Abstract
Covid-19 Nationwide lockdown for social containment was implemented on the 23rd of March 2020. The objective of this study was to look at the impact of lockdown on STEMI (<24hrs window period). This study was done in 2 phases, 43 days before (phase1) and 43 days during lockdown (phase 2). During the lockdown, there was a 31% decrease in hospital admission rates, 11.5% and 9.38% proportional increase in diabetics and hypertensive patients presenting with STEMI. The public must be educated about the existing important health problems in the community along with the pandemic warnings.
Keywords: Covid-19, STEMI, Social containment, Lockdown-government policy, Pandemic impact
1. Introduction
The first cluster of novel corona virus-(SARS-related CoV-2) was identified in Wuhan, a city in central China towards the end of 2019.1 The first confirmed case of COVID-19 in India was reported from Kerala, a south Indian state on 30th January 2020.2 Since then there has been a rapid escalation of COVID-19 cases in the country due to its high secondary attack rate.3 Understanding the epidemic and witnessing the developed countries being crumbled by the pandemic, the Indian government imposed the nationwide lockdown (social containment) from the 23rd of March to buy time for preparedness of health infrastructure and containing the spread in the community.
2. Aim
The objective of the study is to assess the collateral impact of Lockdown on admission rates and in-hospital mortality rates of acute coronary syndrome –ST-elevation Myocardial Infarction (STEMI).
3. Material and methods
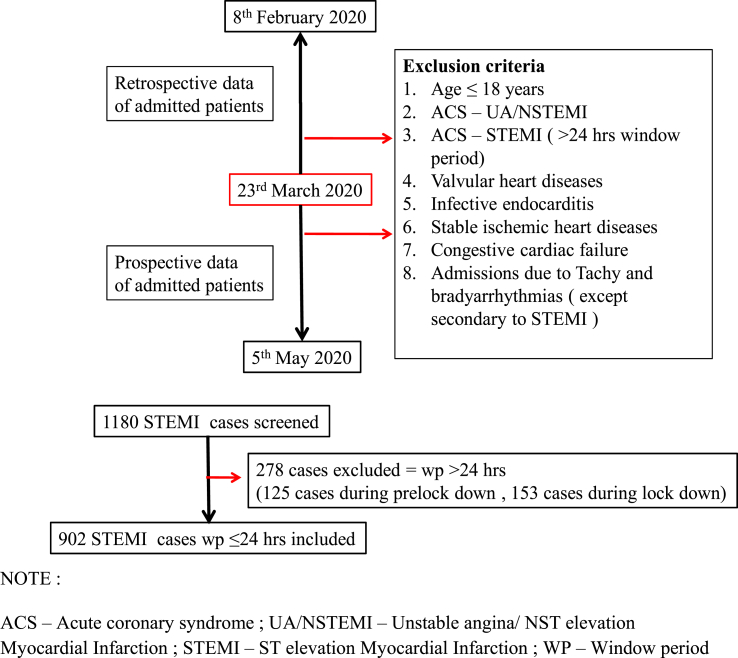
The study was done after Institutional ethics committee approval (Ref No – SJICSR/EC/2020/017). Patients consecutively admitted to the hospital with ACS-STEMI (Window Period < 24 h) were included. The patients were treated with pharmaco invasive therapy which is comparable to primary PCI in outcomes. Patients were initially thrombolysed (with streptokinase predominantly than fibrin specific agents) and the successfully thrombolysed patients were taken for an angiogram on the following day, or the rescue PCI was done as and when needed.4 For Phase 1 of the study, the retrospective data were collected from the Medical record section. During the second phase data was prospectively collected (Fig. 1).
Fig. 1.
Skeleton diagram of working protocol of the study. NOTE: ACS – Acute coronary syndrome; UA/NSTEMI – Unstable angina/NST elevation Myocardial Infarction; STEMI – ST elevation Myocardial Infarction; WP – Window period.
4. Statistical analysis
The analysis was done in SPSS (Statistical Package for the Social Sciences) version 26 software. The Metric variables between 2 phases were analyzed by using an independent T-test or Mann-Whitney test wherever applicable. The odds ratio of risk factors for death was analyzed by Binominal multivariate analysis.
5. Results
It was observed that compared to Prelockdown phase hospital admission rates during lock down phase dropped by 31.04% (Table 1). Anterior wall STEMI was most common in both the phases {335(56.7%) vs. 185(59.5%) (p = 0.418)}.
Table 1.
Demographics, Lipid profile, Risk factors for CAD, Outcomes and Killips presentation of patients.
| PRELOCKDOWN MEAN ± SD/N (%) | LOCKDOWN MEAN ± SD/N (%) | P VALUE | |
|---|---|---|---|
| Total | 591(65.41) | 311(34.58) | |
| Males | 450(76.1) | 241(77.5) | 0.649 |
| AGE (years) | 56.49 ± 12.82 | 56.85 ± 12.325 | 0.683 |
| WP (hours) | 7.66 ± 6.889 | 7.611 ± 6.002 | 0.092 |
| LIPID PROFILE a | |||
|
178.5 ± 43.29 | 173.99 ± 43.295 | 0.218 |
|
35.56 ± 9.39 | 34.0238 ± 8.406 | 0.042 |
|
126.52 ± 38.864 | 124.47 ± 39.11 | 0.526 |
|
193.49 ± 147.78 | 180.54 ± 111.94 | 0.828 |
|
39.72 ± 30.821 | 36.22 ± 22.28 | 0.738 |
| BLOOD SUGAR(mg/dl) b | 192.51 ± 121.17 | 199.98 ± 126.57 | 0.465 |
| EF (%) c | 42.98 ± 11.07 | 43.55 ± 8.76 | 0.481 |
| RISK FACTORS FOR CAD | |||
|
50 (8.5) | 30 (9.6) | 0.551 |
|
190 (32.1) | 111(35.7) | 0.284 |
|
13 (2.2) | 5(1.6) | 0.541 |
|
240(40.6) | 162(52.1) | 0.001 |
|
233 (39.4) | 153(49.2) | 0.005 |
| DEATH | 91(15.4) | 62(19.9) | 0.084 |
| KILLIPS CLASS d | |||
| I | 412(71.3) | 211(68.1) | 0.200 |
| II | 45(7.8) | 34(11) | 0.109 |
| III | 41(7.1) | 29(9.4) | 0.209 |
| IV | 80(13.8) | 36(11.6) | 0.553 |
Note: WP-window period; HDL - High Density Cholesterol; LDL - Low Density Cholesterol; VLDL - Very low density cholesterol; EF - Ejection fraction; CAD - Coronary artery disease; IHD – Ischemic heart disease; T2DM – Type 2 Diabetes Mellitus.
