Abstract
Abstract
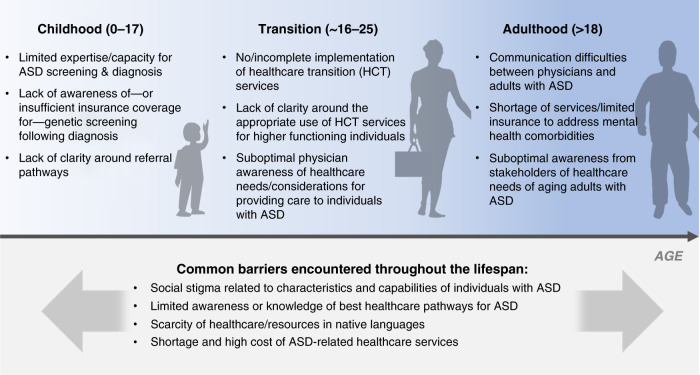
Most individuals with autism spectrum disorder (ASD)—a complex, life-long developmental disorder—do not have access to the care required to address their diverse health needs. Here, we review: (1) common barriers to healthcare access (shortage/cost of services; physician awareness; stigma); (2) barriers encountered primarily during childhood (limited screening/diagnosis; unclear referral pathways), transition to adulthood (insufficient healthcare transition services; suboptimal physician awareness of healthcare needs) and adulthood (shortage of services/limited insurance; communication difficulties with physicians; limited awareness of healthcare needs of aging adults); and (3) advances in research/program development for better healthcare access. A robust understanding of barriers to accessing healthcare across the lifespan of autistic individuals is critical to ensuring the best use of healthcare resources to improve social, physical, and mental health outcomes. Stakeholders must strengthen healthcare service provision by coming together to: better understand healthcare needs of underserved populations; strengthen medical training on care of autistic individuals; increase public awareness of ASD; promote research into/uptake of tools for ASD screening, diagnosis, and treatment; understand specific healthcare needs of autistic individuals in lower resource countries; and conduct longitudinal studies to understand the lifetime health, social, and economic impacts of ASD and enable the evaluation of novel approaches to increasing healthcare access.
Impact
Despite the growing body of evidence, our understanding of barriers to healthcare encountered by individuals with ASD remains limited, particularly beyond childhood and in lower resource countries.
We describe current and emerging barriers to healthcare access encountered by individuals with ASD across the lifespan.
We recommend that stakeholders develop evidence-informed policies, programs, and technologies that address barriers to healthcare access for individuals with ASD and consider broad, equitable implementation to maximize impact.
Introduction
Autism spectrum disorder (ASD, autism) is a complex, life-long disorder characterized by two core symptoms, which range in severity: persistent deficits in social communication and social interaction, and restricted and repetitive patterns of behaviors.1 ASD affects ~1 in 160 children globally2 and contributes to significant social (quality of life) and economic impacts (lifetime cost USD1.4 million and GBP0.80 million) that increase with ASD symptom severity.3–5
Autism is associated with a wide range of co-occurring developmental, mental, and physical health conditions, including intellectual disability (ID), epilepsy, attention-deficit hyperactivity disorder (ADHD), anxiety, depression, behavioral disturbances and tics, abnormal sleep patterns, motor difficulties, eating and elimination disorders, diabetes, hypertension, obesity, and cardiovascular disease.6–8 Each individual with autism has a unique life experience with different onset, combinations, severities, and persistence of ASD symptoms and co-occurring conditions. Accordingly, there is no one-size-fits-all healthcare approach, and healthcare must be agile, responsive, and, above all, accessible.
Despite the growing body of evidence, our understanding of barriers to healthcare encountered by autistic individuals remains limited, particularly beyond childhood and outside of higher resource countries (HRCs). In this review, we present an integrated understanding of healthcare needs and barriers encountered in HRCs, highlight gaps in our knowledge, and uncover important steps that stakeholders can take to improve healthcare service provision and enhance healthcare access for all individuals with ASD.
Methodology
This review is based on an extensive search of scholarly/peer-reviewed and gray literature. Our search of scholarly/peer-reviewed literature was carried out in PubMed using MeSH terms for autism keywords (e.g., autism spectrum disorder, autism, Asperger syndrome), socioeconomic impact (e.g., burden, caregiver, carer, socioeconomic), and access to healthcare (e.g., access, barriers, inequality, disparity). Gray literature was identified by reviewing publications covering socioeconomic impacts of ASD and barriers to healthcare access for autistic individuals released by organizations such as national ministries of health/public health agencies and autism-focused non-governmental organizations. Relevant articles referenced in publications identified from our search were also reviewed. We retrieved 1509 publications and assessed titles and abstracts/summaries to prioritize 248 publications for deeper review. Our search focused on literature published in or after 2010.
Common barriers to accessing medical care
A review of the literature helps characterize common barriers encountered across the lifespan, how they reduce access to care, existing solutions that address barriers and gaps in our understanding of their impact on long-term health, and social or economic outcomes.
