Abstract
Purpose:
To investigate the use of a system using electromagnetic tracking (EMT), post-processing and an error-detection algorithm for detecting errors and resolving uncertainties in high-dose-rate brachytherapy catheter digitization for treatment planning.
Methods:
EMT was used to localize 15 catheters inserted into a phantom using a stepwise acquisition technique. Five distinct acquisition experiments were performed. Noise associated with the acquisition was calculated. The dwell location configuration was extracted from the EMT data. A CT scan of the phantom was performed, and five distinct catheter digitization sessions were performed. No a priori registration of the CT scan coordinate system with the EMT coordinate system was performed. CT-based digitization was automatically extracted from the brachytherapy plan DICOM files (CT), and rigid registration was performed between EMT and CT dwell positions. EMT registration error was characterized in terms of the mean and maximum distance between corresponding EMT and CT dwell positions per catheter. An algorithm for error detection and identification was presented. Three types of errors were systematically simulated: swap of two catheter numbers, partial swap of catheter number identification for parts of the catheters (mix), and catheter-tip shift. Error-detection sensitivity (number of simulated scenarios correctly identified as containing an error/number of simulated scenarios containing an error) and specificity (number of scenarios correctly identified as not containing errors/number of correct scenarios) were calculated. Catheter identification sensitivity (number of catheters correctly identified as erroneous across all scenarios/number of erroneous catheters across all scenarios) and specificity (number of catheters correctly identified as correct across all scenarios/number of correct catheters across all scenarios) were calculated. The mean detected and identified shift was calculated.
Results:
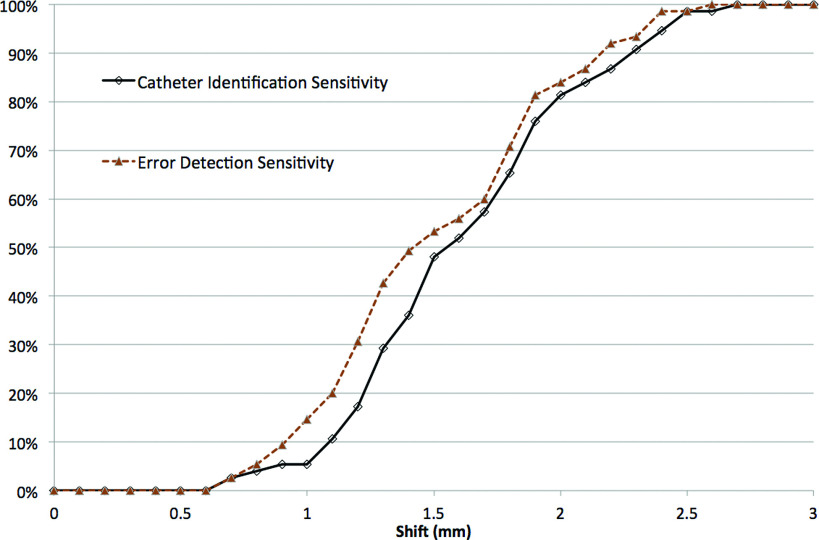
The maximum noise ±1 standard deviation associated with the EMT acquisitions was 1.0 ± 0.1 mm, and the mean noise was 0.6 ± 0.1 mm. Registration of all the EMT and CT dwell positions was associated with a mean catheter error of 0.6 ± 0.2 mm, a maximum catheter error of 0.9 ± 0.4 mm, a mean dwell error of 1.0 ± 0.3 mm, and a maximum dwell error of 1.3 ± 0.7 mm. Error detection and catheter identification sensitivity and specificity of 100% were observed for swap, mix and shift (≥2.6 mm for error detection; ≥2.7 mm for catheter identification) errors. A mean detected shift of 1.8 ± 0.4 mm and a mean identified shift of 1.9 ± 0.4 mm were observed.
Conclusions:
Registration of the EMT dwell positions to the CT dwell positions was possible with a residual mean error per catheter of 0.6 ± 0.2 mm and a maximum error for any dwell of 1.3 ± 0.7 mm. These low residual registration errors show that quality assurance of the general characteristics of the catheters and of possible errors affecting one specific dwell position is possible. The sensitivity and specificity of the catheter digitization verification algorithm was 100% for swap and mix errors and for shifts ≥2.6 mm. On average, shifts ≥1.8 mm were detected, and shifts ≥1.9 mm were detected and identified.
