Abstract
Background
Associations between acne and gastrointestinal comorbidities suggest that microbial dysbiosis and intestinal permeability may promote inflammatory acne, a condition often managed with oral antibiotics.
Objective
We performed a case-control study to investigate the skin and gut microbiota in 8 acne patients before and after receiving oral minocycline compared to controls matched by age ±5 years, sex, and race.
Methods
DNA was extracted from stool samples and facial skin swabs. Sequencing of the V3V4 region of the bacterial 16S rRNA gene was performed using Illumina MiSeq and analyzed using QIIME/MetaStats 2.0 software.
Results
Acne patients included 7 female and 1 male, ages 20~32. Shannon diversity was not significantly different between the skin (p=0.153) or gut (p<0.999) microbiota of acne patients before and after antibiotics. The gut microbiota in pre-antibiotic acne patients compared to acne-free controls was depleted in probiotics Lactobacillus iners (p=0.001), Lactobacillus zeae (p=0.001), and Bifidobacterium animalis (p=0.026). After antibiotics, the gut microbiota of acne patients was depleted in Lactobacillus salivarius (p=0.001), Bifidobacterium adolescentis (p=0.002), Bifidobacterium pseudolongum (p=0.010), and Bifidobacterium breve (p=0.042), while the skin microbiota was enriched in probiotics Bifidobacterium longum (p=0.028) and Leuconostoc mesenteroides (p=0.029) and depleted in Staphylococcus epidermidis (p=0.009) and Prevotella nigrescens (p=0.028). At the phylum level, significant enrichment of Bacteroidetes in stool of acne patients following antibiotic treatment (p=0.033) led to a decreased Firmicutes to Bacteroidetes ratio.
Conclusion
Minocycline produces significant derangements in the microbiota of the skin and gut, including many probiotic species, highlighting the potential for more targeted antimicrobial treatments for acne.
Keywords: Acne vulgaris, Bacteroidetes, Firmicutes, Microbiome, Minocycline, Propionibacterium
INTRODUCTION
Emerging patterns of antibiotic resistance worldwide have called into question the use of both topical and systemic antibiotics in the routine treatment of acne. Dermatologists write more antibiotic prescriptions per provider than any other specialty1 with the majority of prescriptions being given for chronic, non-infectious skin diseases such as acne and rosacea2. Multiple studies have demonstrated that prolonged antibiotic use in the treatment of acne not only breeds resistance to Cutibacterium acnes3,4 resulting in decreased treatment efficacy5, but also promotes changes in microbiota at remote sites, including the back, nares, and oropharynx6,7.
Associations between acne and gastrointestinal (GI) dysfunction (halitosis, gastric reflux, bloating, and constipation) in adolescents are widely reported8. Furthermore, microbial dysbiosis in the GI tract has been considered as a potential etiology for acne for nearly 90 years, since Stokes and Pillsbury9 first suggested that disruptions in gut microbiota caused by stress could increase intestinal permeability, thus leading to systemic inflammation affecting the skin. Overgrowth of bacteria in the small intestine has been shown to increase intestinal permeability, while treatment with antimicrobials can partially restore the integrity of the intestinal border10. Increased intestinal permeability may allow increased passage of lipopolysaccharides (LPS) from gram-negative intestinal bacteria into the systemic circulation11, promoting inflammation and the development of acne lesions through their action on toll-like receptors (TLR) 2 and TLR4, which are significantly upregulated in inflammatory acne12.
Derangements in the gut microbiota have been demonstrated in patients with acne. Compared to controls, patients with acne display a decreased diversity of gut microbiota and a decreased ratio of Firmicutes to Bacteroidetes (F/B)13. Various investigations comparing the GI microbiota between different populations have yielded mixed results, but the majority of studies14,15,16,17 indicate that the Western diet (high in animal protein, sugar, starch, and fat and low in fiber)18 is associated with gut microbiota enriched in Bacteroidetes. As of yet, it is unclear whether the enrichment of gut Bacteroidetes in individuals consuming a Western diet has a coincidental or causal relationship in the development of acne, and what effect, if any, antibiotics have on gut Bacteroidetes levels.
This study uses 16S rRNA gene polymerase chain reaction (PCR) amplification and sequencing followed by taxonomic classification of these sequences to evaluate the skin and gut microbiota in acne patients both before and after systemic antibiotic treatment compared to controls to investigate the relationship between microbiota and the pathophysiology and treatment of acne vulgaris.
MATERIALS AND METHODS
Study design
A single-center, observational, case-control study was approved by the Johns Hopkins Institutional Review Board (IRB no. NA_00083373), and all participants provided written informed consent. Participants included 8 patients with moderate-to-severe acne vulgaris as determined by the Leeds revised acne grading system (RAGS)19 matched to 8 acne-free controls. The study was designed to evaluate the skin and GI microbiota of acne patients before and after antibiotic treatment compared to that of controls matched by age ±5 years, sex, and race. Stool and skin sampling was completed at the baseline clinic visit. Acne patients were prescribed oral minocycline (100 mg twice daily) and followed for 4 weeks, after which stool sampling and skin swabbing were repeated.
Inclusion criteria for all participants included: age ≥18 years, current diagnosis of moderate-to-severe acne for acne patients or lack of acne for healthy controls, and willingness to follow study protocols. Exclusion criteria included: inability to provide informed consent; significant medical history or concurrent illness; current or recently treated (7 days for topical antibiotics/steroids and 2 months for systemic antibiotics) skin diseases; intake of proton pump inhibitors, H2 receptor antagonists, laxatives, non-steroidal anti-inflammatory drugs, antacids, or antidiarrheal medications within 2 weeks of enrollment; history of facial surgeries or cosmetic procedures within 6 months; history of chronic GI disease, diabetes mellitus, cardiac disease, or immunodeficiency; history of major surgery of the GI tract within 5 years; unwillingness to avoid facial washing and cosmetics for 12 hours prior to sampling; known hypersensitivity to tetracyclines or minocycline; and pregnancy.
