Abstract
BACKGROUND AND PURPOSE:
Multigland disease represents a challenging group of patients with primary hyperparathyroidism. Additional lesions may be missed on imaging because they are not considered or are too small to be seen. The aim of this is study was to identify 4D-CT imaging and biochemical predictors of multigland disease.
MATERIALS AND METHODS:
This was a retrospective study of 155 patients who underwent 4D-CT and successful surgery with a biochemical cure that compared patients with multigland and single-gland disease. Variables studied included the size of the largest lesion on 4D-CT, the number of lesions prospectively identified on 4D-CT, serum calcium levels, serum parathyroid hormone levels, and the Wisconsin Index (the product of serum calcium and parathyroid hormone levels). Imaging findings and the Wisconsin Index were used to calculate a composite multigland disease scoring system. We evaluated the predictive value of individual variables and the scoring system for multigland disease.
RESULTS:
Thirty-six patients with multigland disease were compared with 119 patients with single-gland disease. Patients with multigland disease had significantly lower Wisconsin Index scores, smaller lesion size, and a higher likelihood of having either multiple or zero lesions identified on 4D-CT (P ≤ .01). Size cutoff of <7 mm had 85% specificity for multigland disease, but including other variables in the composite multigland disease score improved the specificity. Scores of ≥4, ≥5, and 6 had specificities of 81%, 93%, and 98%, respectively.
CONCLUSIONS:
The composite multigland disease scoring system based on 4D-CT imaging findings and biochemical data can identify patients with a high likelihood of multigland disease. Communicating the suspicion for multigland disease in the radiology report could influence surgical decision-making, particularly when considering re-exploration in a previously operated neck or initial limited neck exploration.
Preoperative parathyroid imaging is routinely performed in patients with primary hyperparathyroidism. In the era of minimally invasive parathyroidectomy, the role of imaging is to localize the parathyroid adenoma with high confidence for surgical planning. Although primary hyperparathyroidism is most commonly caused by a single parathyroid adenoma, 10%–30% of patients will have multigland disease (MGD) due to parathyroid hyperplasia or multiple adenomas.1,2 This group represents a challenge for radiologists and surgeons because these patients have a much higher frequency of nonlocalizing imaging studies and failed surgeries.2–4
The technique of multiphase multidetector CT, also known as 4D-CT, may be advantageous in patients with MGD. Several studies have shown 4D-CT to have higher sensitivity than sonography and scintigraphy for localizing abnormal parathyroid glands, due to higher spatial resolution for the detection of small lesions and an improved ability to visualize adenomas in deep or ectopic locations.4–7 Selected studies analyzed the subgroup of patients with MGD and found 4D-CT to be superior to sonography and scintigraphy, but the sensitivity of 4D-CT for MGD (32%–53%) was still considerably lower compared with single-gland disease (SGD) (88%–93%).4,5,7,8 None of the studies described characteristics of MGD and SGD or attempted to determine predictors of MGD.
Some of the barriers to lesion detection on 4D-CT for MGD include a smaller size than for SGD and overlooking additional lesions after detecting the first lesion. The latter pitfall could be minimized if the radiologist was aware of predictors for MGD that would lead to a more dedicated search for additional lesions. The aim of this study was to identify 4D-CT imaging and biochemical predictors of MGD in patients with primary hyperparathyroidism. Our hypothesis is that the combination of smaller lesion size on imaging and lower serum biochemical markers can predict MGD with high specificity.
Materials and Methods
Study Subjects
We performed a retrospective review of 155 patients from 2 academic institutions who had 4D-CT studies performed between October 2009 and December 2013 before successful parathyroid surgery. There were 87 patients from institution A (University of California, Los Angeles) and 68 from institution B (Duke University). Successful surgery was defined as an intraoperative parathyroid hormone (PTH) drop of >50% and at least 6 months of postoperative eucalcemia. Both institutions obtained institutional review board approval with a waiver of consent.
For all patients, medical records were reviewed for patient demographics, history of prior surgery, operative notes, pathology results, imaging findings on 4D-CT, and preoperative serum calcium and PTH levels.
4D-CT Technique
Institution A.
