ABSTRACT
Objectives:
To assess the frequency of frontal sinus aplasia using computed tomography (CT) of the paranasal sinus among Saudi Arabian population.
Methods:
A retrospective case review of medical records from January 2019 to December 2019 in the Otorhinolaryngology Department, King Abdulaziz University, Riyadh, Saudi Arabia.
Results:
A total of 449 cases were reviewed. The incidence of bilateral frontal sinus aplasia was 3.3%. The incidence of right sinus agenesis was 5.12% and left was 1.33%. The mean age of reviewed patients was 39.15 years.
Conclusion:
The frequency of frontal sinus aplasia is low; however, this must be considered before surgical operations related to the sinuses.
Keywords: frontal sinus, aplasia, agenesis, unilateral, bilateral
The frontal sinuses are pneumatized chambers located within the frontal bone, behind the supraorbital ridge, in close relation with the orbit and anterior skull base. They consist of right and left sinuses, separated by a midline bony nasal septum. The right and left sinuses are usually asymmetrical in the same person because they evolve independently.1 Each of these sinuses drains into the corresponding nasal middle meatus through ethmoid infundibulum or frontonasal duct.2 The frontal sinuses are absent at birth; however, they grow up at 7-8 years and fully mature after puberty. At adulthood, the frontal sinus volume is not consistent, with a mean size of 10 cc. This difference is usually detected among subjects of similar age.2 Through its ciliated mucosae and profuse mucous, it represents a major role in immune defense against foreign bodies introduced through the nose.3
Unilateral or bilateral frontal sinus aplasia can be incidentally detected in the clinical setting. However, this has been rarely reported in the literature, and there are inconsistent statistics among different reports.4-7 In a recent study carried out in India, the incidence of bilateral frontal sinus absence was 2.5% and unilateral 6.2%.7 In another study among Turkish population, the frequency of unilateral frontal sinus aplasia was 1.22%.8
Searching the literature, a recent study of 942 cases in Saudi Arabia revealed that frontal sinus agenesis was detected in 7.3%.9 In addition, it has been established that radiographic imaging and sufficient knowledge of the frontal sinus anatomical variation are substantial parts of the pre-surgical assessment as well as the identification of individuals for forensic purpose.10,11 Therefore, this study aimed to investigate the frequency of frontal sinus aplasia using computed tomography (CT) of the paranasal sinus among the Saudi Arabian population.
Methods
This is a retrospective case review of medical records from the Otorhinolaryngology Department, King Abdulaziz University Hospital, Riyadh, Saudi Arabia. This study has been conducted according to the relevant approved guidelines, regulations, ethics standard of the Helsinki declaration and also approved by the ethics committee of the relevant department. The inclusion criteria entailed reviewing of only CT scans of the paranasal sinus for patients admitted from January 2019 to December 2019. No CT scans before or after that period were considered.
Definitions and data collection
All CT scans of the paranasal sinus have been independently screened to evaluate the presence or absence of frontal sinus aplasia. All CT scan were performed using the same machine with thin cut paranasal sinuses CT for all candidates. Authors of this research have examined the CT scans with help of radiology specialists. Frontal sinus aplasia was defined as the absence of frontal bone pneumatization with no ethmoid cells extending above the supraorbital margin. Frontal sinus aplasia can be either bilateral (Figure 1) or unilateral aplasia (Figure 2).4 There was no potential risks of any kind associated with this study. All data have been analyzed and recorded anonymously, patients’ names were not declared, and only the authors of this research had access to the data. The primary endpoint of this research is the prevalence of unilateral or bilateral frontal sinus aplasia while the secondary endpoint is identifying associated diseases that caused patients’ presentation to the hospital.
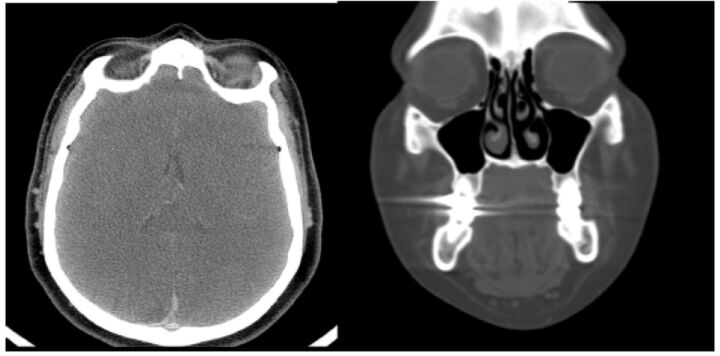
Figure 1.
- Computed tomography of paranasal sinuses, coronal and axial, showing bilateral frontal sinus aplasia.
Figure 2.
- Computed tomography of paranasal sinuses, coronal and axial, showing unilateral frontal sinus aplasia
Statistical analysis
All data analysis was carried out using SPSS software version 26. Simple descriptive statistics of patients’ age, gender, and presence/absence of unilateral or bilateral aplasia were provided. Continuous data were reported as mean±standard deviation while categorical data were reported as numbers and frequencies.
