Abstract
Lichen planopilaris is a rare inflammatory condition that is also known as follicular lichen planus. Although the condition commonly affects the scalp, it sometimes involves the other regions of the body with a variety of clinical presentations. The involvement beyond the scalp is considered to be a generalized nature of disease process. In this report, we present a case of generalized follicular lichen planus in a 34-year-old Thai female presenting with comedone-like lesions on the trunk and extremities as well as scarring alopecia on the scalp. Dermoscopic features were also discussed.
Keywords: Alopecia, Body hair, Dermoscopy, Follicular lichen planus, Hair loss, Lichenoid folliculitis
Introduction
Lichen planopilaris (LPP), initially described by Pringle in 1895 [1], is a follicular variant of lichen planus (also known as follicular lichen planus). LPP is a relatively rare inflammatory disease in which hair follicles are affected [2]. Treatment modalities reported include corticosteroids (topical, intralesional, and systemic) and systemic medications such as hydroxychloroquine, methotrexate, pioglitazone, tetracyclines, mycophenolate mofetil, and cyclosporine [3]. Although it usually presents as patchy alopecia mostly on the scalp leading to cicatricial alopecia [3], the disease affecting other body regions beyond the scalp has been reported [2, 4]. To date, data of extrascalp involvement regarding clinical, histopathological, and dermoscopic findings are relatively sparse [2, 5]. Herein, we report a case of follicular lichen planus presented with comedone-like papules on the trunk and extremities in association with scalp LPP and related dermoscopic features.
Case Report
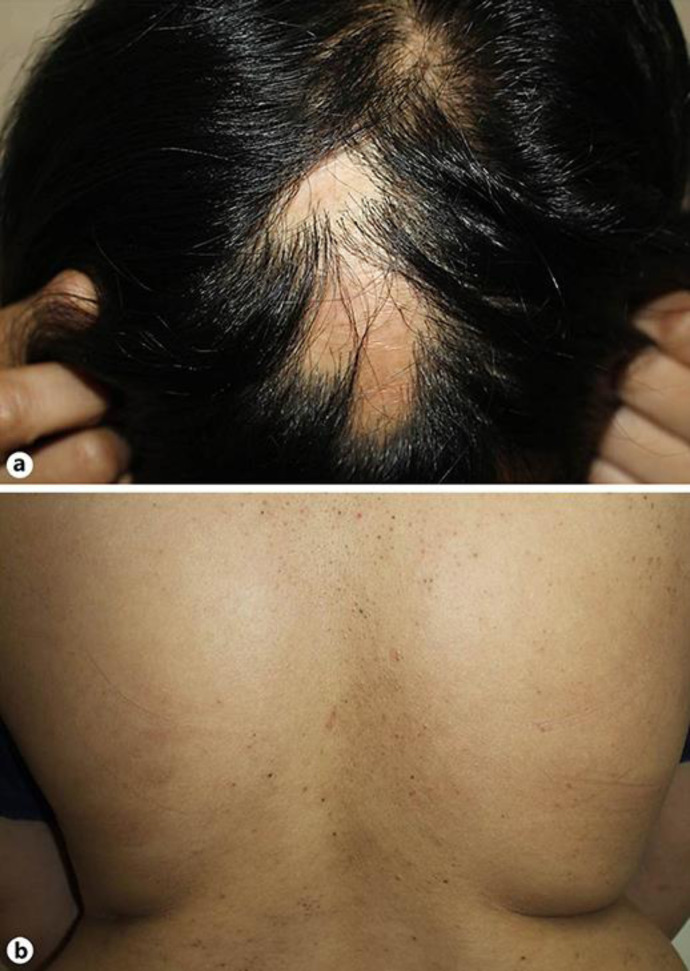
A 34-year-old healthy woman presented to our clinic with asymptomatic skin-colored to brownish tiny papules on the trunk and extremities of 1-month duration. Six months prior to this consultation, she presented with multiple scarring alopecic patches and had been biopsy-confirmed as having scalp LPP on the frontal and midscalp areas. She has been receiving systemic treatment with hydroxychloroquine. Eyebrows, axillary, and pubic hairs were not affected. Dermatologic examination demonstrated multiple discrete brownish comedone-like tiny follicular papules on the face, neck, trunk, and extremities without nail or mucosal involvement (Fig. 1b). No nail or mucosal involvement had been found. Scalp examination showed several discrete scarring alopecic patches on the frontal and midscalp regions (Fig. 1a). The eyebrows, axillary, and pubic hair showed normal appearance.
Fig. 1.
