions and gut mucosal integrity and activation of the enteric nervous system. Supportive and symptomatic care is the mainstay of therapy. However, a minority may require surgical or endoscopic treatment for acute abdomen and GI bleeding.
Keywords: COVID-19, diarrhoea, gastrointestinal manifestations, inflammatory bowel disease, SARS-CoV-2
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It is currently a pandemic and as of 26 December 2020 there have been >79 million cases worldwide and >1.7 million deaths.1 Several vaccines have been developed to control the pandemic.2 The earliest record of coronavirus infections among animals was in the late 1920s, where acute respiratory infections occurred in domesticated chickens in North America.3 Human coronaviruses were discovered in the 1960s4 and presently seven strains cause disease. Human coronavirus OC43 (HCoV-OC43), human coronavirus HKU1 (HCoV-HKU1), human coronavirus 229E (HCoV-229E) and human coronavirus NL63 (HCoV-NL63) cause mild disease, while the severe acute respiratory syndrome coronavirus (SARS-CoV-1), Middle East respiratory syndrome–related coronavirus (MERS-CoV) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may potentially cause severe disease.5–7 Outbreaks of SARS-CoV-1 and MERS-CoV infections occurred in 2002 and 2012, respectively.8 SARS-CoV-2 has 70% and 40% genetic sequence similarity with SARS-CoV-1 and MERS-CoV.9 Although fever and respiratory symptoms predominate in coronavirus infections, gastrointestinal (GI) manifestations were seen in SARS-CoV-1, MERS-CoV and SARS-CoV-2 patients (Table 1).8,10–22 Herein we outline the important GI manifestations of COVID-19 and discuss the possible mechanisms and aspects relating to their diagnosis and management.
Table 1.
GI involvement in SARS-COV-1, MERS and COVID-19
| Disease | SARS-CoV-1 | MERS | COVID-19 |
|---|---|---|---|
| Start of outbreak | 2002 | 2012 | 2019 |
| Virus | SARS-CoV-1 | MERS-CoV | SARS-CoV-2 |
| Origin | bat → civets10; China, Guangdong Province | bat → camels11; Saudi Arabia | bat → unknown12 ; China, Wuhan Province |
| GI symptoms | Diarrhoea, 16–73%8 | Diarrhoea, 25%8 | Diarrhoea, 32.5%15 |
| Nausea and vomiting, 20–35%13 | Nausea, 14%14 | Nausea, 11.7%15 | |
| Vomiting, 8%14 | Vomiting, 3.9%16 | ||
| Abdominal pain | Abdominal pain | Abdominal pain/discomfort, 4.4%15 | |
| Time of onset of diarrhoea | Onset or during illness17 | Onset or during illness 8 | Onset or during illness15 |
| RNA shedding in stools | Maximum duration 126 d18 | Seen in 14.6% of patients14 | Mean duration 17.2 d18 |
| Maximum duration 126 d18 | |||
| Stool RT-PCR positive rate from the time of diagnosis | 47% week 11997% week 21954% week 319 | 16% week 11914% week 219NA week 319 | 25% week 11937.5 week 219NA week 319 |
| Viral load (log10 copies/mL or CT value) | 6.52 week 1197.95 week 219 | 4.5 week 1194 week 219 | 31.65 CT week 11926.5 CT week 219 |
| 5.33 week 319 | 0 week 319 | NA week 319 | |
| Entry receptor | ACE2 receptor | DPP4 receptor | ACE2 receptor |
| Pathology | Intestines: no obvious pathological changes/non-specific changes; depletion of mucosal lymphoid tissue20 | Intestines: no obvious pathological changes reported | Intestines: mucosal damage in oesophagus with multiple round herpetic erosions and ulcers and numerous infiltrating plasma cells and lymphocytes as well as interstitial oedema in the lamina propria of the stomach, duodenum and rectum21,22 |
CT value: cycle threshold value; DPP4: dipeptidyl peptidase-4; NA: not applicable.
Literature search
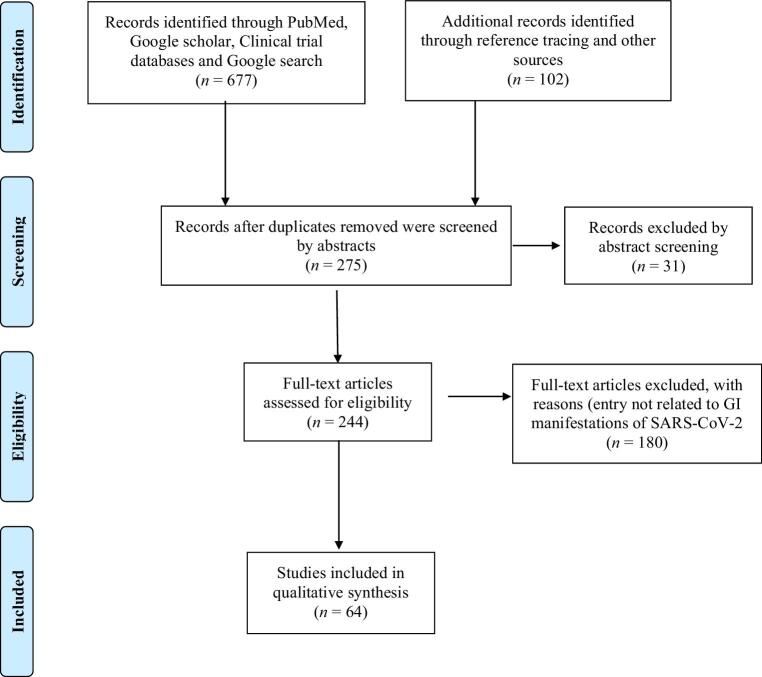
We searched the PubMed, Google Scholar and Clinical Trials databases from 1 January 2020 to 30 December 2020 for articles that describe the GI effects of COVID-19 using the search terms ‘COVID-19 and gastrointestinal tract’, ‘COVID-19 and gastrointestinal symptoms’, ‘COVID-19 and upper gastrointestinal tract’, ‘COVID-19 and lower gastrointestinal tract’, COVID-19 and gastrointestinal inflammation’, ‘SARS-CoV-2 and gastrointestinal tract’, ‘COVID-19 and stool RNA’, ‘gut microbiome and COVID-19’, ‘management of COVD-19’, ‘gastrointestinal tract and coronaviruses’, ‘COVID-19 and GI manifestations’, ‘treatment of COVID-19’ and ‘gastrointestinal side effects and COVID-19’. The article title and abstract were read for the initial selection and then the full-text article was read. Reference lists of the full-text articles were scanned to identify any additional studies. All types of research articles, including original research articles, reviews, case series, short communications and case reports were considered. A total of 244 full-text articles were assessed for eligibility and 87 were included in this review (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart.
Coronaviruses and the gastrointestinal system
There are two genera of human coronaviruses: alpha (HCoV-229E and HCoV-NL63) and beta (HCoV-HKU1, HCoV-OC43, SARS-CoV-1, MERS-CoV and SARS-CoV-2). SARS-CoV-2 and SARS-CoV-1 have high degrees of genomic similarity and use angiotensin-converting enzyme 2 (ACE2) as an entry receptor.9 There is comparatively more literature on the GI effects of SARS-CoV-1 and MERS-CoV than the other coronaviruses. This may be due to differential levels of GI involvement by these coronaviruses.
HCoV-NL63 and HCoV-HKU1
Early studies found coronavirus-like particles in intestinal lesions and the stools of infants with necrotizing enterocolitis.23,24 Esper et al.25 identified HCoV-HKU1 in stool samples from children and adults with GI disease. No stool samples were positive for HCoV-NL63, HCoV-229E or HCoV-OC43. In a study by Vabret et al.26 in France, of six HCoV-HKU1-infected individuals, three were admitted to hospital for acute enteric disease and HCoV-HKU1 was detected in stool samples in two of them. Studies done by Kanwar et al.27 and Kumthip et al.28 found HCoV-HKU1 caused GI symptoms (diarrhoea, vomiting, nausea and abdominal pain) in up to 57% and 38% of infected individuals, respectively. Bouvier et al.29 noted that among otherwise healthy adolescents and adults, HCoV-HKU1-related GI symptoms tend to occur on the fourth day of illness.
SARS-CoV-1
During the SARS-CoV-1 outbreak, 30–70% of patients had GI involvement.17 In a small study, Srikantiah et al.30 found vomiting and diarrhoea in 63% and 75%, respectively, of SARS-CoV-1-infected patients. Hui et al.13 found nausea/vomiting (20–35%) and diarrhoea (20–25%) to be the common GI manifestations. On day 14 of illness, the positivity rates of SARS-CoV-1 in urine, nasopharyngeal aspirate and faeces were 42%, 68% and 97%, respectively. Other studies found diarrhoea in up to 25% of patients.31–33 Chan et al.34 found 5.8% of their patients had fever and diarrhoea (mainly watery without blood or mucus) as the presenting symptom.
MERS-CoV
MERS-CoV patients had high levels of GI involvement.35 Zumla et al.36 reported nausea (21%), vomiting (21–33%) and diarrhoea (26–33%) in MERS-CoV patients. Abdullah et al.37 noted GI manifestations in 35% of patients they studied in eastern Saudi Arabia.
Gastrointestinal manifestations in COVID-19
GI manifestations are reported in 11.4–61.1% of individuals with COVID-19. The majority of COVID-19-associated GI symptoms are mild and self-limiting and include anorexia, diarrhoea, nausea, vomiting and abdominal pain/discomfort (Table 2).15,16,21,22,38–60 In some studies, anorexia and diarrhoea were the most common GI symptoms,61 while in others nausea and vomiting were more prominent.44 Although Han et al.15 found COVID-19-associated GI symptoms to be more common in females (65.7% vs 51.1%), no other studies have found such a pattern.
Table 2.
