Abstract
Background
Early cholecystectomy for acute cholecystitis has proved to reduce hospital length of stay but with no benefit in morbidity when compared to delayed surgery. However, in the literature, early timing refers to cholecystectomy performed up to 96 h of admission or up to 1 week of the onset of symptoms. Considering the natural history of acute cholecystitis, the analysis based on such a range of early timings may have missed a potential advantage that could be hypothesized with an early timing of cholecystectomy limited to the initial phase of the disease. The review aimed to explore the hypothesis that adopting immediate cholecystectomy performed within 24 h of admission as early timing could reduce post-operative complications when compared to delayed cholecystectomy.
Methods
The literature search was conducted based on the Patient Intervention Comparison Outcome Study (PICOS) strategy. Randomized trials comparing post-operative complication rate after early and delayed cholecystectomy for acute cholecystitis were included. Studies were grouped based on the timing of cholecystectomy. The hypothesis that immediate cholecystectomy performed within 24 h of admission could reduce post-operative complications was explored by comparing early timing of cholecystectomy performed within and 24 h of admission and early timing of cholecystectomy performed over 24 h of admission both to delayed timing of cholecystectomy within a sub-group analysis. The literature finding allowed the performance of a second analysis in which early timing of cholecystectomy did not refer to admission but to the onset of symptoms.
Results
Immediate cholecystectomy performed within 24 h of admission did not prove to reduce post-operative complications with relative risk (RR) of 1.89 and its 95% confidence interval (CI) [0.76; 4.71]. When the timing was based on the onset of symptoms, cholecystectomy performed within 72 h of symptoms was found to significantly reduce post-operative complications compared to delayed cholecystectomy with RR = 0.60 [95% CI 0.39;0.92].
Conclusion
The present study failed to confirm the hypothesis that immediate cholecystectomy performed within 24 h of admission may reduce post- operative complications unless surgery could be performed within 72 h of the onset of symptoms.
Keywords: Acute cholecystitis, Laparoscopic cholecystectomy, Timing
Background
Early timing of laparoscopic cholecystectomy is recommended for the treatment of acute cholecystitis since the current literature reports a shorter hospital stay after early cholecystectomy compared to delayed cholecystectomy [1, 2]. However, none of the published meta-analyses on the timing of cholecystectomy have reported any difference in morbidity between the two timings [3–10]. It should be emphasized that the definition of early cholecystectomy reported in the reviews was heterogeneous referring to intervention performed up to 96 h following the admission or up to 1 week following the onset of symptoms [3–10]. By considering such range of early timings within their analysis, the reviews did not allow to assess whether there may be an early timing that may influence outcomes and after which cholecystectomy should be considered no more as early but as delayed.
Based on the general pathology timing, acute inflammation tends to resolve after 72 h of the onset of an inflammatory process and let chronic inflammation take place [11, 12]. In patients with acute cholecystitis, all would therefore theoretically be expected to suffer local and systemic inflammation within 72 h of the onset of symptoms, but local and systemic changes may be, after this time, unpredictable for each patient. A rate of acute cholecystitis may be resolving and a rate may not be improving or even worsening as observed in delayed surgery strategy. As a result, once symptoms have been lasting for more than 72 h, any comparison between any different early and delayed timings could be more balanced. Moreover, having found no difference in morbidity may indicate that the compared early and delayed cholecystectomy within meta-analyses had an overlying risk of complications. It can be supposed therefore that performing cholecystectomy during the initial phase of the disease may prevent the complications related to the on-going cholecystitis at the time of surgery, especially for those evolving into a severe form for which post-operative complications are increased [13].
The Japanese Guidelines TG13 [14] recommended early cholecystectomy to be performed soon after the admission when less than 72 h have passed since the onset of symptoms but the recommendation was mainly based on expert opinion and setting early cholecystectomy within 72 h of symptoms is still controversial. In randomizing cholecystectomy before and after 72 h of symptoms during the same admission [15], a recent small trial found a difference in one oxidative stress marker but no correlation with post-operative complications. The latest Japanese guidelines TG18 [1] confirm the recommendation to perform early cholecystectomy within 72 h of symptoms but recommend also to perform early cholecystectomy as soon as possible even after this time, regardless of the onset of symptoms. According to Gull et al. [16], immediate cholecystectomy should not refer to the onset of symptoms but to admission since referring the timing of early cholecystectomy to the onset of symptoms is not always feasible because of the subjective perception of signs and symptoms. In their trial, the authors compared immediate cholecystectomy performed within 24 h of admission to delayed cholecystectomy and found a significant reduction in overall morbidity rate. However, the trial actually compared an early timing to a delayed timing and did not provide any information on immediate timing compared to other early timings. Moreover, in this trial, overall morbidity included complications occurred while waiting cholecystectomy the rate of which is expected to be greater in the delayed group and above all are poorly related to the early timing.
The clinical question on when early cholecystectomy should be performed has therefore not yet been answered. For the purpose, cholecystectomy performed within 24 h of admission appears to be the most appropriate option to evaluate the effectiveness of an immediate timing in clinical practice, moreover post-operative complications appear more appropriate than overall morbidity when exploring the role of immediate cholecystectomy within the early timing.
This study aimed to explore, through a review of the literature, the hypothesis that in patients with acute cholecystitis fit for urgent surgery, adopting immediate cholecystectomy performed within 24 h of admission as early timing could reduce post-operative complications when compared to delayed cholecystectomy.
Methods
Protocol and registration
A protocol reporting the methods of the meta-analysis was published [17] and registered on the PROSPERO database with number: CRD42020149600. The meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18].
Data sources
Two authors independently conducted a literature search, according to the Patient Intervention Comparison Outcome Study (PICOS) strategy. Subject headings and text words were used to identify randomized studies that included patients with acute cholecystitis submitted to laparoscopic cholecystectomy at different timings and that reported post-operative complications (Table 1). Neither date limits nor language limits were imposed. A translation was foreseen in case of a language not known to any of the authors.
Table 1.
