Abstract
A multisystem inflammatory syndrome mimicking Kawasaki disease has been increasingly reported, mainly in children, in the context of coronavirus disease-2019 (COVID-19). We report on the first case of coronary aneurysm resolution after treatment with steroids and intravenous immunoglobulins in an adult patient with multisystem inflammatory syndrome temporally associated with COVID-19. (Level of Difficulty: Beginner.)
Key Words: coronary aneurysms, COVID-19, intravenous immunoglobulin, MIS COVID-19, SARS-COV-2
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; CRP, C-reactive protein; CT, computed tomography; IVIG, intravenous immunoglobulins; MIS, multisystem inflammatory syndrome; MIS-A, multisystem inflammatory syndrome in adults; PIMS-TS, pediatric inflammatory multisystem syndrome temporally associated with severe acute respiratory syndrome coronavirus 2; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; TTE, transthoracic echocardiogram
Central Illustration

History of Presentation
A 33-year-old man of sub-Saharan African origin was admitted to the intensive care unit for severe hypotension in the context of persistent fever, dyspnea, chest pain, and diarrhea. At referral to the intensive care unit, he presented with a blood pressure of 47/29 mm Hg, tachycardia (116 beats/min), the need for oxygen therapy (2 l/min by nasal cannula to maintain an oxygen saturation >94%), and hepatojugular reflux consistent with cardiogenic shock. Moreover, physical examination revealed bilateral conjunctivitis and cheilitis.
Learning Objectives
-
•
To identify coronary aneurysms in case of unexplained severe heart failure in the context of acute or recent COVID-19 infection.
-
•
To consider prompt initiation of steroids and IVIG if such complications are seen.
Past Medical History
The patient had a medical history of hypertension. Six weeks earlier, he had presented with a fever episode lasting for 5 days, along with myalgia, dysgeusia, and anosmia, which retrospectively was highly suggestive of coronavirus disease-2019 (COVID-19). However, as his condition was not worrying, and in line with the recommendations of the French health authorities at the time, he had not been tested for severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection.
Differential Diagnosis
In the context of cardiac failure associated with fever and hypotension, septic shock was first considered, and broad-spectrum antibiotics were initiated.
Investigations
The patient’s laboratory results included leukocytosis (21 109/l), normocytic anemia (10.7 g/dl), elevated liver enzyme levels (2 times the upper limit of normal), elevated creatine kinase levels (941 IU/l [normal <170 IU/l]), and acute kidney injury (creatinine level 495 μmol/l). C-reactive protein (CRP), brain natriuretic peptide, D-dimer, and troponin levels were 150 mg/l (normal <5.0 mg/l), 1,061 ng/l (normal <100 ng/l), 1,900 mg/l (normal <500 mg/l), and 13,265 pg/ml (normal <40 pg/ml), respectively. An electrocardiogram showed sinus tachycardia with no ST-segment abnormalities. A transthoracic echocardiogram (TTE) showed global hypokinesis with a dilated inferior vena cava and reduced ejection fraction (i.e., 20%) without pericardial effusion, which, in the context of elevated troponin levels, was suggestive of acute myocarditis. Infectious work-up was negative except for the detection of high titers of SARS-CoV-2 immunoglobulin G, suggestive of previous COVID-19 infection; results of repeated tests by polymerase chain reaction (n = 3) were negative. Moreover, a comprehensive etiological work-up for myocarditis, including the search for infectious and autoimmune diseases, was unremarkable. A coronary computed tomography (CT) scan performed 14 days after admission showed multiple coronary aneurysms involving right, interventricular, and left circumflex arteries, with a maximum diameter of 6 mm (Figures 1A, 1C, 2A, and 2D).
Figure 1.
