Abstract
Background
As the coronavirus (COVID-19) epidemic passed initial infection peak in Washington State, phased re-opening lifted stay-at-home orders and restrictions leading to increased non-essential work, social activities and gathering, especially among younger persons.
Methods
A longitudinal cohort analysis of Washington State Department of Health COVID-19 confirmed case age distribution 1) March-April 2020 (N = 13,934) and 2) March-August 2020 (N = 76,032) for proportional change over time using chi square tests for significance.
Results
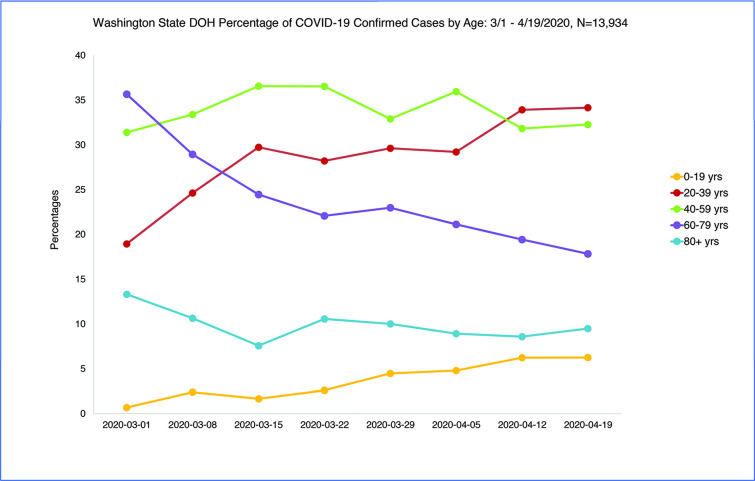
From March 1st to April 19, 2020 COVID-19 age distribution shifted with a 10% decline in cases age 60 years and older and a 20% increase in age 0-19/20-39 years (chi-square = 223.10, p < .001). Number of cases over the initial analysis period were 0–19 years n = 515, 20–39 years n = 4078, 40–59 years n = 4788, 60–79 years n = 3221, 80+ years n = 1332. After the peak (March 22, 2020), incidence declined in older age groups and increased among age 0–19 and 20–39 age groups from 20% to 40% of total cases by April 19 and 50% by May 3. During this time testing expanded with more testing among older age groups and less testing among younger age groups while case positivity shifted young. Percent positive cases age 0-19/20-39 years through August 2020 increased to a consistent average of 60% [age 0–19 increased to 19% (N = 10257), age 20–39 increased to 42% (N = 30215)].
Conclusions
An increased sustained proportion of COVID-19 incidence is present among children (age 0–19) and young adults (age 20–39) indicating an elevated role in disease spread during the epidemic creating a possible reservoir of disease with spillover risk to more vulnerable older persons and those with comorbid conditions. Media savvy age-appropriate messaging to enhance mitigation compliance among less vulnerable, more mobile and lower priority vaccination age groups will be a continued necessity and priority to reduce overall population incidence.
Introduction
The 2019 novel coronavirus (COVID-19) has quickly spread over the globe and positive cases continue to climb. The first reported case of 2019-nCoV infection in the United States was in Washington State (WA) on January 19, 2020 and on March 23rd, a statewide stay-at-home order was announced to remain in effect until May 4th which was extended to May 30, 2020 and then lifted in a move to phased reopening [1, 2]. Change of stay-at-home restrictions, social gathering guidelines and reopening of businesses lead to an increase of non-essential work and social activities, especially among younger persons. Hospitalization and death rates associated with older age and comorbid conditions declined within a short time after stay at home orders were issued. These rates continued to decline over time while the number of confirmed positive cases plateaued, indicating shift to younger age of incident cases if present could explain the changed presentation and severity of cases [3]. Using Washington State Department of Health (DOH) data, we analyzed incidence of COVID-19 cases by age over time for significant change in age distribution as the pandemic progressed.
Methods
Testing of symptomatic patients for COVID-19 in Washington State steadily increased since the outbreak began in January 2020 with drive-through testing beginning in some communities in late March increasing testing availability. Testing expanded rapidly in Washington State as we were the first state in the Union to have a positive COVID-19 case (January 16, 2020). Testing quickly shifted to all symptomatic patients whereas at the beginning in January and February only hospitalized symptomatic patients were tested. We restricted our analysis to March 1, 2020 forward when local testing became available, testing capacity increased and was no longer restricted to hospitalized symptomatic patients.
Initial COVID-19 test kits from CDC were sent to Washington State February 4, 2020. A flaw in the reagents was found right away and reported back to the CDC. The flaw was corrected by February 26, 2020, the State testing lab had authorization and test kits as of 2/27/2020 and began sample testing that day with test results reported 2/29/2020 [4, 5]. The University of Washington Virology lab developed their own testing which was approved and operational by February 27, 2020 [6].
