Abstract
Purpose of Review
The triquetrum is the second most commonly fractured carpal bone, comprising 15–18% of all carpal bone fractures. This review summarizes the current knowledge of triquetral fractures, including the anatomy and pathophysiology, evaluation and diagnosis, treatment and management, post-treatment outcomes, and complications.
Recent Findings
Triquetral fractures are frequently caused by impaction of the ulnar wrist after a fall on an outstretched hand or by avulsion of attached ligaments. There are three main types of triquetral fractures: dorsal cortical fractures, triquetral body fractures, and volar cortical fractures. Dorsal cortical fractures are the most common and are usually benign, while volar cortical fractures are the least common and can be problematic. Nonsurgical management is indicated for most triquetral fractures, which usually results in good outcomes. Surgical treatment is indicated for fractures with significant displacement or evidence of instability. Complications of triquetral fractures include non-union, triangular fibrocartilage complex injury, and pisotriquetral arthritis.
Summary
While less common than scaphoid fractures, triquetral fractures should remain in the differential diagnosis for patients with ulnar-sided wrist pain after falling on an outstretched hand. Most triquetral fractures can be treated with immobilization, though they should be thoroughly evaluated due to their potential to result in instability, loss of motion, and arthrosis. Further research is needed to determine the best method of surgical treatment.
Keywords: Triquetrum, Triquetral fractures, Carpal fractures, Carpal bones, Wrist fracture
Introduction
The wedge-shaped triquetrum is found in the proximal row of the carpus [1]. It is the second most common carpal fracture, behind the scaphoid, comprising 15–18% of all carpal bone fractures, which in turn consist of 8%–19% of all hand and wrist surgeries [2–4]. This review summarizes the current knowledge of triquetral fractures, including the relevant anatomy and pathophysiology, evaluation and diagnosis, treatment and management, post-treatment outcomes, and reported complications.
Anatomy
The triquetrum has three facets for articulation with adjacent carpal bones. The flat facet on the ulnar surface of the triquetrum articulates with the lunate, the concave facet on the distal surface articulates with the hamate, and the oval facet on the volar surface articulates with the pisiform [1]. The articulations between the carpal bones form a concavity for the transverse carpal arch [5]. The triquetrum participates in the motion of the midcarpal and radiocarpal joints of the wrist [6, 7].
Extrinsic ligaments attach the triquetrum to the ulna and radius. On the dorsal surface, these ligaments include the dorsal radiotriquetral and dorsal ulnotriquetral ligaments. Similarly, extrinsic ligaments on the volar surface include the volar radiotriquetral, volar ulnotriquetral, and radiolunotriquetral ligaments [8–10]. The volar ulnotriquetral ligament is a part of the triangular fibrocartilage complex (TFCC), which stabilizes the distal radioulnar joint [11]. The relevant intrinsic ligaments of the wrist include the scaphotriquetral, lunotriquetral, triquetrohamate, and triquetrocapitate ligaments [10].
Pathophysiology
Triquetral fractures are more commonly caused by impaction by adjacent bony structures or avulsion of attached ligaments rather than a direct blow, as the surrounding carpal bones protect the triquetrum from direct impact [12]. The most common type of triquetral fracture is a dorsal cortical fracture involving the dorsal ridge, accounting for 93–95% of all triquetral fractures [13•, 14]. This can occur through impaction by the ulnar styloid or hamate as well as through an avulsion mechanism from the dorsal radiotriquetral or dorsal scaphotriquetral ligaments [12, 13•, 15, 16].
While falling onto an outstretched hand with the wrist in extension and ulnar deviation appears to be the most common cause of triquetral fractures, there are other mechanisms [17, 18]. Impaction by the ulnar styloid is one mechanism based on radiographic images and chisel-like morphology of the ulnar styloid [19]. It has been shown that individuals with a longer ulnar styloid process are more likely to experience dorsal cortical fractures, further supporting this theory [15]. Höcker and Menschik proposed a mechanism based on their radiographic analyses that triquetral fractures are caused by the impaction of the triquetrum by the proximal hamate with the wrist in extension [12]. Later, Becce et al. used magnetic resonance imaging (MRI) to analyze patients with dorsal cortical fractures. This study argues that while fractures caused by impaction were the most common, a significant number of fractures were still caused by avulsion. Regardless of the mechanism, it has been reported that two thirds of all fractures had dorsal radiotriquetral ligament tears, and more than three-quarters had dorsal scaphotriquetral ligament tears [16].
