Abstract
Existing research suggests that approximately 19% of females experience childhood sexual trauma (CST). Little is known, however, about the parenting behaviour of mothers who have experienced CST. Using propensity-matched controls, the present study examines prenatal psychosocial distress, postnatal depressive symptomatology, and caregiving behaviours of women reporting CST at or before the age of 14. Data for these analyses were obtained from mother reports and from observational protocols from a longitudinal study of low-income, rural families. Propensity score methodology was used to create a contrast group matched on family of origin variables in an effort to isolate and examine the long-term associations of CST beyond the effects of other childhood adversities such as poverty. Study findings provide evidence that women with CST histories report greater prenatal psychosocial distress compared to women without trauma histories. Findings further provide evidence for a spillover process from prenatal distress to the broader caregiving system including less sensitive parenting through postnatal depressive symptoms for women with CST histories. These results highlight the importance of screening for CST and psychosocial distress and depression prenatally. Interventions for women with CST histories and directions for future study are proposed.
Keywords: childhood sexual trauma, sensitive parenting, prenatal distress, postnatal depression, propensity matched design
Current estimates suggest that approximately 19% of women report a history of childhood sexual trauma (CST) (Pereda, Guilera, Forns, & Gómez-Benito, 2009). The consequences of CST are profound and long lasting (Putnam, 2003). Not only does the victim of abuse suffer as a child, there is mounting evidence that a history of sexual violence during childhood places subsequent generations at risk for maladaptive developmental outcomes (DiLillo, Tremblay, & Peterson, 2000; Roberts, O’Connor, Dunn, & Golding, 2004). Prior research links CST history with numerous domains of adult interpersonal functioning, including elevated depression with some reports suggesting a four times greater lifetime risk of developing major depression, and significant difficulties with parenting (Banyard, Williams, & Siegel, 2003).
The effects of such early traumas may be particularly salient during periods of stress and transition. Pregnancy represents a vulnerable time for many mothers with a considerable number of pregnant women reporting increases in negative mood and distress during the prenatal period (Bennett, Einarson, Taddio, Koren, & Einarson, 2004). During this time, women are particularly susceptible to stress, given the number of major physical, emotional, social, and practical life changes they face. Research has found that negative life events (e.g. serious family problems, death of a relative) are associated with increased risk of premature birth, low birth weight, and emotional distress in the mother (Glazier, Elgar, Goel, & Holzapfel, 2004). Given the high prevalence of CST, it is likely that a substantial proportion of pregnant women have been victims of sexual trauma in childhood. Despite the significant literature addressing CST and adult functioning, there is little information available as to how prior trauma history might be associated with psychosocial functioning in pregnancy. Even less information is available on how these prenatal factors may be related to early parenting among mothers reporting a history of CST.
In addition, a substantial literature has identified the early postpartum period as particularly important in laying the groundwork for optimal mother–child relationships. Mothers struggling with postpartum depression and related symptomatology may find responding with sensitivity to infant signals for care to be especially challenging. Sensitive parenting, which involves consistent and appropriate responding to infant cues and distress, is important for promoting young children’s abilities to regulate their emotions and form secure attachment relationships (Mark, IJzendoorn, & Bakermans-Kranenburg, 2002). Although a growing literature notes that women with CST report significantly higher depressive symptoms in the postpartum period (Buist & Janson, 2001; Leeners, Richter-Appelt, Imthurn, & Rath, 2006), the association between CST, postpartum depressive symptoms and early parenting behaviour is not well understood.
Childhood Sexual Trauma and Subsequent Parenting Behaviours
The ways in which parents interact with children has been linked to child adjustment in multiple domains, as well as to the development and maintenance of psychopathology (Cassidy, 2008). Reviews of the childrearing literature have identified a parent’s ability to provide emotional nurturance and warmth, referred to as parent sensitivity, as a key mediating process linking parenting behaviour to optimal child development (Cox & Harter, 2003; Grolnick, Gurland, DeCourcey, & Jacob, 2002). Maternal sensitivity is the ability to recognize and respond both effectively and promptly to the distress and needs of one’s child (Cox & Harter, 2003). Parenting during infancy and early childhood has been shown to be particularly important for children’s functioning, with significant implications for children’s later development (Maccoby, 2001).
Numerous reports targeting the parenting of women with CST histories note that mothers with CST histories compared to mothers without trauma histories report greater stress from the demands of parenting and discomfort with the emotional demands of motherhood (DiLillo & Damashek, 2003). Douglas (2000) found that women who had experienced CST reported being significantly more anxious about the intimate aspects of parenting their children than did women without CST histories. Alexander, Teti, and Anderson (2000) reported that sexually abused mothers were more self-focused (as opposed to child-focused) in their interactions with children, and that they relied more heavily than nonabused mothers upon their own children for emotional support (Alexander et al., 2000). Further, Zvara, Mills-Koonce, Carmody, Cox, and Family Life Project Key Investigators (2015) using observational assessments of parenting behaviour reported that females who experienced CST showed poorer functioning across multiple domains of parenting including sensitivity (Zvara et al., 2015). This growing body of work highlights that women with CST histories experience some degree of difficulty with the emotional demands involved in child rearing and may be a significant pathway by which maternal history of CST exerts itself across time to impact the development of subsequent generations.
Pathways to Parenting for Women with CST Histories
Although the collective body of literature highlights numerous parenting difficulties experienced by adult survivors of CST, more recent work has attempted to find explanatory mechanisms that link CST and adulthood parenting. Thus far, much of this work has been related to explicating factors in the early years of parenting that may predict the caregiving behaviour of mothers with CST histories. For example, Schuetze and Eiden (2005) found that maternal depression mediated the relation between CST and parenting outcomes in toddlerhood and early childhood. DiLillo et al. (2000) reported a significant association between CST and subsequent punitive parenting practices that was mediated by maternal anger (DiLillo et al., 2000).
Understanding the mechanisms through which contextual factors (i.e. CST, prenatal distress) influence parenting behaviour of mothers with CST histories may be integral to understanding the intergenerational transmission of childhood trauma. One promising mechanism is the stress/distress spillover process, which has been explored primarily in the marital conflict literature. Stress/distress spillover would occur when stressful events or circumstances from outside the parenting domain (e.g. distress from family problems, negative life events) engender a negative affective response that continues while the parent is interacting with children (Brock & Lawrence, 2008; Östberg & Hagekull, 2000). Given the significant number of CST survivors who report elevated distress and depressive symptoms across the lifespan, including during pregnancy (Douglas, 2000), examining prenatal factors may provide important information in our understanding of the parenting difficulties of women with trauma histories.
Prenatal psychosocial distress
The past decade has seen increased interest in the role of maternal psychosocial distress during pregnancy to the wellbeing of the mother and development of offspring (For a review, see Graignic-Philippe, Dayan, Chokron, Jacquet, & Tordjman, 2014). Studies examining the effects of maternal parental distress suggest associations with complications with pregnancy, including preterm delivery and postpartum depression (Verkerk, Pop, Van Son, & Van Heck, 2003) which in turn has been linked to impaired mother–infant interactions (Field, 2010). Despite growing support for the role of the prenatal period in the long-term health and wellbeing of the mother and child, there is very little information regarding the psychological wellbeing of CST survivors during pregnancy (Jacobs, 1992; Leeners et al., 2006). The handful of studies examining the linkages between CST history and prenatal distress support a positive and statistically significant association between maternal history of CST and prenatal depressive symptoms (see Wosu, Gelaye, & Williams, 2015, for a review).
