Supplemental Digital Content is available in the text.
Abstract
Background.
Regional variation in lung transplantation practices due to local coronavirus disease 2019 (COVID-19) prevalence may cause geographic disparities in access to lung transplantation.
Methods.
Using the United Network for Organ Sharing registry, we conducted a descriptive analysis of lung transplant volume, donor lung volume, new waitlist activations, and waiting list deaths at high-volume lung transplant centers during the first 3 months of the pandemic (March 1. 2020, to May 30, 2020) and we compared it to the same period in the preceding 5 years.
Results.
Lung transplant volume decreased by 10% nationally and by a median of 50% in high COVID-19 prevalence centers (range –87% to 80%) compared with a median increase of 10% (range –87% to 80%) in low prevalence centers (P-for-trend 0.006). Donation services areas with high COVID-19 prevalence experienced a greater decrease in organ availability (-28% range, –72% to –11%) compared with low prevalence areas (+7%, range –20% to + 55%, P-for-trend 0.001). Waiting list activations decreased at 18 of 22 centers. Waiting list deaths were similar to the preceding 5 years and independent of local COVID-19 prevalence (P-for-trend 0.36).
Conclusions.
Regional variation in transplantation and donor availability in the early months of the pandemic varied by local COVID-19 activity.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) in the United States has been characterized by significant regional variation in both case burden and regulations on surgical procedures.1-3 These regional differences may exacerbate existing geographic variation in access to lung transplantation.4 Further characterization of regional variation in lung transplantation practices during the early months of the pandemic may inform policies to ensure fair organ allocation in the wake of COVID-19.
Early studies suggested that the COVID-19 pandemic resulted in a significant decrease in the total number of organ transplants performed in France and the United States, driven largely by a decrease in the number of kidney transplants with smaller reductions in other organs.1,5 A recent editorial reported a near-complete cessation of lung transplant activity in France during the first month of the pandemic.6 In contrast, publicly available data from the United Network for Organ Sharing (UNOS) suggests that lung transplantations continued in the United States after the onset of the pandemic, although fewer were performed compared with 2019.7,8 A nationwide survey in the United States noted that one-fifth of lung transplant centers maintained the same transplant activity, whereas others limited lung transplantation to the sickest patients only or deactivated the majority of their candidates on the waiting lists.9 In France, decreases in transplantation occurred in regions with both high and low COVID-19 prevalence.1 Recent analyses suggest that there may be regional variation in lung transplant volume in the United States during COVID-19,8 although it is unclear if these regional variations correspond to local COVID-19 prevalence.
We conducted an analysis of waiting list activations, lung donors, lung transplantations, and waiting list deaths at high-volume lung transplant centers across the United States during the early months of the COVID-19 pandemic. We describe how lung transplant practices at high-volume transplant centers varied based on COVID-19 prevalence compared with the same period in the preceding 5 years.
MATERIALS AND METHODS
Study Participants
We performed a retrospective cohort study of lung transplant centers in the United States as reported by the UNOS database. This study was exempt from approval from Columbia University Institutional Review Board under Code of Federal Regulations, Title 45, Part 46. We included high-volume lung transplant centers, defined as centers performing on average, >40 lung transplants in each of the last 5 years, which is roughly the top 25% of lung transplant centers by volume.10,11 We included all lung transplants performed on adults and adolescents ≥ 12 years of age.
The expected number of lung transplants, waiting list activations, and waiting list deaths were calculated as the median number of events at each center between March 1 and May 30 in the preceding 5 years. The observed number of transplants, waiting list activations, and waiting list deaths were determined at each center in this same 3-month period in 2020. The expected and observed number of donors was calculated using the same approach but at level of the donation service area (DSA) rather than the center. Donors were defined as those from whom at least 1 lung was transplanted and were included in the DSA in which they were hospitalized. We calculated the percent change in these variables as the observed number of events minus the expected number of events divided by the expected number of events. We used a Wilcoxon rank-sum test using the “nptrend” command in Stata to identify differences between centers by local COVID-19 prevalence. In post hoc analyses, we examined the same measures limited only to the month of April.
COVID-19 prevalence by state is available through COVID Data Tracker (www.covidtracking.com).12,13 We characterized each center’s COVID-19 burden based on the estimated number of cases per million in their state as of April 30, 2020. We subdivided centers into tertiles based on COVID-19 burden in the state (low, moderate, or high).
