ABSTRACT
Background
During the Covid-19 pandemic fake news has been circulating impacting on the general population’s opinion about a vaccine against the SARS-CoV-2. Health literacy measures the capacity of navigating health information.
Methods
We used data from a prospective national online cohort of 1647 participants. Descriptive statistics, Chi2 and ANOVA independence tests and two multivariable multinomial regression models were performed. Interactions between each variable were tested.
Results
Detection of fake news and health literacy scores were associated with intention to get vaccinated against SARS-CoV-2 (p < 0.01). The risk of being “anti-vaccination” or “hesitant”, rather than “pro-vaccination”, was higher among individuals reporting bad detection of fake news, respectively OR = 1.93 (95%CI = [1.30;2.87]) and OR = 1.80 (95%CI = [1.29;2.52]). The risk of being in “hesitant”, rather than “pro-vaccination” was higher among individuals having a bad health literacy score (OR = 1.44; 95%CI = [1.04;2.00]). No interaction was found between detection of fake news and health literacy.
Conclusions
To promote acceptance of a vaccine against SARS-CoV-2, it is recommended to increase individuals’ ability to detect fake news and health literacy through education and communication programs.
Keywords: misinformation, fake news, health literacy, vaccination, Covid-19
Introduction
Misinformation about health-related subjects represents a public health threat. Around Covid-19, fake news has been circulating extensively since the beginning of the pandemic thus making the general audience doubt the veracity of health and political authorities concerning information around the SARS-CoV-2.1 In February, the World Health Organisation’s Director-General declared the global ‘over-abundance’ of Covid-19 information an ‘infodemic’.
One of the challenges for health communication introduced by Covid-19 has been to tackle this increasing amount of false content on several communication channels, including social media platforms.2 Common fake news about Covid-19 include the fact that only older adults can be infected, that swallowing bleach can kill the virus or that the virus is the product of a laboratory.3 For instance, in Iran, hundreds of people died after ingesting alcohol in a bid to treat Covid-19 as a result of misinformation circulating on social media.4
The large spread of misinformation about Covid-19 might be explained by the initial scarce knowledge about the virus among the scientific community and politicians. Confusion generated by the plethora of news across media could have nourished misinformation and lack of trust in scientific evidence, especially in a situation where people have been looking for immediate and reassuring answers regarding the SARS-CoV-2.5 Spread of fake news has been fueled also by public figures and politicians who have been giving, in some cases, contradictory information, as the controversy over the wearing of masks in France.6
Of particular concern is the misinformation concerning Covid-19 vaccines, fueled by conspiracies (e.g., economic interests) and rumors of safety.7 Misinformation and misbeliefs can influence willingness to follow the recommendations by health and political authorities on vaccination. A number of studies found that fake news are a main cause of vaccine hesitancy,8–10 defined as the delay in acceptance or refusal of vaccination despite availability of vaccination services.11 A global survey in 19 world countries has showed that rates of hesitancy concerning a vaccine against the SARS-CoV-2 range from 11.4% (China) to 45.1% (Russia),12 which are not negligible numbers. In the Covid-19 pandemic context, it is important to mitigate the impact of misinformation on the decision of not getting vaccinated.
As a means to counteract misinformation, health literacy (HL) is the extent to which people can access, understand, appraise and apply health-related information through all communication channels.13 Measured through ad hoc scales,14 health literacy can assess the motivation and capacity of people to make informed decisions based on trustworthy information. According to the health literacy theory, it can be hypothesized that engaging in a positive health information seeking can help better navigate news and, consequently promote recognition of misinformation.15 Therefore, HL appears to be in close correlation with detection of fake news. Recent studies have explored separately the spread of fake news,16,17 health literacy18,19 and vaccine hesitancy20,21 in the Covid-19 era, without the exploration of the interrelation of these three factors.
