Abstract
Background: Coronavirus disease (COVID-19) is an infectious disease caused by SARS-CoV-2, clinically presenting with common symptoms of fever, dry cough, and breathlessness within 14 days of exposure. Its severity ranges from mild to severe, latter manifesting into severe acute respiratory syndrome. As a part of multidisciplinary team, physiotherapy along with medical management was administered to patients with COVID-19 in an acute care setup. This retrospective study aims to explore various patient characteristics and will aid in identifying the impairments associated with the disease, giving a direction to the physiotherapy community in planning future management strategy to improve quality of life.
Patients and methods: The present study is a unicentric study wherein prospective analysis of retrospective data of patients referred for physiotherapy from May 13 to July 31, 2020, was performed. (i) Characteristics of patients, (ii) associated comorbidities, (iii) hospital course since the time of admission to discharge, (iv) mode of oxygen delivery, (v) pre- and post-physiotherapy treatment values of oxygen saturation and heart rate, and (vi) physiotherapy treatment were recorded. The archived data were analyzed using the commercially available SPSS software version 24. Wilcoxon's matched pair test was used to compare pre- and post-treatment oxygen saturation and heart rate, and McNemar's test was used to compare mode of oxygen delivery and pre- and post-physiotherapy treatment.
Results: Descriptive analysis of data showed a better outcome in terms of grade of dyspnea and rate of discharge on day 14 of physiotherapy treatment. Hence, a comparative analysis of day 1 and day 14 was performed for mode of oxygen delivery, oxygen saturation, and heart rate. A statistically significant improvement was observed in the heart rate (p = 0.001) and oxygen delivery (p = 0.000). However, no significant difference in the level of oxygen saturation was found (p = 0.6433).
Conclusion: Physiotherapy treatment in conjunction with medical treatment can be effectively administered in patients with COVID-19 in acute care setup taking into consideration the health status and the hemodynamic stability of the patients. It emphasizes the role of physiotherapy in the alleviation of symptoms, facilitating early weaning and recovery enabling early discharge from the hospital.
How to cite this article: Verma CV, Arora RD, Mistry HM, Kubal SV, Kolwankar NS, Patil PC, et al. Changes in Mode of Oxygen Delivery and Physiological Parameters with Physiotherapy in COVID-19 Patients: A Retrospective Study. Indian J Crit Care Med 2021;25(3):317–321.
Keywords: COVID-19, Heart rate, Mode of oxygen delivery, Oxygen saturation, Physiotherapy, Retrospective study
INTRODUCTION
COVID-19 caused by the novel SARS-CoV-2 has affected thousands of lives and presented as an unprecedented challenge for the healthcare system worldwide. India reported its first case of COVID-19 in Kerala on January 30, 2020.1 It was declared a pandemic by the World Health Organization (WHO) on March 11, 2020.2 In order to control a rapid escalation of COVID cases, the Government of India declared a nation-wide lockdown on March 25, 2020.1 Thereafter, within a month, Maharashtra recorded 9,915 COVID cases with Mumbai emerging as an epicenter recording 6,457 cases.3
Patients with COVID-19 present with a wide array of clinical manifestations ranging from mild symptoms of fever, dry cough, and breathlessness to severe fulminating ARDS. Physiotherapists have always been an essential part of the multidisciplinary team in the intensive care unit, playing a role in promoting lung function, maintaining bronchial hygiene, preventing secondary complications of physical deconditioning, facilitating early weaning, and reducing hospital stay.4,5
Chest physiotherapy services and rehabilitation were initiated at our municipal tertiary care hospital on May 13, 2020, wherein physiotherapy treatment was administered with strict monitoring of vitals on one-to-one basis considering the patient's health status and dependency on supplemental oxygen under the guidance of the treating physician.6 In consideration of the pathophysiology of COVID-19, primarily leading to hypoxemia, external oxygen supplementation is essential in the management of patients.7,8 Mode of oxygen delivery is defined as the administration of oxygen at a concentration greater than that found in ambient air with a primary goal of treating or preventing hypoxemia, thus preventing tissue injury or cell death.9 Oxygen delivery systems are categorized into low-flow (nasal cannula, bag and mask rebreather ventilation) and high-flow oxygen systems (BiPAP, CPAP, APAP, HFNC, mechanical ventilation). The selection of appropriate oxygen delivery system depends upon diagnosis, its severity, and degree of hypoxemia. Maximal ventilatory support is administered in a patient through invasive mechanical ventilation (endotracheal intubation or tracheostomy), followed by noninvasive ventilation (HFNC, rebreather mask, and nasal cannula).10
The purpose of this study is to explore various characteristics of patients referred for physiotherapy including demographics, presenting symptoms, comorbidities, length of hospital stay, duration of physiotherapy treatment, and the progression of patient condition in terms of changes observed in the mode of oxygen delivery, concentration of oxygen supplementation, and heart rate owing to physiotherapy treatment in conjunction with medical management. This retrospective study of the data recorded in the span of 10 weeks (May 13 to July 31, 2020) will aid us to identify the impairments associated with the disease and will provide a direction to the physiotherapy community in planning future strategy in physiotherapy management to improve the overall quality of life.
