Abstract
Purpose
Understanding how religion and spirituality influence health-related quality of life (HRQoL) is important for developing holistic, patient-centered treatment. This study determined distinct latent classes of religiousness/spirituality for adult persons living with HIV (PLWH) and associations between latent class membership and HRQoL.
Methods
Baseline data was collected from 223 patients in the FAmily CEntered (FACE) Advance Care Planning (ACP) clinical trial for PLWH. Patients completed the Brief Multidimensional Measurement of Religiousness/Spirituality (BMMRS-adapted), Patient Health Questionnaire (PHQ-9), Medical Outcome Study-HIV Survey (MOS-HIV) and the Palliative care Outcome Scale (POS). The optimal number of latent classes was determined by comparing K-Class model with (K-1)-Class model iteratively. The relationship between latent class membership, HRQoL and demographic characteristics was assessed.
Results
Patients were 56.1% male, 86.1% Black/African American, aged 22–77 (Mean=50.83). 75.3% were Christian. LCA identified three classes: traditionally religious (35%), privately religious (47.1%), and spiritual but not religious (17.9%). MOS-HIV mental health (p < 0.001), MOS-HIV quality of life (p = 0.014) and MOS-HIV health transition (p = 0.016) scores were significantly higher among patients who were traditionally religious. These patients were more likely to be 40+ years and Black. Patients in the privately religious group had the lowest levels of mental health and HRQoL.
Conclusions
Understanding how religiousness and spirituality influence HRQoL can help the medical community develop holistic, patient-centered and culturally-sensitive interventions that could improve outcomes for PLWH and potentially mitigate the impact of health disparities within the Black and LGBTQ communities.
Keywords: HIV/AIDS, health-related quality of life, religion, spirituality, inclusivity
Introduction
Religion and spirituality affect attitudes and preferences for medical treatment and palliative care (Koenig & Davies, 2003; Mazanec & Tyler, 2003; Saguil & Phelps, 2012; Lyon et al., 2019). Although similar, religion and spirituality are distinct concepts (Saguil & Phelps, 2012; Hill & Pargament, 2003). As defined by the 2009 Spiritual Care Consensus Conference (Puchalski et al., 2009), spirituality is concerned with the transcendent, addressing ultimate questions about life’s meaning and purpose. Religion is a spirituality shared by a group of people, often with a common set of beliefs and practices (Puchalski et al., 2009).
Spirituality and religion impact health behaviors and outcomes among persons living with HIV (PLWH) (Dalmida, Koenig, Holstad, & Thomas, 2015; Doolittle, Justice, & Fiellin, 2018; Ironson, Kremer, & Lucette, 2016; Kremer et al., 2015; Trevino et al., 2010; Oji et al., 2017; Lee, Nezu, & Nezu, 2014). In PLWH, higher levels of spirituality are positively associated with overall well-being, medication adherence and slowed disease progression (Oji et al., 2017; Kremer & Ironson, 2014; Pargament, Koenig, Tarakeshwar, & Hahn, 2001; Tuck, McCain, & Elswick, 2001; Cotton et al., 2006; Ironson, Stuetzle, & Fletcher, 2006; Yi et al., 2006; Koenig, 2008; Koenig, Pargament, & Nielsen, 1998). A sense of peace and faith in God is associated with longer survival for PLWH (Ironson et al., 2006; Ironson et al., 2002). The FAmily CEntered (FACE) Advance Care Planning research demonstrated spirituality, specifically a sense of meaning and purpose, was associated with decreased depression and anxiety for adolescents living with HIV (Lyon et al., 2014) and that higher religiousness/spirituality increased the likelihood to want to continue intensive treatment at end-of-life (Lyon et al., 2019).
PLWH can engage in both positive and negative religious coping: the view of God as benevolent and forgiving, “God has not abandoned me because of my HIV”, versus punishing and judgmental, “God has abandoned me because of my HIV” (Ironson et al., 2011). Transactional Stress and Coping Theory suggests positive coping facilitates cognitive reappraisals to support positive psychological states, in this case overcoming spiritual guilt and HIV-related shame (Ironson et al., 2016; Folkman, 1997). Promoting positive religious coping may be relevant to treatment, as it predicts survival rate of PLWH over 17 years independent of medication adherence, substance use and social support (Folkman, 1997). Negative religious coping, on the other hand, is associated with emotional distress and is a robust predictor of decline in health status (Kremer et al., 2015; Lee et al., 2014; Pargament et al., 2001; Fitchett et al., 2004). For example, the belief that “HIV is a punishment from God” predicts disease progression in adults, controlling for confounders (Ironson et al., 2011). Effect sizes were greater than those for depression. Adolescents in the FACE study who held the religious belief that “HIV is a punishment from God” were less medication adherent (p = 0.04), less spiritual (p = 0.05) and were more likely to be behavioral rather than perinatally infected (Lyon et al., 2014; Lyon et al., 2011). This belief was not associated with end-of-life treatment preferences (Lyon et al., 2019).
An innovative method to further investigate the relationship between religion/spirituality and health in PLWH is latent class analysis (LCA). LCA is a statistical method that is used to organize multiple dimensions of outcome measures such that individuals in each latent class share common outcome patterns. LCA can be thought of as a “person-centered” approach to creating empirically-derived typologies. Furthermore, unlike the traditional clustering techniques such as cluster analysis or k-means clustering, LCA is model-based and permits a mathematical evaluation of how well a proposed LCA model represents the data. There is limited information about latent class membership of religion/spirituality for PLWH in the United States. One study of non-HIV positive adolescents identified five distinct religious/spiritual classes and their relationship to sociodemographic variables: girls were more likely to be religious and African-Americans were less likely to be Atheist (Pearce, Foster, & Halliday-Hardie, 2013). In a study conducted by Lyon and colleagues, the authors identified four distinct latent classes of religiousness/spirituality for adolescents living with HIV using the Brief Multidimensional Measurement of Religiousness/Spirituality (BMMRS): highest religiousness/spirituality, attending religious services only, religious experiences without attending services, and lowest religiousness/spirituality (2016). Social quality of life was highest among the group with the highest religiousness/spirituality, suggesting attending religious services is a valuable source of social support (Lyon et al., 2016). However, emotional quality of life was higher in the lowest overall religiousness/spirituality group, supporting findings from a previous latent class analysis that low spirituality scores on the BMMRS were associated with lower depression (Barton & Miller, 2015). These findings demonstrate that religion/spirituality can be either protective or detrimental for health. Differences may be accounted for by the type of religious coping a patient uses (Ironside et al., 2011).
Determining how aspects of spirituality and religion influence health behavior and outcomes is important for developing holistic, patient-centered treatment. Within both primary and palliative care settings patients want to address spirituality as part of treatment: studies found 33% of outpatients in primary care clinics and 77% of inpatients in palliative care want to talk to their physician about religious beliefs (MacLean et al., 2003; King & Bushwick, 1994). If they became gravely ill, 94% of outpatients at a pulmonary clinic and 70% in a primary care clinic would want to discuss religious/spiritual beliefs with physicians (MacLean et al., 2003; Ehman, Ott, & Short, 1999). In a study with adolescents (N = 45), 53% of whom were living with HIV and 80% of whom were African-American, only 9% had ever been asked by their doctor about their spiritual/religious beliefs (Bernstein, D’Angelo, & Lyon, 2013). However, most teens wanted their provider to ask them about their spiritual beliefs, especially when dealing with death/dying or chronic illness (67%). Those with HIV were more likely to endorse wanting their doctors to pray with them (42% vs. 15%). These findings demonstrate circumstances in which healthcare providers should consider discussing religious/spiritual beliefs with patients.