Detailed search strategy on the databases
| Database | Search strategy | Found articles |
|---|---|---|
| PubMed | ((((((((cholecystitis[MeSH Terms]) OR acute cholecystitis[MeSH Terms]) OR cholecystitis, acute[MeSH Terms])) AND ((((laparoscop*) OR celioscop*) OR coelioscop*) OR peritoneoscop*)) AND ((cholecystectomy) OR cholecystectomies)) AND (((((immediate) OR early) OR urgent) OR delayed) OR timing)) AND (((morbidit*) OR complication*) OR post-operative)) AND random* | 66 |
| Cochrane Library | acute cholecystitis and cholecystectomy and randomized (publication type) | 99 |
| Embase | acute AND cholecystitis AND cholecystectomy AND [article]/lim AND [randomized controlled trial]/lim | 107 |
| ClinicalTrials.gov | acute cholecystitis and cholecystectomy and interventional studies and (terminated or completed) | 14 |
| PakiMedNet | acute cholecystitis randomized | 8 |
The literature search was conducted on PubMed, completed by consulting the Cochrane Library, Embase, and ClinicalTrials.gov and by reviewing the references of the found reviews and meta-analyses. Based on the review findings, the search was extended to Google Scholar and PakiMedNet database. Unpublished studies and data from presentations to Congress were not considered.
Studies selection
Two authors independently selected the studies while a third author was in charge in case of disagreement between the two authors. Studies were included in the current analysis only if they were randomized trials comparing different timings of laparoscopic cholecystectomy, in which the criteria for the diagnosis of acute cholecystitis, the population study, timing for surgery, and data on post-operative complications were reported.
Studies were excluded if the timing was defined using imprecise language without an exact numerical timing for the intervention, the population study was not defined, any clinically relevant categories of patients were excluded or patients with diseases other than acute cholecystitis were included.
Data collection
Data were independently collected by two authors and reported in a pre-prepared sheet. Data of studies comparing early timing to delayed timing of cholecystectomy were collected. The main outcome was the post-operative complication rate. Data were grouped based on three different timings of cholecystectomy: early timing within 24 h of admission defining immediate cholecystectomy, early timing over 24 h of admission and delayed timing referring to elective cholecystectomy performed after medical treatment. The hypothesis, that immediate cholecystectomy could reduce post-operative complications was therefore explored by comparing pooled data on early timing within 24 h of admission versus delayed timing of cholecystectomy and pooled data on early timing over 24 h admission versus delayed timing of cholecystectomy within a sub-group analysis.
The findings of studies, the timing of which did not refer to admission but to the onset of symptoms prompted to anticipate a second analysis that in the protocol was foreseen in the sensitivity analysis. These studies appeared to be of interest since they reported data on cholecystectomy performed within 72 h of the onset of symptoms, allowing a more suited analysis to the physiopathological hypothesis. As a result, the studies were included and data collected for a potential second analysis in which early timing within 72 h of symptoms and early timing over 72 h of symptoms were both compared to delayed timing of cholecystectomy within a subgroup analysis.
All complications were attributed to the initial assigned group with no distinction between complications occurred after cholecystectomy completed by laparoscopy and after cholecystectomy that required a conversion to laparotomy. Three other secondary outcomes were registered: bile duct injury, conversion and mortality. All reported bile duct injuries were registered without distinguishing those diagnosed both intra-operatively and immediately repaired from those diagnosed post-operatively. In any case, bile duct injuries were analyzed separately while post-operative bile leaks were considered within post-operative complications. All conversions were registered even when it was reported the reason was an intra-operative diagnosis of bile duct injury.
Risk of bias in individual studies
Two authors independently assessed the risk of bias. The quality assessment focused on the risk of bias arising from the randomization process, allocation concealment, blinding, missing outcome data, the measurement of the outcome, and selective reporting. Three different levels of risk (low, uncertain and high) were incorporated according to the findings of the risk of bias assessment.
Statistical methods
Since studies were all randomized and selected based on defined criteria, neither clinical nor methodological heterogeneities were expected. The relative risk (RR) and its 95% confidence interval (95% CI) were calculated adopting a fixed-effect model [19]. Heterogeneity was estimated with the chi-squared test and the I2 statistic and was excluded when the chi-squared was not significant and I2 < 25% [20, 21]. For sub-group difference analysis a chi-squared test was performed. The level of significance was set at 0.05. The meta-analysis was conducted using ReviewManager (RevMan) software (version 5.3) [22].
Risk of bias across studies
The quality of evidence was evaluated according to the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework [23]. The five domains that can lower the certainty of a body of evidence were considered as follows: risk of bias, inconsistency across studies, indirectness of studies, imprecision of studies, and publication bias. The rating up of the evidence was considered in case of a large effect. Publication bias was explored with a funnel plot by using the asymmetry of trial size against treatment effect to assess this bias [24, 25].
Sensitivity analysis
The fixed-effect model was compared to the random-effects model using the DerSimonian Laird method [26]. A further analysis was performed based on the exclusion of those studies the inclusion of which required a discussion. The role of excluded studies because of incomplete information about the exact timing of cholecystectomy or methodological aspect of the research was explored by including each of them in the immediate or delayed group according to the indicated or best estimate of the cholecystectomy timing.