Testing sites continued to increase into the summer months to more than 25. Total testing capacity statewide continues to change, which means each lab is the best source for current numbers on their own testing capacity. The results from all COVID-19 tests flow into the Washington Disease Reporting System (WDRS), an electronic disease surveillance system that allows public health staff in Washington state to receive, enter, manage, process, track and analyze disease-related data. Aggregate testing data is updated and published daily on the WA State DOH website with an update by age and county weekly.
The data was not collected by the authors and is submitted to the states by the counties who get the test result data from the laboratories conducting the tests. Once submitted to the state the data is reviewed for duplicates by patient identifiers (Name and Residence). There is a two-week lag time in reporting to the state and removal of duplicates. Data that has not been verified is flagged as provisional in the state and county reporting dashboards [7]. The Epidemiologic Curves tab is the most accurate representation of COVID activity and is updated daily as new cases are identified and duplicates are resolved. This is the source of the de-identified data download we used in our study and is made available to the public on the Washington State Department of Health website [7].
The data in this study was IRB exempt as it is publicly available and de-identified (no personal identifiers) available for download on the Washington State Department of Health website [8]. We only used time periods that were two weeks prior to the date of download to account for the two-week lag in reporting to the state by the counties and for data de-duplication process.
For the initial data analysis and trend reporting, weekly updated COVID-19 positive confirmed case data from March 1st to April 19th, Washington State DOH were used which are available to the public on the DOH website [8]. The updated data for trend over time in age distribution for weeks 4/26-8/23/2020 was obtained from the same source. Lab-confirmed COVID-19 cases from hospital, intensive care units, emergency departments and outpatient testing are reported to DOH by acute care hospitals in Washington daily. The data from DOH includes the number of cases, deaths and hospitalizations by week, county and age groups. Additional publicly available data on number of tests performed was also used in our study to address possible bias of changed testing by age over time at the beginning of the pandemic. Our analysis for age trend over time used data through the week of 8/23/2020 to stay in the time frame when schools were still closed, updated September 20, 2020 to allow for a time lag in reporting.
Testing data was only available for the first time period and we used age-specific testing data from 3/1/2020 to 4/19/2020 to match the first time period analysis of COVID-19 positive test results by age. We did not use the first 6 weeks of data to avoid the potential bias of only hospitalized symptomatic patient testing.
Laboratory-confirmed county-assigned cases by state assigned age groups 0–19, 20–39, 40–59, 60–79 and 80+ years in Washington State were enumerated and plotted over time. Statistical analyses were performed using Microsoft Excel for percentage calculations, an online chi square calculator for two-sided significance testing with a .05 level of significance and an online chi-squared test for trend [9–11]. Chi square tests were used to compare the observed proportions of positive COVID-19 tests by age to determine if there is statistically significant difference over time at the p = .05 level.
Weeks for the first analysis were restricted to March 1 to April 19 2020 when a sufficient number of cases (20 or more) had accrued to be statistically relevant and to accommodate the two-week lag time in case reporting and confirmation to WDRS. Age 0–19 was included even though there were only 4 cases in the first analysis week but case counts were greater than 20 in following weeks. Chi-square tests were run comparing the first two weeks of increased cases (3/1/2020, 3/8/2020), the peak week (3/22/2020) and weeks (4/12/2020, 4/19/2020). Initial comparison weeks were restricted to 3 groups and time from 3/1/2020 to 4/19/2020 to avoid the diminishment of statistical validity by multiple comparisons. Chi square statistics were calculated for testing by age to the same initial time period to assess the degree to which age group testing was equivalent to case positive distribution or over sampling was done by age group. The secondary analysis was a chi square test for slope (linear trend) of percentage confirmed positive cases age less than 40 using the last weeks of April through August for significant additional age shift from older to younger cases over time.
Results
Total number of positive cases in Washington State reported from January 16th to April 19th excluding positive cases with unknown age (n = 10) were 14,220 with 13,934 confirmed cases from March 1 to April 19 [0–19 = 515 (4%), 20–39 = 4078 (29%); 40–59 = 4788 (34%); 60–79 = 3221 (23%); 80+ = 1332, (10%)]. The four counties with the highest number of cases by rank order were King (n = 5955), Snohomish (n = 2300), Pierce (n = 1300), and Yakima (n = 1119). As the epidemic progressed and the curve flattened, fewer older and more young persons tested positive for COVID-19 with the percentage of total cases among age 0–19 and 20–39 doubling from 20% to 40% (Fig 1). There was an increase in cases age 0–19 years over time from four cases week 3/1/2020 to 83 cases week 4/19/2020 and 131 cases week 5/3/2020. Incidence among age 60 and older declined 55% off the peak week of 3/22/2020 but 20-39-year-old cases only declined 36% off the peak week. Table 1. The chi-square test statistic for the comparison of confirmed cases by age across the three discrete time periods of weeks 3/1–3/8, 3/22, and 4/12-4/19, was 223.10, p < .001.