There are theoretical reasons to expect that women with CST histories may experience numerous psychosocial difficulties during pregnancy related to their trauma experience. First, a significant literature highlights that depression and distress are two of the most commonly occurring and well-established outcomes for adult female survivors of CST (see reviews by Paolucci, Genuis, & Violato, 2001). The rapid physical and emotional changes during pregnancy could exacerbate or trigger onset of psychopathology in the presence of existing vulnerability such as CST history (Monroe & Simons, 1991). Second, pregnancy and motherhood involve role transitions where early traumatic memories from childhood may likely resurface (Wright, Fopma-Loy, & Oberle, 2012). Becoming a parent could activate cognitive and emotional responses related to adverse childhood experiences, including CST (Kendall-Tackett, 2007; Leeners et al., 2006).
Postnatal depressive symptomology
Numerous reports highlight the comorbid nature of prenatal distress and postpartum depressive symptomology with a significant number of women with postpartum depressive symptoms reporting prenatal distress (Robertson, Grace, Wallington, & Stewart, 2004). These associations may be especially relevant for women with histories of CST given the number of women with CST histories who report depressive symptomatology across the lifespan at higher rates than women without a history of CST (Paolucci et al., 2001; Putnam, 2003).
Over the past two decades several reports have linked a history of CST to elevated rates of postpartum depressive symptoms. Buist and Janson (2001) showed that among women with major depressive episodes in the postpartum period, those with a history of childhood abuse had significantly higher depressive symptoms. Leeners et al. (2006) reported that perinatal women who reported CST were at higher risk for postpartum depressive symptoms compared to women without CST histories. Depressive symptoms are believed to limit a mother’s capacity to engage positively with her infant (Murray et al., 2010) and have been identified as powerful risk factors for a variety of negative developmental outcomes in children (Milne, Greenway, Guedeney, & Larroque, 2009; Tronick & Reck, 2009; Murray et al., 2010).
It is likely that mothers struggling with or preoccupied by distressing thoughts and feelings associated with CST may be less able to respond appropriately to their child’s bid for attention and care (Anthony et al., 2005). Such findings would suggest a contextual cascade in which abuse history is related to prenatal psychosocial distress to postnatal depressive symptoms, which in turn are related to responsive parenting behaviour. However, little empirical evidence has examined such an extensive longitudinal model. While there is considerable interest on the long-term sequela of CST, much of what we know about the effects of maternal trauma on the development of offspring comes from small, cross-sectional studies of at-risk samples. Additional limitations of previous research on the long-term effects of CST include the absence of control groups or the use of control groups with different characteristics which can create problems in terms of comparability between groups (DiLillo, 2001).
Combining the growing literature linking prenatal distress to child adjustment with the considerable literature highlighting the importance of the early caregiving environment to subsequent infant and child development (i.e. maternal depressive symptoms, parenting), along with the elevated rates of depressive symptomatology and parenting problems for women with CST histories, it becomes important to better understand the associations between prenatal distress, postnatal depressive symptoms, and parenting, and the role that CST plays in these associations. Although the literature addressing CST and adult functioning is growing, there is little information available as to how prior CST might be associated with psychosocial functioning (i.e. depressive symptoms, and distress) in pregnancy and the transition to early parenthood. Zvara et al. (2015) reported that mothers with CST histories differed from mothers with no trauma history in their interactions with their young children at age 5. Understanding emerging parenting behaviours for women with CST histories at the earliest ages has important implications for the development of targeted intervention protocols.
CURRENT STUDY
The present study examines the relations between maternal history of CST and early parenting behaviour, and the role of prenatal psychosocial distress, and postnatal depressive symptoms to these associations. Although past research has provided suggestive evidence to support this model, this study is, to the best of our knowledge, the first to explicitly test a meditational pathway from CST and early parenting behaviours through prenatal distress and postnatal depressive symptoms using a propensity matched design.
Our conceptualization for this current study was based on previous research reporting elevated rates of lifetime depression for CST survivors and the literature highlighting the effect of prenatal distress and depression on the early caregiving environment. Importantly, women in general are screened for numerous conditions during the prenatal period such as gestational diabetes and hypertension, which are far less common in pregnancy than depression and other forms of psychiatric illness (Gavin, Gaynes, Lohr, Meltzer-Brody, Gartlehner, & Swinson, 2005). Thus, although women may experience any number of complications in pregnancy, for this study, we focused on the psychosocial distress of CST survivors.
In the current analysis, we focused on CST as compared to child maltreatment more broadly (i.e. physical abuse, neglect) given previous reports suggesting a unique effect of CST on subsequent parenting behaviours. For example, in their study of infant attachment patterns of mothers with childhood experiences of physical or sexual abuse, Lyons-Ruth and Block (147) found that the strongest correlate of affective withdrawal (less empathy and decreased nurturance for the infant) was the severity of CST. Additional work by Bailey, DeOliveira, Wolfe, Evans, and Hartwick (2012) found that childhood sexual abuse history was associated with parenting competence above and beyond the effects of other forms of childhood maltreatment (Bailey et al., 2012). Further, given the elevated rates of depression and depressive symptoms reported by adult CST survivors, and given the limited research on the impact of CST on prenatal distress for women with sexual trauma histories, the current study focuses on the psychosocial factors in pregnancy that may be related to subsequent parenting behaviours.
Given previous findings suggesting that depressed mothers are emotionally less sensitive and attuned to their infant’s cues, we examined the parenting domain of sensitivity. We hypothesized that many of the characteristics associated with depressive symptoms such as being emotionally unavailable, detached, and withdrawn could be important in understanding the parenting difficulties of mothers with depressive symptoms (see review by, Lovejoy, Graczyk, O’Hare, & Neuman, 2000). This may be especially relevant when studying the parenting behaviour of mothers with CST histories because they may be struggling with their own regulatory processes and thereby less responsive to their children’s bids compared to mothers without trauma history.
Towards this end, the present study forwards three hypotheses concerning associations between CST and sensitive parenting behaviours at child age 15 months. First, we hypothesize that a history of CST will be related to lower levels of sensitive parenting in parent–child interactions. Second, based on extant research suggesting that women with CST histories are at risk for mental health problems across the lifespan, we further hypothesize that mothers with CST histories would report greater prenatal psychosocial distress and postpartum depressive symptoms than women without sexual trauma histories. Last, given findings linking depressive symptoms to parenting behaviour we hypothesize prenatal psychosocial distress and postpartum depressive symptoms would be two key mechanisms by which CST is related to parenting behaviour even when controlling for sociodemographic factors.
Importantly, although there has been some discussion in the literature regarding the validity of retrospective accounts of prenatal experiences, in the absence of data on psychosocial functioning measured during pregnancy, retrospective reports from mothers shortly after the birth of their child may be the next best alternative to measure prenatal psychosocial distress (Reich, Todd, Joyner, Neuman, & Heath, 2003). Prior research supports this view. Tomeo et al. (1999) reported that pregnancy appears to be a salient enough event that maternal recall of many factors is both reproducible and accurate many years after delivery. Further, in their study examining agreement between maternally reported questionnaires and medical records for a range of pre- and postnatal factors, Reich et al. (2003) and Rice et al. (2007) found that mothers in their study provided accurate reports in comparison to information from medical records.
METHOD
Sample
The sample for the current study is drawn from the Family Life Project (FLP), a longitudinal, multi-method, multi-respondent study of rural poverty that explores the ways in which child, family, and contextual factors shape child development over time. FLP employed complex sampling procedures to recruit a representative sample in three target counties in eastern North Carolina and three target counties in central Pennsylvania. Mothers were recruited in the hospital the day after giving birth. A total of 1292 families enrolled in the FLP by completing the first home visit when the family’s infant was two months old. Subsequent home visits occurred at 6m, 15m, 24m, 35m, 48m, 60m, and first grade. Additional data collection is underway. Of the 1292 families initially recruited for participation in the study, 144 biological mothers reported through a questionnaire assessment that they had experienced CST at or before the age of 14. In the current study, we focus on women who experienced trauma in the early childhood years given findings suggesting that when the trauma occurs to young children, they may have less refined coping strategies and less ability to control their environments, which may lead to feelings of helplessness (Roth & Lebowitz, 1988). Others suggest that when the abuse occurs during the early years in which identity and cognitive schemas about self and others are developing, the trauma may become a part of the victim’s internal representations of the self and self in relation to others (Toth, Maughan, Manly, Spagnola, & Cicchetti, 2002).
