Abstract
Background/aim
COVID-19 has become the biggest health problem of this century. It has been hypothesized that immunity against hepatitis A virus (HAV) may provide protection from COVID- 19.
Materials and methods
As of 10June 2020, the infection had spread to 213 countries, with 7.3 million people infected and 413,733 dead. This data was combined with the World Health Organization susceptibility classification on the worldwide prevalence of HAV, and the relationship between HAV susceptibility and COVID-19 mortality were analyzed.
Results
When the data from 213 countries were analyzed, it was found that there was a significant increasing trend in COVID-19 mortality rates by HAV susceptibility (P <0.001). Using a cut-off of 200/million population, the mortality risk associated with living in a more susceptible country (medium/high) was 27.8 times higher (95% CI for OR: 3.6–213.2)
Conclusion
The results of this study showed that, despite confounding factors in different countries, hepatitis A susceptibility of the population may have been correlated with COVID-19 mortality. This observation needs to be confirmed by further studies.
Keywords: Hepatitis A, COVID-19, vaccine, mortality
To the Editor,
The COVID-19 pandemic has become the biggest health problem of this century. Several factors have caused the impact of the disease to vary among countries. It had been previously hypothesized that immunity against hepatitis A virus (HAV) may provide protection from COVID-19 [1], and herein, it was aimed to support this hypothesis with data.
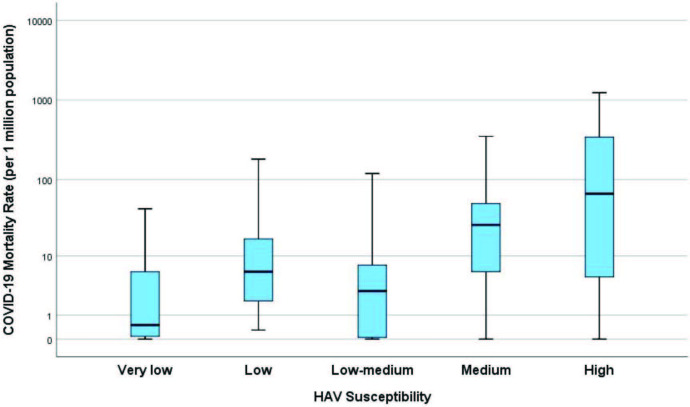
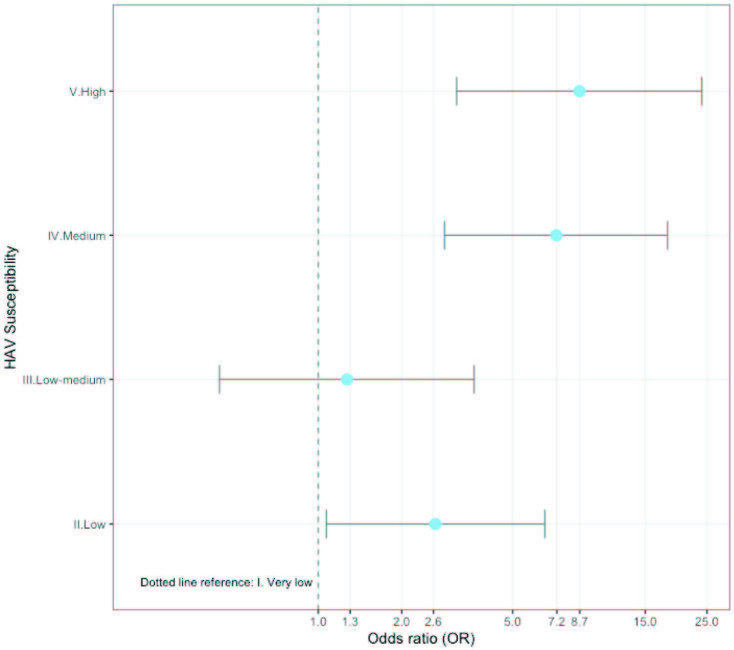
As of 10 June 2020, the infection had spread to 213 countries, with 7.3 million people infected and 413,733 dead Worldometer (2020).Coronavirus COVID-19 Statistics [online]. Website https://www.worldometers.info/coronavirus/ [accessed 10 June 2020].. This publicly available data was combined with the World Health Organization susceptibility classification published in 2009 on the worldwide prevalence of hepatitis A [2]. Figures 1 and 2 show the significant increasing trend in COVID-19 mortality rates by HAV susceptibility (P <0.001, Jonckheere–Terpstra test). Moreover, using a cut-off of 200/million population,the mortality risk associated with living in a more susceptible country (medium/high) was 27.8 times higher (95%CI for OR: 3.6–213.2) (Table).
Figure 1.
Box plots showing the increasing mortality trend by increasing HAV susceptibility in the 213 countries affected by the virus. If the data is limited to countries with more than 1 million population, 5 million population and 5000 tests/1 million population, the associated risk with increasing HAV susceptibility is even stronger (Supplementary file). The analyses do not take into account several confounding factors that may affect the death rates, including, but not limited to, socioeconomic status, accessibility of health services, and government pandemic policies. For example, Australia, New Zealand, Singapore, Japan, and South Korea are countries with excellent policies against the COVID-19 pandemic and have low mortality rates in the high susceptibility group. In contrast, countries with serious socioeconomic problems, such as Ecuador and Peru, have high mortality rates in the low susceptibility group. These are examples of a possible bias towards the null, while it is accepted that other sources of bias away from the null may exist.
