Abstract
Background
The diagnosis of antiphospholipid syndrome (APS) requires the presence of thrombosis and/or recurrent miscarriages along with one or more anti-phospholipid antibodies (aPL). The role of aPL has been largely investigated in systemic lupus erythematosus (SLE) with minimal data on other autoimmune rheumatic diseases. In this review, we aim to assess the prevalence of aPL in patients with inflammatory and autoimmune rheumatic and musculoskeletal diseases (RMDs) other than SLE, and their association with thrombosis.
Results
A total of 20 studies, including 3242 patients, measured aPL in different inflammatory and autoimmune RMDs. The overall median percentage of aPL-positive patients was 14.05% (from 0 to 57.5%). For systemic sclerosis (SSc) patients, the median positivity was 14.05% for aPL, with IgG aCL being detected in up to 35.48% of all SSc aPL-positive patients. Only six studies (30%) performed an antibody confirmation test after 12 weeks, with the median prevalence being 10.88% (from 0 to 29.79%). Only six studies also assessed the number of double or triple aPL-positive patients. A total of eight (40%) studies including 1071 patients investigated the association between aPL and thrombotic events, namely five for SSc, one for SS, one for ANCA associated vasculitides (AAV), and one for RA. A median of 18.75% (7.69–71.43%) of aPL-positive patients experienced an arterial event in comparison to a median of 13.66% (7.69–31.25%) who underwent venous thrombotic event. Taking into consideration only the studies that performed a confirmation test, a median value of 34.36% (12.9–71.43%) of aPL-positive patients underwent an arterial event and a median value of 16.32% (9.68–25%) of aPL-positive patients underwent a venous event.
Conclusions
Anti-phospholipid antibodies can be detected in up to a third of patients with inflammatory and autoimmune RMDs, especially in SSc. However, there was a large heterogeneity among the retrieved studies. Available data supporting a general screening for aPL in all inflammatory and autoimmune RMDs are still insufficient. Screening for aPL in selected scenarios (e.g., pregnancy planning) could be considered.
Keywords: Antiphospholipid antibodies, Connective tissue diseases, Prevalence, Thrombosis
Key Summary Points
| Antiphospholipid antibodies can be detected in up to a third of patients with inflammatory and autoimmune rheumatic diseases, especially in systemic scleroderma. |
| Although the association between antiphospholipid antibodies and thromboembolism has been observed in few studies, there are not enough data to support routine screening for antiphospholipid antibodies in all the rheumatic diseases other than lupus. |
| In some circumstances, such as pregnancy planning and thrombosis in the context a rheumatic disease, screening for antiphospholipid antibodies might be indicated. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to 10.6084/m9.figshare.13415897.
Introduction
Antiphospholipid syndrome (APS) is characterized by vascular thrombosis, pregnancy morbidity, and the detection of one or more anti-phospholipid antibodies (aPL) [1]. Laboratory tests for aPL recommended by the current classification criteria include those for anticardiolipin antibodies (aCL), lupus anticoagulant (LAC), and anti-β2-glycoprotein I antibodies (anti-β2GPI) [2]. APS can occur isolated (known as primary APS) or secondary to connective tissue diseases (CTD), mainly systemic lupus erythematosus (SLE) [3–5].
While it is not unusual in clinical practice to attend patients with autoimmune rheumatic and musculoskeletal diseases (RMDs) other than SLE who tested positive for aPL, the clinical meaning of these findings needs further investigation. Separate studies have shown that aPL could be present in patients with RMDs other than SLE. However, no previous systematic reviews have assessed the prevalence of aPL in most RMDs other than SLE, although certain systematic reviews focused on one disease [6]. It is worth mentioning that the implication of aPL in the pathophysiology of such RMDs other than SLE is still unknown.
Indeed, testing for aPL in all the RMDs to include systemic scleroderma (SSc) [7, 8], Sjögren’s syndrome (SS) [9], and rheumatoid arthritis (RA) [10] patients is not globally part of the routine standard of care [11].
Objectives
This systematic review aims to estimate the prevalence of aPL in inflammatory and autoimmune RMDs other than SLE. Secondly, we investigate the association of the positivity of aPL with thrombotic events.
Methods
Search Methods
A PubMed/MEDLINE search was conducted with keywords specifying the connective tissue diseases “systemic sclerosis, “scleroderma”, “rheumatoid arthritis”, “Sjögren”, “mixed connective tissue disease”, “undifferentiated connective tissue disease”, “vasculitis”, “Churg–Strauss”, “eosinophilic granulomatosis with polyangiitis”, “Wegner’s granulomatosis”, “granulomatosis with polyangiitis”, “polymyositis”, and “dermatomyositis” being added to the keywords “antiphospholipid” or “APS”.
