ABSTRACT
Introduction
The worldwide COVID-19 pandemic poses challenges to healthcare capacity and infrastructure. The authors discuss the structure and efficacy of the U.S. Navy’s response to COVID-19 and evaluate the utility of this endeavor, with the objective of providing future recommendations for managing worldwide healthcare and medical operational demands from the perspective of Navy Neurosurgery.
Materials and Methods
The authors present an extensive review of topics and objectively highlight the efforts of U.S. Navy Neurosurgery as it pertains to the humanitarian mission during the COVID-19 pandemic.
Results
During the humanitarian mission (March 27, 2020–April 14, 2020), the response of active duty and reserve neurosurgeons in the U.S. Navy was robust. Neurosurgical coverage was present on board the U.S. Navy Ships Mercy and Comfort, with additional neurosurgical deployment to New York City for intensive care unit management and coverage.
Conclusions
The U.S. Navy neurosurgical response to the COVID-19 pandemic was swift and altruistic. Although neurosurgical pathologies were limited among the presenting patients, readiness and manpower continue to be strong influences within the Armed Forces. The COVID-19 response demonstrates that neurosurgical assets can be rapidly mobilized and deployed in support of wartime, domestic, and global humanitarian crises to augment both trauma and critical care capabilities.
INTRODUCTION
The COVID-19 pandemic has dominated the healthcare and public sector for the majority of 2020. On January 5, 2020, a communication from the WHO reported 44 patients with pneumonia from Wuhan City, Hubei province, China,1 where the first person was likely infected in November 2019.2 In follow-up, an article published in the Journal of Travel Medicine on January 8, 2020, identified the potential for international spread through commercial air travel.3 The same day, the offending pathogen was identified as a novel coronavirus confirmed to be pathogenic in humans, and by February 11, 2020,4 the health crisis that has reached every corner of the planet had a name—SARS-CoV-2 for the virus and COVID-19 for the disease.5
Preventing the spread of COVID-19 has been the world’s primary health focus since the pandemic began. The reproductive number of COVID-19 (R0) is high, indicating its transmissibility and potential to infect large numbers of people. Mass infection has led to the oversaturation of healthcare infrastructure, as seen in Northern Italy.6 Infection with COVID-19 can be asymptomatic or may develop into a flu-like illness (fever, cough, and shortness of breath).7,8 Rarely, this can progress to severe acute respiratory syndrome, pneumonia, multi-organ failure, thromboembolic events, and death.9 Further delayed neurological complications of COVID-19, including encephalitis and cerebrovascular disease, are currently being elucidated, and their numbers are expected to rise.10
The initial wave of COVID-19 saw significant mobilization of healthcare workers across the globe, with the USA as no exception. Hospitals and other healthcare facilities across the USA began to prepare their staff and facilities to deal with large numbers of very sick and contagious patients. The U.S. Navy began preparations as well, with focus on its both own facilities and humanitarian needs. In this article, we discuss the Navy’s preparation, response, and readiness for the COVID-19 pandemic as it pertains to military neurosurgical practice.
Global Responsibilities
Navy Medicine is comprised of 63,000 medical personnel with a mission to provide well-trained medical experts, operating as high-performance teams, to project medical power in support of naval superiority. Navy Medicine also plays a large role in humanitarian assistance/disaster response missions. The primary objective of Navy Neurosurgery is to provide the highest quality neurosurgical care to U.S. Navy service members and beneficiaries. The current number of Navy neurosurgeons stands at 30 (20 active duty and 10 reservists) (Table I). Most are stationed at one of three MTFs—Naval Medical Center Portsmouth, Walter Reed National Medical Center (dual service Army and Navy), and Naval Medical Center San Diego—in the continental USA. In addition, there is a role III hospital in Okinawa, Japan, which is fully staffed by a neurosurgeon who receives relief on a rotating basis, and a role III hospital11 in Kandahar, Afghanistan, which is also staffed by a single neurosurgeon. Manpower can be shifted as necessary for humanitarian missions.
TABLE I.