RESULTS
Twenty-two centers that performed an average of at least 40 lung transplants per year between 2015 and 2019 were included in this analysis. Between March 1, 2020, and May 30, 2020, 358 transplants, representing 64% of all transplants nationwide, were performed at these high-volume centers and included in this analysis. During that same 3-month period, 562 lung transplants were performed from 530 donors nationwide, compared with an average of 625 transplants from 576 donors, in the same 3-month period between 2015 and 2019 (Figure 1; Table S1, SDC, http://links.lww.com/TP/C92). Centers located in areas of high COVID-19 prevalence performed more transplants in diagnosis group A, the mean lung allocation score (LAS) at the time of transplant was modestly lower compared with prior years, and the median distance traveled to donor hospitals was greater (Table 1). Donors transplanted at low and moderate prevalence centers in 2020 were more likely to be female and donors after circulatory death compared with the preceding 5 years (Table 1).
FIGURE 1.
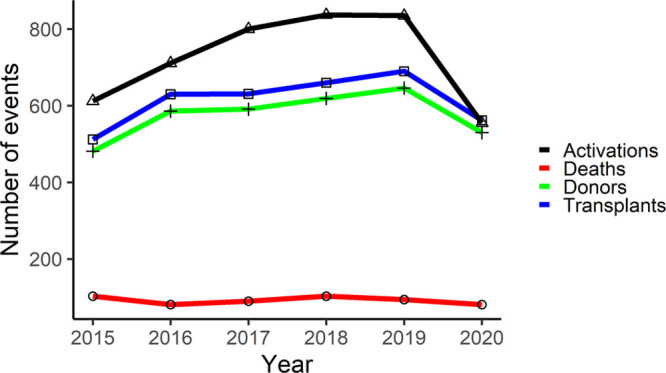
National trends in lung transplants performed, waiting list activations, waiting list deaths, and available donors for March 1 to May 30 from 2015 to 2020.
TABLE 1.
Characteristics of transplants performed in March to May 2020 compared with the same 3-mo period from 2015 to 2019 in areas of low, moderate, and high prevalence of COVID-19
| March to May From 2015 to 2019 | March to May 2020 | |||||
|---|---|---|---|---|---|---|
| Low (N = 818) | Moderate (N = 531) | High (N = 616) | Low (N = 182) | Moderate (N = 101) | High (N = 75) | |
| Recipient characteristics | ||||||
| LAS at transplantation | 41.9 (35.8–53.7) | 40.3 (34.2–57.2) | 44.4 (36.2–68.8) | 42.4 (35.8–54.5) | 38.5 (34.0–52.1) | 38.1 (33.7–52.8) |
| Female | 40.1% (328) | 38.6% (205) | 38.0% (234) | 40.7% (74) | 46.5% (47) | 41.3% (31) |
| Age | 60 (50–67) | 61 (53–66) | 60 (51–66) | 61 (55–67) | 62 (57–67) | 62 (56–68) |
| Diagnosis | ||||||
| Group A | 21.6% (177) | 31.1% (165) | 26.0% (160) | 23.1% (42) | 33.7% (34) | 37.3% (28) |
| Group B | 4.9% (40) | 3.8% (20) | 5.7% (35) | 6.6% (12) | 8.9% (9) | 2.7% (2) |
| Group C | 9.5% (78) | 9.2% (49) | 7.8% (48) | 2.8% (5) | 1.0% (1) | 8.0% (6) |
| Group D | 63.9% (523) | 55.9% (297) | 60.6% (373) | 67.6% (123) | 56.4% (57) | 52.0% (39) |
| Travel distance | 163 (24–311) | 187 (55–359) | 114 (34–241) | 160 (32–296) | 175 (104–330) | 172 (80–243) |
| Race/ethnicity | ||||||
| Black | 8.3% (68) | 7.2% (38) | 10.4% (64) | 12.1% (22) | 14.9 %(15) | 8.0% (6) |