Results
Study selection
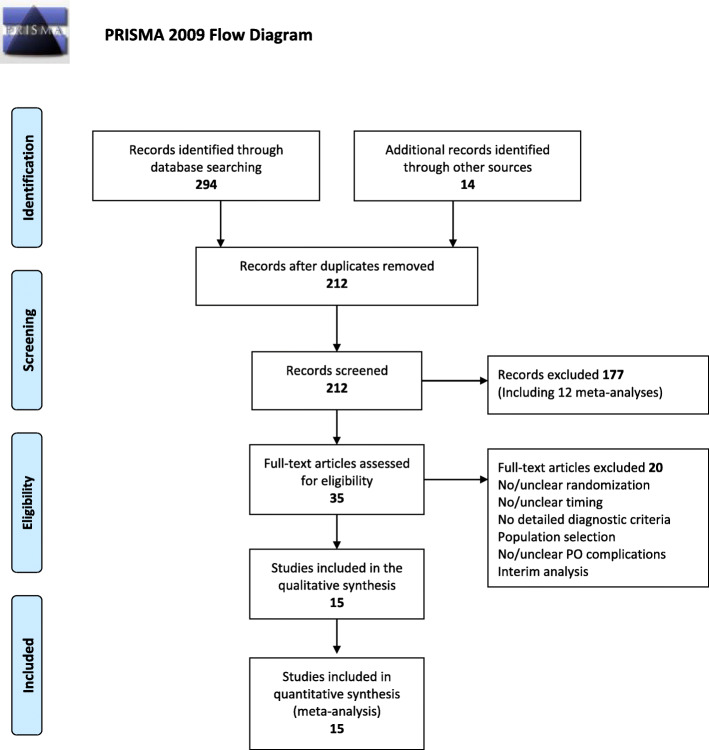
As reported in Fig. 1, there were 294 studies found from the five databases, with another 14 articles from other sources. After reading the titles and abstracts and eliminating duplicates, 35 articles were selected for full-text reading, of which 15 were included in the analysis [15, 27–40].
Fig. 1.
Literature search flow chart
Study characteristics
In total, three studies compared early timing within 24 h of admission to delayed timing of cholecystectomy [27–29] while six studies reported a comparison between early timing over 24 h of admission (from 48 to 72 h) and delayed timing of cholecystectomy [30–35]. However, the studies on early timing within 24 h of admission included in the early group patients with symptoms persisting up to 1 week [27] or up to 96 h [28], while in one study it was not possible to assess the exact timing related to the onset of symptoms [29]. Moreover, six additional studies that compared early timing within 72 h of symptoms to delayed timing of cholecystectomy were selected for a second analysis [15, 36–40]. The inclusion of one study in which patients were randomized to be operated on before and after 72 h of symptoms required discussion [37]. As all patients received medical treatment, the timing of 72 h after the symptoms was considered to be as delayed. The characteristics and the results of the studies reporting data on early timing of cholecystectomy performed within 24 h of admission and within 72 h of symptoms are summarized in Table 2.
Table 2.
Characteristics of studies that reported post-operative complications in comparing immediate cholecystectomy performed within 24 h from admission or within 72 h from on the onset of symptoms, compared to delayed cholecystectomy
| Authors | Year | Patients | Timing | Inclusion criteria | Exclusion criteria | Pathology confirmation | Post-operative complications | P value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Early | Delayed | Early | Delayed | Early | Delayed | ||||||
| Lai [27] | 1998 | 53 | 51 | < 24 h from admission | 6–8 weeks |
Clinical Laboratory Ultrasound |
CBD stone complications Previous surgery High risk for surgery Symptoms for more than 7 days |
Yes | 5 | 3 | 0.8 |
| Kolla [28] | 2014 | 20 | 20 | < 24 h from admission | 6–12 weeks |
Clinical Laboratory Ultrasound HIDA |
CBD stone complications Previous surgery High risk for surgery Symptoms for more than 96 h |
No | 2 | 3 | NR |
| Ozkardes [29] | 2014 | 30 | 30 | < 24 h from admission | 6–8 weeks |
Clinical Laboratory Ultrasound |
CBD stone complications Previous surgery High risk for surgery |
No | 5 | 0 | NR |
| Saber [36] | 2014 | 60 | 60 | < 72 h from symptoms | 6–8 weeks |
Clinical Laboratory Ultrasound |
NR | No | 6 | 4 | NR |
| Jan [37] | 2016 | 50 | 50 | < 72 h from symptoms |
> 72 h from symptoms Up to 7 days |
Clinical Laboratory Ultrasound |
CBD stone complications Previous surgery High risk for surgery Gallbladder malignancy Acalculus cholecystitis Symptoms for more than 7 days |
No | 1 | 3 | NR |
| Rajock [38] | 2016 | 31 | 31 | < 72 h from symptoms | 6–8 weeks |
Clinical Laboratory Ultrasound |
NR | Yes | 3 | 8 | NR |
| Arslan Onuk [15] | 2019 | 32 | 32 | < 72 h from symptoms |
> 72 h from symptoms Up to 6 days after initial treatment |
Clinical Laboratory Ultrasound |
CBD stone complications Previous surgery Perforation Sepsis Pregnancy Immunosuppression |
Yes | 4 | 9 | 0.12 |
| Arafa [39] | 2019 | 74 | 74 | < 72 h from symptoms | 6–12 weeks |
Clinical Laboratory Ultrasound |
CBD stone complications Previous surgery High risk for surgery Free biliary perforation Pregnancy Decompensated cirrhosis No consent available |
Yes | 10 | 17 | NR |
| El Kordy [40] | 2019 | 20 | 20 | < 72 h from symptoms | 6–8 weeks |
Clinical Laboratory Ultrasound |
NR | No | 4 | 6 | NR |
In total, 20 studies were excluded for the following reasons: the absence of or uncertainty about randomization [41–45], lack of reporting or uncertainty about timing [41, 46–50], lack of reporting or uncertainty about diagnostic criteria for acute cholecystitis [41, 45, 46, 51–54], limitation of the population study to the first episode and inclusion of biliary colic cases [53], inclusion of only patients with symptoms persisting for more than 72 h [50], exclusion of elderly patients [54], lack of reporting post-operative complications or lack of specifying whether the reported complications were primarily post-operative [16, 41, 48, 49, 55–58], or because the repoting of interim results of a randomized study [59].
Risk of bias within studies
Only five studies reported a computer-generated randomization sequence allowing a low risk of allocation concealment bias [27, 28, 33, 36, 39], seven studies reported an odd-even simple randomization method [15, 29, 30, 34, 35, 37, 40] and three studies did not report data on randomization method [31, 32, 38], with, as a result, an uncertain or high risk of selection bias. None of the studies reported any blinding. While the absence of information on blinding of operators and patients could be considered to be at low risk of bias (being hardly feasible in surgical trials), the absence of declared blinding of the outcome assessment may be of concern and the risk should be considered as uncertain [60]. The risk of bias related to the missing outcome data, the measurement of the outcome and selective reporting was considered as low for all the studies.