Shortage of healthcare services
Families living outside metropolitan areas have less access to care for ASD than those in urban areas, often due to a shortage of specialists.9,10 In the USA, the number of child and adolescent psychiatrists per 100,000 ranges from 5 in Idaho (many rural communities) to 60 in the District of Columbia (densely populated).11 Similarly, the number of developmental-behavioral pediatricians per 100,000 children is 0.2 in Idaho and 4 in the District of Columbia.12 This results in a service supply shortage, clinician burnout, and long wait times for diagnosis and treatment.13 Families that do not have access to care in their community are less likely to seek care due to the additional cost, time commitment and disruption to daily obligations (e.g., work) associated with long-distance travel.14–16 Tools such as the Extension for Community Healthcare Outcomes (ECHO) Autism Screening Tool for Autism in Toddlers and Young Children (STAT) that connects local physicians to a hub of autism experts are increasing the capacity to screen, diagnose, and treat autism in rural communities; however, additional research is needed to optimize the accuracy of diagnosis using telemedicine and videoconferencing.17,18
Physician knowledge
Delivering the best care to autistic individuals critically depends on physician knowledge and training. Unfortunately, many individuals with ASD, their families, and even physicians have reported that physicians can lack specialized knowledge required to screen, diagnose, and refer individuals with ASD.14,19,20 Further, US medical students have reported not receiving sufficient training on treating autistic children, while those from the UK reported low confidence in their ability to manage care and referral of children and adults with ASD.21,22 Autistic individuals and their caregivers also see a need for physicians to have a better understanding of how to support individuals with severe ASD symptoms, facilitate more effective communication, and accommodate sensory challenges.15,23–27 Initiatives that improve physician awareness in screening and diagnosis of young children show promise, including the ECHO Autism STAT program (described above), which has been implemented in the USA, Canada, Uruguay, Kenya, India, and Vietnam, resulting in patients accessing services 2–6 months sooner.17,28 In addition, AASPIRE’s Autism Healthcare Accommodations Tool—a customized communication and sensory accommodations report builder—has decreased the number of barriers to care faced by autistic adults by 30%, and improved healthcare provider self-efficacy and patient–provider communication.29
Cost of services: the US example
Consistent with the use of a wide range of healthcare services across the lifespan, the cost of healthcare for individuals with ASD is very high. In the USA, annual healthcare costs for autistic individuals increase with age from USD6467 (age 0–5 years) to USD9053 (age 6–17 years) to USD13,580 (age 18+ years) and are significantly higher for individuals with co-occurring ID.3 The amount of out-of-pocket healthcare expenditures also depends on individual health insurance coverage and household income. Indeed, recommended ASD services are often excluded from insurance plans held by families with lower socioeconomic status (SES).30 In recent years, as all 50 US states mandated private health insurance companies to cover diagnostic and treatment services for ASD, healthcare service utilization has increased, suggesting that insurance coverage addresses, at least in part, the financial barrier to accessing healthcare.31,32
Family and individual knowledge
When individuals with ASD and their families know the signs and symptoms of ASD and available care options, they are more likely to alert care providers to a developmental delay and/or advocate for healthcare services. However, building this knowledge can be influenced by situational and social factors. For example, first-time parents are less likely to detect developmental delays than experienced parents who are often more familiar with typical developmental milestones.33 Reduced awareness of ASD and related services is more common in groups with lower SES, less education, and limited access to health professionals (e.g., those living in rural areas).9 The World Health Organization (WHO) has developed and implemented Caregiver Skill Training (CST) programs in over 30 countries, which boosts family awareness of ASD needs and services in local contexts.34,35
Language
Language barriers also hinder access to and navigation of healthcare services for ASD. In Canada, the USA, and the UK, parents of children with ASD, for whom English is not the first language, encountered language barriers when accessing health services, communicating with their physicians, and interpreting/responding to administrative forms.36–38 Recognizing this shortcoming, several organizations, such as Autism Speaks and the University of Southern California, Center for Excellence in Developmental Disabilities, have translated key resources describing the signs of autism, outlining steps to take when signs are detected, and summarizing support available to families into multiple languages.39,40
Stigma
As with many mental health disorders, stigma can contribute to feelings of rejection and isolation among parents of autistic children and can prevent individuals with ASD from engaging with the healthcare system at all stages of life.20,41,42 While stigma is a reality for most families affected by ASD, its impacts on access to diagnosis and treatment services are exacerbated for many racial/ethnic minorities (including immigrants).36,38 Studies from Canada, UK, and the USA have determined that immigrant parents from some cultures do not acknowledge that their children have developmental disabilities because of the associated stigma.36,38 Advocacy and research groups have launched initiatives that have reduced stigma around ASD. For example, Sesame Workshop worked with over 13 autism-related organizations to introduce a Muppet with autism to the television show and digital resources. Sesame Workshop has received global praise for the depiction of a child with ASD and for increasing knowledge, acceptance, and inclusion of autistic children.43,44
Childhood (0–17 years of age)
One of the greatest healthcare needs for children with ASD is securing an accurate clinical diagnosis of ASD and any comorbid conditions. Diagnoses enable primary care practitioners (PCPs) to initiate an individualized cascade of care—including educational, therapeutic, medical, genetic counseling, and family support services—which is recommended by many professional associations.45–49 While this cascade is well defined, many of the barriers to healthcare (described above) can be exacerbated at this stage of life by a number of factors—which can intersect and interact in unique ways for each individual:
Symptom severity: ASD is a spectrum disorder and individuals experience diverse symptoms that can range from mild to severe. This heterogeneity can make it difficult for physicians to consistently identify early signs of developmental delays and/or ASD in children.50 Less severe ASD symptoms are often not detected by clinicians until later in life.51
Comorbid health conditions: autistic individuals often have comorbid health conditions that can be conflated with ASD symptoms, complicating or delaying diagnosis.52 In addition, comorbid health conditions are managed within the healthcare system, while developmental disabilities (including ASD) are typically supported within the social services and education systems, making it difficult to integrate care.53
Differing expression of ASD symptoms: ASD symptoms can be expressed in different ways. For example, females—who often have a different clinical presentation of ASD than males—are commonly diagnosed later in life despite typically being assessed for developmental delays at the same age as boys.54,55
Parents of children with ASD report first having concerns about their child’s development as early as 12–18 months of age and some clinicians are able to diagnose ASD as early as 14 months;56,57 however, diagnosis typically occurs later in Europe (3.5 years), USA (4 years), and Canada (6 years), exposing an opportunity to decrease the age at diagnosis and accelerate access to specialized healthcare.58–60 Early diagnosis and treatment have been linked to greater reduction in the core symptoms of ASD, higher likelihood of receiving behavioral therapy, and a reduction in the use of psychotropic medication.61–63 Yet, little is known about how it can contribute to higher quality of life over time or to better long-term health outcomes such as life expectancy and severity of comorbid conditions.