Clinical characteristics of patients with COVID-19 and GI manifestations
| GI symptoms, n (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First author, year (country) | Article type | Total no of patients | Average age (years) | Patients with GI symptoms, n (%) | Anorexia | Diarrhoea | Nausea or vomiting | Abdominal pain/discomfort | GI/rectal bleeding | Other findings |
| Chen N, 202038 (China) | RA | 99 | 55.5 | 3 (3) | NA | 2 (2) | 1 (1) | NA | NA | NA |
| Chen Y, 202039 (China) | RA | 42 | 52 | 8 (19) | NA | 7 (16.67) | Nausea: 4 (9.52)Vomiting: 3 (7.14) | 5 (11.9) | NA | RNA positive in faeces, 28 (66.67%) |
| Duration of stool viral shedding after negative conversion in pharyngeal swabs was 7 d (range 6–10) | ||||||||||
| Patients who tested SARS-CoV-2 RNA positive exhibited no higher occurrence rate of GI symptoms or severe disease | ||||||||||
| Guan, 202040 (China) | RA | 1099 | 47 | 97 (8.8) | NA | 42 (3.8) | Nausea or vomiting: 55 (5) | NA | NA | NA |
| Han, 202015 (China) | RA | 206 | 62.5 | 117 (56.8) | 102 (49.5) | 67 (32.5) | Vomiting: 24 (11.7) | 9 (4.4) | NA | 19.4% experienced diarrhoea as the first symptom in their illness |
| Concurrent fever was found in 62.4% of patients with a digestive symptom | ||||||||||
| Patients with GI symptoms presented for care later (16 vs 11.6 d; p<0.001) and were more likely to be faecal virus positive (73% vs 14%; p<0.05) | ||||||||||
| Huang, 202041 (China) | RA | 38 | 49 | NA | NA | 1 (3) | NA | NA | NA | NA |
| Jin, 202042 (China) | RA | 651 | 46.14 | 74 (11.4) | NA | 53 (8.1) | Nausea: 10 (1.5) | NA | NA | Occurrence of GI symptoms onset to admission 4 d |
| Vomiting: 11 (1.6) | 10.8% had pre-existing liver disease | |||||||||
| Lin, 202043 (China) | RA | 95 | NA | 58 | 17 (17.9) | 23 (24.2) | Nausea: 17 (17.9) | 2 (2.1) | NA | RNA positive in faeces: 52.4% of patients and it was high among patients with GI symptoms |
| Vomiting: 4 (4.2) | GI symptoms on admission11.6% | |||||||||
| Developed during hospitalisation 49.5% | ||||||||||
| Luo S, 202044 (China) | RA | 1141 | 53.8 | 183 (16) | 180 (98) | 68 (37) | Nausea: 134 (73) | 45 (25) | NA | NA |
| Vomiting: 119 (65) | ||||||||||
| Martin, 202045 (USA) | RA | 41 | 70.4 | 41 | NA | NA | NA | NA | 41 (33.4) | Upper GI bleeding 76%Gastric or duodenal ulcers 12% |
| Lower GI bleeding 24% | ||||||||||
| Rectal ulcers 7% | ||||||||||
| Mauro, 202046 (Italy) | RA | 4871 | 75 | 23 | NA | NA | NA | NA | 23 (0.5) | Occurrence of GI symptoms onset to admission4 d |
| Gastric or duodenal ulcer 44% | ||||||||||
| Erosive or haemorrhagic gastritis 22% | ||||||||||
| Variceal bleeding 6% | ||||||||||
| Mallory–Weiss 11% | ||||||||||
| Dieulafoy's lesion 11% | ||||||||||
| Rebleeding 17% | ||||||||||
| Mo, 202047 (China) | RA | 155 | 54 | NA | 26 (31.7) | 7 (4.5) | Nausea: 3 (3.7)Vomiting: 3 (3.7) | 3 (1.9) | NA | NA |
| Pan, 202016 (China) | RA | 204 | 52.9 | 103 (50.5) | 81 (78.6) | 35 (34) | Vomiting: 4 (3.9) | 2 (1.9) | NA | NA |
| Seeliger, 202021 (France) | RA | 5 | NA | NA | NA | NA | NA | NA | NA | Peritoneal fluid RT-PCR negative in all |
| Shi, 202048 (China) | RA | 81 | 49.5 | NA | 1 (1) | 3 (4) | Vomiting: 4 (5) | NA | NA | NA |
| Wang, 202049 (China) | RA | 138 | 56 | NA | 55 (39.9) | 14 (10.1) | Nausea: 14 (10.1) | 3 (2.2) | NA | NA |
| Vomiting: 5 (3.6) | ||||||||||
| Xu, 202050 (China) | RA | 62 | 41 | NA | NA | 3 (8) | NA | NA | NA | NA |
| Xu, 202051 (China) | RA | 10 | 12 | NA | NA | 3 (30) | NA | NA | NA | Viral RNA in rectal swabs: 80% remained detectable after nasopharyngeal swabs turned negative |
| Young, 202052 (Singapore) | RA | 18 | 47 | NA | NA | 3 (17) | NA | NA | NA | NA |
| Zhang, 202053 (China) | RA | 505 | 51.2 | 164 (32.5) | 93 (56.7) | 62 (37.8) | Nausea: 27 (16.5) | 17 (10.4) | NA | NA |
| Vomiting: 13 (7.9) | ||||||||||
| Zhang, 202054 (China) | RA | 140 | 57 | 55 (39.6) | 17 (12.2) | 18 (12.9) | Nausea: 24 (17.3) | 8 (5.8) | NA | Occurrence of GI symptoms onset to admission 8 d |
| Vomiting: 7 (5.0) | ||||||||||
| Zhou, 202055 (China) | RA | 191 | 56 | NA | NA | 9 (5) | 7 (4) | NA | NA | NA |
| Gadiparthi, 202056 (USA) | BC | 3 | 64 | 3 | NA | 1 (33.33) | NA | NA | 3 (100) | NA |
| Xiao, 202022 (China) | BC | 73 | 43 | NA | NA | 26 (35.6) | NA | NA | NA | NA |
| Case reports | ||||||||||
| Aloysius, 202057 (USA) | CR | 1 | 36 | 1 | NA | Yes | Yes | NA | NA | GI symptoms onset to admission8 d |
| Abdominal signs: epigastric tenderness | ||||||||||
| GI diagnosis: acute pancreatitis complicated with ARDS | ||||||||||
| Coccolini, 202058 (Italy) | CR | 1 | 78 | 1 | NA | NA | NA | Yes | NA | GI diagnosis: intestinal obstruction secondary to small bowel volvulus with no perforation or gut ischaemia |
| RNA positive in peritoneal fluids | ||||||||||
| Holshue, 202059 (USA) | CR | 1 | 35 | 1 | NA | Yes | Yes | Yes | NA | Occurrence of GI symptoms onset to admission 2 d |
| Hosoda, 202060 (Japan) | CR | 1 | 81 | 1 | NA | Yes | NA | Yes | NA | Occurrence of GI symptoms onset to admission 6 d |
| No respiratory symptoms on admission | ||||||||||
| Stool RNA positive until day 15 | ||||||||||
| GI diagnosis: acute enterocolitis without ileus or pneumonia | ||||||||||
BC: brief communication; CR: case report; NA: not available; RA: research article.
Diarrhoea
Diarrhoea has been reported in 2–50% of cases62 and was found to be more common in severe disease (moderate 69.2%, severe 100%).16 Han et al.15 found 20% of their patients experienced diarrhoea as a first symptom, while in the rest it occurred up to 10 d after the onset of respiratory symptoms. A majority of patients are reported to have had non-severe, non-dehydrating, low-volume diarrhoea, lasting on average 5.4 d and showing improvement by day 13 of illness.
Nausea and vomiting
Luo et al.54 found high levels of nausea and vomiting following COVID-19, while the incidence was lower in most other studies. A higher incidence of nausea was associated with more severe disease. Patients presenting with nausea, vomiting and diarrhoea are more likely to have fever than those having one of the symptoms alone.15 Neonates with COVID-19 had vomiting and milk refusal associated with the respiratory symptoms.63
Abdominal pain
Abdominal pain is found at a lower rate than other GI symptoms but was common among patients receiving intensive care unit (ICU) care.49 A minority of patients presenting with abdominal pain had an important abdominal cause such as acute pancreatitis, acute appendicitis, intestinal obstruction, small bowel ischaemia, sigmoid ischaemia, haemoperitoneum, haemopneumoperitoneum or abdominal compartment syndrome. Seelinger et al.21 described seven COVID-19 patients who underwent an emergency surgical procedure due to an acute abdomen.
Anorexia
In a meta-analysis of 60 studies, 26.8% had anorexia as the most common symptom61 and this accounted for difficulties with enteral feeding and maintenance of adequate nutritional status.64 Furthermore, individuals who later developed refractory pneumonia had a higher incidence of anorexia on admission.47
Other GI manifestations
Prominent GI symptoms such as bloody diarrhoea are more common in those with severe disease.40,65 Constipation and haemorrhagic colitis are other less common GI manifestations.65,66 Endoscopic evaluation carried out by Lin et al.43 in a patient presenting with GI bleeding associated with COVID-19 showed multiple round herpetic erosions and ulcers. Similarly, Seeliger et al.21 reported ulcerative and ischaemic changes in rectosigmoidoscopy in patients with severe symptoms.