Clinical presentation. a Several scarring alopecic patches on the frontal and midscalp regions. b Multiple discrete brownish comedone-like tiny follicular papules on the trunk.
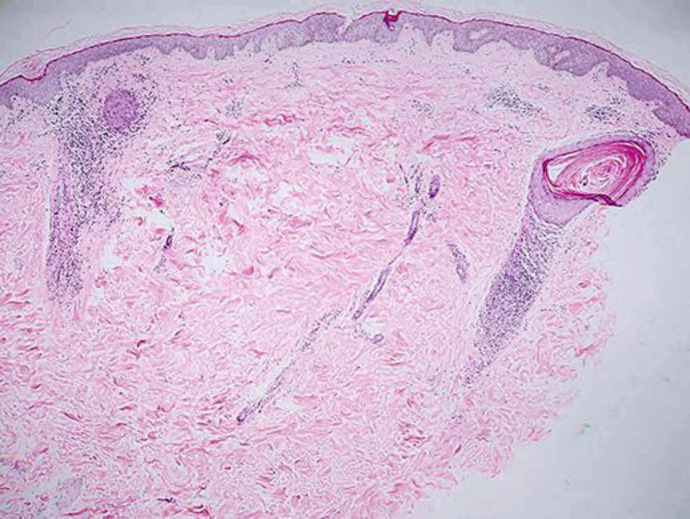
Dermoscopic findings of the follicular papules on the trunk showed perifollicular scaling and gray-brown discoloration of follicular openings (Fig. 2). A skin biopsy was performed and confirmed the diagnosis of follicular lichen planus by revealing perifollicular infiltrate of lymphocytes, melanophages with follicular interface, and dilated follicles (Fig. 3). Based on clinical features, dermoscopic findings, and compatible histopathological findings, follicular lichen planus was diagnosed. Additional laboratory panel including hepatitis B and C profile together with thyroid function were unremarkable.
Fig. 2.
Dermoscopic findings of follicular papules on the trunk show perifollicular scaling and gray-brown discoloration of follicular openings (DL3, 3Gen Inc., CA, magnification ×20).
Fig. 3.
Histopathological findings show perifollicular infiltrate of lymphocytes, melanophages with follicular interface, and dilated follicles (hematoxylin-eosin, original magnification ×40).
Regarding treatment, hydroxychloroquine 200 mg daily has been maintained. Desoximetasone 0.25% lotion was given to apply on the lesions. On the follow-up visit at 2 months, the follicular papules slightly increased in number, and isotretinoin 10 mg once daily was thus added. The patient showed minimal improvement after 4 months of the combined systemic treatment.
Discussion
LPP is a lymphocyte-mediated inflammatory condition and has a considerable range of clinical spectrum. The clinical manifestations involve scarring alopecia of the scalp, non-scarring alopecia of the body hair, and follicular papules, which can be inflammatory or non-inflammatory [3, 6, 7, 8]. LPP can be classified into three clinical variants based on the distribution of the lesions and shared histopathological features: (1) classic LPP, patch/patches of cicatricial alopecia occurring on the scalp, (2) Graham-Little-Piccardi-Lasseur syndrome (GLPLS) characterized by LPP of the scalp, non-cicatricial alopecia of the axillae and pubis, and follicular papules involving the trunk or extremities, and (3) frontal fibrosing alopecia, band-like cicatricial alopecia of the frontotemporal hairline with inconsistent eyebrow loss [9, 10, 11, 12]. Apart from the aforementioned, fibrosing alopecia in a pattern distribution has been introduced as a new type of LPP involving miniaturized hair [13].
As mentioned above, non-scarring alopecia of the axillary and pubic hairs and follicular papules on the trunk or extremities are the characteristic components of GLPLS. Although the onset of these features can occur in any order, the development of the hyperkeratotic papules often precedes the onset of alopecia in any region. In the present case, the presence of scalp LPP and follicular papules may thus indicate an early stage of GLPLS. However, involvement of LPP on the areas beyond the scalp has been described in the literature (Table 1) [2, 5, 6, 14, 15]. Reported clinical manifestations were as follows: facial papules, generalized keratotic follicular papules on the body [5, 6], and focal scarring hair loss or acute patchy hair loss on the limbs [2, 5, 14, 15]. Nevertheless, there is scant information related to histopathological and dermoscopic features of the extra-scalp lesions.
Table 1.