METHODOLOGY
The present retrospective study was conducted at a dedicated COVID municipal tertiary care hospital in a metropolitan city of Mumbai after seeking approval from the Institutional Ethics Committee. Nonprobability convenient sampling technique was used following which a prospective analysis of retrospective data of patients referred for physiotherapy from May 13 to July 31, 2020, was performed. The study population consisted of 3,251 patients who had tested positive for COVID-19 on RT-PCR. After excluding patients whose data were incomplete, 433 adult patients referred for physiotherapy by the treating physician were included in the study. The recorded data comprised of (i) characteristics of patients (demographic data) and grade of dyspnea, (ii) comorbidities, (iii) hospital course including admission and discharge, (iv) mode of oxygen delivery, (v) Pre-treatment and post-treatment values of heart rate, (vi) concentration of oxygen supplementation of day 1 and day 14, and (vii) physiotherapy treatment. The health status of the referred patients was considered, and physiotherapy treatment was administered under complete supervision and continuous monitoring of oxygen saturation and heart rate as per our institutional guidelines.11
Physiotherapy treatment strategy planned for the management of patients as shown in Flowchart 1 was in accordance with our institutional guidelines and was tailored according to the patient's condition and complaints. With an aim of alleviating symptoms and restoring functional independence in the basic ADLs of the patient, physiotherapeutic interventions inclusive of chest physiotherapy along with active mobility exercises were advised to the patient and were progressed according to the patient's health status and hemodynamic stability. All the patients referred for physiotherapy received treatment once a day for 6 days a week.
Flowchart 1.
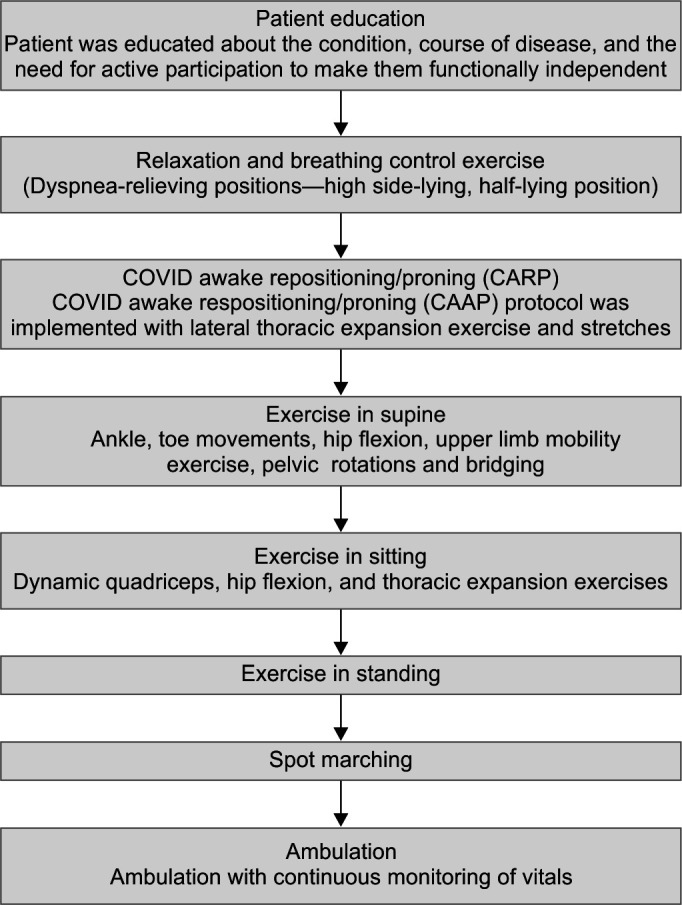
Physiotherapy treatment strategy
Patients were given breathing control and thoracic expansion in dyspnea relieving positions like forward lean sitting and high side-lying position. This helped in improving the ventilation to the lower zones of the lungs, thereby improving gas exchange.12,13 It also helped in reducing anxiety and apprehension seen in the patients. COVID Awake Repositioning/Proning Protocol (CARP) was given every 2 hours.13 In this protocol, the position, i.e., prone, left side lying, upright, and right side lying, was changed every 2 hours. Patients who were