Sample collection
Skin swabs were obtained by vigorously swabbing the skin of three acne-prone regions of the face (bilateral cheeks, nose, and chin) with a sterile cotton-tipped applicator. Each area was separately swabbed for 30 seconds. Swabs were then individually stored in sample tubes and frozen at −80℃ within 24 hours of sample collection.
Stool collection kits were provided to each participant prior to the baseline clinical visit. Stool from a single bowel movement within 24 hours of the clinical visit was collected by the subject and brought in to the clinical visit. A 1~2 g portion of the sample was immediately dispersed in RNALater (Ambion, Austin, TX, USA) and stored at −80℃ until processed.
After initial stool and skin samples were obtained, only the patients with acne initiated oral minocycline. After 4 weeks, patients with acne provided repeat stool and skin samples using the same procedures as above. Patients were instructed to return their empty pill bottles to verify medication compliance.
DNA extraction and sequencing
Extraction of metagenomic DNA (mgDNA) was conducted from skin swabs as previously described20,21. Thawed samples were transferred aseptically to Lysing Matrix B tubes (MP Biomedicals, Solon, OH, USA). Lysozyme, mutanolysin, proteinase K, and lysostaphin enzymatic bacterial lysis was followed by bead-beating mechanical lysis. mgDNA was further purified using a Zymo fecal DNA kit (Zymogen, Irvine, CA, USA). Spectrophotometric measurements on the NanoDrop system (NanoDrop Technologies, Wilmington, DE, USA) and gel electrophoresis were used for DNA quality assurance. Phosphate-buffered saline negative extraction controls were included in sample processing. The V3V4 hypervariable region of the 16S rRNA gene was PCR amplified. The Illumina MiSeq 300-bp paired-reads platform (Illumina, San Diego, CA, USA) was used for sequencing as previously published22.
Statistical analysis
QIIME1 and MetaStats 2.0 software packages23,24 were used to construct bacterial community profiles of each sample, compute alpha- and beta-diversity, and identify differentially abundant taxa. Prior to analysis, reads were demultiplexed and filtered to remove low quality data, vector contaminants, and chimeric reads. The two reads in a pair were joined together based on overlap, yielding between 13,450 and 472,193 fragments per sample with an average of 134,544 fragments. Open clustering with the Green-Genes database (at 99% sequencing identity) was used to assign reads to operational taxonomic units (OTUs). Taxonomic frequency profiles were constructed to represent the community's OTU composition at each phylogenetic level. A maximum sample depth of 12,390 was used for both alpha and beta diversity. Rarefaction plots of alpha diversity were created for the Shannon diversity metric. Alpha diversity comparison between groups was computed using t-tests with Monte Carlo permutations through QIIME1. Beta diversity was calculated using weighted and unweighted UniFrac similarity measures, and statistical significance was computed within QIIME1 using analysis of similarity (ANOSIM)25, distance-based redundancy analysis (dbRDA), and adonis. Bacterial community profiles at each phylogenetic level, from phylum to species, were compared using the MetaStats 2.0 package to identify taxa that were statistically enriched or depleted in one group compared to another. For all comparisons, p<0.05 was considered statistically significant.
RESULTS
Participant demographics
The 8 acne patients included 3 Caucasian, 3 African American, and 2 Asian individuals, ages 20~32, while acnefree controls ranged from age 23~34. Both groups had comparable average body mass index (acne=25.5±4.3, controls=23.4±2.8). Baseline acne severity ranged from Leeds RAGS grade 3~5.
Sequencing dataset
Our complete sequence dataset contained 11,722,597 total read counts, of which 10,677,175 were matched to OTUs. 572 species-level OTUs were identified among the baseline skin samples of acne patients, while 527 were identified in controls. 288 species-level OTUs were identified in stool samples of acne patients at baseline, and 292 species-level OTUs were identified in controls. We identified the following unique, named taxa: 20 phyla, 45 classes, 85 orders, 156 families, 355 genera, and 236 species.
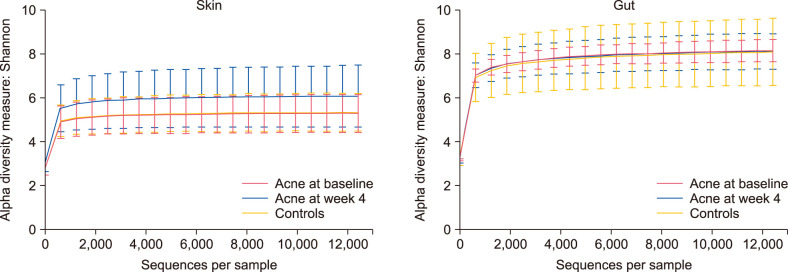
Alpha diversity
Alpha diversity, or intrasample diversity, was computed for each sample using the Shannon diversity metric. Combining all skin sites, swab samples from acne patients after 4 weeks of antibiotics displayed higher mean alpha diversity, though not to a statistically significant degree, compared to acne patients at baseline (p=0.153) and acnefree controls (p=0.264) (Fig. 1). The mean alpha diversity of acne-free controls (all skin=5.344) and acne patients at baseline (all skin=5.283) was highly similar (p<0.999). The mean alpha diversity of stool samples was comparable across all groups, with acne cases at baseline (8.199±0.493) displaying slightly higher mean alpha diversity compared to acne cases following 4 weeks of antibiotics (8.166±0.816, p<0.999) and acne-free controls (8.103±1.511, p<0.999).
Fig. 1. Rarefaction plots of mean alpha diversity were created with the Shannon diversity index metric to compare microbiota of the skin (all sites) and gut in controls, acne patients at baseline, and acne patients after 4 weeks of minocycline.