Keywords: brachytherapy, quality assurance, electromagnetic tracking
1. INTRODUCTION
In the practice of high-dose-rate (HDR) brachytherapy, a key component of the planning process is the digitization of the catheters.1–3 Digitizing catheters permits the planning system to calculate the locations available to the HDR source, called dwell positions. The dose distribution directly depends on the localization of the dwell positions. Digitization is usually performed manually and the procedure can be time consuming. The timeliness of the digitization process may become an issue when a patient awaits treatment and when many catheters need to be digitized. The catheters may not be clearly visible under some imaging modalities [e.g., MR (Ref. 4) or ultrasound5] resulting in uncertainty in catheter digitization. On CT, where clear visibility of catheters is expected, situations may occur where correct assignment of each catheter trace to the correct catheter number may be difficult or impossible. Even in perfect conditions and without time pressure, human error can result in erroneous catheter digitization, which is difficult to detect during plan verification.6
Electromagnetic tracking (EMT) has been proposed for a variety of radiotherapy applications.7–11 Validation of this technology for potential use in ultrasound-guided prostate HDR brachytherapy was recently discussed.3 While previous works offer insight into the utility of this technology,3,12–16 questions remain on the exact use of EMT for automatic catheter reconstruction and for quality assurance of catheter digitization. Previous work focused on the distance between baseline and EMT catheter tracks, while the distance between baseline and EMT-derived dwell positions is more relevant to HDR brachytherapy. The use of EMT technology for quality assurance of digitization has not been discussed previously. In this work, we demonstrate feasibility of an EMT acquisition technique, registration procedure, and digitization error-detection algorithm to permit EMT-assisted digitization brachytherapy quality assurance.
2. METHODS
A trackSTAR electromagnetic tracking system (Ascension Technologies, Shelburne, VT) was used for experiments in this work. The system was composed of a field emitter, an electronic unit, and two Model 90 sensors (0.9 mm outside diameter). matlab (The Mathworks, Natick, MA) was used for data processing and programming.
2.A. Phantom
A 175 × 170 × 155 mm plastic phantom was built with two identical template plates at two opposing ends for catheter insertion (Fig. 1). Fifteen ProGuide plastic catheters (Nucletron, an Elekta Company, Stockholm, Sweden) were inserted in the template. Nine catheters were inserted parallel to each other, from one template hole to the corresponding hole on the opposite template. Three pairs of catheters (one per clustered hole pattern, as shown in Fig. 1) were crossed inside the phantom by inserting them from a template hole to the holes corresponding to the other catheter’s insertion hole on the opposite template.
FIG. 1.

(A) Picture of the phantom filled with AGAR gel; (B) CT scan of the phantom showing the insertion template (an identical template is present on the opposite side, not shown). Insertion holes separation in the x direction was 5 mm for top left and bottom left hole pattern, and 3 mm for bottom right hole pattern. Insertion holes separation in the z direction was 5 mm for top left pattern, and 3 mm for bottom left hole pattern and for bottom right hole pattern. Three pairs of adjacent catheters [marked with an arrow in (B)] were crossed inside the phantom. Catheters visibility on CT is enhanced by the use of copper dummies.
2.B. EMT acquisition
Five distinct EMT acquisition experiments were performed by two users by manually driving a sensor into each catheter. A reference sensor attached to the phantom was used. An acquisition rate of 40 frames/s was used. All acquisitions were made from the tip of the catheter as the sensor was being extracted. The sensor wire used for acquisition was marked at 1 cm intervals. The sensor was retracted between steps, that is, from a mark to the next mark, where it was left for the duration of the step acquisition time. The EMT coordinate system was arbitrary, and no a priori registration of the EMT coordinate system with the CT coordinate system was performed.
A matlab routine was written to process the EMT data. The algorithm recognized points belonging to each step and averaged their positions. Acquired points in the transit between two steps were discarded. Acquisition time per step was calculated from the EMT data. EMT dwell positions were reconstructed through linear interpolation for each catheter, at fixed 5 mm distances along the EMT catheter track starting from the tip dwell location. Acquisition noise for a given catheter was defined as the standard deviation of the distances between acquired points and their centroid for all steps. The centroid is defined as the point with coordinates x, y, and z equal to the mean of the x, y, and z values of all acquired points in a given step. Noise in the x, y, and z directions was also reported. Mean and maximum noise values were reported.
2.C. EMT to CT registration
A CT scan of the phantom was acquired (slice thickness of 1.25 mm). Copper CT markers were used to increase catheter visibility. Five distinct catheter digitization sessions were performed by two users on the Oncentra Brachy treatment planning system (Nucletron, an Elekta Company). Dwell positions were calculated by the planning system with step size of 5 mm and automatically extracted from the DICOM plan with a matlab routine. Rigid registration of all corresponding dwell positions in the EMT and CT frame of reference was automatically performed through a dedicated matlab routine.17 Registration error was calculated by comparing all EMT-generated dwell positions against all dwell positions digitized manually on CT. The error was defined as the distance for the jth dwell position (j = 1, 2, …, Ndwi, with Ndwi being the total number of dwell positions in the ith catheter) in the ith catheter (i = 1, 2, …, Nc catheters, with Nc being total number of catheters) between the position found on CT (CTi,j) and the position found on the registered EMT acquisition ().