Avulsion fractures with associated dorsal radiotriquetral and scaphotriquetral ligament injuries suggest an injury mechanism that involves wrist flexion with radial deviation, in contrast to the previously mentioned mechanism of an extended, ulnarly deviated wrist [18, 20]. It is believed that triquetral fractures can be caused by both mechanisms. This is further qualified as Becce et al. reported that while a few patients sustained injuries with the wrist in flexion, the majority of patients presented with the wrist in extension [16].
Garcia-Elias developed a system to distinguish the patterns of dorsal cortical fractures: Type 1 fractures are nondisplaced; Type 2 fractures are partially displaced at the proximal end; Type 3 fractures are partially displaced at the distal end; Type 4 fractures have a completely displaced fragment; Type 5 fractures have multiple completely displaced fragments; and Type 6 injuries have a fracture line through the coronal plane in which the dorsal side is displaced [15]. The most common type supported by multiple studies is Type 1 [12, 15, 16]. Dorsal cortical fractures can be managed with non-surgical treatment with successful outcomes.
The second most common type of triquetral fracture is fracture of the triquetral body [2, 13•]. Triquetral body fractures are often associated with perilunate fracture dislocations, which are present in 12% to 25% of all triquetral fractures [14, 17]. These injuries tend to result in transverse fractures, sometimes involving the proximal pole. Other mechanisms of injury include axial dislocations and crush injuries, resulting in fractures in the sagittal plane which can flatten the transverse carpal arch. Higher energy trauma tend to produce more comminuted fractures [2, 21]. Other associated wrist injuries with triquetral body fractures include lunotriquetral ligament injury, scaphoid fractures and distal radius and/or ulna fractures [2, 18].
A subtype of body fractures can have fracture line extension into the pisotriquetral joint, which is caused by shearing forces of the distally and dorsally deviated pisiform on the volar medial surface of the triquetrum. Pisiform impaction is usually caused by falling onto an outstretched hand with the wrist in extension [22•]. These fractures may result in pisiform instability or pisotriquetral arthritis [22•, 23]. While triquetral body fractures are typically associated with another injury, isolated triquetral body fractures can occasionally occur [24]. Displaced triquetral body fractures have been reported and the underlying cause of the fractures was a fall onto an outstretched hand with the wrist in extension [25, 26].
The third and least common types of triquetral fracture are volar cortical fractures. These are usually caused by avulsion of the volar ulnotriquetral or lunotriquetral ligaments but may occur through volar scaphotriquetral and radiolunotriquetral ligament avulsion [2, 13, 27]. Lunotriquetral ligament tears and joint instability can occur as a result [27]. Worse prognosis has been reported for this variant of triquetral fracture as there is the potential for carpal instability associated with possible soft tissue injury [14, 27].
After scaphoid fractures, triquetral fractures are the second most common carpal fracture to present in the absence of additional injuries unrelated to the direct fracture mechanism [2]. It is estimated that between 50 and 70% of all triquetral fractures occur in this manner, with some studies reporting up to 80% [12]. Most of these fractures are dorsal cortical fractures. Triquetral body fractures are usually associated with a higher energy mechanism of injury [14].
Evaluation and Diagnosis
A history of excessive load or falls onto the outstretched hand with the wrist in extension should raise concern for a triquetral fracture. Dorsal cortical fractures are most commonly associated with falls with an extended wrist that is also ulnarly deviated. A triquetral fracture typically presents as ulnar-sided wrist pain that is worse with wrist flexion and extension. Patients typically complain of dorsal swelling and localized tenderness over the dorsal edge of the triquetrum [2, 3, 12, 13•, 14]. Some authors believe wrist flexion may be more painful than wrist extension in dorsal cortical fractures because of increased fracture displacement during flexion [12, 17].