| White | 77.0% (630) | 86.8% (461) | 81.7% (503) | 72.0% (131) | 77.2% (78) | 82.7% (62) |
| Hispanic | 10.8% (88) | 3.6% (19) | 4.9% (30) | 12.1% (22) | 4.0% (4) | 4.0% (3) |
| Other | 3.9% (32) | 2.5% (13) | 3.1% (19) | 3.9% (7) | 4.0% (4) | 5.3 % (4) |
| Blood type | ||||||
| A | 36.7% (300) | 40.3% (214) | 40.9% (252) | 34.6% (63) | 49.5% (50) | 48.0% (36) |
| AB | 4.3% (35) | 3.8% (20) | 3.1% (19) | 5.0% (9) | 4.0% (4) | 0% (0) |
| B | 11.0% (90) | 10.7% (57) | 13.8% (85) | 13.2% (24) | 7.9% (8) | 12% (9) |
| O | 48.0% (393) | 45.2% (240) | 42.2% (260) | 47.3% (86) | 38.6% (39) | 40% (30) |
| Donor characteristics | ||||||
| Female | 36.3% (297) | 38.4% (204) | 42.9% (264) | 43.4% (79) | 45.5% (46) | 30.7% (23) |
| Age | 34 (24–47) | 33 (23–48) | 33 (23–47) | 36 (24–46) | 35 (27–46) | 31 (25–48) |
| Smoking status | 6.7% (55) | 7.9% (42) | 9.1% (56) | 4.4% (8) | 10.9% (11) | 8.0% (6) |
| DCD | 2.9% (24) | 7.0% (37) | 5.7% (35) | 9.9% (18) | 13.9% (14) | 4% (3) |
| Race/ethnicity | ||||||
| Black | 14.4% (118) | 17.7% (94) | 18.0% (111) | 11.0% (20) | 16.8% (17) | 24.0% (18) |
| White | 54.2% (443) | 69.9% (371) | 69.3% (427) | 51.1% (93) | 69.3% (70) | 62.7% (47) |
| Hispanic | 23.7% (194) | 9.2% (49) | 8.9% (55) | 28.6% (52) | 9.9% (10) | 9.3% (7) |
| Other | 7.7% (63) | 3.2% (17) | 3.7% (23) | 9.3% (17) | 4.0% (4) | 4.0% (3) |
Values presented are median (interquartile range) for continuous variables and % (N) for categorical variables.
COVID-19, coronavirus disease 2019; DCD, donation after circulatory death; LAS, lung allocation score.
All centers continued to perform lung transplants during the first 3 months of the COVID-19 pandemic in the United States. The number of lung transplants performed between March 1, 2020, and May 30, 2020, appeared to decrease in areas of high COVID-19 prevalence (median change –50%, range –87% to +80%; Figure 2A), and moderate COVID-19 prevalence (median change –50%, range –40% to +81%). Lung transplant volume generally increased in areas of low COVID-19 prevalence (median change +10%, range –26% to +84%, P-for-trend 0.006). In post hoc analyses evaluating patients transplanted in the month of April, high prevalence centers had a median LAS at transplantation of 89.0 (range 46.2–90.4) compared with 45.4 (range 30.3–90.2) in low prevalence centers.
FIGURE 2.
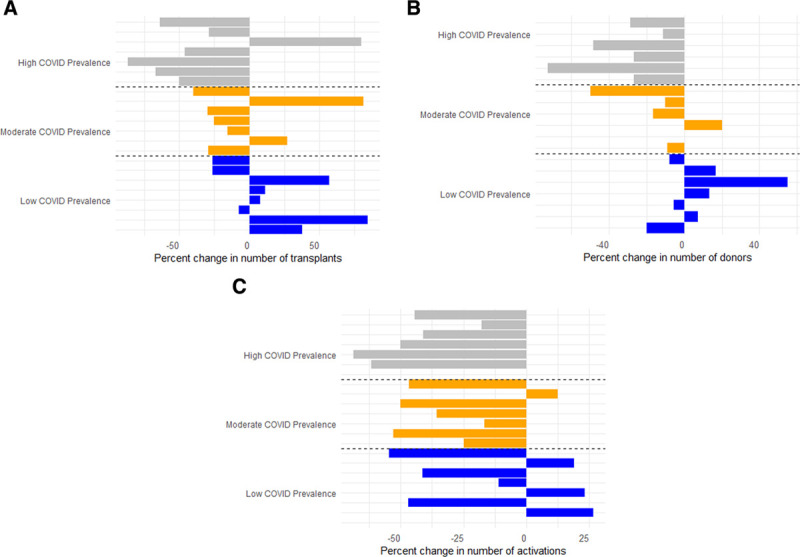
Percent changes by local coronavirus disease (COVID) prevalence in (A) lung transplant volume by center, (B) donor availability by donation service areas, and (C) waiting list activations by centers in 2020 compared with the median number of events during the same 3-mo period in 2015–2019.