The time of onset of GI symptoms is variable. In some they are present at the start of the illness (before the other clinical manifestations), while in most they develop later. Of the 61.1% of COVID-19 patients with GI symptoms reported by Lin et al.,43 only 11.6% had symptoms on admission to hospital, while the rest developed them later. Those with predominant GI symptoms had significantly later hospital admissions than those with respiratory symptoms (9 vs 7.3 d16 and 16 vs 11.6 d15). There was an associated delay in diagnosis and treatment.16 The group of patients with predominantly GI symptoms had a significant delay in presenting to hospital and a delay in the diagnosis as well.16 Their clinical course was stormy and there was a higher incidence of progression to severe disease (needing mechanical ventilation and ICU care) compared with their non-GI counterparts.15,16,42,49,53 They also had a longer hospital stay, as their discharge was delayed until viral clearance was achieved. The causes for this observation may be multifactorial. While treatment delay may have played a part, studies have also found higher viral replication and viral loads in patients with GI manifestations.67 Han et al.15 recommended doing routine reverse transcription polymerase chain reaction (RT-PCR) testing in patients presenting with GI symptoms, as they had higher rates of faecal RT-PCR positivity than others. On the other hand, some studies have not found an association between positive PCR results and the incidence of GI symptoms or disease severity.43,67 Variations in GI manifestations and time of onset may be due to several factors, including ethnic/geographical differences, associated comorbidities or the use of different clinical and diagnostic criteria.68 It is important to be aware of the range of GI manifestations in COVID-19 so as to consider this possibility at an early stage. Clinicians should have a high degree of suspicion in patients with fever and GI symptoms, as this may be the only indicator of COVID-19 and may forecast progression to severe disease and the development of complications. Apart from pre-existing liver disease, there were no other predisposing factors documented for the development of GI manifestations, making the prediction of developing such symptoms challenging.42
Mechanisms for GI involvement in COVID-19
SARS-CoV-2 enters host cells through ACE2 receptors.69 High cell entry efficacy is achieved in three ways: high binding affinity of the receptor-binding domain (RBD) of the spike protein, evasion of the host immune system by reduced exposure of the RBD to the outside and Furin protease activation of the virus before entry into host cells, thus reducing its dependence on target cell proteases such as transmembrane protease, serine 2 (TMPRSS2).70 Upon viral binding, the ACE2 receptor and virus are endocytosed, leading to a reduction in cell surface ACE2 levels.
ACE2 receptor expression
The ACE2 receptor is expressed in both hollow and solid intestinal organs. ACE2 messenger RNA (mRNA) is highly expressed in the GI tract and is stabilized by the neutral amino acid transporter B0AT1 (SLC6A19), found in the intestinal epithelium.22 In gut epithelial cells, ACE2 is needed for maintaining amino acid homeostasis, antimicrobial peptide expression and the ecology of the gut microbiome. Thus a reduction of ACE2 may interrupt these processes and increase inflammation.
A study using single-cell transcriptomics found elevated ACE2 expression in the upper oesophagus.71 However, in a different case–control study, decreased expression of ACE2 and nucleocapsid proteins were found in the oesophagus by immunohistochemistry.22 Such discrepant results may be due to patient or assay-related variations and ACE2 mRNA expression patterns may differ from its protein expression due to post-translational modification. Oesophageal bleeding with erosions is noted in some severe COVID-19 patients and may be due to high expression of ACE2 in stratified epithelial cells.43 SARS-CoV-2 is usually not found in the stomach and this may be because of the highly acidic environment. ACE2 expression has been noted in the lamina propria22 and enterocytes72 of the stomach. Thus, although the virus is able to infect cells in the stomach, the low pH may be preventing this. There is high ACE2 expression in proximal and distal enterocytes of the small intestine,68 with the highest expression seen at the brush border of intestinal enterocytes.72 Interestingly, ACE2 and TMPRSS2 are more highly expressed on absorptive enterocytes of the ileum and colon than in the lung.73
Saliva
SARS-CoV-2 RNA is found in saliva and may play an important role in human-to-human viral transmission. Viral loads in saliva decline with persistence of the disease.74 Saliva may be used for viral detection during the acute phase and has some advantages over nasopharyngeal swabs such as ease of sampling, less risk to healthcare workers and lower cost.
Oesophagus, stomach and small and large intestines
SARS-CoV-2 RNA has been found in biopsies from the oesophagus, stomach, duodenum and rectum.43 Involvement of the GI tract during COVID-19 may be due to direct viral injury and/or an inflammatory immune response and may lead to malabsorption, an imbalance in intestinal secretions and activation of the enteric nervous system.73 Entry of SARS-CoV-2 into host cells may trigger an inflammatory response. This leads to recruitment of T-helper cells, a cytokine storm and organ damage. Individuals with diabetes are more susceptible to cytokine storm effects of COVID-19.75 Virus-induced diarrhoea may be due to an alteration of intestinal permeability leading to enterocyte malabsorption.62 Anal swabs have been reported to be persistently RT-PCR positive for SARS-CoV-2, even after throat swabs become negative.50,76 Positivity rates are higher among asymptomatic children, and this would have implications for its transmission potential.
Histological changes in the GI tract and viral particles on ultrastructure
Histology shows occasional lymphocyte infiltration in the oesophagus and partial epithelial degradation, necrosis and mucosal shedding in the stomach. There is dilation and congestion of small blood vessels and oedema of the lamina propria and submucosa of the stomach and small intestine. Immune cell (lymphocytes, monocytes and plasma cells) infiltration is observed in the stomach and intestines.22,77–79 In human small intestinal organoids, enterocytes are readily infected by SARS-CoV-2, as demonstrated by confocal and electron microscopy. The studies demonstrate that intestinal epithelium supports SARS-CoV-2 replication.72
Stool viral RNA in COVID-19
SARS-CoV-2 viral shedding may occur through faeces. Chen et al.67 did not find an association between stool viral RNA positivity and GI symptoms. Of 42 COVID-19 patients, 66.7% had SARS-CoV-2 RNA in their faeces but only 19% had GI symptoms. However, patients presenting with digestive symptoms are more likely to be faecal viral RNA positive than those with respiratory symptoms (73.3% vs 14.3%). Patients with digestive symptoms also take longer to clear the virus from their stools.15 Zhang et al.80 found a higher positivity rate of the virus in faeces compared with respiratory samples (83% vs 67%). The virus was present in the stools for a longer period compared with upper respiratory specimens (22 vs 14 d).61 Chen et al.67 found faecal shedding to occur for 6–10 d after pharyngeal swabs became negative and a similar pattern was seen among children.51 The presence of faecal viral RNA does not correlate with disease severity.67 The longer positivity of viral RNA in the stools of patients with digestive symptoms compared with those with only respiratory symptoms may be due to the high viral load in such patients. It may also be due to direct viral infectivity of the GI tract. Medications such as corticosteroids affect viral clearance. Ling et al.81 found a significant delay in the viral clearance from faeces compared with oropharyngeal swabs (20 vs 11 d) in patients who received corticosteroids.
Viral proliferation in the digestive tract raises the potential of faecal–oral transmission.82 However, the presence of viral RNA in stools does not correlate with transmissibility, as nucleic acid detection does not differentiate infective from non-infective (dead or antibody-neutralized) viruses.83 The detection of faecal viral RNA by RT-PCR testing in COVID-19 patients at different time points may be helpful in management (especially so in patients with GI symptoms). It may help with evaluating the effectiveness of treatment and for determining when quarantine may be ended.
Gut microbiome and COVID-19
The gut microbiome may play an important role in COVID-19.84 As the gut microbiota is known to affect pulmonary health, it may influence the pathogenesis of SARS-CoV-2 infections. Furthermore, respiratory infections are known to cause a change in the composition of the gut microbiota. Increased mortality and morbidity from COVID-19 is associated with the elderly, those with comorbidities such as diabetes and obesity and immunocompromised individuals. These groups of individuals are known to have an impaired gut microbiome structure and function. SARS-CoV-2 infections may further disturb the commensal microbe composition in the gut and lead to gut dysbiosis. The dysbiosis may cause increased cytokine levels, systemic inflammation and exaggerated immune responses.85 Factors released during systemic inflammation, such as C-reactive protein, are related to the severity of COVID-19. Gou et al.86 reported that around 20 blood proteins are associated with COVID-19.
A study done in Hong Kong characterised the gut microbiome alterations in COVID-19. An abundance of Coprobacillus, Clostridium ramosum and Clostridium hathewayi correlated with COVID-19 severity, while the abundance of Faecalibacterium prausnitzii (an anti-inflammatory bacterium) showed an inverse correlation. Bacteroides dorei, Bacteroides thetaiotaomicron, Bacteroides massiliensis and Bacteroides ovatus were associated with low faecal SARS-CoV-2 viral loads.87 Detailed characterisation of the gut microbiome may be useful in predicting disease severity in COVID-19 and large prospective studies are needed to explore this aspect further. The use of probiotics or prebiotics may help re-establish a more normal gut microbiota. Adequate dietary intake of high-quality proteins, vitamin A and branched chain fatty acids may increase the production of antibodies. Consumption of dietary components with known anti-inflammatory and antioxidant properties (omega-3, vitamin C, vitamin E and phytochemicals such as carotenoids and polyphenols) may help blunt an exaggerated inflammatory response and thus prevent dysregulated immune-mediated damage. Low vitamin D levels increase susceptibility to severe disease and death. Adequate fibre intake reduces the relative risk of mortality from infectious and respiratory diseases by 20–40% and is associated with a lower risk of chronic obstructive pulmonary disease.88
Segal et al.89 found the gut microbiota influences GI ACE-2 receptor expression and thus may play a role in influencing COVID-19 infectivity and disease severity. A study done in India found diet plays a crucial role in modulating the gut microbiota. The authors suggested a plant-based, fibre-rich diet may be advantageous during this pandemic, as it helps replenish the host gut microbiota, leading to various health benefits including enhanced immunity.90 Van der Lelie et al.91 have discussed the ‘gut–lung axis,’ where the gut microbiota composition influences lung susceptibility to viral infections and viral infections of the lung alter the gut microbiota composition toward a pro-inflammatory and dysbiotic state. Such dysregulation may influence disease progression and the risk of developing complications. The gut microbiota could influence immune responses and thus affect COVID-19 disease progression. Both overactive and underactive immune responses may lead to clinical complications in COVID-19. Safe and inexpensive prebiotics and probiotics should be considered as adjunctive treatment to limit COVID-19 progression in infected patients or as a preventive strategy in non-infected persons at risk.92
Management of COVID-19-related GI manifestations
Diagnostic aspects
Most GI manifestations in patients with COVID-19 are mild and self-limiting.93 In such patients, no further investigations specific to the GI system are needed. Routine endoscopy is not useful in the diagnosis of mild disease and should be performed cautiously due to the risk of exposure of healthcare workers. Mild cases have a normal endoscopy, but in one study, endoscopic biopsy showed plasma cells and lymphocytes in the lamina propria of the stomach, duodenum and rectum despite having a macroscopically normal GI epithelium.22 Endoscopy is useful in selected patients with GI bleeding for both diagnostic and therapeutic purposes. Lin et al.43 found multiple round herpetic erosions and ulcers in the oesophagus. Martin et al.45 found gastric or duodenal ulcers in 80% of endoscopies for upper GI bleeding and rectal ulcers in 60% of endoscopies when there was lower GI bleeding. Mauro et al.46 described 11 patients who had active peptic ulcers, erosive gastritis and bleeding from gastro-oesophageal varices. A summary of the reported investigation findings and treatments used are provided in Table 3.15,16,21,22,38–60 Although stool RT-PCR, peritoneal biopsies and peritoneal fluid RNA tests have been performed, their usefulness in management is limited. Selected patients with abdominal manifestations such as acute abdomen and peritonitis should have an abdominal computed tomography scan and angiogram. The reported positive findings include small bowel volvulus, acute enterocolitis, splenic flexure contrast extravasation, acute appendicitis, haemoperitoneum and haemopneumoperitoneum. As there are no accepted protocols for investigation of GI manifestations in COVID-19, the decision should be made based on individual circumstances considering the therapeutic benefit of the intervention and the potential risk of exposure to healthcare workers.
