Abstract
Background
Governmental restrictions of daily life are key elements in reducing the transmission of COVID-19, but they have also put a strain on people’s mental health. Preventive policies differ all over the world as well as over different periods of time, and depend mostly on current infection rates. In Germany, there were two periods of restraint of varying severity, during which the government used different combinations of containment and mitigation measures to protect risk groups and to lower the number of hospitalizations.
Methods
In two online studies, we aimed to determine differences and similarities in COVID-19-related fear, generalized anxiety, depression and distress levels, as well as in the adherence to safety behaviour between the first lockdown in March and April and the second lockdown in November.
Results
This study showed continued high psychological burden and even increased levels of depression symptoms, as well as less safety behaviour in the second phase of restrictions.
Conclusions
The results hint at a prolonged negative impact on people’s mental health and their safety behaviour despite lesser restrictions in the second lockdown, which may be interpreted as pandemic fatigue and hence strengthens the argument for a low-threshold access to psychological care.
Keywords: COVID-19, lockdown, pandemic fatigue, mental health, depression
Introduction
The outbreak of the COVID-19 pandemic crucially defined the year 2020. To reduce the transmission of this now infamous strain of corona viruses, many countries announced preventive policies. These ‘non-pharmaceutical interventions’ (NPIs) varied between countries and had different effects on the spread of the virus.1 In Germany, the first educational institutions were closed on Friday, 13 March 2020. Two days later, German borders were partially closed, followed by a contact ban prohibiting gatherings of more than two people in public spaces on 22 March. This abrupt and unprecedented ‘lockdown’ was deemed necessary to protect risk groups and avoid capacity overload in hospitals.2 Thus, everyday life changed massively: many parents had to provide home schooling while simultaneously working from home, whereas sports and cultural facilities, department stores and restaurants were closed. Visits in hospitals and nursing homes were prohibited and visits to friends and families were strongly discouraged. These measures had a strong impact, not only on public life and the economic development, but also on people’s mental health.3,4 Recent research suggests increased prevalence of generalized anxiety, depression symptoms, psychological distress and COVID-19-related fear in the German population during the first lockdown5,6 with a peak 1 day after the announcement of the lockdown.7
After the expected drop in infection numbers at higher temperatures,8 a majority of the restrictions were gradually removed until late summer 2020. During the July and August holiday season, the infection rate slowly increased again, rapidly peaking in October. Instead of a complete second lockdown, the German government opted for a set of less rigorous strategies in mid-October aiming to reduce the negative impact on the country’s educational and economic activity. As infection numbers increased, governmental authorities reacted with further restrictions, commonly called ‘lockdown-light’, including travel prohibitions, contact bans regarding gatherings of >10 people from a maximum of two different households in public spaces, and the closure of public institutions such as cultural and sports facilities. In contrast to the first lockdown in March and April, wholesale and retail sectors, as well as schools and child day-care facilities remained open in October and November. These efforts have left Germany’s economy visibly less unsettled.9 Also, less strain was imposed on peoples’ everyday life and functioning.
Hence compared to the first lockdown, peoples’ mental health should potentially suffer less from fewer psychological burdens, i.e. from less overall uncertainty and economic stress, while experiencing higher levels of social buffering. With these proposed lower levels of fear, anxiety, depression and stress during the second lockdown, a feeling of putative security may lead to a decrease in adherent and dysfunctional safety behaviours, such as those recommended by the WHO.10
Methods
To test these assumptions, this study compared data from two cross-sectional studies collected in Germany. The surveys had comparable sets of items and were used to capture the critical and acute periods from 15 March to 4 April and from 2 November to 22 November. For the presented analyses, data were used from each respondent completing the survey within the first 20 days of each lockdown. Respondents indicated their subjective levels of COVID-19-related fear, generalized anxiety (GAD-7),11,12 depression (PHQ-2),13 distress (Distress Thermometer),14 adherent and dysfunctional safety behaviour. Adherent safety behaviour includes more frequent handwashing, disinfectant use and measures to avoid an infection with COVID-19, whereas dysfunctional safety behaviour includes buying more hygiene products, canned foods and groceries with the intention to store them for a longer time.10 We applied multiple robust regressions to compute and evaluate differences between the first and the second lockdown, while also controlling for different distributions of gender, age, community size, education and presence of a mental disease.
Results
Figure 1 illustrates the marginal differences in the regression models. Contrary to our initial hypotheses, depression symptoms increased during the ‘lockdown-light’ in November. In a similar fashion, neither generalized anxiety, distress nor COVID-19-related fear increased or decreased. Yet, in line with our assumptions, prevalence of adherent safety behaviour as well as dysfunctional safety behaviour was significantly lower.