All the cohort studies, cross-sectional studies, case–control studies, and randomized clinical trials reporting the prevalence of aPL in RMDs other than SLE were selected. Additionally, reference lists of selected manuscripts were checked manually for eligible articles. All articles not indexed on PubMed/MEDLINE were not included. Ongoing trials registers were also not included.
Selection Criteria
A pair of authors independently selected studies for inclusion. All studies performed since December 2007, excluding case reports, were included regardless of the inherent bias of individual studies and the total number of study individuals (N). The period from 2007 was chosen since most studies at that time started including anti-β2GPI as an aPL after the generation of the Sydney criteria in 2006 [1]. The study period spanned from December 2007 until January 2020.
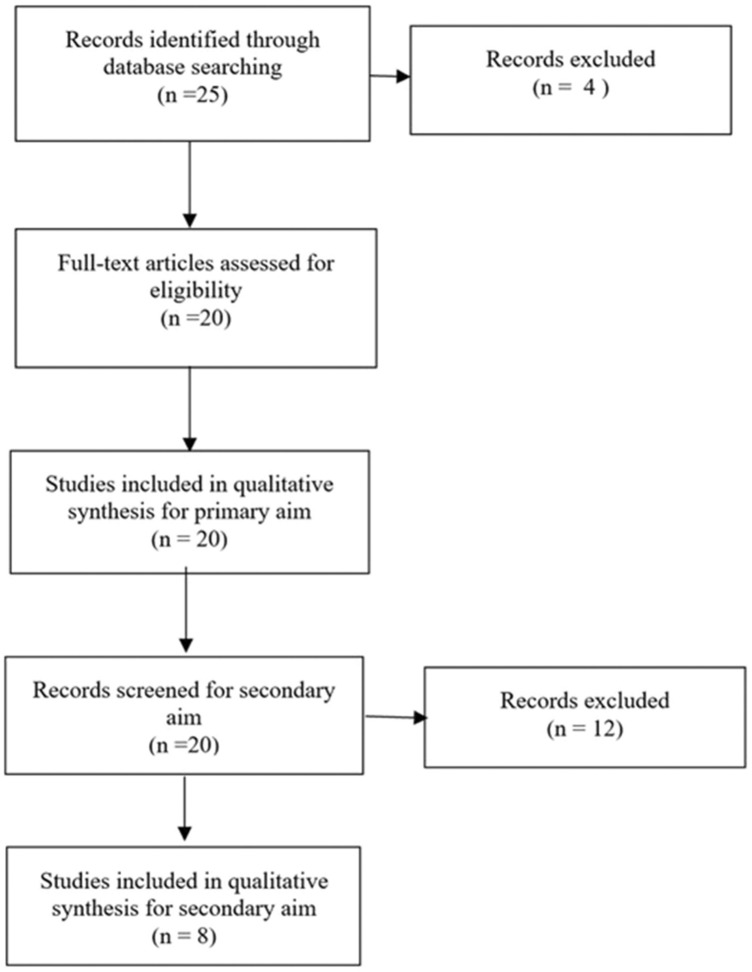
Studies that did not differentiate between patients who tested positive for one aPL and those who tested positive for any other aPL were excluded in order to accurately measure the prevalence of each isotype of aPL among RMDs other than SLE, which is our primary aim. Subsequently, studies which associated thrombotic (arterial or venous) events to positivity of aPL were included to test our secondary aim. However, studies that reported the prevalence of vascular thrombotic events in the total study population, including those testing negative for aPL, were excluded (Fig. 1).
Fig. 1.
Methodology for literature search and inclusion of studies for aims
Data Collection and Analysis
The percentage of patients with a diagnosis of any inflammatory and autoimmune RMDs except SLE who tested positive for either aCL, anti-β2GPI, or LAC was noted. Subsequently, the percentage of patients who tested positive for any aPL undergoing vascular thrombotic event was recorded. The median percentages for the prevalence of aPL with isotypes among patients in each included disease were calculated. Furthermore, the median percentages of patients with positive aPL undergoing arterial or venous thrombosis were calculated.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
The studies included in this review were retrospective cohort studies (N = 936, 25% of all studies), prospective cohort studies (N = 72, 5% of all studies), cross-sectional studies (N = 1836, 55% of all studies), case–control studies (N = 319, 15% of all studies), and randomized clinical trial (N = 176, 5% of all studies). The total number of study individuals varied from a minimum of 15 and a maximum of 940. A total of 3242 patients were included in this analysis, to include (1903, 57.25%) with SSc, (109, 3.28%) with mixed connective tissue disease (MCTD), (418, 12.57%) with undifferentiated connective tissue disease (UCTD), (517, 15.55%) with Sjögren’s syndrome (SS), (292, 8.78%) with ANCA associated vasculitides (AAV), and (97, 2.92%) with RA.