Imaging was performed either on a 64–detector row scanner (Somatom Definition; Siemens, Erlangen, Germany) or a 256–detector row scanner (Somatom Definition Flash; Siemens). Scanning included noncontrast, arterial phase, and delayed phase images from the hard palate to the carina. The parameters for all 3 phases were the following: section thickness, 0.6 mm; tube rotation time, 0.5 seconds; pitch factor, 1; FOV, 24 cm; 120 kV(peak); 230 reference milliampere-second with automated tube current modulation (CARE Dose4D; Siemens). Arterial phase images were performed 25 seconds following the initiation of a 100- to 120-mL IV bolus of iohexol, 350-mg iodine/mL (Omnipaque; GE Healthcare, Piscataway, New Jersey), injected through either a 20- or 22-ga antecubital catheter, at either 4 or 3 mL/s. The delayed phase was acquired 30 seconds after the arterial phase ended. All images were reconstructed at 1-mm section thickness in the axial, coronal, and sagittal planes and sent to the PACS.
Institution B.
Imaging was performed by using a 64–detector row CT scanner (750 HD; GE Healthcare, Milwaukee, Wisconsin) with 3 imaging phases. Scanning included noncontrast, arterial phase, and delayed phase images. The noncontrast phase covered only the thyroid gland (z-axis from the hyoid bone to the clavicular heads) to reduce radiation exposure. The 2 contrast-enhanced phases were scanned from the angle of the mandible to the carina. The parameters for all 3 phases were the following: 0.625-mm section thickness; tube rotation time, 0.4 seconds; pitch factor, 0.516:1; FOV, 20 cm; 120 kVp; and automatic tube current modulation. Tube current modulation (mA Modulation; GE Healthcare) was used with a noise index of 8, minimum 100 mA, and maximum 500 mA for the nonenhanced and delayed phases and 700 mA for the arterial phase. Arterial phase images were obtained 25 seconds following initiation of an injection of 75 mL of intravenous iopamidol (Isovue 300; Bracco, Princeton, New Jersey) through a 20-ga antecubital catheter at a rate of 4 mL/s, followed by a 25-mL saline chaser. The delayed phase was acquired 80 seconds from the start of the injection. Before September 2012, studies were performed with only arterial and delayed phases.9 Reformatted images were sent to a PACS as 2.5-mm-thick contiguous images in the axial plane for all 3 phases, and 2.5-mm-thick images in the coronal and sagittal planes in the arterial and delayed phases.
Lesion Localization
All parathyroid lesions were classified as correctly or incorrectly localized on 4D-CT by correlating the operative notes with the original radiology reports and using anatomic landmarks reported in both the operative and radiology reports. Radiology reports were generated by 2 board-certified neuroradiologists (9 and 12 years' experience in CT interpretation). Sensitivities for lesion localization were based on these original radiology reports. If surgically confirmed lesions were missed on 4D-CT, the images were rereviewed by the 2 radiologists with knowledge of the surgical findings to determine whether lesions could be seen in retrospect.
Predictors of Multigland Disease
4D-CT imaging and biochemical predictors of MGD were proposed on the basis of prior surgical literature.10,11 4D-CT imaging predictors were the number of lesions identified on the original radiology report and lesion size (maximum diameter in any plane). If multiple candidates were seen on 4D-CT, lesion size was represented by the largest prospectively identified lesion. Biochemical predictors were serum calcium levels (milligram/deciliter), serum PTH levels (picogram/milliliter), and the Wisconsin Index (WIN). The WIN is the product of the serum calcium levels (milligram/deciliter) and PTH levels (picogram/milliliter) and was shown to help discriminate MGD and SGD in a prior study.10
A composite MGD score was derived on the basis of 4D-CT imaging and biochemical data of lesion size on 4D-CT, number of prospectively detected lesions on 4D-CT, and the WIN. Each variable contributed up to 2 points to the MGD scores (Table 1). The cutoff values used to assign points in the score were based on prior literature for lesion size and ranges of biochemical markers.10,12 A second scoring system, the 4D-CT MGD score, was based on only the 4D-CT imaging variables of lesion size and the number of prospectively detected lesions on 4D-CT. The composite MGD score ranged from 0 to 6. The 4D-CT MGD score ranged from 0 to 4. For both scoring systems, a higher score more strongly favored MGD.