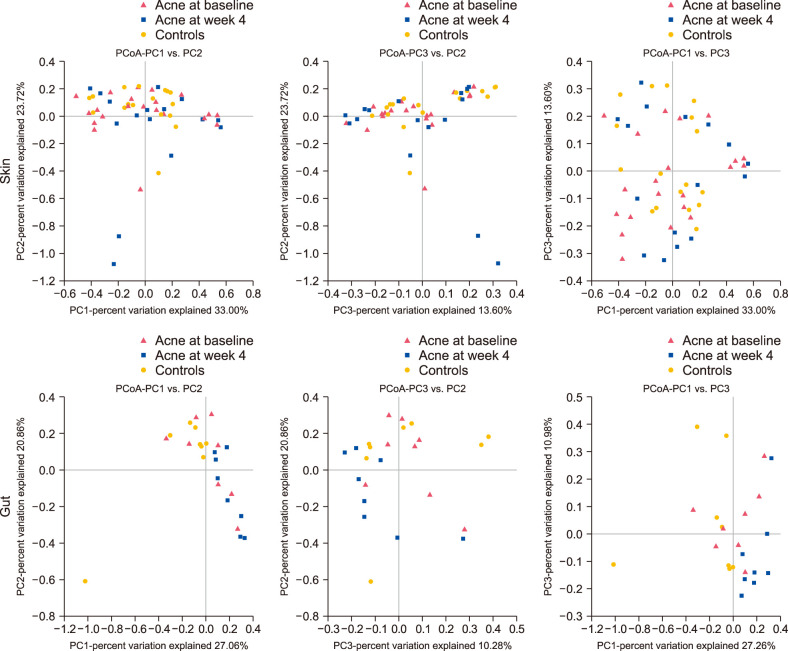
Beta diversity
Beta diversity can be used to measure the similarity in ecological community membership between samples. We used principal coordinates analysis of weighted UniFrac distances to compute beta diversity, or intersample diversity, of stool and skin samples among each participant community: acne-free controls, acne patients at baseline, and acne patients following 4 weeks of antibiotics (Fig. 2). Three principal coordinates (principal coordinates [PC]1, PC2, and PC3) were used to visualize ecologic similarity between communities, with clustering of samples close to one another on these coordinates representing similar bacterial composition between those samples. No significant clustering was observed among skin samples. Significant clustering was observed, however, among stool samples (ANOSIM, R=0.138, p=0.013; dbRDA, p=0.003), signifying that bacterial microbiota structure of stool samples was significantly different between each subject group.
Fig. 2. Principal coordinates analysis (PCoA) plots of weighted UniFrac distances demonstrating beta diversity of the microbiota of the skin (all sites) and gut in controls, acne patients at baseline, and acne patients after 4 weeks of minocycline. PC: principal coordinates.
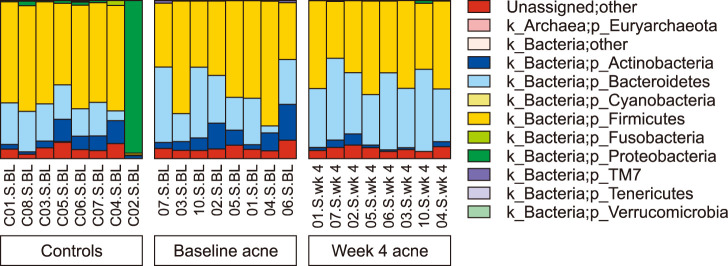
Relative abundance distribution by phylum
Among the skin microbiota, Proteobacteria, Firmicutes, and Actinobacteria dominated each group with varying relative abundances. Proteobacteria was universally present in the highest mean relative abundance: post-antibiotic acne patients (51.523±25.726%), acne-free controls (50.7603±15.666%), and baseline acne patients (50.199±24.100%). In acne-free controls, Proteobacteria was followed by Actinobacteria (31.156±18.160%) then Firmicutes (13.954±11.322%), while in acne patients, Proteobacteria was followed by Firmicutes (baseline: 23.670±21.412%; week 4: 20.196±17.297%) and then Actinobacteria (baseline: 22.677±15.320%; week 4: 20.810±17.225%).
The most abundant phylum among the gut microbiota in each group was Firmicutes (controls: 55.228±22.455%; baseline cases: 54.648±15.943%; week 4 cases: 49.070±8.457%) followed by Bacteroidetes (controls: 18.017±9.528%; baseline cases: 28.207±14.166%; week 4 cases: 41.931±8.338%) (Fig. 3). Bacteroidetes was significantly enriched in the gut microbiota after 4 weeks of antibiotics compared to acne patients at baseline (p=0.033) and acne-free controls (p=0.001). The mean ratio of F/B in the gut microbiota was highest in pre-antibiotic acne cases (3.988±5.950) followed by controls (3.652±2.702) and post-antibiotic acne cases (1.242±0.425).
Fig. 3. Phylum level relative abundance distribution of gut microbiota in controls, acne cases at baseline, and acne cases after 4 weeks of minocycline.
Relative abundance distribution by species
The most abundant species among the skin microbiota of each group was consistently C. acnes, with the highest mean relative abundance in the control group (28.179±18.557%) followed by acne patients before (19.055±15.459%) and after (14.544±15.403%) 4 weeks of antibiotics. The most abundant species within the gut microbiota of acne patients was Prevotella copri both before (4.719±13.346%) and after (4.768±12.936%) antibiotic treatment. The most abundant species in the gut microbiota of acne-free controls was Faecalibacterium prausnitzii (6.320±5.244%).
Significant differences in relative abundance of both skin and gut microbial species were identified between acnefree controls, acne patients at baseline, and acne patients following antibiotic treatment (Table 1, 2). Species with fewer than 15 total reads in both control and acne case groups as well as species present in 2 or fewer individual samples per comparison were excluded.