Fig 1. WA State DOH COVID-19 confirmed cases by age: 3/1/2020-4/19/2020.
Table 1. WA State DOH COVID-19 confirmed cases by age: 3/1/2020-4/19/2020 (n = 13,934) (3/1/2020-5/3/2020 N = 16,698).
| 0–19 N (%) | 20–39 N (%) | 40–59 N (%) | 60–79 N (%) | 80+ N (%) | Row Total | Chi Square | p-value | |
|---|---|---|---|---|---|---|---|---|
| Week | ||||||||
| 3/1 | 4 (.7%) | 111 (19%) | 184 (31%) | 209 (36%) | 78 (13%) | 586 (4%) | 223.10 | < .001 |
| 3/8 | 37 (2%) | 382 (25%) | 518 (33%) | 449 (29%) | 165 (11%) | 1551 (11%) | ||
| 3/15 | 38 (2%) | 680 (30%) | 836 (37%) | 559 (24%) | 178 (8%) | 2286 (16%) | ||
| 3/22 | 65 (3%) | 708 (28%) | 917 (37%) | 548 (22%) | 265 (10%) | 2509 (18%) | ||
| 3/29 | 101 (4%) | 669 (30%) | 743 (33%) | 554 (23%) | 226 (10%) | 2258 (16%) | ||
| 4/5 | 86 (5%) | 524 (29%) | 645 (36%) | 379 (21%) | 160 (9%) | 1794 (13%) | ||
| 4/12 | 101 (6%) | 550 (34%) | 516 (32%) | 315 (19%) | 139 (9%) | 1621 (12%) | ||
| 4/19 | 83 (6%) | 454 (34%) | 429 (32%) | 237 (18%) | 126 (9%) | 1329 (10%) | ||
| Column Total | 515 (4%) | 4078 (29%) | 4788 (34%) | 3221 (23%) | 1332 (10%) | 13934 (100%) | ||
| 4/26* | 131 (8%) | 542 (35%) | 531 (34%) | 219 (14%) | 131 (7%) | 1554 | ||
| 5/3* | 131 (11%) | 466 (39%) | 364 (30%) | 164 (14%) | 85 (7%) | 1210 | ||
| Column Total | 777 (4%) | 5086 (30%) | 5683 (34%) | 3604 (22%) | 1548 (9%) | 16698 |
*not included in chi square test
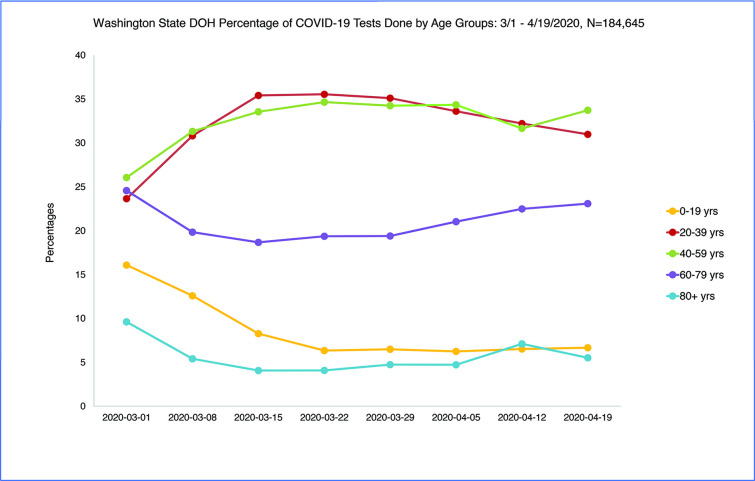
A total of 186,655 Covid-19 tests were run in Washington State from March 1 to April 19 2020 with 7.5% positive over the eight-week time period. Percent positive testing was variable over time and ranged from 12% (3/1/2020) to 5% (4/19/2020). Age distribution of persons tested changed by a small margin over time with an increase in testing among persons age 60 and older (+6%) and a decrease in testing among 0–19 and 20–39 year olds (-3%) from the peak (3/22/2020) to the week of 4/19/2020, a statistically significant but small change [chi square = 263.87, p < .001] (Fig 2) Table 2.
Fig 2. WA State DOH COVID-19 testing by age group: 3/1/2020-4/19/2020.