There is no single best view for detecting all variants of triquetral fractures and multiple radiographs should be evaluated together (Fig. 1). Most recommend a combination of posteroanterior (PA), lateral, 45-degree pronated oblique, and radial deviation views [2, 27]. Dorsal cortical fractures are best visualized using the 45-degree pronated oblique and lateral views [13•, 17]. Triquetral body fractures involving the pisotriquetral joint and volar cortical fractures are better visualized when all three views (PA, lateral, and 45-degree pronated oblique) are obtained [2, 14, 22•, 23]. Volar cortical fractures in which the volar cortical fragment is obscured by the hamate or the triquetral body are best detected with the radial deviation view [21, 27].
Fig. 1.
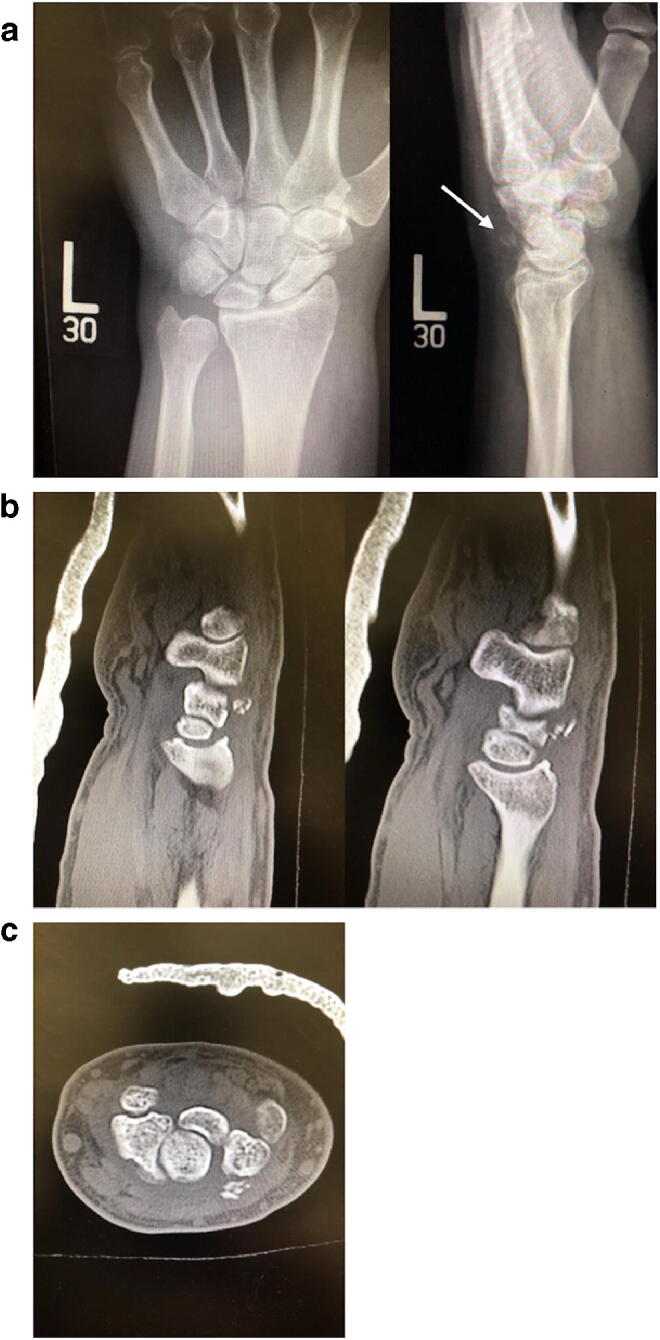
Dorsal cortical fracture of the triquetrum. a PA and lateral radiographic images of a triquetral fracture of the dorsal cortical pattern. b Corresponding sagittal CT images of the dorsal cortical fracture. c Axial CT image of the fracture (Figure is in separate file)
Triquetral fractures are frequently difficult to detect on plain radiographs. Welling et al. reported only being able to visualize 20% of all triquetral fractures through standard x-rays [28]. Krastman et al. reported the sensitivity of repeated physical and x-ray examination after initial examination in detecting triquetral fractures to be less than the sensitivity of repeated examination in detecting other carpal fractures [29••]. Thus, computerized tomography (CT) can be used to detect occult triquetral fractures if clinical suspicion is high.
