Abstract
Background:
The aim of this study was to compare the effectiveness of root coverage through vestibular incision subperiosteal tunnel access (VISTA) technique using platelet rich fibrin (PRF) or subepithelial connective tissue graft (SCTG) in multiple gingival recessions.
Materials and Methods:
A total of 20 patients with multiple gingival recessions were included, and 10 subjects were randomly allocated to test group (VISTA with PRF) and 10 patients to control group (VISTA with SCTG). Clinical parameters were recorded at baseline, 3 months, and 6 months. Patient's response toward the treatment was also assessed by questionnaire.
Results:
All the clinical parameters in the study have showed better results in test group when compared to control group after a follow up period of 6 months with statistical significance.
Conclusion:
The results of the present study suggested that multiple gingival recessions can be successfully treated with both procedures, but better root coverage and a greater increase in keratinized tissue were achieved with the VISTA technique with SCTG. All the patients in both groups felt it was worth undergoing the treatment.
Keywords: Gingival recession, platelet-rich fibrin, root coverage, subepithelial connective tissue graft, vestibular incision subperiosteal tunnel access
Introduction
Periodontal esthetics, which forms an integral part of a healthy and intact periodontium is often disturbed by one of the commonly encountered findings, which happens to be the gingival recession. It is defined as “displacement of gingival margin (GM) apical to cementoenamel junction (CEJ).”[1] While inflammation in the gingiva is the main cause of the recession, other factors such as anatomical factors that constitute thin biotype, abnormal tooth position and shape,[2] faulty tooth brushing,[3] aberrant frenal attachment[4] and iatrogenic factors also have been implicated in the etiology of gingival recession.
Taking these factors into consideration, various procedures have evolved for root coverage over the years encompassing free gingival grafts, subepithelial connective tissue grafts (SCTGs) and pedicle grafts such as laterally repositioned flap, double papilla flap, coronally advanced flap (CAF), semilunar flap, etc., Off late, the use of allografts such as acellular dermal matrix (ADMA) and enamel matrix proteins have also been reported with considerable predictability and success. The majority of these procedures have been implicated in localized or solitary recessions. On the other hand, root coverage of multiple recessions poses a more significant challenge to the periodontist, wherein procedures such as contiguous lateral pedicle flaps, SCTG s, CAF, pouch and tunnel approach etc., have been attempted with varying degrees of success.[5]
One of the recently introduced techniques by Zadeh in 2011 was the vestibular incision subperiosteal tunneling access, i.e., VISTA.[6] Among the various determinants behind successful root coverage, maintenance of adequate vascular supply is one of the most important determinants. Taking into consideration this procedure not only promises adequate blood supply but also it being minimally invasive requires a small opening entailing the undermining of periosteum completely in the area of root coverage, which would further help in the coronal repositioning of the flap passively onto the exposed root surface. However, since successful root coverage also depends on the underlying width of keratinized gingiva augmenting the width of keratinized gingiva in addition to merely covering the exposed roots, also forms an important criterion. In this process, this technique needs subepithelial connective tissue, an autograft to be placed in enhancing the periodontal biotype. VISTA, along with SCTG has provided very favorable results,[7] with the only disadvantage of this technique being the need for the second surgical site and often a large amount of SCTG would be required in order to cover multiple recessions. Placement of other commercially available grafts such as ADMA, amniotic membrane, collagen membrane, bioactive glass, etc., which could be alternatives for the connective tissue can also be advocated, but the major limitation with these materials could be their expensiveness and the patient acceptability due to religious considerations. One alternative to address this problem would be the use of biologic mediators like platelet-rich fibrin (PRF), which is a platelet derivative.
Hence, there is a need to compare the clinical outcome of VISTA with SCTG and VISTA with PRF in the management of multiple gingival recessions, and as few studies have only investigated this problem, the present study envisages to evaluate the efficacy of these procedures in patients seeking root coverage of multiple gingival recessions.
Materials and Methods
Source of the data
This was a randomized prospective clinical comparative study conducted to evaluate the amount of root coverage using the VISTA technique with PRF membrane and SCTG for multiple gingival recessions. CTRI/2018/10/015999.