Several professional associations recommend that diagnosis of ASD should be followed by genetic (including mitochondrial disorders) and metabolic screening to identify syndromes (e.g., Fragile X) or potentially treatable neurometabolic causes of ASD.64–66 This screening can potentially uncover a unifying cause for symptoms of ASD and some comorbid health conditions (e.g., ID, epilepsy), rule out certain mental health disorders, and support physicians in making evidence-based referrals. Despite these recommendations, limited insurance coverage or lack of information regarding the availability and benefits of genetic and metabolic screening prevent some families from accessing this service.67
Transition to adulthood (~16–25 years of age)
Every year, over 50,000 youth with ASD enter adulthood in the USA.68 A smooth and timely transition from a pediatric to an adult PCP is critically important to young adults with ASD having the medical support they need at a time when both the incidence and severity of many mental and physical health comorbidities increase.69–71 However, autistic youth transitioning to adulthood are often reluctant to seek support for their mental health due to social stigma and uncertainty around where to go for care, often leading to the worsening of symptoms.72
Health systems in HRCs have established and implemented healthcare transition (HCT) services to foster continuity between pediatric and adult care. However, HCT services have been difficult to scale—one study found that only one-fifth of autistic youth received HCT services—and many youths with ASD face challenges accessing healthcare.73,74 This may partly explain why scheduled outpatient and inpatient visits decline with age for autistic youth, especially for those with a co-occurring ID75 and why the use of emergency services increases.69,70 A Canadian study reported that 70% of pediatricians did not support youth with ASD in the transition to adult healthcare services and another study found that >50% of families lacked information on the HCT process.19,76 Physicians may feel that HCT services are better suited to lower-functioning autistic individuals and may not be clear on how to include individuals with moderate or mild ASD symptoms in the transition process, underscoring the opportunity to tailor HCT services to the unique needs of individuals with ASD. Further, multiple studies found that there is a lack of adult care physicians who have specialized understanding of the medical, behavioral, and social needs of individuals with ASD during transition.19,77 Topics that could be better addressed during physician training to foster more effective relationships and communication between the patient and provider include sensory sensitivities, value of routine experience, and benefits of preparing autistic adults in advance of appointments.78 A recent adaptation of ECHO, known as ECHO Autism Transition, was successfully piloted to train PCPs on improving self-efficacy in caring for autistic individuals as they transition to adulthood.79
Adulthood (>18 years of age)
As the rate of childhood diagnosis increases, the number of aging individuals with ASD will continue to rise. Based on a recent statistical model using data from the National Study of Children’s Health, 2.2% of US adults are estimated to have ASD.80 Autistic adults encounter many health issues including mental health difficulties (e.g., associated with social disengagement, loneliness, depression, and anxiety) and physical health conditions (e.g., obesity, heart disease).81,82 Adults with ASD also have an increased risk of premature mortality compared to the general population (mean age of mortality: 54 vs 70 years), especially for those who are low functioning (mean age of mortality: 40 years).83 While research on interventions to improve health outcomes in autistic adults is emerging,84 limited research on healthcare barriers indicates that health services, funding, and physician training are not yet meeting the needs of this population.85,86
Long waitlists and lack of funding are major barriers to treatment and support for autistic adults in the UK, forcing many to pay for treatment themselves.87 While in the USA, autistic adults are often unable to find care that addresses developmental delay together with mental health issues and frequently lack the personal funds or insurance coverage to cover the cost of care.88 In fact, adults with ASD, who request help for anxiety or depression and mention their ASD, are often “punted” to a provider with experience in developmental delays who may not have expertise in mental healthcare (or vice versa). Similar to other life stages, both physicians and autistic adults have reported an opportunity to enhance the training of physicians89,90 and caregivers in long-term or residential care facilities.86 Notably, many autistic adults and their families feel that healthcare providers have misconceptions about individuals with autism and commonly over-attribute behaviors to autism instead of looking for a separate illness first.20 Adults with autism also have significantly lower satisfaction scores on patient–provider communication scales.91 Poor communication and common misconceptions (e.g., adults with ASD are not sexually active) may also lead to key health procedures—such as Pap smears or other reproductive health procedures—being overlooked.91,92
There is a need to gather more data on the specific medical needs and barriers to accessing healthcare among adults with ASD to better support this growing population. Notably, little is known about the effects of co-existing psychiatric conditions, long-term pharmacological treatment of comorbidities, and how cognitive decline and dementia affect autistic adults.93 Adult care physicians should also continue to monitor symptoms of ASD—which can intensify and diminish—to guide diagnoses and treatment choices.
Accessing healthcare in lower resource countries
The majority of autistic individuals in lower resource countries (LRCs) do not have access to the healthcare necessary to support their medical needs, and experience many of the barriers described above, especially lack of services, high costs, shortage of physician knowledge, and stigma.94–97 Yet, most of the studies on barriers to healthcare faced by individuals with ASD have been conducted in HRCs. Of the few studies on barriers to healthcare that have been conducted in LRCs, most focus on children, making it difficult to identify regionally relevant approaches to improving access to care for adults.
Effective community-delivered programs have been implemented in many LRCs to increase access to care. These include the WHO-led CST programs (described above), which are active in several LRCs, including the Philippines, Ethiopia, and China,34,35,98 and PASS Plus, a program delivered in rural India, which integrates support for autism comorbidities.99 These initiatives could be modified and adapted to an online delivery format to train families in LRCs on the medical needs of autistic individuals and provide information on navigating local healthcare systems.
The future of ASD screening, diagnosis, and treatment
Determining the etiology of ASD through genetic screening is part of standard clinical practice in many HRCs (see also section “Common barriers to accessing medical care”). While the heritability of ASD has been estimated to be ~80%, only 10–36% of autistic individuals have an identifiable genetic etiology.100–102 Whole-exome sequencing detected etiologic genetic/neurometabolic causes of ID (with or without autism) in 68% of patients tested and has been used to inform tailored and cost-effective medical treatments (e.g., nutritional manipulation) beyond genetic counseling for 44% of patients.103 Similarly, several genetic syndromes associated with ASD have specific co-occurring medical conditions with treatment implications104 or that require ongoing surveillance,105 such as cancer surveillance in individuals with ASD who have germline heterozygous PTEN mutations.106 This points to an opportunity to continue to identify and characterize underlying genomic profiles of ASD (and associated comorbidities) with the potential to personalize ongoing treatment plans.
Complementing smaller-scale research studies, Individualized Treatments for Autism Response using Genetic-Environment Targets (iTARGET; Canada) and the Research Domain Criteria (RDoC; USA) help to determine how genetic and neurobiological profiles can define autism subtypes and inform personalized care for individuals based on both causes and symptoms.107,108 While advances in ASD screening have the potential to improve diagnosis and care, they also have the potential to increase the disparity in care between higher and lower resource settings. Further, in the USA, despite recommendations, disadvantaged groups have less access to genetic testing and counseling, and in Canada’s government-regulated health system, block funding for autistic children is based on the diagnostic label (not the need), and omits funding for testing/counseling for cause, anticipatory needs, or optimized treatments.67,109 As new screening, diagnostic and treatment approaches are developed, all stakeholders, including policymakers, must work together to limit barriers and foster the best possible outcomes for all individuals affected by ASD.
Discussion and recommendations
This review offers a unique contribution to the literature through an integrative review of barriers to healthcare experienced by individuals with autism across the lifespan within the context of healthcare service provision. Recent reviews have been published with a focus on barriers experienced by autistic individuals and their carers when accessing healthcare.26,27 The findings from this review reinforce those brought forward in these studies, including the need to improve physician knowledge and better adapt care environments to sensory sensitivities, while other themes such as challenges experienced by individuals with autism when communicating healthcare needs to providers were not as prominent in our study. Bradshaw et al.25 identify unique healthcare needs among adults with autism that can be improved in the context of healthcare service provision. Our study determines that many of the same barriers are encountered at other life stages, including those related to SES (cost of service, individual/family knowledge), insufficient physician training, and lack of clear referral pathways.25 Nicolaidis et al.20 assessed the healthcare experiences of autistic adults and determined that factors at the patient, provider, and system levels impact the quality of a healthcare experience. Our findings support those of Nicoladis et al., in adulthood, and also determine that the same factors are at play during childhood and the transition to adulthood. We build on the existing body of work by identifying additional barriers encountered by autistic people when seeking or receiving healthcare services across the lifespan. Addressing the barriers to healthcare access (summary in Fig. 1) identified in our review for individuals with ASD requires stakeholders to come together to:
Fig. 1. Barriers to healthcare encountered by individuals with autism spectrum disorder (ASD).