Table 2. WA State DOH testing by age group: 3/1/2020-4/19/2020 (n = 184645).
| Week | 0–19 N (%) | 20–39 N (%) | 40–59 N (%) | 60–79 N (%) | 80+ N (%) | Total | Chi-square | P value |
|---|---|---|---|---|---|---|---|---|
| 3/1 | 313 (16%) | 460 (24%) | 507 (26%) | 478 (25%) | 187 (10%) | 1945 (1%) | 263.87 | p < .001 |
| 3/8 | 2006 (13%) | 4911 (31%) | 4992 (31%) | 3162 (20%) | 863 (5%) | 15934 (9%) | ||
| 3/15 | 2231 (8%) | 9544 (35%) | 9041 (34%) | 5034 (19%) | 1098 (4%) | 26948 (15%) | ||
| 3/22 | 1832 (6%) | 10257 (36%) | 10000 (35%) | 5587 (19%) | 1177 (4%) | 28853 (16%) | ||
| 3/29 | 1825 (7%) | 9851 (35%) | 9611 (34%) | 5445 (19%) | 1331 (5%) | 28063 (15%) | ||
| 4/5 | 1681 (6%) | 9041 (34%) | 9235 (34%) | 5658 (21%) | 1273 (5%) | 26888 (15%) | ||
| 4/12 | 1612 (7%) | 7945 (32%) | 7807 (32%) | 5550 (22%) | 1753 (7%) | 24667 (13%) | ||
| 4/19 | 2094 (7%) | 9711 (31%) | 10572 (34%) | 7238 (23%) | 1732 (6%) | 31347 (17%) | ||
| Total | 13594 (7%) | 61720 (33%) | 61765 (34%) | 38152 (21%) | 9414 (5%) | 184645 |
From the first COVID-19 peak week, 3/22/2020, to week 4/19/2020, the COVID-19 hospitalization rate declined 49% for age 40 and older cases with a 54% decline in COVID-19 incidence. During the same time period, the hospitalization rate among age 20-39-year-olds declined 35% with a 36% decline in COVID-19 incidence [3].
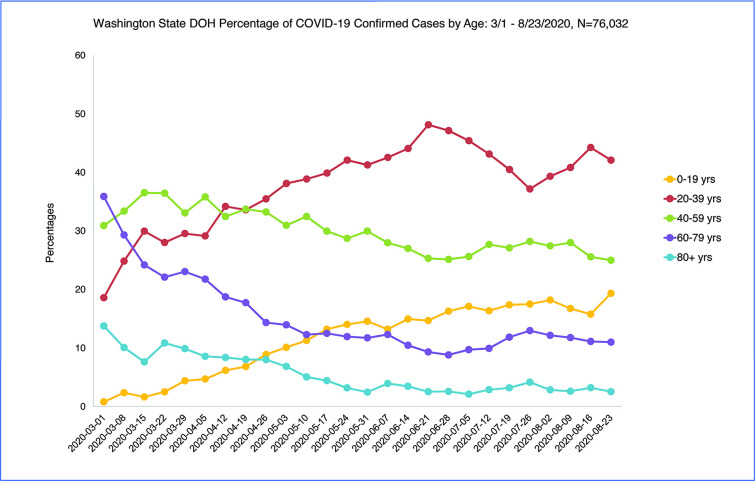
Over the longer time period of April to August 2020 the shift to younger age of COVID-19 confirmed positive cases continued to a sustained average of 60% of cases age less than 40 years June-August 2020 (N = 76,032) (Fig 3). The chi-square test for trend from April to August 2020 using the last week of each month comparing age of confirmed positive cases less than 40 to age 40 and older was significant indicating the slope was not zero over time [chi-square = 82.97, p < .001]. However, the chi-square test for trend for May to August 2020 was not significant indicating the proportion of cases less than age 40 reached a constant plateau in those months [chi-square = 1.41, p = .24].
Fig 3. WA State DOH confirmed cases by age 3/1/2020-8/23/2020.
Discussion
We analyzed trend over time from March to April and from March to August 2020. The first time period analysis was done when we had accurate testing data available from March to April and was done to determine that COVID-19 infections were present not just in older age persons but also in children and younger adults who over time became the highest incidence age group and continued to be the highest incidence age groups as the epidemic progressed. As testing expanded after the beginning of the epidemic (January/February 2020) when only symptomatic hospitalized patients were tested to any symptomatic patient testing (March/April 2020), the existence of infection in younger age groups became evident.
Following COVID-19 incidence by age over time as testing expanded it became evident all age groups were affected by COVID-19 infection and predominantly the most socially active, least likely to be symptomatic younger population. Although morbidity and mortality from COVID-19 infection is highest among the infected population age 60 years and older and those with underlying conditions, the percentage of 0–19 and 20-39-year-old cases in Washington State increased over time with no decline in COVID-19 incidence among 0-19-year-olds and 20-39-year-olds compared to older age groups when stay-at-home orders were enacted at the beginning of the epidemic. Our results show that a persistently high percentage of current infections in Washington State exist among the age 0–19 and 20–39 population who may also be at highest risk of contracting and spreading the virus but not at high risk of hospitalization or mortality. During the first time period from March to April 2020, COVID-19 related hospitalization rates declined without an equivalent rate of decline among confirmed COVID-19 cases.