Table 3.
Assessment and treatment of patients with COVID-19 and GI manifestations
| First author, year (country) | Article type | Total patients, N | Imaging | Endoscopy | Pathology | General management and nutrition | Drugs specific for GI manifestations | Complications and surgical management | Outcome of GI manifestations and follow-up data |
|---|---|---|---|---|---|---|---|---|---|
| Chen, 202038 (China) | RA | 99 | NA | NA | NA | NA | No | No | NA |
| Chen, 202039 (China) | RA | 42 | NA | NA | NA | NA | NA | No | NA |
| Guan, 202040 (China) | RA | 1099 | NA | NA | NA | NA | NA | No | NA |
| Han, 202015 (China) | RA | 206 | NA | NA | Direct invasion of virus through the intestinal mucosa | NA | NA | No | Recovered/discharged: 100% |
| Huang, 202041 (China) | RA | 41 | NA | NA | NA | NA | NA | No | NA |
| Jin, 202042 (China) | RA | 651 | NA | NA | NA | NA | NA | No | ARDS 6.76% |
| Shock 1.35% | |||||||||
| Liver injury 17.57% | |||||||||
| Mechanical ventilation 6.76% | |||||||||
| ICU care 6.76% | |||||||||
| Death 1.35% | |||||||||
| Lin, 202043 (China) | RA | 96 | NA | In patients with GI bleeding, source of bleeding localised to the oesophagus by endoscopy at a distance of 26 cm from incisors | Multiple round herpetic erosions and ulcers in the oesophagus with a diameter of 4–6 mm | NA | NA | No | In hospital 61.1%Discharged 38.9% |
| Luo, 202044 (China) | RA | 1141 | NA | NA | NA | NA | NA | NA | Recovered 96.2% |
| Death 3.8% | |||||||||
| Martin,202045 (USA) | RA | 41 | UGIB, NG | UGIB, esophagogastroduodenoscopy (32%); treated with epinephrine injection, endoclips or cautery in 40% | UGIB, gastric/duodenal ulcers in 80% of endoscopies | Blood transfusion and monitoring | UGIB, high-dose PPIs | GI bleeding (upper 31, lower 10) requiring blood transfusion | ICU care 46% |
| LGIB, CT angiogram in 1 patient >active extravasation at splenic flexure but angiography was negative | LGIB, flexible sigmoidoscopy or colonoscopy (50%) | LGIB, rectal ulcers in 60% of endoscopies | LGIB, NA | Mechanical ventilation 46% | |||||
| Death 27% | |||||||||
| Mauro,202046 (Italy) | RA | 4871 | Radiological embolization in 1 patient with an early rebleed | UGIE in 11 patients; treated with adrenaline injection and clips in 5, cyanoacrylate gel in 1 | UGIB, active peptic ulcers (44%), erosive or haemorrhagic gastritis (22%), variceal bleeding from gastro-oesophageal varices (4.5%) | Blood transfusion and monitoring | High-dose PPIs | Upper GI bleeding in 23 patients | Discharged 78% |
| Endoscopic re-treatment in 1 patient with an early rebleed | Vasoactive agent for suspicious variceal bleeding in 1 patient | Death 22% | |||||||
| Mo, 202047 (China) | RA | 155 | NA | NA | NA | NA | NA | NA | NA |
| Pan, 202016 (China) | RA | 204 | NA | NA | NA | NA | NA | No | Recovered 81.55% |
| Death 18.45% | |||||||||
| ICU care 5.94% | |||||||||
| Seeliger, 202021 (France) | RA | 7 | CT abdomen, small bowel ischaemia, appendicitis, sigmoid ischaemia, haemoperitoneum, haemopneumoperitoneum and stab wound in liver | Sigmoidoscopy, ulcerative and ischaemic changes | Small bowel ischaemia, appendicitis, sigmoid ischaemia, haemoperitoneum, haemopneumoperitoneum and stab wound in liver | NA | NA | Complications, small bowel ischaemia, sigmoid ischaemia, haemoperitoneum, haemopneumoperitoneum, abdominal compartment syndrome | Recovered/discharged 40% |
| Surgical management, yes, open small bowel resection, laparoscopic appendectomy, open drainage of haemoperitoneum/haemopneumoperitoneum, reduction of incarcerated small bowel | ICU care 60% | ||||||||
| Shi, 202048 (China) | RA | 81 | NA | NA | NA | NA | NA | NA | NA |
| Wang, 202049 (China) | RA | 138 | NA | NA | NA | NA | NA | NA | NA |
| Xu, 202050 (China) | RA | 62 | NA | NA | NA | NA | NA | NA | NA |
| Xu, 202051 (China) | RA | 10 | NA | NA | NA | NA | NA | NA | Recovered/discharged 100% |
| Mechanical ventilation 0 | |||||||||
| ICU care 0 | |||||||||
| Young, 202052 (Singapore) | RA | 18 | NA | NA | NA | NA | NA | NA | Mechanical ventilation 25% |
| ICU care 50% | |||||||||
| Recovered/discharged 100% | |||||||||
| Death 0 | |||||||||
| Zhang, 202053 (China) | RA | 505 | NA | NA | NA | NA | NA | NA | NA |
| Zhang, 202054 (China) | RA | 140 | NA | NA | NA | NA | NA | NA | NA |
| Zhou, 202055 (China) | RA | 191 | NA | NA | NA | NA | NA | NA | NA |
| Gadiparthi, 202056 (USA) | BC | 3 | Patient 1, not done | Not done | Patient 1, possibly from an anastomotic ischaemic ulcer from previous Roux-end-Y gastric bypass | Conservative management with blood transfusion and monitoring | All 3 patients were given high-dose PPIs | Complications, GI bleeding requiring blood transfusion | Recovered/discharged 33.3% |
| Patient 2, CT angiogram did not localize the bleeding vessel | Patient 2, gastroduodenal bleeding | Patient 3 underwent a faecal management system for large volume watery diarrhoea | No surgical management | Death 66.7% | |||||
| Patient 3, not done | Patient 3, rectal ulcer or direct trauma from faecal management system | ||||||||
| Xiao, 202022 (China) | BC | 73 | NA | Mucous epithelium of oesophagus, stomach, duodenum and rectum showed no significant damage | Infiltration of occasional lymphocytes in oesophageal squamous epithelium. In lamina propria of stomach, duodenum and rectum, numerous infiltrating plasma cells and lymphocytes seen with interstitial oedema. Positive staining of GI epithelium for ACE2 and viral RNA | NA | NA | NA | NA |
| Case reports | |||||||||
| Aloysius, 2020 57 (USA) | CR | 1 | CT abdomen, normal gall bladder, normal biliary tract and unremarkable pancreas | NA | ACE2 receptor mediated damage to pancreatic islet cells causing acute pancreatitis | Nothing by mouth, fluid resuscitation (crystalloid) | Analgesia, not specified | No | Recovered/discharged |
| Parenteral nutrition | |||||||||
| Coccolini, 202058 (Italy) | CR | 1 | CT abdomen, intestinal occlusion due to a small bowel volvulus with no signs of gut ischaemia | NA | Volvulus due to omental band attached to RIF (past history of open appendectomy 20 years ago). Bowel vital and viable; no perforation, no bowel ischaemia, no colonic diverticula | NA | NA | Complications, intestinal occlusionSurgical management, yes, adhesiolysis without intestinal resection | Recovered |
| Holshue, 202059 (USA) | CR | 1 | NA | NA | NA | Normal saline | Ondansetron | No | Recovered |
| Hosoda, 202060 (Japan) | CR | 1 | CT abdomen, acute enterocolitis without ileus | NA | NA | NA | NA | No | Recovered |
ARDS: acute respiratory distress syndrome; BC: brief communication; CR: case report; LGIB: lower gastrointestinal endoscopy; NA: not available; RA: research article; UGIE: upper gastrointestinal endoscopy.
Protective measures during endoscopy
Procedures such as upper and lower GI endoscopy should follow the recommended guidelines.94 As positive viral RNA is seen in the oesophagus, stomach, duodenum and rectum, endoscopic procedures warrant extra precautions to ensure the safety of staff and prevent cross-contamination and nosocomial outbreaks among patients. During the COVID-19 pandemic, specific infection control guidelines have been implemented in different countries for endoscopic procedures.94 Endoscopies should be performed only after clinical discussion and should be considered when it is essential for reaching a therapeutic decision that cannot be made using other non-invasive tests.