For each catheter i, the catheter error (CEi) was defined as
| (1) |
and the dwell error (DEi) was defined as
| (2) |
To describe registration errors as an aggregate of errors across all catheters, four definitions were used. The maximum catheter error (MCE) was defined as . Similarly, the maximum dwell error (MDE) was defined as . The catheter error can be interpreted as the error associated with the registration of a catheter as a whole, where the mean catheter error is the mean registration error of the catheters, and the maximum catheter error is the maximum registration error of any catheters. The dwell error can be interpreted as the error associated with the registration of the dwell positions, where the mean dwell error is the mean registration error of the dwell positions, and the maximum catheter error is the maximum registration error of any dwell position.
2.D. EMT for quality assurance of CT digitization
matlab routines were written to introduce three possible errors in the CT digitization: swap, mix and shift. The errors are represented in Fig. 2. In a swap error, two catheter numbers are swapped, resulting in an incorrect identification of the catheters. A swap can occur due to an error in digitization or due to a change in catheter labeling on the applicator or implant. In a mix error, two catheters are correctly identified by their associated catheter number at the connector end, but their numbers are switched from the location where the two catheters are the closest to each other up to the tip, resulting in a mix of the two catheters. A mix can occur due to the two catheters with sections in close proximity, where the catheter imaging artifacts cannot be resolved. This error possibility was taken into account in the design of the interstitial phantom, where three pairs of catheters cross paths. A mix can also occur due to human error on a clear image. In a shift error, a catheter is not digitized up to its tip or it is digitized past its tip. A shift can occur due to unclear visibility of the catheter tip on the images or due to human error. The routines were programmed to apply all possible combinations of swap and mix errors between any two catheters and all possible shifts from 0 to 3 mm in 0.1 mm increments. Simulations of mix errors were not restricted to the three pairs with crossed paths but were performed including all possible catheter pairs. The catheter pair proximity (smallest distance between any two dwell positions in the two catheters in the pair) ranged from 1.3 to 105 mm.
FIG. 2.
Exemplification of the three digitization errors introduced for systematic analysis: (A) swap; (B) mix; (C) shift.