Reported cases of lichen planopilaris on the areas beyond the scalp
| Author, year | Patients, n | Clinical features |
Histopathological findings | Dermoscopic examination | Therapy | Outcome | |
|---|---|---|---|---|---|---|---|
| Scalp lesion | Non-scalp lesion (n) | ||||||
| Miteva et al. [15], 2010 | 2 | FFA | Acute patchy hair loss on the limbs | Concentric fibroplasia and follicular lymphocytic interface changes with vacuolar degeneration | NA | NA | NA |
| Chew et al. [14], 2010 | 10 | FFA | Upper limb alopecia | Perifollicular lymphocytic infiltrate with interface change and perifollicular fibrosis, dermal fibrotic tract | NA | NA | NA |
| László [6], 2014 | 1 | LPP (GLPLS) | Follicular dark red adherent tiny papules, axillary and pubic alopecia | Perifollicular lymphocytic infiltrate with focal vacuolar alteration | NA | NA | NA |
| Vendramini et al. [2], 2017 | 1 | None | Isolated body hair loss on the limbs | Perifollicular lichenoid inflammation and scarring | Perifollicular erythema, discrete perifollicular scaling and broken hairs | Doxycycline 100 mg daily and topical clobetasol | Pruritus improved |
| Arshdeep et al. [5], 2018 | 4 | LPP or FFA | Patchy alopecia of trunk, limbs, or eyebrows (4) | Lichenoid folliculitis and follicular scarring | Broken hairs, peripilar casts in active disease | NA | NA |
| Facial papules (2) | Vellus hair LPP | Loss of vellus hairs | |||||
| Generalized KP-like papules (1) | Lichenoid folliculitis and follicular destruction | Peripilar casts, gray-brown discoloration of follicular ostia, broken hairs | |||||
| Present case | 1 | LPP | Generalized comedone-like keratotic papules | Perifollicular lymphocytic infiltrate with lichenoid reaction and dilated follicles | Perifollicular scaling with gray-brown dots | Hydroxychloroquine 200 mg daily, isotretinoin 10 mg daily and topical desoximetasone 0.25% | Slightly improved |
FFA, frontal fibrosing alopecia; GLPLS, Graham-Little-Piccardi-Lasseur syndrome; KP, keratosis pilaris; LPP, lichen planopilaris; n, number of patients; NA, data not available.
Our histopathological features are in agreement with the previously published articles as representing perifollicular lymphocytic infiltrate with lichenoid alteration [2, 5, 6, 14, 15]. One recent report revealed dermoscopic findings of generalized inflammatory keratosis pilaris-like papules as peripilar casts, gray-brown discoloration of follicular ostia, and broken hairs [5]. Likewise, our dermoscopic examination showed consistent findings. We theorize that the involvement beyond the scalp could possibly indicate a generalized nature of the disease process. For early detection and treatment, individuals with LPP should undergo detailed history taking and full-body dermatological examination as LPP can potentially involve multiple sites even with various clinical features. Dermoscopy could be a useful diagnostic tool in making diagnoses, particularly with extra-scalp lesions.
Recently, it has been noted that two groups of diseases including LPP subsets and keratosis pilaris atrophicans subsets share a significant histopathological pattern and also clinically overlap. The term “lichenoid folliculitis” had therefore been proposed to refer to the constellation of diseases with follicular papules and scarring alopecia, scalp or non-scalp, with lichenoid dermatitis in histopathology. The possibility of shared pathogenesis and treatment options may exist but somehow remains to be fully determined [16].
To conclude, LPP has a wide range of clinical spectrum. It can sometimes affect hair follicles on other regions beyond the scalp, and it is considered to have a generalized disease process when present. Early detection and prompt treatment are crucial to prevent further follicular destruction and scarring. In addition to routine histopathological study, dermoscopic evaluation has been proven to be beneficial in helping diagnose.
