Abstract
Disease-modifying therapies (DMT) for relapsing-remitting MS (RRMS) act on the immune system, suggesting a need for caution during the SARS-CoV2/Covid-19 pandemic. A group of experts in MS care from Saudi Arabia convened to consider the impact of Covid-19 on MS care in that country, and to develop consensus recommendations on the current application of DMT therapy. Covid-19 has led to disruption to the care of MS in Saudi Arabia as elsewhere. The Expert Panel considered a DMT's overall tolerability/safety profile to be the most important consideration on whether or not to prescribe at this time. Treatment can be started or continued with interferon beta, teriflunomide, dimethyl fumarate, or natalizumab, as these DMTs are not associated with increased risk of infection (there was no consensus on the initiation of other DMTs). A consensus also supported continuing treatment regimens with fingolimod (or siponimod) and cladribine tablets for a patient without active Covid-19. No DMT should be imitated in a patient with active Covid-19, and (only) interferon beta could be continued in the case of Covid-19 infection. Vaccination against Covid-19 is a therapeutic priority for people with MS. New treatment should be delayed for 2–4 weeks for vaccination. Where treatment is already ongoing, vaccination against Covid-19 should be administered immediately without disruption of treatment (first-line DMTs, natalizumab, fingolimod), when lymphocytes have recovered sufficiently (cladribine tablets, alemtuzumab) or 4 months after the last dose (ocrelizumab). These recommendations will need to be refined and updated as new clinical evidence in this area emerges.
Key words: multiple sclerosis, disease-modifying therapy, covid19, coronavirus
Abbreviations: DMT, disease-modifying therapy; MS, multiple sclerosis; HCP, healthcare professional; MSIF, MS International Federation; ICU, Intensive Care Unit; NGT, nominal group technique; PML, progressive multifocal leukoencephalopathy
Introduction
The evolving SARS-CoV2/Covid-19 pandemic has disrupted normal life, including the provision of routine medical care, around the world. Guidance for the continuing management of patients in all fields of medicine is urgently needed. On July 17 2020, an Expert Panel comprising nine neurologists with practical experience in the clinical management of multiple sclerosis (MS) was convened to discuss and debate issues relating to the impact of SARS-Cov2/Covid-19 on the management of people with MS. The principal objectives of the meeting were to (a) consider the impact of Covid-19 on MS care in Saudi Arabia, and (b) to use formal consensus methodology (described below) to develop practical advice and recommendations that can be implemented in Saudi Arabia to support physicians in caring for people with MS during this challenging time. Here, we report the consensus outcomes from these discussions.
Methods
A literature search was conducted in July 2020 using PubMed, using the search terms “Covid-19 and “MS” to identify publications relevant to management of people with MS Covid-19. A modified nominal group technique (NGT) was then used to capture the outcome of the meeting. NGT is a validated, structured, group meeting technique used to generate and prioritise responses to specific questions and to obtain expert consensus (Humphrey-Murto et al, 2017). This method is particularly well suited for the present situation where limited outcome data are available.
The Chair of the meeting along with a small group of clinical experts in the management of MS defined a list of questions to be addressed in the workshop. For the first question, a number of practical considerations affecting choice of DMTs (interferon beta, dimethyl fumarate, teriflunomide, fingolimod, siponimod, natalizumab, cladribine tablets, ocrelizumab, alemtuzumab) during COVID-19 times were listed. Additionally, four DMT-specific questions were defined. These considerations and DMT-specific questions were drafted using available evidence, expert experiences, current debates and issues raised in other international guidance.
The Expert Panel were then invited to express individually agreement and prioritization of these considerations and to answer the DMT-specific questions, using a dedicated online platform. Each of the practical considerations was rated NA to 5, where NA represented not applicable/no impact, and 5 represented highest impact. Other considerations that were not listed were also identified and rated. Consensus was defined as having been achieved when there was 75% agreement among the Expert Panel. The strength of recommendation was not expressed.
Our article includes a concise review of literature at the time of writing on clinical experience relating to Covid-19 in populations with MS. This is a dynamic area of research, and new evidence is appearing rapidly. Accordingly, we searched the literature for reports of susceptibility to Covid-19, and outcomes in these patients after the expert meeting, at the time of submission to keep the data we present as current as possible. An overview of important recent guidance on MS care in the Covid-19 era, collated after the meeting, is also included.
Potential impact of disease-modifying treatments on the course of Covid-19 infections
Current international expert opinion
General guidance on the management of MS in the Covid-19 era from expert societies and important patient advocacy groups, released in December 2020, supports the continued use of DMTs for people with MS, subject to a risk:benefit assessment considering risk factors for adverse outcomes and the local prevalence of Covid-19 (Table 1; Association of British Neurologists, 2020; Berlit et al 2020 [for the German Society of Neurology], MS Society [UK], 2020a,b; European Multiple Sclerosis Platform, 2020;MS Society [USA], 2020). Table 2 summarises three examples of statements relating to the use of individual DMTs during the Covid-19 pandemic, from institutions with expertise in the management of MS: the MS International Federation (2020), the Association of British Neurologists (2020a), and a group of international MS experts (Giovannoni et al., 2020). The recommendations included in Table 1 relate to the use of DMTs, specifically: important additional advice includes statements to the effect that people with MS currently taking DMTs should not stop their treatment without medical advice; that people who develop symptoms of or test positive for SARS-Cov2 should discuss their MS therapies with their MS care provider or another HCP who is familiar with their care; and that people with MS should discuss with their HCP about which therapy is the best choice for their individual disease course and disease activity in light of COVID-19 risk in the region before starting any new DMT.
Table 2.
International expert opinion on potential impact on the clinical course of a Covid-19 infection of pharmacologic disease-modifying therapies (DMT) in current use within the management of multiple sclerosis (MS).
| Source of opinion | |||
|---|---|---|---|
| DMT | MS International Foundation (2020) | Association of British Neurologists (2020) | St Bartholomew's Hospital, UK (Giovannoni et al., 2020)a |
| Interferon beta | Unlikely to have negative impact on a Covid-19 infection | May be used when and where rates of SARS-CoV2 infection are very high (these drugs do not specifically increase the risk of infection) | Very low risk of adverse impact |
| Glatiramer acetate | |||
| Dimethyl fumarate | Limited evidence suggests no increased risk of severe COVID-19 symptoms or death | Low risk of adverse impact | |
| Teriflunomide | Very low risk of adverse impact | ||
| Fingolimod, siponimod | Use cautiously at very high rates of SARS-CoV2 infection (possible increased risk of viral infections) | Intermediate risk of adverse impact | |
| Anti-CD20 (ocrelizumab, rituximabb) | Possibility of increased risk of admission or intensive care due to Covid-19 | Use cautiously in RRMS where rate of SARS-CoV2 infection is very high. Consider delaying re-treatment until very high infection rates reduce.c | Intermediate-to-high risk of adverse impact |
| Cladribine tablets | Insufficient data are available to make an assessment at this time | Start cautiously on case-by-case basis when SARS-CoV2 risk is very high. Delay re-treatment until infection risk is low or moderate | Intermediate risk of adverse impact |
| Natalizumab | Used if rates of SARS-CoV2 infection are very high if individual's risk of PML is acceptable | Intermediate risk of adverse impact | |
| Alemtuzumab | Only start or retreat, when SARS-CoV2 risk is low, except on case by case basis | High risk of adverse impact | |
St Batholomew's Hospital additionally classified mitoxantrone and autologous haemopoietic stem cell transplantation as “High” risk. bRituximab is not indicated for the management of MS: ocrelizumab and rituximab are included together here as these agents share a common mechanism of action and rituximab is used frequently off-label for the management of MS. cAdditionally, use ocrelizumab in people with PPMS with higher levels of disability, only when the risk of SARS-CoV2 is low, except on a case by case basis, as these patients are more likely to have comorbidities and the risk:benefit ratio of treatment is likely to be reduced. PML: progressive multifocal leukoencephalopathy. Expert opinion has been paraphrased for brevity and clarity.