Patient selection
The patients who attended the Department of Periodontics and Implantology for seeking treatment of multiple gingival recessions were randomly assigned to either of the test and control groups using coin toss method. Out of a sample of 20 patients, 10 patients were subjected to VISTA with PRF membrane that comprised the test group and 10 patients to VISTA with SCTG that comprised the control group. After the ethical committee approval from the institute, an informed signed consent document from the patients, which explained all procedures involved in the protocol and the possible benefits and harm associated with the proposed study was put forth. Sample size was calculated using G power 3.1.9.2 software (SPSS software India by Norman H Nie in 2015 G Power 3.1.9.2) considering 80% power, 95% confidence level, 5% confidence interval with a mean probing pocket depth 2.27 mm, 2.08 mm before and after treatment with a standard deviation of 0.34 mm.[8]
Selection criteria
Patients aged between 18 to 60 years who were systemically healthy with no contraindications for periodontal surgery and with the presence of a minimum of two adjacent recessions of Miller's class I or II along with the absence of clinical signs of active periodontal disease were included in the study.
Patients with recession defects associated with caries, deep abrasions, or restorations with active gingival and periodontal disease, any systemic conditions that would interfere with healing and teeth with excessive root prominence and smokers and pregnant or lactating women were excluded from the study.
Clinical parameters included assessment of plaque index[9] (PI) and gingival index[10] (GI), probing depth (PD), clinical attachment level (CAL), width of recession (RW), depth of recession (RD), width of keratinized tissue (KT), and gingival thickness (GT). All assessments were carried out with the University of North Carolina (UNC-15 periodontal probe) and the measurements were recorded at baseline, 3, and 6 months after the surgery.
All the patients received NonSurgical Periodontal Therapy initial treatment, which consisted of scaling and root planing followed by oral hygiene instructions. The full mouth periodontal condition was ensured to be normal at least 1 week before the planned surgery.
Surgical procedure
The surgical procedure was performed under local infiltration with 2% lignocaine containing adrenaline at a concentration of 1:2,00,000 at the site. The donor palatal site was anesthetized by a greater palatine nerve block in cases where the graft was harvested.
VISTA procedure
Under the local anesthesia, VISTA approach initiates with a vestibular access incision. The location of the access incision depends on the sites being treated, wherein midline frenum was considered for maxillary anterior region, frenal area between canine and lateral incisor was considered for maxillary posterior region and in cases of mandibular anterior and posterior regions area between canine and lateral incisor was taken into consideration.
The access incision was made through the periosteum to elevate a subperiosteal tunnel exposing the facial osseous plate as well as root dehiscences. This tunnel was extended for multiple gingival recessions requiring root coverage to mobilize GMs and facilitate coronal repositioning using the VISTA kit. An SCTG or PRF membrane was then trimmed to fit the dimension of the surgical area and was adjusted to extend at least 3–5 mm beyond the bony dehiscences overlying the root surfaces. Each tooth was then prepared for attachment of the suture to the tooth. The facial enamel surface of each tooth was briefly acid etched for <5 s, thoroughly washed, and dried. The 4.0 vicryl/5.0 monofilament polypropylene sutures were secured to the facial aspect of each tooth by placing a small amount of flowable composite resin over the knot, thereby effectively preventing apical relapse of the GM during the initial stages of healing. The access incision was then approximated and sutured primarily with multiple 4.0 vicryl/5.0 monofilament polypropylene sutures, with a periodontal dressing placed. Sutures at the access incision were removed after 1 week. Coronally anchored bonded sutures were generally removed at the 3-week postoperative visit to allow for immobilization of the GM [Figures 1-4].
Figure 1.

(a) Miller's class I gingival recessions in relation to 14.15 and class II in relation to 16–test site. (b) Under local anesthesia access incision given in the vestibule and subperiosteal tunnel prepared using vestibular incision subperiosteal tunnel access kit. (c) Platelet-rich fibrin membrane placed into the tunnel. (d) Gingival margins coronally repositioned by composite retained horizontal mattress sutures and simple suture placed in access incision region
Figure 4.

Miller's class II gingival recessions in relation to 23, 24 – control site. (a) Baseline, (b) 3 months, (c) 6 months
Figure 2.