Summary of unique barriers to healthcare experienced by autistic individuals during distinct life stages (top panel) and common barriers to healthcare encountered throughout the lifespan (bottom panel).
1. Systematically identify healthcare needs and barriers to healthcare access encountered by subpopulations, particularly underserved populations, to inform the development of tailored solutions: while individuals with ASD have a greater need for healthcare services, they also have less access to appropriate healthcare, even when compared to individuals with other developmental disorders.110 Researchers, care providers, and others within the autism community should dedicate resources to better characterize the healthcare needs and barriers faced by individuals with ASD across the lifespan. Notably, there is a need to focus on underserved populations, including individuals from rural/remote regions; low SES; minoritized groups; and adults.
2. Develop programs in medical and healthcare professional curricula to increase physician knowledge of the standard of care for autistic individuals: there is an opportunity to better prepare physicians to care for individuals with autism to ensure they apply appropriate tools, technologies, and approaches to care (e.g., HCT, management of sensory sensitivities). Faculties of medicine and organizations that accredit medical school curricula and develop healthcare standards should ensure that training reflects current best practices in care for autistic individuals across the lifespan.
3. Continue to develop programs that foster public awareness of ASD to optimize early screening and diagnosis and facilitate access to healthcare for people with ASD: although current assessment tools can diagnose ASD as early as 14 months of age, diagnosis continues to occur much later in life.57,59 Advocacy groups, ASD-focused charities/foundations, and public health organizations should continue to deploy existing and new programs and educational campaigns that focus on reducing stigma and empowering people with ASD and their families with the knowledge to seek early support/diagnosis. Personalizing delivery of information and making resources available in multiple languages and for diverse cultures will facilitate the objectives defined by Autism-Europe,49 best represented in the WHO Mental Health Quality Rights Initiative.111
4. Continue to promote genetic screening following ASD diagnosis and invest in identification/validation of autism subtypes defined by scalable and cost-effective biomarkers: genetic screening has the potential to be used to diagnose ASD earlier in life and, in some instances (e.g., if an older sibling has ASD), may be considered prior to diagnosis.112 While microarray is the current standard of care, exome sequencing with copy number variation analysis has demonstrated significantly higher yield and can be used to inform patient management.101,103 Advancing the potential of genetic screening requires more research on the genetics of ASD, including the potential value of newborn testing, expanding our understanding of ASD etiology, accelerating time to diagnosis, and informing individualized treatment plans stratified by specific autism subtypes and respective biomarkers. Physician associations should continue to promote genetic screening following ASD diagnosis, while advocacy groups can bring focus to educating physicians, the public, and third-party payers on the health and economic benefits of genetic screening. As costs decrease and technology and bioinformatics improve, widespread adoption and insurance coverage of exome or genome sequencing should be considered.
5. Understand specific healthcare needs of individuals with ASD in LRCs and develop programs to increase capacity for early diagnosis and healthcare for ASD: recognizing our incomplete understanding of the healthcare needs of individuals with ASD in LRCs, there is an opportunity to increase country- or region-specific research to understand the current state of ASD (e.g., prevalence, availability of/barriers to healthcare) and support needs (e.g., increasing awareness, existing healthcare services). Existing programs such as CST can be modified and delivered in countries where it is not yet implemented, while new programs are developed to meet context-specific barriers. With the increasing adoption of telemedicine (e.g., during the COVID-19 pandemic) and access to the internet in LRCs, the development of online resources and program delivery presents a powerful opportunity to improve healthcare access for autistic individuals and their caregivers.
6. Conduct longitudinal studies in diverse populations and geographies to understand the long-term health, social and economic impacts of increasing access to healthcare across the lifespan: we have limited understanding of the socioeconomic impacts of autism across the lifespan on individuals, families, and society. Researchers should work together with individuals with autism/their families, advocacy groups, health system leaders, and policymakers to design longitudinal studies, address stakeholder interests, and inform relevant policies/programs.113,114 These studies should include populations from across the globe, in order to build a robust understanding of the global impacts of autism and enable stakeholders, including health systems, policymakers, and insurance companies, to measure and compare the success of new programs/policies aimed at increasing access to healthcare.
Many of the barriers to healthcare faced by autistic individuals also affect individuals with other psychiatric and developmental disabilities (e.g., ID, ADHD). While the recommendations above (summarized in Table 1) are focused on ASD, stakeholders should come together to codevelop solutions that are applicable to multiple psychiatric and developmental disabilities in order to maximize cost-effectiveness and impact on those in need.
Table 1.
Recommendations to improve healthcare access for individuals with ASD.
| Six ways to improve healthcare access for individuals with ASD: |
| 1. Systematically identify healthcare needs and barriers to healthcare access encountered by subpopulations, particularly underserved populations, to inform the development of tailored solutions. |
| 2. Develop programs in medical and healthcare professional curricula to increase physician knowledge of the standard of care for autistic individuals. |
| 3. Continue to develop programs that foster public awareness of ASD to optimize early screening and diagnosis and facilitate access to healthcare for people with ASD. |
| 4. Continue to promote genetic screening following ASD diagnosis and invest in identification/validation of autism subtypes defined by scalable and cost-effective biomarkers. |
| 5. Understand specific healthcare needs of individuals with ASD in LRCs and develop programs to increase capacity for early diagnosis and healthcare for ASD. |
| 6. Conduct longitudinal studies in diverse populations and geographies to understand the long-term health, social, and economic impacts of increasing access to healthcare across the lifespan. |
ASD autism spectrum disorder, LRCs lower resource countries.
Acknowledgements
This work was partially sponsored by F. Hoffman-La Roche Ltd. Shift Health consults with organizations across the health and life sciences sector, including F. Hoffman-La Roche Ltd. Authors from Shift Health (R.E.W., A.E.M., N.M.-S., A.S., H.L.) were employed under contract with Hoffman-La Roche Ltd for the purpose of this work. Authors not employed by Shift Health (S.L., J.F., T.W.F.) did not receive support or remuneration related to this work. S.L. is supported by an IGAP salary award from the BC Children’s Hospital Research Institute, and is an invited contributor on behalf of Autism Canada. The sponsor (F. Hoffman-La Roche Ltd) did not have a role in the: design and conduct of the literature review; synthesis and analysis of evidence; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author contributions
N.M.-S., H.L., A.E.M., and A.S. conceptualized and designed the study, collected the data (e.g., papers reviewed), drafted the initial manuscript, and reviewed and revised the manuscript. R.E.W., S.L., J.F., and T.W.F. conceptualized and designed the study, reviewed. and revised the manuscript. All authors approved the final manuscript as submitted for publication.