Table 1.
Overview of recent general guidance relating to Covid-19 for people with multiple sclerosis (MS)
| Source | Key guidance |
|---|---|
| Association of British Neurologists (2020) | All DMTs should remain available to people with MS during the Covid-19 pandemic, based on individual prescribing decisions that take into account potential risk factors for adverse outcomes, such as greater disability, older age, obesity, male gender, BAME ethnicity, diabetes, cardiorespiratory disease. |
| German Society of Neurology (2020)a | DMTs are unlikely to increase risk of Covid-19 and should be continued in patients with MS, taking into account age, comorbidity, disease activity and locval Covid-19 prevalence. Ecephalopathies are common in MS patients with Covid-19. |
| European Multiple Sclerosis Platform, (2020) | MS does not increase susceptibility to contracting Covid-19, but severe Covid-19 may be more likely in those with progressive MS course, greater disability, older age, male gender, comorbid conditions such as diabetes or cardiorespiratory disease, or receipt of immunosuppressants. |
| MS Society (UK), 2020a, MS Society (UK), 2020b | Little evidence of increased risk of Covid-19 in people with MS, including those receiving a DMT (although certain specific circumstances can increase Covid-19 risk. |
| MS Society (USA), 2021a, MS Society (USA), 2021b | People with MS should continue taking a DMT; if they develop Covid-19 discuss the way forward with their healthcare team, taking into account risk factors cited above. Treatment decisions should be made on a shared basis between the patient and his or her healthcare team. |
BAME: Black, Asian and minority ethnic; EMSP: European Multiple Sclerosis Platform. aBerlit et al (2020)
In general, interferon beta and glatiramer acetate were seen as unlikely to have a serious negative impact on the course of a Covid-19 infection in a person with MS (the Association of British Neurologists also included dimethyl fumarate in this category). The MSIF included dimethyl fumarate, teriflunomide and fingolimod/siponimod in a category that considered there to be no increased risk of severe Covid-19, but based on limited evidence. Anti-CD20 agents are associated with possible risk of adverse impact on a Covid-19 infection, while insufficient data are available for an assessment of cladribine tablets, natalizumab or alemtuzumab. The MSIF counselled caution in the use of higher efficacy DMTs where rates of Covid-19 disease are high, with re-treatments with anti-CD20 agents or cladribine tablets recommended when a prevailing high level of local Covid-19 infection has reduced. The patient's individualised risk of progressive multifocal leukoencephalopathy (PML; Bloomgren et al, 2012; Prezioso et al, 2020) should be considered in parallel with consideration of local Covid-19 infection rates before starting natalizumab, and the use of alemtuzumab was recommended only when Covid-19 rates are low. The MSIF also added a note of caution to the use of anti-CD20 DMT therapy for patients with primary progressive MS (PPMS) at higher levels of disability, as the likelihood of comorbidity in this population may complicate a Covid-19 infection further during the use of this treatment. The recommendations from Professor G Giovannoni via the BartsMS blog adopted a simpler approach: the risk of an adverse impact on Covid-19 infection is very low for interferon beta and glatiramer acetate, high for alemtuzumab, with other DMTs occupying a hierarchy of risk categories between these extremes. Prof. Giovannoni qualified the advice according to other patient characteristics: for example, risk categories associated with treatments that deplete immune cells (cladribine tablets, autologous haemopoietic stem cell transplantation, mitoxantrone) were lower where patients had a lymphocyte count above 1000/mm3.
Review of cases
Table 3 summarises recent publications or presentations in which the course of Covid-19 has been followed in people with MS (Sormani et al, 2020; Roche, 2020; Hughes et al, 2020; MS Covid-19 Meeting, 2020 ; Simpson-Yap et al, 2020; Chaudhry et al., 2020; Merck Healthcare, 2020; Möhn et al, 2020; Kataria et al, 2020; Zabalza et al., 2020). In general, older age, a progressive MS phenotype and male gender have predicted a more adverse course of Covid-19 in these studies (Hughes, 2020). With regard to the effects of individual DMTs, the number of cases remains small, and conclusions based on these data can only be preliminary at this time. Nevertheless, two studies in relatively large cohorts of patients from Italy (Sormani et al, 2020), or pooled from 21 countries in the Global Data Sharing Initiative (Simpson-Yap et al, 2020; Peeters et al, 2020), have identified increased risk of a more severe disease course in patients receiving anti-CD20 therapies, especially rituximab, compared with dimethyl fumarate or natalizumab. A smaller Covid-19 cohort of 65 patients with MS in Sweden reported similar findings, with increased rates of hospitalisation, ICU treatment and need for ventilation in people with MS receiving ocrelizumab or (especially) rituximab (MS Covid-19 Meeting 2020). The authors of this study noted that Sweden is unusual, however, in that more patients receive rituximab for MS, compared with other countries. In addition, there is no sign of an unusual severity of Covid-19 in patients receiving ocrelizumab in the pharmacovigilance database of its pharmaceutical sponsor (Roche, 2020; Hughes et al, 2020). There is as yet no signal for adverse prognosis for Covid-19 in patients receiving other DMTs.
Table 3.