Using propensity score matching (PSM) procedures, a contrast group was created based on carefully chosen covariates (the procedures for the propensity matching are described in greater detail in the analysis plan). The selection of the covariates was based on prior research that identified factors such as household income and parental education as risk factors for CST (Butler, 2013). In addition, early work by Finkelhor (1993) noted that a disproportionate number of CST cases reported to Child Protective Services come from families in the lower socioeconomic classes. Furthermore, there is some debate in the literature about whether it is CST per se that affects the long-term interpersonal problems of adult victims or whether these mental health and parenting problems are related to a general level of family risk that allowed the trauma to occur in the first place (Courtois, 1992; Kendall-Tackett, 2002). Thus, by controlling for early life risk factors, we attempt to isolate the effects of childhood trauma above and beyond the effects of family of origin and other traumas experienced in childhood. Further, we used covariates from the family of origin as matching variables rather than concurrent demographic variables given research suggesting that women with trauma histories may be less likely to be educated, have less income, both of which have been identified as important correlates of parenting (see Conger, Conger, & Martin, 2010, for a review). Women who experienced CST (as assessed by the Trauma History Questionnaire (THQ), Green, 1996) were matched on mothers’ childhood demographic variables to a group of women (controls) who have not experienced CST (n=204). This subsample has been previously validated in published work by Zvara et al. (2015).
Procedures
Trained research assistants collected all data during home visits. All caregivers reading at the 8th grade level or above independently completed the questionnaires, while those reading below the 8th grade level had the questionnaires read to them by research assistants. Primary caregiver literacy was obtained through administration of the K-FAST (Kaufman & Kaufman, 1994) at the 2-month home visit. At each visit, caregivers completed questionnaires regarding demographic variables, as well as questionnaires relating to child behaviour, relationship quality, and parenting.
The data for the proposed study were collected at varying waves of data collection. The covariates for the matching procedure were drawn from the 2-month interview. The trauma history data were collected at two different time points, either at the 36- or 60-month visit depending on time restrictions for the visit. Mothers only completed the trauma questionnaire once. At the 6-month and 15-month visits, in addition to completing questionnaires, the primary caregiver and the child were video recorded in a 10-min dyadic free play activity. A team of coders scored the digital recordings for caregiver behaviour.
Measures
Trauma History Questionnaire
Participants completed the THQ (Green, 1996), a 24-item self-report measure that examines experiences with potentially traumatic events, such as crime, general disaster, and sexual and physical assault, using a yes/no format. For each event endorsed, respondents were asked to provide the frequency of the event, their age at the time the event occurred, and the nature of their relationship with the abuser. For the purposes of the proposed study, the item relating to sexual abuse/assault asked, ‘Has anyone ever done something sexual to you against your will, such as made you have intercourse, oral or anal sex, touched private parts of your body, or made you touch theirs, or otherwise forced you to have unwanted sexual contact?’ If answered yes, follow-up questions asked about the age at the time of the sexual trauma, frequency, and relationship of the victim to the perpetrator. The trauma history data were collected at two different time points, either the 36 visit or the 60 month visit depending on time restrictions for the visit. The subsample of women who reported experiencing sexual trauma at or before the age of 14 was used in this analysis.
Mothers’ family of origin information
The variables for the PSM were drawn from the 2-, 36-, and 60-month interviews. At the 2-month interview, mothers were asked if when they were growing up (aged 0–18) any family members with whom they lived received Aid to Families with Dependent Children (AFDC), food stamps, or Medicaid or lived in public housing. They were also asked the highest grade completed by the primary mother-figure that was in their childhood home, with the scale ranging from 0 =no school to 22=PhD, where values 0–11 indicate highest grade level completed, and values 12–22 include milestones such as obtaining a Graduate Equivalency Diploma (GED) (12), graduating from high school (14), completing a four year college degree (18), and obtaining a PhD (22). From either the 36- or 60-month interview additional non-sexual traumas experienced in childhood (e.g. being mugged or beaten, experiencing natural disasters such as tornadoes or hurricanes) were also used in the matching procedure (i.e. THQ, Green, 1996).
Prenatal psychosocial distress
At the 2-month home visit, mothers completed the perinatal module of the Missouri Assessment of Genetics Interview for Children (MAGIC). This interview is based on the Diagnostic Interview for Children and Adolescents (DICA; Reich, 2000). The parent version of the MAGIC has a section that asks perinatal questions regarding complications in pregnancy. Mothers reported with either a ‘No’ or ‘Yes’ to ‘did you have any complications of pregnancy with this child, such as’: ‘serious family problems which were upsetting to you’ and ‘excessive nausea/vomiting lasting more than 3 months.’ The full set of questions can be found in the table reporting the factor structure (Table 1). Cronbach’s alpha was .67.
Table 1.
Summary of exploratory factor analysis results for maternal report of pregnancy complications (N= 204)
| Item | Factor 1 | Factor loadings Factor 2 |
Factor 3 |
|---|---|---|---|
| 1. Serious family problems | .809 | .164 | −.131 |
| 2. Other illness | .604 | .141 | |
| 3. Emotional problems | .599 | .162 | |
| 4. Happy about pregnancy | −.412 | .106 | −.188 |
| 5. Convulsions | −.221 | .170 | |
| 6. High blood pressure | .676 | .192 | |
| 7. Serious accidents | .127 | .554 | |
| 8. Water retention | .209 | .535 | |
| 9. Excessive nausea | .258 | .713 | |
| 10. Weight loss over 10 lbs | .340 | .521 | |
| 11. Was surprised to be pregnant | −.254 | .446 | |
| 12. Serious infection | .408 | ||
| 13. Heavy bleeding | .143 | −.376 | .401 |
Note: Factor loadings over .40 appear in bold.
Postnatal depressive symptoms
Primary caregivers’ self-reported depressive symptoms were obtained using the Brief Symptoms Inventory (BSI-18, Derogatis, 2000) at the 6-month visit. The BSI-18 is a brief and highly sensitive screening index containing 18 items. Respondents were asked to rate on a 4-point Likert-type scale (where 0 =not at all and 4 =extremely) how distressed they were by each symptom over the past seven days. The mean of the measure’s six-item depression subscale was used in the proposed study. An example item reads ‘[how much were you distressed by]’ ‘feeling blue’ and ‘feeling hopeless about the future.’ Cronbach’s alpha was .81 for depression in the FLP at 6 months.
Observed maternal parenting behaviours
At the 6- and 15-month home visit, mothers were instructed to interact with their children as they typically would if given some free time during the day. All interactions lasted 10 min and were video recorded for later coding by an ethnically diverse team of coders who were blind to other information about the families. Using six global rating scales (Cox & Crnic, 2002: sensitivity/responsiveness, detachment/disengagement, intrusiveness, stimulation of cognitive development, positive regard, negative regard) adapted from those used by the National Institute for Child Health and Human Development Study of Early Child Care (NICHD ECCRN, 1999), coders rated parenting behaviours on a 5-point scale (on which 1= not at all characteristic and 5 =very characteristic). Both frequency and intensity of behaviour or affect towards the child were considered. The sensitivity/responsiveness scale, adapted from Ainsworth, Blehar, Waters, and Wall (1978), describes the degree to which the parent was aware of and responsive to the child’s bids and signals for attention and achieved synchrony with the child. The detachment/disengagement scale describes the degree to which the parent was emotionally distant, uninvolved, or unaware of the child’s signals or needs for appropriate facilitation or care. The stimulation of cognitive development scale measures the degree to which the parent engaged in age-appropriate behaviours that foster cognitive and physical development of the child. The positive regard scale rates the quantity and intensity of the parent’s expression of positive feelings towards the child, including praise, smiling, physical affection, playful behaviour, and overall enjoyment. The intrusiveness scale rates the parent’s respect for the child as an individual and the extent to which the parent understands and recognizes the child’s effort to gain autonomy and self-awareness. The negative regard scale rates the parent’s negative affect for the child including disapproving, harsh, or hostile vocalizations or facial expressions.