Table 1. Significantly enriched and depleted species in acne patients compared to controls.
| Acne patients at baseline | p-value | Acne patients after 4 weeks of antibiotics | p-value |
|---|---|---|---|
| Skin | |||
| Enriched | |||
| Staphylococcus pettenkoferi | 0.001 | Brevibacterium casei | 0.001 |
| Roseomonas mucosa | 0.001 | Eubacterium dolichum | 0.001 |
| Enterobacter cowanii | 0.001 | Alcaligenes faecalis | 0.001 |
| Actinobacillus parahaemolyticus | 0.001 | Klebsiella oxytoca | 0.006 |
| Psychrobacter sanguinis | 0.001 | Rothia dentocariosa | 0.009 |
| Paracoccus marcusii | 0.007 | Ruminococcus bromii | 0.019 |
| Prevotella nigrescens | 0.008 | Bifidobacterium breve | 0.036 |
| Prevotella melaninogenica | 0.035 | Roseburia faecis | 0.036 |
| Rothia mucilaginosa | 0.043 | Parabacteroides distasonis | 0.039 |
| Rothia aeria | 0.047 | ||
| Depleted | 0.001 | ||
| Anoxybacillus kestanbolensis | Corynebacterium kroppenstedtii | 0.001 | |
| Prevotella copri | 0.012 | Anoxybacillus kestanbolensis | 0.001 |
| Acinetobacter johnsonii | 0.025 | Cutibacterium acnes | 0.007 |
| Kocuria rhizophila | 0.028 | Bosea genosp. | 0.032 |
| Brevundimonas diminuta | 0.032 | Kocuria rhizophila | 0.035 |
| Coprococcus eutactus | 0.049 | Coprococcus catus | 0.036 |
| Gut | |||
| Enriched | |||
| Ruminococcus gnavus | 0.023 | Bacteroides plebeius | 0.002 |
| Bacteroides acidifaciens | 0.033 | Parabacteroides distasonis | 0.028 |
| Depleted | Ruminococcus gnavus | 0.034 | |
| Lactobacillus iners | 0.001 | Bifidobacterium adolescentis | 0.001 |
| Lactobacillus zeae | 0.001 | Janthinobacterium lividum | 0.001 |
| Bifidobacterium animalis | 0.026 | Akkermansia muciniphila | 0.020 |
| Rothia mucilaginosa | 0.049 | Clostridium hiranonis | 0.021 |
| Bifidobacterium pseudolongum | 0.041 |
Table 2. Significantly enriched and depleted species in acne patients following antibiotic treatment compared to acne patients at baseline.
| Acne Patients after 4 weeks of antibiotics | p-value |
|---|---|
| Skin | |
| Enriched | |
| Blautia obeum | 0.001 |
| Eubacterium dolichum | 0.001 |
| Klebsiella oxytoca | 0.001 |
| Comamonas terrigena | 0.013 |
| Roseburia faecis | 0.015 |
| Bifidobacterium longum | 0.028 |
| Leuconostoc mesenteroides | 0.029 |
| Dorea formicigenerans | 0.041 |
| Depleted | |
| Bacillus flexus | 0.001 |
| Paracoccus marcusii | 0.001 |
| Actinobacillus parahaemolyticus | 0.001 |
| Acinetobacter rhizosphaerae | 0.001 |
| Staphylococcus epidermidis | 0.009 |
| Prevotella nigrescens | 0.028 |
| Gut | |
| Enriched | |
| None | |
| Depleted | |
| Lactobacillus salivarius | 0.001 |
| Bifidobacterium adolescentis | 0.002 |
| Bifidobacterium pseudolongum | 0.010 |
| Bifidobacterium breve | 0.042 |
| Clostridium hiranonis | 0.04995 |
DISCUSSION
Oral antibiotics are part of the standard of care for moderate-to-severe acne. As of yet, it is unknown whether the efficacy of oral antibiotics in the treatment of acne is due to systemic absorption and action directly within the acne lesion or indirectly by action upon the local intestinal microbiome26. In this study, we sought to better understand the gut and skin microbiota in acne patients and whether it is impacted by antibiotic treatment.
The mean alpha diversity of skin microbiota was slightly higher in post-antibiotic acne patients compared to controls and pre-antibiotic acne patients, indicating no significant skin microbial dysbiosis, generally marked by decreased alpha diversity, between any participant communities. The response of the skin microbiota to antibiotics has been shown to be subject to intrapersonal variability27. Establishing a clear relationship between antibiotic treatment and skin microbial dysbiosis may require more participants than were sampled in this preliminary study. Alpha diversity of gut microbiota was similar across all participant groups, likewise demonstrating no significant gut dysbiosis in our acne participants before or after antibiotics. Investigation of beta diversity of skin microbiota demonstrated no significant similarities across participant groups. Beta diversity of gut microbiota, however, demonstrated statistically significant similarity between the ecological diversity of members within each participant community (controls, cases at baseline, and cases after 4 weeks of antibiotics). This demonstrates that the ecological community of the gut microbiota in acne patients is more affected by antibiotic treatment than it is by the identity of the participant.
While no species were enriched in the gut following antibiotics, the skin microbiota was enriched in probiotics Bifidobacterium longum and Leuconostoc mesenteroides. B. longum is a probiotic species colonizing the human gut28. Enrichment of the gut microbiota with B. longum has been associated with reduced depression scores in irritable bowel syndrome patients29 and reduced daily stress and improved memory in healthy volunteers30. L. mesenteroides is a probiotic lactic acid bacteria widely used in dairy fermentation31 that produces an exopolysaccharide immunostimulant that enhances mucosal immunoglobulin A (IgA) production32 and inhibits several inflammatory mediators such as nuclear factor-kappa B (NF-κB) that may have a role in acne33,34. NF-κB is a transcription factor that promotes the transcription of proinflammatory cytokines. Certain strains of C. acnes are known to provoke significant inflammation in acne. C. acnes directly induces the activation of NF-κB, which upregulates expression of proinflammatory interleukin-8 (IL-8). IL-8 is a neutrophilic chemokine that promotes the significant neutrophilic infiltration observed in inflammatory acne35. Enrichment of the skin microbiota with L. mesenteroides and its subsequent inhibition of C. acnes-induced inflammatory signaling pathways may therefore be involved in the anti-inflammatory properties of minocycline in acne.