Detection of fake news might represent a proxy for other proximal and intermediate causal factors and mechanisms that could explain the acceptance of a vaccine. The mediating role of HL has been assessed in several associations like between socio-economic status and health,22 population characteristics and use of health services23 or between education and health outcomes.24 The role of HL in the relation between detection of fake news and vaccine hesitancy has not been explored,yet.
This study aimed to investigate the relations between intention to get vaccinated against the SARS-CoV-2 and the ability to detect fake news about Covid-19 as well as health literacy among a population-based sample of French adults. We hypothesized that higher acceptance of a vaccine against the SARS-CoV-2 was associated with higher ability to detect fake news related to Covid-19 and that this association was mediated by health literacy levels.
Methods
Design, participants and ethics approval
The data used in this study are from a prospective online cohort exploring the impact of Covid-19 and lockdown on the health and wellbeing of French adults (CONFINS cohort, www.confins.org). The baseline questionnaire was administered in the period between April 8th and May 11th 2020. Participants were recruited via advertisement on traditional (press, radio and TV spots) and social media (e.g., Facebook, LinkedIn). Eligibility criteria were being able to read and understand French, being aged 18+, being confined at the moment of the inclusion and not having declared “other” for the variablesex.
Ethics approval was obtained from the French Committee for the Protection of Individuals (Comité de Protection des Personnes—CPP, nr. 46–2020) and the French National Agency for Data Protection (Commission Nationale Informatique et Libertés—CNIL, nr. MLD/MFI/AR205600). Participants had to electronically sign a consent form before starting the completion of the questionnaire.
Measures
The outcome variable was the intention to get vaccinated against the SARS-CoV-2. We used the item “Would you be willing to get vaccinated against coronavirus even if the vaccine has not yet been fully proven effective?”. Response modalities were: “No”, “Yes” or “I do not know”. We established a priori that the answer “No” corresponded to the “anti-vaccination group”, the answer “Yes” to the “pro-vaccination” group and the answer “I do not know” to the “hesitant group”.
The primary exposure variable was detection of fake news. Participants had to establish whether the following 8 items (i.e., potential fake news) were true (1 point), false (0 point) or I do not know (0 point): “The Covid-19 virus has been developed in a laboratory”, “The virus can be transmitted through the air”, “Only people over 70 years of age can die from Covid-19”, “The virus can only be transmitted by people who have symptoms such as fever and cough”, “All people infected with the virus develop symptoms”, “Drinking very hot drinks prevents contamination from the virus”, “The virus survives on inert surfaces such as doorknobs or bars in public transportation” and “Everybody should wear a mask to effectively protect themselves from the virus”. A score was calculated from 0 to 8, with higher scores corresponding to better detection of fake news. The categories were: bad detection of fake news (0–5) and good detection of fake news.6–8
The secondary exposure variable was HL measured through a 5-item scale scored from 0 to 15. Answers to each item were based on a 4-point Likert scale (from 0 “completely disagree” to 3 “completely agree”). Items were: “I compare health information from different sources”, “When I discover new health information I verify if it is true or not”, “I decide what health information is best for me”, “I can state if health information is adapted to my situation or not”, and “I enquiry health professionals on the quality of information I find”. Higher scores corresponded to better HL. Obtained categories were: bad HL (0–9) and good HL.10–15 The HL questionnaire was developed and used by the French Public Health Agency (Santé publique France).25
Other variables used for the description of the sample and for adjustment in the models included sociodemographic characteristics and vaccine-related items: sex (male, female); age (18–20 years vs 20 years), marital status (single, in a couple since at least three years without being married, married, divorced/widower); having children (no, yes); being a student (no, yes); studying or working in the health domain (no, yes); self-perceived health before the lockdown (poor, good); lifelong medical history including at least one disease among cardiovascular disease, high blood pressure, diabetes, chronic digestive disease, cancer, asthma or other respiratory problems, mental disorders or other illnesses (no/I do not know, yes); being up-to date with vaccination (no, yes, I do not know); and being regularly vaccinated against flu (no,yes).