The shift from older to younger population COVID-19 infection illustrates the absence of a true decline in cases in the first time period and instead a shift to COVID-19 test positive incidence among children and young adults. This changed the need for mitigation messaging and extended the need for health care capacity as the currently infected portion of the population is younger, less likely to report symptoms, at less risk of a severe life-threatening disease requiring hospitalization but fully capable of spreading disease to older, vulnerable adults. It appears persons 60 and older, those with pre-existing conditions and nursing home residents in particular were a harbinger of the serious nature of the epidemic but emphasis on infection in older adults only created a false dichotomy of risk at the beginning between young and old age. In Washington State 53% of the population is age 0–39 years, 25% 0–19 years and 28% aged 20–39, with King County the most populous county in the state [12].
From August 2 to September 5, 2020, weekly COVID-19 cases among persons aged 18–22 years increased 55% nationally with greatest increases in the Northeast (144%) and Midwest (123%). Increases in cases were not solely attributable to increased testing [13]. In Germany from March to April 2020, Goldstein et al report an observed relative increase of COVID-19 cases over time in 15–34 year olds compared to younger and older age groups [14]. In South Korea, people age 20–39 numerically led the epidemic although the elderly suffered the majority of morbidity and mortality [15]. In the southern United States documented regional outbreaks in June 2020, positive COVID-19 cases among 20–39 year-olds preceded increased incidence in older age groups with percentage of cases among 20–39 year-olds increasing over time (May-August 2020) [16]. Even though the largest percentage of cases are among younger age groups in the U.S., less than .3% of deaths are among 0–17 year-olds and 1.9% of deaths are among 18–39 year-olds [17]. In Washington State the percentage of deaths by age are similar with zero deaths 0–19 years of age and 2% of total deaths 20–39 years of age [18]. However, in a clinical profile of 3222 hospitalized young adults age 18–34 years in the United States, 18–34 year-olds did exhibit substantial rates of adverse outcomes although mortality remained low compared to older age groups at 2.7% [19].
As initial public warnings in Washington State and the nation targeted the population age 60 and older and those with underlying conditions, a misconception may have been at large that only persons age 60 and older were at risk for contracting COVID-19. Children were thought to be at low risk for COVID-19 and if infected to have a mild clinical course with few or no symptoms. However, a health alert was issued early in the epidemic by the CDC for Pediatric Multisystem Inflammatory System (MIS-C) linked to COVID-19 indicating serious morbidity risk exists although rare [20–23]. Documented outbreaks in WA State after Phase 2 reopening in 2020 included childcare, K-12 schools, and college/university settings [24].
Findings from a survey by Canning et al, found persons under age 50 had twice the predicted number of close contacts as persons 50 years and older [25]. In a recent Center for Disease Control (CDC) study of persons age 18–23, social interactions, workplace and community transmission contributed to the sharp increase in cases among young adults after a ‘Safer at Home Emergency Order’ was invalidated in the state of Wisconsin [26]. Misinformation and conflicting messaging influenced acceptance of and adherence to mitigation efforts. In a 2020 CDC survey study of engagement in mitigation behaviors, including handwashing, mask wearing and six-foot social distancing, adherence was lowest in those aged 18–29 years of age [27]. The CDC urges colleges and universities to actively promote healthy environments and adherence to recommended mitigation measures [28].
Although children and younger adults may not be at significant risk for serious COVID-19 related morbidity and mortality, evidence supports their ability to transmit disease and higher likelihood to have asymptomatic disease with silent transmission endangering others they come in contact with, especially older adults and those with comorbid conditions. In a CDC outbreak investigation, a single 13-year-old index case was traced to 11 subsequent cases [29]. A larger study of SARS-COV-2 infection in households in two states found when the index patient was less than age 12, secondary infection rate was 53% and for age 13–17 years, secondary infection rate was 38% with 75% of secondary infections occurring within a five-day window of index case symptoms [30]. From modelling studies, it is estimated only 21% of infected children age 10–19 years exhibit symptoms [31]. In a large cohort study in South Korea, 70% of 0–19, 63% of 20–29 and 60% of 30–39 year olds were asymptomatic [32]. In a study by Lee et al of SARS-CoV-2 molecular viral shedding of symptomatic and asymptomatic patients, virus shedding was similar between the two groups [33].