(a) Miller's class II gingival recessions in relation to 25, 26–test site. (b) Under local anesthesia access incision given in the vestibule and subperiosteal tunnel prepared using vestibular incision subperiosteal tunnel access kit. (c) Subepithelial connective tissue graft placed into the tunnel. (d) Gingival margins coronally repositioned by composite retained horizontal mattress sutures and simple sutures placed in access incision region
Figure 3.
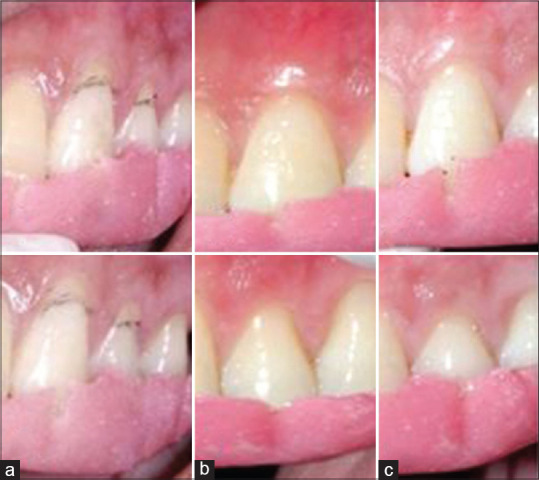
Miller's class I gingival recessions in relation to 23, 24 – test site. (a) Baseline, (b) 3 months, (c) 6 months
Platelet rich fibrin membrane preparation
The PRF was procured as per the method suggested by Choukroun et al.[11] PRF procured without biochemical manipulation of blood and required neither anticoagulant nor bovine thrombin before surgery, 20 ml of venous blood was drawn from the patient by venipuncture of the antecubital vein into two sterile glass test tubes (vacutainer) of 10 ml each centrifuged immediately at 3000 rpm for 10 min using tabletop centrifuge. PRF was converted to membrane by using compressing kit. Choukroun A-PRF12 was the centrifuge used for PRF preparation, PRF DUO Company.
Graft harvesting
The trap door technique proposed by Langer was used to harvest graft from palate,[12] wherein the template was placed in the palate between the distal line angle of the canine and the mesial line angle of the palatal root of the 2nd molar. With the template in place, a horizontal incision was made 2–3 mm away from the GM and two vertical incisions were made at either end of the initial incision. A partial thickness flap was elevated creating a “door.” The underlying connective tissue graft of adequate thickness (2 mm) and without epithelial collar was harvested. The palatal flap was repositioned, and the donor site was compressed with wet gauze to eliminate dead space and control bleeding. The palatal flap was sutured with 4-0 vicryl suture.
Graft placement
The harvested graft was trimmed with a surgical blade if necessary, and was introduced into the tunnel and was placed in the recipient area at the level of CEJ.
Postoperative care
All the subjects received postoperative analgesics (the combination of ibuprofen 400 mg, paracetamol 325 mg thrice daily for 3 days and antibiotics (amoxicillin 500 mg t.i.d for 3 days) with routine postoperative instructions given. The patients were refrained from tooth brushing at the surgical site for 4 weeks and were instructed to rinse the mouth with 0.2% chlorhexidine gluconate mouthwash daily for 6 weeks. They were asked to report immediately if periodontal dressing got displaced in <2 weeks or if they experienced any untoward bleeding from the surgical area (donor and recipient), and no patient reported with these problems. In a 3-week postoperative check-up, the periodontal dressing was removed, and saline irrigation was done at the surgical site. On the other hand, the sutures in the donor site were removed after 1 week. From the 4th week of surgery, the patients were advised to start gentle brushing using a toothbrush with soft bristles in the operated area.
Postsurgical measurements
All clinical measurements were recorded during the recall visits, i.e., at the end of 3 months and 6 months. The patient response toward the treatment was assessed by questionnaire, which included:
Pain experienced by the patient after surgery
Esthetics before surgery
Esthetics after surgery
Do you advise this surgery for others (yes/no).
For the first three questions visual analog scale score was used to elucidate its response, whereas for 4th question, dichotomous score was used.
Statistical analysis
Descriptive statistics were expressed as mean ± standard deviation. Comparison of the study groups with means of all the parameters was made using Mann–Whitney U-test. Intragroup comparison of all the clinical parameters was done by the Wilcoxon Sign Rank test. A level of significance of 5% was assumed (P <0.05).
