Supplemental Digital Content is available in the text.
Key Words: Coronavirus (COVID-19) pandemic, inpatient admissions, elective admission, National Inpatient Sample, economic simulation model
Abstract
Background:
In anticipation of a demand surge for hospital beds attributed to the coronavirus pandemic (COVID-19) many US states have mandated that hospitals postpone elective admissions.
Objectives:
To estimate excess demand for hospital beds due to COVID-19, the net financial impact of eliminating elective admissions in order to meet demand, and to explore the scenario when demand remains below capacity.
Research Design:
An economic simulation to estimate the net financial impact of halting elective admissions, combining epidemiological reports, the US Census, American Hospital Association Annual Survey, and the National Inpatient Sample. Deterministic sensitivity analyses explored the results while varying assumptions for demand and capacity.
Subjects:
Inputs regarding disease prevalence and inpatient utilization were representative of the US population. Our base case relied on a hospital admission rate reported by the Center for Disease Control and Prevention of 137.6 per 100,000, with the highest rates in people aged 65 years and older (378.8 per 100,000) and 50–64 years (207.4 per 100,000). On average, elective admissions accounted for 20% of total hospital admissions, and the average rate of unoccupied beds across hospitals was 30%.
Measures:
Net financial impact of halting elective admissions.
Results:
On average, hospitals COVID-19 demand for hospital bed-days fell well short of hospital capacity, resulting in a substantial financial loss. The net financial impact of a 90-day COVID surge on a hospital was only favorable under a narrow circumstance when capacity was filled by a high proportion of COVID-19 cases among hospitals with low rates of elective admissions.
Conclusions:
Hospitals that restricted elective care took on a substantial financial risk, potentially threatening viability. A sustainable public policy should therefore consider support to hospitals that responsibly served their communities through the crisis.
Without effective mitigation, the novel coronavirus pandemic (COVID-19) was projected to create an unmet demand for hospital beds in the United States and strain hospitals struggling with scarce resources.1 To conserve staff and personal protective equipment, the US Centers for Disease Control and Prevention (CDC) recommended hospitals prioritize urgent and emergent care, delay elective ambulatory visits and inpatient admissions, and delay elective surgeries.2 Accordingly, most US states mandated that hospitals postpone elective admissions and other hospitals voluntarily reduced or eliminated elective admissions.3 However, elective admissions are the primary source of revenue for most US hospitals, cross-subsidizing the lower profit margins of nonelective admissions.4
Hospitals serve a vital role in their communities, especially during crises. However, making room for a potential demand surge can jeopardize their sustainability. From a hospital perspective, whether the net financial impact of eliminating profitable elective admissions in exchange for the ability to admit COVID-19 patients is sustainable (profit) or not (loss) depends on a number of factors.5 Conceptually, the demand for hospital beds-days due to COVID-19 is a function of the rate of COVID-19 hospital admissions, and the length of stay (LOS). Effective mitigation strategies like social distancing can reduced the incidence of infection and, consequently, the number of admissions. In addition, demand could fail to meet hospital capacity if hospitals reduce elective admissions ahead of the demand surge or if the admission rate is otherwise lower than expected. Hospitals’ useable capacity (ie, capacity not dedicated to nonelective admissions) can be maximized by prepping normally unoccupied beds, reducing or eliminating elective admissions, and taking emergency actions to create additional bed-days (eg, doubling occupancy of hospital rooms). Paradoxically perhaps, hospitals with higher rates of elective admissions and unoccupied beds have a greater capacity to meet a demand surge. Furthermore, hospitals’ capacity can be constrained by high rates of absenteeism due to illness among nurses and doctors, limited access to ventilators, a shortage of personal protective equipment, or a scarcity of anesthetic medications or other pandemic-related social factors.6,7 Finally, COVID-19 admissions may yield a lower profit margin per case compared with elective admissions because they represent disproportionately older patients, are more likely to be reimbursed by Medicare, are not associated with surgical procedures, and because the LOS generally increases with age.8,9 In contrast, if demand remains high and COVID-19 admissions are accompanied by a shorter LOS, hospitals will benefit by caring for more patients.