Limitations
While testing overall increased during the period evaluated, the percentage of younger people being tested decreased slightly compared to persons age 60 and older. Absent information to link family and household level data with parent’s occupation to identify the source of exposure in the 0-19-year-old age group, one could assume some infections are driven by contact with family members working outside of the home and social interaction as Washington State public schools have been closed since March 11, 2020 current to January 21, 2021. A study by the American Academy of Pediatrics found only 10 states reported testing by age further hampering the ability to evaluate level of COVID-19 disease incidence in the population by age [34]. Testing by age was only available for Washington State in the first time period of our analysis. The broad age categories of 0–19 years and 20–39 years used by WA State DOH do not allow for more specific analysis regarding transmission and mitigation recommendations. COVID-19 confirmed case positive are not reported by age linked to race in weekly online DOH data.
The Washington State stay-at-home policy is temporally associated with the first observed case decline after March 22, 2020 [35]. However, the decline was only among age 40 and above with no decline in children or younger adults and cases rose again to a second peak in June indicating a persistent transmission rate among the population less than age 40 resistant to public health mitigation efforts. After mask wearing became required in all public spaces in Washington State (June 8, 2020) another decline in cases was observed without a decline in the percentage of cases among children and younger adults all while schools in Washington State remained closed [36].
We document a shift of the majority of COVID-19 cases from older adults to children and younger adults over the eight-week time period after the state reached enough measurable cases to analyze on March 1, 2020. Further tracking of cases by age revealed a trend to majority COVID-19 infection among children and younger adults which continued upward to a sustained plateau regardless of fluctuations in statewide infection or testing rates. Our findings indicate justifiable concern regarding the health and safety of children and teenagers that led to the decision to delay reopening schools. The disproportionate spread of disease among younger adults influenced plans for phased reopening of Washington State counties which were paused at Phase II for most counties until reduced case incidence and disease control testing, tracking and tracing metrics were met [37] but were moved back to Phase I for the entire state due to increased COVID-19 incidence statewide in November 2020 [38, 39].
With the shift in COVID-19 incidence to a majority of current cases in the combined 0-19/20-39-year-old age group statewide, counties with a high percentage population age 0–19 and 20–39 years are more heavily affected. Continued tracking of age trends are warranted and will help target which activities can be opened safely and what extra safeguards and protocols will be required with monitoring for adherence.
We cite observational studies indicating younger persons are less likely to adhere to recommended mitigation behaviors. This is precisely why we conducted our study with our primary recommendation to tailor mitigation and other protection guidelines to meet the needs of all age groups. As the mitigation and stay at home orders in Washington State were initially targeted at persons age 60 and older and those with comorbid conditions regardless of age, the use of print media and television advertising were not tailored to reach young adults or children and their risk of morbidity and mortality was not emphasized.
While adherence to mitigation behaviors appear to have curbed disease spread for a time in older and more vulnerable adults, we have seen a dramatic increase in number of cases and morbidity and mortality from disease in the dark days of fall and winter in the United States. It is logical for mitigation behaviors to be more effective in those that adhere to them. The strategy to prevent morbidity and mortality is to address the issue of continued spread of the disease which in the case of COVID-19 requires focusing mitigation efforts on persons most likely to contract and spread the disease to contain the epidemic, in this case young adults and children as they appear to be the dominant reservoir of disease and not likely to be vaccinated in the current time period.
In the case of future epidemics, it is hoped early recognition of disease in all ages and races in the population would trigger multi-lingual, age-appropriate mitigation messaging to the entire population instead of targeting a singular group most at risk for morbidity and mortality exclusive of groups most at risk of spreading disease. It would also be hoped that consistent messaging from public health and governmental agencies would be coordinated to provide the basis for cohesive and successful messaging and mitigation.
Specific advisories tailored to children and adolescents age 0–19 years and 20-39-year-old adults to increase awareness of COVID-19 transmission and infection are advisable to reduce overall COVID-19 incidence levels and enhance movement towards levels that will allow a continuation of phased reopening of the state and counties. As of January 20, 2021, there are no vaccines approved for children 16 and under and adults age 20–39 are not on the CDC list for phased vaccination until after frontline essential workers, older age groups, persons with comorbid conditions and other essential workers are vaccinated [40]. Adults age 20–39 are more often employed in work sectors with high levels of public contact, more likely to be socially active and less likely to take social distancing and mask wearing precautions. Mitigation by low technical interventions will continue to be a priority for children and young adults including mask wearing, social distancing, hand washing, adequate ventilation, and crowd avoidance [41].