Changes in donor lung availability varied across the 13 UNOS regions (Figure 3). DSAs with a high COVID-19 prevalence experienced a median reduction in donor availability by 28% (range –72% to –11%, Figure 2B), whereas those in areas of moderate COVID-19 prevalence experienced smaller reductions in donor availability (median change of –10%, range –50% to +10%). In contrast, areas with low COVID-19 prevalence experienced similar or increased donor availability in 2020 compared with the preceding 5 years (median change +7%, range –20% to +55%, P-for-trend 0.001).
FIGURE 3.
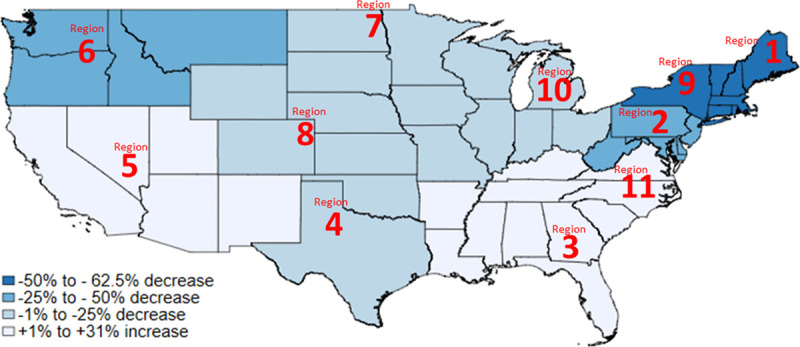
Heat map demonstrating percent change in the number of lung transplants performed in each United Network for Organ Sharing (UNOS) region between March 1, 2020, and May 30, 2020, compared with the preceding 5 y.
The majority of lung transplant programs activated fewer people on the waiting list compared with the same period in the preceding years, independent of COVID-19 prevalence (median change of –38%, range –69% to +23%; Figure 2C; Table S1, SDC, http://links.lww.com/TP/C92; P-for-trend 0.07).
The total number of waiting list deaths in the United States did not appear to increase during the first 3 months of the pandemic though it may have been slightly higher in the month of April (Tables S1 and S2, SDC, http://links.lww.com/TP/C92). Furthermore, waiting list deaths did not appear to vary by COVID-19 prevalence (P-for-trend 0.36). However, the overall waitlist mortality was low at all centers with a median number of 2 waitlist deaths (range 0–11) in this 3-month period of 2020.
DISCUSSION
Lung transplant centers in the United States continued to perform transplants during the early months of the COVID-19 pandemic, although the overall volume decreased nationally. This decrease in transplant volume was largely limited to centers in areas of moderate and high COVID-19 prevalence and was accompanied by decreases in organ availability. Nearly all centers decreased the number of patients added to the waiting list, regardless of local COVID-19 prevalence. Despite the lower transplant volume nationwide, centers did not experience a significant change in waiting list deaths compared with the same period in the preceding 5 years.
Local COVID-19 prevalence contributed to regional variations in access to lung transplantation during the early months of the COVID-19 pandemic in the United States. This differs significantly from renal transplantation in the United States1,12 and lung transplantation in France,6 in important ways: (1) all lung transplant centers continued to perform lung transplants during the early months of the pandemic, (2) areas of low COVID-19 prevalence performed expected or greater than expected numbers of lung transplants, and (3) waiting list deaths did not significantly increase. Despite multiple reports on outcomes from COVID-19 after solid organ transplantation,14-19 there is only 1 other study that has described lung transplant activity during the pandemic.8 Our findings are the first to demonstrate a highly successful risk/benefit assessment by high-volume lung transplant centers based on local COVID-19 activity.