Objective & Hypotheses
This study investigated how spirituality and religion influenced health-related quality of life (HRQoL) outcomes among PLWH in a cultural minority group. Building off of previous research in an adolescent sample (Lyon et al., 2016), the purpose of this study was to determine whether distinct latent classes of religiousness/spirituality exist for adult PLWH, and if so, is latent class membership associated with HRQoL or sociodemographic variables. This study asked two questions: (1) Do different classes of religiousness/spirituality exist for adult PLWH? (2) If classes of religiousness/spirituality exist, is the class membership associated with HRQoL or sociodemographic variables?
Methods
Study Design & Participants
The FACE ACP clinical trial for HIV positive adults was approved by the Institutional Review Board at Children’s National (coordinating center) and the participating study sites. This was a palliative care clinical trial that recruited HIV positive adults who were 21 years or older from five urban, hospital-based outpatient clinics in Washington, DC. Participants selected surrogates as their health care agents, who were adults 18 years or older. We initially recruited individuals based on the following criteria: (1) detectable viral load on two occasions over a 12-month period, (2) a CD4 count (<200), (3) current opportunistic infection, (4) HIV infected with a co-morbidity that may significantly limit life expectancy, including malignancy, cirrhosis, cardiomyopathy, end stage renal/kidney or liver disease, diabetes or HIV Associated Neuropathy, or (5) in/outpatients with AIDS receiving dialysis. The inclusion criteria were broadened in Year 3 of the study to increase enrollment to include all persons 21 years or older ever diagnosed with HIV at any age. This change in inclusion criteria is consistent with the consensus definition of advance care planning as appropriate for any age and any stage of health in understanding and sharing their personal values, life goals and preferences regarding future medical care (Sudore et al., 2017).
Further inclusion criteria required that both patients and surrogates knew of and were willing to discuss the patient’s HIV diagnosis. Exclusion criteria included signs of HIV dementia, homicidality, suicidality, or psychosis, as determined during screening by trained study staff. We also excluded patients who did not have a surrogate decision-maker willing to participate. There were 868 patients assessed for eligibility. 645 individuals were excluded: 192 did not meet initial inclusion criteria, 107 could not identify a surrogate decision-maker, 14 were screening failures (were suicidal, homicidal or psychotic), and 453 declined to participate with the most common reasons being time issues (N = 85) or did not want to talk about ACP (N = 24). Data were not available for all who declined. 223 eligible and enrolled patient/family dyads were randomized. Further details about the study design and methodology are published elsewhere (Kimmel, Wang, Scott, Briggs & Lyon, 2015).
Trained study staff conducted screening and informed written consent with both the patient and the surrogate. Following consent, study staff collected baseline data from 223 patient-surrogate dyads in the FACE ACP trial. A trained research assistant verbally administered questionnaires to participants and recorded answers on the standardized paper forms. Patients and surrogates met with the research assistant independently. Data were later entered into the secure online database REDCap by study staff. Administration of baseline questionnaires occurred before randomization, so all participants completed these surveys regardless of group assignment. Participants were given monetary compensation to complete 15 baseline questionnaires in the course of 60 minutes. Four of the baseline questionnaires administered by the research assistants were the Brief Multidimensional Measurement of Religiousness/Spirituality (BMMRS-adapted), the Patient Health Questionnaire (PHQ-9), the Medical Outcome Study-HIV Survey (MOS-HIV) and the Palliative care Outcome Scale (POS).
Materials
Quality of Life
The MOS-HIV is a comprehensive measure of HRQoL in the past month used with PLWH. The questionnaire consists of 35-items comprising eleven dimensions: general health perceptions, pain, physical functioning, role functioning, social functioning, cognitive functioning, mental health, energy, health distress, QoL and health transition (Wu et al., 1991; Revicki, Sorensen, & Wu, 1998; Wu, Revicki, Jacobson, & Malitz, 1997). Each subscale can be scored from 0–100, with a higher score representing better health. Strengths of the MOS-HIV include that it is internally consistent (α = ≥ 0.70), has good reliability and has good validity- especially when used with African-Americans and individuals with low socioeconomic status (Wu et al., 1997; Henderson et al., 2010). In this analysis, we analyzed latent class membership in relationship to five dimensions of the MOS-HIV that showed significance in a previous study (Lyon et al., 2014). See Tables 2 and 6 for details.
Table 2.
Descriptive Statistics (N=223)
| Variable | Mean (SD) | Cronbach’s Alpha | Note |
|---|---|---|---|
| POS total score (10 items) | 7.1 (5.8) | 0.71 | Full range: 0–40. The higher score, the worse health. |
| PHQ-9 score (9 items) | 3.9 (4.6) | 0.84 | Full range: 0–27. The higher score, the higher depression. |
| MOS-HIV general health perceptions (5 items) | 57.7 (27.3) | 0.83 | Full range: 0–100. The higher score, the higher personal health. |
| MOS-HIV mental health (5 items) | 77.8 (18.5) | 0.78 | Full range: 0–100. The higher score, the higher feelings of calm, peace and happiness. |
| MOS-HIV health distress (5 items) | 80.6 (24.7) | 0.88 | Full range: 0–100. The higher score, the less feeling despair, discouraged and afraid due to health. |
| MOS-HIV quality of life (1 item) | 72.1 (22.3) | - | Full range: 0–100. The higher score, the higher quality of life. |
| MOS-HIV health transition (1 item) | 69.4 (24.8) | - | Full range: 0–100. The higher score, the greater improvement in health over the past 4 weeks. |
POS: Patient Outcomes Scale for over past 3 days. PHQ-9: Patient Health Questionnaire for over the last 2 weeks. MOS-HIV: Medical Outcome Study-HIV Health Survey for during past 4 weeks.
Table 6.
Selected results of 3-step LCA model: The relationship between QOL outcomes and Religious latent class membership
| Religious LCA model | POS | PHQ-9 | MOS-HIV General Health Perception | MOS-HIV Mental Health | MOS-HIV Health Distress | MOS-HIV Quality of Life | MOS-HIV Health Transition |
|---|---|---|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |
| Class 1 | 6.5 (0.9) | 3.0 (0.5) | 61.1 (3.9) | 85.6 (2.0) | 82.9 (3.4) | 78.8 (2.7) | 77.2 (4.0) |
| Class 2 | 7.2 (0.7) | 4.7 (0.5) | 56.6 (3.1) | 72.9 (2.2) | 77.6 (2.9) | 67.3 (2.5) | 67.6 (2.6) |
| Class 3 | 8.1 (1.0) | 3.6 (0.8) | 54.0 (5.6) | 77.0 (3.7) | 85.0 (3.9) | 73.7 (6.5) | 59.1 (5.1) |
| P-value§ | 0.478 | 0.092 | 0.520 | <0.001 | 0.358 | 0.014 | 0.016 |
The POS assesses the physical, psychological, psychosocial, emotional, practical and spiritual needs of palliative care patients in the past three days (Aspinal et al., 2002). All 10 POS questions are scored using a 0–4 Likert scale, which can be summed to create a total score between 0–40. A higher score indicates worse health. Advantages of the POS include good construct validity [35]. Validation research demonstrated adequate internal consistency, α = 0.65 (Hearn & Higginson, 1999).