Summary of key studies of the impact of pre-existing MS on the clinical course of Covid-19.
| Source | Patients | Key findings |
|---|---|---|
| (Sormani et al (2020) | 784 people with MS and suspected (n=593) or confirmed (n=191) Covid-19 in Italy | 83% received DMT therapy at the time of onset of Covid-19 symptoms Use of ocrelizumab was associated with a more severe disease course in a multivariate analysis, along with age, gender, progressive MS course, and recent use of methylprednisolone |
| (Roche (2020); Hughes et al (2020) | 100 confirmed or suspected cases of Covid-19 received via routine pharmacovigilance reporting | Severity of Covid-19 was reported for n=77: asymptomatic/mild/moderate (64%), severe (30%) or critical (6%); of 64 cases where the outcome of Covid-19 infection was known, all were “recovered” or “recovering”. Findings considered to be generally consistent with disease outcomes in other series of patients with Covid-19 |
| MS Covid-19 Meeting (2020) | 65/17,528 people with MS in a registry based in Sweden had MS and confirmed Covid-19 | Mean age of confirmed cases was 52 y for those hospitalized and 50 for those admitted to ICU. 20% of confirmed Covid-19 cases had progressive MS, of whom 50% were admitted to ICU. 85% of Covid-19 cases were on DMT therapy 53% of patients treated with rituximab had Covid-19, compared with 33% in the registry overall 53% of rituximab-treated patients were hospitalised and 67% required ICU admission |
| Simpson-Yap et al (2020) | Global Data Sharing Initiative (1,540 hospitalised patients with MS from 21 countries, most of whom had suspected (31%) or confirmed (50%) Covid-19 infection) | Increased adjusted prevalence rates (aPR) for anti-CD20 therapy vs. dimethyl fumarate or natalizumab for hospitalisation (aPR=1.49 and 1.99, respectiely), ICU admission (aPR=2.55 and 2.39) and need for ventilation (aPR=3.55 and 2.84) Risks were higher for rituximab vs. ocrelizumab for these adverse outcomes Findings persisted when only confirmed Covid-19 cases were considered No association between DMT treatments and death |
| Chaudhry et al (2020) | Review of 40 patients with MS hospitalised with Covid-19 | No association between DMT use and non-use and the severity of the Covid-19 disease course |
| Merck Healthcare KGaA (2020) | Merck Global Safety Database | 47 suspected cases of COVID-19 (18 confirmed) in patients treated with cladribine tablets – severity was reported as serious in 4 patients, 9 have recovered or are recovering, and there were no reported fatalities 50 suspected cases of Covid-19 (20 confirmed) in patients treated with interferon beta1a – severity was reported as serious in 9 patients, 11 have recovered or are recovering, and there was one reported fatality. |
| Möhn et al (2020) | Review of 873 published cases of Covid-19 in people with MS | DMT therapy did not worsen outcome in people with MS and Covid-19 (most recipients of DMTs were on anti-CD20 therapy). There was a suggestion that DMT therapy could have been associated with improved outcomes in subjects with severe Covid-19. |
| Kataria et al (2020) | 3 patients with history of MS | Patients resented with likely pseudo-exacerbation of MS: physicians need to be aware of this possibility |
| Zabalza et al (2020) | Retrospective cohort (48 suspected Covid-19 cases + 45 cases from clinic visits | Similar incidence of and outcomes related to Covid-19 in people with MS and the general population. |
DMT: disease-modifying therapy; ICU: Intensive Care Unit.
Participants’ recent experiences in managing MS – the new normal
Effects on healthcare delivery
Personal experience from the Expert Panel indicated a major impact of the Covid-19 pandemic on the management of MS is Saudi Arabia that was reminiscent of the situation faced by patients and healthcare systems in other countries and regions (Vogel et al, 2020). Specifically, consultations moved online or to contact by telephone, with only select, high-risk MS patients seen in person at the clinic (although more recently some centres have been seeing new patients in face-to face consultations). The remote management of MS relapses was highlighted as presenting a particular challenge, with patients with severe relapse having to attend either the Emergency Department, or the MS clinic, depending on location (one centre has been managing relapses at home for several years). Managing patients living in remote locations presented another challenge. The provision of dedicated nurses has been important in maintaining contact with patients, and for assessing their condition in the event of a suspected MS relapse. A nurse in one centre runs a WhatsApp group for her patients.
Medications have been delivered to patients’ homes, or via drive-through pharmacies, with some initial disruption of supply in some cases. Many routine lab tests and imaging services have been suspended or postponed, with some patients referred to private laboratories. Tests associated with DMTs that require more intensive monitoring (e.g. for lymphopenia on fingolimod) have been preserved largely, however. The use of alemtuzumab has been reduced in at least one centre, although prescription of natalizumab for MS with high disease activity was maintained there.
Sub-optimal understanding of Covid-19 among some nurses and pharmacists was seen as an important barrier to care in the Covid-19 era in one centre. There, pharmacists may not have understood the implications for patients of the known high risk of rebound MS disease activity after interruption of the supply of fingolimod (Barry et al, 2019) or natalizumab (Sellner and Rommer, 2019), and the importance of maintaining continuous supply of these medications. This experience was not replicated elsewhere, however.
Effects on patients
The emergence of Covid-19 has caused adverse neuropsychological impacts or increased levels of anxiety in some populations of patients with MS) Demir et al, 2020; Chiaravalloti et al, 2020) and patients in Saudi Arabia have communicated concerns about Covid-19, their MS and its treatment to their physicians. Common sources of worry for patients have been centred on whether attending the hospital or their place of work will increase their risk of Covid-19 (does the workplace or hospital practise effective social distancing), whether Covid-19 will increase their risk of leukopenia/lymphopenia, whether to go ahead with or postpone scheduled DMT treatments, and how to boost their immunity. Physicians generally saw no harm in patients taking vitamins D or C at recommended doses; there is limited evidence base for this, especially for vitamin C, although recent observational data suggested improved outcomes in patients hospitalised for Covid-19 who were vs. were not, replete for vitamin D (Maghbooli et al, 2020).
Consensus recommendations on the management of MS in the Covid-19 era
Management of MS
The Expert Panel were first tasked with rating the attributes of a DMT that are most important for initiating treatment in the current Covid-19 environment (0 = least important, 5 = most important). The DMT's overall safety profile was the attribute considered most important at this time (average rank 4.4), followed by risk of infection (3.6), low monitoring burden (3.6), need for few hospital visits (3.3), potential effect on a future vaccine for Covid-19 (3.3), and potential anti-SARS-CoV2 activity of a DMT itself (2.3), as has been postulated for interferon beta1 (Sallard et al, 2020).
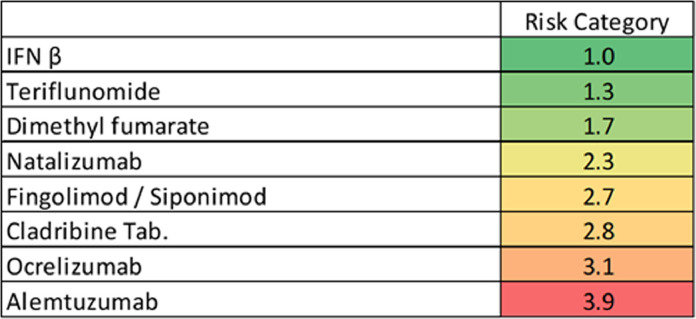
The risk of acquiring an infection during the immunodepletion phase differs between individual DMTs (Yong et al, 2020), and this was explored in more detail, by assigning rankings of the perceived risk of infections associated with each individual DMT (1 = lowest risk of infection, 4 = highest risk) (Fig. 1 ). The risk for infection was seen as highest for alemtuzumab (mean rating 3.9), with successively lower risks attributed to ocrelizumab (3.1), cladribine tablets (2.8), fingolimod/siponimod (2.7), natalizumab (2.3), dimethyl fumarate (1.7), teriflunomide (1.3) and interferon beta (1.0).