Despite a survey suggesting that many centers were limiting lung transplantation to the sickest patients,12 median LAS at the time of transplantation did not significantly increase in the first 3 months of the pandemic.9 In fact, there seemed to be a decrease in LAS at the time of transplant at centers in areas of high COVID-19 prevalence. This may be related to the selected 3-month window. We performed analyses starting at the beginning of March to conservatively include all centers at the local peak of COVID-19, but there were considerable geographic differences in timing of this peak. Center activity in nonpeak times may have diluted changes in LAS, consistent with a dramatic increase in LAS when analyses were limited to the month of April, when the majority of high prevalence centers experienced peak COVID-19 activity. Consistent with survey reports,12 we found that 3 high COVID-19 prevalence centers completely ceased transplantation for the month of April.
While centers adjusted transplant practices based on local COVID-19 prevalence, almost all centers activated fewer patients on their waitlist than in preceding years. This may reflect limits set on outpatient testing, patient preference, decreased appreciation of disease severity and progression, or decreased referrals during the pandemic. Additional work will be necessary to identify whether these potential delays result in the listing and transplantation of sicker patients. It is reassuring that waitlist mortality did not significantly increase during the initial months of the pandemic though these results should be interpreted with caution. This may reflect early self-isolation by our high-risk patients with advanced lung disease, the short study period, or the addition of fewer patients to the waiting list. Further work is required to identify whether waiting list activations will increase over pre-COVID-19 numbers to list a “backlog” of patients as this could both further strain a limited resource and contribute to an increase in waiting list mortality.
DSAs with both moderate and high COVID-19 prevalence experienced decreased donor availability. This is consistent with reports in renal transplantation and likely reflects changes in local resource availability including intensive care unit beds and ventilators, availability of rapid COVID-19 tests for donors, or changes in physician behavior leading to fewer donor candidates.12 Interestingly, donation after circulatory death transplants occurred more commonly during the pandemic than in prior years. This may reflect an emerging change in practice with increased utilization of donation after circulatory death donors that is unrelated to the pandemic.20
This study has several limitations. First, this is a descriptive analysis of transplantation practices due to the relatively small number of procedures performed in this 3-month window. This cross-sectional analysis cannot establish causation. Changes in personnel or longer-term changes in hospital practice may have affected transplant volume during this period. Second, we used state-level data on COVID-19 prevalence, which may not reflect activity near transplant centers in larger states.21 One large volume transplant center, in particular, was characterized as being in a high COVID-19 prevalence area, when, in fact, there was low COVID-19 activity in the city and surrounding DSA. Third, this analysis is limited to the first 3 months of the pandemic, and the ongoing spread of the virus is likely to continue to alter transplant practices across the country. Further longitudinal study of the effects of these changes on lung transplant center practices will be required to inform policy changes and minimize any exacerbation in disparities in access to lung transplantation in the wake of the pandemic. Fourth, our analyses are limited to high-volume centers accounting for 64% of all lung transplantations performed during this time period. Whether lower-volume centers changed their practice in similar ways is unknown.
In summary, in the first 3 months of the COVID-19 pandemic, fewer lung transplantations were performed nationwide, driven largely by reductions in areas of high COVID-19 prevalence. There is extensive literature on the management of patients with COVID-19 after solid organ transplantation14-19; however, centers have been given little guidance on how to balance the risks and benefits of lung transplantation during the pandemic. Further investigation is required to establish whether this will result in permanent geographic disparities in access to lung transplantation, whether lung transplant activity recovers with control of the virus, and whether center behavior will be similar as the pandemic spreads to additional regions.
Supplementary Material
Footnotes
L.B. and M.R.A. participated in conception and design of the research design, writing of the article, performance of the research, data analysis, and interpretation of the work. M.E.S., J.C., L.S., H.R., F.D., J.S., B.P.S., P.L., and S.A participated in conception, design of the research design, interpretation of the work, and revising the work for critical content. M.A. participated in conception and design, interpretation of the work, and revising the work for critical content. S.P. participated in conception and interpretation of the work and revising the work for critical content.
The authors declare no conflicts of interest.
This work was supported by Parker B Francis Foundation, American Society of Transplantation, National Institutes of Health K23 HL-150280, and Cystic Fibrosis Foundation—Cystic Fibrosis Lung Transplant Consortium.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantjournal.com).