General measures and universal precautions
Human-to-human transmission of SARS-CoV-2 occurs mainly through the respiratory tract via infected droplets/aerosols. Contact with contaminated surfaces is another possible mode of transmission. Thus wearing proper face masks, hand hygiene and social distancing are fundamental for infection prevention. Healthcare workers should wear appropriate personal protective equipment. Since the virus is found in stools for varying lengths of time, extra precautions may be needed to avoid faecal–oral transmission. Contact with infected saliva or stools should be avoided. Appropriate infection prevention and control measures should be in place for preventing nosocomial spread. There are case reports of the detection of virus in peritoneal fluid during laparotomy. Therefore adherence to special precautionary infection control measures for preventing aerosolization of the virus during laparoscopic procedures or when using electrocautery in open procedures should be considered.58
Supportive measures
As most virus-induced GI manifestations are mild and self-limiting, supportive care and symptomatic treatment are usually sufficient.95–98 Supportive treatment with oxygen, optimal hydration, analgesics and anti-emetics may be necessary.99 Although studies are limited, endoscopy in selected patients has shown ulceration and bleeding. Avoidance of non-steroidal anti-inflammatory drugs (NSAIDs) and gastric acid prophylaxis should be considered in patients with GI manifestations. Those with paralytic ileus or excessive vomiting may require nasogastric tube decompression and nothing by mouth. Patients with diarrhoea need appropriate rehydration therapy and anti-diarrheal medications. Those with GI manifestations have increased rates of electrolyte disturbance42 and thus regular monitoring and correction of electrolytes is needed and medications that may induce electrolyte imbalance should be administered with caution. Those with severe GI manifestations or acute abdomen should be managed by a specialised multidisciplinary team including a physician, critical care specialist, nutritionist, gastroenterologist and surgeon.
Medications
To date, no specific antiviral medications have been shown to reduce mortality in COVID-19 patients. The antiviral drugs used for treatment of COVID-19 include remdesivir and lopinavir–ritonavir. Remdesivir was shown to reduce hospital stays in patients with severe disease. A myriad of other treatment modalities aimed at symptom control and management of complications have been used. Immunomodulatory agents including glucocorticoids, convalescent plasma and anti-cytokine therapy have been used to reduce the negative effects of the overwhelming systemic inflammatory response.99 However, except for dexamethasone, the other agents have not shown definite therapeutic benefits, although they may be beneficial in selected subgroups.100 Moreover, evidence on the efficacy of these agents in treating GI manifestations is limited and further studies are required. There is an ongoing debate about the use of ACE inhibitors and renin–angiotensin–aldosterone system blockers in the treatment of COVID-19. Although beneficial mechanisms such as blocking viral entry into the host cell have been proposed, the clinical significance of these agents is yet to be conclusively proven.101
The loss of gut mucosal integrity and dysfunction of intestinal flora are important complications in severe viral illnesses, including COVID-19. The use of probiotics has been suggested to improve GI symptoms of SARS-CoV-2 infection.101 Irrational use of broad-spectrum antibiotics should be avoided, as they cause the loss of commensal intestinal flora and alteration of gut mucosal integrity. COVID-19 treatment guidelines in China have included the use of probiotics and micro-ecological regulators for maintaining gut mucosal integrity and to minimise secondary bacterial infections.102
Nutrition
SARS-CoV-2 patients may have a reduced oral intake due to the severity of their disease or as a side effect of the medicines that are used. Enteral nutrition is important for maintaining gut mucosal integrity, especially in patients with severe disease. In patients with severe disease, specialist nutritional assessment should be done and a high-calorie, immunomodulatory diet should be administered. In patients who are mechanically ventilated, nasogastric or nasojejunal tube insertion and enteral feeding is an option. In patients who cannot tolerate enteral feeding, parenteral nutrition should be administered. However, enteral feeding should be commenced early following improvement of the clinical condition.
Surgical measures
Rarely, patients with COVID-19 may present with an acute abdomen either due to a complication of the disease or due to a coexisting pathology. Conditions such as acute pancreatitis and abdominal compartment syndrome have been reported in association with COVID-19.57,103 Thus such conditions should be suspected in a deteriorating SARS-CoV-2 patient with an acute abdomen. As thrombotic complications are well-described in SARS-CoV-2 patients, mesenteric thrombosis should be suspected early in a clinically deteriorating patient with acute abdomen and appropriate anticoagulation should be initiated promptly after confirming the diagnosis through imaging.104 In patients with GI bleeding that does not settle with medical management, therapeutic endoscopy with clipping or cautery has been found to be successful.
Surgical treatment has been reported for conditions such as intestinal obstruction, bowel ischaemia, acute appendicitis and haemoperitoneum/haemopneumoperitoneum in association with SARS-CoV-2 (Table 3). Such cases are extremely rare and require a high degree of clinical suspicion and relevant imaging to reach the diagnosis. Standard surgical procedures have been performed with appropriate personal protective equipment and infection control measures to prevent transmission of infection.105,106 Furthermore, in such critically ill patients, postoperative care in an ICU is necessary.107
GI side effects of medications used for COVID-19
A number of medications used in patients with COVID-19 have documented GI side effects (Table 4).108–130
Table 4.
GI side effects of medications used for COVID-19
| Type | Drug | Dosage | Administration | GI side effects | References |
|---|---|---|---|---|---|
| Antivirals | Remdesivir (in phase 3 clinical trials) | Not needing invasive mechanical ventilation/ECMO: 5 d | Intravenous | 1–10%: nausea, liver enzyme derangement, hyperbilirubinaemia | 108–111 |
| Needs mechanical ventilation or ECMO: 10 d | Frequency not known: vomiting, gastroparesis, rectal bleeding | ||||
| Loading dose 200 mg over 30–120 min on day 1 followed by 100 mg once daily for remaining 4–9 d | |||||
| Lopinavir/ritonavir (Kaletra) | 400/100 mg twice daily or 800/200 mg once daily for 14 d | Oral (administer with or without food) | 1–10%: abnormal appetite, diarrhoea, nausea, vomiting, dry mouth, GI discomfort, GI disorders, hepatic disorders, pancreatitis | 112,113 | |
| 0.1–1%: cholangitis, constipation, hyperbilirubinaemia | |||||
| Ribavirin (in phase 2 clinical trials) | 400 mg twice daily for 14 d (in clinical trials), dosing not defined | Oral (administer with food) | 1–10%: decreased appetite, constipation, diarrhoea, nausea, vomiting, dry mouth, GI discomfort, GI disorders, throat pain | 114 | |
| 0.1–1%: hepatic disorders | |||||
| <0.1%: cholangitis, hepatic failure, pancreatitis; frequency not known: tongue discolouration, ulcerative colitis | |||||
| Favipiravir | 1800 mg twice daily on day 1 followed by 800 mg twice daily on day 2 to maximum of 14 d | Oral | 1–10%: hyperuricaemia (5%), diarrhoea (5%), liver enzyme derangement (2%) | 115,116 | |
| Oseltamivir | 75 mg twice daily for 5 d | Oral | 1–>10%: nausea, vomiting, GI discomfort | 117 | |
| <0.1%: GI haemorrhage (children), hepatic disorders | |||||
| Arbidol | For prevention, 200 mg once a day | Oral | Diarrhoea, nausea, vomiting, deranged liver enzymes | 118 | |
| Therapeutic dose 600 mg/d (200 mg three times/d) for 5 d | |||||
| Immunomodulatory | Interferon-α/β | Interferon-1β 0.25 mg alternated for 3 d (in clinical trials), dosing not established | Subcutaneous injection | 1–>10%: low appetite, diarrhoea, nausea, vomiting | 108 |
| 0.1–1%: hepatic disorders, autoimmune hepatitis | |||||
| <0.1%: haemolytic uraemic syndrome, pancreatitis | |||||
| Frequency not known: abdominal pain, constipation | |||||
| Tocilizumab | 4–8 mg/kg (maximum 800 mg) over 1 h or 400 mg once | Intravenous infusion | 1–>10%: abdominal pain, GI disorders, oral disorders | 108 | |
| Consider additional dose 8–12 h later if continued clinical decompensation (maximum of 2 doses) | Frequency not known: hepatic disorders | ||||
| Sarilumab (Kevzara) IL-6 inhibitor | 400 mg | Intravenous | 1–10%: liver enzyme derangement | 119 | |
| Baricitinib (completed clinical trial) | 4 mg once daily baricitinib+antiviral therapy administration for 2 weeks | Oral | 1–>10%: nausea | 120,121 | |
| Frequency not known: abnormal liver enzymes | |||||
| Antiparasitic | Nitazoxanide | 500 mg twice daily (duration not specified) | Oral (administer with or without food) | 1–10%: abdominal pain (8%), diarrhoea (2%), nausea (3%), vomiting (1%) | 108 |
| <1%: increased ALT, anorexia, increased appetite, flatulence, salivary gland enlargement | |||||
| Chloroquine | 500 g twice daily for 10 d | Oral (administer with food) | <0.1%: hepatitis | 109 | |
| Frequency not known: abdominal pain, GI disorders, nausea, diarrhoea, vomiting, metallic taste | |||||
| Hydroxychloroquine | Loading dose of 400 mg twice daily for 1 d, followed by 200 mg twice daily for 4 d | Oral (administer with food) | 1–>10%: low appetite, diarrhoea, nausea, vomiting, abdominal pain | 108 | |
| Frequency not known: acute hepatic failure | |||||
| Steroids | Dexamethasone | 6 mg daily for 7–10 d | Intravenous | 1–>10%: GI discomfort, peptic ulcer, nausea | 122–124 |
| 0.1–1%: increased appetite, pancreatitis | |||||
| Methylprednisolone | 0.5–1 mg/kg/day in two divided doses | Intravenous | 1–>10%: GI discomfort, peptic ulcer, nausea | 125–127 | |
| 0.1–1%: increased appetite, pancreatitis | |||||
| Frequency not known: diarrhoea, vomiting | |||||
| Budesonide | Levamisole 50–100 mg every 8 h | Oral and inhaled | 1–>10%: GI discomfort, peptic ulcer, nausea | 128 | |
| Budesonide+formoterol inhaled 1–2 puffs every 12 h | 0.1–1%: increased appetite, pancreatitis | ||||
| Immunoglobulins | IVIG with moxifloxacin | 20–25 g/d (0.1–0.5 g/kg/day) for 5–15 d with moxifloxacin | Intravenous | 1–>10%: low appetite, constipation (in adults), diarrhoea, GI discomfort (in adults), nausea, vomiting | 129,130 |
| 0.1–1%: antibiotic-associated colitis (in adults), low appetite (in children), GI discomfort (in children), hepatic disorder, gastritis | |||||
| <0.1%: antibiotic-associated colitis (in children), pancreatitis, abdominal pain |
ALT: alanine transaminase; ECMO: extracorporeal membrane oxygenation.