Laboratory Analysis for Antiphospholipid Antibodies
Lupus anticoagulant was determined in 13 of 20 studies (65%). Anticardiolipin antibodies were tested in 16 studies (80%) while anti-β2GPI were tested in 12 studies (60%). These antibodies were tested with enzyme-linked immunosorbent assay (ELISA), but with different positivity cutoffs used as established from the manufacturers of the kits (Table 1).
Table 1.
Status of different types of aPL in studies which assessed aPL among patients with inflammatory and autoimmune rheumatic and musculoskeletal diseases (RMDs) other than systemic lupus erythematosus (SLE) along with the tests used and cut-offs set
| Study | LAC | LAC test | Repeat? | aCL | aCL test | aCL cutoff | Repeat? | aβGPI | aβGPI test | aβGPI cutoff | Repeat? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gupta et al. [7] | Y | aPTT | Y | Y | ELISA | 12 units | Y | Y | ELISA | 12 units | Y |
| Martin et al. [12] | Y | dRVVT + aPTT | Y | Y | NA | 15 units | Y | Y | NA | 15 units | Y |
| Sobanski et al. [18] | Y | dRVVT + aPTT | N | Y | Organtec ELISA | 10 units | N | Y | Organtec ELISA | 10 units | N |
| Mok et al. [26] | Y | dRVVT + aPTT | N | Y | Cardiolipin vital diagnostic assay | 15 units | N | NA | NA | NA | NA |
| Wielosz et al. [14] | NA | NA | NA | Y | Commercial ELISA | 15 units | N | Y | Euroimmun ELISA | 20 units | N |
| Toure et al. [13] | Y | dRVVT | N | Y | Commercial ELISA | 40 units | N | Y | Commercial ELISA | 40 units | N |
| Morrisroe et al. [17] | Y | dRVVT + aPTT | N | Y | Cardiolipin vital diagnostic assay | 20 units | N | Y | Organtec glycoprotein assay | 20 units | N |
| Boin et al. [15] | NA | NA | NA | Y | Commercial ELISA | NA | N | Y | Commercial ELISA | 20 units | N |
| Marie et al. [8] | Y | Dilute thromboelastin time | N | Y | ELISA | NA | N | Y | ELISA | NA | N |
| Rai et al. [23] | Y | aPTT | Y | Y | ELISA | 12 units | Y | Y | NA | NA | Y |
| Radin et al. [22] | Y | NA | N | Y | NA | NA | N | Y | NA | NA | N |
| Bortoluzzi et al. [27] | Y | dRVVT + aPTT | Y | Y | ELISA | NA | Y | Y | ELISA | NA | Y |
| Radin et al. [28] | Y | NA | Y | Y | NA | NA | Y | Y | NA | NA | Y |
| Lockshin et al. [29] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Price et al. [30] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Pasoto et al. [9] | Y | dRVVT + aPTT | Y | Y | Commercial ELISA | 40 units | Y | Y | Commercial ELISA | 10 units | Y |
| Jeleniewicz et al. [31] | Y | aPTT | N | Y | Standard ELISA | 15 units | N | Y | Commercial ELISA | 20 units | N |
| Jordan and D’cruz [32] | Y | dRVVT + aPTT with mixing studies | N | Y | ELISA | 20 units | N | Y | NA |
IgG 6.5 units IgM 20 units |
N |
| Sebastian et al. [33] | NA | NA | NA | Y | ELISA | 10 units | N | Y | Commercial ELISA | 20 units | N |
Y yes, N no, NA not applicable, aPTT activated partial thromboplastin time, dRVVT dilute Russell’s viper venom time
The overall prevalence of aPL positivity ranged from 0 to 57.5%, with a median prevalence of 14.05%. The majority of studies assessed the prevalence of aPL among SSc patients. Although the highest median prevalence was for RA, only one study assessed aPL among RA (Table 2).
Table 2.