Mental Health
The PHQ-9 is a self-administered version of the PRIME-MD diagnostic instrument for mental health conditions (Kroenke, Spitzer, & Williams, 2001). This questionnaire assesses a person’s mental health for the past two weeks by asking about each of the 9 DSM-IV criteria for depression. Answers range from 0 (not at all) - 3 (nearly every day). The total score ranges from 0–27, with a higher score indicating worse depressive symptoms. The PHQ-9 is a reliable and valid measure of both depression and depression severity, demonstrating internal consistency (α = 0.83 – 0.92), convergent and discriminant validity, responsiveness to change, and appropriateness with PLWH (Kroenke et al., 2001; Cameron, Crawford, Lawton, & Reid, 2008; Titov et al., 2011; Simoni et al., 2011).
Religious Coping
The BMMRS-adapted (Fetzer Institute, 1999) is a 36-item survey developed to assess health-relevant domains of religiousness and spirituality. It includes 12 domains: daily spiritual experiences, meaning, values, beliefs, forgiveness, private religious practices, religious/spiritual coping, religious support, religious/spiritual history, commitment, organizational religiousness and religious preference. No total score is calculated. Investigators pre-select items, domains, or factors for analysis. Reliability (α = ≥ 0.70) and validity are well-established (Harris, Holder, Kulig, Schrier, & Knight, 2007; Cotton, McGrady, & Rosenthal, 2010; Masters et al., 2009). In the current study, five items from the BMMRS-adapted were selected prior to the analysis, based on our previous research indicating that only five items were statistically significantly correlated with outcomes of interest (Lyon et al., 2014). These items were drawn from the subscales (1) Daily Spiritual Experiences (I feel God’s presence from ‘0 = Never’ to ‘5 = Many times a day); (2) Private Religious Practices (How often do you pray privately…at times when you are not attending functions of a religiously based group? From ‘0 = Never’ to ‘7 = More than once a day’); (3) Organizational Religiousness (How often do you go to religious services? From ‘0 = Never’ to ‘5 = Many times a day’); (4) Religious Identity (To what extent do you consider yourself a religious person? From ‘0 = Not at all religious’ to ‘3 = Very religious’); and (5) Spiritual Identity (To what extent do you consider yourself a spiritual person? From ‘0 = Not at all spiritual’ to ‘3 = Very spiritual’). Religiousness/spirituality was operationally defined as higher scores on each these five items. That is, all the five items were recoded as dichotomous measures. For example, Private Religious Practice was recoded as a 1: daily prayer, 0: less than daily prayer; Daily Spiritual Experiences was recoded as 1: everyday or more, 0: less than everyday; Organizational Religiousness was recoded as 1: every week or more, 0: less than every week; Religious Identity was recoded as 1: moderately or very religious, 0: slightly or not religious; Spiritual Identity was recoded as 1: moderately or very spiritual, 0: slightly or not spiritual.
Analysis Plan
The data for this analysis comes from the baseline visit of the FACE clinical trial for adult PLWH. Descriptive statistics summarized demographic and clinical characteristics of patients only (not surrogates). The primary goal of this study is to apply the LCA (Clogg, 1995; Collins & Lanza, 2010; McCutcheon, 1987, Muthén, 2002) to identify unobserved latent classes/groups of patients living with HIV with respect to their religiousness/spirituality measures. The second goal was to assess the relationship of the latent class membership with sociodemographic characteristics and HRQoL, controlling for covariates.
We fit a series of LCA models with increasing number of latent classes and determined the optimal number of latent classes by comparing K-Class model with (K-1)-Class model iteratively. We used Bayesian Information Criterion (BIC), Akaike Information Criterion (AIC), Lo–Mendel–Rubin likelihood ratio (LMR LR), the adjusted LMR LR (ALMR LR) test, and the bootstrap likelihood ratio test (BLRT) for model comparisons. Once the number of latent classes was identified, we classified individuals into their most likely latent classes on the basis of their most likely latent class membership. We assessed the quality of class membership classification via classification probabilities for the most likely latent class membership and the entropy statistic. Next, we classified individuals into appropriate latent classes based on their largest posterior probabilities. We assessed the prevalence rates of the latent classes and the conditional response probabilities of stronger religiousness/spirituality belief measures in each latent class. We defined the classes based on the conditional probabilities of the religiousness/spirituality measures in each class.
Finally, we examined the relationships of the latent class membership with HRQoL and demographic characteristics. To take into account the often inevitable measurement errors in the estimated latent class membership, we applied the 3-step approach (Vermunt, 2010; Asparouhov & Muthén, 2012) to examine the relationships of the latent class membership with the HRQoL and demographics using Mplus 8.2.
Results
Demographics
Although the FACE clinical trial was a dyadic study, for this specific analysis we analyzed results from patients only to assess religious/spiritual aspects of adult PLWH. Surrogate data is not included in this analysis. Patients (N = 223) were 56.1% male, 86.1% Black/African American, aged 22–77 (Mean = 50.83, SD = +/− 12.33). Most patients said their religious affiliation was Christian (N = 168, 75.3%), with 2.2% (N = 5) specifically stating an African Christian affiliation, 29.6% (N = 66) a Baptist affiliation and 7.6% (N = 17) a Catholic affiliation. Additional participant demographics are reported in Table 1.
Table 1.
Patient Demographics (N=223)
| Variable | N (%) |
|---|---|
| Patient Gender | |
| Male | 125 (56.1) |
| Female | 94 (42.2) |
| Transgender | 4 (1.8) |
| Patient Race | |
| Non-Black | 25 (11.2) |
| Black | 192 (86.1) |
| Declined | 6 (2.7) |
| Patient Age | |
| Young Adult (22–39) | 44 (19.7) |
| Adult (40–60) | 128 (57.4) |
| Oldest Adults (61–77) | 51 (22.9) |
| Marital Status | |
| Married or Living together | 60 (26.9) |
| Single, Separated, Divorced and Widowed | 163 (73.1) |
| Sexual Orientation | |
| Heterosexual | 148 (66.4) |
| Non-Heterosexual | 75 (33.6) |
| Patient Religion | |
| Agnostic | 2 (0.9) |
| Atheist | 3 (1.3) |
| Buddhist | 1 (0.5) |
| Muslim | 5 (2.2) |
| Jewish | 2 (0.9) |
| Religious, non-specific | 15 (6.7) |
| No religion | 11 (4.9) |
| Christiana | 168 (75.3) |
| African Christian | 5 (2.2) |
| Baptist | 66 (29.6) |
| Catholic | 17 (7.6) |
| Pentacostal | 8 (3.6) |
| Non-specific | 53 (23.8) |
| Spiritual, not religious | 7 (3.1) |
| Otherb | 6 (2.7) |
Other Christian religions included Adventist (N = 2), Apostolic (N = 2), Assembly of God (N = 1), Episcopalian (N = 2), Jehovah’s Witness (N = 3), Methodist (N = 4), Presbyterian (N = 1), and Protestant (N = 4)
Santa Maria, Wicca, Freedom, Holiness, IFA, PBTLDMT
Descriptive Statistics of HRQoL
In this sample, average POS and PHQ-9 scores were low, 7.1 (SD = +/− 5.8) and 3.9 (SD = +/− 4.6) respectively, indicating better health. The mean scores for all five MOS-HIV dimensions were between 57.7 – 80.6, indicating better health. See Table 2 for more details.