Statistical software: The statistical software namely SPSS 20.0, Stata 8.0, MedCalc 9.0.1, Systat 12.0 were used for analysis of the data and Microsoft Word and Excel have been used to generate graphs and tables.
Results
A total of 20 patients participated in the study. Among them 13 male and 7 female patients with a mean age of 35.64 for VISTA with PRF group and 35.32 for VISTA with SCTG group were included. A total of 58 recessions were included amongst which 37 (19-test, 18-control) comprised of class-I and 21 (14-test, 7-control) comprised of class-II gingival recessions. Patients who presented with a request for coverage of exposed roots were included in the study. All of them participated in the study for the entire period there being no dropouts. All the patients tolerated the surgery well and there were no serious intrasurgical or postsurgical complications. Two patients of the SCTG group had mild painless swelling a day after the surgery which subsided within a few days. No cases of postsurgical bleeding, and paresthesia were reported. Healing in the operated area and that of the donor area in the control group was satisfactory. All the periodontal parameters viz., PI, GI, PD, CAL, RD, RW, of WKT, GT were measured and compared at baseline, 3 months and 6 months after the surgery [Tables 1-3].
Table 1.
Comparision of the test group and control group at baseline
| Parameter | Group | Mean±SD | P (intergroup) |
|---|---|---|---|
| Plaque index | Test group | 0.61±0.13 | 0.796 |
| Control group | 0.65±0.18 | ||
| Gingival index | Test group | 0.62±0.09 | 0.436 |
| Control group | 0.69±0.19 | ||
| Probing depth | Test group | 2.65±0.56 | 0.256 |
| Control group | 2.44±0.31 | ||
| Clinical attachment level | Test group | 5.40±1.55 | 0.011* |
| Control group | 4.64±0.50 | ||
| Recession depth | Test group | 3.24±1.19 | 0.000* |
| Control group | 2.74±0.72 | ||
| Recession width | Test group | 3.87±1.13 | 0.000* |
| Control group | 2.75±0.72 | ||
| Width of keratinised tissue | Test group | 2.03±0.75 | 0.002* |
| Control group | 2.24±0.59 | ||
| Gingival thickness | Test group | 0.80±0.13 | 0.010* |
| Control group | 0.80±0.10 |
*P<0.05 statistically significant, #Applied Mann-Whitney U-test. SD: Standard deviation
Table 3.
Comparision of the test group and control group at 6 months
| Parameter | Group | Mean±SD | P (intergroup) |
|---|---|---|---|
| Plaque index | Test group | 0.44±0.07 | 0.739 |
| Control group | 0.43±0.08 | ||
| Gingival index | Test group | 0.43±0.09 | 0.912 |
| Control group | 0.42±0.08 | ||
| Probing depth | Test group | 2.14±0.39 | 0.878 |
| Control group | 2.10±0.26 | ||
| Clinical attachment level | Test group | 3.73±1.92 | 0.011* |
| Control group | 2.58±0.92 | ||
| Recession depth | Test group | 1.69±1.59 | 0.000* |
| Control group | 1.78±0.30 | ||
| Recession width | Test group | 2.27±1.87 | 0.010* |
| Control group | 1.78±0.30 | ||
| Width of keratinized tissue | Test group | 2.90±0.99 | 0.000* |
| Control group | 3.74±1.00 | ||
| Gingival thickness | Test group | 1.09±0.27 | 0.020* |
| Control group | 0.99±0.08 |
*P<0.05 statistically significant, #Applied Mann-Whitney U-test. SD: Standard deviation
Table 2.
Comparision of the test group and control group at 3 months
| Parameter | Group | Mean±SD | P (intergroup) |
|---|---|---|---|
| Plaque index | Test group | 0.45±0.09 | 0.353 |
| Control group | 0.51±0.11 | ||
| Gingival index | Test group | 0.44±0.10 | 0.043* |
| Control group | 0.51±0.11 | ||
| Probing depth | Test group | 2.15±0.33 | 0.951 |
| Control group | 2.13±0.24 | ||
| Clinical attachment level | Test group | 3.97±1.47 | 0.000* |
| Control group | 2.58±0.91 | ||
| Recession depth | Test group | 1.62±1.34 | 0.000* |
| Control group | 2.11±0.32 | ||
| Recession width | Test group | 2.36±1.91 | 0.010* |
| Control group | 2.11±0.32 | ||
| Width of keratinized tissue | Test group | 2.90±0.96 | 0.000* |
| Control group | 3.64±0.97 | ||
| Gingival thickness | Test group | 1.07±0.28 | 0.020* |
| Control group | 1.02±0.11 |
*P<0.05 statistically significant, #Applied Mann-Whitney U-test. SD: Standard deviation
Comparision of root coverage
In VISTA + PRF group out of 33 recessions, 10 recessions constituted (30.3%) obtained complete root coverage, whereas the remaining 23 constitute 69.67% obtained partial coverage.