Fig. 1.
Perceived disease-modifying therapy-specific at-risk category during Covid-19 pandemic.
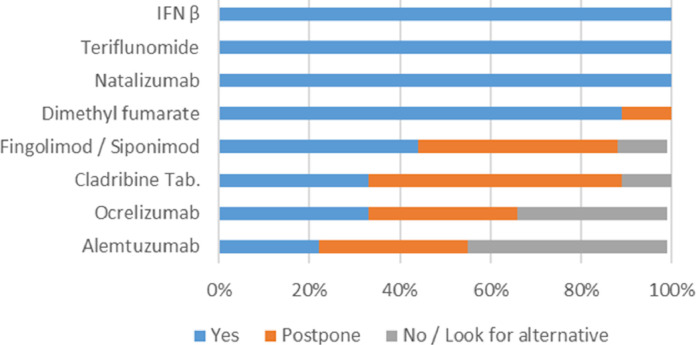
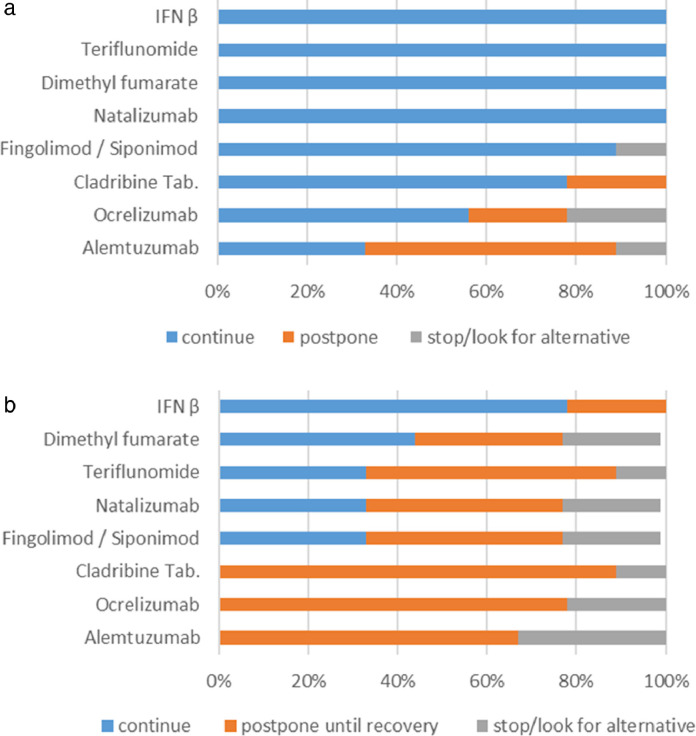
The consensus methodology described above was then used to define recommendations on the initiation or continuance of DMTs in patients with or without active Covid-19 (consensus was defined as >75% agreement). The Panel was unanimous that interferon beta, teriflunomide or natalizumab can be initiated in a patient without signs of Covid-19, with consensus supporting the initiation of dimethyl fumarate (Fig. 2 ). There was no consensus on whether fingolimod/siponimod, cladribine tablets, ocrelizumab, and alemtuzumab may be initiated. With regard to continuing DMTs in a patient without Covid-19 infection, there was unanimity or consensus on the maintenance of treatment courses of interferon beta, teriflunomide, dimethyl fumarate, natalizumab, fingolimod/siponimod and cladribine tablets (Fig. 3 a). Consensus was not reached in the case of ocrelizumab, and the majority of physicians would delay re-treatment with alemtuzumab.
Fig. 2.
Consensus recommendation on initiation of disease-modifying therapy in patients with relapsing-remitting multiple sclerosis without evidence of active Covid-19 infection.
Fig. 3.
Consensus recommendation on continuation of disease-modifying therapy in patients with relapsing-remitting multiple sclerosis
a) Patients without evidence of active Covid-19 infection.
b) Patients with active Covid-19 infection.
The panel were unanimous in that initiation of any DMT should be delayed in people with RRMS with active COVID-19 infection. Interferon beta was the only DMT with consensus support for continuing therapy during an active Covid-19 infection (Fig. 3b). About half of experts would continue dimethyl fumarate at this time, and about one-third would continue teriflunomide, natalizumab or fingolimod/siponimod. There was no support for continuing cladribine tablets, ocrelizumab or alemtuzumab, with strong support for delaying the next application of these treatments.
Vaccination against SARS-Cov2/Covid-19
General considerations
Several vaccines against SARS-CoV2 are already available for use and others are under regulatory consideration or are in late stage clinical development. Mass vaccination programmes are underway around the world, and preliminary evidence of their efficacy in preventing Covid-19 or serious adverse Covid-19 outcomes in general (non-MS), vulnerable populations is beginning to appear (Vasileiou et al., 2021; Lopez Bernal et al., 2021; Dagan et al., 2020; Hunter and Brainard, 2021).
Previous guidance with vaccinations for people with active, DMT-managed MS is of limited support here. Vaccination against common viral infections is advised before initiating some DMTs, including for varicella zoster virus (VZV) in unexposed patients (cladribine tablets, fingolimod, siponimod, ozanimod, alemtuzumab) or HPV (fingolimod), as directed in the Prescribing Information for these DMTs. Recommendations include a delay of 4–6 weeks following vaccination to allow the vaccine to develop its full effect before starting DMT (this varies somewhat between DMTs). Other guidance recommends vaccination against prevalent bacterial infections, e.g. TB, for some DMTs, including cladribine tablets. These recommendations are relevant to new starts of DMT therapy, but do not address the needs of patients already on stable DMT therapy who need protection from Covid-19.
Immunocompromised patients should not receive attenuated live attenuated vaccines. Some novel Covid-19 vaccines (e.g. the Oxford University/AstraZeneca or Russian Sputnik V vaccines) use viral vectors to deliver their nucleic acid payload. These vectors cannot replicate, however, and are thus not considered to be live vaccines.
Patients already receiving treatment with a disease-modifying therapy
Current evidence does not suggest specific adverse effects of Covid-19 vaccines on people with MS: it is clear that the benefits of Covid-19 vaccination appear to outweigh any risk in people with MS and patients should be encouraged to receive any one of these vaccines wherever possible. Table 4 summarises our consensus view on the likely impact of DMT therapy on the efficacy of vaccinations, and Table 5 summarises our recommendations on managing DMT therapy at the time of vaccination. The impact of “first-line” or “platform” DMTs on the vaccine response is likely to be negligible or minor, and vaccination should proceed immediately and without interruption of treatment with interferons, glatiramer acetate, dimethylfumarate, or teriflunomide. Natalizumab, a high-efficacy DMT is also in this category, and vaccination may proceed without interruption of this treatment. Withdrawing natalizumab also risks the appearance of MS rebound disease (Giovannoni et al, 2017).