Studies listing the prevalence of aPL with antibody subtypes among patients with inflammatory and autoimmune rheumatic and musculoskeletal diseases (RMDs) other than systemic lupus erythematosus (SLE)
| Study | Study design | Patients, n | Antibodies tested | aPL-positive (%) | |||
|---|---|---|---|---|---|---|---|
| Total, n (%) | LAC, n (%) | aCL, n (%) | aβGPI, n (%) | ||||
| SSc | |||||||
| Gupta et al. [7] | Prospective cohort | 72 | LAC, aCL and aβGPI | 7 (9.7%) | 2 (28.57%) | 5 IgG (71.43%)–2 IgM (28.57%) | 1 (14.29%) |
| Martin et al. [12] | Cross-sectional | 268 | LAC, aCL, and aβGPI | 31 (11.57%) | 17 (54.84%) | 11 IgG (35.48%)–3 IgM (9.68%) | 8 IgG (25.81%)–8 IgM (25.81%) |
| Sobanski et al. [18] | Cross-sectional | 249 | LAC, aCL and aβGPI | 16 (6.43%) | 4 (25%) | 3 IgG (18.75%) | 11 IgG (68.75%) |
| Mok et al. [26] | Cross-sectional | 53 | LAC, aCL, and aβGPI | 7 (13.21%) | – | – | – |
| Wielosz et al. [14] | Cross-sectional | 50 | aCL and aβGPI | 28 (56%) | – | – | – |
| Toure et al. [13] | Cross-sectional | 40 | aCL and aβGPI | 23 (57.50%) | 2 (8.7%) | 7 IgG (30.44%)–2 IgM (8.7%) | 15 IgG (65.22%)–13 IgM (56.25%) |
| Morrisroe et al. [17] | Cross-sectional | 940 | LAC, aCL, and aβGPI | 226 (24.04%) | 0 (0%) | 98 IgG (43.36%)–133 IgM (58.85%) | 63 (27.88%) |
| Rai et al. [23] | Cross-sectional | 15 | LAC and aCL | 2 (13.33%) | 1 (50%) | 1 (50%) | – |
| Boin et al. [15] | Case–control | 150 | aCL and aβGPI | 78 (52%) | – | 9 IgG (11.54%)–23 IgM (29.49%) | 1 IgG (1.28%)–31 IgM (39.74%) |
| Marie et al. [8] | Case–control | 69 | LAC, aCL, and aβGPI | 13 (18.84%) | 3 (23.08%) | 10 IgG (76.92%)–3 IgM (23.08%) | 2 IgG (15.39%)–1 IgM (7.69%) |
| MCTD | |||||||
| Rai et al. [23] | Cross-sectional | 15 | LAC and aCL | 2 (13.33%) | 1 (50%) | 1 (50%) | – |
| Radin et al. [22] | Cross-sectional | 94 | LAC, aCL, and aβGPI | 28 (29.79%) | 14 (50%) | 11 (39.29%) | 3 (10.71%) |
| UCTD | |||||||
| Bortoluzzi et al. [27] | Retrospective cohort | 285 | LAC, aCL, and aβGPI | 29 (10.18%) | – | – | – |
| Radin et al. [28] | Retrospective cohort | 133 | LAC, aCL, and aβGPI | 33 (24.81%) | 15 (45.45%) | 18 (54.54%) | 18 (54.54%) |
| SS | |||||||
| Rai et al. [23] | Cross-sectional | 15 | LAC and aCL | 0 (0%) | 0 (0%) | 0 (0%) | – |
| Lockshin et al. [29] | Retrospective cohort | 157 | – | 3 (1.91%) | – | – | – |
| Price et al. [30] | Retrospective cohort | 245 | – | 7 (2.86%) | – | – | – |
| Pasoto et al. [9] | Case–control | 100 | LAC, aCL, and aβGPI | 16 (16%) | 9 (56.25%) | 1 IgG (6.25%)–3 IgM (18.75%) | 4 IgG (25%)–2 IgM (12.5%) |
| RA | |||||||
| Jeleniewicz et al. [31] | Cross-sectional | 97 | LAC, aCL and aβGPI | 27 (27.8%) | 1 (1%) | 12 IgG (12.5%)–11 IgM (11.3%) | 0 IgG (0%)–12 IgM (12.4%) |
| AAV | |||||||
| Jordan and D’cruz [32] | Retrospective cohort | 116 | aCL and aβGPI | 60 (52%) | 13 (21.6%) | 4 IgG (6.6%)–3 IgM (5%) | – |
| Granulomatosis with polyangiitis | |||||||
| Sebastian et al. [33] | Randomized trial | 176 | aCL and aβGPI | 26 (14.77%) | – | 1 IgG (3.85%)–20 IgM (76.92%) | 1 IgG (3.85%)–5 IgM (19.23%) |
SSc systemic sclerosis, MCTD mixed connective tissue disease, UCTD undifferentiated connective tissue disease, SS Sjögren’s syndrome, RA rheumatoid arthritis, AAV antineutrophil cytoplasmic antibody-associated vasculitis
Anticardiolipin antibodies were sub-divided into two isotypes IgG and IgM in 11 studies. The overall percentage of positive patients ranged from 3.85 to 76.92% (median value 18.75%) for IgG and from 8.7 to 76.92% (median value: 20.92%) for IgM (Table 2). Antibodies against β2-glycoprotein were also sub-divided into isotypes IgG and IgM in a total of seven studies with overall positivity ranging from 1.28 to 68.75% (median value 25%) for IgG and from 7.69 to 56.25% (median value 22.52%) for IgM (median value 32.78%) (Table 2). The percentage of positive LAC patients varied from 0 to 56.25% with a median of 28.57% (Table 2).
