Abstract
Periodontitis has a multifactorial etiology as a result of interactions between periodontal pathogens and the host response. Due to the complex etiology and esthetic complications, the management of such patients is a challenging task. Vast arrays of treatment modalities are employed in the treatment of generalized periodontitis with varying success rates. Placental-derived tissues as allografts have recently been introduced for guided tissue regeneration in dentistry with favorable results. In this case report, successful periodontal treatment of a 25-year-old male patient with generalized periodontitis; Stage IV, Grade C, is presented with a 3-year follow-up. An interdisciplinary approach using regenerative periodontal surgery and a modified Andrew's bridge was used to successfully rehabilitate the patient. In a compliant patient with a well-structured interdisciplinary approach, questionable and hopeless teeth too can be retained over an extended period of time with no detrimental effect on the adjacent teeth.
Keywords: Bone grafts, case report, generalized periodontitis, guided tissue regeneration, India
Introduction
Periodontitis has a multifactorial etiology as a result of interactions between periodontal pathogens and the host response.[1] Vast arrays of treatment modalities are employed in the treatment of generalized periodontitis with varying success rates. Placental-derived tissues such as allografts have recently been introduced for guided tissue regeneration (GTR) in dentistry with favorable results. This case presents the successful and long-term management of a patient diagnosed with generalized periodontitis; Stage IV, Grade C;[2,3] currently unstable, with GTR and allografts, results of which were followed up for 36 months. In a patient with optimal patient compliance, surgical periodontal treatment is effective even in hopeless teeth and may therefore be an alternative to extraction of the teeth with hopeless prognosis. The modified Andrew Bridge is a viable option in a patient with a Siebert's class III defect thus negating the need for invasive and less predictable surgical ridge augmentation procedures.
Case Report
This 25-year-old male patient presented to the Department of Periodontology, Government Dental College and Hospital, Mumbai, India in 2016 with a chief complaint of pain and bleeding gums with intermittent purulent discharge in his teeth for 1 year. The patient was systemically healthy, and nonsmoker. A brief perio-charting revealed generalized bleeding on probing (BOP) with severe periodontal destruction evident with clinical attachment loss ranging from 6 to 8 mm and probing pocket depth (PPD) ranging from 8 to 10 mm. A panoramic radiograph [Figure 1] and intraoral periapical X-rays revealed the generalized distribution of horizontal and vertical alveolar bone loss with large periapical radiolucencies surrounding the roots of teeth #15, 25, 26, 36, 37, and 46, and the teeth were nonvital and associated with degree II mobility. Based on the World workshop 2017 classification of periodontal and peri-implant diseases and conditions, periodontal diagnosis of generalized periodontitis; Stage IV, Grade C; currently unstable, with combined periodontic-endodontic lesions (primary periodontal with secondary endodontic lesion) on teeth #15, 25, 36, and 46 was established. Permanent maxillary right central and lateral incisors, maxillary left central incisor, and maxillary third molars had degree III mobility with hopeless prognosis and were subsequently extracted. An acrylic partial denture was given to the patient as an interim restoration after 3 weeks.
Figure 1.
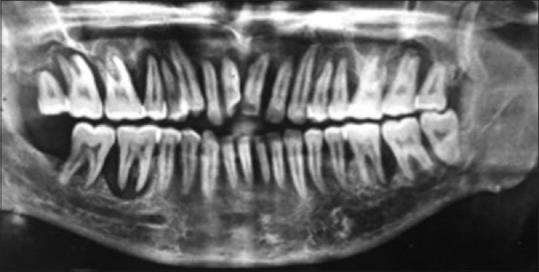
Preoperative panoramic radiograph of a 28-year male patient with generalized periodontitis
BOP, PPD, and relative attachment loss (RAL) were recorded at six sites per tooth (distobuccal, mediobuccal, mesiobuccal, distolingual, mediolingual, and mesiolingual with a standard periodontal manual probe (PCP-UNC 15, Hu-Friedy) using an acrylic customized stent with markings at six fixed reference points. RAL was evaluated by measuring the distance between the margin of the stent and the bottom of the clinical pocket.