Coders underwent training until acceptable reliability (ICC>.80) was achieved and maintained for each coder on every scale. Once acceptable reliability was established, coders began coding in pairs while continuing to code at least 20% of their weekly cases with a criterion coder. Reliability was based on the independent scores of coders. Each coding pair met biweekly to reconcile scoring discrepancies; the final consensus scores were used in all analyses.
To inform compositing of variables, exploratory factor analysis was conducted with an oblique rotation (i.e. promax). The orthogonal factor analysis suggested the presence of two distinct, relatively independent composites for parenting behaviour. On the basis of these factors, the individual subscales were composited to obtain overall sensitive parenting and harsh intrusive parenting scores. Only sensitive parenting was used in the present analysis. Sensitive parenting consisted of the mean of the reverse score for the detachment/disengagement scale and the scores for sensitivity/responsiveness, positive regard, and stimulation of cognitive development scales. Accordingly, higher scores on the sensitivity subscale reflect parenting behaviours that are child-centred, engaged, warm, and stimulating. These measures have been successfully tested in other investigations (Zvara et al., 2015; Barnett, Shanahan, Deng, Haskett, & Cox, 2010). Intercoder reliability, which was determined by ICCs across coders, yielded reliabilities of .80 and .87 for maternal sensitivity at the 6- and 15-month time points, respectively.
Control variables
Although childhood demographic variables from the family of origin were used in the PSM, the present study uses current demographic information as control variables. Poverty status, maternal education, and race have each been identified as important correlates of parenting (see Conger et al., 2010, for a review) and thus, the family’s income-to-needs ratio, maternal education, child sex, and race were included as covariates in this model. Income-to-needs ratios were calculated by dividing the total household income from all possible sources by the federally determined poverty threshold for the number of people living in the household for that year. Income-to-needs ratios above 1.0 indicate that a family is able to provide for basic needs, whereas values below 1.0 indicate that they are not. Given that the overwhelming majority of African American families resided in one of the two study sites, study location was included to address a potential confound between site and ethnicity.
Analytic Strategy
Analyses proceeded in three phases. First, a PSM procedure was conducted to control for pre-existing differences between the treatments (experienced CST) and the controls (no CST). Second, the structure of the 10 indicators of pregnancy complications was examined using a combination of principle components analyses (PCA) and exploratory factor analyses (EFA). Third, structural equation modelling (SEM) was used to test the proposed models (Schumacker & Lomax, 1996). Models were parameterized using the Mplus 6.0 software package (Muthén & Muthén, 2006) using the robust maximum likelihood estimator. Full information maximum likelihood (FIML) was used as the missing data technique (Arbuckle, 1996). FIML estimation uses all available observations and provides unbiassed estimation of model parameters in the presence of missing data. There was less than 1% missing data across the covariates and mediators. Model fit was examined using a number of fit indices, including the comparative fit index (CFI; Bentler, 1990), the Tucker-Lewis index (TLI; Tucker & Lewis, 1973), the root mean squared error of approximation (RMSEA; Browne & Cudeck, 1993), and the standardized root mean square residual (SRMR, Hu & Bentler, 1999). CFI and TLI values above .95 and RMSEA values between .05 and .06 (Kline, 2005), and SRMR below .08 indicate excellent model fit.
RESULTS
Preliminary Analyses
Matching results and balance checking for matched sample
PSM for this study followed the method developed by Rosenbaum and Rubin (1983) and was conducted in several steps including the selection of the appropriate covariates from which to create the treatment (mothers with CST) and comparison mothers. In the current study, the PSM procedure yielded a sample of 204 women; 105 who experienced CST matched to 99 women who did not. Diagnostic tests determined that the two groups were more similar to each other than with the larger sample from which the subsample was derived (i.e. the full FLP sample from which the comparison group was drawn). This means that, based on childhood family of origin variables, the two groups were statistically not different leaving CST (yes or no) as the one differentiator among those variables considered. Details of the matching procedures can be found in Zvara et al. (2015).
Structure of prenatal stress
In order to assess the first question, PCA was performed on indicators of pregnancy complications. Following best practices, scree plots and parallel analyses were evaluated to determine the optimal number of factors to retain (Floyd & Widaman, 1995; Dinno, 2009). Both methods favoured a three-factor solution. A follow-up EFA model was examined (see Table 1), which forced extraction of three factors. We labelled the first of these factors prenatal psychosocial distress (factor 1) because of the psychosocial and emotional content of the questions in this factor. The two additional factors were clustered around questions relating to perinatal complications such as high blood pressure or excessive nausea. In the present analysis, we used only the prenatal psychosocial distress factor in the SEM analysis as a latent variable given our hypotheses that mothers with CST histories would report greater prenatal psychosocial distress and that prenatal distress would be related to the early caregiving environment (i.e. depressive symptoms and parenting).
Descriptive statistics
Of the 105 women in the CST group, 12% of the women reported sexual trauma before the age of 4, 59% between the ages of 4 and 11, and 29% between the ages of 12 and 14. Approximately half of the women in the CST group reported four or more sexual trauma experiences, and 55% reported that the perpetrator was either a parent or other relative (e.g. grandparent, uncle). Furthermore, of mothers with CST histories, 23% also reported serious injury from beating and 32% reported having had a serious accident. Mothers without CST histories reported 3% and 16% respectively.
Descriptive statistics are presented in Table 2. Independent sample t-tests were conducted to compare mean differences between the two groups across numerous demographic variables and found the two groups to differ only with regards to mean family income-to-needs, (M=1.40, sd=1.13) and (M=2.1, sd=2.56), t (198)=2.53, p<.001, meaning that on average, the CST group reported significantly less current household income compared to the no childhood sexual trauma control (NCST) group.
Table 2.
Descriptive statistics for childhood sexual trauma (CST) group and matched no childhood sexual trauma controls (NCST) on key variables
| Variable | CST group (N = 105) M (sd) |
NCST group (N = 99) M (sd) |
|---|---|---|
| Maternal and household characteristics: | ||
| Maternal age ^ | 25.5 (5.2) | 26.1 (5.4) |
| Income to needs ^ | 1.40 (1.13) | 2.10 (2.56) |
| Maternal education^ | 14.1 (2.9) | 14.5 (2.6) |
| Prenatal distress* | 1.51 (.92) | 1.17 (.71) |
| Depressive symptoms at 6 months | .51 (.66) | .34 (.48) |
| Maternal sensitivity at 15 months | 2.6 (.88) | 2.8 .(77) |
Note:
Assessed at the 6-month visit.
SUMMED across indicators.
In addition, there was a significant group difference noted with regards to prenatal psychosocial distress (summed across indicators), t (202) =14.3, p<.001, and maternal sensitive parenting at 15 months, t (184) =4.1, p<.05, meaning that on average, the mothers with CST histories reported significantly more prenatal psychosocial distress and were rated as being less sensitive in their parenting compared to the NCST group. T-tests further revealed that the group difference for maternal depressive symptoms at 6 months was just significant at p=.054.