After antibiotics, the skin microbiota was depleted in Staphylococcus epidermidis and Prevotella nigrescens. S. epidermidis is a biofilm-producing gram-positive coccus that colonizes normal human skin and has been shown to inhibit C. acnes growth36 and C. acnes-induced inflammation in the skin37. P. nigrescens is a black-pigmented rod found in the oral cavity that is a predominant organism in gingivitis38. It is unclear whether depletion of these organisms with antibiotics is coincidental or beneficial in acne treatment.
The gut microbiome in acne patients, at baseline relatively enriched in the phylum Bacteroidetes compared to controls, underwent a statistically significant increase in Bacteroidetes levels following antibiotic treatment. Enrichment with Bacteroidetes has been suggested as the “enterotype” of the Western diet14,15,16,17, and this finding has been shown to be more common in acne patients than in acne-free controls13. The role of diet in acne has long been under investigation. A high-protein, low glycemic-load diet has been associated with a decrease in total acne lesion counts compared to a conventional Western high glycemic-load diet39. It has been suggested that the increase in Bacteroidetes in the gut microbiome in individuals consuming a Western diet is therefore associated with the development of acne lesions13. We found that treatment of acne with antibiotics did not return Bacteroidetes abundance down to the level that is present in acne-free controls; on the contrary, Bacteroidetes was significantly enriched following antibiotics. This important finding suggests that, while the gut microbiome in acne patients differs from that of acne-free controls, it is not the enrichment with Bacteroidetes that is directly correlated with the presence of acne lesions. The association between the Western diet and the enrichment of the gut microbiota with Bacteroidetes may therefore be coincidental, rather than causal, in the development of acne in the absence of antibiotic therapy.
The gut microbiota in baseline acne patients compared to controls was depleted in probiotic gram-positive rods Lactobacillus iners40, Lactobacillus zeae41, and Bifidobacterium animalis42. After antibiotics, the gut microbiota of acne patients was depleted in Lactobacillus salivarius, Bifidobacterium adolescentis, Bifidobacterium pseudolongum, and Bifidobacterium breve. L. salivarius and B. adolescentis are lactic acid bacteria frequently isolated from the human GI tract that are thought to have probiotic activity43,44,45,46,47,48,49.
B. pseudolongum is associated with promoting the thickness of the intestinal mucus layer50, perhaps playing a protective role in inflammatory bowel disease51. The intestinal mucous layer acts as a physical barrier that minimizes contact between intestinal bacteria and the intestinal epithelium52. Secretory IgA, abundantly present in the mucus layer, traps bacteria and protects the intestinal epithelial cells from enteric toxins53. Disruption of the intestinal barrier increases translocation of pathogens and other antigens from the intestinal lumen to the lamina propria, stimulating an inflammatory response54. Increased passage of LPS into the systemic circulation and its action on TLR2 and TLR4 may promote the development of inflammatory acne11,12. B. breve is a probiotic that can stimulate intestinal cells in vitro to produce the cytokines IL-6 and IL-10, reducing inflammation.55,56,57 Administration of B. breve in celiac disease has been shown to temporarily decrease production of tumor necrosis factor alpha (TNF-α)58. C. acnes stimulates the release of proinflammatory cytokine TNF-α, which is significantly upregulated in nodular acne compared to papulopustular lesions, suggesting that its expression may be correlated with the severity of acne59. Because these probiotic species have a natural role in decreasing inflammation, including pathways associated with inflammation in acne, the depletion of these species with antibiotics is undesirable.
In a study investigating the efficacy of probiotics in alleviating the adverse effects of antibiotics in acne treatment, an oral probiotic mixture containing Lactobacillus acidophilus, Lactobacillus delbrueckii ssp. bulgaricus, and Bifidobacterium bifidum was demonstrated to have a synergistic effect with minocycline in decreasing lesion counts, suggesting a role for probiotics in the treatment of inflammatory acne60. While antibiotics have an important anti-inflammatory role in the treatment of acne, consideration should be given to replenishing the probiotic species that are depleted by this treatment.
This study was limited by a small participant size and a lack of strain-level resolution. Future work including additional participants and advanced sequencing techniques would provide valuable insight in this area. Additionally, our study focused on bacterial microbiota. Studies examining viruses and fungi would be needed to comprehensively profile the microbiota in acne.
This study investigated the differences in the microbiota of the skin and gut between acne patients before and after antibiotic treatment compared with acne-free controls. Oral minocycline produced significant derangements in the gut microbiota, including the undesirable depletion of multiple probiotic species: L. salivarius, B. adolescentis, B. pseudolongum, and B. breve. We identified several probiotic species that are significantly enriched in the gut microbiota of acne-free controls compared to acne patients that could potentially serve as targeted probiotic therapies for acne: L. iners, L. zeae, and B. animalis. Understanding the role of the gut microbiota in acne can provide insight into new treatment modalities.