Table 1:
MGD scoresa
| Criterion | Scoring |
|---|---|
| No. of candidate lesions identified on 4D-CT | Single lesion: 0 |
| Multiple lesions: 2 | |
| No lesions: 2 | |
| Maximum diameter of largest lesion on 4D-CT | >13 mm: 0 |
| 7–13 mm: 1 | |
| <7 mm or no lesion identified: 2 | |
| WIN | >1600: 0 |
| 800–1600: 1 | |
| <800: 2 |
Note:—WIN indicates serum calcium level (milligram/deciliter) × serum parathyroid hormone level (picogram/milliliter).
The composite MGD score includes all 3 components in the Table and ranges from 0 to 6. The 4D-CT MGD score does not include the Wisconsin Index and ranges from 0 to 4.
Data Analysis
The characteristics of MGD were compared with those of SGD for individual variables and the scoring system. The Fisher exact test was used to assess differences in patients with MGD and SGD for categoric data. The Student t test was used to assess differences between MGD and SGD for continuous variables. Receiver operating characteristic (ROC) analysis was performed to determine the sensitivity and specificity of each feature for predicting MGD. P values of <.05 were the threshold used for statistical significance for all tests. The data were entered into an Excel spreadsheet (2007 version; Microsoft, Redmond, Washington). Statistical analyses were performed by using SAS Enterprise (Version 4.2; SAS Institute, Cary, North Carolina).
Results
Study Subjects
Of the 155 patients, 36 had MGD (23 from institution A and 13 from institution B) and 119 had SGD (64 from institution A and 55 from institution B) (Table 2). There were 97 abnormal glands in patients with MGD, resulting in 216 abnormal glands in this study. The mean gland size was 11 ± 6 mm, and the median size was 10 mm (interquartile range, 7–13).
Table 2:
Characteristics of patients with MGD and SGDa
| All subjects | MGD | SGD | P Value | |
|---|---|---|---|---|
| No. of patients | 155 | 36 | 119 | |
| No. of glands | 216 | 97 | 119 | |
| Mean age (yr) | 60 (range, 14–88) | 59 | 60 | |
| Female | 108 (67%) | 25 (69%) | 83 (70%) | |
| 4D-CT characteristics | ||||
| Mean size of abnormal glands (mm) | 10.9 (5.9) | 8.8 (4.0) | 11.7 (6.4) | .002 |
| Median size of abnormal glands (mm) (IQR) | 10 (7–13) | 8 (6–11) | 11 (7–13) | |
| No. <10 mm (%) | 79 (37%) | 39 (64%) | 40 (34%) | |
| No. <7 mm (%) | 30 (14%) | 19 (31%) | 11 (9%) | |
| No. >13 mm (%) | 39 (18%) | 6 (10%) | 33 (28%) | |
| Prospectively detected lesions | ||||
| 1 | 100 | 10b | 90 | <.001 |
| ≥2 | 46 | 20 | 26 | |
| None | 9 | 6 | 3 | |
| Biochemical markers | ||||
| Serum calcium level (mg/dL) | 11.0 (0.7) | 10.8 (0.4) | 11.1 (0.7) | .07 |
| Serum parathyroid hormone level (pg/mL) | 117 (69) | 92 (44) | 122 (73) | .02 |
| WIN | 1279 (744) | 1005 (501) | 1357 (783) | .01 |
| MGD scores | ||||
| Composite MGD score | 2.6 (1.6) | 4.1 (1.4) | 2.2 (1.4) | <.001 |
| 4D-CT MGD score | 1.6 (1.4) | 2.9 (1.1) | 1.2 (1.2) | <.001 |
| 4D-CT sensitivity based on original radiology reports | ||||
| Detection of lesions | 167 (77%) | 53 (55%) | 114 (95%) | |
| Detection of all lesions in individual patients | 126 (81%) | 12 (33%) | 114 (95%) |
Note:—IQR indicates interquartile range.
Values are expressed as mean (SD) except as specified.