Mediation analysis
We tested an initial model to determine the association between CST and maternal sensitive parenting at 15 months above and beyond the covariates. The model fit the data well, χ2 (5, N=204)=17, p=.001, CFI =1.00, TLI =1.00, RMSEA=0.00. Maternal CST predicted maternal sensitive parenting at 15 months, (β =−.20, p<.05). Having confirmed the association between CST and early parenting, in the next set of the analyses we tested the full theoretical model linking maternal childhood sexual trauma to early parenting behaviour at 15 months through maternal prenatal distress and maternal depressive symptoms at 6 months, while controlling for early parenting behaviour at 6 months, the family’s current income-to-needs ratio, maternal education, data collection site, child sex, and race. Paths were estimated to include all covariates and subsequent predictors of sensitive parenting. The analyses reported in Figure 1 simultaneously consider the associations between CST, prenatal distress, 6-month maternal depressive symptom, and 15-month sensitive parenting. Results from the final model include standardized parameter estimates and only significant paths (p<.05) are depicted. This model was a good fit to the data, χ2 (51, N=204) =72, p=.03, CFI=.97, TLI=.96, RMSEA=0.05. In a model with two mediators linking maternal CST and parenting at 15 months, and, after controlling for early caregiving at 6 months, the family’s current income-to-needs ratio, child sex, race, maternal education, and the data collection site, there was a main effect of childhood sexual trauma on sensitive parenting at 15 months, (β =−.04, p<.05). There was a main effect of CST on prenatal distress (β=.34, p<.01), which in turn was related to postnatal depressive symptoms (β =.43, p<.001), which in turn was related maternal sensitivity at 15 months (β = −.51, p<.01).
Figure 1.
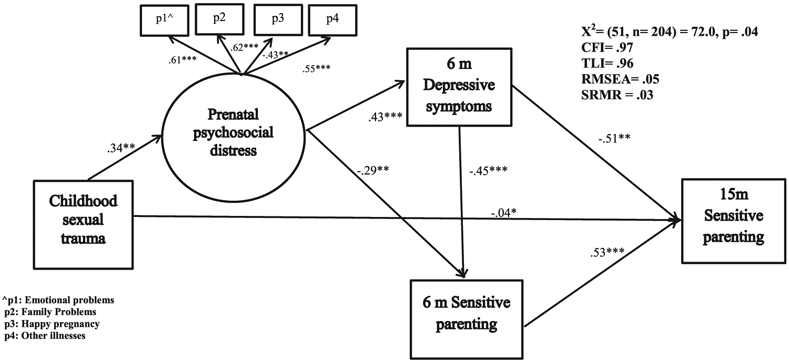
Full theoretical model of the mediating roles of maternal prenatal psychosocial distress and postnatal depressive symptoms in the associations between maternal childhood sexual trauma and maternal sensitive parenting.
In addition, there were three significant indirect pathways from maternal CST and sensitive parenting at 15 months. One pathway was through prenatal distress and 6-month parenting (childhood sexual trauma→prenatal distress→6-month sensitive parentin→15-month sensitive parenting, β =.05, p<.05). A second pathway through prenatal distress and 6-month maternal depressive symptoms (childhood sexual trauma→prenatal distress→6-month maternal depressive symptoms→15-month sensitive parenting, β =.08, p<.05). Last, a third pathway was through prenatal distress, 6-month depressive symptoms, and early parenting at 6 months (childhood sexual trauma→prenatal distress→6-month maternal depressive symptoms→6-month sensitive parenting→15-month sensitive parenting, (β =.04, p<.01)). Standardized parameter estimates for the final SEM can be found in Table 3.
Table 3.
Standardized parameter estimates for the structural equation model
| β | SE | ||
|---|---|---|---|
| Target child’s sex → | 15m Sensitive parenting | .01 | .02 |
| Target child’s race → | 15m Sensitive parenting | −.02 | .02 |
| Income to needs → | 15m Sensitive parenting | .01 | .05 |
| Maternal education → | 15m Sensitive parenting | .01 | .02 |
| Study site → | 15m Sensitive parenting | .01 | .02 |
| 6m Depressive symptoms → | 15m Sensitive parenting | −.51** | .03 |
| 6m Sensitive parenting → | 15m Sensitive parenting | .53*** | .02 |
| Childhood sexual trauma → | 15m Sensitive parenting | −.04* | .02 |
| Target child’s sex → | 6m Sensitive parenting | .02 | .03 |
| Target child’s race → | 6m Sensitive parenting | −.07 | .10 |
| Income to needs → | 6m Sensitive parenting | .11 | .08 |
| Maternal education → | 6m Sensitive parenting | .02 | .07 |
| Study site → | 6m Sensitive parenting | .07 | .05 |
| 6m Depressive symptoms → | 6m Sensitive parenting | −.45*** | .09 |
| Prenatal psychosocial distress → | 6m Sensitive parenting | −.29** | .11 |
| Childhood sexual trauma → | 6m Sensitive parenting | .05 | .08 |
| Target Child’s sex → | 6m Depressive Symptoms | .02 | .03 |
| Target Child’s race → | 6m Depressive Symptoms | .01 | .19 |
| Income to needs → | 6m Depressive Symptoms | −.18* | .19 |
| Maternal education → | 6m Depressive Symptoms | −.02 | .03 |
| Study site → | 6m Depressive Symptoms | .02 | .09 |
| Prenatal psychosocial distress → | 6m Depressive Symptoms | .43*** | .05 |
| Childhood sexual trauma → | 6m Depressive Symptoms | .05 | .08 |
| Target Child’s sex → | Prenatal psychosocial distress | .17 | .08 |
| Target Child’s race → | Prenatal psychosocial distress | .15 | .26 |
| Income to needs → | Prenatal psychosocial distress | −.14 | .25 |
| Maternal education → | Prenatal psychosocial distress | −.05 | .03 |
| Study site → | Prenatal psychosocial distress | .15 | .12 |
| Childhood sexual trauma → | Prenatal psychosocial distress | .34** | .09 |
Notes:
p<.05.
p<.01.
p<.001.
DISCUSSION
By using a large sample of mothers with extensive self-report and observational data, we were able to employ propensity matching techniques to create groups of mothers with and without CST histories while controlling for additional maltreatment and trauma, as well as other experiences of childhood adversity that may confound the experience of a history of CST. We reported in earlier work (Zvara et al., 2015) that mothers with CST histories differed in their parenting behaviours across multiple domains of parenting including sensitive parenting. The current study extends these previous findings by demonstrating that many of the parenting problems reported by women with trauma histories begin early in the postpartum period. Furthermore, this study provides evidence for a possible causal association between prenatal distress and the early caregiving environment including sensitive parenting behaviour.
Given research findings linking prenatal distress to child functioning, the findings of this study bring attention to prenatal distress as an important pathway by which CST may exert itself across time to influence the development of the next generation. Consistent with expectations, this study found support for the notion that maternal CST is related to parenting behaviour of offspring. More specifically, even after controlling for numerous demographic characteristics associated with child and family risk, there were three significant indirect pathways by which maternal CST was related to sensitive parenting at 15 months. The results highlight the unique roles of prenatal psychosocial distress and postnatal depressive symptoms as key mediators linking CST and parenting at 15 months.