In VISTA + SCTG group out of 25 recessions, 15 recessions (60%) were completely covered whereas 10 (40%) were partially covered.
9 out of 10 patients treated by VISTA + PRF felt that their aesthetics considerably improved after the surgery, whereas all the 10 out of 10 patients treated by VISTA + SCTG felt that their aesthetics considerably improved following the treatment.
A majority of the patients in both the groups did experience mild to moderate pain after the surgery but did not complain of severe pain causing disability to carry out their routine.
All the patients in both the groups felt it was worth undergoing the treatment and responded that they would recommend the treatment to others having similar problems.
Discussion
Among all the procedures involved in periodontal plastic surgery root coverage is the most commonly performed technique which has gained tremendous popularity among both clinicians and patients. Reports from various epidemiological surveys have clearly revealed that gingival recession happens to be one of the common clinical finding affecting most of the adult population.[13]
Although a large amount of data available in the literature is made up of reports of few cases or case series with varying results, as it often happens and that studies only with positive results would be published with scarce information on failure rates. It is only in recent years some strong and well designed systematic reviews have been published,[13,14,15] which provided insight into the predictability and success of various procedures. Further, the ambit of such procedures has been enlarged beyond coverage of the root. Augmentation of the keratinised gingiva and gingival biotype, esthetically acceptable color match, maintenance of the root coverage over a long time are some of the objectives one aims at. In addition, the procedure itself should be less technique sensitive and devoid of excessively stressful surgery and morbidity. Last but not the least is the patient's acceptance which is the ultimate yardstick to evaluate the usefulness of any procedure.
However, a majority of these reports have dealt with root coverage of solitary recessions of Miller's class I and II. Although many procedures have been attempted for covering multiple adjacent recessions, there are no systematic reviews which would place the efficacy of these procedures in their proper perspective. Multiple recession defects present different set of challenges to the clinician. Apart from a larger avascular area which usually happens to be difficult in restoring blood supply to the grafted tissue and which is also so vital for healing, the need for large amount of donor tissue and the presence of noncarious cervical lesions which are often associated with multiple gingival recessions compound the problem. Procedures such as Pouch and tunnel approach, dentoepithelial transfer have been attempted but the results have not been predictable. Taking all these factors into consideration, a technique which is minimally invasive, which did not compromise the blood supply and yet resulted in improvement of all the clinical parameters was the need of the day. The VISTA technique is one that answered most of the requirements. Undermining the periosteum through a very minimal incision released the overlying gingival tissue to be easily advanced coronally without compromising the blood supply and helped in covering many adjacent exposed roots in a single session. However, VISTA by itself did not result in augmentation of the keratinised gingiva, increase in the GT or prevent recurrence of the recession due to muscle pull. One way to achieve all the desired end points was to harvest SCTG and sandwich the same in to the prepared tunnel. While this improved the predictability of the VISTA procedure, it still suffered from the drawback of a second surgical site, the requirement of a large amount of connective tissue at a distant donor site thereby increasing the potential for postharvesting morbidity. An alternative to SCTG was the use of allografts such as acellular dermal matrix, collagen membrane etc.
In recent years, PRF which is obtained from the same patient known to contain abundant growth factors has also been used effectively in many surgical procedures. PRF is easy to prepare, inexpensive and has high patients acceptance as it is not derived from other species. However, as mentioned earlier the success of VISTA with PRF has been reported only in a few case reports there being no systematic reviews. Hence, this study was envisaged to evaluate the effectiveness of VISTA with PRF as against a proven technique that is VISTA with SCTG in adjacent multiple gingival recessions.