Competing interests
T.W.F. has received funding or research support from, acted as a consultant to, received travel support from, and/or received a speaker’s honorarium from Quadrant Biosciences, Impel NeuroPharma, F. Hoffmann-La Roche AG Pharmaceuticals, the Cole Family Research Fund, Simons Foundation, Ingalls Foundation, Forest Laboratories, Ecoeos, IntegraGen, Kugona LLC, Shire Development, Bristol-Myers Squibb, Roche Pharma, National Institutes of Health, and the Brain and Behavior Research Foundation and has an investor stake in Autism EYES LLC. J.F. has received research support from Policlinica Gipuzkoa Foundation (PGF), Servier, and AIMS-2 Trials/Project ID 777394. He has received partial support for professional meetings attendance from PGF, ESCAP & AACAP.
Patient consent
Not required for this study.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
- 2.Elsabbagh M, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5:160–179. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168:721–728. doi: 10.1001/jamapediatrics.2014.210. [DOI] [PubMed] [Google Scholar]
- 4.Knapp M, Romeo R, Beecham J. Economic cost of autism in the UK. Autism. 2009;13:317–336. doi: 10.1177/1362361309104246. [DOI] [PubMed] [Google Scholar]
- 5.Markowitz LA, et al. Development and psychometric evaluation of a psychosocial quality-of-life questionnaire for individuals with autism and related developmental disorders. Autism. 2016;20:832–844. doi: 10.1177/1362361315611382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brookman-Frazee L, Stadnick N, Chlebowski C, Baker-Ericzén M, Ganger W. Characterizing psychiatric comorbidity in children with autism spectrum disorder receiving publicly funded mental health services. Autism. 2018;22:938–952. doi: 10.1177/1362361317712650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davignon MN, Qian Y, Massolo M, Croen LA. Psychiatric and medical conditions in transition-aged individuals with ASD. Pediatrics. 2018;141:S335–S345. doi: 10.1542/peds.2016-4300K. [DOI] [PubMed] [Google Scholar]
- 8.Vohra R, Madhavan S, Sambamoorthi U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism. 2017;21:995–1009. doi: 10.1177/1362361316665222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antezana L, Scarpa A, Valdespino A, Albright J, Richey JA. Rural trends in diagnosis and services for autism spectrum disorder. Front. Psychol. 2017;8:590. doi: 10.3389/fpsyg.2017.00590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas KC, Ellis AR, McLaurin C, Daniels J, Morrissey JP. Access to care for autism-related services. J. Autism Dev. Disord. 2007;37:1902–1912. doi: 10.1007/s10803-006-0323-7. [DOI] [PubMed] [Google Scholar]
- 11.American Psychological Association. Education and Socioeconomic Status (American Psychological Association, 2019).
- 12.American Board of Pediatrics. Pediatric Physicians Workforce Data Book, 2018–2019 (American Board of Pediatrics, 2019).
- 13.American Academy of Child and Adolescent Psychiatry. Workforce Maps by State: Practicing Child and Adolescent Psychiatrists (American Academy of Child and Adolescent Psychiatry, 2019).
- 14.Elder JH, Brasher S, Alexander B. Identifying the Barriers to early diagnosis and treatment in underserved individuals with autism spectrum disorders (ASD) and their families: a qualitative study. Issues Ment. Health Nurs. 2016;37:412–420. doi: 10.3109/01612840.2016.1153174. [DOI] [PubMed] [Google Scholar]
- 15.Raymaker DM, et al. Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism. 2017;21:972–984. doi: 10.1177/1362361316661261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dudley KM, Klinger MR, Meyer A, Powell P, Klinger LG. Understanding service usage and needs for adults with ASD: the importance of living situation. J. Autism Dev. Disord. 2019;49:556–568. doi: 10.1007/s10803-018-3729-0. [DOI] [PubMed] [Google Scholar]
- 17.Mazurek MO, Curran A, Burnette C, Sohl K. ECHO autism STAT: accelerating early access to autism diagnosis. J. Autism Dev. Disord. 2019;49:127–137. doi: 10.1007/s10803-018-3696-5. [DOI] [PubMed] [Google Scholar]
- 18.Juárez AP, et al. Early identification of ASD through telemedicine: potential value for underserved populations. J. Autism Dev. Disord. 2018;48:2601–2610. doi: 10.1007/s10803-018-3524-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuhlthau KA, et al. Health care transition services for youth with autism spectrum disorders: perspectives of caregivers. Pediatrics. 2016;137(Suppl. 2):S158–S166. doi: 10.1542/peds.2015-2851N. [DOI] [PubMed] [Google Scholar]
- 20.Nicolaidis C, et al. “Respect the way I need to communicate with you”: healthcare experiences of adults on the autism spectrum. Autism. 2015;19:824–831. doi: 10.1177/1362361315576221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Austriaco K, Aban I, Willig J, Kong M. Contemporary trainee knowledge of autism: how prepared are our future providers? Front. Pediatr. 2019;7:165. doi: 10.3389/fped.2019.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Unigwe S, et al. GPs’ confidence in caring for their patients on the autism spectrum: an online self-report study. Br. J. Gen. Pract. 2017;67:e445–e452. doi: 10.3399/bjgp17X690449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muskat B, et al. Autism comes to the hospital: the experiences of patients with autism spectrum disorder, their parents and health-care providers at two Canadian paediatric hospitals. Autism. 2015;19:482–490. doi: 10.1177/1362361314531341. [DOI] [PubMed] [Google Scholar]
- 24.Saqr Y, Braun E, Porter K, Barnette D, Hanks C. Addressing medical needs of adolescents and adults with autism spectrum disorders in a primary care setting. Autism. 2018;22:51–61. doi: 10.1177/1362361317709970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradshaw P, Pellicano E, van Driel M, Urbanowicz A. How can we support the healthcare needs of autistic adults without intellectual disability? Curr. Dev. Disord. Rep. 2019;6:45–56. doi: 10.1007/s40474-019-00159-9. [DOI] [Google Scholar]
- 26.Mason D, et al. A systematic review of what barriers and facilitators prevent and enable physical healthcare services access for autistic adults. J. Autism Dev. Disord. 2019;49:3387–3400. doi: 10.1007/s10803-019-04049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doherty, A. J. et al. Barriers and facilitators to primary health care for people with intellectual disabilities and/or autism: an integrative review. BJGP Open4, bjgpopen20X101030 (2020). [DOI] [PMC free article] [PubMed]
- 28.Sohl K, Mazurek MO, Brown R. ECHO Autism: using technology and mentorship to bridge gaps, increase access to care, and bring best practice autism care to primary care. Clin. Pediatr. 2017;56:509–511. doi: 10.1177/0009922817691825. [DOI] [PubMed] [Google Scholar]