Analysis
A descriptive analysis was performed, presenting all variables and measures in the form of numbers and percentages for qualitative variables and means and standard deviations (SD) for quantitative variables, stratified by the degree of acceptance of the vaccine against the SARS-CoV-2 (anti-vaccination, pro-vaccination, hesitant). Chi2 and ANOVA independence tests were performed in order to compare the three groups. A first multivariable multinomial regression model investigated the association between intention to get vaccinated against the SARS-CoV-2 and the capacity to detect Covid-19-related fake news as well as levels of HL, adjusted on the sociodemographic variables which were significantly different among the three groups. Interactions between each variable in the model were also tested. A second model, identical to the first, but with additional stratification between the ability to detect fake news and the level of HL was performed to study the association between the intention to get vaccinated against the SARS-CoV-2 and the capacity to detect Covid-19-related fake news according to HL levels. Statistical significance was defined with a p-value<0.05. Data were analyzed with SAS® version 9.4.
Results
Sample characteristics
A total of 2344 individuals completed the CONFINS questionnaire. We performed a complete-case analysis, thus excluding participants not meeting the inclusion criteria and with missing values in the variables under study. The final sample was composed of 1647 participants: 18.6% (306/1647) anti-vaccination, 10.9% (180/1647) hesitant and 70.5% (1161/1647) pro-vaccination (Figure 1).
Fig. 1.
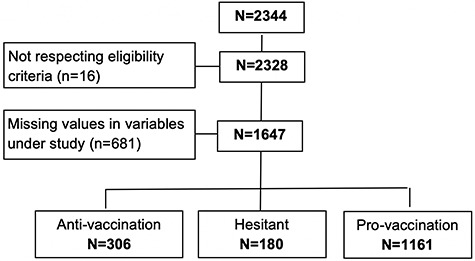
Study flow-chart.
Table 1 presents the sociodemographic characteristics of the study population, plus the variables HL and detection of fake news stratified by the three groups of vaccine acceptance. The total sample was composed of 78.5% (1293/1647) female participants. The mean age was 28.2 years (standard deviation ±11.5).
Table 1.
Description of the study population stratified by vaccination groups (n = 1647)
|
Anti-vaccination
(n = 306) |
Hesitant
(n = 180) |
Pro-vaccination
(n = 1161) |
p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Sex | <0.01 | ||||||
| Male | 45 | 14.7 | 31 | 17.2 | 278 | 23.9 | |
| Female | 261 | 85.3 | 149 | 82.8 | 883 | 76.1 | |
| Age (years) | 0.10 | ||||||
| 18–34 | 271 | 88.6 | 149 | 82.8 | 978 | 83.8 | |
| 35 or more | 35 | 11.4 | 31 | 17.2 | 188 | 16.2 | |
| Marital status | 0.13 | ||||||
| Single | 129 | 42.2 | 87 | 48.3 | 491 | 42.3 | |
| In a couple since at least three years without being married |
134 | 43.8 | 61 | 33.9 | 469 | 40.4 | |
| Married | 37 | 12.1 | 24 | 13.3 | 177 | 15.2 | |
| Divorced/Widower | 6 | 2.0 | 8 | 4.4 | 24 | 2.1 | |
| Having children | 0.17 | ||||||
| No | 274 | 89.5 | 156 | 86.7 | 991 | 85.4 | |
| Yes | 32 | 10.5 | 24 | 13.3 | 170 | 14.6 | |
| Student | 0.53 | ||||||
| No | 96 | 31.4 | 65 | 36.1 | 374 | 32.2 | |
| Yes | 210 | 68.6 | 115 | 63.9 | 787 | 67.8 | |
| Studying or working in the health domain | <0.01 | ||||||
| No | 228 | 74.5 | 113 | 62.8 | 649 | 55.9 | |