LAC, aCL, and anti-β2GPI were confirmed in six studies (30%); three for SSc, two for SS, two for UCTD, and one for MCTD. Among studies which confirmed aPL positivity, the overall prevalence of aPL ranged from 0 to 29.79%, with a median prevalence of 10.88%. Among SSc alone, the median prevalence was 11.57%. LAC prevalence ranged between 0 and 56.25%, with a median prevalence of 50%. Regarding aCL, the median prevalence of the IgG isotype (35.48%) was higher than that of IgM (18.75%) with only three studies assessing these isotypes [7, 9, 12]. As for anti-β2GPI, the median prevalence of the IgG isotype (25.41%) was slightly higher than that of IgM (19.16%), despite that only two studies assessed the prevalence of these isotypes [9, 12].
Six studies assessed the number of patients with double- or triple-positive aPL. Four patients were specified as triple-positive, whereas ten patients were double-positive, all of which had SSc. The percentage of the antibodies which tested negative after 12 weeks was not reported in any study.
Association Between Thrombotic Events and aPL
In total, eight studies (40%) including 1071 patients assessed the association of thrombosis with aPL in non-SLE RMDs. Five studies for SSc (N = 698), one for GPA (N = 176), one for SS (N = 100), and one for RA (N = 97) reported either arterial or venous thrombotic events.
For arterial events, a minimum of 7.69% and a maximum of 71.43% (median value 18.75%) of aPL-positive patients experienced an event. In comparison, a minimum of 7.69% and a maximum of 31.25% (median value 13.66%) underwent venous thrombotic events. Among SSc patients, five patients were triple aPL-positive and two patients were double-positive. The results on thrombotic complications among aPL-positive RMDs other than SLE is presented in Table 3.
Table 3.
Studies listing the prevalence of thrombotic events in aPL-positive non-SLE inflammatory and autoimmune rheumatic and musculoskeletal diseases (RMDs) patients
| Study | Study design | Patients, n | Antibody tested | Thrombotic events | In positive aPL | |
|---|---|---|---|---|---|---|
| Total aPL, n (%) | Arterial, n (%) | Venous, n (%) | ||||
| SSc | ||||||
| Gupta et al. [7] | Prospective cohort | 72 | LAC, aCL, and aβGPI | 7 (9.72%) | 5 (71.43%) | 1 (14.29%) |
| Martin et al. [8] | Cross-sectional | 268 | LAC, aCL, and aβGPI | 31 (11.57%) | 4 (12.90%) | 3 (9.68%) |
| Sobanski et al. [18] | Cross-sectional | 249 | LAC, aCL, and aβGPI | 16 (6.43%) | 3 (18.75%) | 5 (31.25%) |
| Toure et al. [13] | Cross-sectional | 40 | aCL and aβGPI | 23 (57.5%) | – | 3 (13.04%) |
| Marie et al. [8] | Case–control | 69 | LAC, aCL, and aβGPI | 13 (18.84%) | 1 (7.69%) | 1 (7.69%) |
| SS | ||||||
| Pasoto et al. [9] | Case–control | 100 | LAC, aCL, and aβGPI | 16 (16%) | 3 (18.75%) | 4 (25%) |
| RA | ||||||
| Jeleniewicz et al. [31] | Cross-sectional | 97 | LAC, aCL, and aβGPI | 27 (27.8%) | – | 4 (14.8%) |
| AAV | ||||||
| Granulomatosis with polyangiitis | ||||||
| Sebastian et al. [33] | Randomized trial | 176 | aCL and aβGPI | 26 (14.77%) | – | 3 (11.54%) |
SSc systemic sclerosis, SS Sjögren’s syndrome, RA rheumatoid arthritis, AAV antineutrophil cytoplasmic antibody-associated vasculitis
Two studies in the SSc cohort and one study in the SS cohort, which assessed thrombotic complications, performed a confirmation testing. A median value of 34.36% of aPL-positive patients underwent an arterial event and a median value of 16.32% of aPL-positive patients underwent a venous event.
Since the studies which did the confirmation test only reported the results according to the confirmation test, it is not known whether the prevalence of thrombosis was higher among patients who tested positive only upon initial test.
Discussion
When adding together 3242 patients with RMDs from a total of 20 studies investigating the prevalence of aPL in different inflammatory and autoimmune RMDs, we found an overall median percentage of aPL-positive patients of 14.05% (from 0 to 57.5%). These findings present wide fluctuations of aPL prevalence which can be explained by a variety of factors. The difference in the number of patients enrolled by each study can lead to a heterogeneity of prevalence. In addition, the lack of confirmation tests by some studies can alter the real prevalence. For example, the studies by Toure et al. [13] and Wielosz et al. [14], which reported the highest two prevalences of aPL among all studies included, did not perform a confirmation test after 12 weeks, which might have led to a decreased prevalence if performed.
