Supplemental Digital Content is available in the text
It is unclear if percutaneous transforaminal endoscopic discectomy (PTED) has comparable outcomes compared with open microdiscectomy (OM). Multiple online databases were systematically searched up to April 2020 for prospective studies. There is moderate quality evidence suggesting no difference in leg pain or functionality at intermediate and long-term follow-up between PTED and OM in the treatment of lumbar disk herniation.
Keywords: endoscopic discectomy, lumbar disc herniation, sciatica, systematic review and meta-analysis
Abstract
Study Design.
Systematic review and meta-analysis.
Objective.
To give a systematic overview of effectiveness of percutaneous transforaminal endoscopic discectomy (PTED) compared with open microdiscectomy (OM) in the treatment of lumbar disk herniation (LDH).
Summary of Background Data.
The current standard procedure for the treatment of sciatica caused by LDH, is OM. PTED is an alternative surgical technique which is thought to be less invasive. It is unclear if PTED has comparable outcomes compared with OM.
Methods.
Multiple online databases were systematically searched up to April 2020 for randomized controlled trials and prospective studies comparing PTED with OM for LDH. Primary outcomes were leg pain and functional status. Pooled effect estimates were calculated for the primary outcomes only and presented as standard mean differences (SMD) with their 95% confidence intervals (CI) at short (1-day postoperative), intermediate (3–6 months), and long-term (12 months).
Results.
We identified 2276 citations, of which eventually 14 studies were included. There was substantial heterogeneity in effects on leg pain at short term. There is moderate quality evidence suggesting no difference in leg pain at intermediate (SMD 0.05, 95% CI –0.10–0.21) and long-term follow-up (SMD 0.11, 95% CI –0.30–0.53). Only one study measured functional status at short-term and reported no differences. There is moderate quality evidence suggesting no difference in functional status at intermediate (SMD –0.09, 95% CI –0.24–0.07) and long-term (SMD –0.11, 95% CI –0.45–0.24).
Conclusion.
There is moderate quality evidence suggesting no difference in leg pain or functional status at intermediate and long-term follow-up between PTED and OM in the treatment of LDH. High quality, robust studies reporting on clinical outcomes and cost-effectiveness on the long term are lacking.
Level of Evidence: 2
Sciatica is a frequently used term to describe radiating leg pain. It is mostly caused by lumbar disc herniation (LDH).1,2 Even though the natural course of sciatica is favorable and most cases respond to conservative treatment, surgery is deemed necessary in some cases.3 The current standard procedure to decompress the nerve root by removing disc fragments, is open microdiscectomy (OM).4
In attempts to reduce the surgical invasiveness, techniques which use endoscopes to remove disc fragments were developed. The expectation was that by causing less tissue damage during surgery, patients would have less postoperative back pain, recover sooner from surgery, and have shorter duration of hospitalization.5 Development of methods facilitating insertion of surgical endoscopes into the safe entry zone in the neuroforamen formed (also known as Kambin triangle), enabled the development of percutaneous transforaminal endoscopic discectomy (PTED).6,7 During PTED no paraspinal muscles are deattached from their origin and bony anatomy is affected limited. Previous studies which have examined PTED demonstrated favorable clinical outcomes, with the result that percutaneous full-endoscopic discectomy has made its way into small scale clinical practice.4,8,9
A previous review published in 2009 which compared the effects of PTED with OM concluded that the quality of the evidence regarding effectiveness of PTED is low10 and PTED could not be recommended for the treatment of LDH. Since then large observational studies as well as randomized controlled trials (RCTs) have examined the effects of endoscopic discectomy techniques versus OM, which have been summarized in recent reviews, including meta-analyses.11–16 Despite similar aims, these meta-analyses differ in methodology. As a result, the uncertainty regarding the effectiveness of PTED compared with OM remains.
In 2014, a systematic review was published by our research group, comparing minimally invasive surgery with OM.17 Due to the low number and high risk of bias of the included studies as well as small sample sizes, no pooled effect estimates were calculated for the effects of PTED versus OM.18 Preliminary analysis of studies published since then, suggested that there were sufficient studies to warrant an update of our previous review, focusing on the effects of PTED versus OM in the treatment of LDH.
METHODS
This review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.18–20 This study was registered in the international prospective register of systematic reviews (Prospero CRD 42020177053).
Inclusion Criteria for Studies
Studies were considered to be eligible according to the following inclusion criteria: (1) prospective studies, including RCTs and quasi-randomized studies (e.g., randomization which could include allocation by alternating the date of birth); (2) compared PTED with OM in the treatment of sciatica caused by a primary LDH; (3) measured one of the clinical outcomes (i.e., visual analogue scale [VAS] for leg pain, back pain, functional status, improvement, work status), surgical outcomes (i.e., blood loss, length of stay, complications, reoperations); radiological or biochemical outcomes; or costs (i.e., costs of interventions, health care utilization, total costs); (4) were published in English, German, or Dutch. Retrospective studies were excluded because the level of evidence provided by these studies is low compared with prospective observational and randomized studies.