A routine was written in matlab to detect the presence of an error and to identify the erroneous catheters. The algorithm is described in Fig. 3. Input parameters are the EMT coordinates and the CT digitization coordinates of all dwell positions in the N = 15 catheters. Starting from the full set of dwell positions, the algorithm performs a rigid registration of corresponding dwell positions and calculates the MCE and MDE between the registered EMT dwell positions (EMTr) and the CT dwell positions. If the MCE is equal to or less than the mean error threshold (AET) and the MDE is equal to or less than the maximum error threshold (MET), then no error is found in the CT digitization. Otherwise, all sets of k = 14, 13, …, 1 catheters of the 15 are registered sequentially, until a registration with errors less than or equal to the threshold is found. All catheters that have been excluded in order to obtain a registration lower than or equal to the threshold are marked as erroneously digitized.
FIG. 3.
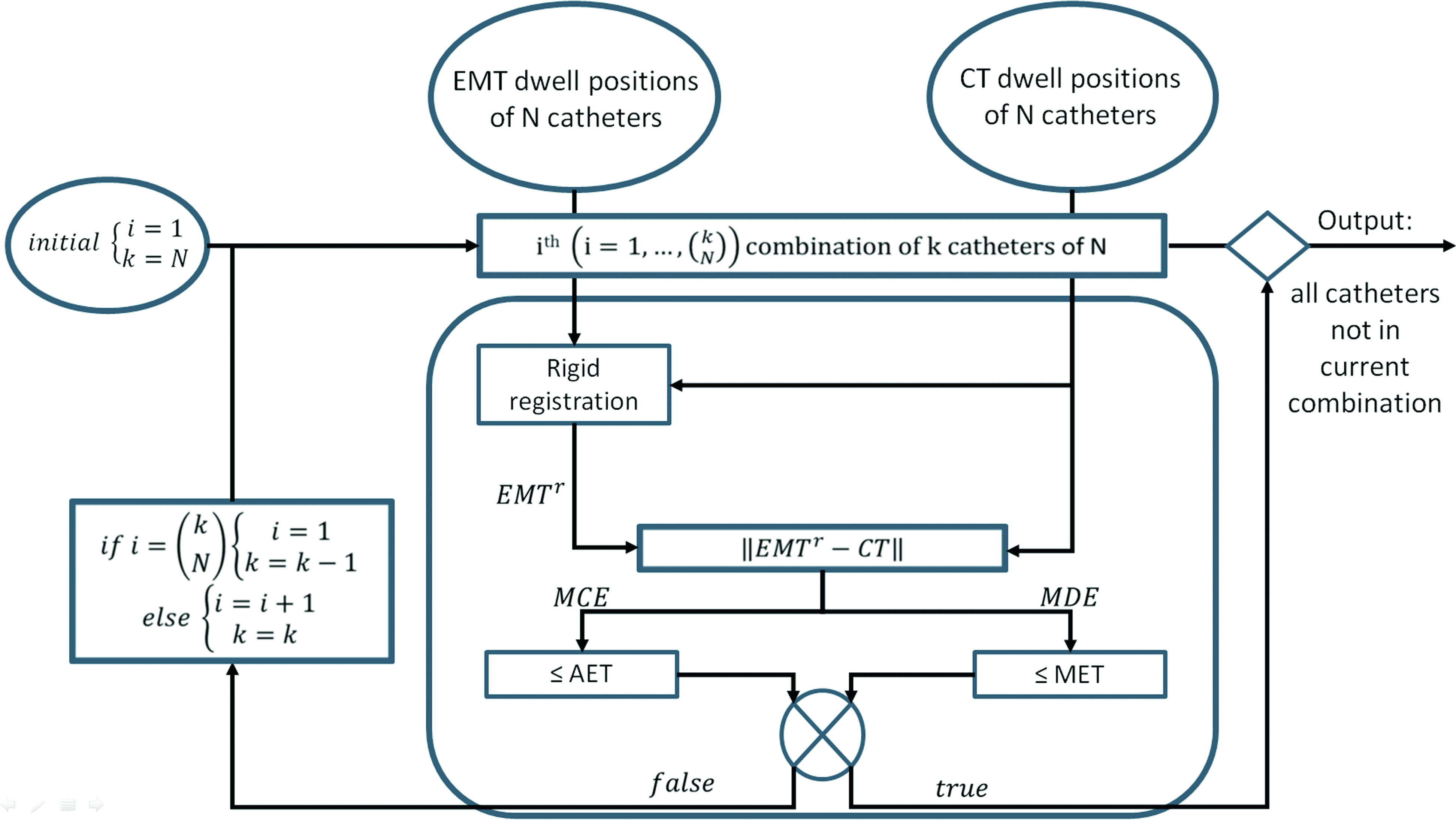
Flowchart of the algorithm for error detection and identification.
The error-detection sensitivity (number of simulated scenarios correctly identified as containing an error/number of simulated scenarios containing an error) and the error-detection specificity (number of scenarios correctly identified as not containing errors/number of correct scenarios) were calculated for AET ranging from 1 to 3 mm (in 0.25 mm increments) and MET ranging from 2 to 3.5 mm (in 0.5 mm increments). Optimal AET and MET values were identified as the smallest AET and MET ensuring an error-detection sensitivity and specificity of 100% calculated on scenarios composed of the first two acquisition/digitization “training” experiments (with no error, and with all swap and mix error combinations possible). The error-detection sensitivity and specificity, and the catheter identification sensitivity (number of catheters correctly identified as erroneous across all scenarios/number of erroneous catheters across all scenarios) and the catheter identification specificity (number of catheters correctly identified as correct across all scenarios/number of correct catheters across all scenarios) were calculated with optimal AET and MET for swap, mix and shift errors of the remaining three acquisition/digitization “validation” experiments. All five acquisitions and digitizations (training and validation) were performed using the same methodology, described in Secs. 2.B and 2.C. The mean detected and identified shift was also calculated.
3. RESULTS
3.A. EMT acquisition
The mean ±1 standard deviation of the mean time to acquire each EMT step per catheter was 4.7 ± 1.2 s, the maximum noise associated with a step was 1.0 ± 0.1 mm (x = 0.6 ± 0.3 mm; y = 1.2 ± 0.2 mm; z = 0.7 ± 0.4 mm), and the mean noise was 0.6 ± 0.1 mm (x = 0.3 ± 0.1 mm; y = 0.6 ± 0.1 mm; z = 0.3 ± 0.2 mm). Results per catheter are reported in Table I.
TABLE I.
Electromagnetic tracker stepwise acquisition time and noise. SD = standard deviation.
