Abstract
Purpose:
The purpose of this study is to evaluate the clinical efficacy of enhancing deficient interdental papilla with hyaluronic acid gel injection.
Materials and Methods:
Eight patients (three males and five females) were included. Patients had papillary deficiency in the upper anterior area. Prior to treatment, photographic images were taken for each patient. After the administration of a local anesthetic, a 23G needle was used to inject <0.2 mL of a commercially available and Food and Drug Administration-approved hyaluronic acid gel this treatment was repeated up to 2–3 times. Clinical photographic measurements of the black triangle area (BTA), black triangle height, and black triangle width were undertaken before the treatment and during follow-up. The interdental papilla reconstruction rate was calculated to determine the percentage change of the BTA between the initial and final examinations of the interdental papilla by means of injectable hyaluronic acid gel were evaluated.
Results:
Eight sites had complete interdental papilla reconstruction and six sites showed improvements ranging from 78.5 ± 19.83%. More specifically, when contact point and the bone crest reached 6 mm, virtually complete interdental papilla reconstruction was achieved.
Conclusions:
The results from this study are encouraging and present evidence that small papillary deficiencies between teeth can be enhanced by the injection of a hyaluronic acid gel.
Keywords: Esthetic, hyaluronic acid, interdental papilla, periodontal treatment
Introduction
Patient demands for esthetically pleasing results after periodontal or implant therapy present significant challenges to the dental team. In the modern dentistry, patients' recovery of lost masticatory function and recovery of dental esthetics for the case of the upper anterior area, the patient's esthetic demands can be met when restorations are made such that the gingival topography matches the gingival contour. However, creating natural-looking soft tissue in the upper anterior area is a difficult task.[1] The criteria for successful soft-tissue formation in the anterior area largely rely on the existence of a healthy interdental papilla and the formation of a matching gingival contour.[2] A deficiency in interdental papillae creates problems with pronunciation and food impaction, along with esthetic issues.[3] Interdental papillae not only play a role in protecting the periodontal tissue in the anterior area by blocking food impaction but also and serve an esthetic purpose.[4]
To date, many studies have analyzed the factors influencing deficient interdental papillae. Among such studies, Tarnow et al.[5] reported that interdental papillae were often present when the distance between the contact point and the bone crest (CP-BC) was ≤5 mm. Moreover, in a study by Cho et al.[6] on the effects of the interproximal distance between the roots (IDR) on the presence of interdental papillae, according to the CP-BC, it was reported that, as IDR or CP-BC increased, the interdental papillae were less frequently present. In particular, when the CP-BC was 4–6 mm, an increase in the IDR resulted in a sensitive decrease in the presence of interdental papilla. Unlike the study by Tarnow et al.[5] which included both the anterior and posterior areas, Chen et al.[7] conducted a study on only the upper anterior area and reported that, when the CP-BC was ≤4 mm, interdental papillae were present in 100% of the cases, whereas when this distance was ≥7 mm, interdental papillae were always deficient. Although other studies have reported that gender, interproximal embrasure area, interdental papilla length, and crown morphology are the associated factors,[8,9,10] CP-BC is considered the most important associated factor for the presence of the interdental papilla.[5,6,7,8,9,10]
Various periodontal plastic surgery methods have been suggested for the reconstruction of deficient interdental papillae. Although a variety of surgical procedures and flap designs have been suggested,[11,12,13,14,15] they have had limited success and have lacked predictability; as such, interdental papilla reconstruction is considered one of the most challenging periodontal plastic surgery procedures.[15] Therefore, plastic surgeons and dermatologists have a long history of using various substances to enhance the esthetics in the oral facial regions.[16] Recently, a gel of hyaluronic acid generated by Streptococcus species of bacteria, chemically cross-linked with butanediol diglycidyl ether, stabilized and suspended in phosphate-buffered saline at pH 7 and concentration of (20 mg/mL, pH 7) and fee of animal protein has been successfully used to reduce or eliminate facial creases and various other abnormalities.[17,18,19,20] The product is approved by the Federal Food and Drug Administration. Its primary role is to bind water to maintain tissue structure and its characteristics, including consistency, biocompatibility, and hydrophilicity, have made it an excellent moisturizer in cosmetic dermatology and skin-care products. To date, injectable hyaluronic acid gel has been successfully used to reduce wrinkles and improve other similar facial deformities.[21]
Accordingly, the present study aimed to investigate the effects of hyaluronic acid gel injection for the reconstruction of deficient interdental papillae in the upper anterior area, assessing the clinical factors influencing reconstruction of the interdental papilla.