Latent Class Analysis
Model fit indices/statistics for different LCA models are shown in Table 3. Results show that this population is not homogeneous with respect to religiousness/spirituality. The single-class model has the largest information criterion indices and the p-values of all the statistical tests in the 2-class model are <0.05, indicating that the single-class model was rejected and a model with at least 2 latent classes is in favor. The 3-class model fits data better than the 2 or 4-class model because (1) its information criterion indices are smaller; (2) the LMR LR, ALMR LR, and BLRT tests are all statistically significant for rejecting the 2-class model; and (3) the LMR LR, ALMR LR, and BLRT tests are all statistically insignificant for the 4-class model, indicating that the 3-class model can’t be rejected. Thus, we favor the 3-Class model.
Table 3.
Latent Class Model Fit Comparison (N=223)
| Model | AIC | BIC | aBIC | LMR LR P-value | ALMRLR P-value | BLRT P-value |
|---|---|---|---|---|---|---|
| 1-Class | 1374.60 | 1391.63 | 1375.79 | - | - | - |
| 2-Class | 1242.73 | 1280.21 | 1245.35 | <0.0001 | <0.0001 | <0.0001 |
| 3-Class | 1211.48 | 1235.33 | 1213.15 | <0.0001 | <0.0001 | <0.0001 |
| 4-Class | 1234.40 | 1312.76 | 1239.87 | 0.1530 | 0.1632 | 0.2650 |
AIC: Akaike Information Criterion. BIC: Bayesian Information Criterion. aBIC: Adjusted BIC. LMR LR: Vuong-Lo-Mendell-Rubin Likelihood Ratio Test. ALMRLR: Lo-Mendell-Rubin Adjusted LMR Test. BLRT: Parametric Bootstrapped Likelihood Ratio Test. - : Not applicable.
The classification probabilities for the most likely latent class membership are shown in Table 4. that are all higher than the cutoff point of 0.70 (Nagin, 2005), indicating good quality of class classification.
Table 4.
Quality of classification: 3-Class LCA (N=223)
| Latent Class | Most Likely Latent Class Membership | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| 1 (N=78, 35.0%) | 0.963 | 0.037 | 0.000 |
| 2 (N=105, 47.1%) | 0.015 | 0.966 | 0.019 |
| 3 (N=40, 17.9%) | 0.000 | 0.015 | 0.985 |
| Entropy = 0.702 | |||
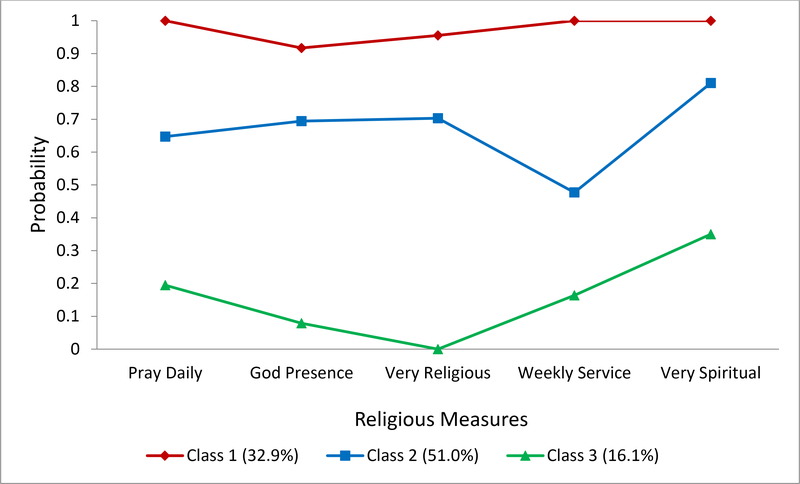
The class prevalence rates are also shown in Table 4: 35.0% (N = 78) of the sample were classified into Class 1, 47.1% (N = 105) into Class 2, and 17.9% (N = 40) into Class 3. The classes are defined based on the conditional response probabilities (see Figure 1). We define Class 1 as traditional: highest overall religiousness/spirituality because the conditional probabilities are very high for all the five religious/spiritual items (i.e., prayed daily, felt God’s presence, attended weekly religious services, and identified themselves as religious and spiritual).
Fig 1.
Patterns of religiousness and spirituality estimated from the 3-class LCA model.
Note. The classification of latent classes that Mplus uses for plotting is based on estimated posterior probabilities that is slightly different from that based on the most likely latent class membership.
Class 2 was defined as privately religious: religious experiences without attending services regularly. Patients in this class were less likely than those in Class 1 to pray daily, experience God’s presence, attend weekly religious services, or identify as religious or spiritual.
Class 3 was defined as spiritual but not religious because patients in this class were the least likely to report praying daily, were very unlikely to feel God’s presence or attend weekly religious, had 0.00 probability of identifying as religious but a 0.35 probability of identifying as spiritual.
Class Relationship Between Latent Class, Demographics and HRQoL
Examining the latent class membership by demographics, patients who were Black were more likely to be in Class 1 (OR = 10.55, 95% CI: 1.31 to 84.90) or Class 2 (OR = 5.55, 95% CI: 1.44 to 21.36) than in Class 3, meaning they were more likely to be traditionally or privately religious (Table 5). Adults and older adults ages 40–77 were also more likely to be in Class 1 (Table 5). There is no significant relationship of gender, marital status or sexual orientation with religious latent classes (Table 5).
Table 5.
Selected results of 3-step LCA model: Effects of demographics on latent class membership (N=217a)
| Demographic | Latent Class |
||
|---|---|---|---|
| Class 1 OR (95% CI) |
Class 2 OR (95% CI) |
Class 3 - |
|
| Race | - | ||
| Non-Black | - | - | - |
| Black | 10.55 (1.31, 84.90)* | 5.55 (1.44, 21.36)* | - |
| Age | - | ||
| Young Adult (22–39) | - | - | |
| Adult (40–60) | 6.43 (1.56, 26.47)* | 2.91 (0.95, 8.92) | - |
| Oldest Adults (61–77) | 11.16 (2.00, 62.24)* | 1.64 (0.31, 8.76) | - |
| Gender | |||
| Female, Transgender | - | - | - |
| Male | 0.30 (0.08, 1.19) | 1.70 (0.46, 6.26) | - |
| Marital Status | |||
| Single, Separated, Divorced, or Widowed | - | - | - |
| Married or Living together | 0.79 (0.23, 2.71) | 0.69 (0.22, 2.16) | - |
| Sexual Orientation | |||
| Non-Heterosexual | - | - | - |
| Heterosexual | 1.62 (0.38, 6.89) | 1.51 (0.40, 5.70) | - |
6 patients with declined race were excluded.
