Abstract
Atraumatic splenic rupture (ASR) is a rare complication of acute pancreatitis with high mortality and morbidity rates. We present a case of a 63-year-old woman with a history of hypertension, presenting with acute pancreatitis who subsequently developed a splenic rupture requiring a laparotomy and splenectomy. ASR is a rare but life-threatening complication requiring prompt recognition and management and should be considered in patient with pancreatitis who develops sudden haemodynamic compromise and worsening anaemia.
Keywords: pancreatitis, general surgery, drugs: gastrointestinal system
Background
Atraumatic splenic rupture (ASR) is a rare clinical presentation with a mortality rate ranging from 12.2% to 20%.1 Acute-onset left upper quadrant pain, guarding and haemodynamic instability should raise a high index of suspicion of an ASR. ASR can occur in both diseased and non-diseased spleen, with the former being more common (93% and 7%, respectively).2 Approximately 10% ASR arise from local inflammatory processes.3 ASR associated with pancreatitis has a reported prevalence of 0.4% in a study by Malka et al who assessed splenic complications among 500 patients with pancreatitis.4 5 The morbidity and mortality of splenic complications in pancreatitis range from 39% to 79% and 0.8% to 3.5%, respectively,3 and so its early recognition and management is vital. We present a case of an ASR secondary to acute pancreatitis.
Case presentation
A 63-year-old woman presented to the emergency department (ED) with a 1-day history of postprandial band-like upper abdominal pain, accompanied by vomiting and poor oral intake. The patient had undergone stereotactic excision of a right parafalcine frontal meningioma 1 week before presentation by the neurosurgical team. Postoperatively, she was prescribed a regimen of dexamethasone 4 mg two times per day and discharged 3 days later with a weaning regimen over 3 days. Besides hypertension requiring perindopril and amlodipine, for which she has been taking for several years, she reported no other comorbidities or recent medication changes. She is, however, a social drinker, with a 30 pack-year smoking history.
On her sixth postoperative day, after meningioma excision, she presented again to the ED with abdominal pain. On presentation, she appeared uncomfortable and had a blood pressure of 120/70 mm Hg, heart rate of 58 beats per minute, respiratory rate of 16 per minute and a temperature of 35.2°C. Her abdomen was soft with epigastric tenderness on examination. The patient denied any recent alcohol consumption and recent history of trauma, however, she had sustained recurrent falls 2 weeks prior to her neurosurgical intervention.
Investigations
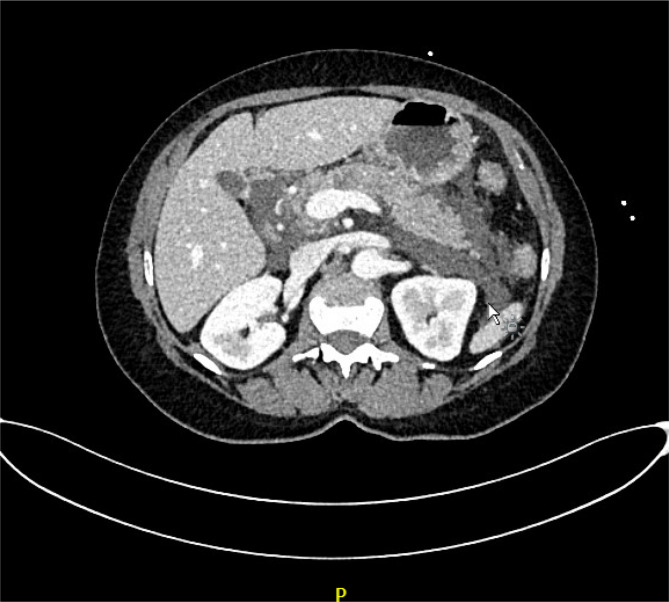
Her serum laboratory test results on second admission were as follows: white cell count (WCC)—24.4×109/L, C reactive protein (CRP)—8.9 mg/L, lipase—8554 units/L, haemoglobin—116 g/L, lactate—1.2 mmol/L and lactate dehydrogenase—289 units/L. A CT scan was performed which demonstrated acute interstitial edematous pancreatitis with foci of pancreatic calcification (figure 1). The patient was subsequently diagnosed with acute steroid- induced pancreatitis based on her history and recent administration of steroids.