able to perform active movements against gravity (manual muscle testing grade III) were given active exercise. Exercises were given in supine position and progressed to sitting, standing, spot marching, and walking. Oxygen saturation and heart rate were monitored throughout the session. Adequate rest pauses were given in between exercises. Exercises were terminated if oxygen saturation dropped by more than 3% or if it dropped below 90% and if heart rate increased above 100 bpm in elderly and 120 bpm in young adults. Oxygen supplementation was increased prior to exercise to prevent exercise-induced hypoxia.14 The data inclusive of mode of oxygen delivery, amount of oxygen supplementation, heart rate, and oxygen saturation of all the patients were monitored and documented on the daily basis.
The archived data segregated in the Excel sheets were analyzed using commercially available software, SPSS (V24, 2016). Descriptive analysis was performed, and data were tested for normality distribution using the Kolmogorov–Smirnov test.
As the data did not pass normality, Wilcoxon's matched pair test was used to compare the pre- and post-values of heart rate and oxygen supplementation for day 1 and day 14. McNemar's test was used to compare the pre- and post-supplemental oxygen status expressed as dichotomous data in terms of Yes/No.
RESULTS
A total of 3,251 COVID-positive patients were admitted in the span of 10 weeks from May 13 to July 31, 2020, of which 433 patients with a mean age of 53.88 ± 13.44 years were referred for physiotherapy by the treating physicians. Out of these 433 patients, 68.82% (n = 298) patients were males and 31.17% (n = 135) were females. Majority of the patients (77.82%) presented with comorbidities, most commonly diabetes mellitus (30.25%) and hypertension (32.10%). Both diabetes mellitus and hypertension were reported in 15.47% of patients, whereas 22.18% reported no comorbidities. Patients requiring intensive care constituted 37.87% (n = 164) of the sample, and the remaining 62.12% (n = 269) were managed in COVID wards. Length of hospital stay ranged from 2–62 days with a mean of 18.39 ± 9.49 days. The day on which patients were referred for physiotherapy after hospital admission varied from 1–30 days with a mean of 7.67 ± 5.47 days. Physiotherapy treatment was administered for a period of 11–47 days with a mean of 11.84 ± 7.6 days. It was observed that maximum number of patients were discharged on day 7 and day 14 of physiotherapy treatment as shown in Figure 1.
Fig. 1.