ACKNOWLEDGMENT
This work was supported in part by an American Acne and Rosacea Society grant.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
References
- 1.Hicks LA, Bartoces MG, Roberts RM, Suda KJ, Hunkler RJ, Taylor TH, Jr, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis. 2015;60:1308–1316. doi: 10.1093/cid/civ076. [DOI] [PubMed] [Google Scholar]
- 2.Del Rosso JQ, Webster GF, Rosen T, Thiboutot D, Leyden JJ, Gallo R, et al. Status report from the scientific panel on antibiotic use in dermatology of the American Acne and Rosacea Society: part 1: antibiotic prescribing patterns, sources of antibiotic exposure, antibiotic consumption and emergence of antibiotic resistance, impact of alterations in antibiotic prescribing, and clinical sequelae of antibiotic use. J Clin Aesthet Dermatol. 2016;9:18–24. [PMC free article] [PubMed] [Google Scholar]
- 3.Coates P, Vyakrnam S, Eady EA, Jones CE, Cove JH, Cunliffe WJ. Prevalence of antibiotic-resistant propionibacteria on the skin of acne patients: 10-year surveillance data and snapshot distribution study. Br J Dermatol. 2002;146:840–848. doi: 10.1046/j.1365-2133.2002.04690.x. [DOI] [PubMed] [Google Scholar]
- 4.Ross JI, Snelling AM, Carnegie E, Coates P, Cunliffe WJ, Bettoli V, et al. Antibiotic-resistant acne: lessons from Europe. Br J Dermatol. 2003;148:467–478. doi: 10.1046/j.1365-2133.2003.05067.x. [DOI] [PubMed] [Google Scholar]
- 5.Simonart T, Dramaix M. Treatment of acne with topical antibiotics: lessons from clinical studies. Br J Dermatol. 2005;153:395–403. doi: 10.1111/j.1365-2133.2005.06614.x. [DOI] [PubMed] [Google Scholar]
- 6.Levy RM, Huang EY, Roling D, Leyden JJ, Margolis DJ. Effect of antibiotics on the oropharyngeal flora in patients with acne. Arch Dermatol. 2003;139:467–471. doi: 10.1001/archderm.139.4.467. [DOI] [PubMed] [Google Scholar]
- 7.Mills O, Jr, Thornsberry C, Cardin CW, Smiles KA, Leyden JJ. Bacterial resistance and therapeutic outcome following three months of topical acne therapy with 2% erythromycin gel versus its vehicle. Acta Derm Venereol. 2002;82:260–265. doi: 10.1080/000155502320323216. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H, Liao W, Chao W, Chen Q, Zeng H, Wu C, et al. Risk factors for sebaceous gland diseases and their relationship to gastrointestinal dysfunction in Han adolescents. J Dermatol. 2008;35:555–561. doi: 10.1111/j.1346-8138.2008.00523.x. [DOI] [PubMed] [Google Scholar]
- 9.Stokes JH, Pillsbury DM. The effect on the skin of emotional and nervous states Iii. Theoretical and practical consideration of a gastro-intestinal mechanism. Arch Derm Syphilol. 1930;22:962–993. [Google Scholar]
- 10.Lauritano EC, Valenza V, Sparano L, Scarpellini E, Gabrielli M, Cazzato A, et al. Small intestinal bacterial overgrowth and intestinal permeability. Scand J Gastroenterol. 2010;45:1131–1132. doi: 10.3109/00365521.2010.485325. [DOI] [PubMed] [Google Scholar]
- 11.Juhlin L, Michaëlsson G. Fibrin microclot formation in patients with acne. Acta Derm Venereol. 1983;63:538–540. [PubMed] [Google Scholar]
- 12.Terhorst D, Kalali BN, Ollert M, Ring J, Mempel M. The role of toll-like receptors in host defenses and their relevance to dermatologic diseases. Am J Clin Dermatol. 2010;11:1–10. doi: 10.2165/11311110-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Deng Y, Wang H, Zhou J, Mou Y, Wang G, Xiong X. Patients with acne vulgaris have a distinct gut microbiota in comparison with healthy controls. Acta Derm Venereol. 2018;98:783–790. doi: 10.2340/00015555-2968. [DOI] [PubMed] [Google Scholar]
- 14.Ou J, Carbonero F, Zoetendal EG, DeLany JP, Wang M, Newton K, et al. Diet, microbiota, and microbial metabolites in colon cancer risk in rural Africans and African Americans. Am J Clin Nutr. 2013;98:111–120. doi: 10.3945/ajcn.112.056689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Obregon-Tito AJ, Tito RY, Metcalf J, Sankaranarayanan K, Clemente JC, Ursell LK, et al. Subsistence strategies in traditional societies distinguish gut microbiomes. Nat Commun. 2015;6:6505. doi: 10.1038/ncomms7505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomez A, Petrzelkova KJ, Burns MB, Yeoman CJ, Amato KR, Vlckova K, et al. Gut microbiome of coexisting BaAka pygmies and bantu reflects gradients of traditional subsistence patterns. Cell Rep. 2016;14:2142–2153. doi: 10.1016/j.celrep.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 18.De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107:14691–14696. doi: 10.1073/pnas.1005963107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Brien SC, Lewis JB, Cunliffe WJ. The Leeds revised acne grading system. J Dermatolog Treat. 1998;9:215–220. [Google Scholar]
- 20.Roghmann MC, Lydecker AD, Hittle L, DeBoy RT, Nowak RG, Johnson JK, et al. Comparison of the microbiota of older adults living in nursing homes and the community. mSphere. 2017;2:e00210–e00217. doi: 10.1128/mSphere.00210-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bromberg JS, Hittle L, Xiong Y, Saxena V, Smyth EM, Li L, et al. Gut microbiota-dependent modulation of innate immunity and lymph node remodeling affects cardiac allograft outcomes. JCI Insight. 2018;3:121045. doi: 10.1172/jci.insight.121045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fadrosh DW, Ma B, Gajer P, Sengamalay N, Ott S, Brotman RM, et al. An improved dual-indexing approach for multiplexed 16S rRNA gene sequencing on the Illumina MiSeq platform. Microbiome. 2014;2:6. doi: 10.1186/2049-2618-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White JR, Nagarajan N, Pop M. Statistical methods for detecting differentially abundant features in clinical metagenomic samples. PLoS Comput Biol. 2009;5:e1000352. doi: 10.1371/journal.pcbi.1000352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clarke KR. Non-parametric multivariate analyses of changes in community structure. Austral Ecol. 1993;18:117–143. [Google Scholar]