Albeit the heterogeneity of the retrieved studies, it is worth noting that three out of a total of ten studies performed in the last 12 years reported that more than half of their SSc cohort had at least one positive aPL. However, these three studies had a relatively low number of patients except for Boin et al. [15].
The median prevalence of aPL was lower among the studies that performed a confirmation test. Similar results were found in a database analysis of 33,456 individuals who were tested for aPL whereby only 10.6% of individuals tested positive on the confirmation test compared to 17% of initially positive aPL [16].
Although six out of eight studies did not find a significantly increased risk of thromboembolism in aPL-positive patients [7, 8, 12, 13, 15, 17], the cross-sectional study by Sobanski et al. [18] found an association between aPL positivity and thromboembolism in univariate and in multivariate analysis. The high percentage of aPL-positive patients who recorded an event of arterial thrombosis (digital ulceration) in Gupta et al. [7] questions whether other epitopes are playing a role in thrombosis in SSc. In addition, the only patient who had triple-positive aPL underwent abortion, which might suggest the need for special anticoagulation care of triple aPL-positive SSc patients. No study assessed the association of thrombosis with the prevalence of specific antibody isotype.
When comparing the studies that performed a confirmation test to those that did not, it was noted that arterial events were more prevalent among patients who confirmed their aPL. On the other hand, venous events were more prevalent among patients who did not confirm their aPL. The risk of vascular events is usually increased among patients with two or more positive tests for specific aPL [19, 20]. LAC and aCL are both associated with significant risk for arterial and venous events, although aCL positivity has a higher risk for arterial events than venous events and LAC has higher risk for venous events than arterial events [21]. Due to the limited number of studies, the association of aPL isotypes with specific vascular events could not be assessed.
Along with the manifestation of thrombosis, aPL can be associated with other vascular manifestations. Wielosz et al. [14] reported that 21% of their aPL-positive SSc had a scleroderma renal crisis event in comparison to 0% of aPL-negative SSc patients. However, both Sobanski et al. [18] and Morrisroe et al. [17] did not find any association. Therefore, more studies are needed to determine whether aPL can predispose SSc patients to manifestations of vascular events other than thrombosis, such as renal crisis or pulmonary arterial hypertension.
In the MCTD cohort, Radin et al. [22] documented around double the prevalence of Rai et al. [23] taking into consideration that the subjects used in Radin et al.’s study were pregnant MCTD women. Notably, aPL-positive MCTD women had poorer fetal outcomes, which proposes whether MCTD pregnant patients should be regularly screened for aPL in order to receive higher doses of anticoagulation. It is worth mentioning that Radin et al. did not note the assay used to evaluate any of the aPL or the cutoffs used, which can also explain the variety in the results.
Although neither of the studies associated the presence of aPL in MCTD patients with thrombosis risk, a previous case report by Jackson et al. [24] described a patient with MCTD who presented with thrombosis of the right femoral artery in association with aPL. On the other hand, a previous cross-sectional study by Doria et al. [25] noted that aCL was associated with thrombocytopenia but not with recurrent thrombosis and/or abortions in MCTD patients.
In the time interval of this review, only one study assessed the prevalence of aPL in RA patients. Since anti–β2GP1-dependent aCL antibodies are responsible for thrombotic events [10], the absence of IgG anti–β2GP1 in our RA cohort might have contributed to a lower prevalence of thrombotic complications.
For AAV and GPA, a higher percentage of AAV patients showing aPL positivity was reported in comparison to GPA. The analysis of this difference necessitates additional studies, since only one study in each group has been included in this review.
Limitations of the Study
This systematic review has some limitations. All the included studies were observational, and therefore subject to the biases inherent to such study designs. In addition, there was heterogeneity in the data in terms of inclusion criteria, clinical outcome definition, detected immunoglobulin isotypes, clinical details, and control groups. While the association between aPL and the clinical manifestations of the syndrome appears robust, the added value of testing for these antibodies in specific settings (vasculitis, connective tissue diseases beyond SLE…) lacks well-designed studies to be confirmed.
Conversely, this study is strengthened by the defined protocol that we strictly applied, which potentially strengthened the reproducibility of the results compared to previous analyses of the literature.