Figure 1.
Acute interstitial oedematous pancreatitis.
An abdominal ultrasound then revealed three gallbladder polyps with no evidence of calculi. Apart from a slightly elevated low-density lipoprotein cholesterol level of 2.2 mmol/L, her pancreatic screening results were normal. She remained clinically well, not requiring intensive care support. Her CRP levels were upward trending, peaking at 338 mg/L on admission day 4. On admission day 7, she developed worsening abdominal pain and had a presyncopal event. On examination, she had a blood pressure of 87/51 mm Hg, abdominal distention and marked left upper quadrant tenderness. Repeat examination of her serum laboratory tests demonstrated a haemoglobin of 46 g/L, WCC 13.1×109/L and lactate of 4.6 mmol/L. An urgent CT angiogram of the abdomen revealed a 14.8 cm subcapsular splenic haematoma in its inferior portion and a 6 cm haematoma overlying the left lateral lobe of the liver with no signs of active arterial extravasation (figure 2). A massive transfusion protocol was subsequently activated with high suspicions of acute ASR.
Figure 2.
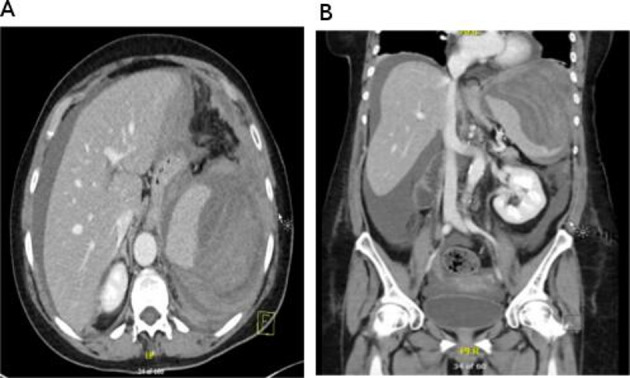
Axial (A) and coronal (B) images showing subcapsular splenic haematoma with haemoperitoneum.
Outcome and follow-up
The patient was rapidly taken to surgery for an emergency laparotomy and splenectomy. Intraoperative findings included a moderate volume of haemoperitoneum with a large haematoma surrounding the spleen and intruding into the left paracolic gutter. A splenectomy, evacuation of haematoma and peritoneal lavage were performed with an estimated 2.5 L blood loss. She recovered well postoperatively and was discharged after 7 days. During her inpatient stay, besides her regular medications, she received analgesia with acute pain service input which included regular paracetamol and an oxycodone patient-controlled analgesia. She continued to take her prescribed regular amlodipine and perindopril on discharge. Following addition to the spleen registry, she also received pneumococcal, meningococcal and Haemophilus influenzae vaccinations. A regimen of 250 mg of oral amoxicillin daily was initiated for prophylaxis as per Spleen Australia guidelines.6 The histology revealed a capsular defect, lending evidence to a rupture with no splenic parenchymal pathology. She received a follow-up CT abdomen and pelvis 2 months postoperation which revealed a complete resolution of pancreatitis with minor atrophy of the body of the pancreas corresponding with the site of the previous pancreatic necrosis.