MRI may be used if carpal instability is suspected, concern exists for extrinsic carpal ligament injury, or if occult triquetral fractures are suspected with a negative CT scan [14, 16, 21]. Carpal instability, which can be present in volar cortical fractures, is best evaluated with MRI [21, 27]. MRI can also help identify any bony edema in occult fractures or abnormal vascularity—a potential consideration in the athletic population [13•, 18].
Treatment and Management
Nonsurgical management is recommended for the majority of triquetral fractures, especially for the dorsal cortical or nondisplaced fracture pattern. Triquetral fractures largely respond favorably to immobilization for 4–6 weeks as they become an asymptomatic fibrous union. In this way, most triquetral fractures are well tolerated even without a true bony union.
Depending on clinical suspicion, multiple views of plain film can be obtained and followed by more advanced imaging as necessary. Need for advanced imaging will largely depend on concomitant injuries and clinician judgment. First-line treatment is conservative with immobilization in a volar splint with the wrist in slight extension for a week. Once the swelling subsides, most authors state that the patient can be transitioned to a short arm cast [2, 3, 13•, 21]. At 4 weeks, they can be transitioned to a removable wrist splint and begin weight bearing with transition to all activities by 8 weeks out of the brace [3, 12, 21, 30].
Surgical treatment should be considered for fractures with significant displacement or those associated with fracture dislocation concerning for instability. For triquetral body fracture dislocations, Porter and Seehra reported good outcomes using an open dorsal approach with Herbert bone screw fixation followed by stabilization of the lunotriquetral joint with Kirschner wires (K-wires) from the triquetrum into the lunate. Final follow-up showed reduced wrist flexion by 20° and extension by 10° with no signs of instability [25].
To treat transverse body fractures in the context of perilunate dislocation, Leung et al. utilized multiple K-wires for fixation, while Rhind et al. stabilized the triquetral fracture using a headless compression screw [31, 32•]. Following surgery, Leung et al. immobilized the wrist and arm using a short arm cast for 6 weeks followed by a removable brace for 4 more weeks with the K-wires removed 8 weeks after the surgery. The recovery was overall satisfactory, and full return to physical activity was observed, with wrist flexion reduced by 10° and extension by 15 degrees at final follow-up [31]. On the other hand, Rhind et al. immobilized the wrist for only 6 weeks. Wrist flexion was reduced by 15° with no reduction in wrist extension after surgery [32•].
For triquetral body fractures extending into the pisotriquetral joint and associated with pisiform subluxation, Suzuki et al. showed that the surgical excision of the pisiform can result in the elimination of pain [23]. Gan et al. also showed that open reduction and internal fixation of the triquetrum with an interfragmentary screw can restore wrist function [33]. But for those without pisiform subluxation, Athanasiou et al. demonstrated that nonsurgical immobilization was sufficient even if the fracture extended into the pisotriquetral joint [22•].
Lunotriquetral ligament injury is known to be associated with triquetral body fractures and should be appropriately treated through pinning if unstable [2]. Other associated injuries include scaphoid fracture in the context of perilunate injury [18].
For triquetral fractures involving the volar cortex, treatment should focus on the restoration of carpal stability [21]. There is no consensus on whether such fractures require fixation. In their studies of volar cortical fractures caused by avulsion, Smith and Murray reported that neither nonsurgical splinting nor arthroscopic debridement with synovectomy eliminated pain and instability entirely 1 year after the injury [27]. Generally, surgical treatment should be considered if there is clinical concern for carpal instability or fracture dislocation.
Outcomes
Triquetral fractures can be treated satisfactorily with immobilization in most cases. Höcker and Menschik reported that 86% of patients in their study experienced significant pain reduction following 3 weeks of wrist immobilization [12]. For fracture patterns other than dorsal cortical, there have also been reports of good outcomes with 6 weeks of immobilization [22•, 24]. Supervised occupational therapy and wrist exercises are recommended [30]. It is reported that reduction in wrist pain and return of motion can be expected 6–8 weeks after beginning non-operative treatment [12].