Current Navy Neurosurgery Personnel
| Facility/location | Number of neurosurgeons |
|---|---|
| Naval Medical Center San Diego, San Diego, CA, USA | 6 |
| Walter Reed National Military Medical Center, Bethesda, MD, USA | 6 |
| Naval Medical Center Portsmouth, Portsmouth, VA, USA | 7 |
| U.S. Naval Hospital, Okinawa, Japan | 1 |
| NATO Role III, Kandahar Airfield in Afghanistan | (1a) |
| Active duty total | 20 |
| Navy reservists | 10 |
| Total | 30 |
The neurosurgeon at this instillation comes from one of three continental U.S. MTFs as a rotation.
During peacetime when there are no augmented humanitarian missions ongoing, the neurosurgery coverage is sufficient at these facilities. As the COVID-19 epidemic drew resources away for humanitarian mission activations, the neurosurgical capabilities at the three MTFs continued despite new decrements in staff. As national COVID-19 case levels rose and health systems threatened saturation, these institutions temporarily stopped elective surgical cases to protect bed, intensive care unit (ICU), ventilator, and personal protective equipment (PPE) capacity. Navy neurosurgeons at each MTF followed guidelines issued from national governing bodies (e.g., Congress of Neurological Surgeons and American Association of Neurological Surgeons), together with command-specific instruction, in determining elective versus urgent versus emergent neurosurgical need. The bulk of patient clinic visits were shifted to telehealth encounters to minimize potential virus transmission and to offer a means of triage to those in need of urgent neurosurgical intervention; in those patients harboring such a need, surgical intervention was not delayed. In parallel, neurosurgical staff were additionally cross-trained to augment MTF COVID-19 efforts, in recognition of the broad intensive care medicine training that every neurosurgeon must complete as part of residency training.
Humanitarian Missions
Navy Medicine plays an important role in humanitarian assistance/disaster response missions, and these missions remain an integral component of the comprehensive maritime strategy. This has been evident on numerous occasions, including relief efforts from domestically and globally. The Navy’s response to COVID-19 was no less committed.
Mobilization During Pandemic
Concern for overburdened healthcare infrastructure and depletion of resources (ICU beds, personnel, and PPE) prompted the Federal Emergency Management Agency, Department of Homeland Security, and Health and Human Services to request DoD support; the DoD responded by prompting the U.S. Armed Forces mobilization for a domestic humanitarian mission. The mission was to decompress the healthcare systems in high-density COVID-19 areas in the USA and provide logistical and clinical expertise. Although this was a DoD endeavor, here we have focused on the mobilization and efforts of the U.S. Navy neurosurgical specialty response.
Nearly 1,600 U.S. Navy Selected Reserve Sailors were deployed globally to combat the COVID-19 pandemic. On March 18, 2020, the DoD outlined a plan to employ the U.S. Naval Ship USNS Comfort (T-AH 20) and USNS Mercy (T-AH 19) in response to the growing threat of COVID-19 (Fig. 1).12 The Mercy-class hospital ships are converted supertankers retrofitted as hospital ships in the 1980s. Both Comfort and Mercy have seen deployment in support of combat casualty care and humanitarian missions. These high-visibility humanitarian missions have been included as a core tenant of the U.S. maritime strategy since 2007.13 In support of combat operations for Operation Iraqi Freedom, 630 wartime procedures were performed aboard Comfort between March 20, 2003, and May 6, 2003, including 11 neurosurgical procedures.14 Outside their combat casualty care missions, the Mercy-class hospital ships are typically deployed without neurosurgical assets. During the Pacific Partnership humanitarian exercises, neurosurgeons have deployed in support and performed procedures at host-nation facilities. During the COVID-19 pandemic, Navy Neurosurgery was tasked to participate, with neurosurgeons deployed on both ships. Each vessel’s original neurosurgical staffing consisted of one U.S. Navy reservist and one active duty neurosurgeon drawn from a tertiary care MTF.
FIGURE 1.

(A) Photograph of the USNS Mercy arriving in Los Angeles, CA (photo by Cpl. Alexa Hernandez). (B) Photograph of a U.S. Navy neurosurgeon and a U.S. Navy orthopedic surgeon in the operative theatre aboard the USNS Mercy (photo by Petty Officer 2nd Class Ryan Breeden). (C) Photograph of a U.S. Navy neurosurgeon performing a sacral washout and closure (case presented in Fig. 3) aboard the USNS Comfort. (D) Photograph of the USNS Comfort docked at New York, NY. The appearance of the U.S. DoD visual information does not imply or constitute DoD endorsement.