Discussion
Splenic complications secondary to pancreatitis are relatively rare, and the pathophysiology is not completely understood. However, one of the major contributory factors is the proximity of the pancreatic tail to the splenic hilar structures. The lienorenal ligament which enters the splenic hilum contains the splenic artery, vein, and pancreatic tail and is thought to contribute to associated complications. Common complications in chronic pancreatitis include subcapsular haematoma, splenic rupture and pseudocysts, whereas intrasplenic haemorrhage and splenic infarction occur more commonly as complications of acute pancreatitis.1 7 8
In splenic ruptures, the extravasation of pancreatic fluid or direct erosion from pseudocysts causing injury to the adjacent spleen is one of the proposed pathophysiology. A literature review done by Jain et al describing 28 cases of pancreatitis complicated by subcapsular splenic haematoma or rupture revealed further potential mechanisms for splenic rupture, including splenic vein thrombosis, in which venous outflow obstruction can cause hypertension and splenic parenchymal congestion, as well as adhesions from recurrent pancreatitis. The most common aetiology of pancreatitis in this study was alcohol consumption (67.9%). It was also noted that most cases had chronic pancreatitis or previous episodes of pancreatitis (70%).7
ASR can be classified into six categories: neoplastic processes such as leukaemia, lymphoma and multiple myeloma; infections such as Malaria, Epstein-Barr virus, Babesia Microti, cytomegalovirus and epatitis A, B and C; haematological causes; inflammatory processes such as acute or chronic pancreatitis and lupus erythematosus; primary splenic disorders such as splenic infarcts or portal hypertension; and iatrogenic causes such as anticoagulation or peritoneal dialysis.2 9 ASR in a non-diseased spleen, however, is extremely rare. Gorg et al performed a study describing ultrasound patterns, diagnosis and follow-up in 41 cases with ASR, which revealed that the aetiology includes infection and various malignant diseases in 82% of the cases.
Various nomenclatures have been used to describe ASR, which include ‘true spontaneous’, ‘spontaneous’, ‘pathological’ and ‘occult’. Spontaneous and pathological splenic ruptures are the most common terms used, where the former is used to describe a splenic rupture in the absence of trauma irrespective of the histopathological findings, while the latter is used to describe ASRs in a histopathologically normal spleen.10 Orloff and Peskin developed a criteria-based diagnosis for true spontaneous splenic rupture which included no history of trauma, no pre-existing disease of the spleen, no scarring and adhesion in the spleen, and normal histology of spleen both macroscopically and microscopically.11–13 Our case fits the criteria for a true spontaneous splenic rupture. Although a specific investigation to rule out the various causes of ASR was not performed, our patient had no risk factors or preceding infective symptoms to suggest the aetiology was an infectious process. She also did not have any relevant comorbidities, and the normal histological finding of the spleen makes other causes of the splenic rupture unlikely.
A CT scan has a 96%–100% sensitivity and specificity for splenic injury and is considered the gold standard investigation tool in haemodynamically stable patients. However, it is reported that a dual phase study, including the arterial and portal venous phases, is more sensitive and specific than single phase study, such as that of the portal venous phase only. Although less sensitive, the negative single-phase CT scan performed on the patient on her second admission to the hospital would still reasonably rule out any obvious splenic injury which might have occurred secondary to blunt trauma from the patient’s multiple falls prior to her presentation in the ED.14
Diagnosing a splenic haematoma or rupture is time critical. It can be especially challenging without a preceding history of trauma. This diagnosis should be suspected when a patient develops increasing left upper quadrant pain radiating to the left shoulder, develops a palpable mass in the left upper quadrant, has a sudden drop in haemoglobin levels, or is haemodynamic unstable. A contrast-enhanced CT abdomen should then be performed to assess for complications of acute pancreatitis.15 Depending on the degree of haemoperitoneum, the clinical status of the patient and the extent of splenic injury according to the American Association for the Surgery of Trauma scale, the management of subcapsular splenic haematoma can range from conservative management to splenic artery embolisation. In contrast, splenic ruptures are typically treated with a laparotomy and splenectomy, with or without a distal pancreatectomy.13 15 In ASR, consideration should be given to underlying aetiology and so, a splenectomy in haemodynamically stable patients can be justified as first, histological examination can aid in diagnosis and second, a significant number of malignancies can cause ASR, thereby prohibiting an organ preserving approach.10 In our case, the patient uncommonly presented with a first episode of acute pancreatitis secondary to steroid use. She then suffered a rare complication of acute pancreatitis—atraumatic spontaneous splenic rupture. She received prompt and adequate treatment and made an uneventful recovery.
Learning points.
Atraumatic splenic rupture (ASR) is a rare but life-threatening complication requiring prompt recognition and management and should be considered in patient with pancreatitis who develops sudden haemodynamic compromise and worsening anaemia.
ASRs carry a mortality rate of 12%–20%.
All splenic ruptures require prompt recognition, management, close monitoring and follow-up.