Given these uncertainties, we created a simulation model to estimate the demand surge for hospital beds due to COVID-19 and to determine the net financial impact to hospitals caused by eliminating elective admissions in order to meet the demand surge. The results from these analyses can inform hospitals about the magnitude and key drivers of financial impact that they might realize in their specific circumstances. In addition, the analysis provides information to policy makers considering how to optimize resources or distribute stimulus reimbursement in the context of the current or future demand surges.
METHODS
From a hospital perspective, we created an economic simulation model to estimate net financial impact of suspending elective admissions in favor of COVID-19 admission over a 90-day period. Combining US population demographics, disease characteristics, and cost estimates from a variety of sources, we estimated a standard profit/loss equation to consider the fundamental trade-off between maximizing a higher volume of lower profit COVID-19 admissions versus maintaining a lower volume of relatively higher profit elective admissions. As with many simulation models, several inputs represent uncertain information, are subject to variable state policy, or are heterogeneous across hospitals. For this reason, model inputs were sourced with estimated variances and integrated into the profit (loss) estimate with confidence intervals (CIs). In addition, deterministic sensitivity analyses allowed us to explore the extremes of the net financial benefit based on varying assumptions for (a) hospitals’ unoccupied bed rate, (b) hospitals’ normal elective admission rate, (c) impact of medical worker absenteeism, and (d) the level by which COVID-19 demand for bed-day could fail to reach capacity.
Data Sources for Model Inputs
The following sources inform our simulation model:
The National Inpatient Sample (NIS) is a complex national sample of hospital discharges representative of US inpatient care.10 As the largest publicly available all-payer inpatient discharge database in the United States, NIS was used to estimate strata-specific hospital costs and LOS. Strata were defined by age group, US census division, primary payer, and elective versus coronavirus admissions. Influenza admissions were used as a surrogate for average costs and LOS for COVID-19 and calibrated based on recently published COVID-19 reports (described below). We used NIS data from 2017 because it is the most recent data available. Released annually by the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project, NIS is a uniform administrative dataset describing discharges from 20% sample of the hospitals that are part of the American Hospital Association (AHA). All discharges from each sampled hospital are included. Stratification by US region, urban or rural location, teaching status, ownership, and bed size is used to perform a complex sampling strategy that allows for unbiased national estimates of admissions, including hospital charges, LOS, patient demographics, and diagnosis codes from the International Classification of Diseases, version 10. Cost-to-charge ratio files accompany NIS to estimate operational costs based on Medicare Cost Reports.
US Census data were used to aggregate age-specific US resident population, by US Census Division.11 The 9 US Census Divisions are defined in Appendix A1, Supplemental Digital Content 1 (http://links.lww.com/MLR/C170). We limited our analysis to those over age 20 or older, as admissions in those under 20 is relatively uncommon and because the reliability of admissions for those under age 20 within the NIS is uncertain. The population count was grouped by age as 20–39, 40–59, 60–79, 80+.
The Annual Survey of the AHA from 2015 was used to describe the number of hospitals within each state, the total number of beds within hospitals, the total annual admissions, and total inpatient bed-days.12 We derived the total capacity in bed-days, taken as the total number of beds multiplied by 90 days, the time period of interest. Hospitals’ normal occupancy rate—the ratio of inpatient days over total capacity—was varied in our sensitivity analysis.
We multiplied reimbursement-over-cost factors reported by Braithwaite and colleagues, which focused on the H1N1 pandemic in the Fall of 2009, to estimate profit (loss) for commercial (24%), Medicare (0%), Medicaid (−19%), and others payers including self-pay and charity case (−13%). Braithwaite et al5 cite MedPAC (2006) for these factors.
State-specific details, including the number of hospitals and beds were also obtained from the Kaiser Family Foundation.13 Reassuringly, total beds were consistent with the AHA.
The age-specific cumulative COVID-19 hospitalization rate was reported on August 7 by the CDC: 137.6 per 100,000, with the highest rates in people aged 65 years and older (378.8 per 100,000) and 50–64 years (207.4 per 100,000).14
Defining Capacity
As shown in Figure 1, total hospital capacity as measured by bed-days can be thought of as the sum of elective, nonelective, and unoccupied beds. We assume that nonelective admissions are unchanged because they are not the target of state or hospitals policies to maximize capacity of bed-days for COVID-19 cases. Thus, availability of beds to accommodate COVID-19 cases is taken as the sum of elective and normally unoccupied bed-days. We assumed that hospitals could create an additional 10% capacity by emergent actions such as doubling patients to a room. We then compared available capacity in bed-days to estimated demand for bed-days caused by a surge in admission rates for COVID-19. We describe excess demand as the extent that COVID-19 demand for bed-days exceeded available capacity. Excess demand could be negative if the available capacity exceeds the demand from COVID-19 patients.