The results obtained in this study following the use of SCTG has been good with 15 out of 25 recessions showing complete root coverage, which sustained even at the 6-month follow-up and reasonable root coverage in the remaining defections. In addition, the width of keratinized gingiva was also increased along with an increase in the thickness of gingiva, thereby improving the gingival biotype. Thus the results obtained are in accordance with that of earlier randomized controlled clinical trials done by Chenchev et al.[8] in 2016, and case series done by Reddy et al.,[7] in 2016, Gupta et al.[16] in 2014, Chatterjee et al.,[17] Garg S et al.,[18] Kumar TA et al.19, in 2018, a systematic review on CAF by Cairo et al.[20] in 2008, randomized controlled clinical trial by Zucchelli and De Sanctis et al.[21] in 2014, Jankovic et al. 2010,[22] randomized clinical trial by Elif[23] in 2017 on MCAF + PRF and MCAF + SCTG, and a study done by Eren et al.[24] in 2016 on CAF combined with PRF or SCTG.
It can hence be confidently concluded that SCTG is the gold standard of periodontal plastic surgical procedures. Not, withstanding the above-said advantages, the main limitation of the SCTG is the need for the second surgery, wherein also the thickness of the palatal mucosa and the shape of the palate play a vital role in the harvestment of the graft.[12] Hence, various other substitutes have been tried in place of SCTG, Which included Acellular dermal matrix and collagen membranes enriched with growth factors such as rh PDGF-BB, β-TCP carrier matrix.[13] However, these are expensive and may discourage the patients from undergoing the procedure due to increased cost. Further, the origin of these biomaterials (usually bovine/porcine) may not be acceptable to many patients due to religious constraints. Hence, an alternative is the increasingly popular PRF. PRF, which is an autologous leukocyte-PRF matrix, is composed of a tetra-molecular structure with cytokines, platelets, and stem cells within it. With all the above-said properties, it has the potential to act as a biodegradable scaffold that favored the development of micro vascularization and its ability to guide epithelial cell migration to its surface. It has been extensively used in various periodontal regenerative procedures, often in combination with other bone replacement grafts.[11] It is also easy to prepare and acceptable to patients. In this study, 10 out of 33 defects had complete root coverage when PRF was used. However, compared to SCTG, the extent of root coverage and the gain in width was less, and there was no difference between the two with regards to the change in the gingival biotype. However, this procedure was more acceptable to the patients as there was no second surgical site. However, no difference in the type of tissue that formed regarding the color match, and the texture was elicited.
Overall, both techniques produced satisfactory results in the study, but comparatively, VISTA with SCTG gave superior results. While this was a totally clinical study showing only improvement in clinical parameters, the type of attachment that formed could not be ascertained as only histological studies could highlight the same. In addition, PRF if augmented with other biomaterials such as tricalcium phosphate or other absorbable barrier membranes, may provide results similar to VISTA with SCTG. Notwithstanding the fact that further studies with higher samples and longer follow-up periods are required, it can be concluded that the VISTA technique is a potentially predictable and efficient method to cover multiple gingival recessions.
Conclusion
Both the procedures, i.e., VISTA with PRF and VISTA with SCTG, resulted in root coverage to a variable extent. However, VISTA with SCTG was distinctly superior to VISTA with PRF in all the parameters, i.e., greater reduction in recession depth, recession width, CAL gain, increase in the keratinised tissue and GT. Both the procedures, i.e., VISTA with PRF and VISTA with SCTG resulted in stable outcomes with no recurrence of gingival recession, during the study period. Both the techniques gave excellent color match with the adjacent tissue. VISTA with PRF can be employed if the sole objective is to obtain root coverage, provided there is an adequate zone of KT apical to existing recession.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
References