Reference group.
Odds ratio.
Significant level of 0.05.
The relationships of latent class membership with the HRQoL measures are shown in Table 6. MOS-HIV mental health (p < 0.001), MOS-HIV quality of life (p = 0.014) and MOS-HIV health transition (p = 0.016) scores significantly varied across the three latent religiousness/spirituality classes. POS total score, PHQ-9 total score, MOS-HIV general health perceptions and MOS-HIV health distress were not significantly correlated with the latent classes (Table 6). Compared to the other two groups, significantly higher levels of mental health, HRQoL and health transition (health improvement over the past four weeks) were found among patients who identified as traditionally religious (Class 1). Patients in Class 2, privately religious, had the lowest levels of mental health and HRQoL.
Discussion
This study explored religiousness and spirituality among PLWH and the effects on HRQoL. Three unobserved distinct latent classes were identified: Traditional- highest overall religiousness/spirituality (Class 1); Privately religious- identifies as religious, engages in religious activities at home but doesn’t attend service on a regular basis (Class 2); and Spiritual but not religious-more likely to identify as spiritual but not involved in organized religion, has the lowest overall religiousness/spirituality (Class 3).
The group comprising the highest overall religiousness/spirituality, Class 1, consisted of 35% of PLWH. They were more likely to attend weekly religious services, to pray daily, to feel God’s presence, and identify as religious and spiritual. Results suggest race plays a role in the likelihood of being traditionally religious, as Black patients were more likely to be in this group. This is relevant because the Black community faces health disparities that may be mitigated by incorporating or encouraging religion/spirituality as a part of treatment. Since religiousness/spirituality has been shown to improve emotional health and slow the progression of HIV, developing culturally-sensitive interventions for this population could improve treatment satisfaction and outcomes (Oji et al., 2017; Kremer & Ironson, 2014; Pargament et al., 2001; Tuck et al., 2001; Cotton et al., 2006; Ironson et al., 2006; Yi et al, 2006; Koenig, 2008; Koenig et al., 1998; Ironson et al., 2002; Lyon et al., 2014).
Results of this analysis also suggest older age plays a role in the likelihood of being traditionally religious (Class 1). Perhaps these individuals had more time to explore the meaning and purpose of life, create an established sense of identity and feel comfortable joining a religious community. Younger adults, ≤39 years, may still be forming their religious/spiritual identity and therefore less likely to be in Class 1. This theory is supported by previous work that found the youngest individuals had the lowest overall religiousness/spirituality (Cobb, Kor, & Miller, 2015).
47.1% of PLWH, Class 2, were privately religious. Despite not attending regular religious services, they often prayed privately, experienced God’s presence, and thought of themselves as somewhat religious and spiritual. Results suggest these individuals developed an internal, as opposed to external, locus of religious self-identity. They may be comfortable in their religion/spirituality and do not feel the need to join an organized community. Alternatively, these individuals may not feel accepted by religious communities. HIV-related stigma, defined by UNAIDS as a “social process of evaluation that reinforces negative thoughts about persons living with HIV and AIDS” is described as one of the greatest barriers to prevention and treatment (Piot, 2000; Brooks, Etzel, Hinojos, Henry, & Perez, 2005). There is still stigma regarding HIV, which includes negative beliefs such as “HIV is a punishment from God” and “God has abandoned me because of my HIV” (Kremer et al., 2015; Lee et al., 2014; Pargament et al., 2001; Lyon et al., 2011; Ironson et al., 2011; Fitchett et al., 2004). Perhaps individuals in Class 2 avoid social settings such as religious services as a way to avoid prejudice and discrimination (Brooks et al., 2005). This finding may also be related to sexuality. In particular, members of the LGBTQ community face further discrimination within their (religious) communities (Brooks et al., 2005). Future research should investigate if LGBTQ members living with HIV do not attend religious services due to fear of judgment and, if so, does minority sexual orientation play a role.
17.9% of PLWH were in Class 3, the lowest overall religiousness/spirituality. Although they did not attend religious services, pray privately, feel God’s presence, or consider themselves as religious, they sometimes identified as spiritual. This is consistent with previous findings that individuals who consider themselves spiritual are less likely to identify as religious (Saguil & Phelps, 2012; Astin et al., 2005; Walker et al., 2007; Koenig, 2018). Despite having feelings concerned with life’s meaning and purpose, this group was not associated with organized religion (Puchalski et al., 2009). This group had significantly higher levels of mental health and quality of life as compared to Class 2, suggesting there is a benefit to identifying as spiritual even if an individual is not traditionally religious and does not receive the social support associated with attendance at religious services.
Three of the seven dimensions of HRQoL that were assessed were significantly higher among Class 1, the traditionally religious group. The high level of religiousness/spirituality in Class 1 was associated with increased HRQoL, mental health and improvement of health status over the past month. This finding supports previous research that spirituality is associated with higher well-being, slowed disease progression and decreased anxiety (Oji et al., 2017; Kremer & Ironson, 2014; Pargament et al., 2001; Tuck et al., 2001; Cotton et al., 2006; Ironson et al., 2006; Yi et al., 2006; Koenig, 2008; Koenig et al., 1998; Lyon et al., 2014). Being committed to a religious group may provide social support, a firm sense of identity/community, and a way to cope with stressors (Saguil & Phelps, 2012; Folkman, 1997). Patients in Class 2, privately religious, had the lowest levels of mental health and quality of life. Previous research has demonstrated that low HRQoL is not due to being privately religious; instead because of their low HRQoL these patients have turned to religion to deal with challenges, derive meaning and hope (Koenig, 2018). The fact that these patients did not turn to organized religious communities could indicate that this group felt stigmatized by and isolated from (religious) communities.
The majority of patients in this study, 75.3% (N = 168) identified with some sect of Christianity. Future research may consider if latent class membership is determined by membership of a specific church or religion, such as Christianity vs. Judaism vs. Islam.
Earlier FACE research using a 4-latent class model found higher levels of emotional well-being, as measured by the Pediatric Quality of Life Inventory 4.0 (PedsQL) (Varni, Burwinkle, Seid, & Skarr, 2003), among young perinatally infected adolescents who attended religious services but did not pray privately, feel God’s presence, or identify as religious/spiritual (Lyon, Kimmel, Cheng, & Wang, 2016). This profile represented 11% of the sample. This adolescent subpopulation may represent a more secular, but compliant group who received the social support of attending services without necessarily accepting religious or spiritual beliefs. Adolescents may have attended religious services due to parental influence (Francis & Casson, 2019; Francis, Penny & Powell, 2018). There was no latent class with this profile in the adult sample, perhaps because adults are less likely to live at home and feel obligated to their parents to attend religious services (Francis et al., 2018). This developmental difference could explain why the adult sample had a 3-latent class model, because this ‘parental influence/attends religious services only’ latent class did not exist. Assuming the latent class structure is due to differing developmental stages, then it is possible the relationship between psychological outcomes and the latent classes may also be due to developmental differences. This may account for the finding that emotional well-being was not significantly related to any of the adult latent classes while it was related to the ‘parental influence/attends religious services only’ adolescent latent class. Additionally, it is possible that these findings are due to using different measures of emotional well-being. The Patient Health Questionnaire (PHQ-9) used in the adult sample assesses depression severity (Pratt, Lamson, Swanson, Lazorick, & Collier, 2012). The PedsQL used in the adolescent sample assesses physical, emotional, social and school functioning (Pratt et al., 2012). While depression has been shown to influence HRQoL in PLWH, depression and HRQoL are different psychological outcomes (Jia et al., 2004). Lastly, estimated class classification varies between populations because the distributions of responses to questions vary between the two samples.