FIGURE 1.
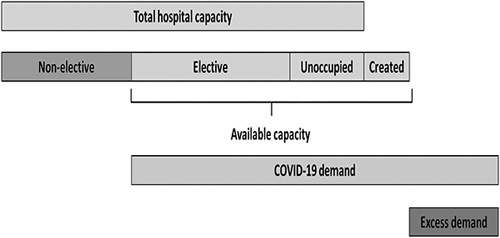
Defining hospital capacity and excess COVID-19 demand for bed-days. Source: Author’s conceptual model of hospital demand and capacity.
Type of Admission and COVID-19 Cases
A variable reported by hospitals within NIS indicates admissions that are deemed to be classified as “elective” versus “non-elective.” Nonelective admission included emergent, urgent, newborn, and traumatic admissions. We used this variable as provided in NIS to estimate the proportion of all admissions that were deemed elective. We estimate a mean elective admission rate of 20%, ranging across US Census Divisions from 17% to 27%.
Estimating Admission Characteristics for COVID-19 Cases
Admissions coded with a primary ICD-10 diagnosis code for influenza with or without pneumonia served as a proxy to describe mean costs and LOS for COVID-19 cases (Appendix Table A2, Supplemental Digital Content 1, http://links.lww.com/MLR/C170).15 As a proxy for COVID-19 LOS and cost, influenza likely underestimates the complexity associated with COVID-19. Therefore, we calibrated the proxy derived LOS data to COVID-19-specific LOS of 11.3 days (95% CI, 0.8–32.9), as reported by Lewnard et al.16 The mean COVID-19 LOS was 2.13 times greater than the influenza proxy.
Hospital Reimbursement
Estimating hospital reimbursement required several calculations. Total hospital charges, excluding professional fees and postacute care, are provided with NIS. We applied hospital-specific cost-to-charge ratios from the Healthcare Cost and Utilization Project to derive costs. Within each admission type, we estimated strata-specific mean costs using survey-weighted generalized linear regression with a γ-distribution and log link, an approach that is robust to typically highly skewed health care cost distributions (as described above, strata were defined by age group, US Census Division, and payer type).17 On the basis of payer type, we then applied the income-over-cost factors provided by Braithwaite to estimate hospital income. We then increased estimated income by 20% across all payers to account for additional reimbursement to hospitals included in the Coronavirus Aid, Relief, and Economic Security (CARES) Act.18 As with LOS, we calibrated proxy-based costs using recently published cost data specific to COVID-19 of $15,792 (Medicare), $11,390 (Medicaid), $38,059 (commercial), and $15,792 (other/uninsured). The ratio of COVID-specific to proxy-based costs were 1.37 (Medicare), 0.76 (Medicaid), 3.33 (commercial), and 1.47 (other/uninsured).19 Our estimates of admission cost were similar to COVID-19-specific costs reported by Bartsch et al.20 Finally, within each admission type, mean income for the admissions was divided by the LOS to acquire an average income per bed-day, assuming a uniform profit per bed-day.
Estimating Hospital Demand for Bed-Days
We applied the CDC’s reported rate of COVID-19-related hospital admission to the population from the US Census to estimate the number of COVID-19 admissions. To estimate the surge in demand for bed-days due to COVID-19, we then multiplied the number of COVID-19 admissions by the average strata-specific LOS.
Health Care Provider Absenteeism
Even if bed-days are made available for COVID-19 patient admissions, nurse and physician absenteeism due to sickness could be a constraint to this capacity. In addition to a reduction in available medical workforce, capacity constraints could be due to scarcity of personal protective equipment or ventilators. Although these constraints could take a variety of forms, we operationalized them in our model by assuming reductions in available capacity ranging from 0% to 40%.