Conclusions
Despite the heterogeneity of the retrieved study, we found an overall median prevalence of 14.05% in patients with inflammatory and autoimmune RMDs. In some conditions, e.g., SSc, aPL positivity was observed in a third of the patients. Our analysis also highlights several gaps in the current knowledge of the field. Repeated confirmatory aPL test was performed in 30% of the studies, potentially limiting the estimations. Moreover, while the association between aPL positivity and thromboembolism has been observed in some cross-sectional and case–control studies, to date, there are not enough data to support routine screening for aPL in all the RMDs. However, some conditions, namely MCTD, UCDT, and SSc, might represent an expectation, especially in some circumstances, such as when planning a pregnancy.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Georges El Hasbani, Mario Viola, Savino Sciascia, Ali T. Taher, and Imad Uthman have no personal, financial, commercial, or academic conflicts of interest to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) J Thromb Haemost. 2006;4:295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 2.Ortel TL. Antiphospholipid syndrome: laboratory testing and diagnostic strategies. Am J Hematol. 2012;87(Suppl 1):S75–81. doi: 10.1002/ajh.23196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tubach F, Hayem G, Marchand JL, et al. IgG anti-beta2-glycoprotein I antibodies in adult patients with systemic lupus erythematosus: prevalence and diagnostic value for the antiphospholipid syndrome. J Rheumatol. 2000;27:1437–1443. [PubMed] [Google Scholar]
- 4.Long AA, Ginsberg JS, Brill-Edwards P, et al. The relationship of antiphospholipid antibodies to thromboembolic disease in systemic lupus erythematosus: a cross-sectional study. Thromb Haemost. 1991;66:520–524. doi: 10.1055/s-0038-1646452. [DOI] [PubMed] [Google Scholar]
- 5.Sebastiani GD, Passiu G, Galeazzi M, et al. Prevalence and clinical associations of anticardiolipin antibodies in systemic lupus erythematosus: a prospective study. Clin Rheumatol. 1991;10:289–293. doi: 10.1007/bf02208692. [DOI] [PubMed] [Google Scholar]
- 6.Merashli M, Alves J, Ames PRJ. Clinical relevance of antiphospholipid antibodies in systemic sclerosis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2017;46:615–624. doi: 10.1016/j.semarthrit.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R, Thabah MM, Gupta S, et al. Clinical significance of antiphospholipid antibodies in Indian scleroderma patients. Rheumatol Int. 2009;30:277–279. doi: 10.1007/s00296-009-1107-0. [DOI] [PubMed] [Google Scholar]
- 8.Marie I, Jouen F, Hellot M-F, et al. Anticardiolipin and anti-beta2 glycoprotein I antibodies and lupus-like anticoagulant: prevalence and significance in systemic sclerosis. Br J Dermatol. 2008;158:141–144. doi: 10.1111/j.1365-2133.2007.08309.x. [DOI] [PubMed] [Google Scholar]
- 9.Pasoto SG, Chakkour HP, Natalino RR, et al. Lupus anticoagulant: a marker for stroke and venous thrombosis in primary Sjögren’s syndrome. Clin Rheumatol. 2012;31:1331–1338. doi: 10.1007/s10067-012-2019-z. [DOI] [PubMed] [Google Scholar]
- 10.Olech E, Merrill JT. The prevalence and clinical significance of antiphospholipid antibodies in rheumatoid arthritis. Curr Rheumatol Rep. 2006;8:100–108. doi: 10.1007/s11926-006-0049-8. [DOI] [PubMed] [Google Scholar]
- 11.Giannakopoulos B, Krilis SA. The pathogenesis of the antiphospholipid syndrome. N Engl J Med. 2013;368:1033–1044. doi: 10.1056/NEJMra1112830. [DOI] [PubMed] [Google Scholar]
- 12.Martin M, Martinez C, Arnaud L, et al. Association of antiphospholipid antibodies with active digital ulceration in systemic sclerosis. RMD Open. 2019 doi: 10.1136/rmdopen-2019-001012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Touré AO, Ly F, Sall A, et al. Antiphospholipid antibodies and systemic scleroderma. Turk J Haematol. 2013;30:32–36. doi: 10.4274/tjh.2012.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wielosz E, Dryglewska M, Majdan M. Antiphospholipid antibodies and kidney involvement in patients with systemic sclerosis. Clin Rheumatol. 2009;28:955–959. doi: 10.1007/s10067-009-1188-x. [DOI] [PubMed] [Google Scholar]