Synthesis of results
The comparison of pooled data on immediate versus delayed cholecystectomy failed to find any difference. The risk of post-operative complications was not significantly different when early timing within 24 h of admission was compared to delayed timing of cholecystectomy with RR = 1.89 [95% CI 0.76; 4.71]. Also, no difference was found by comparing early timing over 24 h of admission to delayed timing of cholecystectomy with RR = 1.37 [95% CI 0.85; 2.21]. Heterogeneity could not be excluded in the first comparison. The test for differences between sub-groups did not provide a significant result with p = 0.54 (Fig. 2).
Fig. 2.
Sub-group comparisons on post-operative complications based on timing related to time from admission: early timing of cholecystectomy within 24 h of admission defining immediate cholecystectomy and early timing of cholecystectomy over 24 h admission, both compared to delayed cholecystectomy
Within the second analysis, pooling data showed a statistically significant reduction in the rate of post-operative complications with RR = 0.60 [95% CI 0.39; 0.92] when early timing within 72 h of symptoms was compared to delayed timing of cholecystectomy. No heterogeneity was found. Among the included studies, eight of them reported a comparison between early cholecystectomy the timing of which was in all over 72 h of symptoms, and delayed cholecystectomy [28–35]. This finding allowed a sub-groups analysis based on the two different early timings, before and after 72 h of symptoms, both compared to delayed cholecystectomy. Pooled data from these studies did not show a significant difference between early timing over 72 h of symptoms and delayed cholecystectomy with RR = 1.32 [95% CI 0.86; 2.04]. No heterogeneity was found. Moreover, the comparison between the two sub-groups showed a statistically significant difference with p = 0.01, giving strength to the results concerning cholecystectomy performed within 72 h of symptoms (Fig. 3). The details of the post-operative complications related to this sub-group comparisons are reported in Table 3.
Fig. 3.
Sub-group comparison on post-operative complications based on timing related to time from the onset of symptoms: early cholecystectomy performed within 72 h of symptoms and early timing of cholecystectomy all over 72 h of symptoms, both compared to delayed cholecystectomy
Table 3.
Detailed post-operative complications reported within the studies included in the sub-group analysis that considered early timing related to the onset of symptoms
| Early timing of cholecystectomy within 72 h of symptoms | Delayed cholecystectomy | |
| Bile leak | 5 | 3 |
| Ileus | 1 | 6 |
| Intra-abdominal collection | 2 | 5 |
| Intra-abdominal bleeding | 1 | 3 |
| Wound and parietal hematoma or bleeding | 1 | 2 |
| Wound infection | 18 | 27 |
| Retained stones | 0 | 1 |
| Total | 28 | 47 |
| Early timing of cholecystectomy over 72 h of symptoms | Delayed cholecystectomy | |
| Bile leak | 11 | 4 |
| Ileus | 0 | 2 |
| Intra-abdominal collection | 5 | 7 |
| Intra-abdominal bleeding | 0 | 1 |
| Wound infection | 10 | 8 |
| Retained stones | 3 | 0 |
| Other infections | 9 | 6 |
| Respiratory complications | 3 | 3 |
| Atrial fibrillation | 0 | 1 |
| Total | 41 | 32 |
Overall ten studies reported data on biliary injury [27, 28, 30–35, 37, 39]. Among the studies that focused on immediate cholecystectomy performed within 24 h of admission compared to delayed cholecystectomy, two of them reported data on biliary injury [27, 28] but RR was not estimable because, one study reported no biliary injury [27] and one only one case in the immediate cholecystectomy group [28]. When considering studies that compared early cholecystectomy performed within 72 h of symptoms to delayed cholecystectomy, two studies reported data on biliary injury [37, 39], no significant difference was found with RR = 0.23 [95% CI 0.04; 1.34].
All included studies reported data on conversion. The analysis based on studies that compared immediate cholecystectomy performed within 24 h of admission to delayed cholecystectomy [27–29] reported no significant difference in conversion with RR = 1.21 [95% CI 0.68; 2.17] and I2 = 15%. When considering studies for which timing referred to the onset of symptoms [15, 36–40], cholecystectomy performed within 72 h of symptoms significantly reduced the rate of conversion compared to delayed cholecystectomy with RR = 0.53 [95% CI 0.32; 0.89] and I2 = 0%.
Reported mortality was very low and data were not sufficient to perform a meta-analysis on this variable.
Quality of evidence
As the present meta-analysis only included randomized studies, the level of evidence should first be considered high according to the GRADE rule. The only domain that should be considered in rating down the quality of evidence has been the potential risk of bias. None of the dedicated domains could allow the level of evidence to be rated up. The risk of bias involved not only the method of randomization, allocation concealment and blinding but also the lack of pathological confirmation of a diagnosis of acute cholecystitis. While all cases are expected to be non-acute at the time of surgery in the delayed group, an unknown rate of non-acute cases in the immediate group because of a diagnostic error may be source of an overestimation of the benefit of immediate cholecystectomy.
A large magnitude of the effect was not found, the dose-response gradient was not applicable and no potential residual confounders would decrease the magnitude of the effect. The funnel plot shown in Fig. 4 illustrates the low risk for potential publication bias in this study. Overall, the quality of evidence of this meta-analysis should be considered moderate.
Fig. 4.

Funnel plot assessing the risk for potential publication bias
Sensitivity analysis
The sensitivity analysis performed by applying the random-effects model revealed similar results compared to the fixed-effect model, for both immediate cholecystectomy performed within 24 h of admission and for cholecystectomy performed within 72 h of symptoms. About early timing within 24 h of admission versus delayed timing of cholecystectomy RR = 1.61 [95% CI 0.44; 5.85] with I2 = 33%; about early timing over 24 h of admission versus delayed timing of cholecystectomy RR = 1.38 [95% CI 0.77; 2.46] with I2 = 20%; p = 0.83 for the sub-group comparison. About early timing within 72 h of symptoms versus delayed timing of cholecystectomy RR = 0.60 [95% CI 0.39; 0.93] with I2 = 0%; about early cholecystectomy over 72 h of symptoms versus delayed cholecystectomy RR = 1.29 [95% CI 0.82; 2.03] with I2 = 0%; p = 0.02 for the sub-group comparison.