Materials and Methods
Patient selection
The present study was conducted with approval from the Institutional Review Board of the Maharashtra University of Health Science in accordance with the World Medical Association declaration of Helsinki. All participants in the study were provided with an overview of the clinical trial, and the study was conducted after signed consent forms were obtained from each participant.
Among the patients of the department of periodontology, eight were recruited (three males and five females). Participants' age ranged between 27 and 35 years, with a mean age of 32 years. The inclusion criteria included patients with at least one papillary deficient site in the upper anterior area and with a plaque index[22] and gingival index[23] between zero and one. Patients who were pregnant and patients taking medication known to increase the risk of gingival enlargement and those who were currently receiving orthodontic treatment on the upper anterior area were excluded.
The experiment was conducted on a total of 22 sites in the upper anterior area with papillary deficiency. Among these sites, five sites were excluded because the black triangle area (BTA) was too small to be measured through an image analysis, and three sites were excluded because of the absence of contact points due to the presence of diastema. Consequently, the study was conducted on a total of 14 sites in the upper anterior area with papillary deficiency.
Procedure
We explained the purpose of the study to patients before treatment, and a short-acting local anesthetic was administered. The values for variables, BTA, black triangle height (BTH), and black triangle width (BTW) were measured from at the initial examination and followed up for 3 months. Furthermore, in case of complete interdental papilla reconstruction, [Figure 1] pixel values on the clinical photograph equivalent to a periodontal probe length of 10 mm were used as a reference for converting the variable values expressed in pixels to physical length (in mm). The portion of the black triangle that was measured was demarcated on the image and BTA, BTH, and BTW were automatically converted to millimeters. A single assessor with no knowledge of the procedures took all of the measurements, and the mean value for each site was calculated from 10 measurements taken at each site.
Figure 1.
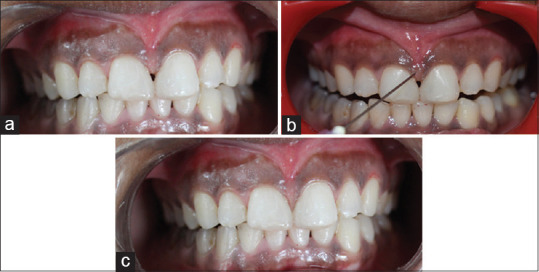
A case of complete interdental papilla reconstruction. (a) At baseline. (b) While hyaluronic acid dermal filler injection. (c) Follow-up after 3 months
A commercially available hyaluronic-based dermal filler (<0.2 mL) was injected 2–3 mm apical to the tip of the papilla [Figure 1]. After the treatment, individual patients' syringes were capped, identified with the patient's name, and stored in a refrigerator for future use on the same patient. The needles were discarded. Patients were seen 3 weeks after the initial treatment, and if the dark space remained another injection was applied. This sequence was repeated up to three times. Patients were followed from 3 months after the initial gel application. At study completion, the clinical slides were reviewed and presented to an outside consultant (I. G.) for the determination of measurement changes between the initial and final photographs.
For the analysis of the effects of the injectable hyaluronic acid gel, the interdental papilla reconstruction rate (IPRR) was defined as the percentage of change in the initial BTA to the final BTA after 3 months.[24]
When the final clinical measurements were taken, cases that showed no clinical signs of a black triangle were categorized into the complete interdental papilla reconstruction (CIPR) [Figure 1], while cases that still had a clinically observable black triangle were categorized as the follow partial interdental papilla reconstruction (PIPR) group.