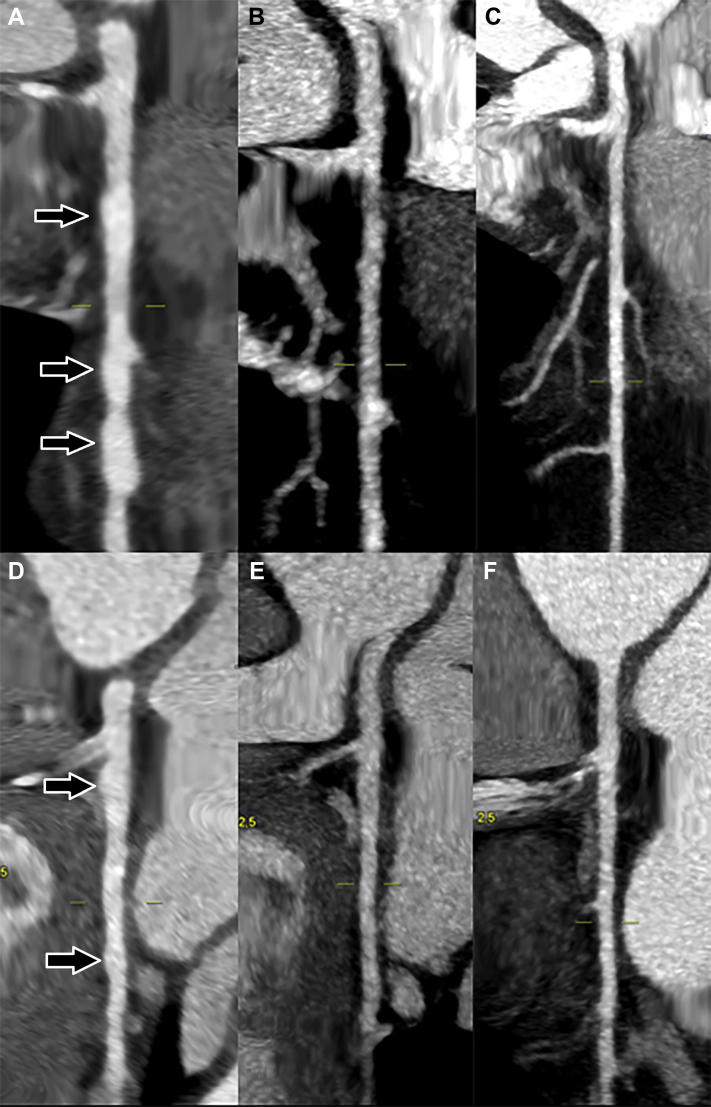
Multiple Coronary Aneurysms on Cardiac Computed Tomography Scans
3-Dimensional reconstruction of cardiac computed tomography scan showing multiple coronary aneurysms (black arrows) involving right, left anterior descending (LAD), and left circumflex arteries (A and C) and subsequent recovery after 5 months (B and D).
Figure 2.
Cardiac Computed Tomography Scans at 3 Different Time Points Showing Regression of the Aneurysms
Coronary computed tomography scan reconstruction at 3 different time points. Left anterior descending artery with multiple aneurysms (arrows) during the acute phase (A), with partial regression after 2 months (B) and total regression after 5 months (C). Circumflex artery with multiple aneurysms (arrows) during the acute phase (D), with partial regression after 2 months (E) and total regression after 5 months (F).
Management
The patient initially received hemodynamic support (norepinephrine and dobutamine infusion) for 5 days, which enabled dramatic improvement in both cardiac and renal functions. He subsequently received intravenous immunoglobulins (IVIG) (1 g/kg) and prednisone (1 mg/kg) for 10 days and aspirin (75 mg). This treatment allowed resolution of all symptoms by day 10 while CRP levels dropped to 10 mg/l. Control TTE showed normal left ventricular function, and a cardiac magnetic resonance imaging performed 7 days after admission was unremarkable. The patient was discharged on day 12.
Discussion
To our knowledge, this report is the first case of resolution of multiple coronary aneurysms after treatment with steroids and IVIG in an adult patient with multisystem inflammatory syndrome (MIS) temporally associated with COVID-19 and mimicking Kawasaki disease. In the context of the worldwide spread of a previously unknown infectious disease, physicians should search for coronary aneurysms in cases of unexplained severe heart failure in the setting of acute or recent COVID-19 infection. When such aneurysms are evidenced, this patient’s history along with recently published pediatric data advocated for prompt initiation of both IVIG and/or steroids.
Pediatricians have reported the temporal association of an inflammatory condition mimicking Kawasaki disease (so-called pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 [PIMS-TS], also known as Kawa-COVID-19]) occurring shortly (21 to 42 days) after onset of COVID-19 (1, 2, 3). Most of the latter patients fulfill the American Heart Association diagnostic criteria for complete Kawasaki disease, and they often (38% to 73%) present with a cardiac involvement (i.e., myocarditis, coronary dilatation), which seems even more frequent than in Kawasaki disease (1). In previous studies, early coronary dilations were reported in up to 15% to 20% of patients with PIMS-TS (1,2), yet none of the latter showed persistent aneurysms after 10 days of remission. In those study, most of the patients received IVIG (either a single or multiple infusions), steroids, or both. Conversely, a 15-year-old girl presented with symptoms consistent with PIMS-TS and subsequently developed persistent multiple coronary aneurysms despite one 120-g dose of IVIG, oral aspirin, and steroids (4). Interestingly, due to acute kidney injury, treatment with IVIG was delayed in our patient, who exhibited persistent aneurysms 2 months after clinical improvement, the latter disappearing only at a later stage.