Analysis
Our Monte Carlo simulation model calculated the potential demand for hospital bed-days due to COVID-19 compared with the available capacity of bed-days by US states over a 90-day period. Using estimates for COVID-19 admissions and LOS for individuals infected by COVID-19, we calculated the total number of bed-days that would be needed to accommodate these COVID-19 patients. We compared these estimates to available capacity to determine the excess demand for bed-days caused by COVID-19 patients after filling elective, unoccupied, and newly created bed-days. Finally, we used the reimbursement rates across payers to calculate the net financial gains or losses to hospitals admitting COVID-19 patients.
A profit (loss) equation was calculated as the difference in the population-weighted ”)(“ω”) sum of 144 strata-specific daily income for bed use between maintaining elective cases, compared with the strategy of maximizing availability for COVID-19 cases. Strata were defined by the combination of age groups (4 levels, “i”), US Census Division (9 levels, “j”), and payer type (4 groups, “k”), for a total of 144 strata (“s”). Specifically, profit (loss) equations were calculated separately for the scenario in which elective patients were admitted as usual (“u,” equation (1)) and for the COVID-19 scenario in which bed capacity was increased, elective admissions were suspended, and COVID-19 patients were admitted instead (“c,” equation (2)). We then calculated the incremental profit as the difference between the estimated profit under these 2 scenarios (equation (3)). Volume was defined as the number of hospital bed-days over a 90-day period occupied by elective or COVID-19 patients depending on the scenario.
| 1 |
| 2 |
| 3 |
We analyzed our model using 10,000 Monte Carlo simulations in which parameter estimates were drawn from distributions based on the estimated mean and SDs for our input parameters. We conducted several multiway sensitivity analyses to express the results over a range for the rate of absenteeism, the rate of elective procedures, the rate of normally unoccupied bed-days, the proportion of hospital admissions from commercially insured cases, and over a range of reduced COVID-19 demand.
RESULTS
COVID-19 Demand
Inputs regarding admission rates and inpatient utilization were representative of the US population. Our base case analysis relied on a COVID-19 admission rate of 378.8 per 100,000 among those aged 65 years and older and 207.4 per 100,000 among those 20–64 years. On average, elective admissions accounted for 20% of total hospital admissions, and 30% of hospital beds are unoccupied under normal circumstances. Given the observed COVID-19 hospital admission rate, we estimate that aggregated national demand will reach 13.9% of the available national capacity, leaving 86.1% unused. Increased demand for bed-days sharply increases with an increased COVID-19 admission rates, a greater rate of absenteeism, a lower rate of unoccupied beds, and lower rates of elective admissions (Table 1). For example, a hospital with 0% absenteeism, 20% elective admissions, and 30% unoccupied beds could expect an excess capacity of 6477 bed-days. Excess capacity ranged from about 11,000 bed-days over a 90-day period in Delaware to about 3000 in Montana (Appendix Fig. A3, Supplemental Digital Content 2, http://links.lww.com/MLR/C171).
TABLE 1.
Difference in Demand Versus Capacity for Hospitals Bed-Days During a 90-Day Surge of COVID-19, by Rate of Absenteeism and Capacity
| Unoccupied Capacity | Unoccupied Capacity | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Absenteeism | 50% | 40% | 30% | 20% | 10% | 50% | 40% | 30% | 20% | 10% |
| Rate (%) | Hospital rate of elective admission=15% | Hospital rate of elective admission=20% | ||||||||
| 0 | −8663 | −7206 | −5748 | −4291 | −2834 | −9391 | −7934 | −6477 | −5020 | −3563 |
| 10 | −7716 | −6404 | −5093 | −3781 | −2470 | −8371 | −7060 | −5748 | −4437 | −3126 |
| 20 | −6768 | −5603 | −4437 | −3271 | −2105 | −7351 | −6186 | −5020 | −3854 | −2688 |
| 30 | −5821 | −4801 | −3781 | −2761 | −1741 | −6331 | −5311 | −4291 | −3271 | −2251 |
| 40 | −4874 | −4000 | −3126 | −2251 | −1377 | −5311 | −4437 | −3563 | −2688 | −1814 |
| Rate (%) | Hospital rate of elective admission=25% | Hospital rate of elective admission=30% | ||||||||
| 0 | −10,120 | −8663 | −7206 | −5748 | −4291 | −10,849 | −9391 | −7934 | −6477 | −5020 |
| 10 | −9027 | −7716 | −6404 | −5093 | −3781 | −9683 | −8371 | −7060 | −5748 | −4437 |
| 20 | −7934 | −6768 | −5603 | −4437 | −3271 | −8517 | −7351 | −6186 | −5020 | −3854 |
| 30 | −6841 | −5821 | −4801 | −3781 | −2761 | −7351 | −6331 | −5311 | −4291 | −3271 |
| 40 | −5748 | −4874 | −4000 | −3126 | −2251 | −6186 | −5311 | −4437 | −3563 | −2688 |
Negative values indicate excess capacity of hospital beds. Analysis based on a hospital admission rate of 207/100,000 among those age 20–60 and 379/100,000 among those age 60+.