Antivirals
Antivirals and antibiotics may cause diarrhoea and alter the gut microbiome.131 Remdesivir has a number of GI side effects, including nausea, vomiting, gastroparesis and constipation.132,133 The antimalarial agents chloroquine/hydroxychloroquine and lopinavir/ritonavir cause nausea, vomiting, loss of appetite and abdominal cramps.108,113
Immunomodulatory agents
Immunomodulatory agents such as corticosteroids can increase the risk of peptic ulceration and GI bleeding.134 The Janus kinase inhibitor baricitinib can cause diarrhoea.108 Immunomodulators such as tocilizumab may cause GI bleeding, nausea, vomiting and ulceration. The GI side effects of intravenous immunoglobulins are minimal (Table 4).
Proton pump inhibitors (PPIs) and COVID-19
The use of PPIs are a risk factor for rotavirus, influenza virus, norovirus and MERS viral infections.135 Individuals using PPIs once or twice daily had significantly higher odds of a positive COVID-19 test compared with those not taking it.136 A larger study done by Lee et al.137 in 14 163 current and 6242 past PPI users with COVID-19 found SARS-CoV-2 test positivity was not associated with current or past use of PPIs. However, current use of PPIs conferred a 79% higher risk of severe clinical outcomes following SARS-CoV-2 infection. In contrast, Taştemur and Ataseven138 hypothesised that PPI may be used for treatment and prophylaxis of COVID-19, owing to their anti-inflammatory, antioxidant, immunomodulatory and antifibrotic properties.
COVID-19 in patients with diagnosed GI disorders
The presence of comorbidities (including pre-existing digestive disorders) is associated with poor clinical outcome in COVID-19.
Inflammatory bowel disease (IBD)
Chronic inflammatory conditions such as IBD have a theoretical risk of making an individual more susceptible to COVID-19 or to a more severe course of illness. Thus far there has not been definite evidence for either scenario. Of the patients who contracted COVID-19, the most prominent clinical manifestations were fever and cough, similar to the general population. Diarrhoea was noted in about 20% of patients, making the clinical distinction between disease flare and COVID-19 essential for further management.139 In those who do not have COVID-19, continuation of biologic therapy for IBD is recommended. However, in those with COVID-19, the severity of the IBD needs to be considered and treatment balanced with the severity of COVID-19.140
Bezzio et al.141 found that active IBD leads to a negative outcome requiring longer hospitalization and assisted ventilation. Treatment did not change this, emphasizing the importance of prevention of acute flares by adherence to therapy. IBD patients >70 y of age or with other associated comorbidities were at highest risk of complications.142 IBD patients who are pregnant may have a high risk of COVID-19. A woman in the first trimester with an acute severe ulcerative colitis and COVID-19 suffered an abortion, but the exact reason for this was not clear. Optimal management of IBD in pregnancy during the COVID-19 pandemic is yet to be defined. No or limited use of steroids and the use cyclosporine and infliximab as salvage therapy on a case-by-case basis has been suggested.143 Symptomatic anal fistula in Crohn's disease requires proper and timely treatment. Although exploration under anaesthesia is the gold standard for diagnosis, during the COVID-19 pandemic outpatient exploration may be a more suitable option. This would minimize the number of medical personnel required and avoid higher-risk anaesthetic procedures.144
GI malignancies
The pandemic has affected multiple steps in the diagnosis and management of GI malignancies.145,146 Interruption of endoscopic services due to the increased risk of disease transmission and added cost of infection prevention measures (especially in developing countries) has caused considerable delays in the diagnosis of GI malignancies.147 Elective cancer therapies and surgeries have been delayed to allow increased capacity for dealing with COVID-19 patients.148,149 Such delays may adversely impact optimal care for cancer patients and worsen long-term outcomes. A delay in surgical resection in colorectal cancer worsens the survival rate and studies have found disease progression in patients with pancreatic malignancies.150 Patients with GI cancers needing frequent hospital visits may be at higher risk of hospital-acquired COVID-19 transmission. Yu et al.151 studied 1524 cancer patients and found them to have a twofold increased risk of COVID-19 infection when compared with the general population.
Other GI disorders
The outcomes of patients with pancreatitis, celiac disease or irritable bowel syndrome who get COVID-19 have been poorly studied.64
Limitations
Limitations of this review include the small number of studies reporting on certain GI manifestations, making it difficult to provide more definitive conclusions on such aspects. It is possible that subtle GI findings were not documented (and thus underestimated) during the early part of the pandemic. Well-conducted studies from different regions of the world will help expand the evidence base and provide better answers to the many questions at hand. Ours is a broad overview of the main reported GI manifestations in COVID-19 and their management. A more comprehensive and detailed profile of specific aspects should emerge as more data are published from different countries.
Future recommendations
During the present pandemic, testing for SARS-CoV-2 should be considered in patients with GI symptoms, irrespective of them not having the other typical symptoms of COVID-19. The long-term effects of the different GI manifestations should become better defined as more studies using GI imaging and histological findings become available. Detailed and systematically conducted histopathology and autopsy studies should shed light on aspects of pathogenesis and pathology that are still undefined.
Conclusions
GI manifestations are an important feature in some COVID-19 patients. The findings reported so far provide us with new and important insights for understanding the GI effects of SARS-CoV-2 and their underlying pathogenesis. Further studies should help with better delineation of the many uncertain aspects of COVID-19 and the GI tract. In this review we outlined the important GI manifestations of COVID-19 and discussed the possible mechanisms and aspects relating to their diagnosis and management.
Acknowledgements
None.
Contributor Information
Jayani C Kariyawasam, Institute of Biochemistry, Molecular Biology and Biotechnology, University of Colombo, Colombo, Sri Lanka.
Umesh Jayarajah, Postgraduate Institute of Medicine, University of Colombo, Colombo, Sri Lanka.
Rishdha Riza, Colombo South Teaching Hospital, Colombo, Sri Lanka.
Visula Abeysuriya, Nawaloka Hospital Research and Education Foundation, Nawaloka Hospitals, Colombo, Sri Lanka.
Suranjith L Seneviratne, Nawaloka Hospital Research and Education Foundation, Nawaloka Hospitals, Colombo, Sri Lanka.
Authors’ contributions
JCK and SLS designed the study. The search was conducted by JCK, RR, VA and UJ. JCK, UJ, RR and VA wrote the first version of the manuscript and SLS performed the final editing. All the authors reviewed and approved the final version. All authors had full access to the data in the study and final responsibility for the decision to submit for publication.
Funding
None.
Competing interests
None declared.
Ethical approval
Not required.
Data availability
The data underlying this article are available in the article.
References
- 1. Word Health Organization . Coronavirus disease (COVID-2019) situation reports. Geneva: World Health Organization; 2020. [Google Scholar]
- 2. Seneviratne S, Jayarajah U, Abeysuriya V et al. COVID-19 vaccine landscape. J Ceylon Coll Physicians. 2020;51(2):120–31. [Google Scholar]
- 3. Estola T. Coronaviruses, a new group of animal RNA viruses. Avian Dis. 1970;14(2):330–6. [PubMed] [Google Scholar]
- 4. Kahn JS, McIntosh K. History and recent advances in coronavirus discovery. Pediatr Infect Dis J. 2005;24(11 Suppl):S223–7, discussion S6. [DOI] [PubMed] [Google Scholar]
- 5. Corman VM, Muth D, Niemeyer D et al. Hosts and sources of endemic human coronaviruses. Adv Virus Res. 2018;100:163–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Forgie S, Marrie TJ, eds. Healthcare-associated atypical pneumonia. Semin Respir Crit Care Med; 2009;30(1):67–85. [DOI] [PubMed] [Google Scholar]
- 8. Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5(4):335–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chu H, Fuk-Woo Chan J, Wang Y et al. SARS-CoV-2 induces a more robust innate immune response and replicates less efficiently than SARS-CoV in the human intestines: an ex vivo study with implications on pathogenesis of COVID-19. Cell Mol Gastroenterol Hepatol. 2021;11(3):771–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wenzel RP, Edmond MB. Managing SARS amidst uncertainty. N Engl J Med. 2003;348(20):1947–8. [DOI] [PubMed] [Google Scholar]
- 11. Fact sheet on Middle East respiratory syndrome coronavirus (June 2015). Wkly Epidemiol Rec. 2015;90(24):305–8. [PubMed] [Google Scholar]
- 12. Word Health Organization . Origin of SARS-CoV-2, 26 March 2020. WHO/2019-nCoV/FAQ/Virus_origin/2020.1. Geneva: World Health Organization; 2020. Available from: https://apps.who.int/iris/handle/10665/332197 [accessed 2 March 2021]. [Google Scholar]
- 13. Hui DS, Wong PC, Wang C. SARS: clinical features and diagnosis. Respirology. 2003;8(Suppl 1):S20–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim MN, Kim EC. Considering revision the criteria for patients under investigations for MERS-CoV infections: diarrhea or not. J Korean Med Sci. 2018;33(53):e344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Han C, Duan C, Zhang S et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115(6):916–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pan L, Mu M, Yang P et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leung WK, To KF, Chan PK et al. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125(4):1011–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cevik M, Tate M, Lloyd O et al. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe. 2021;2(1):e13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yan Y, Chang L, Wang L. Laboratory testing of SARS-CoV, MERS-CoV, and SARS-CoV-2 (2019-nCoV): current status, challenges, and countermeasures. Rev Med Virol. 2020;30(3):e2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gu J, Korteweg C. Pathology and pathogenesis of severe acute respiratory syndrome. Am J Pathol. 2007;170(4):1136–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Seeliger B, Philouze G, Benotmane I et al. Is the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) present intraperitoneally in patients with coronavirus disease 2019 (COVID-19) infection undergoing emergency operations? Surgery. 2020;168(2):220–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Xiao F, Tang M, Zheng X et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831–3.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rousset S, Moscovici O, Lebon P et al. Intestinal lesions containing coronavirus-like particles in neonatal necrotizing enterocolitis: an ultrastructural analysis. Pediatrics. 1984;73(2):218–24. [PubMed] [Google Scholar]