- 1.Guttiganur N, Aspalli S, Sanikop MV, Desai A, Gaddale R, Devanoorkar A. Classification systems for gingival recession and suggestion of a new classification system. Indian J Dent Res. 2018;29:233–7. doi: 10.4103/ijdr.IJDR_207_17. [DOI] [PubMed] [Google Scholar]
- 2.Alldritt WA. Abnormal gingival form. Proc R Soc Med. 1968;61:137–42. doi: 10.1177/003591576806100211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gillette WB, Van House RL. Ill effects of improper oral hygeine procedure. J Am Dent Assoc. 1980;101:476–80. doi: 10.14219/jada.archive.1980.0295. [DOI] [PubMed] [Google Scholar]
- 4.Jargin SV. On the minimally invasive approach to the gingival recession. J Indian Soc Periodontol. 2013;17:394–6. doi: 10.4103/0972-124X.115655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134:220–5. doi: 10.14219/jada.archive.2003.0137. [DOI] [PubMed] [Google Scholar]
- 6.Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31:653–60. [PubMed] [Google Scholar]
- 7.Reddy S, Prasad MG, Bhowmik N, Singh S, Pandit H, Vimal SK. Vestibular Incision Subperiosteal Tunnel Access with platelet rich fibrin and connective tissue graft in the management of multiple gingival recession-a case series. Int J Appl Dent Sci. 2016;2:34–7. [Google Scholar]
- 8.Chenchev IV, Neichev D, Vicheva D, Atanasov D, Noncheva V. VISTA technique and platelet-rich fibrin membrane for treatment of multiple adjacent gingival recessions-6 month follow-up. IOSR J Dent Med Sci. 2016;15:128–33. [Google Scholar]
- 9.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 10.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 11.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715–20. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- 13.Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: A systematic review from the AAP regeneration Workshop. J Periodontol. 2015;86:8–51. doi: 10.1902/jop.2015.130674. [DOI] [PubMed] [Google Scholar]
- 14.Cairo F, Pagliaro U, Buti J, Baccini M, Graziani F, Tonelli P, et al. Root coverage procedures improve patient aesthetics. A systematic review and Bayesian network meta-analysis. J Clin Periodontol. 2016;43:965–75. doi: 10.1111/jcpe.12603. [DOI] [PubMed] [Google Scholar]
- 15.Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root-coverage procedures for the treatment of localized recession-type defects: A Cochrane systematic review. J Clin Periodontol. 2015;86:8–51. doi: 10.1902/jop.2010.090540. [DOI] [PubMed] [Google Scholar]
- 16.Gupta G, Puri K, Bansal M, Khatri M, Kumar A. Platelet rich fibrin–reinforced vestibular incision subperiosteal tunnel access technique for recession coverage. Clin Adv Periodontics. 2015;5:248–53. [Google Scholar]
- 17.Chatterjee A, Sharma E, Gundanavar G, Subbaiah SK. Treatment of multiple gingival recessions with vista technique: A case series. J Indian Soc Periodontol. 2015;19:232–5. doi: 10.4103/0972-124X.145836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garg S, Arora SA, Chhina S, Singh P. Multiple gingival recession coverage treated with vestibular incision subperiosteal tunnel access approach with or without platelet-rich fibrin – A case series. Contemp Clin Dent. 2017;8:464–8. doi: 10.4103/ccd.ccd_142_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar TA, Gowda TM, Mehta DS, Kumar A. Management of multiple gingival recessions with the VISTA technique: An 18-month clinical case series. Int J Periodontics Restorative Dent. 2018;38:245–51. doi: 10.11607/prd.2990. [DOI] [PubMed] [Google Scholar]
- 20.Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J Clin Periodontol. 2008;35:136–62. doi: 10.1111/j.1600-051X.2008.01267.x. [DOI] [PubMed] [Google Scholar]
- 21.Zucchelli G, De Sanctis M. Treatment of multiple recession-type defects in patients with esthetic demands. J Periodontol. 2000;71:1506–14. doi: 10.1902/jop.2000.71.9.1506. [DOI] [PubMed] [Google Scholar]
- 22.Jankovic S, Aleksic Z, Milinkovic I, Dimitrijevic B. The coronally advanced flap in combination with platelet-rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: A comparative study. Eur J Esthet Dent. 2010;5:260–73. [PubMed] [Google Scholar]
- 23.Elif O. The use of platelet rich fibrin versus subepithelial connective tissue graft in treatment of multiple gingival recessions: A randomised clinical trial. Int J Periodontics Restor Dent. 2017;37:265–71. doi: 10.11607/prd.2741. [DOI] [PubMed] [Google Scholar]
- 24.Eren G, Kantarcı A, Sculean A, Atilla G. Vascularization after treatment of gingival recession defects with platelet-rich fibrin or connective tissue graft. Clin Oral Investig. 2016;20:2045–53. doi: 10.1007/s00784-015-1697-8. [DOI] [PubMed] [Google Scholar]