Source: Author’s results from simulation analysis.
Hospital Financial Impact
In our base case analysis, the strategy to replace elective admissions with COVID-19 admissions yielded a net financial loss across all levels of elective admission rates (Table 2). Because demand was below capacity, these findings were not sensitive to the rates of unoccupied beds or absenteeism. For example, a hospital normally operating with 20% elective admissions could expect a 90-day loss of $1,916,278 (95% CI, $1,914,108–$1,918,448) over the strategy of not eliminating elective admissions. Net financial losses were greater for hospitals with higher rates of elective admissions.
TABLE 2.
Estimated Financial Impact for an Average US Hospital Accommodating a 90-Day Demand Surge Due to COVID-19, by Rate of Elective Admissions
| Hospital Rate of Elective Admission | ||||
|---|---|---|---|---|
| Outcome | 15% | 20% | 25% | 30% |
| Financial impact | −$1,256,574 | −$1,916,278 | −$2,575,981 | −$3,235,685 |
Analysis based on a hospital admission rate of 207/100,000 among those age 20–60 and 379/100,000 among those age 60+, unoccupied bed capacity of 20%, and absenteeism set at 0%. Because demand did not reach capacity, these results were not sensitive to varying rates of absenteeism or unoccupied capacity.
Source: Author’s results from simulation analysis.
Demand Versus Capacity
Importantly, demand for COVID beds might remain below capacity if the admission rate of COVID-19 declines or if hospitals eliminate elective procedures well ahead of the COVID-19 demand curve. A lower than expected demand could result from successful effects of social distancing, for example. We performed an additional sensitivity analysis to describe the effect of COVID-19 demand for hospitals bed-days over a range of admission rates (Table 3). Not surprisingly, if COVID-19 demand does not reach available capacity (elective beds+unoccupied beds+10% added capacity), hospitals’ net financial loss is substantial. For example, if actual demand reaches only 30% of available capacity, an average hospital with 0% absenteeism and 20% elective cases, could expect a 90-day net financial loss of $1,105,358 (95% CI, $1,104,018–$1,106,698). The net financial loss substantially increases with absenteeism, a higher elective admission, and a lower rate of demand.
TABLE 3.