- 24. Resta S, Luby JP, Rosenfeld CR et al. Isolation and propagation of a human enteric coronavirus. Science. 1985;229(4717):978–81. [DOI] [PubMed] [Google Scholar]
- 25. Esper F, Ou Z, Huang YT. Human coronaviruses are uncommon in patients with gastrointestinal illness. J Clin Virol. 2010;48(2):131–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vabret A, Dina J, Gouarin S et al. Detection of the new human coronavirus HKU1: a report of 6 cases. Clin Infect Dis. 2006;42(5):634–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kanwar A, Selvaraju S, Esper F. Human coronavirus-HKU1 infection among adults in Cleveland, Ohio. Open Forum Infect Dis. 2017;4(2):ofx052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kumthip K, Khamrin P, Ushijima H et al. Enteric and non-enteric adenoviruses associated with acute gastroenteritis in pediatric patients in Thailand, 2011 to 2017. PLoS One. 2019;14(8):e0220263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bouvier M, Chen WJ, Arnold JC et al. Species-specific clinical characteristics of human coronavirus infection among otherwise healthy adolescents and adults. Influenza Other Respir Viruses. 2018;12(2):299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Srikantiah P, Charles MD, Reagan S et al. SARS clinical features, United States, 2003. Emerg Infect Dis. 2005;11(1):135–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Booth CM, Matukas LM, Tomlinson GA et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289(21):2801–9. [DOI] [PubMed] [Google Scholar]
- 32. Hsu L-Y, Lee C-C, Green JA et al. Severe acute respiratory syndrome (SARS) in Singapore: clinical features of index patient and initial contacts. Emerg Infect Dis. 2003;9(6):713–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Poutanen SM, Low DE, Henry B et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. 2003;348(20):1995–2005. [DOI] [PubMed] [Google Scholar]
- 34. Chan PK, Tang JW, Hui DS. SARS: clinical presentation, transmission, pathogenesis and treatment options. Clin Sci. 2006;110(2):193–204. [DOI] [PubMed] [Google Scholar]
- 35. Zhou J, Li C, Zhao G et al. Human intestinal tract serves as an alternative infection route for Middle East respiratory syndrome coronavirus. Sci Adv. 2017;3(11):eaao4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zumla AI, Memish ZA. Middle East respiratory syndrome coronavirus: epidemic potential or a storm in a teacup? Eur Respir J. 2014;43(5):1243–8. [DOI] [PubMed] [Google Scholar]
- 37. Assiri A, McGeer A, Perl TM et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369(5):407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chen N, Zhou M, Dong X et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Chen Y, Chen L, Deng Q et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92(7):833–40. [DOI] [PubMed] [Google Scholar]
- 40. Guan WJ, Ni ZY, Hu Y et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jin X, Lian JS, Hu JH et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lin L, Jiang X, Zhang Z et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69(6):997–1001. [DOI] [PubMed] [Google Scholar]
- 44. Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol. 2020;18(7):1636–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Martin TA, Wan DW, Hajifathalian K et al. Gastrointestinal bleeding in patients with coronavirus disease 2019: a matched case–control study. Am J Gastroenterol. 2020;115(10):1609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mauro A, De Grazia F, Lenti MV et al. Upper gastrointestinal bleeding in COVID-19 inpatients: incidence and management in a multicenter experience from northern Italy. Clin Res Hepatol Gastroenterol. 2020; doi: 10.1016/j.clinre.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mo P, Xing Y, Xiao Y et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020; doi: 10.1093/cid/ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Shi H, Han X, Jiang N et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang D, Hu B, Hu C et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Xu XW, Wu XX, Jiang XG et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Xu Y, Li X, Zhu B et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26(4):502–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Young BE, Ong SWX, Kalimuddin S et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zhang H, Liao YS, Gong J et al. Clinical characteristics of coronavirus disease (COVID-19) patients with gastrointestinal symptoms: a report of 164 cases. Dig Liver Dis. 2020;52(10):1076–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zhang JJ, Dong X, Cao YY et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730–41. [DOI] [PubMed] [Google Scholar]
- 55. Zhou F, Yu T, Du R et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Gadiparthi C, Perisetti A, Sayana H et al. Gastrointestinal bleeding in patients with severe SARS-CoV-2. Am J Gastroenterol. 2020;115(8):1283–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Aloysius MM, Thatti A, Gupta A et al. COVID-19 presenting as acute pancreatitis. Pancreatology. 2020;20(5):1026–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Coccolini F, Tartaglia D, Puglisi A et al. SARS-CoV-2 is present in peritoneal fluid in COVID-19 patients. Ann Surg. 2020;272(3):e240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Holshue ML, DeBolt C, Lindquist S et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hosoda T, Sakamoto M, Shimizu H et al. SARS-CoV-2 enterocolitis with persisting to excrete the virus for approximately two weeks after recovering from diarrhea: a case report. Infect Control Hosp Epidemiol. 2020;41(6):753–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Cheung KS, Hung IFN, Chan PPY et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;159(1):81–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. D'Amico F, Baumgart DC, Danese S et al. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention, and management. Clin Gastroenterol Hepatol. 2020;18(8):1663–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wang J, Wang D, Chen GC et al. [SARS-CoV-2 infection with gastrointestinal symptoms as the first manifestation in a neonate]. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22(3):211–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Aguila EJT, Cua IHY, Fontanilla JAC et al. Gastrointestinal manifestations of COVID-19: impact on nutrition practices. Nutr Clin Pract. 2020;35(5):800–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Carvalho A, Alqusairi R, Adams A et al. SARS-CoV-2 gastrointestinal infection causing hemorrhagic colitis: implications for detection and transmission of COVID-19 disease. Am J Gastroenterol. 2020;115(6):942–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wang Z, Chen X, Lu Y et al. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends. 2020;14(1):64–8. [DOI] [PubMed] [Google Scholar]
- 67. Chen Y, Chen L, Deng Q et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92(7):833–40. [DOI] [PubMed] [Google Scholar]
- 68. Liang W, Feng Z, Rao S et al. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. Gut. 2020;69(6):1141–3. [DOI] [PubMed] [Google Scholar]
- 69. Hoffmann M, Kleine-Weber H, Schroeder S et al. SARS-CoV-2 Cell entry depends on aCE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–80.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shang J, Wan Y, Luo C et al. Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci USA. 2020;117(21):11727–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Zhang H, Kang Z, Gong H et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. BioRxiv. 2020; 10.1101/2020.01.30.927806. [DOI] [Google Scholar]
- 72. Lamers MM, Beumer J, van der Vaart J et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369(6499):50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Zhang H, Kang Z, Gong H et al. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69(6):1010–8. [Google Scholar]
- 74. To KK, Tsang OT, Yip CC et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71(15):841–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93(1):250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Wu J, Liu J, Li S et al. Detection and analysis of nucleic acid in various biological samples of COVID-19 patients. Travel Med Infect Dis. 2020;37:101673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tian S, Xiong Y, Liu H et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33(6):1007–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Yao X, Li T, He Z et al. [A pathological report of three COVID-19 cases by minimally invasive autopsies]. Zhonghua Bing Li Xue Za Zhi. 2020;49(5):411–7. [DOI] [PubMed] [Google Scholar]
- 79. Deshmukh V, Motwani R, Kumar A et al. Histopathological observations in COVID-19: a systematic review. J Clin Pathol. 2021;74(2):76–83. [DOI] [PubMed] [Google Scholar]
- 80. Zhang W, Du RH, Li B et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9(1):386–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ling Y, Xu SB, Lin YX et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl). 2020;133(9):1039–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158(6):1518–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Joynt GM, Wu WK. Understanding COVID-19: what does viral RNA load really mean? Lancet Infect Dis. 2020;20(6):635–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Dhar D, Mohanty A. Gut microbiota and Covid-19– possible link and implications. Virus Res. 2020;285:198018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Villapol S. Gastrointestinal symptoms associated with COVID-19: impact on the gut microbiome. Transl Res. 2020;226:57–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Guo W, Li M, Dong Y et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020; doi: 10.1002/dmrr.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Zuo T, Zhan H, Zhang F et al. Alterations in fecal fungal microbiome of patients with COVID-19 during time of hospitalization until discharge. Gastroenterology. 2020;159(4):1302–10.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Baud D, Dimopoulou Agri V, Gibson GR et al. Using probiotics to flatten the curve of coronavirus disease COVID-2019 pandemic. Front Public Health. 2020;8:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Segal JP, Mak JWY, Mullish BH et al. The gut microbiome: an under-recognised contributor to the COVID-19 pandemic? Therap Adv Gastroenterol. 2020;13:1756284820974914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Rishi P, Thakur K, Vij S et al. Diet, gut microbiota and COVID-19. Indian J Microbiol. 2020;60(4):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. van der Lelie D, Taghavi S. COVID-19 and the gut microbiome: more than a gut feeling. mSystems. 2020;5(4):e00453–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Donati Zeppa S, Agostini D, Piccoli G et al. Gut microbiota status in COVID-19: an unrecognized player? Front Cell Infect Microbiol. 2020;10:576551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Borges do Nascimento IJ, Cacic N, Abdulazeem HM et al. Novel coronavirus infection (COVID-19) in humans: a scoping review and meta-analysis. J Clin Med. 2020;9(4):941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lui RN, Wong SH, Sánchez-Luna SA et al. Overview of guidance for endoscopy during the coronavirus disease 2019 pandemic. J Gastroenterol Hepatol. 2020;35(5):749–59. [DOI] [PubMed] [Google Scholar]