Data analysis
Statistical analysis was conducted using commercially available statistical software (SPSS version 20.2, IBM Corp., Armonk, NY, USA). A Shapiro–Wilk test of normality was done. Mean comparisons of each item between the CIPR group and the PIPR group were carried out using a parametric t-test, whereas a Mann-Whitney U test was used for nonparametric data. P < 0.05 was considered to be statistically significant.
Results
After performing interdental papilla reconstruction using injectable hyaluronic acid gel on a total of eight patients at 14 interdental papilla sites in the upper anterior area, a mean IPRR of 89.25% was found with 2.57 injections, whereas BTA, BTH, and BTW showed a mean decrease of 0.25, 0.85, and 0.34 mm2, respectively [Table 1].
Table 1.
Overall outcomes of interdental papilla reconstruction
| Patient number | Site | ΔBTA (mm2) | ΔBTH (mm) | ΔBTW (mm) | IPRR | Number of applications |
|---|---|---|---|---|---|---|
| 1 | A | 0.10 | 0.79 | 0.28 | 100 | 1 |
| B | 0.20 | 1.08 | 0.36 | 100 | 2 | |
| 2 | A | 0.27 | 0.91 | 0.46 | 100 | 2 |
| 3 | A | 0.34 | 0.36 | 0.10 | 39 | 3 |
| 4 | A | 0.51 | 1.25 | 0.30 | 79 | 3 |
| B | 0.40 | 1.18 | 0.61 | 100 | 3 | |
| C | 0.26 | 0.75 | 0.67 | 100 | 3 | |
| 5 | A | 0.09 | 0.70 | 0.25 | 100 | 2 |
| B | 0.41 | 1.22 | 0.27 | 92 | 3 | |
| 6 | A | 0.11 | 0.82 | 0.24 | 100 | 3 |
| 7 | A | 0.32 | 0.84 | 0.31 | 85 | 3 |
| B | 0.26 | 1.00 | 0.34 | 89 | 3 | |
| 8 | A | 0.14 | 0.43 | 0.36 | 100 | 2 |
ΔBTA: Reduction in black triangle area; ΔBTH: Reduction in black triangle height; ΔBTW: Reduction in black triangle width; IPRR: Interdental papilla reconstruction rate; SD: Standard deviation
CIPR was found in eight treated sites, whereas the remaining six sites showed an IPRR ranging from 16% to 91%. With respect to the comparison of the mean values of clinical variables between the partial interproximal papilla reconstruction (PIPR) groups and complete interproximal papilla reconstruction (CIPR), the initial BTA, BTH, and BTW showed statistically significant differences [Table 2]. The initial BTA, BTH, and BTW also increased and were strongly positively correlated.
Table 2.
Comparison between the complete interdental papilla reconstruction group and the partial interdental papilla reconstruction group
| Mean±SD |
P | ||
|---|---|---|---|
| CIPR (8 sites) | PIPR (6 sites) | ||
| IPRR | 100±0.00 | 78.5±19.83 | <0.001 |
| Number of application | 2.25±0.70 | 3.00±0.00 | <0.001 |
| Clinical variables | |||
| ΔBTA | 0.19±0.10 | 0.33±0.11 | <0.001 |
| ΔBTH | 0.83±0.23 | 0.87±0.35 | <0.001 |
| ΔBTW | 0.40±0.16 | 0.26±0.08 | <0.001 |
Statistically significant (P<0.05) using the Mann-Whitney U-test; and Statistically significant (P<0.05) using the Student t-test. IPRR: Interdental papilla reconstruction rate; BTA: Black triangle area; BTH: Black triangle height; BTW: Black triangle width; CIPR: Complete interdental papilla reconstruction; PIPR: Partial interdental papilla reconstruction; SD: Standard deviation
Discussion
Some studies have already reported that successful interdental papilla reconstruction is possible by using commercial injectable hyaluronic acid gel. In a study by Becker et al.,[23] it was possible to achieve 100% CIPR at three of 14 sites with a maximum of three injections of injectable hyaluronic acid gel at 3-week intervals, whereas the remaining 11 sites showed an IPRR of 57%–97%. Mansouri et al.[24] used the same experimental methods as Becker et al.[23] and reported a wide-ranging IPRR of 22%–100% at a 6-month follow-up of a total of 21 sites in the upper anterior area, with nine sites showing an IPRR of ≥50%. In the present study, 13 of a total of 14 sites showed an IPRR of ≥50%. Moreover, CIPR occurred at 08 sites, which is a higher percentage than that reported in other studies, whereas the remaining sites showed wide-ranging partial reconstruction (18%–91%). These differences might be attributable to differences in the initial interdental papillary deficiency levels and the experimental design. The studies by Becker et al.[23] and Mansouri et al.[24] did not provide information on the initial interdental papillary deficiency levels, making it difficult to make a direct comparison with the results from the present study; however, it is possible that areas with less initial interdental papillary deficiency might have been included in the present study.