Vertical two walled defects were present on mesial surfaces of permanent mandibular and maxillary second molars and distal surfaces of maxillary and mandibular first molars and premolars with depth of the defects in the range of 5–7 mm. The patient was informed about the questionable prognosis of teeth #25 and #46 (more than 50% bone loss); however, he was reluctant to undergo extraction, and hence, an attempt was made to salvage them.
The treatment plan included a concerted protocol, which included endodontic and periodontal treatment steps. After endodontic therapy, a full-mouth scaling and root planning was done along with systemic antibiotics (Amoxicillin 500 mg three times a day and Metronidazole 400 mg three times a day for 8 days. There was an over-all marked reduction in PPD and BOP, and the patient was scheduled for the periodontal surgical phase.
After obtaining written, informed consent for surgery from the patient, a quadrant-wise full-mouth flap surgery was performed under antibiotic prophylaxis. Local anesthesia was administered using 2% lignocaine containing adrenaline at a concentration of 1:80,000. A Kirkland flap was made on the buccal and lingual aspect of the teeth one tooth distal and mesial to the involved tooth, and full thickness flaps were reflected; root planing was done and the teeth with vertical defects were thoroughly degranulated with hand and ultrasonic instruments.
After presuturing, an allograft DFDBA with particle size <500 microns (Tata Memorial tissue bank) was hydrated in sterile saline for 5 minute before placement into the intrabony defects and condensed into the defect site with light incremental pressure without overfilling the two-walled defect. The allograft chorionic membranes (Tata Memorial tissue bank) were gently trimmed and adapted to the defect site to cover 2–3 mm of the surrounding alveolar bone. Finally, the mucoperiosteal flap was repositioned and sutured at the original level using 4–0 silk with interrupted sutures which were removed after 10 days. Patient was prescribed analgesics and given oral hygiene instructions, which included chlorhexidine mouth wash (0.2%) twice a day for the first two postoperative weeks and also use of interdental cleansing aids. Re-evaluation of the outcome of the etiotropic phase was done after 3 months based on Merin's criteria. Diligent periodontal maintenance visits were conducted wherein supragingival scaling was meticulously done and postoperative instructions were re-enforced. A maintenance program was set up for all patients at three monthly intervals.
At the 36-month recall, there was significant reduction in BOP and PPD which was found to be <5 mm on maxillary and mandibular second premolars and permanent mandibular first molars and with significant radiographic bone fill around the grafted vertical defects [Figure 2]. There was also significant gain of attachment after 6 and 12 months compared to the baseline with marked reduction in mobility of the teeth.
Figure 2.

Postoperative panoramic radiograph 36 months after surgery. Note the radiographic bone fill at the distal roots of permanent maxillary second premolars, and permanent mandibular first molars
The Siebert's Class III alveolar ridge defect in the anterior maxilla was a prosthodontic challenge and was successfully restored with a modified Andrew's bridge using teeth#13 and #23 which had adequate bone support as abutments [Figure 3].
Figure 3.

Final cementation of porcelain fused to metal fixed partial denture and the removable pontic assembly of Modified Andrew's Bridge
Discussion
Treatment of advanced forms of periodontitis is based on evidence-based protocols; research has shown that GTR in conjunction with bone grafting has better potential for regeneration compared with either technique alone,[4,5] and this outcome has also been confirmed in advanced periodontitis with the use of bioresorbable membranes.[6,7] Chorion has also been assessed for its properties in treating periodontal infrabony pockets in periodontitis patients with significant improvement in radiographic and clinical parameters such as PPD and RAL when compared to periodontal therapy alone.[7]
In treatment planning, De Van's statement should always be a cornerstone in the dentist's mind: “Our goal should be the preservation of what remains rather than the meticulous restoration of what is missing.”[8] Although some teeth had more than 50% bone loss, such teeth with guarded prognosis could be salvaged after endodontic treatment and periodontal surgery. In a compliant patient, questionable and hopeless teeth can be retained over an extended period of time with no detrimental effect on adjacent teeth.[9]
Alveolar ridge defects are a restorative challenge to the dentist and different treatment modalities are adopted for their prosthetic rehabilitation. These include implant-supported fixed dental prosthesis with onlay grafting and guided bone regeneration. However, this may not only be expensive and unpredictable but may also have an extended period of treatment. The modified Andrew's bridge prosthesis uses a removable prosthesis which is retained by a bar and sleeve attachment on their intaglio surface to fixed retainers and has favorable stress distribution to the abutments.[10] Limited reports of the failure of such prosthesis are found in the literature,[9] which were mainly attributed to soldering failures.