According to the literature finding and selected studies, no other sensitivity analysis was feasible for comparisons based on immediate cholecystectomy performed within 24 h of admission. The two further planned sensitivity analyses were therefore limited to the comparisons based on cholecystectomy performed within 72 h of symptoms. By excluding the study which was a matter of discussion [37], sensitivity analysis confirmed the results on the risk of post-operative complications: RR = 0.61 [95% CI 0.40; 0.95] with I2 = 0% for cholecystectomy performed within 72 h of symptoms compared to delayed cholecystectomy; RR = 1.32 [95% CI 0.86; 2.04] with I2 = 0% when other early timings were compared to delayed cholecystectomy; p = 0.01 for the sub-group comparison.
When investigating the effect of the inclusion of studies that had been omitted because of incomplete information regarding the exact timing of cholecystectomy, the absence of reported criteria for the diagnosis of acute cholecystitis, or other methodological aspects of the studies, the sensitivity analysis confirmed the results of the main comparison: RR = 0.60 [95% CI 0.39; 0.92] with I2 = 0% for cholecystectomy performed within 72 h of symptoms compared to delayed cholecystectomy; RR = 1.10 [95% CI 0.83; 1.46] with I2 = 7% when other early timings were compared to delayed cholecystectomy; p = 0.02 for the sub-group comparison.
Discussion
The present review failed to confirm the hypothesis that immediate cholecystectomy performed within 24 h of admission may influence post-operative complications but a limited number of studies were found, which furthermore included patients with late presentation. However, an additional timing analysis based on the natural history of acute cholecystitis found that early timing within 72 h of symptoms reduced post-operative complications compared to delayed timing of cholecystectomy. Moreover, the finding that conversions were also reduced when adopting such timing gives strength to the hypothesis that cholecystectomy may be safer if performed, when possible, in the initial phase of acute cholecystitis.
The quality of evidence was rated as moderate because of the finding of a potential risk of selection bias. The risk was due to the method of randomization, allocation concealment, and blinding, as well as a lack of pathological confirmation of the diagnosis of acute cholecystitis. Among the selected studies on early timing of cholecystectomy within 24 h of admission or within 72 h of symptoms, only three reported a computer-generated randomization [27, 28, 39] while one did not report data on the randomization process [38] and four reported a simple randomization method with an uncertain or high allocation concealment risk [15, 29, 37, 40]. Globally, the level of risk related to the absence of blinding of operators and patients was considered being low while that related to the absence of blinding of the outcome assessment was uncertain [60]. Although the combined clinical, laboratory, and imaging criteria for acute cholecystitis have a low risk of diagnostic error [1], without a pathological confirmation of the diagnosis, which was reported only in one among the studies on immediate cholecystectomy performed within 24 h [27] and in three among the studies on early cholecystectomy performed within 72 h of symptoms [30, 38, 39], the inclusion of non-acute cases within the studies could not be excluded [2]. Randomization would equally distribute these patients in both arms but, while all patients are expected to be non-acute in the delayed group, a percentage of non-acute cases within the early group may be a cause of bias in estimating the effect of early timing of cholecystectomy. Moreover, the rate of confirmed severe cholecystitis in immediate cholecystectomy within 24 h of admission or within 72 h of symptoms compared to other timings is reported only in two studies [27, 30], not allowing to extrapolate any conclusive data on the rate of on-going acute cholecystitis according to the timing of surgery.
Signficant results on post-operative complications are limited to patients submitted to early surgery performed within 72 h of symptoms, but surgery is not feasible within such timing for all patients because of possible late presentation as reported in the selected studies [27, 28, 30–35]. Moreover, the data on the feasibility of surgery within such timing in the general population are limited. Among the studies on early timing within 72 h of symptoms [15, 36–40], only one study [15] reported the rate of excluded patients because of symptoms lasting for more than 72 h at admission, such rate was 54% of all the patients admitted for acute cholecystitis during the study period. Some reported exclusion criteria, such as patients with sepsis, severe cholecystitis with organ failure, perforation, or those at high surgical risk because of medical illness, were mandatory for ethical reasons. Nevertheless, only complications related to biliary migration in the common bile duct and previous surgery [15, 37, 39] as well as pregnancy [15] should be considered when defining the population to which the results of the present meta-analysis should be applied.
The present study focused on post-operative complications as the main outcome. For the purpose of the meta-analysis, both local as well as systemic complications whenever reported by the selected studies were considered. The main result of the present study has not confirmed the finding of the analysis reported within TG 18 guidelines [1] according to which complications were reduced in early cholecystectomy even when performed after 72 h of the onset of symptoms. The finding of TG 18 referred to a comparison reported within a meta-analysis [8], which was however limited to wound infections. Within the analysis comparing cholecystectomy performed within 72 h of symptoms to delayed cholecystectomy in the present study, wound infections were the most frequently reported post-operative complication but were not the only one that favoured early cholecystectomy [36–38, 40].
Perioperative or overall morbidity could have been considered for the evaluation of the timing of cholecystectomy, but such outcomes should include not only post-operative complications but also, when reported, intra-operative complications and complications while awaiting cholecystectomy. Intra-operative complications do not substantially change the course of a patient’s history unless they require conversion or involve bile duct injury. Both have been analyzed as secondary outcomes in the present review, with the finding that cholecystectomy performed within 72 h of symptoms reduced conversion when compared to delayed cholecystectomy, while no significant differences were found in instances of bile duct injury with low prevalence in both early and delayed cholecystectomy. Moreover, none of the selected studies reported which was the rate of complications while awaiting cholecystectomy.