Twenty-five patients with MGD showed multiple lesions, and 5 showed single lesions after rereview of imaging studies following surgery.
Prior parathyroid surgery had been performed in 9 (25%) patients with MGD and 34 (29%) with SGD. The leading cause of persistent or recurrent hyperparathyroidism in our group was a missed single adenoma. The Fisher exact test showed no significant difference between MGD and SGD with respect to whether prior surgery had been performed (P = .83).
Lesion Localization
Of the 97 abnormal glands seen in 36 patients with MGD, 53 (55%) were identified prospectively and an additional 9 (9%) could be identified in retrospect. The others could not be detected even with knowledge of the surgical findings. Institution A prospectively identified 55% (36/65) of abnormal glands in the setting of MGD. Institution B prospectively identified 53% (17/32) of abnormal glands in the setting of MGD. The sensitivity of detecting all MGD lesions in a patient was 35% (8/23) for Institution A and 31% (4/13) for Institution B.
Of abnormal glands in patients with SGD, 95% (113/119) were identified prospectively. Institution A prospectively identified 95% (62/65) of glands with SGD. Institution B prospectively identified 94% (51/54) of glands with SGD. Of the 6 abnormal glands in SGD that were not identified prospectively, 4 could be identified in retrospect. The missed lesions not seen in retrospect were typically juxtathyroid in location. It is not clear whether they were not seen due to the small size or poor contrast between the adenoma and surrounding tissues.
Predictors of Multigland Disease
MGD had a smaller mean lesion size of 9 mm compared with 12 mm for SGD (P = .002). The WIN was lower for MGD at 1005 compared with 1357 for SGD (P = .01). Statistically significant differences were also seen for the number of lesions identified prospectively (P < .001) and serum PTH levels (P = .02).
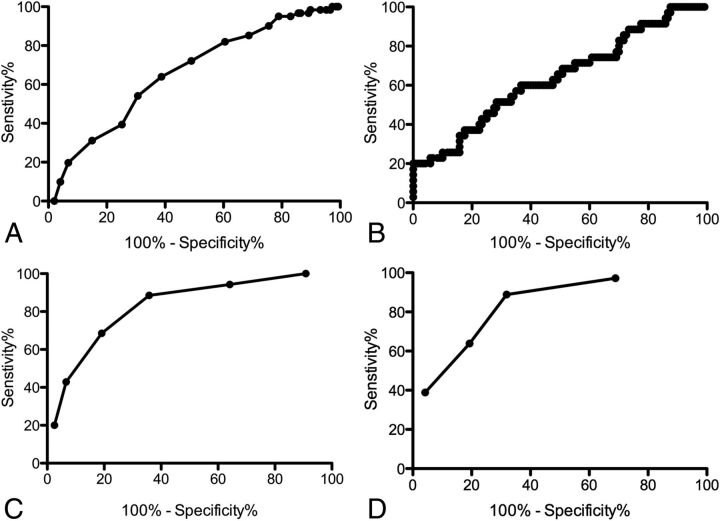
Despite significant differences between MGD and SGD with respect to multiple continuous variables, ROC analyses of each of these individual variables did not find clinically useful cutoff values. Areas under the ROC curves were <0.66 (Fig 1A, -B). Prospective identification of either multiple or no abnormal glands (rather than a single gland) was 76% sensitive and 72% specific for MGD. Using the median lesion size of ≤10 mm as a size cutoff was only 64% sensitive and 61% specific for MGD.
Fig 1.
Receiver operating characteristic curves showing performance in predicting MGD for the largest lesion size (A), Wisconsin Index (B), the composite MGD score (C), and the 4D-CT MGD score (D).
Cutoff values of 7 and 13 mm used for the scoring systems had higher specificity for MGD and SGD, respectively. A lesion size of <7 mm had a high specificity of 85% for MGD. Conversely, a lesion size of >13 mm had a high specificity for SGD of 85%. The <7 and >13 mm cutoff values both had a low sensitivity of 31%. A WIN of <661 had 90% specificity for MGD but only 26% sensitivity. Similarly, a WIN of >1629 had 91% specificity for SGD but only 23% sensitivity.