That prenatal distress would be related to postnatal depressive symptoms is in keeping with prior studies (Milgrom et al., 2008; Kaplan, Evans, & Monk, 2008). Heron et al. (2004) reported that, in their study of the associations between pre- and postnatal depressive symptoms, the majority of cases of postnatal depressive symptoms were preceded by prenatal depressive symptomatology. Finding an independent path from CST→prenatal distress→parenting above and beyond the effects of postnatal depression provides key information. First, it provides support for the construct validity for our measure of prenatal psychosocial distress as a unique predictor of postnatal depressive symptoms and early parenting behaviour. Further, results from this study also suggest that prenatal distress makes a unique contribution to maternal caregiving as a function of maternal CST. Although limited, early work examining the transition to parenthood noted that mothers who reported greater distress prenatally were rated as less expressive in interactions with their infants (Goldstein, Diener, & Mangelsdorf, 1996). More recent work examining the associations between prenatal factors and subsequent parenting suggests a direct relation between prenatal distress and early parenting stress in mothers (Misri, Kendrick, & Oberlander, 2010). The independent path from CST to prenatal distress to parenting behaviour may be reflective of a continuation of the distress from the prenatal period resulting in mothers being less responsive and sensitive to their infants.
The current study provides evidence for a distress/stress spillover process such that the distress experienced prenatally as a function of CST, spills over into the early caregiving environment including parenting behaviours. Stress spillover is hypothesized in the broader parenting literature to occur when stress (a negative affective state) generated in response to difficulties within one domain of functioning (i.e. prenatal distress) spills over into other domains of functioning, such as sensitive parenting (Brock & Lawrence, 2008; Östberg & Hagekull, 2000). An indirect pathway, CST→prenatal distress→postnatal depressive symptoms→parenting, adds further evidence of a spillover process from prenatal distress to the broader early caregiving system, specifically, parenting. Mothers with childhood sexual trauma histories who are struggling with elevated depressive symptoms may be overwhelmed by their child care responsibilities and may thereby be less responsive to their children’s bids for attention and care compared to mothers without childhood sexual trauma histories.
This indirect pathway, a unique finding of this study, is in keeping with and extends prior research linking prenatal distress to postnatal depressive symptoms. Our study, to the best of our knowledge, is among the first to highlight the associations between pre- and postnatal psychological factors with early parenting behaviour among a sample of women with CST history and comparison women. While Buist and Janson (2001) reported impaired mother–infant interaction in their sample of women with postpartum depression, their observers were not blind to maternal abuse history, which may have biassed their findings.
It is also plausible, however, that the findings may be suggestive of distress around becoming a parent and the demands of parenting more broadly. Douglas (2000) reported that women who had experienced CST and were seeking mental health services reported being significantly more anxious about the intimate aspects of parenting their children than did women seeking mental health services who had not experienced such trauma. Therefore, the findings from this study may be reflective of apprehension or distress around becoming a parent.
Limitations
Despite the many strengths of this study, there are also numerous limitations. One issue is the reliance on retrospective reports of CST, childhood demographic factors from the family of origin and prenatal psychosocial distress. As numerous researchers investigating the long-term effects of CST have posited, the passage of time may alter participants’ recollections of the past (Goodman et al., 2003; Widom & Morris, 1997). Additionally, some women may not have felt comfortable reporting their trauma history in the context of the research study. Therefore, it is possible that, within our control group, there may be women who experienced CST but did not report it. To the extent that women under-reported their trauma experiences, the findings reported here may be conservative estimates. Furthermore, we relied on maternal retrospective recall to characterize their childhood sociodemographic characteristics, which played a critical role in selecting a group of comparison families. Although it could be argued that many adults may not be aware, much less be able to recall their family’s SES status or highest grade completed by their mothers, early work by Krieger and colleagues support the validity of adult recall of measures of childhood socioeconomic factors in childhood including parental education (Krieger, Okamoto, & Selby, 1998; see also, Batty, Lawlor, Macintyre, Clark, & Leon, 2005; Mckenzie & Carter, 2009). Similarly, although retrospective accounts of prenatal psychosocial stress may be subject to certain biases, prior research has found that mothers are accurately able to retrospectively report on prenatal factors (Tomeo et al., 1999; Rice et al., 2007).
In addition, although we used numerous variables from the family of origin for the matching procedure, we did not account for all of the potential confounders that might have been relevant to subsequent parenting of survivors, such as family dysfunction in the women’s family of origin (e.g. parental marital conflict, mental health, or substance use). Similarly, we did not consider factors such as the severity, or chronicity, or age of abuse initiation in our analysis which could affect the impact that sexual abuse has on subsequent functioning. Examining additional aspects of the abuse experience will provide a more nuanced approach to understanding the long-term parenting outcomes of women with CST histories.
Implications and Future Directions
In order to fully understand the impact of CST on parenting behaviour and thus, the development of offspring, future research will need to examine additional explanatory mechanisms to tease apart the effects of the trauma experience. Emerging evidence from a range of disciplines has identified posttraumatic stress disorder (PTSD) as a core manifestation of childhood trauma because of the high frequency with which this disorder and related symptoms appear in sexually abused children and adult victims of childhood trauma (Kaplow, Dodge, Amaya-Jackson, & Saxe, 2005; Muzik et al., 2013). Although we did not assess PTSD, it is plausible that mothers in our sample were also struggling with PTSD, given the comorbid nature of these pathologies. Future research will need to examine the role of PTSD in early parenting behaviour for mothers with CST histories.
Given the significant number of women who report childhood sexual trauma, understanding the parenting behaviours among survivors is critical to understanding the potential for CST to have an indirect impact across multiple generations. Future research will need to further elucidate the associations between pre-and postnatal maternal functioning in women with CST histories. Similarly, prenatal psychosocial distress may also have been a result of prenatal depression. Future research will need to tease apart the effects of prenatal depression and prenatal distress on postpartum depressive symptoms and early parenting.
Importantly, the results of this study add to the burgeoning evidence highlighting the importance of screening for maternal depressive symptoms in the pre- and postpartum period. Prenatal care provides a unique opportunity to evaluate the impact of life history and current life events during pregnancy, and to develop a coordinated intervention plan. Indeed, the prenatal period may be an optimal time to screen for and treat mental health problems because pregnant women are under regular care and thus available for referrals and follow up interventions. Screening pregnant women for childhood trauma, prenatal stress, and depressive symptoms would allow for the delivery of well-designed, sensitive, and systematic interventions that target different domains of functioning, such as depressive symptoms, and parenting behaviour.
Along the same lines, the findings from this study highlight the importance of considering the effects of women’s mental health during the pre- and postnatal periods on subsequent parenting and child development. Pregnant women are routinely screened for numerous pregnancy related disorders and issues. For example, gestational diabetes is far less common than depression and other mental health disorders during pregnancy; however, women are routinely screened for this condition, but not for depression or depressive symptoms (Gazmararian et al., 2000). Therefore, improved surveillance of mental health during pregnancy and the early postpartum period for women with CST histories will likely lead to targeted interventions for this population.
ACKNOWLEDGEMENTS
Support for this research was provided by the National Institute of Child Health and Human Development (PO1-HD-39667), with co-funding from the National Institute on Drug Abuse. Additional support was provided by the National Institute on Alcohol Abuse and Alcoholism (A12-0934) awarded as a predoctoral fellowship (F31) to the lead author.
Appendix
The Family Life Project (FLP) Key Investigators include Lynne Vernon Feagans, The University of North Carolina; Martha Cox, The University of North Carolina; Clancy Blair, New York University; Peg Burchinal, The University of North Carolina; Linda Burton, Duke University; Keith Crnic, The Arizona State University; Ann Crouter, The Pennsylvania State University; Patricia Garrett-Peters, The University of North Carolina; Mark Greenberg, The Pennsylvania State University; Stephanie Lanza, The Pennsylvania State University; Roger Mills-Koonce, The University of North Carolina at Greensboro; Emily Werner, The Pennsylvania State University; and Michael Willoughby, The University of North Carolina.