Comfort left Norfolk, Virginia, on March 29, 2020, and arrived in New York City on March 30. Comfort was ordered to assume care of non-COVID-related illnesses from New York area hospitals to ease the burden on overworked ICUs. Mercy departed San Diego, CA, and arrived in Los Angeles, CA, on March 27, 2020, with the same mission. Exponential growth of California’s COVID-19 numbers was predicted, prompting assignment to Los Angeles although case density was higher in Seattle, WA, at the time.
Both vessels were designated to act as trauma and emergency surgery beacons for the metropolitan landscape and to remain COVID-19 free. The neurosurgical mission aboard both Comfort and Mercy initially was one of preparation and readiness. Previous medical missions for the Mercy class have primarily involved orthopedic, ophthalmologic, and dental procedures. Typically, more complex surgical care requiring staged procedures, involving complication management beyond the mission window, and/or lacking appropriate local postoperative care are typically deferred, including all but the simplest neurosurgical procedures.15 For the COVID-19 response, more than 30 trays of surgical instruments were inventoried to create an emergency craniotomy kit and implants for spinal stabilization procedures. With the help of dedicated corpsmen, both ships were able to quickly augment surgical capacity to provide emergency neurosurgery, with areas of specific need identified for future expanded capabilities.
Both hospital ships carry the ability to run 12 onboard operating rooms, and each ship has a functional operating microscope. The ships were additionally equipped with loaned instrument sets supplied from the MTFs to allow cranial and spinal surgery capabilities. Shortly after the arrival of Mercy in Los Angeles and before the departure of Comfort from Norfolk, the neurosurgical staffing was reduced to one reserve neurosurgeon per vessel. While working toward making each ship “neurosurgery ready,” the neurosurgeons also functioned as general surgical liaisons and assistants for other surgical specialties.
Ultimately, given the difficulty in reorganizing emergency medical services systems to route patients to ships in large cities with pre-established emergency activation systems, the mission goals necessarily evolved. Following a request from New York Governor Cuomo on April 6, Comfort transformed from a 1,000-bed hospital with 12 operating rooms and an 80-bed ICU capacity for 60 mechanically ventilated patients13 to a 500-bed isolation-capable hospital for COVID-19 patients. Adaptive leadership and communication allowed a refocus toward treating COVID-19 patients. Flexibility is a trait particularly emphasized in deployed military medicine; in fact, military medicine trains to adapt to fluctuating battle scenarios, making its providers the ideal response team to this crisis.
A total of three patients received neurosurgical operative treatment between the two vessels: one patient underwent custom cranioplasty after an initial decompression performed for left hemispheric stroke at a civilian metropolitan hospital (Fig. 2), and two patients requiring wound revisions were treated. One of these was a COVID-19-positive patient with a decubitus ulcer (Fig. 3), and the other had a postoperative infection from an initial decompression performed elsewhere. The two neurosurgeons aboard the hospital ships participated in six total operations and saw several patient consults. In total, Comfort treated 182 patients while in port and departed New York Harbor on April 30 to return to Norfolk, VA. A neurosurgeon served aboard this vessel for 31 days. Mercy treated 77 patients and departed Los Angeles on May 14. A neurosurgeon served aboard this vessel for 60 days.
FIGURE 2.

(A,B) 3D CT reconstructions of a 55-year-old man with a history of hypertension, hyperlipidemia, and diabetes who experienced a large right hemispheric stroke and underwent a right hemicraniectomy by a neurosurgical team at Bellevue Hospital (New York, NY). He was transferred to the USNS Comfort for postoperative monitoring to relieve the overwhelmed hospital. (C,D) As his neurological examination findings improved to following commands, he underwent a right cranioplasty with a custom implant on post-hemicraniectomy day 24 onboard the ship. Postoperatively, his examination remained stable.
FIGURE 3.