- 29.Nicolaidis C, et al. The development and evaluation of an online healthcare toolkit for autistic adults and their primary care providers. J. Gen. Intern. Med. 2016;31:1180–1189. doi: 10.1007/s11606-016-3763-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pickard KE, Ingersoll BR. Quality versus quantity: the role of socioeconomic status on parent-reported service knowledge, service use, unmet service needs, and barriers to service use. Autism. 2016;20:106–115. doi: 10.1177/1362361315569745. [DOI] [PubMed] [Google Scholar]
- 31.Barry CL, et al. Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Aff. 2017;36:1754–1761. doi: 10.1377/hlthaff.2017.0515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mandell DS, et al. Effects of autism spectrum disorder insurance mandates on the treated prevalence of autism spectrum disorder. JAMA Pediatr. 2016;170:887–893. doi: 10.1001/jamapediatrics.2016.1049. [DOI] [PubMed] [Google Scholar]
- 33.Herlihy L, Knoch K, Vibert B, Fein D. Parents’ first concerns about toddlers with autism spectrum disorder: effect of sibling status. Autism. 2015;19:20–28. doi: 10.1177/1362361313509731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salomone E, et al. Development of the WHO caregiver skills training program for developmental disorders or delays. Front. Psychiatry. 2019;10:769. doi: 10.3389/fpsyt.2019.00769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou B, et al. Effects of Parent-Implemented Early Start Denver model intervention on Chinese toddlers with autism spectrum disorder: a non-randomized controlled trial. Autism Res. 2018;11:654–666. doi: 10.1002/aur.1917. [DOI] [PubMed] [Google Scholar]
- 36.Fox F, Aabe N, Turner K, Redwood S, Rai D. “It was like walking without knowing where I was going”: a qualitative study of autism in a UK Somali migrant community. J. Autism Dev. Disord. 2017;47:305–315. doi: 10.1007/s10803-016-2952-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kairys SW, Petrova A. Role of participation of pediatricians in the “Activated Autism Practice” program in practicing children with autism spectrum disorders at the primary care setting. Glob. Pediatr. Health. 2016;3:2333794X16663544. doi: 10.1177/2333794X16663544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khanlou N, et al. Access barriers to services by immigrant mothers of children with autism in Canada. Int. J. Ment. Health Addict. 2017;15:239–259. doi: 10.1007/s11469-017-9732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Autism Speaks. Autism speaks non-English resources. https://www.autismspeaks.org/non-english-resources (2021).
- 40.University Southern California. Autism fact sheets. http://www.uscucedd.org/publications-resources/autism-pubs/autism-fact-sheets (2011).
- 41.Kinnear SH, Link BG, Ballan MS, Fischbach RL. Understanding the experience of stigma for parents of children with autism spectrum disorder and the role stigma plays in families’ lives. J. Autism Dev. Disord. 2016;46:942–953. doi: 10.1007/s10803-015-2637-9. [DOI] [PubMed] [Google Scholar]
- 42.Vogan V, Lake JK, Tint A, Weiss JA, Lunsky Y. Tracking health care service use and the experiences of adults with autism spectrum disorder without intellectual disability: a longitudinal study of service rates, barriers and satisfaction. Disabil. Health J. 2017;10:264–270. doi: 10.1016/j.dhjo.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 43.Pasha SB, Qadir TF, Fatima H, Hussain SA. Sesame Street’s recognition of autism. Lancet Psychiatry. 2017;4:520–521. doi: 10.1016/S2215-0366(17)30239-0. [DOI] [PubMed] [Google Scholar]
- 44.Anthony BJ, et al. Increasing autism acceptance: the impact of the Sesame Street “See Amazing in All Children” initiative. Autism. 2020;24:95–108. doi: 10.1177/1362361319847927. [DOI] [PubMed] [Google Scholar]
- 45.Ip A, Zwaigenbaum L, Brian JA. Post-diagnostic management and follow-up care for autism spectrum disorder. Paediatr. Child Health. 2019;24:461–468. doi: 10.1093/pch/pxz121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization. Autism spectrum disorders. https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders (2019).
- 47.Hyman SL, Levy SE, Myers SM. Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020;145:e20193447. doi: 10.1542/peds.2019-3447. [DOI] [PubMed] [Google Scholar]
- 48.National Institute for Health and Care Excellence. Autism. https://www.nice.org.uk/guidance/qs51/resources/autism-pdf-2098722137029 (2014).
- 49.Barthélémy, C., Fuentes, J., Howlin, P. & Jan van der Gaag, R. People with Autism Spectrum Disorder. Identification, Understanding, Intervention 3rd edn (Autism Europe, 2019).
- 50.Weitlauf AS, Gotham KO, Vehorn AC, Warren ZE. Brief report: DSM-5 “levels of support”: a comment on discrepant conceptualizations of severity in ASD. J. Autism Dev. Disord. 2014;44:471–476. doi: 10.1007/s10803-013-1882-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lord C, et al. Autism spectrum disorder. Nat. Rev. Dis. Prim. 2020;6:5. doi: 10.1038/s41572-019-0138-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Happé FG, et al. Demographic and cognitive profile of individuals seeking a diagnosis of autism spectrum disorder in adulthood. J. Autism Dev. Disord. 2016;46:3469–3480. doi: 10.1007/s10803-016-2886-2. [DOI] [PubMed] [Google Scholar]
- 53.World Health Organization. Comprehensive and Coordinated Efforts for the Management of Autism Spectrum Disorders, Sixty-Seventh World Health Assembly (World Health Organization, 2014).
- 54.Rutherford M, et al. Gender ratio in a clinical population sample, age of diagnosis and duration of assessment in children and adults with autism spectrum disorder. Autism. 2016;20:628–634. doi: 10.1177/1362361315617879. [DOI] [PubMed] [Google Scholar]
- 55.Giarelli E, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil. Health J. 2010;3:107–116. doi: 10.1016/j.dhjo.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guinchat V, et al. Very early signs of autism reported by parents include many concerns not specific to autism criteria. Res. Autism Spectr. Disord. 2012;6:589–601. doi: 10.1016/j.rasd.2011.10.005. [DOI] [Google Scholar]
- 57.Pierce K, et al. Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatr. 2019;173:578–587. doi: 10.1001/jamapediatrics.2019.0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maenner MJ, et al. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill. Summ. 2020;69:1–12. doi: 10.15585/mmwr.ss6904a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Salomone E, Charman T, McConachie H, Warreyn P. Child’s verbal ability and gender are associated with age at diagnosis in a sample of young children with ASD in Europe. Child Care Health Dev. 2016;42:141–145. doi: 10.1111/cch.12261. [DOI] [PubMed] [Google Scholar]
- 60.Public Health Agency of Canada. Autism spectrum disorder among children and youth in Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/autism-spectrum-disorder-children-youth-canada-2018.html (2018).