Modelling studies with real data simultaneously incorporating race and county location with more precise age categories would be a tremendous asset to targeting specific public health mitigation and vaccination strategies. Vaccination first priority will be for medical workers and vulnerable persons by age or condition with children and young adults a lower priority creating a continued if not elevated need for specific mitigation for years to come as we await herd immunity with full population COVID-19 vaccination achievement. As in-person education can be a vector for COVID-19 transmission to households and beyond and testing of school age children is not on par with older age groups due to lower incidence of symptomatic disease, re-opening schools for in-person learning should be approached with caution and an eye to general population COVID-19 infection and vaccination rates.
Acknowledgments
The authors wish to express their heartfelt thanks and gratitude for the invaluable assistance of Michelle Holshue, RN, MPH of the Washington State Department of Health and the CDC Epidemiologic Intelligence Service. The authors also wish to thank the Public Health staff in every county in Washington State and the Washington State Department of Health for their hard work collecting the data and their contribution to the Washington Disease Reporting System.
Data Availability
All excel files are available from the Washington State Department of Health database online at https://www.doh.wa.gov/Emergencies/COVID19/DataDashboard#downloads.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Holshue ML, DeBolt C, Lundquist S, et al. Washington State 2019-nCoV Case Investigation Team. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Governor of Washington, Proclamation by the Governor amending proclamation 20–05. https://www.governor.wa.gov/sites/default/files/proclamations/20-28.2%20-%20COVID-19%20Open%20Govt%20Waivers%20Ext%20%28tmp%29.pdf. Accessed May 5, 2020.
- 3.Malmgren J, Guo B, Kaplan HG. COVID-19 Confirmed Case Incidence Age Shift to Young Persons Age 0–19 and 20–39 Years Over Time: Washington State March—April 2020. medRxiv 2020.05.21.20109389; 10.1101/2020.05.21.20109389 [DOI] [Google Scholar]
- 4.Personal communication with the Washington State Department of Health, State Public Health Lab, COVID-19 Branch Manager, Denny Russel. March 5, 2021
- 5.CDC Has Fixed Issue Delaying Coronavirus Testing In U.S., Health Officials Say: Shots—Health News: NPR. https://www.npr.org/sections/health-shots/2020/02/27/809936132/cdc-fixes-issue-delaying-coronavirus-testing-in-u-s Accessed March 5, 2021.
- 6.UW Medicine deploys new, and needed, test for coronavirus (fredhutch.org). https://www.fredhutch.org/en/news/center-news/2020/03/new-covid19-lab-test.html. Accessed March 5, 2021.
- 7.https://www.doh.wa.gov/Emergencies/COVID19/DataDashboard#technical. Accessed January 21, 2021. [Google Scholar]
- 8.Washington State Department of Health, 2019. Novel Coronavirus Outbreak (COVID-19). Current Status in Washington State. 2020. Download May 4, 2020 and May 17, 2020. https://www.doh.wa.gov/Emergencies/Coronavirus. [Google Scholar]
- 9.Microsoft Excel Version 10. Microsoft Corporation Redmond WA. 2019.
- 10.Stangroom J. Chi-Square Test Calculator. Social Science Statistics. https://www.socscistatistics.com/tests/chisquare2/default2.aspx (accessed April 29, 2020). [Google Scholar]
- 11.Sergeant, ESG, 2018. Epitools Epidemiological Calculators. Ausvet. http://epitools.ausvet.com.au.
- 12.https://www.towncharts.com/Washington/Washington-state-Demographics-data.html. Accessed October 31, 2020
- 13.Salvatore PP, Sula E, Coyle JP, et al. Recent Increase in COVID-19 Cases Reported Among Adults Aged 18–22 Years—United States, May 31-September 5, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1419–1424. 10.15585/mmwr.mm6939e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldstein E, Lipsitch M. Temporal rise in the proportion of younger adults and older adolescents among coronavirus disease (COVID-19) cases following the introduction of physical distancing measures, Germany, March to April 2020. Euro Surveill 2020;25(17):pii200596. 10.2807/1560-7917.ES.2020.25.17.2000596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu X, Duan J, Jiang Y, Zhang H. Distinctive trajectories of the COVID-19 epidemic by age and gender: A retrospective modeling of the epidemic in South Korea. Int J Infect Dis 2020;98:200–205. 10.1016/j.ijid.2020.06.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boehmer TK, DeVies J, Caruso E, et al. Changing Age Distribution of the COVID-19 Pandemic—United States, May-August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1404–1409. 10.15585/mmwr.mm6939e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gold JA, Rossen LM, Ahmad FB, et al. Race, Ethnicity, and Age Trends in Persons Who Died from COVID-19—United States, May-August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1517–1521. 10.15585/mmwr.mm6942e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.https://www.doh.wa.gov/Emergencies/COVID19/DataDashboard#tables. Accessed October 31, 2020.