Most studies focused on the failure rate of conservative treatment and re-admission for the recurrence of symptoms of acute cholecystitis while awaiting cholecystectomy [27, 28, 30–32, 34–36, 38, 46, 50, 51, 53]. These outcomes however concern the delayed cholecystectomy that is performed weeks after the acute phase of cholecystitis and have no interest when investigating different early timings of cholecystectomy. However, the risk of failure of conservative treatment and of re-admission for the recurrence of acute cholecystitis in delayed surgery, as well as the reduction in length of hospital reported in all the meta-analyses [3–10], the related cost reduction [16, 29, 34] and better quality of life [61] favoring early surgery, should be considered when deciding the timing of cholecystectomy for those patients whose symptoms were lasting for more than 72 h at the time of a feasible surgery.
Conclusions
The present study failed to confirm the hypothesis that immediate cholecystectomy performed within 24 h of admission may reduce post-operative complications. However, the finding of studies in which timing did not refer to admission but to the onset of symptoms allows to suggest that immediate cholecystectomy should be preferred to delayed cholecystectomy when feasible within 72 h of the onset of symptoms. Once symptoms have persisted for more than 72 h at the time of a feasible surgery, others outcomes and risk factors should be considered when deciding the timing of cholecystectomy.
Acknowledgements
Many thanks to Dr. Annalisa CASTELLI for her valuable contribution to the manuscript revision process.
Abbreviations
- PICOS
Patient Intervention Comparison Outcome Study
- RR
Relative risk
- CI
Confidence interval
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- GRADE
Grading of Recommendations, Assessment, Development and Evaluations
Authors’ contributions
GB conceived the systematic review and meta-analysis, developed the search and data collection strategy, designed and wrote the protocol, and participated in the assessment of the quality of the studies and risk of bias assessment, statistical analyses, the interpretation of findings, assessment of the quality of evidence and the drafting of the manuscript. SK contributed to the development of the review protocol and participated in the literature search and the selection of the studies. MS participated in the literature search and the selection of studies. MP contributed to the development of the review protocol, data collection, and the assessment of the quality of the studies, as well as the risk of bias assessment and revision of the manuscript. NA participated in data collection, statistical analyses, the interpretation of findings, the assessment of the quality of evidence, and the revision of the manuscript. LA provided critical revision of the manuscript. YK acted as an arbitrator in cases of disagreement between two authors and provided critical revision of the manuscript. All authors read, provided feedback, and approved the final version of the protocol and all authors read, provided feedback, and approved the final version of the manuscript.
Funding
There were no sources of funding for this research study.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Not applicable
Ethical approval was not be required for this systematic review and meta-analysis, as only a secondary analysis of data already available in scientific databases were conducted.
Consent for publication
Not applicable. The manuscript does not contain data from any person.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, Iwashita Y, Hibi T, Pitt HA, Umezawa A, Asai K, Han HS, Hwang TL, Mori Y, Yoon YS, Huang WSW, Belli G, Dervenis C, Yokoe M, Kiriyama S, Itoi T, Jagannath P, Garden OJ, Miura F, Nakamura M, Horiguchi A, Wakabayashi G, Cherqui D, de Santibañes E, Shikata S, Noguchi Y, Ukai T, Higuchi R, Wada K, Honda G, Supe AN, Yoshida M, Mayumi T, Gouma DJ, Deziel DJ, Liau KH, Chen MF, Shibao K, Liu KH, Su CH, Chan ACW, Yoon DS, Choi IS, Jonas E, Chen XP, Fan ST, Ker CG, Giménez ME, Kitano S, Inomata M, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25(1):55–72. doi: 10.1002/jhbp.516. [DOI] [PubMed] [Google Scholar]
- 2.Ansaloni L, Pisano M, Coccolini F, Peitzmann AB, Fingerhut A, Catena F, Agresta F, Allegri A, Bailey I, Balogh ZJ, Bendinelli C, Biffl W, Bonavina L, Borzellino G, Brunetti F, Burlew CC, Camapanelli G, Campanile FC, Ceresoli M, Chiara O, Civil I, Coimbra R, de Moya M, di Saverio S, Fraga GP, Gupta S, Kashuk J, Kelly MD, Khokha V, Jeekel H, Latifi R, Leppaniemi A, Maier RV, Marzi I, Moore F, Piazzalunga D, Sakakushev B, Sartelli M, Scalea T, Stahel PF, Taviloglu K, Tugnoli G, Uraneus S, Velmahos GC, Wani I, Weber DG, Viale P, Sugrue M, Ivatury R, Kluger Y, Gurusamy KS, Moore EE. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg. 2016;11(1):25. doi: 10.1186/s13017-016-0082-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papi C, Catarci M, D'Ambrosio L, Gili L, Koch M, Grassi GB, Capurso L. Timing of cholecystectomy for acute calculous cholecystitis: a meta-analysis. Am J Gastroenterol. 2004;99(1):147–155. doi: 10.1046/j.1572-0241.2003.04002.x. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqui T, MacDonald A, Chong PS, Jenkins JT. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. 2008;195(1):40–47. doi: 10.1016/j.amjsurg.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Syst Rev. 2013;(6):CD005440. [DOI] [PubMed]