- 61.Clark MLE, Vinen Z, Barbaro J, Dissanayake C. School age outcomes of children diagnosed early and later with autism spectrum disorder. J. Autism Dev. Disord. 2018;48:92–102. doi: 10.1007/s10803-017-3279-x. [DOI] [PubMed] [Google Scholar]
- 62.Dawson G, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125:e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zuckerman K, Lindly OJ, Chavez AE. Timeliness of autism spectrum disorder diagnosis and use of services among U.S. elementary school-aged children. Psychiatr. Serv. 2017;68:33–40. doi: 10.1176/appi.ps.201500549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.American Academy of Pediatrics. Initial medical evaluation of a child diagnosed with an autism spectrum disorder. https://www.aap.org/en-us/Documents/cocd_fact_sheet_initialmedicine.pdf (2013).
- 65.Canadian Paediatric Society. Standards of diagnostic assessment for autism spectrum disorder. https://www.cps.ca/en/documents/position/asd-diagnostic-assessment#ref24 (2019). [DOI] [PMC free article] [PubMed]
- 66.Schaefer GB, Mendelsohn NJ, Professional Practice and Guidelines Committee. Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genet. Med. 2013;15:399–407. doi: 10.1038/gim.2013.32. [DOI] [PubMed] [Google Scholar]
- 67.Barton KS, et al. Pathways from autism spectrum disorder diagnosis to genetic testing. Genet. Med. 2018;20:737–744. doi: 10.1038/gim.2017.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shattuck PT, et al. Services for adults with an autism spectrum disorder. Can. J. Psychiatry. 2012;57:284–291. doi: 10.1177/070674371205700503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shea LL, et al. Brief report: service use and associated expenditures among adolescents with autism spectrum disorder transitioning to adulthood. J. Autism Dev. Disord. 2018;48:3223–3227. doi: 10.1007/s10803-018-3563-4. [DOI] [PubMed] [Google Scholar]
- 70.Weiss JA, et al. Health concerns and health service utilization in a population cohort of young adults with autism spectrum disorder. J. Autism Dev. Disord. 2018;48:36–44. doi: 10.1007/s10803-017-3292-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bennett AE, Miller JS, Stollon N, Prasad R, Blum NJ. Autism spectrum disorder and transition-aged youth. Curr. Psychiatry Rep. 2018;20:103. doi: 10.1007/s11920-018-0967-y. [DOI] [PubMed] [Google Scholar]
- 72.Crane L, Adams F, Harper G, Welch J, Pellicano E. “Something needs to change”: mental health experiences of young autistic adults in England. Autism. 2019;23:477–493. doi: 10.1177/1362361318757048. [DOI] [PubMed] [Google Scholar]
- 73.Cheak-Zamora NC, Yang X, Farmer JE, Clark M. Disparities in transition planning for youth with autism spectrum disorder. Pediatrics. 2013;131:447–454. doi: 10.1542/peds.2012-1572. [DOI] [PubMed] [Google Scholar]
- 74.Rast JE, Shattuck PT, Roux AM, Anderson KA, Kuo A. The medical home and health care transition for youth with autism. Pediatrics. 2018;141:S328–S334. doi: 10.1542/peds.2016-4300J. [DOI] [PubMed] [Google Scholar]
- 75.Nathenson RA, Zablotsky B. The transition to the adult health care system among youths with autism spectrum disorder. Psychiatr. Serv. 2017;68:735–738. doi: 10.1176/appi.ps.201600239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Autism Community, Newfoundland Labrador. Report: needs assessment survey. https://www.autism.nf.net/wp-content/uploads/2017/03/Needs-Assesment-2015.pdf (2015).
- 77.Cheak-Zamora NC, Teti M. “You think it’s hard now … It gets much harder for our children”: youth with autism and their caregiver’s perspectives of health care transition services. Autism. 2015;19:992–1001. doi: 10.1177/1362361314558279. [DOI] [PubMed] [Google Scholar]
- 78.Kuhlthau KA, Warfield ME, Hurson J, Delahaye J, Crossman MK. Pediatric provider’s perspectives on the transition to adult health care for youth with autism spectrum disorder: current strategies and promising new directions. Autism. 2015;19:262–271. doi: 10.1177/1362361313518125. [DOI] [PubMed] [Google Scholar]
- 79.Mazurek MO, et al. ECHO Autism Transition: enhancing healthcare for adolescents and young adults with autism spectrum disorder. Autism. 2020;24:633–644. doi: 10.1177/1362361319879616. [DOI] [PubMed] [Google Scholar]
- 80.Dietz PM, Rose CE, McArthur D, Maenner M. National and state estimates of adults with autism spectrum disorder. J. Autism Dev. Disord. 2020;50:4258–4266. doi: 10.1007/s10803-020-04494-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Croen LA, et al. The health status of adults on the autism spectrum. Autism. 2015;19:814–823. doi: 10.1177/1362361315577517. [DOI] [PubMed] [Google Scholar]
- 82.Hand BN, Angell AM, Harris L, Carpenter LA. Prevalence of physical and mental health conditions in Medicare-enrolled, autistic older adults. Autism. 2020;24:755–764. doi: 10.1177/1362361319890793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hirvikoski T, et al. Premature mortality in autism spectrum disorder. Br. J. Psychiatry. 2016;208:232–238. doi: 10.1192/bjp.bp.114.160192. [DOI] [PubMed] [Google Scholar]
- 84.Benevides, T. W. et al. Interventions to address health outcomes among autistic adults: a systematic review. Autism 1362361320913664 (2020). [DOI] [PMC free article] [PubMed]
- 85.Warfield ME, Crossman MK, Delahaye J, Der Weerd E, Kuhlthau KA. Physician perspectives on providing primary medical care to adults with autism spectrum disorders (ASD) J. Autism Dev. Disord. 2015;45:2209–2217. doi: 10.1007/s10803-015-2386-9. [DOI] [PubMed] [Google Scholar]
- 86.Autism Canada. Aging and autism: a think tank round table. https://autismcanada.org/research/scientific-symposium/ (2017).