Limitations and Future Research
Limitations of this study include a cross-sectional analysis, possible selection bias, information bias, confounding, and lack of generalizability beyond an urban population of primarily Black and African-American PLWH receiving HIV medical care in Washington, DC. Data for the study relied exclusively on self-report, collected in an outpatient hospital setting; therefore, scores may represent individual self-representational biases and also may be affected by measuring religiousness/spirituality in a secular setting.
A limitation of this study is that we do not know if the race effect of the LCA is specific to individual spirituality or an increased availability of social support via the church. Social support is beneficial to dealing with health issues (Holt-Lunstad, Smith, & Layton, 2010); perhaps if church attendance and social interactions play a more important role in the lives of Black participants than non-Black participants, this race difference may be due to a higher amount of social support than religious/spiritual beliefs. Furthermore, we did not ask participants if their churches or religious communities were LQBTQ-friendly.
We did not assess use of psychotherapy or social support outside of the church, which may have influenced health outcomes. Additionally, traits of introversion and extroversion as related to attendance of religious services was not addressed. Lastly, we do not have information about whether or not members of any latent classes were spiritual/religious before HIV diagnosis. Future researchers may consider studying changes in spiritual/religious beliefs overtime in relation to health status and illness progression or the relationship between positive/negative religious coping and latent class membership. Additionally, future research in this area could address spiritual/religious beliefs that are harmful to individual or public health, allowing for intervention in a culturally-sensitive manner (Hills et al., 2005). Yarhouse and Tan (2005) provide suggestions for addressing such conflicts, specifically when they relate to sexual identify. They identified possible interventions as follows: (1) Discussion about spiritual/religious beliefs in relation to the patient’s identity (LGBTQ, PLWH) to facilitate reflection within a safe therapeutic context; (2) Permission to explore negative emotions about God and acknowledgment that many people share this experience, to normalize their feelings and reduce shame; (3) Emphasize ways in which the religion promotes love and acceptance, in the context of individual or family therapy. Additionally, researchers and clinicians could capitalize on spiritual beliefs that improve health by incorporating them into current treatment programs, such as spiritual or religious prayer, meditation, reading of spiritual/religious texts, and attendance of community events (Saguil & Phelps, 2012; Yarhouse & Tan, 2005). Healthcare professionals must take care not to impose their individual beliefs on patients or let their beliefs influence their bed-side manner. As identified by Yarhouse and Tan (2005), a useful clinical approach is to learn about religious beliefs that may be impacting health, point out possible areas of tension between beliefs and other spiritual/religious values like love and acceptance, and further explore the topic within the therapeutic context if needed.
Conclusions
Latent class analysis of religiousness/spirituality identified three classes among PLWH. Compared to the other two groups, higher levels of emotional and physical well-being were found among patients who regularly attended religious services, prayed daily, felt God’s presence, and identified as religious and spiritual. These patients were more likely to be 40+ years and Black. The lowest levels of mental health and HRQoL were found among patients in the privately religious group, which comprised 47.1% of the sample. This group was more likely to be Black and potentially felt stigmatized by and ostracized from their religious communities.
Religion and spirituality affect attitudes and preferences for medical treatment and palliative care (Koenig et al., 2003; Mazanec & Tyler, 2003; Saguil & Phelps, 2012; Lyon et al., 2019). Spirituality may help PLWH address questions related to meaning and purpose, including life beyond death. Organized religion provides a sense of community and social support, so long as PLWH feel welcomed instead of stigmatized. Understanding how religiousness/spirituality influences HRQoL can help the medical community develop holistic, patient-centered and culturally-sensitive interventions that could improve outcomes for PLWH and potentially mitigate the impact of health disparities within the Black and LGBTQ communities.
Supplementary Material
Acknowledgments
Funding
This research is supported by the National Institute of Nursing Research at the National Institute of Health Award Number R01NR014-052-05; National Institute of Health National Center for Advancing Translational Sciences CTSI-CN UL1RR031988. This research has been facilitated by the services and resources provided by the District of Columbia Center for AIDS Research, an NIH funded program (AI117970), which is supported by the following NIH Co-Funding and participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, FIC, NIGMS, NIDDK, and OAR. These institutions were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. This content is solely the responsibility of the authors and do not necessarily represent the official views of the NINR or the NIH, CTSI-CN or DC-CFAR.
Conflicts of Interest and Source of Funding: This research is supported by the National Institute of Nursing Research at the National Institute of Health Award Number R01NR014-052-05; National Institute of Health National Center for Advancing Translational Sciences CTSI-CN UL1RR031988. These institutions were not involved in the present analysis, the interpretation of the data, the writing of the manuscript, or the decision to submit for publication. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Nursing Research (NINR) or the National Institutes of Health (NIH).
Our study sites were: Children’s National Hospital, MedStar Health Research Institute/Washington Hospital Center, MedStar Georgetown University Hospital, The George Washington Medical Faculty Associates and the Washington DC Veterans Affairs Medical Center/Institute for Clinical Research, Inc. There are no conflicts of interest to report. Data have not been published previously. We thank the study participants for their contributions to the success of this study.
Compliance with Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This research was approved by the IRB at Children’s National (coordinating center) and at all participating study sites. The Children’s National Medical Center IRB’s Federal Wide Assurance (FWA) number is FWA00004487. The institutional organization number is IORG0000245. Informed consent was obtained from all individual participants included in the study. The authors declare there are no conflicts of interest to report.