Estimated 90-Day Financial Impact for an Average US Hospital Accommodating COVID-19 Cases Under a Scenario Where Demand Surge Falls Short of Capacity, by Rate of Available Capacity Filled, Elective Admissions, and Medical Worker Absenteeism
| Percent of Available Capacity Filled | Percent of Available Capacity Filled | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Absenteeism | 10 | 20 | 30 | 40 | 50 | 10 | 20 | 30 | 40 | 50 |
| Rate (%) | Hospital rate of elective admission=15% | Hospital rate of elective admission=20% | ||||||||
| 0 | −$1,531,852 | −$1,084,594 | −$637,336 | −$190,078 | $257,180 | −$2,127,662 | −$1,616,510 | −$1,105,358 | −$594,205 | −$83,053 |
| 10 | −$1,576,578 | −$1,174,046 | −$771,514 | −$368,981 | $33,551 | −$2,178,777 | −$1,718,740 | −$1,258,703 | −$798,666 | −$338,629 |
| 20 | −$1,621,304 | −$1,263,497 | −$905,691 | −$547,885 | −$190,078 | −$2,229,892 | −$1,820,970 | −$1,412,049 | −$1,003,127 | −$594,205 |
| 30 | −$1,666,030 | −$1,352,949 | −$1,039,868 | −$726,788 | −$413,707 | −$2,281,007 | −$1,923,201 | −$1,565,394 | −$1,207,588 | −$849,781 |
| 40 | −$1,710,755 | −$1,442,401 | −$1,174,046 | −$905,691 | −$637,336 | −$2,332,122 | −$2,025,431 | −$1,718,740 | −$1,412,049 | −$1,105,358 |
| Rate (%) | Hospital rate of elective admission=25% | Hospital rate of elective admission=30% | ||||||||
| 0 | −$2,723,471 | −$2,148,425 | −$1,573,379 | −$998,333 | −$423,287 | −$3,319,280 | −$2,680,340 | −$2,041,400 | −$1,402,460 | −$763,520 |
| 10 | −$2,780,976 | −$2,263,434 | −$1,745,893 | −$1,228,351 | −$710,810 | −$3,383,174 | −$2,808,128 | −$2,233,082 | −$1,658,036 | −$1,082,990 |
| 20 | −$2,838,480 | −$2,378,443 | −$1,918,407 | −$1,458,370 | −$998,333 | −$3,447,068 | −$2,935,916 | −$2,424,764 | −$1,913,612 | −$1,402,460 |
| 30 | −$2,895,985 | −$2,493,453 | −$2,090,920 | −$1,688,388 | −$1,285,856 | −$3,510,962 | −$3,063,704 | −$2,616,446 | −$2,169,188 | −$1,721,930 |
| 40 | −$2,953,489 | −$2,608,462 | −$2,263,434 | −$1,918,407 | −$1,573,379 | −$3,574,856 | −$3,191,492 | −$2,808,128 | −$2,424,764 | −$2,041,400 |
Analysis based on a hospital admission rate of 207/100,000 among those age 20–60 and 379/100,000 among those age 60+, normally unoccupied bed capacity fixed at 20%. Available capacity is defined as unoccupied beds+typical elective beds+10% created additional capacity.
Source: Author’s results from simulation analysis.
We also performed 2-way sensitivity analysis to examine the impact over a range of COVID-19 admission rates, and the proportion of hospital admissions that were among commercially insured patients (Table 4). As expected, for an average hospital that added capacity by eliminating elective admissions, a lower COVID-19 admission rate and a higher proportion of commercially insured patients results in substantial greater financial losses.
TABLE 4.
Estimated 90-Day Financial Impact for an Average US Hospital Accommodating COVID-19 Cases, by Rates of Hospital Admission
| Population rate of COVID-19 hospital admissions | Percent of Hospital Admissions From Patients With Commercial Insurance | |||||
|---|---|---|---|---|---|---|
| Age 20–60 | Age 60+ | 43.5 | 38.5 | 33.5 | 8.5 | 23.5 |
| 50/100,000 | 250/100,000 | −$2,281,901 | −$2,058,834 | −$1,797,472 | −$1,583,959 | −$1,367,565 |
| 100/100,000 | 300/100,000 | −$2,143,609 | −$1,924,943 | −$1,704,747 | −$1,440,670 | −$1,236,968 |
| 150/100,000 | 350/100,000 | −$2,016,020 | −$1,788,428 | −$1,559,032 | −$1,345,700 | −$1,110,784 |
| 200/100,000 | 400/100,000 | −$1,895,330 | −$1,645,518 | −$1,438,064 | −$1,210,128 | −$994,078 |
| 250/100,000 | 450/100,000 | −$1,812,871 | −$1,562,740 | −$1,338,505 | −$1,104,155 | −$882,565 |
This 2-way sensitivity analysis was performed while fixing absenteeism at 0%, elective admissions and normally unoccupied beds at 20% each.
Sensitivity analysis based on fixing absenteeism at 0%, elective admissions and normally unoccupied beds at 20% each.
Source: Author’s results from simulation analysis.