REFERENCES
- Ainsworth MDS, Blehar MC, Waters E & Wall S (1978). Patterns of attachment: A psychological study of the strange situation. USA: Lawrence Erlbaum. [Google Scholar]
- Alexander PC, Teti L & Anderson CL (2000). Childhood sexual abuse history and role reversal in parenting. Child Abuse & Neglect, 24, 829–838. [DOI] [PubMed] [Google Scholar]
- Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C & Shaffer S (2005). The relationships between parenting stress, parenting behavior and preschoolers’ social competence and behavior problems in the classroom. Infant and Child Development, 14(2), 133–154. [Google Scholar]
- Arbuckle JL (1996). Full information estimation in the presence of incomplete data. In Marcoulides GA & Schumacker RE (Eds.), Advanced structural equation modeling (edn, pp. 243–277). Mahwah, NJ: Erlbaum. [Google Scholar]
- Bailey HN, DeOliveira CA, Wolfe VV, Evans EM & Hartwick C (2012). The impact of childhood maltreatment history on parenting: A comparison of maltreatment types and assessment methods. Child Abuse & Neglect, 36(3), 236–246. [DOI] [PubMed] [Google Scholar]
- Banyard VL, Williams LM & Siegel JA (2003). The impact of complex trauma and depression on parenting: An exploration of mediating risk and protective factors. Child Maltreatment, 8(4), 334–349. [DOI] [PubMed] [Google Scholar]
- Barnett MA, Shanahan L, Deng M, Haskett ME & Cox MJ (2010). Independent and interactive contributions of parenting behaviors and beliefs in the prediction of early childhood behavior problems. Parenting: Science and Practice, 10(1), 43–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty GD, Lawlor DA, Macintyre S, Clark H & Leon DA (2005). Accuracy of adults’ recall of childhood social class: Findings from the Aberdeen children of the 1950s study. Journal of Epidemiology and Community Health, 59(10), 898–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett HA, Einarson A, Taddio A, Koren G & Einarson TR (2004). Prevalence of depression during pregnancy: Systematic review. Obstetrics & Gynecology, 103(4), 698–709. [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. [DOI] [PubMed] [Google Scholar]
- Brock RL & Lawrence E (2008). A longitudinal investigation of stress spillover in marriage: Does spousal support adequacy buffer the effects? Journal of Family Psychology, 22(1), 11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW & Cudeck R (1993). Alternative ways of assessing model fit. Sage Focus Editions, 154, 136–162. [Google Scholar]
- Buist A & Janson H (2001). Childhood sexual abuse, parenting and postpartum depression-a 3-year follow-up study. Child Abuse & Neglect, 25(7), 909–921. [DOI] [PubMed] [Google Scholar]
- Butler AC (2013). Child sexual assault: Risk factors for girls. Child Abuse & Neglect, 37(9), 643–652. [DOI] [PubMed] [Google Scholar]
- Cassidy J (2008). The nature of the child’s ties. In Cassidy J & Shaver PR (Eds.), Handbook of attachment (2nd edn, pp. 3–22). New York: Guilford Press. [Google Scholar]
- Conger RD, Conger KJ & Martin MJ (2010). Socioeconomic status, family processes, and individual development. Journal of Marriage and Family, 72(3), 685–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtois CA (1992). The memory retrieval process in incest survivor therapy. Journal of Child Sexual Abuse, 1(1), 15–31. [Google Scholar]
- Cox MJ, & Crnic K (2002). Qualitative ratings for parent–child interaction at 3–12 months of age. Unpublished manuscript, University of North Carolina at Chapel Hill. [Google Scholar]
- Cox MJ & Harter KSM (2003). Parent–child relationships. In Bornstein MH, Davidson L, Keyes CLM & Moore KA (Eds.), Wellbeing: Positive development across the life course (edn, pp. 191–204). Mahwah, NJ: Erlbaum. [Google Scholar]
- Derogatis L (2000). Brief symptom inventory 18. Minneapolis, MN: NCS Pearson. [Google Scholar]
- DiLillo D (2001). Interpersonal functioning among women reporting a history of childhood sexual abuse: Empirical findings and methodological issues. Clinical Psychology Review, 21, 553–576. [DOI] [PubMed] [Google Scholar]
- DiLillo D & Damashek A (2003). Parenting characteristics of women reporting a history of childhood sexual abuse. Child Maltreatment, 8(4), 319–333. [DOI] [PubMed] [Google Scholar]
- DiLillo D, Tremblay GC & Peterson L (2000). Linking childhood sexual abuse and abusive parenting: The mediating role of maternal anger. Child Abuse & Neglect, 24(6), 767–779. [DOI] [PubMed] [Google Scholar]
- Dinno A (2009). Exploring the sensitivity of Horn’s parallel analysis to the distributional form of random data. Multivariate Behavioral Research, 44(3), 362–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas AR (2000). Reported anxieties concerning intimate parenting in women sexually abused as children. Child Abuse & Neglect, 24, 425–434. [DOI] [PubMed] [Google Scholar]
- Field T (2010). Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behavior and Development, 33(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D (1993). Epidemiological factors in the clinical identification of child sexual abuse. Child Abuse & Neglect, 17(1), 67–70. [DOI] [PubMed] [Google Scholar]
- Floyd FJ & Widaman KF (1995). Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment, 7(3), 286–299. [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G & Swinson T (2005). Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology, 106(5 Part 1), 1071–1083. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Petersen R, Spitz AM, Goodwin MM, Saltzman LE & Marks JS (2000). Violence and reproductive health: Current knowledge and future research directions. Maternal and Child Health Journal, 4(2), 79–84. [DOI] [PubMed] [Google Scholar]
- Glazier RH, Elgar FJ, Goel V & Holzapfel S (2004). Stress, social support, and emotional distress in a community sample of pregnant women. Journal of Psychosomatic Obstetrics & Gynecology, 25(3-4), 247–255. [DOI] [PubMed] [Google Scholar]
- Goldstein LH, Diener ML & Mangelsdorf SC (1996). Maternal characteristics and social support across the transition to motherhood: Associations with maternal behavior. Journal of Family Psychology, 10(1), 60–71. [Google Scholar]
- Goodman GS, Ghetti S, Quas JA, Edelstein RS, Alexander KW, Redlich AD, … & Jones DP (2003). A prospective study of memory for child sexual abuse new findings relevant to the repressed-memory controversy. Psychological Science, 14(2), 113–118. [DOI] [PubMed] [Google Scholar]
- Graignic-Philippe R, Dayan J, Chokron S, Jacquet AY & Tordjman S (2014). Effects of prenatal stress on fetal and child development: A critical literature review. Neuroscience & Biobehavioral Reviews, 43, 137–162. [DOI] [PubMed] [Google Scholar]
- Green BL (1996). Trauma history questionnaire. In Stamm BH (Ed.), Measurement of stress trauma and adaptation (edn, pp. 366–369). Lutherville, MD: Sidran. [Google Scholar]
- Grolnick WS, Gurland SG, DeCourcey W & Jacob K (2002). Antecedents and consequences of mothers’ autonomy support: An experimental investigation. Developmental Psychology, 38, 143–155. [PubMed] [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, Glover V & ALSPAC Study Team (2004). The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders, 80(1), 65–73. [DOI] [PubMed] [Google Scholar]
- Hu LT & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Jacobs JL (1992). Child sexual abuse victimization and later sequelae during pregnancy and childbirth. Journal of Child Sexual Abuse, 1(1), 103–112. [Google Scholar]
- Kaplan LA, Evans L & Monk C (2008). Effects of mothers’ prenatal psychiatric status and postnatal caregiving on infant biobehavioral regulation: Can prenatal programming be modified? Early Human Development, 84(4), 249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, Dodge KA, Amaya-Jackson L & Saxe GN (2005). Pathways to PTSD, Part II: Sexually abused children. American Journal of Psychiatry, 162, 1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman AS & Kaufman NL (1994). Kaufman functional academic skills test. Toronto, Canada: PSYCAN. [Google Scholar]