Footnotes
Contributors: RN: conception of the work, design of the work, acquisition of data, drafting the work, revising the work critically for important intellectual content, final approval of the version to be published, agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. ZY: conception of the work, design of the work, acquisition of data, drafting the work, revising the work critically for important intellectual content, final approval of the version to be published. KM: revising the work critically for important intellectual content, final approval of the version to be published. AA: revising the work critically for important intellectual content, final approval of the version to be published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Toussi HR, Cross KS, Sheehan SJ, et al. Spontaneous splenic rupture: a rare complication of acute pancreatitis. ireland: department of surgery, Beaumont Hospital. The British Journal of Surgery 1996;83 https://pubmed.ncbi.nlm.nih.gov/8689204/ [DOI] [PubMed] [Google Scholar]
- 2.Dumic I, Patel J, Hart M, et al. Splenic rupture as the first manifestation of Babesia microti infection: report of a case and review of literature. Am J Case Rep 2018;19:335–41. 10.12659/AJCR.908453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hernani BL, Silva PC, Nishio RT, et al. Acute pancreatitis complicated with splenic rupture: a case report. World J Gastrointest Surg 2015;7:219–22. 10.4240/wjgs.v7.i9.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang S, Liu F, Buch H, et al. Large subcapsular splenic hematoma with a large pancreatic pseudocyst was successfully treated with splenic arterial embolization and ultrasound-guided percutaneous drainage of pancreatic pseudocyst.. Case Rep Med 2017;2017:6381479. 10.1155/2017/6381479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malka D, Hammel P, Lévy P, et al. Splenic complications in chronic pancreatitis: prevalence and risk factors in a medical-surgical series of 500 patients. Br J Surg 1998;85:1645–9. 10.1046/j.1365-2168.1998.00952.x [DOI] [PubMed] [Google Scholar]
- 6.Kanhutu K, Jones P, Cheng AC, et al. Spleen Australia guidelines for the prevention of sepsis in patients with asplenia and hyposplenism in Australia and New Zealand. Intern Med J 2017;47:848–55. 10.1111/imj.13348 [DOI] [PubMed] [Google Scholar]
- 7.Jain D, Lee B, Rajala M. Atraumatic splenic hemorrhage as a rare complication of pancreatitis: case report and literature review. Clin Endosc 2020;53:311–20. 10.5946/ce.2019.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gandhi V, Philip S, Maydeo A, et al. Ruptured subcapsular giant haematoma of the spleen--a rare complication of acute pancreatitis. Trop Gastroenterol 2010;31:123–4. [PubMed] [Google Scholar]
- 9.Lam GY, Chan AK, Powis JE. Possible infectious causes of spontaneous splenic rupture: a case report. J Med Case Rep 2014;8:396. 10.1186/1752-1947-8-396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Renzulli P, Hostettler A, Schoepfer AM, et al. Systematic review of atraumatic splenic rupture. Br J Surg 2009;96:1114–21. 10.1002/bjs.6737 [DOI] [PubMed] [Google Scholar]
- 11.Debnath J, Sonkar S, Sharma V, et al. Spontaneous rupture of spleen masquerading as acute pancreatitis. Am J Emerg Med 2014;32:394.e1–3. 10.1016/j.ajem.2013.10.036 [DOI] [PubMed] [Google Scholar]
- 12.ORLOFF MJ, PESKIN GW. Spontaneous rupture of the normal spleen; a surgical enigma. Int Abstr Surg 1958;106:1–11. [PubMed] [Google Scholar]
- 13.S S, Olakkengil S, Rozario AP. Occult splenic rupture in a case of chronic calcific pancreatitis with a brief review of literature. Int J Surg Case Rep 2015;14:95–7. 10.1016/j.ijscr.2015.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coccolini F, Montori G, Catena F, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 2017;12:1–26. 10.1186/s13017-017-0151-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cengiz F, Yakan S, Enver İlhan. A rare cause of acute abdomen: splenic hematoma and rupture resulting from pancreatitis. Ulus Cerrahi Derg 2013;29:81–3. 10.5152/UCD.2013.20 [DOI] [PMC free article] [PubMed] [Google Scholar]