Results
Data of 449 patients were reviewed. Of them, 226 (50.3%) were males and 223 (49.7%) were females. The mean age of the whole subjects was 39.15 years. Bilateral frontal sinus agenesis was detected in 15 (3.3%) patients. Right was reported in 23 (5.1%) and left aplasia in 6 (1.3%) cases. Stratification of data according to gender along with group mean age are shown in Table 1. Deviated nasal septum, rhinosinusitis, headache, and allergic rhinitis were the most commonly reported diagnosis at presentation (Appendix 1).
Table 1.
- Frequency of frontal sinus aplasia.
| Variables | Number | Frontal sinus aplasia | ||
|---|---|---|---|---|
| Bilateral | Unilateral | |||
| Right | Left | |||
| Male | 226 (50.3) | 8 (3.53) | 9 (4.0) | 2 (0.9) |
| Female | 223 (49.7) | 7 (3.13) | 14 (6.3) | 4 (1.8) |
| Total sample | 449 (100.0) | 15 (3.34) | 23 (5.1) | 6 (1.3) |
| Age (mean±SD) | 39.15±15.39 | 39.86±13.18 | 47.52±16.6 | 36.66±13.66 |
All data are presented as N(%) unless indicated.
Discussion
The present study is a retrospective case review of CT of the paranasal sinus to report frontal sinus aplasia. Knowing the anatomical difference of the frontal sinus is essential for both forensic and surgical purposes. In the current report, the overall incidence of bilateral frontal sinus aplasia was 3.34%. In a recent study among 167 Jordanian individual, the prevalence of bilateral frontal sinus aplasia was 4.2%.12 In another cross-sectional study of 730 patients in India, the frequency of bilateral aplasia was 2.5%.7 The present study had no limitation on age; however, the authors of the aforementioned study only enrolled subjects over 10 years.7 In addition, another larger study of 1200 cases, aged or above 15 years, concluded that the frequency of frontal sinus aplasia was 3.8%.4 Within a similar incidence rate, another 2 studies published in 1943 reported overall bilateral absence of 5% and in 1977 was 3.4%.5,6 These frequencies are not consistent with the report of Cakur et al,8 where the retrospective analysis of 410 patients revealed bilateral frontal sinus agenesis of only 0.37%.
In our results, the frequency of right frontal sinus absence was 5.12% while the left side aplasia was 1.33%. In Al-Balas et al12 report, prevalence of unilateral frontal sinus aplasia was 6.6% among Jordanian patients. In the Sheriff et al study,7 the incidence of right agenesis was 3.7% and left was 2.5%. In 2003,4 a study of 1200 cases reported a unilateral incidence of frontal sinus absence of 4.8% (males: 23, females: 35). Interestingly, a study of 35 Japanese cases reported that the frequency of unilateral frontal sinus absence was 16.8 on the left side and 4.9% on the right side.13 By way of contrast, the Cakur et al8 study revealed that the frequency of unilateral frontal sinus absence was 0.73% for the right sinus and 0.49% for the left sinus.
In terms of gender difference, bilateral sinus aplasia was reported in 8 males compared to 9 females. Notably, both right and left unilateral sinus aplasia were higher among females in comparison to males (6.27 versus 3.98) and (1.79 versus 0.88), respectively. This is consistent with the Sheriff et al7 findings, where females had higher frequencies for unilateral (4% versus 2.2%) and bilateral aplasia (1.50% versus 0.95%). Similarly, the Turkish report of 1200 cases reported a higher incidence of frontal sinus absence among females than males for unilateral (5.9% versus 3.8%) and bilateral aplasia (5.1% versus 1.3%).4 Furthermore, the Cakur et al8 study reported that bilateral aplasia was higher among females (0.49%) compared to males (0.24%). Knowing the anatomical variation of frontal sinus is essential for forensic medicine professionals as well as neurosurgeons. For instance, proper identification of subjects can be reached through comparing the frontal sinus radiographs ante- and post mortem, since these images are characteristic for each individual.11,14,15 This method is not appropriate for cases with absent frontal sinus; thus, sphenoid sinus can be used along with other standard methods of identification.11,14,15 On another hand, a better understanding of anatomical differences will assist neurosurgeons performing pterional or supraorbital operations, and lessens the complications due to the close relation of the sinus to the surroundings including orbit and frontal skull base.10 Although the present study is the first report among the Saudi Arabian population, it has been limited by being conducted as a single-center and including a relatively small number of cases.
In conclusion, the frequency of frontal sinus aplasia in the present study is low and similar percentages were reported in the literature; however, this must be taken into consideration. Multiple reports, including the present one, revealed that females had higher frequencies of bilateral and unilateral frontal sinus absence. Furthermore, the incidence of right frontal sinus aplasia was higher than the left side. Comprehensive knowledge of the frontal sinus anatomy is essential for those practicing surgical interventions approximate to the sinuses, such as endoscopic sinus and anterior skull base operations. Future multi-center studies are recommended to investigate the incidence and associated pathologies.
Acknowledgment.
This study was supported by King Saud University, Deanship of Scientific Research, College of Medicine Research Center, Riyadh, Kingdom of Saudi Arabia. We would like to thank Editage (www.editage.com) for English language editing.