- 87.Camm-Crosbie L, Bradley L, Shaw R, Baron-Cohen S, Cassidy S. ‘People like me don’t get support’: autistic adults’ experiences of support and treatment for mental health difficulties, self-injury and suicidality. Autism. 2019;23:1431–1441. doi: 10.1177/1362361318816053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Maddox BB, Gaus VL. Community mental health services for autistic adults: good news and bad news. Autism Adulthood. 2019;1:15–19. doi: 10.1089/aut.2018.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bruder MB, Kerins G, Mazzarella C, Sims J, Stein N. Brief report: the medical care of adults with autism spectrum disorders: identifying the needs. J. Autism Dev. Disord. 2012;42:2498–2504. doi: 10.1007/s10803-012-1496-x. [DOI] [PubMed] [Google Scholar]
- 90.Zerbo O, Massolo ML, Qian Y, Croen LA. A study of physician knowledge and experience with autism in adults in a large integrated healthcare system. J. Autism Dev. Disord. 2015;45:4002–4014. doi: 10.1007/s10803-015-2579-2. [DOI] [PubMed] [Google Scholar]
- 91.Nicolaidis C, et al. Comparison of healthcare experiences in autistic and non-autistic adults: a cross-sectional online survey facilitated by an academic-community partnership. J. Gen. Intern. Med. 2013;28:761–769. doi: 10.1007/s11606-012-2262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zerbo O, et al. Health care service utilization and cost among adults with autism spectrum disorders in a U.S. Integrated Health Care System. Autism Adulthood. 2019;1:27–36. doi: 10.1089/aut.2018.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roestorf A, et al. “Older Adults with ASD: The Consequences of Aging”. Insights from a series of special interest group meetings held at the International Society for Autism Research 2016–2017. Res. Autism Spectr. Disord. 2019;63:3–12. doi: 10.1016/j.rasd.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Altay MA. Family physicians’ awareness of autism spectrum disorder: results from a survey study. Open Access Maced. J. Med. Sci. 2019;7:967–972. doi: 10.3889/oamjms.2019.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.de Vries PJ. Thinking globally to meet local needs: autism spectrum disorders in Africa and other low-resource environments. Curr. Opin. Neurol. 2016;29:130–136. doi: 10.1097/WCO.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 96.Rahbar MH, Ibrahim K, Assassi P. Knowledge and attitude of general practitioners regarding autism in Karachi, Pakistan. J. Autism Dev. Disord. 2011;41:465–474. doi: 10.1007/s10803-010-1068-x. [DOI] [PubMed] [Google Scholar]
- 97.Mahapatra P, et al. Parental care-seeking pathway and challenges for autistic spectrum disorders children: a mixed method study from Bhubaneswar, Odisha. Indian J. Psychiatry. 2019;61:37–44. doi: 10.4103/psychiatry.IndianJPsychiatry_257_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tekola B, et al. Adapting and pre-testing the World Health Organization’s Caregiver Skills Training programme for autism and other developmental disorders in a very low-resource setting: findings from Ethiopia. Autism. 2020;24:51–63. doi: 10.1177/1362361319848532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Divan G, et al. The feasibility and effectiveness of PASS Plus, a lay health worker delivered comprehensive intervention for autism spectrum disorders: Pilot RCT in a rural low and middle income country setting. Autism Res. 2019;12:328–339. doi: 10.1002/aur.1978. [DOI] [PubMed] [Google Scholar]
- 100.Bai D, et al. Association of genetic and environmental factors with autism in a 5-Country Cohort. JAMA Psychiatry. 2019;76:1035–1043. doi: 10.1001/jamapsychiatry.2019.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Srivastava S, et al. Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet. Med. 2019;21:2413–2421. doi: 10.1038/s41436-019-0554-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Feliciano P, et al. Exome sequencing of 457 autism families recruited online provides evidence for autism risk genes. NPJ Genom. Med. 2019;4:19. doi: 10.1038/s41525-019-0093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tarailo-Graovac M, et al. Exome sequencing and the management of neurometabolic disorders. N. Engl. J. Med. 2016;374:2246–2255. doi: 10.1056/NEJMoa1515792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wolff M, et al. Genetic and phenotypic heterogeneity suggest therapeutic implications in SCN2A-related disorders. Brain. 2017;140:1316–1336. doi: 10.1093/brain/awx054. [DOI] [PubMed] [Google Scholar]
- 105.Frazier TW, et al. Molecular and phenotypic abnormalities in individuals with germline heterozygous PTEN mutations and autism. Mol. Psychiatry. 2015;20:1132–1138. doi: 10.1038/mp.2014.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Frazier TW. Autism spectrum disorder associated with germline heterozygous PTEN mutations. Cold Spring Harb. Perspect. Med. 2019;9:037002. doi: 10.1101/cshperspect.a037002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Beversdorf DQ, Missouri Autism Summit Consortium. Phenotyping, etiological factors, and biomarkers: toward precision medicine in autism spectrum disorders. J. Dev. Behav. Pediatr. 2016;37:659–673. doi: 10.1097/DBP.0000000000000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.The University of British Columbia. iTARGET Autism Initiative (individualized Treatments for Autism Recovery using Genetic-Environmental Targets). http://www.itargetautism.ca/ (2017).
- 109.Shea L, Newschaffer CJ, Xie M, Myers SM, Mandell DS. Genetic testing and genetic counseling among Medicaid-enrolled children with autism spectrum disorder in 2001 and 2007. Hum. Genet. 2014;133:111–116. doi: 10.1007/s00439-013-1362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Karpur A, Lello A, Frazier T, Dixon PJ, Shih AJ. Health disparities among children with autism spectrum disorders: analysis of the National Survey of Children’s Health 2016. J. Autism Dev. Disord. 2019;49:1652–1664. doi: 10.1007/s10803-018-3862-9. [DOI] [PubMed] [Google Scholar]
- 111.WHO. WHO mental health quality rights initiative. https://www.who.int/mental_health/policy/quality_rights/QRs_flyer_eng_2017.pdf?ua=1 (2017).
- 112.Ozonoff S, et al. Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics. 2011;128:e488–e495. doi: 10.1542/peds.2010-2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Frazier TW, et al. Brief report: a survey of autism research priorities across a diverse community of stakeholders. J. Autism Dev. Disord. 2018;48:3965–3971. doi: 10.1007/s10803-018-3642-6. [DOI] [PubMed] [Google Scholar]
- 114.Hudry K, Pellicano E, Uljarević M, Whitehouse AJO. Setting the research agenda to secure the wellbeing of autistic people. Lancet Neurol. 2020;19:374–376. doi: 10.1016/S1474-4422(20)30031-4. [DOI] [PubMed] [Google Scholar]