Outcomes of surgical treatment are more variable as various methods of treatment have been reported. Studies reported different levels of recovery of wrist motion and function, but all recoveries were determined to be satisfactory [25, 31, 32]. Arthroscopic debridement with synovectomy, as reported by Smith and Murray, does not appear to lead to reliable pain relief at one year postop [27].
Complications
Overall, complications are rare, and most triquetral fractures can be treated as benign injuries with good results. However, it is important for clinicians to be mindful of concomitant injuries. Dorsal cortical fractures are associated with TFCC injury, which may necessitate TFCC debridement and synovectomy [34].
Triquetral fractures may occasionally result in fibrous non-union, but these are usually asymptomatic and patients are likely to have good functional outcomes in terms of pain reduction and recovery of wrist motion [3, 18, 21]. In the rare instance of a symptomatic non-union, a treatment option could be to excise the fracture fragment as done in hamate fractures [35]. Another option is to consider fixation using headless mini-compression screws [26]. Depending on the fracture pattern, both options appear supported by the literature and can be utilized as deemed appropriate by the treating surgeon [26, 35].
Pisotriquetral arthrosis may also develop as a result of a fracture extending into the pisotriquetral joint or from a rare symptomatic triquetrum non-union [22•, 23]. The incidence is not known. Pisiform excision can be considered for symptomatic pisotriquetral arthritis with good outcomes [36].
Conclusion
Triquetral fractures should be in the differential diagnosis for those presenting with ulnar-sided wrist pain in the context of falling on an outstretched hand, though scaphoid fractures are more common. Fractures are usually caused by indirect trauma through impaction of surrounding bony structures or by avulsion of attached ligaments to the triquetrum. Of the three types of triquetral fractures, the dorsal cortical fracture pattern is the most common type and the most well characterized in terms of diagnosis and treatment. While most triquetral fractures can be treated satisfactorily with immobilization, it is important to consider the mechanism of injury and surrounding soft tissue injury in pursuing further imaging. CT or MRI can be useful to determine occult fracture, instability, or ligament injury. Surgery is generally indicated for symptomatic nonunion, instability, or fracture dislocation. This can be either percutaneous pinning or open fixation with screws, with outcomes using either generally being satisfactory. There is no consensus on the best treatment for these fractures and further studies are needed to compare these treatments.
Data Availability
Not applicable.
Compliance with Ethical Standards
Conflict of Interest
Raymond Guo, Justin Cardenas, and Chia Wu declare that they have no conflict of interest.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Human and Animal Rights Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Raymond C. Guo, Email: Raymond.Guo@bcm.edu
Justin M. Cardenas, Email: justin.cardenas@bcm.edu
Chia H. Wu, Email: wu.chia.h@gmail.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Gray H. The carpus. In: Lewis WH, editor. Anatomy of the human body. 21. Philadelphia and New York: Lea & Febiger; 1924. pp. 224–225. [Google Scholar]