References
- Asparouhov T, & Muthén B (2012). Auxiliary variables in mixture modeling: A 3-step approach using Mplus. Mplus web notes: No. 15. [Google Scholar]
- Aspinal F, Hughes R, Higginson I, Chidgey J, Drescher U, & Thompson M (2002). A user’s guide to the Palliative care Outcome Scale. London: Palliative Care and Policy Publications, 10. [Google Scholar]
- Astin AW, Astin HS, Lindholm JA, & Bryant AN (2005). The spiritual life of college students: A national study of students’ search for meaning and purpose. Los Angeles, CA: Higher Education Research Institute, UCLA. [Google Scholar]
- Barton YA, & Miller L (2015). Spirituality and positive psychology go hand in hand: An investigation of multiple empirically derived profiles and related protective benefits. Journal of Religion and Health, 54(3), 829–843. [DOI] [PubMed] [Google Scholar]
- Bernstein K, D’Angelo LJ, & Lyon ME (2013). An exploratory study of HIV+ adolescents’ spirituality: will you pray with me?. Journal of Religion and Health, 52(4), 1253–1266. [DOI] [PubMed] [Google Scholar]
- Brooks RA, Etzel MA, Hinojos E, Henry CL, & Perez M (2005). Preventing HIV among Latino and African American gay and bisexual men in a context of HIV-related stigma, discrimination, and homophobia: perspectives of providers. AIDS Patient Care & STDs, 19(11), 737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron IM, Crawford JR, Lawton K, & Reid IC (2008). Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. British Journal of General Practice, 58(546), 32–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clogg CC (1995). Latent class models. In Arminger G, Clogg CC, & Sobel ME (Eds.), Handbook of statistical modeling for the social and behavioral sciences (pp. 311–359). New York: Plenum Press. [Google Scholar]
- Cobb E, Kor A, & Miller L (2015). Support for adolescent spirituality: Contributions of religious practice and trait mindfulness. Journal of Religion and Health, 54(3), 862–870. [DOI] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2010). Latent class and latent transition analysis: With applications in the social, behavioural, and health sciences. New York: Wiley. [Google Scholar]
- Cotton S, Puchalski CM, Sherman SN, Mrus JM, Peterman AH, & Feinberg J (2006). Spirituality and religion in patients with HIV/AIDS. Journal of General Internal Medicine, 21(5), S5–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, McGrady ME, & Rosenthal SL (2010). Measurement of religiosity/ spirituality in adolescent health outcomes research: Trends and recommendations. Journal of Religion and Health, 49(4), 414–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalmida SG, Koenig HG, Holstad MM, & Thomas TL (2015). Religious and psychosocial covariates of health-related quality of life in people living with HIV/aids. HIV/aids Research and Treatment: Open Journal [Internet], 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doolittle BR, Justice AC, & Fiellin DA (2018). Religion, spirituality, and HIV clinical outcomes: a systematic review of the literature. AIDS and Behavior, 22(6), 1792–1801. [DOI] [PubMed] [Google Scholar]
- Edwards A, Pang N, Shiu V, & Chan C (2010). The understanding of spirituality and the potential role of spiritual care in end-of-life and palliative care: a meta-study of qualitative research. Palliative Medicine, 24(8), 753–770. [DOI] [PubMed] [Google Scholar]
- Fetzer Institute. (1999). National Institute on Aging Working Group. Multidimensional measurement of religiousness, spirituality for use in health research. A report of the national working group. MI: Fetzer Institute, 2003. [Google Scholar]
- Fitchett G, Murphy PE, Kim J, Gibbons JL, Cameron JR, & Davis JA (2004). Religious struggle: Prevalence, correlates and mental health risks in diabetic, congestive heart failure, and oncology patients. The International Journal of Psychiatry in Medicine, 34(2), 179–196. [DOI] [PubMed] [Google Scholar]
- Folkman S (1997). Positive psychological states and coping with severe stress. Social Science & Medicine, 45(8), 1207–1221. [DOI] [PubMed] [Google Scholar]
- Francis L, Penny J, G., & Powell R (2018). Assessing peer and parental influence on the religious attitudes and attendance of young churchgoers: Exploring the Australian National Church Life Survey. Journal of Beliefs & Values, 39(1), 57–72. [Google Scholar]
- Francis LJ, & Casson A (2019). Retaining young catholics in the church: assessing the importance of parental example. Journal of Religious Education, 67(1), 1–16. [Google Scholar]
- Harris SS, Holder DW, Kulig J, Schrier LA, & Knight JR (2007). Reliability and validity of the brief multidimensional measure of religiousness/spirituality among adolescents. Journal of Religion and Health, 47(4), 438–457. [DOI] [PubMed] [Google Scholar]
- Hearn J, & Higginson IJ (1999). Development and validation of a core outcome measure for palliative care: the Palliative care Outcome Scale. Palliative Care Core Audit Project Advisory Group. British Medical Journal of Quality & Safety, 8(4), 219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson WA, Schlenk EA, Kim KH, Hadigan CM, Martino AC, & Sereika SM(2010). Validation of the MOS-HIV as a measure of health-related quality of life in persons living with HIV and liver disease. AIDS Care, 22(4), 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PC, & Pargament KI (2003). Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. American Psychologist, 58, 64–74 [DOI] [PubMed] [Google Scholar]
- Hills J, Paice JA, Cameron JR, & Shott S (2005). Spirituality and distress in palliative care consultation. Journal of Palliative Medicine, 8(4), 782–788. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: a meta-analytic review. PLoS medicine, 7(7), e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ironson G, Solomon GF, Balbin EG, O’cleirigh C, George A, Kumar M, & Woods TE (2002). The Ironson-Woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine, 24(1), 34–48. [DOI] [PubMed] [Google Scholar]
- Ironson G, Stuetzle R, & Fletcher MA (2006). An increase in religiousness/spirituality occurs after HIV diagnosis and predicts slower disease progression over 4 years in people with HIV. Journal of General Internal Medicine, 21(5), S62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ironson G, Stuetzle R, Ironson D, Balbin E, Kremer H, George A, & Fletcher MA (2011). View of God as benevolent and forgiving or punishing and judgmental predicts HIV disease progression. Journal of Behavioral Medicine, 34(6), 414–425. [DOI] [PubMed] [Google Scholar]
- Ironson G, Kremer H, & Lucette A (2016). Relationship between spiritual coping and survival in patients with HIV. Journal of General Internal Medicine, 31(9), 1068–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia H, Uphold CR, Wu S, Reid K, Findley K, & Duncan PW (2004). Health-related quality of life among men with HIV infection: effects of social support, coping, and depression. AIDS Patient Care & STDs, 18(10), 594–603. [DOI] [PubMed] [Google Scholar]
- Kimmel AL, Wang J, Scott R, Briggs L, Lyon ME (2015). FAmily CEntered (FACE) advance care planning: study design and methods for a patient-centered communication and decision-making intervention for patients with HIV/AIDS and their surrogate decision-makers. Contemporary Clinical Trials, 43(1), 172–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DE, & Bushwick B (1994). Beliefs and attitudes of hospital inpatients about faith healing and prayer. Journal of Family Practice, 39(4), 349–352. [PubMed] [Google Scholar]
- Koenig HG, Pargament KI, & Nielsen J (1998). Religious coping and health status in medically ill hospitalized older adults. The Journal of Nervous and Mental Disease, 186(9), 513–521. [DOI] [PubMed] [Google Scholar]
- Koenig BA, Davies E. Cultural dimensions of care at life’s end for children and their families. In: Field MJ, & Behrman RE (2003). Cultural dimensions of care at life’s end for children and their families. In When children die: Improving palliative and end-of-life care for children and their families. National Academies Press (US).: pp. D1–D41. [PubMed] [Google Scholar]