| Catheter number | Number of steps | Acquisition time per step (s) | Mean/maximum noise per step (mm) | |||
|---|---|---|---|---|---|---|
| x | y | z | Distance | |||
| 1 | 14.0 ± 0.0 | 5.6 ± 1.6 | 0.3 ± 0.1/0.5 ± 0.2 | 0.7 ± 0.1/0.9 ± 0.1 | 0.3 ± 0.1/0.5 ± 0.3 | 0.6 ± 0.1/0.8 ± 0.1 |
| 2 | 14.0 ± 0.0 | 5.2 ± 0.8 | 0.3 ± 0.1/0.5 ± 0.2 | 0.6 ± 0.2/0.8 ± 0.2 | 0.3 ± 0.2/0.5 ± 0.2 | 0.5 ± 0.1/0.7 ± 0.2 |
| 3 | 14.8 ± 0.8 | 4.8 ± 0.9 | 0.3 ± 0.1/0.4 ± 0.2 | 0.6 ± 0.1/0.8 ± 0.2 | 0.3 ± 0.1/0.5 ± 0.2 | 0.5 ± 0.1/0.7 ± 0.1 |
| 4 | 14.0 ± 0.0 | 4.8 ± 1.2 | 0.3 ± 0.1/0.4 ± 0.1 | 0.6 ± 0.1/0.8 ± 0.2 | 0.3 ± 0.1/0.5 ± 0.2 | 0.5 ± 0.1/0.7 ± 0.1 |
| 5 | 14.0 ± 0.0 | 4.4 ± 1.2 | 0.3 ± 0.1/0.4 ± 0.2 | 0.6 ± 0.1/0.9 ± 0.3 | 0.3 ± 0.2/0.5 ± 0.2 | 0.5 ± 0.1/0.7 ± 0.2 |
| 6 | 14.6 ± 0.5 | 4.4 ± 1.2 | 0.3 ± 0.1/0.4 ± 0.2 | 0.7 ± 0.1/1.0 ± 0.3 | 0.3 ± 0.1/0.5 ± 0.3 | 0.6 ± 0.1/0.9 ± 0.2 |
| 7 | 14.2 ± 0.4 | 4.4 ± 1.3 | 0.3 ± 0.1/0.4 ± 0.2 | 0.7 ± 0.1/0.9 ± 0.2 | 0.3 ± 0.1/0.5 ± 0.3 | 0.6 ± 0.1/0.7 ± 0.1 |
| 8 | 14.8 ± 0.4 | 4.6 ± 1.5 | 0.3 ± 0.1/0.4 ± 0.1 | 0.6 ± 0.1/0.9 ± 0.2 | 0.3 ± 0.1/0.5 ± 0.3 | 0.6 ± 0.1/0.8 ± 0.1 |
| 9 | 14.6 ± 0.5 | 4.4 ± 1.2 | 0.3 ± 0.1/0.5 ± 0.2 | 0.6 ± 0.1/0.8 ± 0.1 | 0.3 ± 0.1/0.5 ± 0.3 | 0.6 ± 0.1/0.7 ± 0.1 |
| 10 | 14.6 ± 0.5 | 4.4 ± 1.5 | 0.3 ± 0.1/0.4 ± 0.1 | 0.7 ± 0.1/0.9 ± 0.2 | 0.3 ± 0.1/0.4 ± 0.2 | 0.6 ± 0.1/0.7 ± 0.1 |
| 11 | 14.2 ± 0.4 | 4.6 ± 1.3 | 0.3 ± 0.2/0.5 ± 0.3 | 0.6 ± 0.1/0.9 ± 0.2 | 0.3 ± 0.2/0.5 ± 0.2 | 0.6 ± 0.1/0.7 ± 0.1 |
| 12 | 14.2 ± 0.8 | 4.6 ± 1.6 | 0.3 ± 0.1/0.4 ± 0.2 | 0.6 ± 0.1/0.8 ± 0.2 | 0.3 ± 0.2/0.4 ± 0.3 | 0.5 ± 0.1/0.7 ± 0.1 |
| 13 | 14.6 ± 0.5 | 4.4 ± 1.5 | 0.3 ± 0.1/0.5 ± 0.3 | 0.6 ± 0.2/0.8 ± 0.3 | 0.3 ± 0.2/0.5 ± 0.3 | 0.6 ± 0.1/0.7 ± 0.2 |
| 14 | 14.4 ± 0.5 | 4.6 ± 1.4 | 0.3 ± 0.2/0.4 ± 0.3 | 0.7 ± 0.2/0.9 ± 0.3 | 0.3 ± 0.2/0.6 ± 0.4 | 0.6 ± 0.1/0.8 ± 0.2 |
| 15 | 14.2 ± 0.4 | 4.8 ± 1.4 | 0.3 ± 0.1/0.4 ± 0.2 | 0.7 ± 0.2/0.9 ± 0.2 | 0.3 ± 0.2/0.5 ± 0.4 | 0.6 ± 0.1/0.8 ± 0.2 |
| Mean | 14.3 ± 0.2 | 4.7 ± 1.2 | 0.3 ± 0.1/0.4 ± 0.2 | 0.6 ± 0.1/0.9 ± 0.2 | 0.3 ± 0.2/0.5 ± 0.3 | 0.6 ± 0.1/0.7 ± 0.1 |
| SD | 0.5 ± 0.1 | 0.6 ± 0.2 | 0.0 ± 0.0/0.1 ± 0.0 | 0.0 ± 0.0/0.1 ± 0.0 | 0.0 ± 0.0/0.1 ± 0.1 | 0.0 ± 0.0/0.1 ± 0.0 |
| Minimum | 13.8 ± 0.4 | 4.0 ± 1.3 | 0.2 ± 0.1/0.3 ± 0.1 | 0.6 ± 0.1/0.7 ± 0.1 | 0.2 ± 0.1/0.3 ± 0.2 | 0.5 ± 0.1/0.6 ± 0.1 |
| Maximum | 15.2 ± 0.4 | 6.1 ± 1.2 | 0.3 ± 0.2/0.6 ± 0.3 | 0.7 ± 0.1/1.2 ± 0.2 | 0.4 ± 0.2/0.7 ± 0.4 | 0.6 ± 0.1/1.0 ± 0.1 |
3.B. EMT to CT registration
Registration of all EMT and CT dwell positions was associated with a mean catheter error of 0.6 ± 0.2 mm, a maximum catheter error of 0.9 ± 0.4 mm, a mean dwell error of 1.0 ± 0.3 mm, and a maximum dwell error of 1.3 ± 0.7 mm. The catheter error and dwell error for each catheter are represented in Fig. 4.