Table 4.
Likely impact of treatment with a disease-modifying therapy (DMT) for MS on the efficacy of anti-SARS-CoV2 vaccination.
| DMT | Implication for Covid-19 vaccination |
|---|---|
| Interferons | Vaccination response is likely to be intact |
| Teriflunomide, natalizumab, dimethylfumarate | Vaccination response is probably intact |
| Cladribine tablets, anti-CD20, alemtuzumab | Vaccination response is possibly diminished |
| Fingolimod, siponimod | Vaccination response is mostly diminished |
Note that these are expert opinions based on mechanisms of action of DMTs
Table 5.
Recommended washout periods between withdrawal of a disease-modifying therapy (DMT) and vaccination.
| DMT | Recommended washout before Covid-19 vaccination |
|---|---|
| Interferons, teriflunomide, natalizumab, dimethylfumarate | No washout required, vaccinate immediately |
| Cladribine tablets, | When lymphocytes have recovered On average, absolute lymphocyte count remained at or above the lower limit of normal during year 1 of treatment and recovered to this level by week 36 of the year 2 course of treatmenta |
| Alemtuzumab | When lymphocyte counts have recovered On average, total lymphocytes remained below lower limit of normal for about 6 months after the year 1 and year 2 courses of treatmentb |
| Fingolimod, siponimod | Vaccinate without washout, even if the response is possibly diminished (to avoid MS rebound disease) |
| Anti-CD20 (ocrelizumab) | Vaccinate 4 months after last infusion. Next dose can be delayed by 2 weeks of vaccination occurred ≥3 months after last infusion. |
CLARITY Phase III study (Comi et al 2019).
CARE-MS-I and CARE-MS-II randomised Phase III studies (Li et al, 2018).
DMTs hypothesised to act as immune reconstitution therapies (cladribine tablets and alemtuzumab) induce reductions in circulating immune cells that persist for months before recovering (Sorensen and Sellebjerg, 2019). The mean absolute lymphocyte count (ALC) did not fall below the normal range for the year following the administration of the first course of cladribine tablets in the randomised CLARITY trial (Comi et al, 2019). In the second year of treatment with cladribine tablets, ALC fell below the lower limit of normal, and recovered to this level after 36 weeks of year 2 (Comi et al, 2019). In theory, reduced lymphocyte counts following treatment with cladribine tablets could reduce the efficacy of an anti-SARS-CoV2 vaccine, although data are not yet available on this. We do have early but encouraging data from patients with MS who had received cladribine tablets who demonstrated a subsequent normal response to an influenza or VZV vaccine during year 1 or year 2 of treatment (Wu et al., 2021; Roy and Boschert, 2021). Similar considerations apply to a patient receiving treatment with alemtuzumab; total lymphocyte count reached nadir at one month after treatment with this DMT, recovering to the lower limit of normal at about 6 months following each of the year 1 and year 2 treatment courses (Li et al, 2018). Finally, anti-CD20 DMTs, e.g. ocrelizumab, also have the potential to act via immune reconstitution, but are administered continuously according to current labelling (Sorensen et al, 2019). Vaccination may proceed 4 months after the last dose of ocrelizumab.
In practice, the timing of vaccination for a patient receiving IRT will be individualised. The decision on when to vaccinate will be shared between patient and physician, taking into account several factors, including the patients’ immunological status, the patient's preference, the local prevalence of Covid-19, and the presence or absence of risk factors for a severely adverse Covid-19 outcome.
Durable lymphopenia during treatment with fingolimod would be expected to induce a stronger suppression of the immune response to vaccination, and reduced titres in response to vaccination have been observed in MS patients receiving this treatment (Sharifian-Dorche et al, 2021). Nevertheless, fingolimod (or other DMTs sharing its mechanism) should not be withdrawn due to the risk of rebound MS disease (Giovannoni et al, 2017) and vaccination should proceed without interruption of treatment.
Our consensus recommendations are largely consistent with other expert recommendations published in 2021 (MS Society (USA), 2021a, MS Society (USA), 2021b; Barts NHS Trust, 2020; St Michael's Unity Health, 2021; MS International Federation, 2021). The NMMS and MSIF recommend that the relative timimgs of vaccination and of treatment with cladribine tablets, alemtuzumab or anti-CD20 agents should be agreed between the patient and the healthcare team. Other recommendations suggest varying time periods between a dose of the DMT and the next treatment with these agents.
Restarting disease-modifying treatment after vaccination against Covid-19
Where a DMT is withdrawn to allow vaccination against Covid-19, we advise waiting for 2–4 weeks before resuming treatment to allow the vaccine to take effect. This is easily accommodated for DMTs withy a long inter-dose interval, such as immune reconstitution therapies or ocrelizumab. The next infusion of ocrelizumab could be delayed for up to 2 weeks if necessary.
Looking ahead: perceived gaps in knowledge
We have insufficient data on the prevalence of Covid-19 in people with MS, on the clinical course of Covid-19 in people with MS, and on the impact of Covid-19 infection on the clinical course of MS. While data in the literature so far are encouraging in that they suggest no increased risk of Covid-19 in people with MS or with most DMTs (see above), this is based on very few cases so far. Importantly, review of a database of MS patients in Switzerland indicated that <1% were at high or very high risk factors for death from Covid-19, based on demographic parameters and known comorbidities, and that these patients were not receiving immunosuppressive treatment (Bsteh et al., 2020). There are mechanistic grounds that increased levels of cytokines activation of inflammatory pathways during Covid-19 infection might worsen MS prognosis over the longer term, however, and further data on prognosis following the Covid-19 infection will be needed (Di Stadio et al, 2020).
In principle, an additional dose of a Covid-19 vaccine may be beneficial where immunotherapy has reduced the immune response to the standard one- or two-injection regimen, but data are lacking on this. A similar proposal has been made recently for people with obesity, following observations of a reduced immunological response to a Covid-19 vaccine in this population (Ledford, 2020). Further research is needed to determine the optimum schedule for vaccination for Covid-19 for patients already receiving a DMT for MS.
Conclusions
People with a new diagnosis of MS require prompt treatment with a DMT, and people with active MS disease require maintained treatment, to reduce the frequency of relapses, and to preserve their long-term functional status (Ghezzi, 2018; Yamout et al, 2020). However, some DMTs, especially those which maintain a permanent state of immunosuppression, are associated with an increased risk of infection (Yong and Kim, 2020). The pharmacologic management of MS is already complex, due to the diverse range of disease characteristics of individual patients, and the increasingly large armamentarium of available DMTs. The current need to balance the needs to suppress MS disease activity, while not placing the patient at risk of an adverse clinical course of a future Covid-19 infection has added a new layer of difficulty in managing these patients.