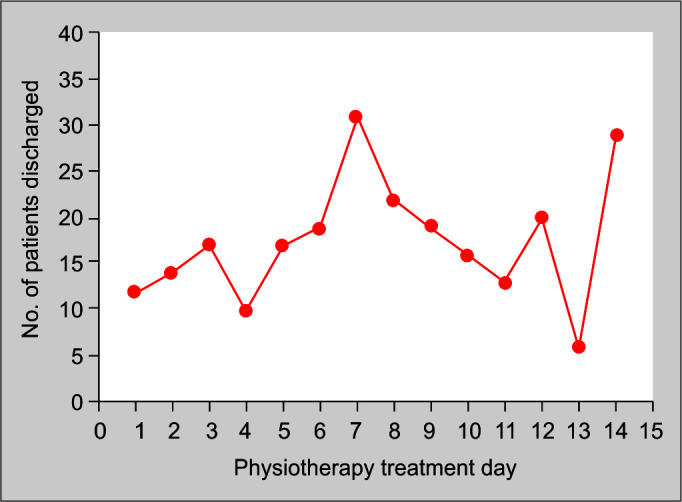
Discharge in accordance with the day of physiotherapy treatment
Within 14 days of commencement of physiotherapy treatment, 56.58% (n = 245) patients were discharged and 10.39% (n = 45) succumbed to the disease, whereas after 14 days of commencement of physiotherapy treatment, 32.56% (n = 141) got discharged and 0.47% (n = 2) succumbed to the disease. Out of the 433 patients, 89.15% (n = 386) patients were discharged, whereas 10.85% (n = 47) succumbed to the disease.
Dyspnea was graded using the modified Medical Research Council (mMRC) scale. On day 1 of physiotherapy treatment, 19.39% (n = 84) patients presented with grade IV dyspnea, 25.17% (n = 109) presented with grade III dyspnea, 31.17% (n = 135) presented with grade II dyspnea, and 19.63% (n = 85) presented with grade I dyspnea. After the implementation of physiotherapy treatment with medical management, considerable improvement was observed in the patients on day 14 with only 7.62% (n = 33) reporting grade IV dyspnea, 3.23% (n = 14) reporting grade III dyspnea, 0.46% (n = 2) reporting grade II dyspnea, and 2.54% (n = 11) reporting grade I dyspnea. A significantly higher number of patients with no symptoms of dyspnea were observed on day 14 (86.14%, n = 373) as compared to day 1 (4.61%, n = 20) of physiotherapy treatment.
Owing to a better outcome in terms of grade of dyspnea and rate of discharge observed on day 14 of physiotherapy treatment, a further comparative analysis of day 1 and day 14 was performed for mode of oxygen delivery as shown in Figure 2, concentration of oxygen supplementation, and heart rate as seen in Tables 1–3, respectively.
Fig. 2.
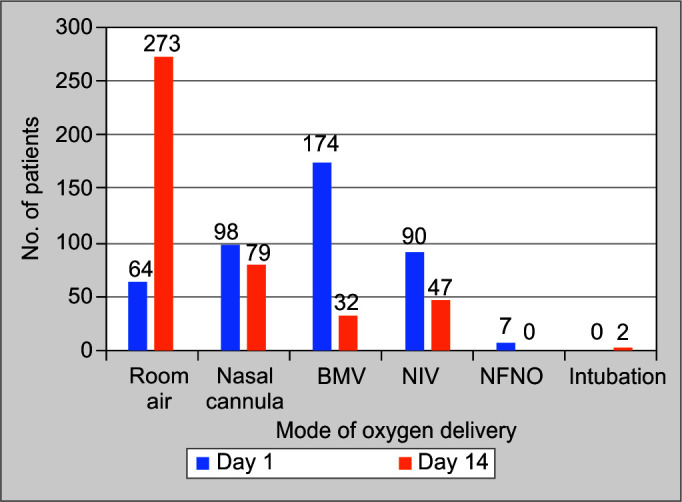
Comparison of modes of oxygen delivery
Table 1.