- 26.Loveman DE, Noojin RO, Winkler CH., Jr Comparative studies of enteric bacterial flora in acne vulgaris. J Invest Dermatol. 1955;25:135–137. doi: 10.1038/jid.1955.110. [DOI] [PubMed] [Google Scholar]
- 27.Chien AL, Tsai J, Leung S, Mongodin EF, Nelson AM, Kang S, et al. Association of systemic antibiotic treatment of acne with skin microbiota characteristics. JAMA Dermatol. 2019;155:425–434. doi: 10.1001/jamadermatol.2018.5221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fukuda S, Toh H, Hase K, Oshima K, Nakanishi Y, Yoshimura K, et al. Bifidobacteria can protect from enteropathogenic infection through production of acetate. Nature. 2011;469:543–547. doi: 10.1038/nature09646. [DOI] [PubMed] [Google Scholar]
- 29.Romijn AR, Rucklidge JJ, Kuijer RG, Frampton C. A doubleblind, randomized, placebo-controlled trial of Lactobacillus helveticus and Bifidobacterium longum for the symptoms of depression. Aust N Z J Psychiatry. 2017;51:810–821. doi: 10.1177/0004867416686694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allen AP, Hutch W, Borre YE, Kennedy PJ, Temko A, Boylan G, et al. Bifidobacterium longum 1714 as a translational psychobiotic: modulation of stress, electrophysiology and neurocognition in healthy volunteers. Transl Psychiatry. 2016;6:e939. doi: 10.1038/tp.2016.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pujato SA, Guglielmotti DM, Martínez-García M, Quiberoni A, Mojica FJM. Leuconostoc mesenteroides and Leuconostoc pseudomesenteroides bacteriophages: Genomics and cross-species host ranges. Int J Food Microbiol. 2017;257:128–137. doi: 10.1016/j.ijfoodmicro.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Matsuzaki C, Takagaki C, Tomabechi Y, Forsberg LS, Heiss C, Azadi P, et al. Structural characterization of the immunostimulatory exopolysaccharide produced by Leuconostoc mesenteroides strain NTM048. Carbohydr Res. 2017;448:95–102. doi: 10.1016/j.carres.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Zununi Vahed S, Barzegari A, Rahbar Saadat Y, Goreyshi A, Omidi Y. Leuconostoc mesenteroides-derived anticancer pharmaceuticals hinder inflammation and cell survival in colon cancer cells by modulating NF-κB/AKT/PTEN/MAPK pathways. Biomed Pharmacother. 2017;94:1094–1100. doi: 10.1016/j.biopha.2017.08.033. [DOI] [PubMed] [Google Scholar]
- 34.Wang YY, Ryu AR, Jin S, Jeon YM, Lee MY. Chlorin e6-mediated photodynamic therapy suppresses P. acnes-induced inflammatory response via NFκB and MAPKs signaling pathway. PLoS One. 2017;12:e0170599. doi: 10.1371/journal.pone.0170599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen Q, Koga T, Uchi H, Hara H, Terao H, Moroi Y, et al. Propionibacterium acnes-induced IL-8 production may be mediated by NF-kappaB activation in human monocytes. J Dermatol Sci. 2002;29:97–103. doi: 10.1016/s0923-1811(02)00013-0. [DOI] [PubMed] [Google Scholar]
- 36.Wang Y, Kuo S, Shu M, Yu J, Huang S, Dai A, et al. Staphylococcus epidermidis in the human skin microbiome mediates fermentation to inhibit the growth of Propionibacterium acnes: implications of probiotics in acne vulgaris. Appl Microbiol Biotechnol. 2014;98:411–424. doi: 10.1007/s00253-013-5394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xia X, Li Z, Liu K, Wu Y, Jiang D, Lai Y. Staphylococcal LTA-induced miR-143 inhibits propionibacterium acnes-mediated inflammatory response in skin. J Invest Dermatol. 2016;136:621–630. doi: 10.1016/j.jid.2015.12.024. [DOI] [PubMed] [Google Scholar]
- 38.Lie MA, van der, Timmerman MF, Loos BG, van Steenbergen TJ, van der Velden U. Occurrence of Prevotella intermedia and Prevotella nigrescens in relation to gingivitis and gingival health. J Clin Periodontol. 2001;28:189–193. doi: 10.1034/j.1600-051x.2001.028002189.x. [DOI] [PubMed] [Google Scholar]
- 39.Smith RN, Mann NJ, Braue A, Mäkeläinen H, Varigos GA. The effect of a high-protein, low glycemic-load diet versus a conventional, high glycemic-load diet on biochemical parameters associated with acne vulgaris: a randomized, investigator-masked, controlled trial. J Am Acad Dermatol. 2007;57:247–256. doi: 10.1016/j.jaad.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 40.Falsen E, Pascual C, Sjödén B, Ohlén M, Collins MD. Phenotypic and phylogenetic characterization of a novel Lactobacillus species from human sources: description of Lactobacillus iners sp. nov. Int J Syst Bacteriol. 1999;49 Pt 1:217–221. doi: 10.1099/00207713-49-1-217. [DOI] [PubMed] [Google Scholar]