REFERENCES
- 1.Loupy A, Aubert O, Reese PP, et al. Organ procurement and transplantation during the COVID-19 pandemic. Lancet. 2020; 395:e95–e96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeFilippis EM, Sinnenberg L, Reza N, et al. Trends in US heart transplant waitlist activity and volume during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Cardiol. 2020; 5:1048–1052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Jabir A, Kerwan A, Nicola M, et al. Impact of the coronavirus (COVID-19) pandemic on surgical practice - Part 2 (surgical prioritisation). Int J Surg. 2020; 79:233–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benvenuto LJ, Anderson DR, Kim HP, et al. From the Columbia University Lung Transplant Program Geographic disparities in donor lung supply and lung transplant waitlist outcomes: a cohort study. Am J Transplant. 2018; 18:1471–1480 [DOI] [PubMed] [Google Scholar]
- 5.Ahmed O, Brockmeier D, Lee K, et al. Organ donation during the COVID-19 pandemic. Am J Transplant. 2020; 20:3081–3088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Picard C, Le Pavec J, Tissot A. Groupe Transplantation Pulmonaire de la Société de Pneumologie de Langue Française SPLF Impact of the COVID-19 pandemic and lung transplantation program in France. Respir Med Res. 2020; 78:100758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Network for Organ Sharing COVID-19 and solid organ transplant. 2020. Available at https://unos.org/covid/. Accessed August 15, 2020
- 8.Chan EG, Chan PG, Harano T, et al. Trends in lung transplantation practices across the US during the COVID-19 pandemic. Transplantation. 2021; 105:187–192 [DOI] [PubMed] [Google Scholar]
- 9.Boyarsky BJ, Po-Yu Chiang T, Werbel WA, et al. Early impact of COVID-19 on transplant center practices and policies in the United States. Am J Transplant. 2020; 20:1809–1818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valapour M, Lehr CJ, Skeans MA, et al. OPTN/SRTR 2018 annual data report: lung. Am J Transplant. 2020; 20Suppl 1427–508 [DOI] [PubMed] [Google Scholar]
- 11.Mooney JJ, Weill D, Boyd JH, et al. Effect of transplant center volume on cost and readmissions in medicare lung transplant recipients. Ann Am Thorac Soc. 2016; 13:1034–1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boyarsky BJ, Werbel WA, Durand CM, et al. Early national and center-level changes to kidney transplantation in the United States during the COVID-19 epidemic. Am J Transplant. 2020; 20:3131–3139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Covid Tracking Project 2020. Available at https://covidtracking.com/. Accessed August 15, 2020
- 14.Pereira MR, Aversa MM, Farr MA, et al. Tocilizumab for severe COVID-19 in solid organ transplant recipients: a matched cohort study. Am J Transplant. 2020; 20:3198–3205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aversa M, Benvenuto L, Anderson M, et al. From the Columbia University Lung Transplant Program COVID-19 in lung transplant recipients: a single center case series from New York City. Am J Transplant. 2020; 20:3072–3080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pereira MR, Mohan S, Cohen DJ, et al. COVID-19 in solid organ transplant recipients: initial report from the US epicenter. Am J Transplant. 2020; 20:1800–1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiss MJ, Lalani J, Patriquin-Stoner C, et al. Summary of international recommendations for donation and transplantation programs during the coronavirus disease (COVID-19) pandemic. Transplantation. 2021; 105:14–17 [DOI] [PubMed] [Google Scholar]
- 18.Crespo M, Mazuecos A, Rodrigo E, et al. Spanish Society of Nephrology COVID-19 Group Respiratory and gastrointestinal COVID-19 phenotypes in kidney transplant recipients. Transplantation. 2020; 104:2225–2233 [DOI] [PubMed] [Google Scholar]
- 19.Azzi Y, Bartash R, Scalea J, et al. COVID-19 and solid organ transplantation: a review article. Transplantation. 2021; 105:37–55 [DOI] [PubMed] [Google Scholar]
- 20.Cypel M, Levvey B, Van Raemdonck D, et al. International Society for Heart and Lung Transplantation International Society for Heart and Lung Transplantation donation after circulatory death registry report. J Heart Lung Transplant. 2015; 34:1278–1282 [DOI] [PubMed] [Google Scholar]
- 21.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020; 323:2192–2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