Figure 2.
Increased risk of high mortality by increasing HAV susceptibility. High mortality is defined as having a mortality rate of more than 7/million (the median of 213 countries). The plotted ORs were from the univariate logistic regression model. The reference is the very low susceptibility group. Countries in the medium and high HAV-susceptible groups may be observed to have 7–8 times higher risk when compared to the reference (very low susceptibility) group.
Table.
Risk associated with high or medium HAV susceptibility in the countries by subgroups.
| Mortality rate | Mortality rate | |||||||
|---|---|---|---|---|---|---|---|---|
| <200 per million | ≥200 per million | OR (95% CI) | <7/million | ≥7/million | OR (95%CI) | All countries | ||
| All countries(N = 213) | Very low, low, or low-medium | 121 | 1 | Reference | 80 | 42 | Reference | 122 |
| Medium or high | 74 | 17 | 27.8 (3.6–213.2) | 26 | 65 | 4.76 (2.6–8.6) | 91 | |
| Total | 195 | 18 | 106 | 107 | 213 | |||
| Countries with >1 million population | Very low, low, or low-medium | 106 | 1 | Reference | 70 | 37 | Reference | 107 |
| Medium or high | 38 | 11 | 30.7 (3.8–245.7) | 8 | 41 | 9.69 (4.1–22.8) | 49 | |
| Total | 144 | 12 | 78 | 78 | 156 | |||
| Countries with >5 million population | Very low, low, or low-medium | 85 | 1 | Reference | 58 | 28 | Reference | 86 |
| Medium or high | 26 | 10 | 32.6 (4.00–267.5) | 6 | 30 | 10.4 (3.9–27.8) | 36 | |
| Total | 111 | 11 | 64 | 58 | 122 | |||
| Countries with >5000 tests/1 million population | Very low, low, or low-medium | 50 | 1 | Reference | 26 | 25 | Reference | 51 |
| Medium or high | 61 | 17 | 13.9 (1.8–108.4) | 18 | 60 | 3.5 (1.6–7.4) | 78 | |
| Total | 111 | 18 | 44 | 85 | 129 | |||
Association of high HAV susceptibility and high COVID-19 mortality holds in different subgroups. Two cut-offs were used: 7 (the median) and 200 (derived from the receiver operator curve analysis). OR: odds ratio showing risk in medium, high group when compared to the very low, low, low-medium group.
Several known facts supported the hypothesis. Although children constitute a very significant risk group for several respiratory viruses, they seemed to have been spared from COVID-19. The immunity of children against HAV (a virus with similar taxonomy to coronaviruses), acquired either by vaccination in developed countries or by infection in underdeveloped countries, may have contributed to this protection. The loss of immunity to HAV as the result of aging may have led to an increased COVID-19 morbidity in the elderly.
The Diamond Princess ship experience also supported this theory. Of the 3711 passengers and crew members, 58% were over the age of 60. In total, 712 of the passengers were infected and 13 died (1.8% fatality).The asymptomatic infection rate was 57% in elderly individuals over the age of 60 [3]. Thus far, the reason for this extremely low fatality and unusually high asymptomatic infection rate has not been explained. The Centers for Disease Control and Prevention recommendation that all susceptible people traveling for any purpose, frequency, or duration to countries with high or intermediate HAV endemicity should be vaccinated before departure, which all notable cruise lines to Asia comply with, may have been one explanation [4].
We are aware that this ecological analysis is far from pointing to a causal relationship. However, given the simplicity and the very low risk/benefit ratio of the preventive measures, it is far from being negligible.
We are proceeding with detailed analyses, to try and find confounders that may have led to this association, but with this letter, we are urging the medical community to help in challenging this hypothesis. If confirmed, the consequences of this simple discovery will be enormous.
Informed consent
As this was an evaluation of publicly available open access data, informed consent was not required.
Acknowledgment/Disclaimers/Conflict of interest
There was no funding provided for this work. The authors declare that there are no conflicts of interest.
References
- Sarialioglu F Belen Apak FB Haberal M. Can hepatitis A vaccine provide protection against. COVID-19? Experimental and Clinical Transplantation . 2020;18:141–143. doi: 10.6002/ect.2020.0109. [DOI] [PubMed] [Google Scholar]
- The global prevalence of hepatitis A virus infection and susceptibility: a systematic review. Report number: WHO/IVB/10 . 2009.
- Sakurai A Sasaki T Kato S Hayashi M Tsuzuki SI Natural history of asymptomatic SARS-CoV-2 infection. The New England Journal of Medicine . 2020;383:885–886. doi: 10.1056/NEJMc2013020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travel related infectious diseases- hepatitis A. Centers for Disease Control and Prevention. CDC Yellow Book . 2020.