The expert consensus meeting reported here has attempted to find a way through this maze, with practical recommendations, based on the data available today. For someone without Covid-19, the Panel supported the initiation and continuation of treatment with DMTs with good general safety, particularly with regard to infection risk: interferon beta, teriflunomide, dimethyl fumarate natalizumab. The initiation of fingolimod/siponimod, cladribine tablets, ocrelizumab and alemtuzumab can be delayed where possible, or considered on a case-by case basis. Where the patient presents with Covid-19, no DMT should be started until recovery from the infection, and only interferon beta is generally suitable for uninterrupted treatment throughout the course of a Covid-19 infection; again, individual risk: benefit considerations come into play for other DMTs.
These considerations are largely consistent with a recent statement on MS therapy and Covid 19 from the European Academy of Neurology (EAN), which states that “In any case of acute signs of infection, immune therapies must not be initiated or continued, especially immune depleting agents should be delayed until symptoms have disappeared” (European Academy of Neurology, 2020). The panel's recommendations are also consistent with the EAN's recommendation that the next treatment in an ongoing course of an immune-depleting therapy should be delayed, where possible, until the patient has recovered from Covid-19.
Overall, at this time, the benefit of all approved Covid-19 vaccines appears to outweigh any possible risks of vaccination against Covid-19, and this is a therapeutic priority for people with MS where the prevalence of Covid-19 is high. Vaccines for Covid-19 are not live or attenuated-live and there is thus no reason to suggest a safety issue with any of the new generation of anti-Covid-19 vaccines for people with MS. The timing of vaccination in relation to DMT administration is the main consideration, especially while limited vaccine availability precludes schedule the timing of Covid-19 vaccination electively. Some DMTs may diminish the immune response to vaccines, with risk of not achieving adequate immunity against Covid-19 infection, although recent experience showing an adequate serological response to other vaccines in patients treated with DMTs ,such as cladribine tablets, is reassuring (Wu et al., 2021; Roy and Boschert, 2021). Immunological studies to monitor humoral and cellular immune responses to Covid-19 vaccines in people with MS using some DMTs are needed. These immunological studies can provide instructions regarding additional booster vaccinations for patients with insufficient immunological response to COVID19 vaccines, if required.
New treatment should be delayed for 2–4 weeks to allow vaccination to proceed. Where treatment is already ongoing, one of these vaccines should be performed immediately without disruption of treatment (first-line DMTs, natalizumab, fingolimod), when lymphocytes have recovered sufficiently (cladribine tablets, alemtuzumab) or 4 months after the last dose (ocrelizumab).
Further experience with the therapeutic use of DMTs in patients who develop Covid-19 will be needed to refine evidence-based strategies for the management of RRMS. Until then, a cautious approach is warranted, where exposure to DMTs, especially those that induce long-term immunosuppression, is limited.
Duality of interest
All authors participated in the closed meeting that gave rise to this article, which was organised and supported by Merck Serono Middle East FZ-Ltd, United Arab Emirates, an affiliate of Merck KGaA, Darmstadt, Germany. HA, FAl, MalK, RB, SQ, and SS reported no additional duality of interest. Additionally, HAlN reports personal fees and non-financial support from Merck for the submitted work, and personal fees from Roche and personal fees from Novartis. AA reports personal fees and non-financial support from Merck for the submitted work. MAlM reported personal fees and non-financial support from Merck for the submitted work; personal fees from Biologix and personal fees from Bayer. SB reports personal fees and non-financial support from Merck for the submitted work; grants from King Abdulaziz city for Science and technology, and King Salman Center for Disability Research, personal fees from Biogen/Biologix, Sanofi, Novartis, Abbvie, and Merck; non-financial support from Biogen/Biologix, Sanofi, Novartis, Merck, and Abbvie, outside the submitted work. EJC reports personal fees and non-financial support from Merck for the submitted work; personal fees and non-financial support from Roche, personal fees and non-financial support from Sanofi, personal fees and non-financial support from Biogen/Biologix, personal fees from Novartis, personal fees and non-financial support from Merck, grants from MENACTRIMS, outside the submitted work. AElB is an employee of Merck KGaA, Riyadh, Saudi Arabia. MAlJ reports personal fees and non-financial support from Merck for the submitted work; grants from KACST, KAIMRC, Merck, personal fees from Merck, Biogen, Biologix, Bayer, Novartis, Roche, Sanofi, Genzyme, Genpharm, non-financial support from Merck, Biogen, Biologix, Bayer, Roche, Sanofi, outside the submitted work. YAlM reports personal fees and non-financial support from Merck for the submitted work; grants, personal fees and non-financial support from Roche, personal fees from Novartis, personal fees from Biogen/Biologix, personal fees and non-financial support from Genzyme, personal fees and non-financial support from Merck, outside the submitted work. SM reports personal fees and non-financial support from Merck for the submitted work; personal fees and non-financial support from Roche, Merck, Sanofi and Novartis outside the submitted work. RB reported no additional duality of interest.
Conflict of interest and role of funding source
All authors participated in the closed meeting that gave rise to this article, which was organised and supported by Merck Serono Middle East FZ-Ltd, United Arab Emirates, an affiliate of Merck KGaA, Darmstadt, Germany. HA, MAlm, FAl, MalK, SQ, and SS reported no additional duality of interest. Additionally, SB reports personal fees and non-financial support from Merck for the submitted work; grants from King Abdulaziz city for Science and technology, and King Salman Center for Disability Research, personal fees from Biogen/Biologix, Sanofi, Novartis, Abbvie, and Merck; non-financial support from Biogen/Biologix, Sanofi, Novartis, Merck, and Abbvie, outside the submitted work. EJC reports personal fees and non-financial support from Merck for the submitted work; personal fees and non-financial support from Roche, personal fees and non-financial support from Sanofi, personal fees and non-financial support from Biogen/Biologix, personal fees from Novartis, personal fees and non-financial support from Merck, grants from MENACTRIMS, outside the submitted work. A El B is an employee of Merck KGaA, Riyadh, Saudi Arabia. M AlJ reports personal fees and non-financial support from Merck for the submitted work; grants from KACST, KAIMRC, Merck, personal fees from Merck, Biogen, Biologix, Bayer, Novartis, Roche, Sanofi, Genzyme, Genpharm, non-financial support from Merck, Biogen, Biologix, Bayer, Roche, Sanofi, outside the submitted work. Y Al M reports personal fees and non-financial support from Merck for the submitted work; grants, personal fees and non-financial support from Roche, personal fees from Novartis, personal fees from Biogen/Biologix, personal fees and non-financial support from Genzyme, personal fees and non-financial support from Merck, outside the submitted work.
Acknowledgements
A medical writer (Dr Mike Gwilt, GT Communications) provided editorial assistance, funded by Merck Serono Middle East FZ LTD, an affiliate of Merck KGaA, Darmstadt, Germany.