The mean composite MGD score was significantly higher for MGD at 4.1 compared with 2.2 for SGD (P < .001), with an improved area under the ROC curve of 0.82 (Fig 1C). 4D-CT MGD scores were similarly strongly predictive of MGD (P < .001), with an area under the ROC curve of 0.83 (Fig 1D). In the subset of patients without a history of prior surgery, the mean composite MGD score was 4.4 in MGD and 2.4 in SGD (P < .001), while the mean 4D-CT MGD score was 3.1 in MGD and 1.6 in SGD (P < .001). The sensitivities, specificities, and positive predictive values for MGD versus SGD based on the composite MGD and 4D-CT MGD scores are shown in Tables 3 and 4. High composite MGD scores of ≥4, ≥5, and 6 had specificities of 81%, 93%, and 98%, respectively, for predicting MGD.
Table 3:
Performance of the composite MGD score for predicting MGD on the basis of the size of the largest lesion, the number of lesions prospectively identified, and the Wisconsin Indexa
| MGD Score | No. of Patients | Sensitivity | Specificity | Positive Predictive Value |
|---|---|---|---|---|
| ≥1 | 35 | 100% | 9% | 24% |
| ≥2 | 33 | 94% | 36% | 30% |
| ≥3 | 31 | 89% | 64% | 43% |
| ≥4 | 24 | 69% | 81% | 51% |
| ≥5 | 15 | 43% | 93% | 65% |
| 6 | 7 | 20% | 98% | 70% |
There were no patients with scores of zero. One patient did not have recent serologic data.
Table 4:
Performance of the 4D-CT MGD score for predicting MGD, based on the size of largest lesion and the number of lesions prospectively identified
| MGD Score | No. of Patients | Sensitivity | Specificity | Positive Predictive Value |
|---|---|---|---|---|
| 0 | 36 | 100% | 0% | 23% |
| ≥1 | 35 | 97% | 31% | 30% |
| ≥2 | 32 | 89% | 68% | 46% |
| ≥3 | 23 | 64% | 81% | 50% |
| 4 | 14 | 39% | 96% | 74% |
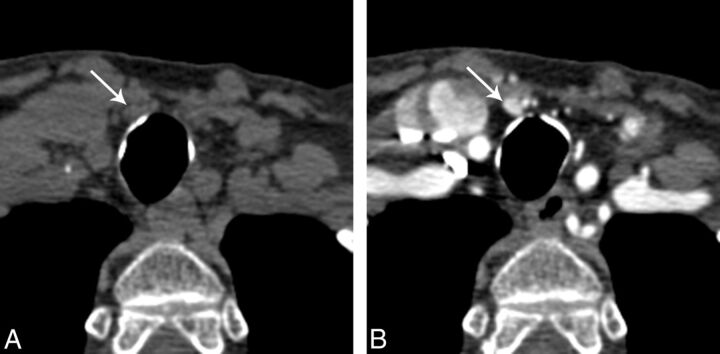
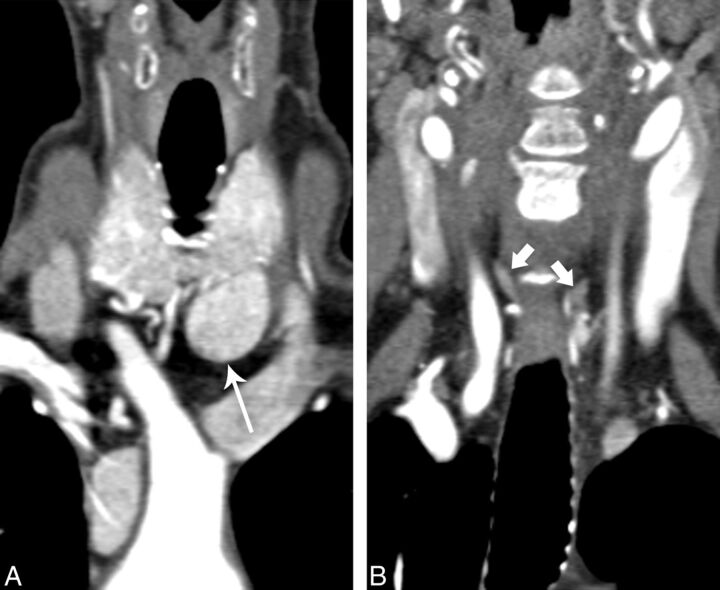
Figures 2 and 3 illustrate how the multifactorial composite MGD score can guide interpretation. Figure 2 shows an example of MGD in the setting of only a single prospectively identified lesion, but with a composite MGD score of 4 due to small lesion size and mild biochemical disease. Figure 3 shows an example of SGD in the setting of multiple candidate lesions but a low MGD score of 2.