- Koenig HG (2008). Concerns about measuring “spirituality” in research. The Journal of Nervous and Mental Disease, 196(5), 349–355. [DOI] [PubMed] [Google Scholar]
- Koenig HG (2018). Religion and mental health: Research and Clinical Applications. San Diego, Ca: Academic Press (Elsevier). [Google Scholar]
- Kremer H, & Ironson G (2014). Longitudinal spiritual coping with trauma in people with HIV: Implications for health care. AIDS Patient Care and STDS, 28(3), 144–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer H, Ironson G, Kaplan L, Stuetzele R, Baker N, & Fletcher MA (2015). Spiritual coping predicts CD4-cell preservation and undetectable viral load over four years. AIDS Care, 27(1), 71–79. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ‐9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M, Nezu AM, & Nezu CM (2014). Positive and negative religious coping, depressive symptoms, and quality of life in people with HIV. Journal of Behavioral Medicine, 37(5), 921–930. [DOI] [PubMed] [Google Scholar]
- Lyon ME, Garvie PA, Kao E, Briggs L, He J, et al. (2011). Spirituality in HIV-infected adolescents and their families: FAmily CEntered (FACE) advance care planning and medication adherence. Journal of Adolescent Health, 48(6), 633–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon ME, Garvie PA, He J, Malow R, McCarter R, & D’Angelo L (2014). Spiritual well-being among HIV-infected adolescents and their families. Journal of Religion and Health, 53(3), 637–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon ME, Kimmel AL, Cheng YI, & Wang J (2016). The role of religiousness/spirituality in health-related quality of life among adolescents with HIV: a latent profile analysis. Journal of Religion and Health, 55(5), 1688–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon ME, D’Angelo LJ, Cheng YI, Dallas RH, Garvie PA, Wang J (2019). The influence of religious beliefs and practices on health care decision-making among HIV positive adolescents. AIDS Care. DOI: 10.1080/09540121.2019.1668523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean CD, Susi B, Phifer N, Schultz L, Bynum D, Franco M, & Cykert S (2003). Patient preference for physician discussion and practice of spirituality: Results from a multicenter patient survey. Journal of General Internal Medicine, 18(1), 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters KS, Carey KB, Maisto SA, Caldwell PE, Wolfe TV, & Hackney HL (2009). Psychometric examination of the brief multidimensional measure of religiousness/spirituality among college students. The International Journal for the Psychology of Religion, 19(2), 106–120. [Google Scholar]
- Mazanec P, & Tyler MK (2003). Cultural Considerations in End-of-Life Care: How ethnicity, age, and spirituality affect decisions when death is imminent. The American Journal of Nursing, 103(3), 50–58. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL (1987). Latent class analysis. Quantitative applications in the social sciences series no. 64. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Muthén B (2002). Beyond SEM: General latent variable modeling. Behaviormetrika, 29,(1), 81–117. [Google Scholar]
- Muthén LK, & Muthén BO (1998–2012). Mplus user’s guide (6th edn.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nagin DS (2005). Group-based modeling of development. London: Harvard University Press. [Google Scholar]
- Oji VU, Hung LC, Abbasgholizadeh R, Hamilton FT, Essien EJ, & Nwulia E (2017). Spiritual care may impact mental health and medication adherence in HIV+ populations. HIV/AIDS (Auckland, NZ), 9, 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N, & Hahn J (2001). Religious struggle as a predictor of mortality among medically ill elderly patients: A 2-year longitudinal study. Archives of Internal Medicine, 161(15), 1881–1885. [DOI] [PubMed] [Google Scholar]
- Pearce LD, Foster EM, & Hardie JH (2013). A person‐centered examination of adolescent religiosity using latent class analysis. Journal for the Scientific Study of Religion, 52(1), 57–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piot P (2000). Report by the Executive Director. Programme Coordinating Board. Joint United Nations Program on AIDS. Rio de Janeiro: UNAIDS, 14–15. [Google Scholar]
- Pratt KJ, Lamson AL, Swanson MS, Lazorick S, & Collier DN (2012). The importance of assessing for depression with HRQOL in treatment seeking obese youth and their caregivers. Quality of Life Research, 21(8), 1367–1377. [DOI] [PubMed] [Google Scholar]
- Puchalski C, Ferrell B, Virani R, Otis-Green S, Baird P, Bull J, & Pugliese K (2009). Improving the quality of spiritual care as a dimension of palliative care: the report of the Consensus Conference. Journal of Palliative Medicine, 12(10), 885–904. [DOI] [PubMed] [Google Scholar]
- Revicki DA, Sorensen S, & Wu AW (1998). Reliability and validity of physical and mental health summary scores from the Medical Outcomes Study HIV Health Survey. Medical Care, (S), 126–137. [DOI] [PubMed] [Google Scholar]
- Saguil A, & Phelps K (2012). The spiritual assessment. American Family Physician, 86(6), 546. [PubMed] [Google Scholar]
- Simoni JM, Safren SA, Manhart LE, Lyda K, Grossman CI, Rao D, & DiClemente R (2011). Challenges in addressing depression in HIV research: assessment, cultural context, and methods. AIDS and Behavior, 15(2), 376–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ, & Kutner JS (2017). Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. Journal of Pain and Symptom Management, 53(5), 821–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N, Dear BF, McMillan D, Anderson T, Zou J, & Sunderland M (2011). Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cognitive Behaviour Therapy, 40(2), 126–136. [DOI] [PubMed] [Google Scholar]
- Trevino KM, Pargament KI, Cotton S, Leonard AC, Hahn J, Caprini-Faigin CA, & Tsevat J (2010). Religious coping and physiological, psychological, social, and spiritual outcomes in patients with HIV/AIDS: Cross-sectional and longitudinal findings. AIDS and Behavior, 14(2), 379–389. [DOI] [PubMed] [Google Scholar]
- Tuck I, McCain NL, & Elswick RK Jr (2001). Spirituality and psychosocial factors in persons living with HIV. Journal of Advanced Nursing, 33(6), 776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Seid M, & Skarr D (2003). The PedsQL™* 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambulatory Pediatrics, 3(6), 329–341. [DOI] [PubMed] [Google Scholar]
- Vermunt JK (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18(4), 450–469. [Google Scholar]
- Walker C, Ainette MG, Wills TA, & Mendoza D (2007). Religiosity and substance use: Test of an indirect-effect model in early and middle adolescence. Psychology of Addictive Behaviors, 21(1), 84–96. [DOI] [PubMed] [Google Scholar]
- Wasner M, Longaker C, Fegg MJ, & Borasio GD (2005). Effects of spiritual care training for palliative care professionals. Palliative Medicine, 19(2), 99–104. [DOI] [PubMed] [Google Scholar]
- Wu AW, Rubin HR, Mathews WC, Ware JE Jr, Brysk LT, Hardy WD, & Richman DD (1991). A health status questionnaire using 30 items from the Medical Outcomes Study. Medical Care, (S), 786–798. [DOI] [PubMed] [Google Scholar]
- Wu AW, Revicki DA, Jacobson D, & Malitz FE (1997). Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV). Quality of Life Research Journal, 6(6), 481–493. [DOI] [PubMed] [Google Scholar]
- Yarhouse MA, & Tan ES (2005). Addressing Religious Conflicts in Adolescents Who Experience Sexual Identity Confusion. Professional Psychology: Research and Practice, 36(5), 530. [Google Scholar]
- Yi MS, Mrus JM, Wade TJ, Ho ML, Hornung RW, Cotton S, & Tsevat J (2006). Religion, spirituality, and depressive symptoms in patients with HIV/AIDS. Journal of General Internal Medicine, 21(5), S21–S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.