| Yes | 78 | 25.5 | 67 | 37.2 | 512 | 44.1 | |
| Self-perceived health before lockdown | 0.21 | ||||||
| Bad | 45 | 14.7 | 30 | 16.7 | 144 | 12.4 | |
| Good | 261 | 85.3 | 150 | 83.3 | 1017 | 87.6 | |
| Lifelong medical history | 0.06 | ||||||
| No or I do not know | 153 | 50.0 | 87 | 48.3 | 500 | 43.1 | |
| Yes | 153 | 50.0 | 93 | 51.7 | 661 | 56.9 | |
| Up-to date vaccination | <0.01 | ||||||
| No | 27 | 8.8 | 6 | 3.3 | 61 | 5.3 | |
| Yes | 239 | 78.1 | 162 | 90.0 | 1019 | 87.8 | |
| I do not know | 40 | 13.1 | 12 | 6.7 | 81 | 7.0 | |
| Being regularly vaccinated against flu | <0.01 | ||||||
| No | 276 | 90.2 | 137 | 76.1 | 787 | 67.8 | |
| Yes | 30 | 9.8 | 43 | 23.9 | 374 | 32.2 | |
| General health literacy scale – HL(mean (±SD)) | 9.9 | (±2.6) | 9.5 | (±3.2) | 10.3 | (±2.9) | <0.01 |
| Categories | <0.01 | ||||||
| Bad (0–9) | 143 | 46.7 | 82 | 45.6 | 404 | 34.8 | |
| Good10–15 | 163 | 53.3 | 98 | 54.4 | 757 | 65.2 | |
| Detection of fake news (mean (±SD)) | 6.3 | (±1.1) | 6.2 | (±1.2) | 6.6 | (±1.0) | <0.01 |
| Categories | <0.01 | ||||||
| Bad (0–5) | 67 | 21.9 | 40 | 22.2 | 143 | 12.3 | |
| Good6–8 | 239 | 78.1 | 140 | 77.8 | 1018 | 87.7 | |
Concerning the detection of fake news, the mean score for the total population was 6.5 (SD ±1.0) out of 8. Those reporting a bad score (0–5) were 15.2% (250/1647) vs 84.8% (1397/1647) reporting a good score.6–8 The total study population reported a mean of 10.2 (SD ±2.9) out of 15 for HL. Those reporting a bad HL score (0–9) were 38.2% (629/1647) vs. 61.8% (1018/1647) reporting a good HL score.10–15 We observed significant associations between intention to get vaccinated against the SARS-CoV-2 and sex (p < 0.01), studying or working in the health domain (p < 0.01), having their vaccination up-to-date (p < 0.01), being regularly vaccinated against flu (p < 0.01) and the two exposure variables detection of fake news (p < 0.01) and HL (p < 0.01).
We also assessed which were the most challenging fake news for participants. The item which rose more problems to participants was the one on the transmission of the virus through the air, with similar percentages between “true” and “false” answers, 43.3% and 36.9% respectively. Participants were more doubtful about the item on the development of the Covid-19 virus in a laboratory (29.1% answered “I do not know”). See Supplementary Table S1 in the Supplementary Material for more details.
Intention to get vaccinated and associations with detection of fake news and HL
Table 2 presents the results of the first multivariable multinomial regression model. The reference category was the “pro-vaccination” group. Based on their significance in the descriptive analysis (p < 0.05), we inserted in the model the following covariates: sex, being regularly vaccinated against flu, having up-to-date vaccination and studying or working in the health domain. We also inserted in the model the only interaction we found, i.e., between being regularly vaccinated against flu and studying or working in the health domain (p = 0.04). No interaction was found between detection of Covid-19-related fake news and HL (p = 0.55).
Table 2.