References
- Association of British Neurologists . 2020. ABN guidance on the use of disease-modifying therapies in multiple sclerosis in response to the Covid19 pandemic.https://www.theabn.org/resource/collection/6750BAE6-4CBC-4DDB-A684-116E03BFE634/ABN_Guidance_on_DMTs_for_MS_and_COVID19_05_Nov_2020.pdf [Google Scholar]
- Barry B, Erwin AA, Stevens J, Tornatore C. Fingolimod Rebound: A Review of the Clinical Experience and Management Considerations. Neurol Ther. 2019;8(2):241–250. doi: 10.1007/s40120-019-00160-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barts NHS Trust. 2020. Barts MS COVID-19 vaccine advice. Available at https://multiple-sclerosis-research.org/2020/12/bartsms-Covid-19-vaccine-advice (accessed March 2021).
- Berlit P, Bösel J, Gahn G, et al. Neurological manifestations of COVID-19" - guideline of the German society of neurology. Neurol Res Pract. 2020;2:51. doi: 10.1186/s42466-020-00097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloomgren G, Richman S, Hotermans C, et al. Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N Engl J Med. 2012;366:1870–1880. doi: 10.1056/NEJMoa1107829. [DOI] [PubMed] [Google Scholar]
- Bsteh G, Bitschnau C, Hegen H, Auer M, Di Pauli F, Rommer P, Deisenhammer F, Berger T. Multiple sclerosis and COVID-19: how many are at risk? Eur J Neurol. 2020 doi: 10.1111/ene.14555. (advance publication online, doi:10.1111/ene.14555. doi: 10.1111/ene.14555) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhry F, Bulka H, Rathnam AS, et al. COVID-19 in multiple sclerosis patients and risk factors for severe infection. J Neurol Sci. 2020;418 doi: 10.1016/j.jns.2020.117147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiaravalloti ND, Amato MP, Brichetto G, Chataway J, Dalgas U, DeLuca J, Meza C, Moore NB, Feys P, Filippi M, Freeman J, Inglese M, Motl R, Rocca MA, Sandroff BM, Salter A, Cutter G, Feinstein A. CogEx Research Team. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J Neurol. 2020:1–10. doi: 10.1007/s00415-020-10160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comi G, Cook S, Giovannoni G, et al. Effect of cladribine tablets on lymphocyte reduction and repopulation dynamics in patients with relapsing multiple sclerosis. Mult Scler Relat Disord. 2019;29:168–174. doi: 10.1016/j.msard.2019.01.038. [DOI] [PubMed] [Google Scholar]
- Dagan N, Barda N, Kepten E, et al. 2020. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. Advance publication online, doi:10.1056/NEJMoa2101765).
- Demir CF, Bilek F, Balgetir F. Neuropsychiatric changes during the COVID-19 pandemic in multiple sclerosis patients. Arq Neuropsiquiatr. 2020 doi: 10.1590/0004-282X20200122. S0004-282 × 2020005023202. [DOI] [PubMed] [Google Scholar]
- Di Stadio A, Romani L, Bernitsas E. Could Sars-Cov2 affect MS progression? Mult Scler Relat Disord. 2020;46 doi: 10.1016/j.msard.2020.102540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Academy of Neurology . 2020. Immunotherapy for patients with neuroimmunological disorders during the COVID-19 pandemic. Available at https://www.eanpages.org/2020/04/01/immunotherapy-for-patients-with-neuroimmunological-disorders-during-the-Covid-19-pandemic. [Google Scholar]
- European Multiple Sclerosis Platform . 2020. Updated global COVID-19 advice for people with MS. Available at http://www.emsp.org/news-messages/coronavirus-disease-Covid-19-and-multiple-sclerosis (accessed January 2021) [Google Scholar]
- Ghezzi A. European and American Guidelines for Multiple Sclerosis Treatment. Neurol Ther. 2018;7:189–194. doi: 10.1007/s40120-018-0112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovannoni G, Hawkes C, Lechner-Scott J, Levy M, Waubant E, Gold J. The COVID-19 pandemic and the use of MS disease-modifying therapies. Mult Scler Relat Disord 2020;39:102073. [DOI] [PMC free article] [PubMed]
- Giovannoni G, Hawkes C, Waubant E, Lublin F. The 'Field Hypothesis': rebound activity after stopping disease-modifying therapies. Mult Scler Relat Disord. 2017;15 doi: 10.1016/j.msard.2017.06.005. A1-A2. [DOI] [PubMed] [Google Scholar]
- Hughes R, Pedotti R, Koendgen H. COVID-19 in persons with multiple sclerosis treated with ocrelizumab - A pharmacovigilance case series. Mult Scler Relat Disord. 2020;42 doi: 10.1016/j.msard.2020.102192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes S. Increased risk of severe COVID with anti-b-cell MS drugs? Medscape. 2020. Available at https://www.medscape.com/viewarticle/938277.
- Humphrey-Murto S, Varpio L, Gonsalves C, Wood TJ. Using consensus group methods such as Delphi and Nominal Group in medical education research. Medical Teacher. 2017;39:14–19. doi: 10.1080/0142159X.2017.1245856. [DOI] [PubMed] [Google Scholar]
- Hunter PR, Brainard J. 2021. Estimating the effectiveness of the Pfizer COVID-19 BNT162b2 vaccine after a single dose. A reanalysis of a study of ‘real-world’ vaccination outcomes from Israel. Preprint of research article, available at https://www.medrxiv.org/content/10.1101/2021.02.01.21250957v1 (accessed March 2021).
- Kataria S, Tandon M, Melnic V, Sriwastava S. A case series and literature review of multiple sclerosis and COVID-19: Clinical characteristics, outcomes and a brief review of immunotherapies. eNeurologicalSci. 2020;21 doi: 10.1016/j.ensci.2020.100287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford H. How obesity could create problems for a COVID vaccine. Researchers fear that vaccines might not be as effective in people who are obese, a population already highly vulnerable to COVID-19. Nature. 2020 doi: 10.1038/d41586-020-02946-6. Available at https://www.nature.com/articles/d41586-020-02946-6 (accessed March 2021) [DOI] [PubMed] [Google Scholar]
- Li Z, Richards S, Surks HK, Jacobs A, Panzara MA. Clinical pharmacology of alemtuzumab, an anti-CD52 immunomodulator, in multiple sclerosis. Clin Exp Immunol. 2018;194:295–314. doi: 10.1111/cei.13208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez Bernal J, Andrews N, Gower C et al. 2021. Early effectiveness of COVID-19 vaccination with BNT162b2 mRNA vaccine and ChAdOx1 adenovirus vector vaccine on symptomatic disease, hospitalisations and mortality in older adults in the UK: a test negative case control study. Preprint of research article, available at https://khub.net/documents/135939561/430986542/Early%20effectiveness%20of%20COVID%20vaccines.pdf/ffd7161c-b255-8e88-c2dc-88979fc2cc1b?t=1614617945615 (accessed March 2021).
- Möhn N, Konen FF, Pul R, et al. Experience in multiple sclerosis patients with Covid-19 and disease-modifying therapies: A Review of 873 Published Cases. J Clin Med. 2020;9:4067. doi: 10.3390/jcm9124067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM, Hadadi A, Montazeri M, Nasiri M, Shirvani A, Holick MF. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS One. 2020;15 doi: 10.1371/journal.pone.0239799. e0239799. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Merck Healthcare KGaA. 2020. Merck Safety Database (Merck Healthcare KGaA, data on file).