When the mean values of each variable were compared between the CIPR and PIPR groups, the initial interdental papillary deficiency level and final interdental papillary deficiency level were a statistically significant degree. Previous studies[5,6,7,8,9,10] have reported that the CP-BC was the most important factor in interdental papillary deficiency. Moreover, the deficient area of the interdental papilla also increased as the BTA, BTH, and BTW increased. However, in present study we didn't calculate CP-BC level and IDR. Earlier studies[6,9] reported that the presence of the interdental papilla decreased with an increasing IDR, but recent studies[7,10] have reported that when the CP-BC variable was controlled, the influence of the IDR on the presence of the interdental papilla disappeared. Thus, the IDR has a minimal influence on interdental papilla reconstruction using injectable hyaluronic acid gel; hence, we did not studied IDR in the present study.
Interestingly, most cases with a CP-BC of up to 6 mm showed CIPR, but as the distance increased beyond this cutoff, the IPRR tended to decrease. Interdental papillae are generally considered biologically safe and stable with a CP-BC of up to 5 mm.[7] Tarnow et al.[5] have also reported that there was virtually no interdental papillary deficiency at a CP-BC ≤5 mm. The injectable hyaluronic acid gel has a predictable interdental papilla reconstruction effect of approximately 1 mm in the vertical direction. Therefore, a CP-BC value of 6 mm can be used as a cutoff value for interdental papilla reconstruction using hyaluronic acid gel.
In the present study, we used clinical measurements by two operators to increase the reproducibility of clinical measurements taken at interdental papilla areas. In studies by Becker et al.[23] and Mansouri et al.,[24] initial photographs were taken perpendicular to teeth of interest, and these were used to take subsequent photos as close to the original photos as possible without a special device. Such a method required the utmost effort to reproduce the same horizontal and vertical angles during the photography. However, it was still difficult to reproduce a photo at the same corresponding angle. Therefore, more studies are needed in the development of a more precise reproducible alignment device and method.
Within the limitations of this study, the CP-BC and IDR were not studied with the BTA, BTH, and BTW. Interdental papilla reconstruction using injectable hyaluronic acid gel allowed successful reconstruction when the CP-BC was ≤6 mm, but for the CP-BC >6 mm, the increased distance resulted in a decreased IPRR. Therefore, the CP-BC is closely associated with the efficacy of hyaluronic acid gel injection for the reconstruction of deficient interdental papillae in the upper anterior area.
Conclusions
The application of hyaluronic acid gel was somehow effective for interdental papilla reconstruction and might be used as a minimally invasive technique for the reconstruction of interdental papilla by dentists.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
Acknowledgments
The authors gratefully thank Dr. Hardik Rana, Dr. Abinesh M, and Dr. Manjiree Awad Sennerby for their advice and encouragement during the course of this study.