Effect of capacity to detect fake news and health literacy on intention to get vaccination against Covid-19, estimated with a multivariate multinomial regression model (N = 1647)
| Anti-vaccination vs Pro-vaccination | Hesitant vs Pro-vaccination | |||
|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | |
| Detection of fake news | ||||
| Bad (0–5) vs Good6–8 | 1.80 | [1.29;2.52] | 1.93 | [1.30;2.87] |
| Health Literacy Score | ||||
| Bad (0–9) vs Good10–15 | 1.25 | [0.96;1.63] | 1.44 | [1.04;2.00] |
| Being regularly vaccinated against flu (No vs Yes) | ||||
| Individuals studying or working in the health domain | 2.48 | [1.44;4.26] | 1.94 | [1.12;3.35] |
| Individuals studying or working in another domain | 4.50 | [2.28;8.86] | 0.92 | [0.55;1.54] |
Adjusted on sex, being regularly vaccinated against flu, having their vaccination up-to-date and studying or working in the health domain. OR: odd ratio; 95%CI: confidence interval at 95%.
The risk of being “anti-vaccination” or “hesitant”, rather than “pro-vaccination”, was higher among individuals reporting a bad detection of fake news, compared to individuals with a good detection of fake news, and the risk of being “hesitant” was more important than the risk of being “anti-vaccination”, respectively OR = 1.93 (95%CI = [1.30;2.87]) and OR = 1.80 (95%CI = [1.29;2.52]), adjusted on covariates. The risk of being “hesitant”, rather than “pro-vaccination” was higher among individuals having a bad HL score, compared to individuals with a good HL score (OR = 1.44; 95%CI = [1.04;2.00]), adjusted on covariates.
Among participants studying or working in the health domain, the risk of being “anti-vaccination” or “hesitant” was higher among those who were not regularly vaccinated against flu compared to those who were vaccinated, and the risk of being “anti-vaccination” was greater than that of being “hesitant”, respectively OR = 2.48 (95%CI = [1.44;4.26]) vs. OR = 1.94 (95%CI = [1.12;3.35]), adjusted on covariates. Among those studying or working in a field other than the health one, the odds of being “anti-vaccination” were 4.5 times higher among those who were not regularly vaccinated against flu compared with those who were vaccinated (OR = 4.5; 95%CI = [2.28;8.86]), adjusted on covariates.
The same model was performed with a supplementary forced-interaction between detection of fake news and HL in order to obtain stratified results according to HL (Table 3). Among individuals having a bad HL score, the risk of being “anti-vaccination” or “hesitant”, rather than “pro-vaccination”, was higher among those having a bad detection of fake news, compared to those with a good detection of fake news, and the risk of being “anti-vaccination” was higher than the risk of being “hesitant”, respectively OR = 2.18 (95%CI = [1.36;3.49]) and OR = 2.08 (95%CI = [1.17;3.71]), adjusted on covariates. Among individuals having a good HL score, the risk of being “hesitant”, rather than “pro-vaccination”, was higher among those reporting a bad detection of fake news, compared to those with a good detection of fake news (OR = 1.83; 95%CI = [1.05;3.18]), adjusted on covariates.
Table 3.
Effect of detection of fake news on intention to get vaccination against SARS-CoV-2, stratified on HL, estimated through a multivariate multinomial regression model (N = 1647)
| Anti-vaccination vs Pro-vaccination | Hesitant vs Pro-vaccination | |||
|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | |
| Detection of fake news (Bad vs good) | ||||
| Individuals having a bad HL | 2.18 | [1.36;3.49] | 2.08 | [1.17;3.71] |
| Individuals having a good HL | 1.50 | [0.93;2.42] | 1.83 | [1.05;3.18] |
Adjusted on sex, being regularly vaccinated against flu, having their vaccination up-to-date and studying or work in health domain with an interaction between being regularly vaccinated against flu and study or work in health domain and an interaction between detection of fake news and health literacy; OR: odd ratio; 95% CIs: confidence interval at 95%.