Fig. 1.
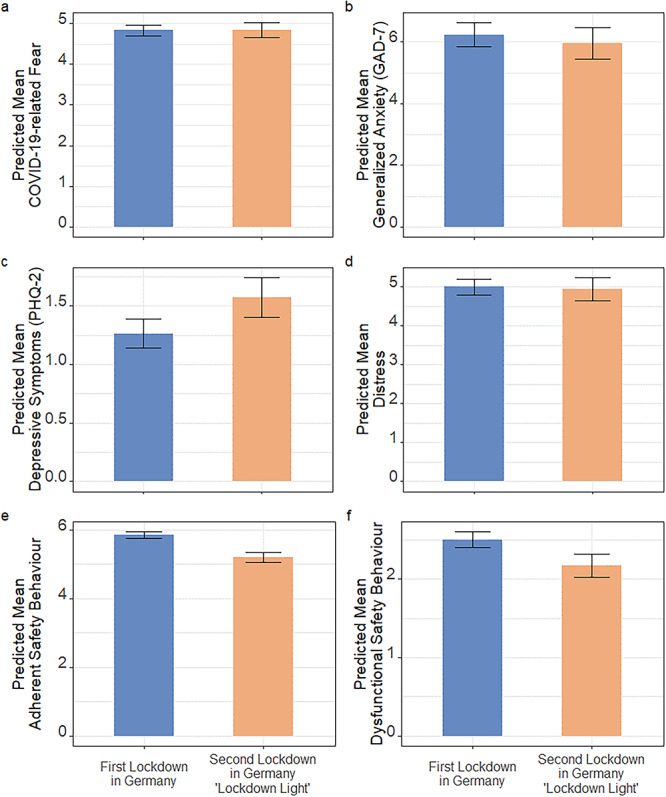
Results of the impact of the spread of COVID-19 on mental health and safety behaviour during the first and the second lockdown in Germany. Self-reported levels of (a) COVID-19-related fear (1 self-generated item, 7-point-likert-scale), (b) anxiety measured by GAD-7 (Generalized Anxiety Disorder-7, 7 items, 4-point Likert Scale from 0 = never to 3 = nearly every day), (c) depression using PHQ-2 (Patient health Questionnaire-2, 2 items on a 4-point Likert Scale from 0 = never to 3 = nearly every day), (d) distress using DT (distress thermometer, visual analogue scale from 0 = no distress to 10 = extreme distress), (e) adherent safety behaviour and (f) dysfunctional safety behaviour using self-generated Likert-type items on a 7-pointlikert scale. Bars represent the predicted marginal means. Error bars represent robust 95% CIs. Overall 7288 respondents participated.
Conclusions
This study showed continued high psychological burden, rising depression symptoms and less safety behaviour in the second lockdown despite lesser restrictions. Possible reasons for such developments are manifold and any mechanistic explanation would need direct causal evidence. One factor influencing these results may be the onset of ‘pandemic fatigue’, describing general mental exhaustion with pandemic ongoings and demotivation to follow recommended safety behaviours.15 This phenomenon may act as a destructive countermotion to governmental efforts to ‘flatten the curve’, i.e. reducing the spread of infections, which relies heavily on public adherence to restrictions. An explanation for the results could be paucity of positive reinforcement: People were more precluded from social contacts and sports compared to the summer following the first lockdown, which possibly provided a sense of relief and reward for the restraint shown in March and April.
Recent economic history may corroborate such a pattern: The economic repercussions of the COVID-19 crisis were still clearly evident in the German stock index DAX until June 2020.9 Although the government was beginning to loosen restrictions, economic insecurity continued until mid-summer. Such economic shocks have been shown to easily protract over longer periods of time.16,17 Here, a bidirectional effect may be possible: Increasing fear may influence consumption behaviour negatively and economic insecurity may add to COVID-19-fear resulting in continuing high anxiety symptoms in the population.18
In conclusion, this study shows increased depression symptoms and continued high psychological burden despite lesser restrictions in November. It also shows less safety behaviour despite higher infection rates. Hence, the question arises if the results promote more severe restrictions in times of a global pandemic. Besides, providing psychological emergency infrastructure for people suffering from the ongoing pandemic—especially those already burdened with mental health issues—remains crucial. As the crisis continues, further research may deliver insight to containing the spread of the disease by better understanding the reasons for decreased safety behaviour and finding ways to motivate people to adhere to recommended behaviours.
Acknowledgements
This study was supported by the Essen University Medicine Foundation. The funder had no role in the design and conduct of the study; management, collection, analysis, and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Sheila Moradian (SM), researcher.