Values are based on 427 patients during Prelockdown and 218 patients during lockdown.
Values are based on 541 patients during Prelockdown and 286 patients during lockdown.
Values are based on 462 patients during Prelockdown and 244 patients during lockdown.
Values are based on 578 patients during Prelockdown and 310 patients during lockdown.
Among the risk factors, T2DM and HTN were more prevalent during the lockdown phase. Other risk factors like prior IHD, smoking, and tobacco chewing didn’t show any difference. The case fatality rate didn’t differ between the two groups.
Higher blood sugars, development of renal dysfunction, and heart blocks predicted higher mortality in both the phases whereas better Ejection fraction before thrombolysis was protective (Table 2).
Table 2.
Predictors of mortality.
| PREDICTORS OF MORTALITY | OR | 95% CI | P VALUE |
|---|---|---|---|
| BLOOD SUGAR (mg/dl) | 1.005 | 1.002–1.009 | 0.002 |
| EF (%) | 0.871 | 0.822–0.924 | <0.001 |
| RENAL DYSFUNCTION | 3.755 | 1.30–10.82 | 0.014 |
| AV BLOCK | 20.67 | 3.89–109.69 | <0.001 |
Note: AV block – Atrioventricular block.
6. Discussion
The study centre witnessed a significant drop in admission rates from 14 to 8 per day due to lock down, as witnessed in other countries.5 The centre is one of the largest cardiac set up in South Asia which caters cardiac admission to three southern states of India. Our country is still dependent on public transport for health care access. The cardiac specialty is available at only tertiary care hospitals at districts or state headquarters, the ban on inter-district and interstate travel due to lockdown may have decreased access to the transport facilities causing reduced hospital admissions. The fear of hospital-acquired corona infections could be the other possible explanation.6 Also, the MI with atypical presentations that otherwise would have been picked up might not have been diagnosed.
There was increased proportion of T2DM {231(40.81%) vs. 169(50.59%), p = 0.004} and hypertension {223(39.39%) vs. 166(49.70%), p = 0.003} during the lockdown period. The prior sensitization of DM and HTN groups about their risk of CAD during their regular hospital visits and to seek medical attention with the onset of symptoms could be the possible reason. This stresses the need for health education of the prevailing diseases among the general public along with the pandemic warnings.
Apart from the admission rates, there was no significant difference in case fatality rates during these two periods 91(15.4%) vs. 62(19.9%), p = 0.084. Our death rate is significantly higher than in Kerala ACS and CREATE registry possibly due to tertiary centre bias, exclusion of evolved STEMI, late presentation, fibrinolysis being the preferred treatment due to multiple socioeconomic factors, and Covid-19 related logistics for interventional management.7
7. Study limitations
In-hospital mortality may not represent true long-term outcomes that were not assessed in our study. Details on guideline directed medical therapy, duration of hospital stay and risk factors for mortality such as arrhythmias haven’t been included in the study. Our study may not reflect the true population incidence of MI due to transport issues and referral bias. The true decrease in MI can be deciphered only from birth and death registries.
8. Conclusion
Nationwide lockdown provided time for the preparedness of the medical system for the impact of COVID 19 by curbing the rate of rising in the number of cases. However, it did have its collateral impacts on all other areas including the difficulty in access of patients to health care due to transportation issues. This study emphasizes that people without risk factors may have been hesitant to visit health care. Along with the COVID warnings for the general public, there must be health education to contact health care facilities with the onset of symptoms and the existing diseases cannot be ignored because of the pandemic.
Declaration of competing interest
All the authors have no conflicts of interests and financial disclosure.
References
- 1.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Mar 26;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MoHFW | Home [Internet]. [cited 2020 Jul 5]. Available from: https://www.mohfw.gov.in/.
- 3.Bi Q., Wu Y., Mei S. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis [Internet] 2020 Apr 27 doi: 10.1016/S1473-3099(20)30287-5. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30287-5/abstract [cited 2020 Jul 5];0(0). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sim D.S., Jeong M.H., Ahn Y. Pharmacoinvasive strategy versus primary percutaneous coronary intervention in patients with ST-segment-elevation myocardial infarction: a propensity score-matched analysis. Circ Cardiovasc Interv. 2016 Sep;9(9) doi: 10.1161/CIRCINTERVENTIONS.115.003508. [DOI] [PubMed] [Google Scholar]
- 5.De Rosa S., Spaccarotella C., Basso C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020 Jun 7;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanner R., MacDaragh Ryan P., Caplice N.M. COVID-19—where have all the STEMIs gone? Can J Cardiol. 2020 May doi: 10.1016/j.cjca.2020.04.032. S0828282X20304293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013 Jan;34(2):121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]