Discussion
Main findings of this study
The present study assessed the associations and their combinations between intention to get vaccinated against the SARS-CoV-2 and detection of fake news about Covid-19 as well as HL. We intended to verify whether the detection of fake news changed or not the intention to get vaccinated based on the levels of HL. We observed that there was no interaction between the ability of detecting fake news and HL, but that both these variables were associated with the acceptance of a vaccine against the SARS-CoV-2. HL did not have a moderating role, thus confuting our hypothesis. A possible explanation might be that our fake news scale was not too discriminating (i.e., questions were not too difficult) and that individuals with a low HL score could provide a good answer. Only near one participant out of six reported bad detection of fake news about the pandemic. However, the stratification of the results of the second model confirmed that bad HL and bad detection of fake news were both related to being hesitant or anti-vaccination.
What is already known on this topic
In a previous observational study conducted in Italy,16 among more than 2000 online articles related to Covid-19, articles containing fake news were shared more than 2 million times accounting for 78% of the total shares of all reviewed articles. This high percentage throws light on the fake news phenomenon and calls for an improvement of HL to better navigate information on the net. Previous research also reported that HL in general helps identification of fake news26: this is especially true in crisis contexts like that generated by Covid-19.18
A group of researchers from Germany developed a SARS-CoV-2-related HL measure and administered it among 1153 adult Internet users.27 A total of 15.2% of participants were found to have “inadequate HL”, 34.9% had “problematic HL”, and 49.9% had “sufficient HL” with reference to Covid-19. The item where participants scored the lowest was that on the capacity to “judge if information on SARS-CoV-2 and the SARS-CoV-2 epidemic in the media is reliable”.
Concerning fake news and vaccination, the association between misinformation and vaccine hesitancy is well documented.8 A study conducted in England noted a link between belief in Covid-19 conspiracies and an increase in vaccine hesitancy.28 On the other hand, previous research has also found that HL is associated with preferences for vaccination in general.29 Following the inoculation theory, preemptive refutation of misinformation weakens the misinformation, just as a medical vaccine is often comprised of weakened virus.30
What this study adds
This was one of the first studies assessing through a large cohort the association between intention to get vaccinated, misinformation and HL in relation to Covid-19. Our findings allow for a better understanding of the relation between our variables of interest providing a solid ground for policymakers and health professionals to design and implement programs to tackle Covid-19-related ‘infodemic’.
We found that intention to get vaccinated was associated with agreement with fake news. Even if this result has been already assessed in studies describing the relation between spread of misinformation and decrease in immunization,8,31 our study was specifically addressing Covid-19, which has not been explored before. The fight against SARS-CoV-2-related fake news is pivotal, especially considering that even an effective vaccine against Covid-19 runs the risk of falling victim of fake news by increasing vaccine hesitancy. Correcting misinformation should be considered as a vitally important science and health policy activity.
Our study also found a significant association between vaccine hesitancy and low levels of HL. Thus, evidence is provided for the need to propose a series of strategies to help the general public find the correct information and thereby better engage them to adhere to correct guidelines.5
Vaccine communication strategies should support the identification of fake news and promote HL in target audiences: consistent communication by institutions is crucial to building public confidence in vaccine programs.
Limitations
This study was large and diverse but not representative of the national population. As any online survey, participants who have a special interest in the topic might have been recruited (i.e. self-selection bias). Caution is needed in generalising from the prevalence findings. Another limitation is the labelling of the misinformation items as these particular beliefs are likely contextual and subjective. However, we proposed the most diffused fake news in the French context at the moment of the survey. Finally, we excluded some individuals because of missing values in the variables of interest. The final sample was not extensively affected counting more than 1600 participants.
In conclusion, findings suggest that the spread of fake news can influence vaccine uptake, but also that better HL can help evaluate information about Covid-19. For this, interventions are needed at the education and political levels to contain misinformation and promoteHL.