CONCLUSIONS
Given the observed rate of hospital admissions for COVID-19, we estimate that an average hospital’s bed capacity remained well above demand for beds due to COVID-19. Although the actual demand-to-capacity might be variable for a specific hospital, the finding might be reflective of successful mitigation such as social distancing. Owing to the excess capacity, our model predicts that, on average, hospitals will encounter a net financial loss over a 90-day period, with a magnitude of loss that is sensitive to COVID-19 admissions rates, a hospital’s normal rate of elective admissions, staff absenteeism, and proportion of commercially insured patients. Hospitals that eliminate elective cases will face a substantially greater financial loss if community mitigation strategies, such as social distancing, effectively reduce the admission rate. Furthermore, by assuming that nonelective admissions are immutable during a COVID-19 surge, our results are likely conservative. Admissions that hospital typically report as “non-elective,” which includes trauma cases, might actually decline due to reduced exposure to accidents or having some degree of discretion. The effects of this possibility can be seen by interpreting a higher rate of elective admission in our sensitively analysis.
Our results are broadly consistent with other groups that have modelled the demand surge or its financial impact on the US health system.5,21–23 Arguing for a greater stimulus reimbursement to hospitals treating COVID-19 cases, Strata Decision Technology, for example, demonstrated a net financial loss to hospitals due to a marginal revenue loss caused by deferred elective inpatient cases. Our findings add to this result by demonstrating a potentially greater financial loss if the expected surge in demand does not reach added capacity. Paradoxically, for hospitals that reduced elective cases in anticipation of a demand surge, the more successful mitigation strategies such as social distancing are at reducing transmission of COVID-19, the larger the financial losses are. Especially if the demand surge does not reach added capacity, additional financial relief from Federal or State stimulus might be justified.
As with most simulation models, the results of our analysis should be considered in the context of key assumptions for the inputs that we relied on. These include (a) the reliance on CDC reported COVID-19 admissions rates, (b) use of ICD-10 codes for admissions associated with influenza with/without pneumonia as a proxy for estimating LOS and hospital costs for COVID-19 admissions, (c) an estimate that elective admissions account for 20% of total hospital admissions, (d) that nonelective admissions have no influence on available beds, and (e) that hospital costs are uniform across the hospital bed-days, although we acknowledge that daily costs are often greater in the first days of admission than in the later days. For each of these inputs we summarized the best available knowledge and cited their sources. We also performed a sensitivity analysis to explore the effects over a range of credible values where there was greater uncertainty for specific inputs.
Additional limitations should be accounted for with ongoing efforts. Although our sensitivity analysis illustrated the effect when demand fails to meet capacity, we did not explicitly account for the time-varying rise in demand. Many hospitals cancelled elective admissions days or weeks in advance of any increased demand. These unused admissions days represent a significant loss in revenue. Our analysis is also strictly focused on the profit/loss associated with inpatient admissions. However, many health systems also reduced or eliminated ambulatory and office-based care. Because of this, our estimates on financial impact are likely optimistic from a hospital perspective. Finally, some might argue that the financial loss is minimized once hospitals can ramp up elective admissions again and “make up” any revenue losses. However, addressing the “pent up” demand for elective admissions is not likely to be easily achieved as it will be rate limited by availability of operating rooms and providers.
On average, halting elective inpatient admissions resulted in a net financial loss over a 90-day period, but is sensitive to hospitals’ normal rates of elective admissions, COVID-19 admission rates, and rate of commercially insured admissions. Under favorable circumstances, hospitals with low elective admission rates that maximize capacity by eliminating or reducing elective admissions in anticipation of a demand surge for COVID-19 cases appear to have a slightly favorable probability for a relatively small net financial benefit. However, this opportunity quickly deescalates with unfavorable conditions, yielding higher probabilities for a relatively larger magnitude of net financial loss.
The net financial impact should be carefully considered by hospitals considering steps to increase capacity, and by policy makers considering how to best support such hospitals. Hospitals that created added capacity took on a substantial financial risk that potentially threatened their viability. A sound and sustainable public policy should therefore consider greater support to hospitals that responsibly served their communities through the crisis.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Footnotes
Coauthors B.I.M. and R.E.N. receive partial salary support from an AHRQ-Funded R01 (Grant #R01HS024714) paid directly to the institution. The remaining authors declare no conflict of interest.
Contributor Information
Brook I. Martin, Email: Brook.Martin@hsc.utah.edu.