- Kendall-Tackett K (2002). The health effects of childhood abuse: Four pathways by which abuse can influence health. Child Abuse & Neglect, 26(6), 715–729. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA (2007). Violence against women and the perinatal period, the impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma, Violence & Abuse, 8(3), 344–353. [DOI] [PubMed] [Google Scholar]
- Kline RB (2005). Principles and practice of structural equation modeling (2nd edn). New York: The Guilford Press. [Google Scholar]
- Krieger N, Okamoto A & Selby JV (1998). Adult female twins’ recall of childhood social class and father’s education: A validation study for public health research. American Journal of Epidemiology, 147(7), 704–708. [DOI] [PubMed] [Google Scholar]
- Leeners B, Richter-Appelt H, Imthurn B & Rath W (2006). Influence of childhood sexual abuse on pregnancy, delivery, and the early postpartum period in adult women. Journal of Psychosomatic Research, 61(2), 139–151. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E & Neuman G (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20(5), 561–592. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K & Block D (1996). The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Mental Health Journal, 17(3), 257–275. [Google Scholar]
- Maccoby EE (2001). Parenting and its effects on children: On reading and misreading behavior genetics. The Science of Mental Health: Personality and Personality Disorder, 51, 201. [DOI] [PubMed] [Google Scholar]
- Mark IL, IJzendoorn MHV & Bakermans-Kranenburg MJ (2002). Development of empathy in girls during the second year of life: Associations with parenting, attachment, and temperament. Social Development, 11(4), 451–468. [Google Scholar]
- Mckenzie SK & Carter KN (2009). Are retrospective measures of childhood socioeconomic position in prospective adult health surveys useful? Australasian Epidemiologist, 16(3), 2224. [Google Scholar]
- Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, … & Buist A (2008). Antenatal risk factors for postnatal depression: A large prospective study. Journal of Affective Disorders, 108(1), 147–157. [DOI] [PubMed] [Google Scholar]
- Milne L, Greenway P, Guedeney A & Larroque B (2009). Long term developmental impact of social withdrawal in infants. Infant Behavior and Development, 32(2), 159–166. [DOI] [PubMed] [Google Scholar]
- Misri S, Kendrick K & Oberlander T (2010). Antenatal depression and anxiety affect postpartum parenting stress: a longitudinal, prospective study. Canadian Journal of Psychiatry, 55, 222–228. [DOI] [PubMed] [Google Scholar]
- Monroe SM & Simons AD (1991). Diathesis/stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin, 110, 406–425. [DOI] [PubMed] [Google Scholar]
- Murray L, Halligan S & Cooper P (2010). Effects of postnatal depression on mother-infant interactions and child development. Wiley-Blackwell Handbook of Infant Development, (2nd ed., pp. 192–220). Malden: Wiley-Blackwel. [Google Scholar]
- Muthén LK & Muthén BO (2006). Mplus version 4 user’s guide. Los Angeles (CA): Muthén & Muthén. [Google Scholar]
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K & Seng JS (2013). Mother–infant bonding impairment across the first 6 months postpartum: The primacy of psychopathology in women with childhood abuse and neglect histories. Archives of Women’s Mental Health, 16(1), 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. (1999). Child care and mother-child interaction in the first three years of life. Developmental Psychology, 35, 1399–1413. [PubMed] [Google Scholar]
- Östberg M & Hagekull B (2000). A structural modeling approach to the understanding of parenting stress. Journal of Clinical Child Psychology, 29(4), 615–625. [DOI] [PubMed] [Google Scholar]
- Paolucci EO, Genuis ML & Violato C (2001). A meta-analysis of the published research on the effects of child sexual abuse. The Journal of Psychology, 135(1), 17–36. [DOI] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M & Gómez-Benito J (2009). The prevalence of child sexual abuse in community and student samples: A meta-analysis. Clinical Psychology Review, 29(4), 328–338. [DOI] [PubMed] [Google Scholar]
- Putnam FW (2003). Ten-year research updates review: Child sexual abuse. Journal of the American Academy of Child & Adolescent Psychiatry, 42(3), 269–278. [DOI] [PubMed] [Google Scholar]
- Reich W (2000). Diagnostic interview for children and adolescents (DICA). Journal of the American Academy of Child and Adolescent Psychiatry, 39, 59–66. [DOI] [PubMed] [Google Scholar]
- Reich W, Todd RD, Joyner CA, Neuman RJ & Heath AC (2003). Reliability and stability of mothers’ reports about their pregnancies with twins. Twin Research, 6, 85–88. [DOI] [PubMed] [Google Scholar]
- Rice F, Lewis A, Harold G, van den Bree M, Boivin J, Hay DF, … & Thapar A (2007). Agreement between maternal report and antenatal records for a range of pre- and perinatal factors: The influence of maternal and child characteristics. Early Human Development, 83(8), 497–504. [DOI] [PubMed] [Google Scholar]
- Roberts R, O’Connor T, Dunn J & Golding J (2004). The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child Abuse & Neglect, 28(5), 525–545. [DOI] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T & Stewart DE (2004). Antenatal risk factors for postpartum depression: A synthesis of recent literature. General Hospital Psychiatry, 26(4), 289–295. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR & Rubin DB (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70(1), 41–55. [Google Scholar]
- Roth S & Lebowitz L (1988). The experience of sexual trauma. Journal of Traumatic Stress, 1(1), 79–107. [Google Scholar]
- Schuetze P & Eiden RD (2005). The relationship between sexual abuse during childhood and parenting outcomes: Modeling direct and indirect pathways. Child Abuse & Neglect, 29(6), 645–659. [DOI] [PubMed] [Google Scholar]
- Schumacker RE & Lomax RG (1996). A beginner’s guide to structural equation modeling. Mahwah, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Tomeo CA, Rich-Edwards JW, Michels KB, Berkey CS, Hunter DJ, Frazier AL, … & Buka SL (1999). Reproducibility and validity of maternal recall of pregnancy-related events. Epidemiology, 10(6), 774–776. [PubMed] [Google Scholar]
- Toth SL, Maughan A, Manly JT, Spagnola M & Cicchetti D (2002). The relative efficacy of two interventions in altering maltreated preschool children’s representational models: Implications for attachment theory. Development and Psychopathology, 14(4), 877–908. [DOI] [PubMed] [Google Scholar]
- Tronick E & Reck C (2009). Infant of depressed mothers. Harvard Review of Psychiatry, 17, 147–156. [DOI] [PubMed] [Google Scholar]
- Tucker LR & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. [Google Scholar]
- Verkerk GJ, Pop VJ, Van Son MJ & Van Heck GL (2003). Prediction of depression in the postpartum period: A longitudinal follow-up study in high-risk and low-risk women. Journal of Affective Disorders, 77(2), 159–166. [DOI] [PubMed] [Google Scholar]
- Widom CS & Morris S (1997). Accuracy of adult recollections of childhood victimization, part 2: Childhood sexual abuse. Psychological Assessment, 9(1), 34–46. [Google Scholar]
- Wosu AC, Gelaye B & Williams MA (2015). History of childhood sexual abuse and risk of prenatal and postpartum depression or depressive symptoms: An epidemiologic review. Archives of Women’s Mental Health, 18(5), 659–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright MOD, Fopma-Loy J & Oberle K (2012). In their own words: The experience of mothering as a survivor of childhood sexual abuse. Development and Psychopathology, 24(02), 537–552. [DOI] [PubMed] [Google Scholar]
- Zvara BJ, Mills-Koonce WR, Carmody KA, Cox M & Family Life Project Key Investigators (2015). Childhood sexual trauma and subsequent parenting beliefs and behaviors. Child Abuse & Neglect, 44, 87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]