Role of the funding source
The i-Share and CONFINS team are currently supported by an unrestricted grant of the Nouvelle-Aquitaine Regional Council (Conseil Régional Nouvelle-Aquitaine) (grant N° 4370420) and by the Bordeaux ‘Initiatives d’excellence’ (IdEx) program of the University of Bordeaux (ANR-10-IDEX-03-02). The team has also received grants from Public Health France (Santé Publique France, contract N° 19DPPP023–0) and the Nouvelle-Aquitaine Regional Health Agency (Agence Régionale de Santé Nouvelle-Aquitaine). The funding bodies were neither involved in the study design, or in the collection, analysis, or interpretation of thedata.
Data availability statement
All data generated or analysed during this study are included in this published article. The full dataset is available upon request from the CONFINS cohortteam.
Ethical standards
The study follows the principles of the Declaration of Helsinki and the collection, storage and analysis of the data comply with the General Data Protection Regulation (EU GDPR).
The study was approved by the French Committee for the Protection of Individuals (Comité de Protection des Personnes—CPP IDF X, nr. 46–2020) and by the National Commission on Informatics and Liberty (Commission Nationale de l’Informatique et des Libertés -CNIL, nr. MLD/MFI/AR205600).
Supplementary Material
Acknowledgements
We wish to thank all members of the CONFINS group including the i-Share, Kappa Santé and Kap Code team members: Stéphane Schück, Nathalie Texier and Christophe Tzourio conceived and designed the study cohort; Edwige Pereira, Garance Perret, Aude Pouymayou and Mathilde Pouriel analysed the data; Julie Arsandaux, Shérazade Kinouani, Mélissa Macalli and Ilaria Montagni wrote and revised manuscripts; Raphaël Germain and Clothilde Pollet were in charge of the regulatory affairs; Vanessa Marie-Joseph, Adel Mebarki, Elena Milesi and Marie Mougin were in charge of the study communication. The authors are also grateful to all the participants who volunteered to take part in the study.
I Montagni, Researcher and Lecturer
K Ouazzani-Touhami, Public Health Medical Doctor
A Mebarki, General Co-Director
N Texier, Director
S Schuck, Chief Executive Officer
C Tzourio, Professor and Head
Contributor Information
I Montagni, Univ.Bordeaux, Inserm, Bordeaux Population Health Research Center, U1219, F-33000, Bordeaux, France.
K Ouazzani-Touhami, Univ.Bordeaux, Inserm, Bordeaux Population Health Research Center, U1219, F-33000, Bordeaux, France; Polyclinique Inkermann, groupe Elsan, F-79000 Niort, France.
A Mebarki, Kap Code, F-75010 Paris, France.
N Texier, Kap Code, F-75010 Paris, France; Kappa Santé, F-75002 Paris, France.
S Schück, Kap Code, F-75010 Paris, France; Kappa Santé, F-75002 Paris, France.
C Tzourio, Univ.Bordeaux, Inserm, Bordeaux Population Health Research Center, U1219, F-33000, Bordeaux, France.
References
- 1. Ahmed W, Vidal-Alaball J, Downing J, López Seguí F. COVID-19 and the 5G conspiracy theory: social network analysis of twitter data. J Med Internet Res 2020;22(5):e19458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ratzan SC, Sommariva S, Rauh L. Enhancing global health communication during a crisis: lessons from the COVID-19 pandemic. Public Heal Res Pract 2020;30(2). [DOI] [PubMed] [Google Scholar]
- 3. Freckelton QCI. COVID-19: fear, quackery, false representations and the law. Int J Law Psychiatry 2020;72:101611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. AP NEWS . False belief poison cures virus kills over 700 in Iran [Internet]. 2020. [cited 2020 Sep 16]. Available from: https://apnews.com/fece5d0e017849911aa86c0c07799e6b.