Reports of MIS in adults (MIS-A) in the context of COVID-19 are scarce (5,6). A recent review of 27 patients managed in the United Kingdom and the United States depicted a clinical presentation very similar to that presented by our patient (5). Indeed, 56% of the patients were African American, and 81% of the patients had gastrointestinal symptoms. Among the detailed case reports, all of the 16 patients had cardiac involvement, including electrocardiogram abnormalities such as arrhythmias, elevated troponin levels, or echocardiographic evidence of left or right ventricular dysfunction. However, no case of coronary aneurysms was reported in either this series or in another French study of 11 patients with COVID-19, acute myocarditis, and MIS-A (7). It should be noted that in adult patients, TTE and magnetic resonance imaging may have a lower sensitivity to highlight coronary aneurysms and that a screening coronary CT scan should be performed in this setting.
Although treatment with IVIG is effective in the acute phase of Kawasaki disease, its effectiveness in preventing the development of aneurysms continues to be debated (8). A recent report from the International Kawasaki Disease Registry states that IVIG is the most widely used treatment in the context of PIMS-TS in combination with steroids in worrying situations (9). Due to the severity of the clinical picture and the lack of evidenced-based data regarding the management of this condition, both treatments were used simultaneously in our patient, with a good clinical outcome. Further studies are needed, however, to better define the optimal therapeutic regimen in this setting.
Follow-Up
Two months later, while the patient felt fully recovered and his CRP level was <1 mg/L, a second coronary CT scan showed a partial regression of coronary aneurysms (Figures 2B and 2E). A TTE was repeated and confirmed the normalization of left ventricular function. Last, a third coronary CT scan performed 5 months after admission showed complete disappearance of all aneurysms (Figures 1B, 1D, 2C, and 2F).
Conclusions
MIS-A and coronary aneurysms are potential life-threatening complications that should be included in the spectrum of severe COVID-19, even in adult patients. Treatment with IVIG and steroids may be useful in this setting to prevent the advent of aneurysms and potential long-term morbidity.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Pouletty M., Borocco C., Ouldali N. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. 2020;79:999–1006. doi: 10.1136/annrheumdis-2020-217960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belhadjer Z., Méot M., Bajolle F. Acute heart failure in multisystem inflammatory syndrome in children in the context of global SARS-CoV-2 pandemic. Circulation. 2020;142:429–436. doi: 10.1161/CIRCULATIONAHA.120.048360. [DOI] [PubMed] [Google Scholar]
- 3.Dufort E.M., Koumans E.H., Chow E.J. Multisystem inflammatory syndrome in children in New York state. N Engl J Med. 2020;383:347–358. doi: 10.1056/NEJMoa2021756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson C., Ishimine P., Hayden S.R., Correia M., Wardi G. Multisystem inflammatory syndrome in children (MIS-C) in an adolescent that developed coronary aneurysms: a case report and review of the literature. J Emerg Med. 2020;59:699–704. doi: 10.1016/j.jemermed.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris S.B., Schwartz N.G., Patel P. Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 infection—United Kingdom and United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1450–1456. doi: 10.15585/mmwr.mm6940e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chau V.Q., Giustino G., Mahmood K. Cardiogenic shock and hyperinflammatory syndrome in young males with COVID-19. Circ Heart Fail. 2020;13 doi: 10.1161/CIRCHEARTFAILURE.120.007485. [DOI] [PubMed] [Google Scholar]
- 7.Hékimian G., Kerneis M., Zeitouni M. COVID-19 acute myocarditis and multisystem inflammatory syndrome in adult intensive and cardiac care units. Chest. 2021;159:657–662. doi: 10.1016/j.chest.2020.08.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin M.T., Sun L.C., Wu E.T., Wang J.K., Lue H.C., Wu M.H. Acute and late coronary outcomes in 1073 patients with Kawasaki disease with and without intravenous γ-immunoglobulin therapy. Arch Dis Child. 2015;100:542–547. doi: 10.1136/archdischild-2014-306427. [DOI] [PubMed] [Google Scholar]
- 9.Elias M.D., McCrindle B.W., Larios G. Management of multisystem inflammatory syndrome in children associated with COVID-19: a survey from the International Kawasaki Disease Registry. CJC Open. 2020;2:632–640. doi: 10.1016/j.cjco.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]