Appendix 1. - Reported diagnosis of patients with frontal sinus aplasia at presentation
| Condition | Frontal sinus aplasia | ||
|---|---|---|---|
| Bilateral | Unilateral | ||
| Right | Left | ||
| Allergic rhinitis | 0 | 3 | 2 |
| Brain ischemia | 0 | 1 | 0 |
| Concha bullosa | 0 | 1 | 0 |
| Convulsion | 1 | 0 | 0 |
| Deviated nasal septum | 6 | 3 | 2 |
| Dizziness | 0 | 1 | 0 |
| Facial trauma | 1 | 0 | 0 |
| Headache | 0 | 4 | 1 |
| Hypertrophy inferior turbinates | 1 | 0 | 0 |
| Nasal polyposis | 1 | 1 | 0 |
| Nasopharyngeal mass | 0 | 1 | 0 |
| Rhinosinusitis | 2 | 6 | 0 |
| Septal perforation | 1 | 1 | 0 |
| Thyroid mass | 1 | 1 | 1 |
| Thyroid nodule | 1 | 0 | 0 |
Footnotes
References
- 1.Wormald PJ, Hoseman W, Callejas C, Weber RK, Kennedy DW, Citardi MJ, et al. . The International Frontal Sinus Anatomy Classification (IFAC) and Classification of the Extent of Endoscopic Frontal Sinus Surgery (EFSS). Int Forum Allergy Rhinol 2016; 6: 677–696. [DOI] [PubMed] [Google Scholar]
- 2.Sommer F, Hoffmann TK, Harter L, Döscher J, Kleiner S, Lindemann J, et al. . Incidence of anatomical variations according to the International Frontal Sinus Anatomy Classification (IFAC) and their coincidence with radiological sings of opacification. Eur Arch Otorhinolaryngol 2019; 276: 3139–3146. [DOI] [PubMed] [Google Scholar]
- 3.Godinho RM, O’Higgins P.. The biomechanical significance of the frontal sinus in Kabwe 1 (Homo heidelbergensis). J Hum Evol 2018; 114: 141–153. [DOI] [PubMed] [Google Scholar]
- 4.Aydinlioğlu A, Kavakli A, Erdem S.. Absence of frontal sinus in Turkish individuals. Yonsei Med J 2003; 44: 215–218. [DOI] [PubMed] [Google Scholar]
- 5.Schuller A. A note on the identification of skulls by x-ray pictures of the frontal sinuses. Medical Journal of Australia 1943; 1: 554–556. [Google Scholar]
- 6.Nowak R, Mehlis G. “Aplasia of the sinus maxillares and frontales under the special regard of the pneumatisation of cleft patients”. Anat Anz 1977; 142: 441–450. [PubMed] [Google Scholar]
- 7.Sheriff RM, Moideen CP.. Incidence of frontal sinus aplasia in Indian population. International Journal of Otorhinolaryngology and Head and Neck Surgery 2017; 3: 108. [Google Scholar]
- 8.Çakur B, Sumbullu MA, Durna NB.. Aplasia and agenesis of the frontal sinus in Turkish individuals: a retrospective study using dental volumetric tomography. Int J Med Sci 2011; 8: 278–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alshaikh N, Aldhurais A.. Anatomic variations of the nose and paranasal sinuses in saudi population: computed tomography scan analysis. The Egyptian Journal of Otolaryngology 2018; 34: 234. [Google Scholar]
- 10.Ozgursoy OB, Comert A, Yorulmaz I, Tekdemir I, Elhan A, Kucuk B.. Hidden unilateral agenesis of the frontal sinus: human cadaver study of a potential surgical pitfall. Am J Otolaryngol 2010; 31: 231–234. [DOI] [PubMed] [Google Scholar]
- 11.Gnanavelraja C, Nalinakumari S, Rajajeyakumar M.. Anatomical variation in the drainage pattern of frontal sinus-A cadaveric study. National Journal of Clinical Anatomy 2019; 8: 117. [Google Scholar]
- 12.Al-Balas HI, Nuseir A, Alzoubi F, Alomari A, Bani-Ata M, Almehzaa S, et al. . Prevalence of Frontal Sinus Aplasia in Jordanian Individuals. J Craniofac Surg 2020; 31: 2040–2042. [DOI] [PubMed] [Google Scholar]
- 13.Yoshino M, Miyasaka S, Sato H, Seta S.. Classification system of frontal sinus patterns by radiography. Its application to identification of unknown skeletal remains. Forensic Sci Int 1987; 34: 289–299. [DOI] [PubMed] [Google Scholar]
- 14.Cameriere R, Scendoni R, Lin Z, Milani C, Palacio LAV, Turiello M, et al. . Analysis of frontal sinuses for personal identification in a Chinese sample using a new code number. J Forensic Sci 2020; 65: 46–51. [DOI] [PubMed] [Google Scholar]
- 15.Buyuk SK, Karaman A, Yasa Y.. Association between frontal sinus morphology and craniofacial parameters: A forensic view. J Forensic Leg Med 2017; 49: 20–23. [DOI] [PubMed] [Google Scholar]