Alexander Bäuerle (AB), deputy head of research.
Adam Schweda (AS), researcher.
Venja Musche (VM), researcher.
Hannah Kohler (HK), researcher.
Madeleine Fink (MF), researcher.
Benjamin Weismüller (BW), researcher.
Anke-Verena Benecke (AVB), researcher.
Nora Dörrie (ND), head of the outpatient clinic.
Eva-Maria Skoda (E-MS), head of research.
Martin Teufel (MT), director
Contributor Information
Sheila Moradian, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Alexander Bäuerle, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Adam Schweda, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Venja Musche, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Hannah Kohler, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Madeleine Fink, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Benjamin Weismüller, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Anke-Verena Benecke, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Nora Dörrie, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Eva-Maria Skoda, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Martin Teufel, University of Duisburg-Essen, Clinic for Psychosomatic Medicine and Psychotherapy, LVR Hospital Essen, 45147 Essen, Germany.
Conflict of interest
None declared.
References
- 1. Brauner JM, Mindermann S, Sharma M et al. Inferring the effectiveness of government interventions against COVID-19. Science 2020;eabd9338. doi: 10.1126/science.abd9338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bedford J, Enria D, Giesecke J et al. COVID-19: towards controlling of a pandemic. Lancet 2020;395:1015–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bäuerle A, Steinbach J, Schweda A et al. Mental health burden of the COVID-19 outbreak in Germany: predictors of mental health impairment. J Prim Care Community Health 2020;11:2150132720953682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Skoda EM, Spura A, De Bock F et al. Veränderung der psychischen Belastung in der COVID-19-Pandemie in Deutschland: Ängste, individuelles Verhalten und die Relevanz von information sowie Vertrauen in Behörden. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021;1–12German. doi: 10.1007/s00103-021-03278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bäuerle A, Teufel M, Musche V et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health (Oxf) 2020;42:672–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Petzold MB, Bendau A, Plag J et al. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav 2020;10:e01745. doi: 10.1002/brb3.1745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Teufel M, Schweda A, Dörrie N et al. Not all world leaders use twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J Public Health (Oxf) 2020;42:644–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dzien A, Dzien-Bischinger C, Lechleitner M et al. Will the COVID-19 pandemic slow down in the northern hemisphere by the onset of summer? An epidemiological hypothesis. Infection 2020;48:627–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Statista (2020). Monthly development of the German Stock Index (DAX). Germany: Statista Research Department. https://de.statista.com/statistik/daten/studie/162176/umfrage/monatliche-entwicklung-des-dax/. (01 Feburary 2021, date last assessed)
- 10. Weismüller B, Schweda A, Dörrie N et al. Different correlates of COVID-19-related adherent and dysfunctional safety behavior. Front Public Health 2020;8. doi: 10.3389/fpubh.2020.625664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kertz S, Bigda-Peyton J, Bjorgvinsson T. Validity of the generalized anxiety Disorder-7 scale in an acute psychiatric sample. Clin Psychol Psychother 2013;20:456–64. [DOI] [PubMed] [Google Scholar]
- 12. Löwe B, Decker O, Müller S et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care 2008;46:266–74. [DOI] [PubMed] [Google Scholar]
- 13. Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res 2005;58:163–71. [DOI] [PubMed] [Google Scholar]
- 14. Hinz A, Mitchell AJ, Dégi CL, Mehnert-Theuerkauf A. Normative values for the distress thermometer (DT) and the emotion thermometers (ET), derived from a German general population sample. Qual Life Res 2019;28:277–82. [DOI] [PubMed] [Google Scholar]
- 15. World Health Organization. Regional Office for Europe . (2020). Pandemic fatigue: reinvigorating the public to prevent COVID-19: policy considerations for Member States in the WHO European Region. Denmark, Regional Office for Europe, Lead authors Katrine Bach Habersaat and Andrea Elisabeth Scheel. https://apps.who.int/iris/handle/10665/335820. (01 February 2021, date last assessed)
- 16. Reeves A, McKee M, Gunnell D et al. Shocks, resilience, and male suicides in the great recession: cross-national analysis of 20 EU countries. Eur J Public Health 2015;25:404–9. [DOI] [PubMed] [Google Scholar]
- 17. Haushofer J, Fehr E. On the psychology of poverty. Science 2014;344:862–7. [DOI] [PubMed] [Google Scholar]
- 18. Hetkamp M, Schweda A, Bäuerle A et al. Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: relation to infection rates, deaths, and German stock index DAX. Sleep Med 2020;75:350–3. [DOI] [PMC free article] [PubMed] [Google Scholar]