- 5. Tagliabue F, Galassi L, Mariani P. The “pandemic” of disinformation in COVID-19. SN Compr Clin Med 2020;2(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hassenteufel P. Handling the COVID-19 crisis in France: paradoxes of a centralized state-led health system. Eur Policy Anal 2020;00:1–10. [Google Scholar]
- 7. Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carrieri V, Madio L, Principe F. Vaccine hesitancy and (fake) news: quasi-experimental evidence from Italy. Heal Econ (United Kingdom) 2019;28(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Donzelli G, Palomba G, Federigi I et al. Misinformation on vaccination: a quantitative analysis of YouTube videos. Hum Vaccin Immunother 2018;14(7):1654–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Broadbent JJ. Vaccine hesitancy: misinformation on social media. The BMJ 2019;366. [DOI] [PubMed] [Google Scholar]
- 11. MacDonald NE, SAGE Working Group on Vaccine Hesitancy., SAGE Working Group on Vaccine Hesitancy et al. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33(34):4161–4. [DOI] [PubMed] [Google Scholar]
- 12. Lazarus JV, Ratzan SC, Palayew A et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sørensen K, Van Den Broucke S, Fullam J et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Altin SV, Finke I, Kautz-Freimuth S, Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Song S, Zhao YC, Song X, Zhu Q. The Role of Health Literacy on Credibility Judgment of Online Health Misinformation. In: 2019 IEEE International Conference on Healthcare Informatics, ICHI 2019. 2019.
- 16. Moscadelli A, Albora G, Biamonte MA et al. Fake news and covid-19 in Italy: results of a quantitative observational study. Int J Environ Res Public Health 2020;17(16):5850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van der Linden S, Roozenbeek J, Compton J. Inoculating against fake news about COVID-19. Front Psychol 2020;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Spring H. Health literacy and COVID-19. Health Info Libr J 2020;37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paakkari L, Okan O. COVID-19: health literacy is an underestimated problem. Lancet Public Health 2020;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dror AA, Eisenbach N, Taiber S et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Res Square, Prepr 2020;1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Detoc M, Bruel S, Frappe P et al. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020;38(45). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lastrucci V, Lorini C, Caini S et al. Health literacy as a mediator of the relationship between socioeconomic status and health: a cross-sectional study in a population-based sample in Florence. PLoS One 2019;14(12):e0227007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim YS, Rhee TG, Lee HY et al. Mental health literacy as a mediator in use of mental health services among older Korean adults. Int Psychogeriatr 2017;29(2). [DOI] [PubMed] [Google Scholar]
- 24. Yamashita T, Keene JR, Moonie SA et al. Literacy activity and health among older adults in the USA. Educ Gerontol 2018;44(10):627–38. [Google Scholar]
- 25. Santé Publique France . Covid-19 : Une enquête pour suivre l’évolution des comportements et de la santé mentale pendant l’épidémie [internet]. 2020. [cited 2021 Jan 7]. Available from: https://www.santepubliquefrance.fr/etudes-et-enquetes/covid-19-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie#block-242829.
- 26. Jones-Jang SM, Mortensen T, Liu J. Does media literacy help identification of fake news? Information literacy helps, but other literacies Don’t. Am Behav Sci 2019. [Google Scholar]
- 27. Okan O, Bollweg TM, Berens EM et al. Coronavirus-related health literacy: a cross-sectional study in adults during the COVID-19 infodemic in Germany. Int J Environ Res Public Health 2020;17(15). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Freeman D, Waite F, Rosebrock L et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol Med 2020;1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Veldwijk J, van der Heide I, Rademakers J et al. Preferences for vaccination. Med Decis Making 2015;35(8):948–58. [DOI] [PubMed] [Google Scholar]
- 30. McGuire WJ. Resistance to persuasion conferred by active and passive prior refutation of the same and alternative counterarguments. J Abnorm Soc Psychol 1961;63(2):326–32. [Google Scholar]
- 31. Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines 2014;14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article. The full dataset is available upon request from the CONFINS cohortteam.