References
- 1.Grunder U. The inlay-graft technique to create papillae between implants. J Esthet Dent. 1997;9:165–8. [PubMed] [Google Scholar]
- 2.Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72:1364–71. doi: 10.1902/jop.2001.72.10.1364. [DOI] [PubMed] [Google Scholar]
- 3.Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546–9. doi: 10.1902/jop.2000.71.4.546. [DOI] [PubMed] [Google Scholar]
- 4.Tarnow DP, Eskow RN. Considerations for single-unit esthetic implant restorations. Compend Contin Educ Dent. 1995;16:778, 780, 782–4. [PubMed] [Google Scholar]
- 5.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 6.Cho HS, Jang HS, Kim DK, Park JC, Kim HJ, Choi SH, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006;77:1651–7. doi: 10.1902/jop.2006.060023. [DOI] [PubMed] [Google Scholar]
- 7.Chen MP, Chan CP, Tu YK, Liao YF, Ku YC, Kwong LK, et al. Factors influencing the length of the interproximal dental papillae between maxillary anterior teeth. J Dent Sci. 2009;4:103–9. [Google Scholar]
- 8.Kim JH, Cho YJ, Lee JY, Kim SJ, Choi JI. An analysis on the factors responsible for relative position of interproximal papilla in healthy subjects. J Periodontal Implant Sci. 2013;43:160–7. doi: 10.5051/jpis.2013.43.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang LC. Assessment of parameters affecting the presence of the central papilla using a non-invasive radiographic method. J Periodontol. 2008;79:603–9. doi: 10.1902/jop.2008.070376. [DOI] [PubMed] [Google Scholar]
- 10.Beagle JR. Surgical reconstruction of the interdental papilla: Case report. Int J Periodontics Restorative Dent. 1992;12:145–51. [PubMed] [Google Scholar]
- 11.Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17:326–33. [PubMed] [Google Scholar]
- 12.Nemcovsky CE. Interproximal papilla augmentation procedure: A novel surgical approach and clinical evaluation of 10 consecutive procedures. Int J Periodontics Restorative Dent. 2001;21:553–9. [PubMed] [Google Scholar]
- 13.Lee EK, Herr Y, Kwon YH, Shin SI, Lee DY, Chung JH. I-shaped incisions for papilla reconstruction in second stage implant surgery. J Periodontal Implant Sci. 2010;40:139–43. doi: 10.5051/jpis.2010.40.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nemcovsky CE, Moses O, Artzi Z. Interproximal papillae reconstruction in maxillary implants. J Periodontol. 2000;71:308–14. doi: 10.1902/jop.2000.71.2.308. [DOI] [PubMed] [Google Scholar]
- 15.Dover JS, Carruthers A, Carruthers J, Alam M. Clinical use of restylane. Skin Therapy Lett. 2005;10:5–7. [PubMed] [Google Scholar]
- 16.Rohrich RJ. Introduction to the restylane consensus statement. Plast Reconstr Surg. 2006;117:1S–2S. doi: 10.1097/01.prs.0000204756.22188.c8. [DOI] [PubMed] [Google Scholar]
- 17.Rohrich RJ, Ghavami A, Crosby MA. The role of hyaluronic acid fillers (restylane) in facial cosmetic surgery: Review and technical considerations. Plast Reconstr Surg. 2007;120:41S–54S. doi: 10.1097/01.prs.0000248794.63898.0f. [DOI] [PubMed] [Google Scholar]
- 18.Soparkar CN, Patrinely JR, Skibell BC, Tower RN. Hyaluronidase and restylane. Arch Facial Plast Surg. 2007;9:299–300. doi: 10.1001/archfaci.9.4.299. [DOI] [PubMed] [Google Scholar]
- 19.Strand A. Reuse of restylane syringes after patient injection. J Am Acad Dermatol. 2006;54:741–2. doi: 10.1016/j.jaad.2005.11.1048. [DOI] [PubMed] [Google Scholar]
- 20.Necas J. J, Bartosikova L, Brauner P, Kolar J. Hyaluronic acid (hyaluronan): A review. Vet Med (Praha) 2008;53:397–411. [Google Scholar]
- 21.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 22.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 23.Becker W, Gabitov I, Stepanov M, Kois J, Smidt A, Becker BE. Minimally invasive treatment for papillae deficiencies in the esthetic zone: A pilot study. Clin Implant Dent Relat Res. 2010;12:1–8. doi: 10.1111/j.1708-8208.2009.00247.x. [DOI] [PubMed] [Google Scholar]
- 24.Mansouri SS, Ghasemi M, Salmani Z, Shams N. Clinical application of hyaluronic acid gel for reconstruction of interdental papilla at the esthetic zone. J Islam Dent Assoc Iran. 2013;25:191–6. [Google Scholar]