- 6.Zhou MW, Gu XD, Xiang JB, Chen ZY. Comparison of clinical safety and outcomes of early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis. Sci World J. 2014;2014:274516. doi: 10.1155/2014/274516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu XD, Tian X, Liu MM, Wu L, Zhao S, Zhao L. Meta-analysis comparing early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2015;102(11):1302–1313. doi: 10.1002/bjs.9886. [DOI] [PubMed] [Google Scholar]
- 8.Cao AM, Eslick GD, Cox MR. Early cholecystectomy is superior to delayed cholecystectomy for acute cholecystitis: a meta-analysis. J Gastrointest Surg. 2015;19(5):848–857. doi: 10.1007/s11605-015-2747-x. [DOI] [PubMed] [Google Scholar]
- 9.Menahem B, Mulliri A, Fohlen A, Guittet L, Alves A, Lubrano J. Delayed laparoscopic cholecystectomy increases the total hospital stay compared to an early laparoscopic cholecystectomy after acute cholecystitis: an updated meta-analysis of randomized controlled trials. HPB (Oxford) 2015;17:857–862. doi: 10.1111/hpb.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyu Y, Cheng Y, Wang B, Zhao S, Chen L. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: an up-to-date meta-analysis of randomized controlled trials. Surg Endosc. 2018;32(12):4728–4741. doi: 10.1007/s00464-018-6400-0. [DOI] [PubMed] [Google Scholar]
- 11.Bochsler PN, Slauson DO. Inflammation and repair of tissue. In: Slauson DO, Cooper BJ, editors. Mechanisms of disease: a textbook of comparative general pathology. 3. St. Louis: Mosby; 2002. p. 141. [Google Scholar]
- 12.Kumar V, Abbas AK, Fausto N. Chapter 2. In: Kumar V, Abbas AK, Fausto N, editors. Robbins and Cotran pathologic basis of disease. 7. Elsevier Saunders; 2005. p. 47. [Google Scholar]
- 13.Borzellino G, Sauerland S, Minicozzi AM, Verlato G, Pietrantonj CD, Manzoni G, et al. Laparoscopic cholecystectomy for severe acute cholecystitis. A meta-analysis of results. Surg Endosc. 2008;22(1):8–15. doi: 10.1007/s00464-007-9511-6. [DOI] [PubMed] [Google Scholar]
- 14.Yamashita Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Gomi H, Dervenis C, Windsor JA, Kim SW, de Santibanes E, Padbury R, Chen XP, Chan ACW, Fan ST, Jagannath P, Mayumi T, Yoshida M, Miura F, Tsuyuguchi T, Itoi T, Supe AN, Tokyo Guideline Revision Committee TG13 surgical management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20(1):89–96. doi: 10.1007/s00534-012-0567-x. [DOI] [PubMed] [Google Scholar]
- 15.Arslan Onuk ZA, Gündüz UR, Koç Ü, Kızılateş E, Gömceli İ, Akbaş SH, Bülbüller N. Same-admission laparoscopic cholecystectomy in acute cholecystitis: the importance of 72 hours and oxidative stress markers. Ulus Travma Acil Cerrahi Derg. 2019;25(5):440–446. doi: 10.14744/tjtes.2019.17807. [DOI] [PubMed] [Google Scholar]
- 16.Gutt CN, Encke J, Koninger J, Harnoss JC, Weigand K, Kipfmuller K, et al. Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial. Ann Surg. 2013;258(3):385–393. doi: 10.1097/SLA.0b013e3182a1599b. [DOI] [PubMed] [Google Scholar]
- 17.Borzellino G, Khuri S, Pisano M, Mansour S, Allievi N, Ansaloni L, Kluger Y. Timing of early laparoscopic cholecystectomy for acute calculous cholecystitis revised: protocol of a systematic review and meta-analysis of results. World J Emerg Surg. 2020;15(1):1. doi: 10.1186/s13017-019-0285-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med. 1987;6(3):341–350. doi: 10.1002/sim.4780060325. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Review Manager (RevMan) [Computer program]. Version 5.3. The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- 23.Schünemann H, Brożek J, Guyatt G, Oxman A. The GRADE Working Group. GRADE handbook for grading quality of evidence and strength of recommendations. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html Updated Oct 2013.
- 24.Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001;20(4):641–654. doi: 10.1002/sim.698. [DOI] [PubMed] [Google Scholar]
- 26.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 27.Lai PBS, Kwong KH, Leung KL. Randomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 1998;85(6):764–767. doi: 10.1046/j.1365-2168.1998.00708.x. [DOI] [PubMed] [Google Scholar]
- 28.Kolla SB, Aggarwal S, Kumar A, Kumar R, Chumber S, Parshad R, Seenu V. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc. 2004;18(9):1323–1327. doi: 10.1007/s00464-003-9230-6. [DOI] [PubMed] [Google Scholar]
- 29.Ozkardes AB, Tokaz M, Dumlu EG, Bozkurt B, Ciftci AB, Yetisir F, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized study. Int Surg. 2014;99(1):56–61. doi: 10.9738/INTSURG-D-13-00068.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lo C, Liu C, Fan S, Lai ECS, Wong J. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1998;227(4):461–467. doi: 10.1097/00000658-199804000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandler CF, Lane JS, Ferguson P, Thompson JE, Ashley SW. Prospective evaluation of early versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis. Am Surg. 2000;66(9):896–900. [PubMed] [Google Scholar]
- 32.Johansson M, Thune A, Blomqvist A, Nelvin L, Lundell L. Management of acute cholecystitis in the laparoscopic era: results of a prospective, randomized clinical trial. J Gastrointest Surg. 2003;7(5):642–645. doi: 10.1016/S1091-255X(03)00065-9. [DOI] [PubMed] [Google Scholar]
- 33.Gul R, Dar RA, Sheikh RA, Salroo NA, Matoo AR, Wani SH. Comparison of early and delayed laparoscopic cholecystectomy for acute cholecystitis: experience from a single center. N Am J Med Sci. 2014;5:414–418. doi: 10.4103/1947-2714.115783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghnnam WM, Alzahrany E, Elbeshry MAS, Alqarni A, Al-Shahrani M. Early versus interval cholecystectomy for acute cholecystitis: 5 years local experience. Int J Surg Med. 2017;3:150–155. [Google Scholar]