FIG. 4.
Registration errors as mean per catheter (catheter error) and as maximum error of the dwell positions in each catheter (dwell errors). Error bars denote the ±1 standard deviation across the five distinct EMT acquisition and catheter digitization experiments.
3.C. EMT for quality assurance of CT digitization
Optimal AET and MET, that is, the smallest AET and MET associated with error-detection sensitivity and specificity of 100% for all scenarios except shift errors derived from the first two acquisition/digitization experiments, were 1.5 and 2.5 mm, respectively. For swap and mix errors of the remaining three acquisition/digitization experiments, with optimal AET and MET, the error-detection and catheter-identification sensitivity and specificity was 100%. An error-detection sensitivity and specificity of 100% was observed for shifts ≥2.6 mm and a catheter identification sensitivity and specificity of 100% was observed for shifts ≥2.7 mm. Error-detection and catheter-identification sensitivity as a function of the shift size is shown in Fig. 5; error-detection specificity was 100% for all shifts, and catheter-identification specificity was 100% for all shifts ≥2.7 mm and >99.7% for all shifts. A mean detected shift of 1.8 ± 0.4 mm and a mean identified shift of 1.9 ± 0.4 mm were observed.
FIG. 5.
Catheter identification and error-detection sensitivity as a function of shift size. Error-detection specificity was 100% for all shift sizes, and catheter-identification specificity was 100% for shifts ≥2.7 mm and >99.7% for all shifts.
4. DISCUSSION
Without a priori registration of the EMT coordinate system with the CT coordinate system, we demonstrated the use of EMT for the quality assurance of catheter digitization for brachytherapy treatment planning. We presented an EMT acquisition technique with a mean noise of 0.6 mm and mean catheter registration error <1 mm. We developed an algorithm for the detection and identification of digitization errors and validated it through systematic simulations of three common types of error.
We reported a mean noise of 0.6 mm for our stepwise acquisition technique. Differences in equipment, acquisition technique, and calculation of noise do not allow for an exact comparison to reported noise in the literature. For instance, Zhou et al.3 reported a mean standard deviation of 1.0 mm (1.1 mm if interference from metallic objects is considered) for stationary measurements acquired with a trackSTAR system (600 samples at 40 Hz). Wagner et al.16 reported a standard deviation of 1.1 mm in the measurements acquired with a Polhemus Isotrac II (Polhemus, Inc., Colchester, VT) and Yaniv13 reported a standard deviation of 0.78 mm for an Aurora system (NDI, Waterloo, Canada) in a ferromagnetically clean environment. The mean noise of 0.6 mm in our analysis is low compared to those in the above-mentioned literature. The stepwise acquisition technique utilized in this work was designed to decrease the effect of the noise in the sensor readings. Postprocessing of the EMT raw data allowed for the averaging of each step while discarding more noise data from the transition between one step and the following one.
Localization accuracies <1 mm have been reported in the literature for various EMT systems.3,12,13,16 While our mean catheter error of 0.6 mm is in line with the literature, we also observed a mean maximum dwell error (±1 standard deviation across the five acquisitions) of 1.3 ± 0.7 mm. A maximum dwell error exceeding 1 mm is likely due to the joint effect of localization inaccuracy, noise in the measurement, and uncertainty in the localization of the dwell position in a CT with slice thickness of 1.25 mm. It is likely that the maximum localization inaccuracy of the EMT system was <1 mm. This result may suggest that EMT localization was more accurate than CT localization, and therefore should be preferred. Unfortunately, such an approach is not practical as it would require the EMT and the CT to share the same native coordinate system, thus bypassing the need for registration. Given the intrinsic uncertainties in catheter digitization on CT, a maximum registration error <2 mm suggests that excellent registration of the two coordinate systems was possible. This result was based on the registration of all dwell positions calculated based on EMT data and on manual digitization on CT. Prior knowledge of the CT digitization is required to perform this registration. This requirement is consistent with the scope of this work (quality assurance of catheter digitization); our results cannot be generalized to other uses of an EMT system, such as automatic digitization or navigation. The expansion of this work to these scenarios will be the topic of future work.