Comparison of mode of oxygen delivery
| Type of oxygen delivery | Day 1 of PT treatment | Day 14 of PT treatment | p value (McNemar's test) |
|---|---|---|---|
| Room air | 64 (14.78%) | 273 (63.04%) | 0.000 (significant) |
| Nasal cannula | 98 (22.63%) | 79 (18.24%) | |
| Bag and mask ventilation | 174 (40.18%) | 32 (7.39%) | |
| NIV | 90 (20.78%) | 47 (10.85%) | |
| HFNC | 7 (1.61%) | 0 | |
| Intubated | 0 | 2 (0.46%) |
Table 3.
Comparison of heart rate
| Day 1 of PT treatment | Day 14 of PT treatment | p value | |
|---|---|---|---|
| Number of values | 433 | 433 | 0.001 (significant) |
| Mean | 92.46 | 100.4 | |
| Std deviation | 14.93 | 13.25 | |
| Minimum | 53.00 | 65.00 | |
| Median | 92.00 | 99.00 | |
| Maximum | 154.0 | 148.0 | |
| Range | 101.0 | 83.00 |
Table 2.
Comparison of concentration of oxygen supplementation
| Day 1 of PT treatment | Day 14 of PT treatment | p value | |
|---|---|---|---|
| Number of values | 433 | 433 | 0.000 (significant) |
| Mean | 60.9606 | 34.7685 | |
| Std. deviation | 25.39 | 24.9882 | |
| Minimum | 20.00 | 20.00 | |
| Median | 60.00 | 20.00 | |
| Maximum | 100.0 | 100.0 | |
| Range | 80 | 80 |
DISCUSSION
In view of the characteristics of the population, the data collected and analyzed in the present study were in conjunction with studies conducted by Sharma et al., Argenziano et al., and Yao et al.12,15,15 wherein they studied the characteristics, clinical course, and outcomes in adult patients with COVID-19. Majority of the patients included in this study were males (68.82%), in the middle age-group (40–60 years) with comorbidities (77.83%). The cohort reported high rates of comorbidities mainly hypertension, diabetes mellitus, or both. The literature has shown a higher predisposition of males to COVID-19 owing to factors including sex hormones, addictions, and comorbidities (most commonly diabetes mellitus and hypertension).17
A study by Argenziano et al. reported that 23.6% of patients with COVID-19 required intensive care, whereas 61.4% were managed in the COVID wards, which was in consensus with our study where 37. 87% and 62.12% were admitted in ICUs and wards, respectively. The median overall length of hospital stay was observed to be 17 days, which was comparable to two cohorts, in China (12 days) and New York (23 days).15,18
The management plan for the patients who tested positive for COVID on RT-PCR was formulated by the treating physicians on the basis of clinical and radiological findings mainly HRCT. After ensuring hemodynamic stability, patients were referred for physiotherapy treatment by the treating physician approximately within a span of 2–12 days from the day of hospital admission. On the first day of referral, majority of the patients complained of grade III dyspnea on mMRC. The patients received supplementary oxygen through invasive or noninvasive modes of ventilation with majority receiving oxygen through bag and mask ventilation. The physiotherapy treatment was planned on the basis of our institutional guidelines, and the exercise protocol was tailored according to the patient's condition and complaints.
Patients referred after attaining hemodynamic stability after 14 days of hospital admission showed favorable results. A significant increase in the heart rate of the patients immediately post-physiotherapy treatment was observed owing to the increase in the metabolic demand during physiotherapy exercises. Studies have suggested that chest physiotherapy accelerates depolarization of the sinoatrial node by stimulating the sympathetic nerves along with the release of catecholamine, which collectively causes an increase in the heart rate as observed in our study.19
Not many studies have been conducted on the required span of physiotherapy treatment in COVID-19 patients. This study showed a mean of physiotherapy treatment till discharge to be 12 days, with maximum patients discharged between day 7–8 and day 14–15 after physiotherapy treatment.
Frequency and intensity of the physiotherapy protocol are shown to be responsible for the increased rate of discharge from the hospital. In this study, more than 50% of patients were discharged within 14 days, while around 32.56% were discharged after 14 days of physiotherapy treatment.20
A significant improvement in the grade of breathlessness was observed with 86.14% of patients having no breathlessness after 14 days of physiotherapy treatment, which was only 4.61% before the physiotherapy referral.