- 19.Cunningham JW, Vaduganathan M, Claggett BL, et al. Clinical Outcomes in Young US Adults Hospitalized With COVID-19. JAMA Intern Med. Published online September 9, 2020. 10.1001/jamainternmed.2020.5313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19) https://emergency.cdc.gov/han/2020/han00432.asp. Accessed May 15, 2020
- 21.Godfred-Cato S, Bryant B, Leung J, et al. COVID-19-Associated Multisystem Inflammatory Syndrome in Children—United States, March-July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1074–1080. 10.15585/mmwr.mm6932e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Health Department-Reported Cases of Multisystem Inflammatory Syndrome in Children (MIS-C) in the United States. https://www.cdc.gov/mis-c/cases/index.html. Accessed October 31, 2020.
- 23.Dingens AS, Crawford KHD, Adler A et al. Serological identification of SARS-CoV-2 infections among children visiting a hospital during the initial Seattle outbreak. Nat Commun 2020;11(4378). 10.1038/s41467-020-18178-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Washington State Department of Health. Statewide COVID-19 Outbreak Report 10/29/2020. https://www.doh.wa.gov/Portals/1/Documents/1600/coronavirus/StatewideCOVID-19OutbreakReport.pdf
- 25.Canning D, Karra M, Dayalu R, Guo M, Bloom DE. The association between age, COVID-19 symptoms, and social distancing behavior in the United States. medRxiv preprint, 18th April 2020. 10.1101/2020.04.19.20065219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson RF, Sharma AJ, Schluechtermann S, et al. Factors Influencing Risk for COVID-19 Exposure Among Young Adults Aged 18–23 Years-Winnebago County, Wisconsin, March-July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1497–1502. 10.15585/mmwr.mm6941e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hutchins HJ, Wolff B, Leeb R, et al. COVID-19 Mitigation Behaviors by Age Group—United States, April-June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1584–1590. 10.15585/mmwr.mm6943e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Colleges, universities, and higher learning. Updated October 16, 2020. Accessed November 12, 2020.https://www-cdc-gov.offcampus.lib.washington.edu/coronavirus/2019-ncov/community/colleges-universities/index.html.
- 29.Schwartz NG, Moorman AC, Makaretz A, et al. Adolescent with COVID-19 as the Source of an Outbreak at a 3-Week Family Gathering—Four States, June-July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1457–1459. 10.15585/mmwr.mm6940e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grijalva CG, Rolfes MA, Zhu Y, et al. Transmission of SARS-COV-2 Infections in Households—Tennessee and Wisconsin, April-September 2020. MMWR Morb Mortal Wkly Rep 2020;69:1631–1634. 10.15585/mmwr.mm6944e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davies NG, Klepac P, Liu Y, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med 2020;26:1205–1211. 10.1038/s41591-020-0962-9 [DOI] [PubMed] [Google Scholar]
- 32.Jung C-Y, Park H, Kim DW, et al. Clinical Characteristics of Asymptomatic Patients with COVID-19: A Nationwide Cohort Study in South Korea. Int J Infect Dis 2020;99:266–268. 10.1016/j.ijid.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee S, Kim T, Lee E, et al. Clinical Course and Molecular Viral Shedding Among Asymptomatic and Symptomatic Patients With SARS-CoV-2 Infection in a Community Treatment Center in the Republic of Korea. JAMA Intern Med. 2020;180(11):1447–1452. 10.1001/jamainternmed.2020.3862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.A joint report from the American Academy of Pediatrics and the Children’s Hospital Association. Children and COVID-19: State Data Report. Version 10/29/2020. Online accessed October 31, 2020. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- 35.Institute for Health Metrics. University of Washington, Seattle WA. Covid-19 Projections State of Washington. Accessed May 4, 2020 https://covid19.healthdata.org/united-states-of-america/washington
- 36.https://coronavirus.wa.gov/information-for/you-and-your-family/face-masks-or-cloth-face-covering. Accessed October 31, 2020.
- 37.https://www.governor.wa.gov/news-media/inslee-announces-updates-safe-start-reopening-plan. Accessed October 31, 2020.
- 38.https://www.governor.wa.gov/news-media/inslee-announces-statewide-restrictions-four-weeks. Accessed January 17, 2021.
- 39.https://www.governor.wa.gov/issues/issues/covid-19-resources/covid-19-reopening-guidance-businesses-and-workers. Accessed January 17, 2021.
- 40.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html Accessed January 20, 2021.
- 41.Lerner AM, Folkers GK, Fauci AS. Preventing the Spread of SARS-CoV-2 With Masks and Other “Low-tech” Interventions. JAMA. Published online October 26, 2020. 10.1001/jama.2020.21946 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All excel files are available from the Washington State Department of Health database online at https://www.doh.wa.gov/Emergencies/COVID19/DataDashboard#downloads.