Fig 2.
A 78-year-old woman with multigland disease, with a single small candidate lesion. A, Axial noncontrast CT just inferior to the thyroid gland shows a 6-mm nodule just deep to the strap muscles on the right (arrow). B, Axial arterial phase CT scan shows intense enhancement of this nodule. The serum calcium level was 10.1, and the serum parathyroid hormone level was 76. Despite identification of only a single lesion with 4D-CT, the composite MGD score was 4, and the probability of multigland disease was moderate. Surgical exploration revealed hyperplasia of the gland seen here and also hyperplastic bilateral superior parathyroid glands, neither of which could be seen even in retrospect.
Fig 3.
A 67-year-old woman with single-gland disease with multiple prospective candidate lesions. A, Coronal arterial phase CT image shows an intensely enhancing nodule in an orthotopic left inferior gland location (long arrow), measuring 20 mm in diameter. B, Coronal arterial phase CT image posterior to A, viewed in the same window width/level, shows ovoid nodular lesions in the orthotopic right and left superior positions (short arrows). Despite appropriate location and shape, these lesions show less intense enhancement than is typical of parathyroid adenoma. The serum calcium level is 11.7, and the serum parathyroid hormone level is 211. Despite the presence of multiple candidate lesions, the composite MGD score is only 2 and the findings are predictive of single-gland disease.
Discussion
Identifying cases of MGD preoperatively is an important role of parathyroid imaging when considering whether to offer minimally invasive parathyroidectomy rather than traditional bilateral neck exploration as an initial operation. In potential reoperation cases, MGD poses particular challenges due to distorted anatomy and scar tissue, and appropriate preoperative suspicion is essential in guiding surgical decision-making and preoperative counseling. Although prior studies using 4D-CT have described a range of sensitivities and specificities for MGD, typically superior to scintigraphy and sonography, no existing studies compare the imaging characteristics of MGD and SGD on 4D-CT.4–8,13 In this study, we found that a size threshold of <7 mm on 4D-CT favors MGD over SGD, but additional imaging and biochemical data can be used to calculate MGD scores and identify a subset of patients with a high likelihood of MGD.
In clinical practice, radiologists will first suspect MGD on the basis of detection of >1 candidate lesion for hyperplastic glands or adenoma. Our study found that identifying multiple lesions on 4D-CT is neither sensitive nor specific for MGD. Almost one-quarter of patients with MGD only had 1 gland seen prospectively (false-negative), while more than one-quarter of patients with SGD had additional less suspicious candidate lesions (false-positive). Thus, the sign of multiple lesions is not sufficient to guide clinical decision-making, and additional criteria are needed for the radiologist to call MGD with confidence.
Another imaging sign of MGD on 4D-CT is smaller lesion size than that in SGD, which corroborates previous reports based on pathology findings.10 A single cutoff value based on the mean or median lesion size was not helpful, but categorization of lesions by <7 and >13 mm had higher specificity (85%) for predicting and excluding MGD, respectively. Using size alone is limited for predicting MGD in most patients, however, who have lesions between 7 and 13 mm. Our MGD prediction model improves the ability to predict MGD in more patients by using size in combination with other variables. Our study found that composite MGD scores of ≥4, ≥5, and 6 had specificities of 81%, 93%, and 98%, respectively, and could be applied to more patients than a size cutoff of <7 mm. The composite MGD score was also an improvement over biochemical data alone. The cutoff values for WIN that were required to achieve high specificity for either MGD or SGD resulted in very low sensitivities.