Darrel S. Brodke, Email: Darrel.Brodke@hsc.utah.edu.
Fernando A. Wilson, Email: fernando.wilson@utah.edu.
Nathorn Chaiyakunapruk, Email: Nathorn.Chaiyakunapruk@utah.edu.
Richard E. Nelson, Email: Richard.Nelson@utah.edu.
REFERENCES
- 1.Ferguson N, Laydon D, Nedjati-Gilani G, et al. Report 9: Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID19 Mortality and Healthcare Demand. London, UK: Medical Research Council. 2020:1–20. Available at: https://spiral.imperial.ac.uk:8443/handle/10044/1/77482. Accessed October 6, 2020. [Google Scholar]
- 2.National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases Healthcare Facilities: Preparing for Community Transmission. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html. Accessed October 6, 2020.
- 3.Ambulatory Surgery Center Association. State guidance on elective surgeries. 2020. Available at: https://www.ascassociation.org/asca/resourcecenter/latestnewsresourcecenter/covid-19/covid-19-state. Accessed October 6, 2020.
- 4.David G, Lindrooth RC, Helmchen LA, et al. Do hospitals cross-subsidize? J Health Econ. 2014;37:198–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braithwaite S, Friedman B, Mutter R, et al. Microsimulation of financial impact of demand surge on hospitals: the H1N1 influenza pandemic of fall 2009. Health Serv Res,. 2013;48(2, pt 2):735–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barr HL, Macfarlane JT, Macgregor O, et al. Ethical planning for an influenza pandemic. Clin Med (Lond). 2008;8:49–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martinese F, Keijzers G, Grant S, et al. How would Australian hospital staff react to an avian influenza admission, or an influenza pandemic? Emerg Med Australas. 2009;21:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project, National Inpatient Database, HCUP NIS Database Documentation. 2019. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed October 6, 2020.
- 11.Ruggles S Flood S Goeken R, et al. IPUMS USA: Version 10.0 [dataset]. University of Minnesota, ed. 2020. Available at: 10.18128/D010.V10.0. Accessed October 6, 2020. [DOI]
- 12.Health Forum, American Hospital Association. AHA Annual Survey Database. 2015. Available at: https://www.ahadata.com/aha-annual-survey-database. Accessed October 6, 2020.
- 13.Keiser Family Foundation. Providers and service use indicators. 2020. Available at: https://www.kff.org/state-category/providers-service-use/. Accessed October 6, 2020.
- 14.Centers for Disease Control and Prevention. COVIDView Summary Ending on, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/08072020.html. Accessed October 6, 2020.
- 15.National Center for Health Statistics: Center for Disease Control and Preventions. World Health Organization’s International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Available at: https://www.cdc.gov/nchs/icd/icd10cm.htm. Accessed October 6, 2020.
- 16.Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mihaylova B, Briggs A, O’Hagan A, et al. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20:897–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.H.R. 748 116th Congress (2019–2020). Coronavirus Aid, Relief, and Economic Security Act or the CARES Act. 2020. Available at: https://www.congress.gov/bill/116th-congress/house-bill/748. Accessed October 6, 2020.
- 19.Sloan C Markward N Young J, et al. . COVID-19 hospitalizations projected to cost up to $17B in US in 2020. Available at: https://avalere.com/insights/covid-19-hospitalizations-projected-to-cost-up-to-17b-in-us-in-2020. Accessed December 22, 2020.
- 20.Bartsch SM, Ferguson MC, McKinnell JA, et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff (Millwood). 2020;39:927–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strata Decision Technology. Report: Hospitals Face Massive Losses on COVID-19 cases even with proposed increase in Federal reimbursement. 2020. Available at: https://www.stratadecision.com/blog/report-hospitals-face-massive-losses-on-covid-19-cases-even-with-proposed-increase-in-federal-reimbursement/. Accessed October 6, 2020.
- 22.Qventus. Predicting the Effects of the COVID Pandemic on US Health System Capacity. 2020. Available at: https://qventus.com/blog/predicting-the-effects-of-the-covid-pandemic-on-us-health-system-capacity/#tableau-3. Accessed October 6, 2020.
- 23.Weissman GE, Crane-Droesch A, Chivers C, et al. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann Intern Med. 2020;173:21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