A topic broadly discussed in the literature is the effect of interference due to surrounding ferromagnetic equipment; all authors agree that greater error between EMT-acquired position and real position is observed in that scenario. This problem is unavoidable in applications requiring the use of EMT intraprocedure, where control over the surrounding equipment is limited. For quality assurance purposes, care should be taken to perform the measurement in an environment with as few sources of interference as possible. For the quality assurance of a surface applicator (e.g., facemasks), data acquisition can be done in a controlled environment. For interstitial applications, measurements should be acquired when the patient is not in close proximity to known sources of interference, e.g., while on a CT table.
We demonstrated that catheter digitization quality assurance with an EMT system and a dedicated error-detection algorithm is possible. Of the 44 medical events reported to the Nuclear Regulatory Commission between 1999 and 2012, 8 (20%) were associated with catheter reconstruction errors or misidentified first dwell positions.6 In a failure mode and effect (FMEA) analysis of HDR brachytherapy, Wilkinson6 identified five possible catheter reconstruction errors: wrong choice of top/connector end, mislabeling of catheters (swap error), incorrect indexer point (shift error), catheter length reconstruction errors, and inability to distinguish catheters that overlap (mix error). FMEA analysis found that of the six possible errors associated with the highest risk priority number, three were catheter reconstruction errors. In his analysis, it was noted that catheter reconstruction errors are in general associated with a detectability rating of “unlikely” to “highly unlikely.” This result is justified by the difficulty of performing quality assurance of catheter digitization manually. The use of EMT has the potential to drastically improve the detectability of digitization errors.
In this work, the tolerance levels used in the algorithm were found by optimization based on acceptable values of sensitivity and specificity (100% in the present work) on two training experiments; validation was then performed on three validation experiments. Alternatively, users may opt to select the tolerance levels based on the calculation of receiver operating characteristic (ROC) curves. Given the presence of two threshold parameters in the algorithm, the interpretation of multiparameter ROC curves may not be straightforward.
Although our analysis focused on swap, shift, and mix errors, any error in digitization resulting in one or more catheters presenting with a registration error exceeding the tolerance would result in the detection of an error. Moreover, the use of EMT for quality assurance can be expanded to the verification of catheter length measurement, which is a known source of medical events.6 Similarly, the use of this technology for the detection and evaluation of implant displacements and deformations will be explored.18 The main limitation of this approach is that systematic digitization errors may not be detectable. For instance, a digitization error affecting all catheters due to the use of incorrect dummies or to lack of training may not be detected by our methodology.
5. CONCLUSION
We demonstrated that EMT can be used to assist in catheter digitization quality assurance. We presented an EMT acquisition technique with a mean noise of 0.6 mm, which was used to reconstruct the dwell positions in the EMT frame of reference. Dwell positions in the CT frame of reference were calculated by our clinical planning system based on manual digitization performed by a qualified medical physicist specialized in HDR brachytherapy. Registration of the EMT dwell positions to the CT dwell positions was possible with a residual mean error per catheter of 0.6 mm. These low residual registration errors show that quality assurance of the general characteristics of the catheters and of possible errors affecting one specific dwell position is possible. We developed an algorithm for the detection and identification of digitization errors and validated it through a systematic introduction of three kinds of digitization errors (swap of two catheters, mix between two catheters, and shift of a catheter). All swap and mix errors were detected and identified. Error-detection sensitivity of 100% was observed for shifts ≥2.6 mm. On average, shifts ≥1.8 mm were detected, and shifts ≥1.9 mm were detected and identified.
ACKNOWLEDGMENTS
The authors would like to thank Barbara Silver for reviewing this paper. This work was funded by Kaye Family Award. The authors report no conflicts of interest in conducting the research.