The present study showed a significant improvement in the mode of oxygen delivery and concentration of oxygen supplementation on day 14 as compared to that on day 1. An observational study conducted in 2013 similarly showed a reduced need of mechanical ventilation in ICU patients and early rate of recovery with a reduced hospital stay, owing to frequent physiotherapy sessions (approximately half the period of hospital stay).21
CONCLUSION
Thus, our retrospective study concluded that physiotherapy treatment in conjunction with medical treatment is advisable to be administered in patients with COVID-19 in acute care setup taking into consideration the health status and the hemodynamic stability of the patients. Additionally, it emphasizes the role of physiotherapy in the alleviation of symptoms, facilitating early weaning and recovery enabling early discharge from the hospital.
Footnotes
Source of support: Nil
Conflict of interest: None
Orcid
Chhaya V Verma https://orcid.org/0000-0002-3432-0251
Rachna D Arora https://orcid.org/0000-0001-7724-2823
Hetal M Mistry https://orcid.org/0000-0002-8449-0259
Swati V Kubal https://orcid.org/0000-0003-4783-8217
Nandini S Kolwankar https://orcid.org/0000-0002-6994-1699
Pranali C Patil https://orcid.org/0000-0002-2030-0452
Anushka A Dalvi https://orcid.org/0000-0002-7831-9156
Sonal A Vichare https://orcid.org/0000-0002-7396-6901
Akhila Natesan https://orcid.org/0000-0002-4298-9473
Anagha N Mangaonkar https://orcid.org/0000-0003-3518-317X
Dolly D Kanakia https://orcid.org/0000-0003-2039-5073
Gayatri S Jere https://orcid.org/0000-0002-1986-9510
Karan Y Bansode https://orcid.org/0000-0001-6326-778X
Madhura R Patil https://orcid.org/0000-0002-6127-7826
Rajvi D Sheth https://orcid.org/0000-0001-6474-0700
Sandhya D Dudhavade https://orcid.org/0000-0002-3798-9401
Sayali D Mhatre https://orcid.org/0000-0001-7337-7560
Suresh K Patel https://orcid.org/0000-0001-9687-4885
Akanksha G Mohite https://orcid.org/0000-0002-2808-4387
Ankita N Bhavsar https://orcid.org/0000-0003-1056-3571
Jessica E Alfonso https://orcid.org/0000-0002-2029-1605
Maryam NA Syed https://orcid.org/0000-0002-2186-0937
Nidhi P Savla https://orcid.org/0000-0002-3225-0202
Riya N Rajgond https://orcid.org/0000-0003-2773-8905
Rutuja A Bute https://orcid.org/0000-0002-5156-9753
Samiksha M Mane https://orcid.org/0000-0003-1241-3550
Shubham R Jaiswal https://orcid.org/0000-0003-2784-3721
Vibhawari A Parab https://orcid.org/0000-0002-3409-3458
Abhiram M Kasbe https://orcid.org/0000-0001-9146-8458
Mohan A Joshi https://orcid.org/0000-0003-2479-5314
Ramesh N Bharmal https://orcid.org/0000-0002-4702-0362
References
- 1.https://thewire.in/covid-19-india-timeline. Sep 18,, 2020].. https://thewire.in/covid-19-india-timeline [Last accessed on.
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;;91((1):):157––160.. doi: 10.23750/abm.v91i1.9397. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Municipal Corporation Greater Mumbai—Public Health Department COVID 19 daily update dated 29-04-2020. Sep 18,, 2020].. [Last accessed on.
- 4.Bonvento B, Wallace S, Lynch J, Coe B, McGrath BA. Role of the multidisciplinary team in the care of the tracheostomy patient. J Multidiscip Healthc. 2017;;10::391––398.. doi: 10.2147/JMDH.S118419. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.physio-pedia.com/Physiotherapists_Role_in_ICU. Sep 18,, 2020].. physio-pedia.com/Physiotherapists_Role_in_ICU [Last accessed on.