- 35.Parmar KD, Patel MV, Bengali IS. Comparative study of outcomes of early versus interval laparoscopic cholecystectomy in acute calculus cholecystitis. IOSR J Dent Med Sci. 2017;16:68–73. [Google Scholar]
- 36.Saber A, Hokkam EN. Operative outcome and patient satisfaction in early and delayed laparoscopic cholecystectomy for acute cholecystitis. Minim Invasive Surg. 2014;2014:162643. doi: 10.1155/2014/162643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jan Y, Shah M, Hussain S, Waqas, Din A, Khan A. Variables affecting outcome of laparoscopic cholecystectomy in acute cholecystitis. Pak J Surg. 2016;32:16–21. [Google Scholar]
- 38.Rajcok M, Bak V, Danihel L, Kukucka M, Schnorrer M. Early versus delayed laparoscopic cholecystectomy in treatment of acute cholecystitis. Bratisl Lek Listy. 2016;117(6):328–331. doi: 10.4149/bll_2016_065. [DOI] [PubMed] [Google Scholar]
- 39.Arafa AS, Khairy MM, Amin MF. Emergency versus delayed laparoscopic cholecystectomy for acute cholecystitis. Egypt J Surg. 2019;38:171–179. [Google Scholar]
- 40.El-Kordy MM, Basiony Aboulyazid AS, Ahmed Mahmoud AF. Comparison of outcomes of early versus delayed laparoscopic cholecystectomy in acute calcular cholecystitis. Egypt J Hosp Med. 2019;76:4162–4168. [Google Scholar]
- 41.Ghani AA, Haq A. Acute cholecystitis: immediate versus interval cholecystectomy. J Postgrad Med Inst. 2005;19:192–195. [Google Scholar]
- 42.Agrawal R, Sood KC, Agarwal B. Evaluation of early versus delayed laparoscopic cholecystectomy in acute cholecystitis. Surg Res Pract. 2015;2015:349801. doi: 10.1155/2015/349801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taha AM, Mohamed Yousef A, Gaber A. Early versus delayed laparoscopic cholecystectomy for uncomplicated acute cholecystitis. J Surg. 2016;4(3):29–33. doi: 10.11648/j.js.s.2016040301.16. [DOI] [Google Scholar]
- 44.Khalid S, Iqbal Z, Bhatti AA. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. J Ayub Med Coll Abbottabad. 2017;29:570–573. [PubMed] [Google Scholar]
- 45.Abbasi F, Ahmed S. Laparoscopic cholecystectomy; comparison of early versus delayed laparoscopic cholecystectomy in acute cholecystitis: a randomized control trial. Prof Med J. 2019;26:474–478. [Google Scholar]
- 46.Khan SSA. Early versus delayed cholecystectomy for acute cholecystitis, a prospective randomized study. Pak J Gastroenterol. 2002;16:30–34. [Google Scholar]
- 47.Yadav RP, Adhikary S, Agrawal CS, Bhattarai B, Gupta RK, Ghimire A. A comparative study of early vs. delayed laparoscopic cholecystectomy in acute cholecystitis. Kathmandu Univ Med J. 2009;7:16–20. doi: 10.3126/kumj.v7i1.1759. [DOI] [PubMed] [Google Scholar]
- 48.Faizi KS, Ahmed I, Ahmad H. Comparison of early versus delayed laparoscopic cholecystectomy: choosing the best. Pak J Med Health. 2013;7:212–215. [Google Scholar]
- 49.Akhtar NN, Fawad A, Allam KM. Early versus delayed laparoscopic cholecystectomy in acute cholecystitis. Pak J Med Health Sci. 2016;10:1039–1043. [Google Scholar]
- 50.Roulin D, Saadi A, Di Mare L, Demartines N, Halkic N. Early versus delayed cholecystectomy for acute cholecystitis, are the 72 hours still the rule? A randomized trial. Ann Surg. 2016;264(5):717–722. doi: 10.1097/SLA.0000000000001886. [DOI] [PubMed] [Google Scholar]
- 51.Davila D, Manzanares C, Picho ML, Albors P, Cardenas F, Fuster E, et al. Experience in the treatment (early vs. delayed) of acute cholecystitis via laparoscopy. Cir Esp. 1999;66:233. [Google Scholar]
- 52.Imbisat MZ, Rizvi SAA, Ali I. An evaluation of early and delayed laparoscopic cholecystectomy for acute cholecystitis. Int Surg J. 2019;6(9):3147–3151. doi: 10.18203/2349-2902.isj20193680. [DOI] [Google Scholar]
- 53.Macafee DA, Humes DJ, Bouliotis G, Beckingham IJ, Whynes DK, Lobo DN. Prospective randomized trial using cost-utility analysis of early versus delayed laparoscopic cholecystectomy for acute gallbladder disease. Br J Surg. 2009;96(9):1031–1040. doi: 10.1002/bjs.6685. [DOI] [PubMed] [Google Scholar]
- 54.Abdalgaleil MM, Shaat AM, Elbalky OS, Ibrahim MM, Elnagaar MS. Is it safe to do laparoscopic cholecystectomy for acute cholecystitis up to 7 days? Menoufia Med. 2020;32:1267–1271. doi: 10.4103/mmj.mmj_206_19. [DOI] [Google Scholar]
- 55.Javed I, Fahim M, Malik NA, Khan MS, Adalat I, Khan JS, et al. Evaluation of early urgent versus delayed urgent laparoscopic cholecystectomy in the treatment of acute cholecystitis. J Rawal Med Coll. 2013;17:185–188. [Google Scholar]
- 56.Verma S, Agarwal PN, Bali RS, Singh R, Talwar N. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Minim Invasive Surg. 2013;2013:486107. [Google Scholar]
- 57.Mustafa MIT, Mustafa AIT, Chaudhry SM, Mustafa RIT. Early vs delayed laparoscopic cholecystectomy in acute cholecystitis. Pak J Med Health Sci. 2016;10:371–373. [Google Scholar]
- 58.Hegazy OT, Soliman SS. Early versus interval laparoscopic cholecystectomy for treatment of non-complicated acute calcular cholecystitis. Egypt J Surg. 2018;37(4):543–548. doi: 10.4103/ejs.ejs_82_18. [DOI] [Google Scholar]
- 59.Mare LD, Saadi A, Roulin D, Demartines N, Halkic N. Delayed versus early laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized study. HPB. 2012;14:130. [Google Scholar]
- 60.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yu H, Chan EE, Lingam P, Lee J, Woon WWL, Low JK, et al. Index admission laparoscopic cholecystectomy for acute cholecystitis restores Gastrointestinal Quality of Life Index (GIQLI) score. Ann Hepatobiliary Pancreat Surg. 2018;22(1):58–65. doi: 10.14701/ahbps.2018.22.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.