- 41.Zhou M, Yu H, Yin X, Sabour PM, Chen W, Gong J. Lactobacillus zeae protects Caenorhabditis elegans from enterotoxigenic Escherichia coli-caused death by inhibiting enterotoxin gene expression of the pathogen. PLoS One. 2014;9:e89004. doi: 10.1371/journal.pone.0089004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jungersen M, Wind A, Johansen E, Christensen JE, Stuer-Lauridsen B, Eskesen D. The science behind the probiotic strain Bifidobacterium animalis subsp. lactis BB-12(®) Microorganisms. 2014;2:92–110. doi: 10.3390/microorganisms2020092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Messaoudi S, Manai M, Kergourlay G, Prévost H, Connil N, Chobert JM, et al. Lactobacillus salivarius: bacteriocin and probiotic activity. Food Microbiol. 2013;36:296–304. doi: 10.1016/j.fm.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 44.O'Shea EF, O'Connor PM, Raftis EJ, O'Toole PW, Stanton C, Cotter PD, et al. Production of multiple bacteriocins from a single locus by gastrointestinal strains of Lactobacillus salivarius. J Bacteriol. 2011;193:6973–6982. doi: 10.1128/JB.06221-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee J, Ametani A, Enomoto A, Sato Y, Motoshima H, Ike F, et al. Screening for the immunopotentiating activity of food microorganisms and enhancement of the immune response by bifidobacterium adolescentis M101-4. Biosci Biotechnol Biochem. 1993;57:2127–2132. [Google Scholar]
- 46.Li D, Breiman A, le Pendu J, Uyttendaele M. Anti-viral Effect of Bifidobacterium adolescentis against noroviruses. Front Microbiol. 2016;7:864. doi: 10.3389/fmicb.2016.00864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.An HM, Lee DK, Kim JR, Lee SW, Cha MK, Lee KO, et al. Antiviral activity of Bifidobacterium adolescentis SPM 0214 against herpes simplex virus type 1. Arch Pharm Res. 2012;35:1665–1671. doi: 10.1007/s12272-012-0918-9. [DOI] [PubMed] [Google Scholar]
- 48.Cha MK, Lee DK, An HM, Lee SW, Shin SH, Kwon JH, et al. Antiviral activity of Bifidobacterium adolescentis SPM1005-A on human papillomavirus type 16. BMC Med. 2012;10:72. doi: 10.1186/1741-7015-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim MJ, Lee DK, Park JE, Park IH, Seo JG, Ha NJ. Antiviral activity of Bifidobacterium adolescentis SPM1605 against Coxsackievirus B3. Biotechnol Biotechnol Equip. 2014;28:681–688. doi: 10.1080/13102818.2014.945237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mangin I, Dossou-Yovo F, Lévêque C, Dessoy MV, Sawoo O, Suau A, et al. Oral administration of viable Bifidobacterium pseudolongum strain Patronus modified colonic microbiota and increased mucus layer thickness in rat. FEMS Microbiol Ecol. 2018;94 doi: 10.1093/femsec/fiy177. [DOI] [PubMed] [Google Scholar]
- 51.Pélissier MA, Vasquez N, Balamurugan R, Pereira E, Dossou-Yovo F, Suau A, et al. Metronidazole effects on microbiota and mucus layer thickness in the rat gut. FEMS Microbiol Ecol. 2010;73:601–610. doi: 10.1111/j.1574-6941.2010.00916.x. [DOI] [PubMed] [Google Scholar]
- 52.van der Waaij LA, Harmsen HJ, Madjipour M, Kroese FG, Zwiers M, van Dullemen HM, et al. Bacterial population analysis of human colon and terminal ileum biopsies with 16S rRNA-based fluorescent probes: commensal bacteria live in suspension and have no direct contact with epithelial cells. Inflamm Bowel Dis. 2005;11:865–871. doi: 10.1097/01.mib.0000179212.80778.d3. [DOI] [PubMed] [Google Scholar]
- 53.Mantis NJ, Rol N, Corthésy B. Secretory IgA's complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunol. 2011;4:603–611. doi: 10.1038/mi.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van der Meulen TA, Harmsen H, Bootsma H, Spijkervet F, Kroese F, Vissink A. The microbiome-systemic diseases connection. Oral Dis. 2016;22:719–734. doi: 10.1111/odi.12472. [DOI] [PubMed] [Google Scholar]
- 55.Mogna L, Del Piano M, Deidda F, Nicola S, Soattini L, Debiaggi R, et al. Assessment of the in vitro inhibitory activity of specific probiotic bacteria against different Escherichia coli strains. J Clin Gastroenterol. 2012;46 Suppl:S29–S32. doi: 10.1097/MCG.0b013e31826852b7. [DOI] [PubMed] [Google Scholar]
- 56.Aloisio I, Santini C, Biavati B, Dinelli G, Cencič A, Chingwaru W, et al. Characterization of Bifidobacterium spp. strains for the treatment of enteric disorders in newborns. Appl Microbiol Biotechnol. 2012;96:1561–1576. doi: 10.1007/s00253-012-4138-5. [DOI] [PubMed] [Google Scholar]
- 57.Drago L, De Vecchi E, Gabrieli A, De Grandi R, Toscano M. Immunomodulatory effects of Lactobacillus salivarius LS01 and Bifidobacterium breve BR03, alone and in combination, on peripheral blood mononuclear cells of allergic asthmatics. Allergy Asthma Immunol Res. 2015;7:409–413. doi: 10.4168/aair.2015.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klemenak M, Dolinšek J, Langerholc T, Di Gioia D, Mičetić-Turk D. Administration of Bifidobacterium breve decreases the production of TNF-α in children with celiac disease. Dig Dis Sci. 2015;60:3386–3392. doi: 10.1007/s10620-015-3769-7. [DOI] [PubMed] [Google Scholar]
- 59.Ozkanli S, Karadag AS, Ozlu E, Uzuncakmak TK, Takci Z, Zemheri E, et al. A comparative study of MMP-1, MMP-2, and TNF-α expression in different acne vulgaris lesions. Int J Dermatol. 2016;55:1402–1407. doi: 10.1111/ijd.13275. [DOI] [PubMed] [Google Scholar]
- 60.Jung GW, Tse JE, Guiha I, Rao J. Prospective, randomized, open-label trial comparing the safety, efficacy, and tolerability of an acne treatment regimen with and without a probiotic supplement and minocycline in subjects with mild to moderate acne. J Cutan Med Surg. 2013;17:114–122. doi: 10.2310/7750.2012.12026. [DOI] [PubMed] [Google Scholar]