The sensitivities for predicting MGD were low for composite MGD scores ≥4, but the scoring system does not aim to detect all patients with MGD. The primary aim is to identify a subset of patients in whom MGD should be suspected. One clinical implication to the radiologist is that a higher composite MGD score may prompt the radiologist to search for additional lesions after the first lesion is found, thereby avoiding “satisfaction of search” errors. However, the radiologist should be aware that even on detailed review, it may not be possible to see the additional lesions; a third of MGD lesions in our study could not be seen on 4D-CT, even with knowledge of the surgical findings. In the setting in which there is a single lesion but a high composite MGD score (ie, small lesion and relatively low serum PTH and calcium levels), the radiologist should still communicate the increased probability of MGD. The surgeon can use this information to counsel the patient about parathyroidectomy. Conversely, when >1 lesion is seen in a patient with a low composite MGD score (ie, a large lesion and high serum PTH and calcium levels), additional smaller lesions can be reported as much less suspicious if they are not clearly abnormal.
Previous clinical models for MGD have also emphasized the value of high specificity rather than high sensitivity.10,14 Kebebew et al14 proposed a multifactorial model based on serum calcium levels, serum PTH levels, and concordant-versus-discordant results of sonography and scintigraphy. Mazeh et al10 proposed a multifactorial model for predicting MGD with high specificity, by using a combination of WIN and the weight of the resected parathyroid lesion. Our scoring system offers advantages over these models, which did not include imaging signs and were only helpful to the surgeon for decision-making after imaging was complete, or intraoperatively.
We proposed 2 scoring systems to predict MGD and found both to have similar results in predicting it. For the radiologist, the 4D-CT MGD score has the advantage of using only imaging findings, but the composite MGD score may be more reproducible and reliable. This possibility is because the 4D-CT MGD score is based on only 2 sets of data, lesion size and the ability to visualize additional lesions. The latter characteristic may be interpreted with high interobserver variability because the second lesion may be overlooked if not suspected. In contrast, lesion size and biochemical markers are objective criteria.
There were several limitations to this study. First, this was a retrospective study from 2 academic institutions with 2 different neuroradiologists interpreting the original 4D-CT examinations. There were minor technical differences between the acquisition and reconstruction parameters from the 2 institutions, but imaging protocols were alike with regard to the number of phases acquired and timing of the arterial phase, which we believe are the most important controllable factors. Both institutions achieved similar interpretation accuracy for both SGD and MGD, which is reassuring for confirming the external validity of the data. Second, the characteristics of the lesions were based on the original radiology reports. We did not re-interpret the imaging because we thought there would be recall bias. The fact that we did not re-interpret the imaging studies under blinded conditions is potentially a confounding factor because the original radiology reports were often influenced by clinical information such as surgical history and data from previous sonography and scintigraphy results. However, the use of the original reports is, to some extent, a strength of this study because it reflects the performance of 4D-CT under true clinical conditions. A third potential limitation is the heterogeneity of the study group with respect to whether prior surgery was performed. In theory, there may be differences between patients undergoing initial surgery and those undergoing a reoperation with respect to the presence of MGD, particularly because undertreated MGD is a cause of failed parathyroidectomy. However, these differences did not appear to be a confounding factor in our study. Patients undergoing reoperation were distributed between SGD and MGD in a proportion similar to that of patients undergoing initial exploration, and a missed single adenoma was the leading cause of recurrent/persistent hyperparathyroidism in our group, which was in keeping with findings in the existing literature.15,16 Given the importance of determining the probability of MGD in the setting of a potential reoperation, it is essential to include these patients in the analysis.
Conclusions
4D-CT imaging findings of lesion size and the number of lesions detected can be combined with biochemical data to calculate a composite MGD score. The scoring system can help determine the overall probability of MGD, even if only 1 lesion is detected, and can identify a subset of patients with a high likelihood of MGD. Communicating the suspicion for MGD in the radiology report could influence surgical decision-making, particularly when considering re-exploration in a previously operated neck or initial limited neck exploration.