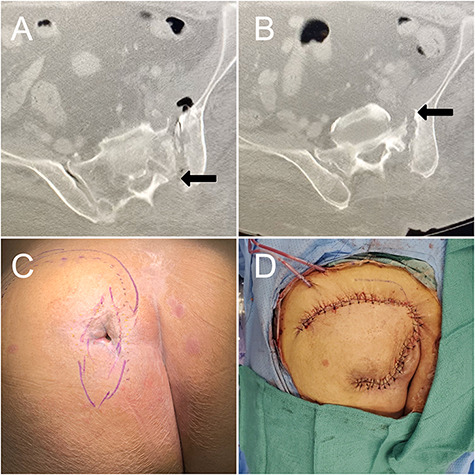
A 66-year-old woman with a history of sacral osteomyelitis leading to cutaneous fistula; she was COVID-positive but asymptomatic. Axial CT imaging showing destruction of the left posterior superior iliac spine (A, white arrow), left lateral sacrum, into the (B, black arrow) sacroiliac joint and anterior sacrum. She was admitted to the USNS Comfort after intravenous antibiotic treatment failed, and the wound began draining purulent material (C). She underwent a lumbosacral incision and drainage with gluteal flap with a combined neurosurgery and plastic surgeon involvement (D). The patient denied mechanical pain and without lumbosacral deformity, and no lumbopelvic stabilization was necessary.
While the efforts of Mercy and Comfort were underway, a reserve neurosurgeon was mobilized with Operation Gotham as part of the Navy Medicine Support Team (NMST). It is estimated that nearly 30% of the New York hospitals’ nurse and physician workforce was directly impacted by COVID-19 during the height of the pandemic. In another effort to augment healthcare personnel resources, the DoD activated the NMST with a total of 77 Navy doctors and 133 Navy nurses along with Army and Air Force colleagues to embed in 11 civilian public hospitals in New York City. The reserve neurosurgeon was activated and integrated into the civilian facility, Bellevue Hospital, within 36 hours and remained mobilized for a total of 84 days. Although no neurosurgical procedures were performed during this mobilization, skills were adapted, transitioned, or quickly learned for medical ICU work. This represented over 300 ICU encounters at Bellevue Hospital over the duration of deployment, including typical ICU procedures and advanced cardiopulmonary resuscitation. Collectively, the NMST treated nearly 31,000 patients in New York City during its mobilization.
Concomitant to the missions of Mercy and Comfort, active duty neurosurgeons at each of the MTFs were placed on 48-hour standby for mobilization with Expeditionary Medical Force (EMF) units. An EMF functions as an austere-environment expeditionary hospital with full resuscitation and emergency surgical capabilities.16 An EMF can be constructed and be operational within a 10-day period from initiation and to function as a self-sustaining medical facility. Each EMF is staffed in advance and activated when the need for such support presents itself. Although several of the EMF platforms have embedded neurosurgeons, most do not. As an example, Navy Reserve EMF Bethesda provided support to the medical relief at Javits Federal Medical Station, which was an alternative care facility set up at the Javits Convention Center in New York City. Ultimately, no neurosurgery support was necessary from EMF activation from any of the MTFs.
Diversifying Skill Sets
Critical care medicine is essential to the practice of neurosurgery. Neurosurgeons are therefore ideal to assist in the care of critically ill COVID-19 patients. Navy neurosurgeons underwent rapid, rigorous cross-training to help with ICU coverage for COVID-19 patients following guidance set forth by the American Association of Neurological Surgeons/Congress of Neurological Surgeons Joint Section on Neurotrauma and Critical Care. This training was executed by our military colleagues in anesthesiology and critical care medicine and included advanced airway management, ventilator support for COVID-19 patients, and intensive care medical management.
Logistical Challenges to Navy Neurosurgery During COVID-19
The Navy Neurosurgery footprint allows for providing care across the globe (Table I); however, even this coverage has limitations, and a number of challenges have arisen because of COVID-19. Currently, one neurosurgeon is assigned to support the forward medical mission in both Afghanistan and Japan, which results in significant burden on these two individuals. The installation at U.S. Naval Hospital Okinawa is a resource-limited, community-sized hospital in Southeast Asia. In addition to one full-time neurosurgeon, rotating coverage is usually supplied by active duty neurosurgeons from the continental USA. As a response to the pandemic, however, the DoD placed a travel restriction on service members,17 preventing relief coverage for an extended period of time.
Similar challenges affected the Navy’s only combat hospital, the North Atlantic Treaty Organization Role III, Kandahar Airfield, in Afghanistan. The DoD-imposed travel restrictions caused a delay in turnover at this facility. During this time, the mission of the combat hospital has also been transformed to meet the medical need while, importantly, minimizing risk to the facility. With orders to identify and isolate COVID-19, extreme measures are in place to ensure safety and preparation, including mandatory 15% monthly screening for all “high-risk” personnel. To date, there have been no COVID-19-related ICU admissions at Kandahar; however, preparedness for escalating case density remains integral to mission planning and execution. The threat of COVID-19 has also curtailed recreational activities and meal services to facilitate social distancing and reduce disease transmission. Although protecting personnel from COVID-19, these measures have created psychological stresses by socially isolating an already geographically isolated population.