- 2.Suh N, Ek ET, Wolfe SW. Carpal Fractures. J Hand Surg Am. 2014;39(4):785–791. doi: 10.1016/j.jhsa.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 3.Christie BM, Michelotti BF. Fractures of the carpal bones. Clin Plast Surg. 2019;46(3):469–477. doi: 10.1016/j.cps.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 4.Raghupathi AK, Kumar P. Nonscaphoid carpal injuries – incidence and associated injuries. J Orthop. 2014;11(2):91–95. doi: 10.1016/j.jor.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Elias M, An K-N, Cooney WP, et al. Stability of the transverse carpal arch: an experimental study. J Hand Surg Am. 1989;14(2, Part 1):277–282. doi: 10.1016/0363-5023(89)90021-x. [DOI] [PubMed] [Google Scholar]
- 6.Ambrose L, Posner MA. Lunate-triquetral and midcarpal joint instability. Hand Clin. 1992;8(4):653–668. [PubMed] [Google Scholar]
- 7.Helms JT, Maldonado, KA, Burns B. Anatomy, shoulder and upper limb, hand Radiocarpal joint. In: StatPearls. StatPearls Publishing. 2020. http://www.ncbi.nlm.nih.gov/books/NBK539744/. Accessed 10 April 2020. [PubMed]
- 8.Bateni CP, Bartolotta RJ, Richardson ML, Mulcahy H, Allan CH. Imaging key wrist ligaments: what the surgeon needs the radiologist to know. AJR Am J Roentgenol. 2013;200(5):1089–1095. doi: 10.2214/AJR.12.9738. [DOI] [PubMed] [Google Scholar]
- 9.Sandman E, Boily M, Martineau PA. “Hockey wrist”: dorsal ulnotriquetral ligament injury. Can J Surg. 2018;61(6):398–404. doi: 10.1503/cjs.012917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown RR, Fliszar E, Cotten A, Trudell D, Resnick D. Extrinsic and intrinsic ligaments of the wrist: normal and pathologic anatomy at MR arthrography with three-compartment enhancement. RadioGraphics. 1998;18(3):667–674. doi: 10.1148/radiographics.18.3.9599390. [DOI] [PubMed] [Google Scholar]
- 11.Ng AWH, Griffith JF, Fung CSY, et al. MR imaging of the traumatic triangular fibrocartilaginous complex tear. Quant Imaging Med Surg. 2017;7(4):443–460. doi: 10.21037/qims.2017.07.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Höcker K, Menschik A. Chip fractures of the triquetrum. Mechanism, classification and results. J Hand Surg Br. 1994;19(5):584–588. doi: 10.1016/0266-7681(94)90120-1. [DOI] [PubMed] [Google Scholar]
- 13.Mahmood B, Lee SK. Carpal fractures other than scaphoid in the athlete. Clin Sports Med. 2020;39(2):353–371. doi: 10.1016/j.csm.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Urch EY, Lee SK. Carpal fractures other than scaphoid. Clin Sports Med. 2015;34(1):51–67. doi: 10.1016/j.csm.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Elias M. Dorsal fractures of the triquetrum—avulsion or compression fractures? J Hand Surg Am. 1987;12(2):266–268. doi: 10.1016/s0363-5023(87)80285-x. [DOI] [PubMed] [Google Scholar]
- 16.Becce F, Theumann N, Bollmann C, Omoumi P, Richarme D, Guerini H, Campagna R, Meuli R, Drapé JL. Dorsal fractures of the Triquetrum: MRI findings with an emphasis on dorsal carpal ligament injuries. AJR Am J Roentgenol. 2013;200(3):608–617. doi: 10.2214/AJR.12.8736. [DOI] [PubMed] [Google Scholar]
- 17.Vigler M, Aviles A, Lee SK. Carpal fractures excluding the scaphoid. Hand Clin. 2006;22(4):501–516. doi: 10.1016/j.hcl.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Marchessault J, Conti M, Baratz ME. Carpal fractures in athletes excluding the scaphoid. Hand Clin. 2009;25(3):371–388. doi: 10.1016/j.hcl.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 19.Levy M, Fischel RE, Stern GM, Goldberg I. Chip fractures of the os triquetrum: the mechanism of injury. J Bone Joint Surg Br. 1979;61-B(3):355–357. doi: 10.1302/0301-620X.61B3.479259. [DOI] [PubMed] [Google Scholar]
- 20.Bonnin JG, Greening WP. Fractures of the triquetrum. Br J Surg. 1944;31(123):278–283. doi: 10.1002/bjs.18003112314. [DOI] [Google Scholar]
- 21.Wolfe SW. Fractures of the Carpal Bones. In: Pederson WC, Hotchkiss RN, Kozin SH, Cohen MS, editors. Green’s Operative Hand Surgery E-Book: Elsevier Health Sciences; 2016. p. 624–6.