- MS Covid-19 Meeting – May 20, 2020. Available at https://multiple-sclerosis-research.org/2020/05/mscovid19-swedish-experience/.
- MS International Federation, 2020a. Global COVID-19 advice for people with MS. Available at: http://www.msif.org/wp-content/uploads/2020/06/MSIF-Global-advice-on-COVID-19-for-people-with-MS-_-updated17June2020.pdf.
- MS International Federation. MS, the coronavirus and vaccines – updated global advice, MS. 2021. Available at https://www.msif.org/news/2020/02/10/the-coronavirus-and-ms-what-you-need-to-know (accessed March 2021).
- MS Society (UK) 2020. MS and coronavirus care and support. https://www.mssociety.org.uk/care-and-support/ms-and-coronavirus-care-and-support. [Google Scholar]
- MS Society (UK) 2020. COVID-19 coronavirus and MS treatments.https://www.mssociety.org.uk/about-ms/treatments-and-therapies/disease-modifying-therapies/Covid-19-coronavirus-and-ms [Google Scholar]
- MS Society. 2021a. COVID-19 Vaccine Guidance for People Living with MS. Available at https://www.nationalmssociety.org/coronavirus-Covid-19-information/multiple-sclerosis-and-coronavirus/Covid-19-vaccine-guidance (accessed March 2021).
- MS Society (USA). 2021b. MS and the COVID-19 vaccines. Available at https://www.mssociety.org.uk/care-and-support/ms-and-coronavirus-care-and-support/ms-and-Covid-19-vaccines (updated 12 March 2021).
- MS Society (USA) Coronavirus (COVID-19). 2020 https://www.nationalmssociety.org/coronavirus-Covid-19-information [Google Scholar]
- Peeters LM, Parciak T, Walton C, et al. COVID-19 in people with multiple sclerosis: A global data sharing initiative. Mult Scler. 2020;26:1157–1162. doi: 10.1177/1352458520941485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prezioso C, Zingaropoli MA, Iannetta M, et al. Which is the best PML risk stratification strategy in natalizumab-treated patients affected by multiple sclerosis? Mult Scler Relat Disord. 2020;41 doi: 10.1016/j.msard.2020.102008. [DOI] [PubMed] [Google Scholar]
- Roche. 2020. Ocrevus and Coronavirus Disease (COVID-19) in Multiple Sclerosis. Available at https://medinfo.roche.com/content/dam/medinfo/documents/Covid-19/Ocrevus_GL-019956.pdf.
- Roy S, Boschert U. 2021. Analysis of Influenza and Varicella Zoster Virus Vaccine Antibody Titers in Patients with Relapsing Multiple Sclerosis Treated with Cladribine Tablets. Abstract P059 presented at the ACTRIMS Virtual Forum. available at https://www.abstractsonline.com/pp8/#!/9245/session/23 (accessed March 2021) [Google Scholar]
- Sallard E, Lescure FX, Yazdanpanah Y, Mentre F, Peiffer-Smadja N. Type 1 interferons as a potential treatment against COVID-19. Antiviral Res. 2020;178 doi: 10.1016/j.antiviral.2020.104791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellner J, Rommer PS. A review of the evidence for a natalizumab exit strategy for patients with multiple sclerosis. Autoimmun Rev. 2019;18:255–261. doi: 10.1016/j.autrev.2018.09.012. [DOI] [PubMed] [Google Scholar]
- Sharifian-Dorche M, Sahraian MA, Fadda G, et al. COVID-19 and disease-modifying therapies in patients with demyelinating diseases of the central nervous system: A systematic review. Mult Scler Relat Disord. 2021;50 doi: 10.1016/j.msard.2021.102800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson-Yap S, De Brouwer E, Kalincik T, et al. 8th Joint ACTRIMS-ECTRIMS Meeting, available at. 2020. First results of the COVID-19 in MS Global Data Sharing Initiative suggest antiCD20 DMTs are associated with worse COVID-19 outcomes.Abstract SS02-4.04, presented at the MSVirtual.https://msvirtual2020.org/wp-content/uploads/2020/09/SS02.04.pdf [Google Scholar]
- Sorensen PS, Sellebjerg F. Pulsed immune reconstitution therapy in multiple sclerosis. Ther Adv Neurol Disord. 2019;12 doi: 10.1177/1756286419836913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sormani M, Rossi N, Schiavetti I, et al. Disease Modifying Therapies and COVID-19 Severity in Multiple Sclerosis. SSRN Electronic Journal. 2020 doi: 10.2139/ssrn.3631244. available at https://ssrn.com/abstract=3631244. [DOI] [Google Scholar]
- St Michaels Unity Health Toronto. 2021. Multiple Sclerosis Clinic. MS Clinic COVID-19 updates. Guidance statements regarding COVID-19 vaccine by the Neurologists at the St. Michael's Hospital MS Clinic (January 11, 2021). Available at https://www.stmichaelshospital.com/programs/multiple-sclerosis/Covid-19.php (accessed March 2021).
- Vasileiou E, Simpson CR, Robertson C, et al. 2021. Effectiveness of first dose of COVID-19 vaccines against hospital admissions in Scotland: national prospective cohort study of 5.4 million people. Preprint of research article, available at https://www.ed.ac.uk/files/atoms/files/scotland_firstvaccinedata_preprint.pdf (accessed March 2021).
- Vogel AC, Schmidt H, Loud S, McBurney R, Mateen FJ. Impact of the COVID-19 pandemic on the health care of >1,000 People living with multiple sclerosis: A cross-sectional study. Mult Scler Relat Disord. 2020;46 doi: 10.1016/j.msard.2020.102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu GF, Boschert U, Hayward B, Lebson LA, CrossAH. 2021. Evaluating the impact of cladribine tablets on the development of antibody titres: interim results from the CLOCK-MS Influenza Vaccine Sub-Study. Abstract P071 presented at the ACTRIMS Virtual Forum 2021, available at https://www.abstractsonline.com/pp8/#!/9245/session/23 (accessed March 2021).
- Yamout B, Sahraian M, Bohlega S, et al. Consensus recommendations for the diagnosis and treatment of multiple sclerosis: 2019 revisions to the MENACTRIMS guidelines. Mult Scler Relat Disord. 2020;37 doi: 10.1016/j.msard.2019.101459. [DOI] [PubMed] [Google Scholar]
- Yong KP, Kim HJ. Disease modifying therapies and infection risks in multiple sclerosis-a decision-making conundrum. Ann Transl Med. 2020;8:722. doi: 10.21037/atm.2020.01.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabalza A, Cárdenas-Robledo S, Tagliani P, et al. COVID-19 in multiple sclerosis patients: susceptibility, severity risk factors and serological response. Advance publication online. 2020 doi: 10.1111/ene.14690. [DOI] [PubMed] [Google Scholar]