Around the world, the COVID-19 pandemic has negatively affected the routine access to regional hospitals and obstructed—in some cases, prohibited—the transfer of patients to tertiary care centers18; these significant restrictions have been placed as a measure to limit the spread of the virus. For MTFs located in foreign locations, this prohibited any local transfer of patients, despite isolation and rigorous testing to rule out COVID-19 infection. For example, the lack of access to care posed a significant challenge recently in Southeast Asia. A young dependent with a ruptured arteriovenous malformation, expanding hematoma, and neurological decline requiring emergent surgical evacuation could not be transferred to a host-nation tertiary care facility after decompression and resection of the lesion25. Although CT angiography demonstrated no residual lesion, postoperative angiography could not be obtained to verify complete removal. The patient’s need for critical care and further imaging studies necessitated a trans-Pacific aeromedical evacuation to a U.S. MTF using a critical care air transport team. Aeromedical transport services were introduced in World War I19 to improve outcomes via rapid patient transport from forward-deployed MTFs to tertiary care centers.20,21 As a military neurosurgeon, devising treatment in far-forward, austere environments to deliver the “next-best” treatment for patients is mandatory.12,22 The constraints of the COVID-19 pandemic required alteration in the standard of care for this patient, albeit with no impact on her outcome to date. Nevertheless, this raises the issue of how postsurgical care for this patient or others at remotely located MTFs would have been handled without access to the medical evacuation resources.
Lessons Learned
For Navy Neurosurgery, there were several positives gained from the experience. Although the COVID-19 pandemic did not fully stress the available neurosurgical resources, the experience does offer a framework for future missions with similar casualty profiles. As such, this study may not be useful in evaluating the response and readiness to a more diverse and intensive event (natural disaster and major military conflict). From a manpower perspective, the ability to activate three Navy Reserve neurosurgeons within a period of 48 hours was an amazing demonstration of military agility. Because of the need to transition from citizen to sailor, reservists are usually given as much lead time as possible. Typical mobilization provides a 30-day notice, but during times of crisis this is not always the case.23 This speaks to the commitment of the reserve neurosurgeons to Navy medicine and its mission during a time of global crisis. Although the original objective of Mercy and Comfort was to function as a “relief valve” for busy metropolitan centers with a focus on trauma and other non-COVID-19 overflow patients, this quickly changed, particularly in New York City. Once the mission transitioned to one of COVID-19 management, the structure of operations and overall focus transitioned to managing exposure and keeping patients and service members safe. Because COVID-19 spreads primarily through respiratory droplets from coughing or sneezing,13 the close quarters on a hospital ship make transmission among crew, healthcare workers, and patients a significant concern.
Although the neurosurgical case volume was limited, the U.S. Navy neurosurgery’s response to COVID-19 demonstrates that neurosurgical assets can be rapidly mobilized to augment both trauma and critical care support during a humanitarian mission and highlights the potential to pivot these skillsets during combat operations and global health engagements. Three patients received neurosurgical operative treatment between the two vessels, and both ships were rapidly made neurosurgically capable, but the vast majority of surgical procedures were performed by general surgeons, otolaryngologists, and orthopedic surgeons—consistent with past missions.
Once the goals of the mission changed, the appropriation of neurosurgery personnel and resources could have been different. As evidenced by the efforts of NMST Gotham, transitioning additional neurosurgery support to an EMF unit or an intensive care setting would more effectively use skills possessed by these individuals. Readiness is a principle tenet of military medicine and should be at the forefront of Navy neurosurgeons’ minds when preparing for global disaster missions. Staging basic neurosurgical equipment aboard both hospital ships to perform a craniotomy, burr hole placement, ventriculostomy, and laminectomy should be planned moving forward. Although both ships carry surgical equipment, regular inventory and quality assessments are needed to avoid hastened augmentation of such resources should supplies expire or become incomplete.