- 95. Minodier L, Charrel RN, Ceccaldi P-E et al. Prevalence of gastrointestinal symptoms in patients with influenza, clinical significance, and pathophysiology of human influenza viruses in faecal samples: what do we know? Virol J. 2015;12(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Jayarajah U, Silva PK, Jayawardana P et al. Pattern of dengue virus infections in adult patients from Sri Lanka. Trans R Soc Trop Med Hyg. 2018;112(3):144–53. [DOI] [PubMed] [Google Scholar]
- 97. Jayarajah U, Madarasinghe M, Hapugoda D et al. Clinical and biochemical characteristics of dengue infections in children from Sri Lanka. Glob Pediatr Health. 2020;7:2333794X20974207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Jayarajah U, Lahiru M, De Zoysa I et al. Dengue infections and the surgical patient. Am J Trop Med Hyg. 2020;104(1):52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Borges do Nascimento IJ, von Groote TC, O'Mathúna DP et al. Clinical, laboratory and radiological characteristics and outcomes of novel coronavirus (SARS-CoV-2) infection in humans: a systematic review and series of meta-analyses. PLoS One. 2020;15(9):e0239235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Horby P, Lim WS, Emberson JR et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Ye Q, Wang B, Zhang T et al. The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19. Am J Physiol Gastrointest Liver Physiol. 2020;319(2):G245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wei PF. Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7). Chin Med J. 2020;133(9):1087–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Shah R, Klumpp LC, Syed N et al. Abdominal compartment syndrome in a patient suspected of coronavirus 2019 (COVID-19). J Infect Dis Epidemiol. 2020;6(4):139. [Google Scholar]
- 104. Rahman A, Niloofa R, Jayarajah U et al. Haematological abnormalities in COVID-19: a narrative review. Am J Trop Med Hyg. 2021; doi: 10.4269/ajtmh.20-1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Jayasinghe R, Jayarajah U, Seneviratne S. Consensus in surgical practice during the COVID-19 pandemic: an appraisal of the literature. Preprints. 2020; doi: 10.20944/preprints202006.0109.v1. [Google Scholar]
- 106. Collaborative C . Preoperative nasopharyngeal swab testing and postoperative pulmonary complications in patients undergoing elective surgery during the SARS-CoV-2 pandemic. Br J Surg. 2021;108(1):88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Jayasinghe R, Jayarajah U, Seneviratne S. Consensus on peri-operative surgical practice during the COVID-19 pandemic: an appraisal of the literature. Sri Lanka J Surg. 2020;38(2):57–61. [Google Scholar]
- 108. Barlow A, Landolf KM, Barlow B et al. Review of emerging pharmacotherapy for the treatment of coronavirus disease 2019. Pharmacotherapy. 2020;40(5):416–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Wang M, Cao R, Zhang L et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. A trial of remdesivir in adults with severe COVID-19. NCT04257656. Available from: https://clinicaltrials.gov/ct2/show/NCT04257656 [accessed 29 July 2020]. [Google Scholar]
- 111. A trial of remdesivir in adults with mild and moderate COVID-19. NCT04252664. Available from: https://clinicaltrials.gov/ct2/show/NCT04252664 [accessed 29 July 2020]. [Google Scholar]
- 112. MERS-CoV infection treated with a combination of lopinavir/ritonavir and interferon beta-1b (MIRACLE). NCT02845843. Available from: https://clinicaltrials.gov/ct2/show/NCT02845843 [accessed 18 March 2020]. [Google Scholar]
- 113. Deng L, Li C, Zeng Q et al. Arbidol combined with LPV/r versus LPV/r alone against corona virus disease 2019: a retrospective cohort study. J Infect. 2020;81(1):e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Lopinavir/ritonavir, ribavirin and IFN-beta combination for nCoV treatment. NCT04276688. Available from: https://clinicaltrials.gov/ct2/show/NCT04276688 [accessed 29 July 2020]. [Google Scholar]
- 115. Control of COVID-19 outbreaks in long term care. NCT04448119. Available from: https://clinicaltrials.gov/ct2/show/NCT04448119 [accessed 29 July 2020]. [Google Scholar]
- 116. Joshi S, Parkar J, Ansari A et al. Role of favipiravir in the treatment of COVID-19. Int J Infect Dis. 2020;102:501–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Tan Q, Duan L, Ma Y et al. Is oseltamivir suitable for fighting against COVID-19: in silico assessment, in vitro and retrospective study. Bioorg Chem. 2020;104:104257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Yang C, Ke C, Yue D et al. Effectiveness of arbidol for COVID-19 prevention in health professionals. Front Public Health. 2020;8:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Della-Torre E, Campochiaro C, Cavalli G et al. Interleukin-6 blockade with sarilumab in severe COVID-19 pneumonia with systemic hyperinflammation: an open-label cohort study. Ann Rheum Dis. 2020;79(10):1277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Baricitinib therapy in COVID-19. NCT04358614. Available from: https://clinicaltrials.gov/ct2/show/NCT04358614?term=NCT04358614&draw=2&rank=1 [accessed 2 March 2021]. [Google Scholar]
- 121. Richardson P, Griffin I, Tucker C et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395(10223):e30–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. COVID-19-associated ARDS treated with dexamethasone: alliance Covid-19 Brasil III (CoDEX). NCT04327401. Available from: https://clinicaltrials.gov/ct2/show/NCT04327401 [accessed 29 July 2020]. [Google Scholar]
- 123. Efficacy of dexamethasone treatment for patients with ARDS caused by COVID-19 (DEXA-COVID19). NCT04325061. Available from: https://clinicaltrials.gov/ct2/show/NCT04325061 [accessed 29 July 2020]. [Google Scholar]
- 124. Ferner RE, DeVito N, Aronson JK. Drug vignettes: dexamethasone . Available from: https://www.cebm.net/covid-19/dexamethasone/ [accessed 2 March 2021]. [Google Scholar]
- 125. Glucocorticoid therapy for COVID-19 critically ill patients with severe acute respiratory failure. NCT04244591. Available from: https://clinicaltrials.gov/ct2/show/NCT04244591 [accessed 29 July 2020]. [Google Scholar]
- 126. The efficacy of different hormone doses in 2019-nCoV severe pneumonia. NCT04263402. Available from: https://clinicaltrials.gov/ct2/show/NCT04263402 [accessed 29 July 2020]. [Google Scholar]
- 127. Fu H-Y, Luo Y, Gao J-P et al. Effects of short-term low-dose glucocorticoids for patients with mild COVID-19. BioMed Res Int. 2020;2020:2854186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Evaluation of efficacy of levamisole and formoterol+budesonide in treatment of COVID-19. NCT04331470. Available from: https://www.clinicaltrials.gov/ct2/show/NCT04331470 [accessed 29 July 2020]. [Google Scholar]
- 129. Cao W, Liu X, Bai T et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open Forum Infect Dis. 2020;7(3):ofaa102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Pourahmad R, Moazzami B, Rezaei N. Efficacy of plasmapheresis and immunoglobulin replacement therapy (IVIG) on patients with COVID-19. SN Compr Clin Med. 2020; doi: 10.1007/s42399-020-00438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Song Y, Liu P, Shi XL et al. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut. 2020;69(6):1143–4. [DOI] [PubMed] [Google Scholar]
- 132. Kujawski SA, Wong KK, Collins JP et al. Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med. 2020;26(6):861–8. [DOI] [PubMed] [Google Scholar]
- 133. Grein J, Ohmagari N, Shin D et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382(24):2327–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Sulkowski MS, Cooper C, Hunyady B et al. Management of adverse effects of Peg-IFN and ribavirin therapy for hepatitis C. Nat Rev Gastroenterol Hepatol. 2011;8(4):212–23. [DOI] [PubMed] [Google Scholar]
- 135. Charpiat B, Bleyzac N, Tod M. Proton pump inhibitors are risk factors for viral infections: even for COVID-19? Clin Drug Invest. 2020;40(10):897–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Almario CV, Chey WD, Spiegel BM. Increased risk of COVID-19 among users of proton pump inhibitors. Am J Gastroenterol. 2020;115(10):1707–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Lee SW, Ha EK, Yeniova AÖ et al. Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching. Gut. 2020;70(1):76–84. [DOI] [PubMed] [Google Scholar]
- 138. Taştemur Ş, Ataseven H. Is it possible to use proton pump inhibitors in COVID-19 treatment and prophylaxis? Med Hypotheses. 2020;143:110018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Rodríguez-Lago I, Ramírez de la Piscina P, Elorza A et al. Characteristics and prognosis of patients with inflammatory bowel disease during the SARS-CoV-2 pandemic in the Basque Country (Spain). Gastroenterology. 2020;159(2):781–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Rubin DT, Feuerstein JD, Wang AY et al. AGA clinical practice update on management of inflammatory bowel disease during the COVID-19 pandemic: expert commentary. Gastroenterology. 2020;159(1):350–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Bezzio C, Saibeni S, Variola A et al. Outcomes of COVID-19 in 79 patients with IBD in Italy: an IG-IBD study. Gut. 2020;69(7):1213–7. [DOI] [PubMed] [Google Scholar]
- 142. Kennedy NA, Jones GR, Lamb CA et al. British Society of Gastroenterology guidance for management of inflammatory bowel disease during the COVID-19 pandemic. Gut. 2020;69(6):984–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Rosen MH, Axelrad J, Hudesman D et al. Management of acute severe ulcerative colitis in a pregnant woman with COVID-19 infection: a case report and review of the literature. Inflamm Bowel Dis. 2020;26(7):971–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Divizia A, Sensi B, Sica GS. Ambulatory management of perianal Crohn's disease during the COVID-19 pandemic. Colorectal Dis. 2020;22(6):645–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. COVIDSurg Collaborative. Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Colorectal Dis. 2020; doi: 10.1111/codi.15431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Glasbey JC, Nepogodiev D, Simoes JFF et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol. 2021;39(1):66–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Bhat PKR, Santosh Kumar KY, Sorake C et al. Gastrointestinal malignancies and the COVID-19 pandemic: evidence-based triage to surgery. J Gastrointest Surg. 2020;24(11):2698–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. HO Al-Shamsi, Alhazzani W, Alhuraiji A et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25(6):e936–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. COVIDSurg Collaborative. Delaying surgery for patients with a previous SARS-CoV-2 infection. Br J Surg. 2020;107(12):e601–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Fligor SC, Wang S, Allar BG et al. Gastrointestinal malignancies and the COVID-19 pandemic: evidence-based triage to surgery. J Gastrointest Surg. 2020;24(10):2357–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Yu J, Ouyang W, Chua MLK et al. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6(7):1108–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article.