REFERENCES
- 1.Kirisits C. et al. , “Review of clinical brachytherapy uncertainties: Analysis guidelines of GEC-ESTRO and the AAPM,” Radiother. Oncol. 110(1), 199–212 (2014). 10.1016/j.radonc.2013.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Awunor O. A., Dixon B., and Walker C., “Direct reconstruction and associated uncertainties of 192 Ir source dwell positions in ring applicators using gafchromic film in the treatment planning of HDR brachytherapy cervix patients,” Phys. Med. Biol. 58(10), 3207–3225 (2013). 10.1088/0031-9155/58/10/3207 [DOI] [PubMed] [Google Scholar]
- 3.Zhou J., Sebastian E., Mangona V., and Yan D., “Real-time catheter tracking for high-dose-rate prostate brachytherapy using an electromagnetic 3D-guidance device: A preliminary performance study,” Med. Phys. 40(2), 021716 (8pp.) (2013). 10.1118/1.4788641 [DOI] [PubMed] [Google Scholar]
- 4.Kapur T., Egger J., Damato A., Schmidt E. J., and Viswanathan A. N., “3-T MR-guided brachytherapy for gynecologic malignancies,” Magn. Reson. Imaging 30(9), 1279–1290 (2012). 10.1016/j.mri.2012.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmid M. et al. , “A phantom study to assess accuracy of needle identification in real-time planning of ultrasound-guided high-dose-rate prostate implants,” Brachytherapy 12(1), 56–64 (2013). 10.1016/j.brachy.2012.03.002 [DOI] [PubMed] [Google Scholar]
- 6.Wilkinson D. A. and Kolar M. D., “Failure modes and effects analysis applied to high-dose-rate brachytherapy treatment planning,” Brachytherapy 12(4), 382–386 (2013). 10.1016/j.brachy.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 7.Keall P. J. et al. , “The first clinical implementation of electromagnetic transponder-guided MLC tracking,” Med. Phys. 41(2), 020702 (5pp.) (2014). 10.1118/1.4862509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang P., Hunt M., Happersett L., Yang J., Zelefsky M., and Mageras G., “Robust plan optimization for electromagnetic transponder guided hypo-fractionated prostate treatment using volumetric modulated arc therapy,” Phys. Med. Biol. 58(21), 7803–7813 (2013). 10.1088/0031-9155/58/21/7803 [DOI] [PubMed] [Google Scholar]
- 9.Fast M. F., Wisotzky E., Oelfke U., and Nill S., “Actively triggered 4d cone-beam CT acquisition,” Med. Phys. 40(9), 091909 (14pp.) (2013). 10.1118/1.4817479 [DOI] [PubMed] [Google Scholar]
- 10.Litzenberg D. W. et al. , “A measurement technique to determine the calibration accuracy of an electromagnetic tracking system to radiation isocenter,” Med. Phys. 40(8), 081711 (8pp.) (2013). 10.1118/1.4813910 [DOI] [PubMed] [Google Scholar]
- 11.Lin Y., Liu T., Yang X., Wang Y., and Khan M. K., “Respiratory-induced prostate motion using wavelet decomposition of the real-time electromagnetic tracking signal,” Int. J. Radiat. Oncol., Biol., Phys. 87(2), 370–374 (2013). 10.1016/j.ijrobp.2013.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hummel J., Figl M., Kollmann C., Bergmann H., and Birkfellner W., “Evaluation of a miniature electromagnetic position tracker,” Med. Phys. 29(10), 2205–2212 (2002). 10.1118/1.1508377 [DOI] [PubMed] [Google Scholar]
- 13.Yaniv Z., Wilson E., Lindisch D., and Cleary K., “Electromagnetic tracking in the clinical environment,” Med. Phys. 36(3), 876–892 (2009). 10.1118/1.3075829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hagedorn J. G., Satterfield S. G., Kelso J. T., Austin W., Terrill J. E., and Peskin A. P., “Correction of location and orientation errors in electromagnetic motion tracking,” Presence-Teleop. Virt. 16(4), 352–366 (2007). 10.1162/pres.16.4.352 [DOI] [Google Scholar]
- 15.Bo L. E., Leira H. O., Tangen G. A., Hofstad E. F., Amundsen T., and Lango T., “Accuracy of electromagnetic tracking with a prototype field generator in an interventional OR setting,” Med. Phys. 39(1), 399–406 (2012). 10.1118/1.3666768 [DOI] [PubMed] [Google Scholar]
- 16.Wagner A. et al. , “Quantitative analysis of factors affecting intraoperative precision and stability of optoelectronic and electromagnetic tracking systems,” Med. Phys. 29(5), 905–912 (2002). 10.1118/1.1469625 [DOI] [PubMed] [Google Scholar]
- 17.Horn B. K., “Closed-form solution of absolute orientation using unit quaternions,” J. Opt. Soc. Am. A 4(4), 629–642 (1987). 10.1364/JOSAA.4.000629 [DOI] [Google Scholar]
- 18.Damato A. L., Cormack R. A., and Viswanathan A. N., “Characterization of implant displacement and deformation in gynecologic interstitial brachytherapy,” Brachytherapy 13(1), 100–109 (2014). 10.1016/j.brachy.2013.09.010 [DOI] [PubMed] [Google Scholar]