Personnel requirements for both Comfort and Mercy initially included two neurosurgeons but were quickly changed to one after a week or two. Overstaffing is a superior strategy when the mission remains dynamic and was adjusted appropriately as the mission evolved. The original mission of the hospital ships was to perform trauma operations; however, emergency systems in each of the two cities were not set up for such a transition to allow this. Thus, improved central command and coordination within the regional disaster network may have helped execute the initial mission. Although the efforts of the Navy have come under scrutiny in the lay press,24 it is inappropriate to ignore the altruistic work and self-sacrifice of many to achieve a common goal of treating patients and providing service to those in need when the logistical challenges were systemic. Recognizing these challenges now will allow better planning and preparation for activation during future emergencies.
CONCLUSIONS
The U.S. Navy Neurosurgery response to the COVID-19 pandemic was swift and altruistic. Although treatment of neurosurgical pathologies was limited in the efforts, readiness and manpower continue to be strong influences within the Armed Forces. The COVID-19 response was proof-in-concept that neurosurgical assets stand ready for mobilization to augment trauma and critical care in future wartime, domestic, and global crises.
ACKNOWLEDGMENT
The authors thank Kristin Kraus, MSc, for her editorial assistance in preparing this paper.
Contributor Information
LCDR Vijay M Ravindra, Department of Neurosurgery, Naval Medical Center San Diego, San Diego, CA 92134, USA.
LCDR Gavin P Dunn, Department of Neurosurgery, Washington University in Saint Louis, St. Louis, MO 63110, USA.
CDR Shawn Belverud, Department of Neurosurgery, Naval Medical Center San Diego, San Diego, CA 92134, USA.
LCDR Christopher P Carroll, Department of Brain & Spine Surgery, Naval Medical Center, Portsmouth, VA 23708, USA.
LCDR Scott L Zuckerman, Department of Neurosurgery, Columbia University, New York, NY 10032, USA.
LCDR Richard Menger, Departments of Neurosurgery and Political Science, University of Southern Alabama, University of South Alabama, Mobile, AL 36604, USA.
CAPT David Malone, Department of Neurosurgery, Ascension St. John, Tulsa, OK 74104, USA.
CDR Jonathon Cooke, Department of Neurosurgery, Naval Medical Center San Diego, San Diego, CA 92134, USA.
CDR Paul Porenksy, Department of Neurosurgery, Naval Medical Center San Diego, San Diego, CA 92134, USA.
CAPT Arnett Klugh III, Department of Neurosurgery, Naval Medical Center San Diego, San Diego, CA 92134, USA.
CAPT Jonathan Gilhooly, Department of Neurosurgery, Walter Reed National Military Medical Center, Bethesda, MD 20814, USA.
CAPT Jeffrey Tomlin, Department of Brain & Spine Surgery, Naval Medical Center, Portsmouth, VA 23708, USA.
CAPT Randy Bell, Department of Neurosurgery, Walter Reed National Military Medical Center, Bethesda, MD 20814, USA.
CDR Daniel S Ikeda, Department of Surgery, US Naval Hospital Okinawa, Chatan, Okinawa 904-0103, Japan.
FUNDING
There was no funding received for this work.
CONFLICT OF INTEREST STATEMENT
There are no financial or non-financial disclosures to report.
REFERENCES
- 1. World Health Organization : Pneumonia of unknown cause. Available at https://www.who.int/csr/don/05-january-2020-pneumonia-of-unknown-cause-china/en/; accessed July 10, 2020.
- 2. Berger K: The man who saw the pandemic coming. Nautilus, 2020(83). Available at http://nautil.us/issue/83/intelligence/the-man-who-saw-the-pandemic-coming; accessed March 20, 2020.
- 3. Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K: Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med 2020; 27(2): taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. ProMED : Undiagnosed pneumonia—China (HU)(07): official confirmation of novel coronavirus. Available at https://scholar.harvard.edu/files/kleelerner/files/20200110_promed_-_undiagnosed_pneumonia_-_china_hubei_09-_novel_coronavirus_more_information_first_fatality.pdf; accessed June 10, 2020.
- 5. World Health Organization : Naming the coronavirus disease (COVID-19) and the virus that causes it. Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it; February 11, 2020; accessed July 11, 2020.
- 6. Romagnani P, Gnone G, Guzzi F, et al. : The COVID-19 infection: lessons from the Italian experience [published online ahead of print May 29, 2020]. J Public Health Policy. 10.1057/s41271-020-00229-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention : Coronavirus disease 2019 (COVID-19): symptoms of coronavirus. 2020. Available at https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html; accessed July 16, 2020.