Conclusion
This case presents the successful and long-term management generalized periodontitis with GTR and allografts, results of which were followed up for 36 months. In a compliant patient with a well-structured interdisciplinary approach, questionable and hopeless teeth too can be retained over an extended period of time with no detrimental effect on the adjacent teeth.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge the Department of Periodontology for their technical and logistic support.
References
- 1.Kornman KS. Mapping the pathogenesis of periodontitis: A new look. J Periodontol. 2008;79:1560–8. doi: 10.1902/jop.2008.080213. [DOI] [PubMed] [Google Scholar]
- 2.Caton J, Armitage G, Berglundh T, Chapple I, Jepsen S, Kornman K, et al. 2017 World Workshop A new classification scheme for periodontal and peri-implant diseases and conditions– Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1–8. doi: 10.1111/jcpe.12935. [DOI] [PubMed] [Google Scholar]
- 3.Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol. 2018;45(Suppl 20):S149–S161. doi: 10.1111/jcpe.12945. [DOI] [PubMed] [Google Scholar]
- 4.Murphy KG, Gunsolley JC. Guided tissue regeneration for the treatment of periodontal intrabony and furcation defects. A systematic review. Ann Periodontol. 2003;8:266–302. doi: 10.1902/annals.2003.8.1.266. [DOI] [PubMed] [Google Scholar]
- 5.Gottlow J, Nyman S, Lindhe J, Karring T, Wennström J. New attachment formation in the human periodontium by guided tissue regeneration. Case reports. J Clin Periodontol. 1986;13:604–16. doi: 10.1111/j.1600-051x.1986.tb00854.x. [DOI] [PubMed] [Google Scholar]
- 6.Reynolds MA, Aichelmann-Reidy ME, Branch-Mays GL, Gunsolley JC. The efficacy of bone replacement grafts in the treatment of periodontal osseous defects. A systematic review. Ann Periodontol. 2003;8:227–65. doi: 10.1902/annals.2003.8.1.227. [DOI] [PubMed] [Google Scholar]
- 7.Kothiwale SV. The evaluation of chorionic membrane in guided tissue regeneration for periodontal pocket therapy: A clinical and radiographic study. Cell Tissue Bank. 2014;15:145–52. doi: 10.1007/s10561-013-9386-9. [DOI] [PubMed] [Google Scholar]
- 8.DeVan MM. Basic principles in impression making.1952. J Prosthet Dent. 2005;93:503–8. doi: 10.1016/j.prosdent.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Graetz C, Dörfer CE, Kahl M, Kocher T, Fawzy El-Sayed K, Wiebe JF, et al. Retention of questionable and hopeless teeth in compliant patients treated for aggressive periodontitis. J Clin Periodontol. 2011;38:707–14. doi: 10.1111/j.1600-051X.2011.01743.x. [DOI] [PubMed] [Google Scholar]
- 10.Christenson GJ, Guyer SE, Lefkowitz W, Malone WF, Sproull RC. Evaluation of a fixed removable partial denture: Andrews bridge system. J Prosthet Dent. 1983;50:180–4. doi: 10.1016/0022-3913(83)90008-2. [DOI] [PubMed] [Google Scholar]