- 6.Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL et al. Physiotherapy management for COVID-19 in the acute hospital setting: recommendations to guide clinical practice. J Physiother. 2020;;33((1).) doi: 10.1016/j.jphys.2020.03.011. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;;215::108427.. doi: 10.1016/j.clim.2020.108427. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;;324((8):):782––793.. doi: 10.1001/jama.2020.12839. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Singh V, Gupta P, Khatana S, Bhagol A. Supplemental oxygen therapy: important considerations in oral and maxillofacial surgery. Natl J Maxillofac Surg. 2011;;2((1):):10––14. 10–4.. doi: 10.4103/0975-5950.85846. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tabashi S, Mirkheshti A, Dahi M, Abtahi D, Vosoughian M, Sayyadi S. Supplemental oxygen therapy and non-invasive ventilation in corona virus disease (COVID-19). J Cell Mol Anesth. 2020;;5((1):):27––31.. doi: 10.22037/jcma.v5i1.29689. DOI: [DOI] [Google Scholar]
- 11.Verma CV, Arora RD, Shetye JV, Karnik ND, Patil PC, Mistry HM et al. Guidelines of physiotherapy management in acute care of COVID-19 at dedicated COVID-19 centre in Mumbai. Physiother J Indian Assoc Physiother. 2020;;14((1):):55––60.. doi: 10.4103/PJIAP.PJIAP_33_20. DOI: [DOI] [Google Scholar]
- 12.Sharma AK, Ahmed A, Baig VN, Dhakad P, Dalela G, Kacker S et al. Characteristics and outcomes of hospitalized young adults with mild to moderate covid-19 at a University Hospital in India. medRxiv. 2020 Jan 1.; doi: 10.1101/2020.06.02.20106310. DOI: [DOI] [PubMed] [Google Scholar]
- 13.Weatherald J, Solverson K, Zuege DJ, Loroff N, Fiest KM, Parhar KK. Awake prone positioning for COVID-19 hypoxemic respiratory failure: a rapid review. J Crit Care. 2021;;61::63––70.. doi: 10.1016/j.jcrc.2020.08.018. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenhalgh T, Javid B, Knight M, Inada-Kim M. What is the efficacy and safety of rapid exercise tests for exertional desaturation in covid-19? Centre Evid Based Med. 2020;:1––9.. doi: 10.13140/RG.2.2.23706.80325. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Argenziano MG, Bruce SL, Slater CL, Tiao, Baldwin MR, Barr RG. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;:369.. doi: 10.1136/bmj.m1996. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yao Q, Wang P, Wang X, Qie G. Retrospective study of risk factors for severe SARS-Cov-2 infections in hospitalized adult patients. Polish Arch Intern Med. 2020;;130((5).) doi: 10.20452/pamw.15312. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Bwire GM. Coronavirus: why men are more vulnerable to covid-19 than women? SN Compr Clin Med. 2020::1––3.. doi: 10.1007/s42399-020-00341-w. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;;382((18):):1708––1720.. doi: 10.1056/NEJMoa2002032. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McArdle WD, Katch IF, Katch LV. 4th ed. Lippincott Williams and Wilkins;; 2001.. Exercise physiology; energy, nutrition and human performance. [Google Scholar]
- 20.Hartley P, Adamson J, Cunningham C, Embleton G, Romero-Ortuno R. Higher physiotherapy frequency is associated with shorter length of stay and greater functional recovery in hospitalized frail older adults: a retrospective observational study. J Frailty Aging. 2016;;5((2):):121––125.. doi: 10.14283/jfa.2016.95. DOI: [DOI] [PubMed] [Google Scholar]
- 21.Bernardi L, Spadacini G, Bellwon J, Hajric R, Roskamm H, Frey AW. Effect of breathing rate on oxygen saturation and exercise performance in chronic heart failure. Lancet. 1998;;351((9112):):1308––1311.. doi: 10.1016/S0140-6736(97)10341-5. DOI: [DOI] [PubMed] [Google Scholar]