- 8. Chen N, Zhou M, Dong X, et al. : Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395(10223): 507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hui DS, Azhar EI, Madani TA, et al. : The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis 2020; 91: 264–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ellul MA, Benjamin L, Singh B, et al. : Neurological associations of COVID-19. Lancet Neurol 2020; 19(9): 767–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cubano M, Butler F, Borden Institute (U.S.) : Emergency War Surgery. Borden Institute. US Army Medical Department Center and School. Health Readiness Center of Excellence. Office of the Surgeon General, U.S. Army; 2018. [Google Scholar]
- 12. Lopez C: Hospital ships, other DOD assets prepare for coronavirus response. US Department of Defense. Available at https://www.defense.gov/Explore/News/Article/Article/2116862/hospital-ships-other-dod-assets-prepare-for-coronavirus-response/; accessed July 11, 2020.
- 13. Centers for Disease Control and Prevention : Coronavirus Transmission. 2020. [Google Scholar]
- 14. Paine GF, Bonnema CL, Stambaugh TA, Capacchione JF, Sipe PS: Anesthesia services aboard USNS COMFORT (T-AH-20) during Operation Iraqi Freedom. Mil Med 2005; 170(6): 476–82. [DOI] [PubMed] [Google Scholar]
- 15. Provencher MT, Douglas TD: Humanitarian assistance and disaster relief aboard the USNS Mercy (TAH-19). J Surg Orthop Adv 2011; 20(1): 38–43. [PubMed] [Google Scholar]
- 16. Navy Expeditionary Combat Command Public Affairs : Expeditionary medical facility training at PacBlitz19. U.S. Navy. NNS190325-190312. Available at https://www.navy.mil/submit/display.asp?story_id=109015; accessed July 11, 2020.
- 17. U.S. Department of Defense: Update to travel restrictions: Available at https://www.defense.gov/Newsroom/Releases/Release/Article/2156918/update-to-travel-restrictions; April 20, 2020; accessed July 11, 2020.
- 18. Cenzato M, DiMeco F, Fontanella M, Locatelli D, Servadei F: Editorial. Neurosurgery in the storm of COVID-19: suggestions from the Lombardy region, Italy (ex malo bonum) [published online ahead of print April 10, 2020]. J Neurosurg. 10.3171/2020.3.JNS20960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Loyd JW, Larsen T, Swanson D: Aeromedical transport. StatPearls, 2020. Available at https://www.ncbi.nlm.nih.gov/books/NBK518986/; accessed July 13, 2020. [PubMed]
- 20. Fang R, Dorlac GR, Allan PF, Dorlac WC: Intercontinental aeromedical evacuation of patients with traumatic brain injuries during Operations Iraqi Freedom and Enduring Freedom. Neurosurg Focus 2010; 28(5): E11. [DOI] [PubMed] [Google Scholar]
- 21. Boyd LR, Borawski J, Lairet J, Limkakeng AT Jr.,: Critical Care Air Transport Team severe traumatic brain injury short-term outcomes during flight for Operation Iraqi Freedom/Operation Enduring Freedom. J R Army Med Corps 2017; 163(5): 342–6. [DOI] [PubMed] [Google Scholar]
- 22. Neff LP, Cannon JW, Charnock KM, Farmer DL, Borgman MA, Ricca RL: Elective pediatric surgical care in a forward deployed setting: what is feasible vs. what is reasonable. J Pediatr Surg 2016; 51(3): 409–15. [DOI] [PubMed] [Google Scholar]
- 23. Times M: 2012. Insider’s guide to the guard & reserve handbook: activation and deployment. Available at http://ec.militarytimes.com/guard-reserve-handbook/activation-deployment/types-of-activation/; accessed July 11, 2020.
- 24. Schwirtz M: The 1,000-bed comfort was supposed to aid New York. It has 20 patients. The New York Times. April 2, 2020; updated April 7, 2020. Available at https://www.nytimes.com/2020/04/02/nyregion/ny-coronavirus-usns-comfort.html; accessed July 21, 2020.
- 25. Ikeda DS, Dryden JR, Van Gent JM, et al. : Transpacific aeromedical evacuation for a ruptured brain arteriovenous malformation during the COVID-19 pandemic. Mil Med November 20, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]