ABBREVIATIONS:
- MGD
multigland disease
- PTH
parathyroid hormone
- ROC
receiver operating characteristic
- SGD
single-gland disease
- WIN
Wisconsin Index
REFERENCES
- 1. Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 2005;132:359–72 [DOI] [PubMed] [Google Scholar]
- 2. Fraker DL, Harsono H, Lewis R. Minimally invasive parathyroidectomy: benefits and requirements of localization, diagnosis, and intraoperative PTH monitoring: long-term results. World J Surg 2009;33:2256–65 [DOI] [PubMed] [Google Scholar]
- 3. Hoang JK, Sung WK, Bahl M, et al. How to perform parathyroid 4D CT: tips and traps for technique and interpretation. Radiology 2014;270:15–24 [DOI] [PubMed] [Google Scholar]
- 4. Rodgers SE, Hunter GJ, Hamberg LM, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery 2006;140:932–40; discussion 940–41 [DOI] [PubMed] [Google Scholar]
- 5. Kukar M, Platz TA, Schaffner TJ, et al. The use of modified four-dimensional computed tomography in patients with primary hyperparathyroidism: an argument for the abandonment of routine sestamibi single-positron emission computed tomography (SPECT). Ann Surg Oncol 2015;22:139–45 [DOI] [PubMed] [Google Scholar]
- 6. Eichhorn-Wharry LI, Carlin AM, Talpos GB. Mild hypercalcemia: an indication to select 4-dimensional computed tomography scan for preoperative localization of parathyroid adenomas. Am J Surg 2011;201:334–38; discussion 338 [DOI] [PubMed] [Google Scholar]
- 7. Galvin PL, Oldan J, Bahl M, et al. Discordant parathyroid 4DCT and scintigraphy results: what factors contribute to missed parathyroid lesions? In: Proceedings of the Annual Meeting of the American Society of Neuroradiology and the Foundation of the ASNR Symposium, Montreal, Quebec, Canada. May 17–22, 2014 [Google Scholar]
- 8. Sepahdari AR, Yeh MW, Rodrigues D, et al. Three-phase parathyroid 4-dimensional computed tomography initial experience: inexperienced readers have high accuracy and high interobserver agreement. J Comput Assist Tomogr 2013;37:511–17 [DOI] [PubMed] [Google Scholar]
- 9. Gafton AR, Glastonbury CM, Eastwood JD, et al. Parathyroid lesions: characterization with dual-phase arterial and venous enhanced CT of the neck. AJNR Am J Neuroradiol 2012;33:949–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mazeh H, Chen H, Leverson G, et al. Creation of a “Wisconsin index” nomogram to predict the likelihood of additional hyperfunctioning parathyroid glands during parathyroidectomy. Ann Surg 2013;257:138–41 [DOI] [PubMed] [Google Scholar]
- 11. McCoy KL, Chen NH, Armstrong MJ, et al. The small abnormal parathyroid gland is increasingly common and heralds operative complexity. World J Surg 2014;38:1274–81 [DOI] [PubMed] [Google Scholar]
- 12. Siperstein A, Berber E, Barbosa GF, et al. Predicting the success of limited exploration for primary hyperparathyroidism using ultrasound, sestamibi, and intraoperative parathyroid hormone: analysis of 1158 cases. Ann Surg 2008;248:420–28 [DOI] [PubMed] [Google Scholar]
- 13. Starker LF, Mahajan A, Bjorklund P, et al. 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Ann Surg Oncol 2011;18:1723–28 [DOI] [PubMed] [Google Scholar]
- 14. Kebebew E, Hwang J, Reiff E, et al. Predictors of single-gland vs multigland parathyroid disease in primary hyperparathyroidism: a simple and accurate scoring model. Arch Surg 2006;141:777–82; discussion 782 [DOI] [PubMed] [Google Scholar]
- 15. Shen W, Duren M, Morita E, et al. Reoperation for persistent or recurrent primary hyperparathyroidism. Arch Surg 1996;131:861–67; discussion 867–69 [DOI] [PubMed] [Google Scholar]
- 16. Udelsman R, Donovan PI. Remedial parathyroid surgery: changing trends in 130 consecutive cases. Ann Surg 2006;244:471–79 [DOI] [PMC free article] [PubMed] [Google Scholar]