- 15.Boin F, Franchini S, Colantuoni E, et al. Independent association of anti-beta(2)-glycoprotein I antibodies with macrovascular disease and mortality in scleroderma patients. Arthritis Rheum. 2009;60:2480–2489. doi: 10.1002/art.24684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egiziano G, Widdifield J, Rahman A, et al. Antiphospholipid antibody testing in a general population sample from the USA: an administrative database study. Sci Rep. 2020;10:3102. doi: 10.1038/s41598-020-59990-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morrisroe KB, Stevens W, Nandurkar H, et al. The association of antiphospholipid antibodies with cardiopulmonary manifestations of systemic sclerosis. Clin Exp Rheumatol. 2014;32:S133–S137. [PubMed] [Google Scholar]
- 18.Sobanski V, Lemaire-Olivier A, Giovannelli J, et al. Prevalence and clinical associations of antiphospholipid antibodies in systemic sclerosis: new data from a French cross-sectional study, systematic review, and meta-analysis. Front Immunol. 2018 doi: 10.3389/fimmu.2018.02457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brandt JT, Triplett DA, Rock WA, et al. Effect of lupus anticoagulants on the activated partial thromboplastin time Results of the College of American Pathologists survey program. Arch Pathol Lab Med. 1991;115:109–114. [PubMed] [Google Scholar]
- 20.Galli M, Luciani D, Bertolini G, et al. Lupus anticoagulants are stronger risk factors for thrombosis than anticardiolipin antibodies in the antiphospholipid syndrome: a systematic review of the literature. Blood. 2003;101:1827–1832. doi: 10.1182/blood-2002-02-0441. [DOI] [PubMed] [Google Scholar]
- 21.Reynaud Q, Lega J-C, Mismetti P, et al. Risk of venous and arterial thrombosis according to type of antiphospholipid antibodies in adults without systemic lupus erythematosus: a systematic review and meta-analysis. Autoimmun Rev. 2014;13:595–608. doi: 10.1016/j.autrev.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Radin M, Schreiber K, Cuadrado MJ, et al. Pregnancy outcomes in mixed connective tissue disease: a multicentre study. Rheumatology. 2019;58:2000–2008. doi: 10.1093/rheumatology/kez141. [DOI] [PubMed] [Google Scholar]
- 23.Rai R, Swetha T. Association of anti-phospholipid antibodies with connective tissue diseases. Indian Dermatol Online J. 2015;6:89–91. doi: 10.4103/2229-5178.153009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson J, McDonald M, Casey E, et al. Mixed connective tissue disease with arterial thrombosis, antiphospholipid antibodies and heparin induced thrombocytopenia. J Rheumatol. 1990;17:1523–1524. [PubMed] [Google Scholar]
- 25.Doria A, Ruffatti A, Calligaro A, et al. Antiphospholipid antibodies in mixed connective tissue disease. Clin Rheumatol. 1992;11:48–50. doi: 10.1007/BF02207083. [DOI] [PubMed] [Google Scholar]
- 26.Mok MY, Lau CS, Chiu SSH, et al. Systemic sclerosis is an independent risk factor for increased coronary artery calcium deposition. Arthritis Rheum. 2011;63:1387–1395. doi: 10.1002/art.30283. [DOI] [PubMed] [Google Scholar]
- 27.Bortoluzzi A, Furini F, Campanaro F, et al. Application of SLICC classification criteria in undifferentiated connective tissue disease and evolution in systemic lupus erythematosus: analysis of a large monocentric cohort with a long-term follow-up. Lupus. 2017;26:616–622. doi: 10.1177/0961203316671814. [DOI] [PubMed] [Google Scholar]
- 28.Radin M, Schreiber K, Cecchi I, et al. A multicentre study of 244 pregnancies in undifferentiated connective tissue disease: maternal/fetal outcomes and disease evolution. Rheumatology. 2020 doi: 10.1093/rheumatology/kez620. [DOI] [PubMed] [Google Scholar]
- 29.Lockshin MD, Levine AB, Erkan D. Patients with overlap autoimmune disease differ from those with “pure” disease. Lupus Sci Med. 2015;2:e000084. doi: 10.1136/lupus-2015-000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Price EJ, Collins D, Williamson L, et al. The burden of systemic disease in patients with primary Sjögren’s syndrome. Rheumatology. 2016;55:i179–i180. doi: 10.1093/rheumatology/kew186.004. [DOI] [Google Scholar]
- 31.Jeleniewicz R, Majdan M, Targońska-Stępniak B, et al. Prevalence of antiphospholipid antibodies in rheumatoid arthritis patients and relationship with disease activity. Pol Arch Med Wewn. 2012;122:480–486. doi: 10.20452/pamw.1415. [DOI] [PubMed] [Google Scholar]
- 32.Jordan N, D’cruz DP. Association of lupus anticoagulant with long-term damage accrual in antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Care Res. 2016;68:711–715. doi: 10.1002/acr.22723. [DOI] [PubMed] [Google Scholar]
- 33.Sebastian JK, Voetsch B, Stone JH, et al. The frequency of anticardiolipin antibodies and genetic mutations associated with hypercoagulability among patients with Wegener’s granulomatosis with and without history of a thrombotic event. J Rheumatol. 2007;34:2446–2450. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.