Statement of Ethics
The patient provided written informed consent to perform all necessary investigations, to take clinical photographs, and use them for research purposes and publication. The patient understood that her name and initials will not be published and due efforts will be made to conceal her identity. This case report was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have no funding sources to declare.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for the manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
References
- 1.Lyakhovitsky A, Amichai B, Sizopoulou C, Barzilai A. A case series of 46 patients with lichen planopilaris: Demographics, clinical evaluation, and treatment experience. J Dermatolog Treat. 2015 Jun;26((3)):275–9. doi: 10.3109/09546634.2014.933165. [DOI] [PubMed] [Google Scholar]
- 2.Vendramini DL, Silveira BR, Duque-Estrada B, Boff AL, Sodré CT, Pirmez R. Isolated Body Hair Loss: An Unusual Presentation of Lichen Planopilaris. Skin Appendage Disord. 2017 Jan;2((3-4)):97–9. doi: 10.1159/000449229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babahosseini H, Tavakolpour S, Mahmoudi H, Balighi K, Teimourpour A, Ghodsi SZ, et al. Lichen planopilaris: retrospective study on the characteristics and treatment of 291 patients. J Dermatolog Treat. 2019 Sep;30((6)):598–604. doi: 10.1080/09546634.2018.1542480. [DOI] [PubMed] [Google Scholar]
- 4.Ramos-e-Silva M, Pirmez R. Red face revisited: disorders of hair growth and the pilosebaceous unit. Clin Dermatol. 2014 Nov-Dec;32((6)):784–99. doi: 10.1016/j.clindermatol.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 5.Arshdeep BM, Batrani M, Kubba A, Kubba R. Lichen planopilaris beyond scalp: a case series with dermoscopy-histopathology correlation. Int J Dermatol. 2018 Nov;57((11)):e127–31. doi: 10.1111/ijd.14168. [DOI] [PubMed] [Google Scholar]
- 6.László FG. Graham-Little-Piccardi-Lasseur syndrome: case report and review of the syndrome in men. Int J Dermatol. 2014 Aug;53((8)):1019–22. doi: 10.1111/j.1365-4632.2012.05672.x. [DOI] [PubMed] [Google Scholar]
- 7.Mehregan DA, Van Hale HM, Muller SA. Lichen planopilaris: clinical and pathologic study of forty-five patients. J Am Acad Dermatol. 1992 Dec;27((6 Pt 1)):935–42. doi: 10.1016/0190-9622(92)70290-v. [DOI] [PubMed] [Google Scholar]
- 8.Suchonwanit P, Iamsumang W, Rojhirunsakool S. Efficacy of Topical Combination of 0.25% Finasteride and 3% Minoxidil Versus 3% Minoxidil Solution in Female Pattern Hair Loss: A Randomized, Double-Blind, Controlled Study. Am J Clin Dermatol. 2019 Feb;20((1)):147–53. doi: 10.1007/s40257-018-0387-0. [DOI] [PubMed] [Google Scholar]
- 9.Harnchoowong S, Suchonwanit P. PPAR-γ Agonists and Their Role in Primary Cicatricial Alopecia. PPAR Res. 2017;2017:2501248. doi: 10.1155/2017/2501248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suchonwanit P, Pakornphadungsit K, Leerunyakul K, Khunkhet S, Sriphojanart T, Rojhirunsakool S. Frontal fibrosing alopecia in Asians: a retrospective clinical study. Int J Dermatol. 2020 Feb;59((2)):184–90. doi: 10.1111/ijd.14672. [DOI] [PubMed] [Google Scholar]
- 11.Leerunyakul K, Suchonwanit P. Asian Hair: A Review of Structures, Properties, and Distinctive Disorders. Clin Cosmet Investig Dermatol. 2020 Apr;13:309–18. doi: 10.2147/CCID.S247390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suchonwanit P, Chalermroj N, Khunkhet S. Low-level laser therapy for the treatment of androgenetic alopecia in Thai men and women: a 24-week, randomized, double-blind, sham device-controlled trial. Lasers Med Sci. 2019 Aug;34((6)):1107–14. doi: 10.1007/s10103-018-02699-9. [DOI] [PubMed] [Google Scholar]
- 13.Triyangkulsri K, Srisuwanwattana P, Sriphojanart T, Suchonwanit P. Fibrosing Alopecia in a Pattern Distribution: A Case Report and Literature Review. Case Rep Dermatol. 2019 Oct;11((3)):297–302. doi: 10.1159/000503681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chew AL, Bashir SJ, Wain EM, Fenton DA, Stefanato CM. Expanding the spectrum of frontal fibrosing alopecia: a unifying concept. J Am Acad Dermatol. 2010 Oct;63((4)):653–60. doi: 10.1016/j.jaad.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 15.Miteva M, Camacho I, Romanelli P, Tosti A. Acute hair loss on the limbs in frontal fibrosing alopecia: a clinicopathological study of two cases. Br J Dermatol. 2010 Aug;163((2)):426–8. doi: 10.1111/j.1365-2133.2010.09807.x. [DOI] [PubMed] [Google Scholar]
- 16.Turegano MM, Sperling LC. Lichenoid folliculitis: A unifying concept. J Cutan Pathol. 2017 Jul;44((7)):647–54. doi: 10.1111/cup.12938. [DOI] [PubMed] [Google Scholar]