- 22.Athanasiou V, Panagopoulos A, Iliopoulos ID, et al. Intra-articular fracture of the distal part of the triquetrum within the pisotriquetral joint: case report and review of literature. Open Orthop J. 2018;12:84–90. doi: 10.2174/1874325001812010084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suzuki T, Nakatsuchi Y, Tateiwa Y, Tsukada A, Yotsumoto N. Osteochondral fracture of the triquetrum: a case report. J Hand Surg Am. 2002;27(1):98–100. doi: 10.1053/jhsu.2002.28944. [DOI] [PubMed] [Google Scholar]
- 24.Horras N, Barthlen W, Wildbrett P. A rare case of an isolated triquetrum body fracture in a 14-year-old boy. Afr J Paediatr Surg. 2012;9(2):157. doi: 10.4103/0189-6725.99405. [DOI] [PubMed] [Google Scholar]
- 25.Porter M, Seehra K. Fracture-dislocation of the triquetrum treated with a Herbert screw. J Bone Joint Surg Br. 1991;73-B(2):347–348. doi: 10.1302/0301-620X.73B2.2005177. [DOI] [PubMed] [Google Scholar]
- 26.Rasoli S, Ricks M, Packer G. Isolated displaced non-union of a triquetral body fracture: a case report. J Med Case Rep. 2012;6:54. doi: 10.1186/1752-1947-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith DK, Murray PM. Avulsion fractures of the volar aspect of triquetral bone of the wrist: a subtle sign of carpal ligament injury. AJR Am J Roentgenol. 1996;166(3):609–614. doi: 10.2214/ajr.166.3.8623636. [DOI] [PubMed] [Google Scholar]
- 28.Welling RD, Jacobson JA, Jamadar DA, Chong S, Caoili EM, Jebson PJL. MDCT and radiography of wrist fractures: radiographic sensitivity and fracture patterns. AJR Am J Roentgenol. 2008;190(1):10–16. doi: 10.2214/AJR.07.2699. [DOI] [PubMed] [Google Scholar]
- 29.•• Krastman P, Mathijssen NM, Bierma-Zeinstra SMA, et al. Diagnostic accuracy of history taking, physical examination and imaging for phalangeal, metacarpal and carpal fractures: a systematic review update. BMC Musculoskelet Disord. 2020;21. 10.1186/s12891-019-2988-zThis article demonstrates that advanced imaging may be necessary to visualize occult triquetral fractures. The authors report that the sensitivity of repeated physical and x-ray examination after initial examination in detecting triquetral fractures can be less than the sensitivity of repeated examination in detecting other carpal fractures. [DOI] [PMC free article] [PubMed]
- 30.Titus SJ, Scott DW. Chapter 18 - wrist and hand fractures. In: Seidenberg PH, Beutler AI, editors. The sports medicine resource manual. Philadelphia: W.B. Saunders; 2008. pp. 178–199. [Google Scholar]
- 31.Leung YF, Ip SPS, Wong A, et al. Trans-triquetral dorsal perilunate fracture dislocation. J Hand Surg Eur Vol. 2007;32(6):647–648. doi: 10.1016/j.jhse.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Rhind J-H, Gulihar A, Smith A. Trans-triquetral Perilunate fracture dislocation. Trauma Case Rep. 2018;14:27–30. doi: 10.1016/j.tcr.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gan LP, Satkunanantham M, Sreedharan S, et al. Triquetral fracture with associated pisiform subluxation. Singapore Med J. 2015;56:39–41. doi: 10.11622/smedj.2015049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee S, Rathod CM, Park K-W, Hwang JH. Persistent ulnar-sided wrist pain after treatment of triquetral dorsal chip fracture: six cases related to triangular fibrocartilage complex injury. Arch Orthop Trauma Surg. 2012;132(5):671–676. doi: 10.1007/s00402-011-1416-0. [DOI] [PubMed] [Google Scholar]
- 35.Geissler WB. Carpal fractures in athletes. Clin Sports Med. 2001;20(1):167–188. doi: 10.1016/s0278-5919(05)70254-4. [DOI] [PubMed] [Google Scholar]
- 36.Aiki H, Wada T, Yamashita T. Pisotriquetral Arthrosis after Triquetral Malunion: a case report. J Hand Surg Am. 2006;31(7):1157–1159. doi: 10.1016/j.jhsa.2006.05.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