Intervention
PTED is defined as a lateral, full-endoscopic approach in which the disc fragments are removed through the neuroforamen. PTED is usually performed under local anesthesia.21
Control Group
OM is defined as removing the disc fragments from an open transflaval approach by laminotomy.22 OM is usually performed under general anesthesia.
Search Strategy
An experienced librarian conducted a systematic search using a combination of terms related to endoscopic techniques, percutaneous techniques, and LDH. As this study updates our previously published review, the previous search terms were optimized and this search only included studies published after January 2013, the search date used by Kamper et al.17 The updated search is available in supplementary Table 1. On the April 20, 2020 MEDLINE, PubMed, Embase, Emcare, Web of Science, and the Cochrane library were systematically searched for eligible articles. In addition, additional eligible articles were searched for by reference checking the included studies. All available records were screened by two reviewers independently based on title and/or abstract. In case of disagreements, a third independent reviewer was consulted. Following this step, two authors independently screened the full-text of the manuscripts based on the inclusion criteria. Disagreements were resolved through consensus with the involvement of a third reviewer.
Data Collection and Analysis
Two authors independently extracted all data in a prespecified spreadsheet. Discrepancies in extraction were resolved by consensus. This spreadsheet included (1) study characteristics; (2) clinical outcomes; (3) surgical outcomes; (4) biochemical outcomes, namely c-reactive protein (CRP) and creatine kinase (CK) which are indicators of inflammation and muscle injury, respectively; (5) radiological outcomes (6) costs; and (7) timing of the outcomes.
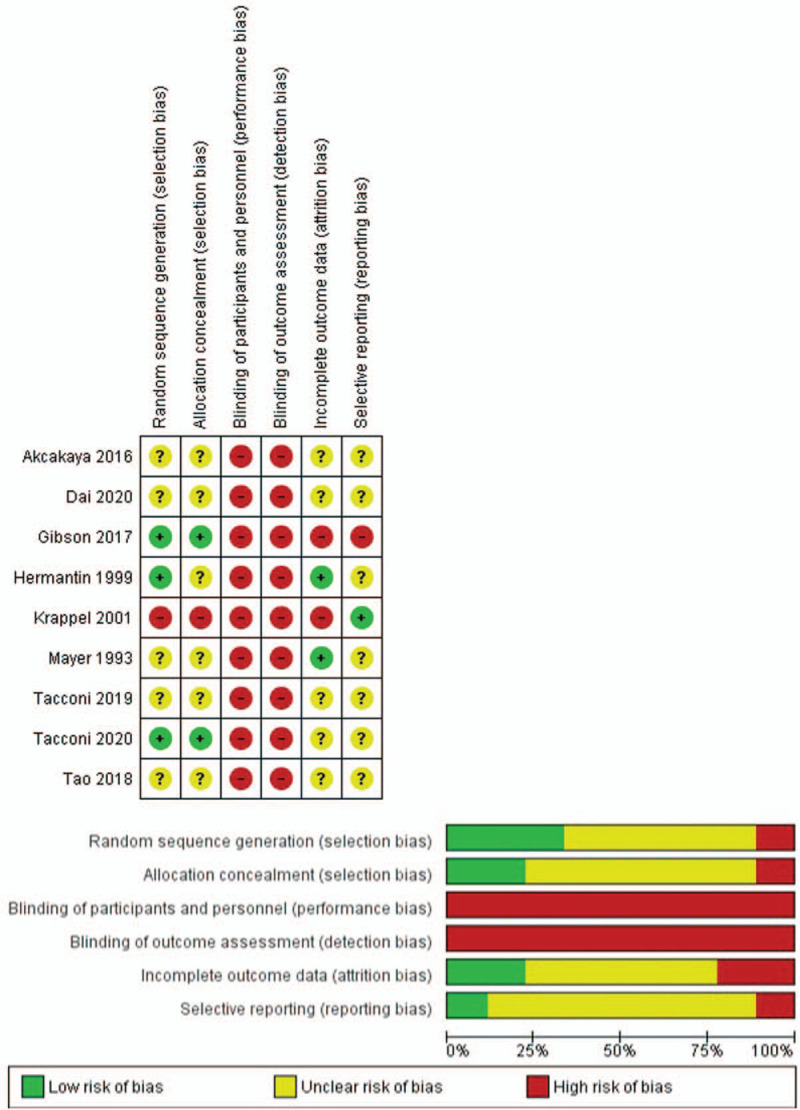
Assessment of Risk of Bias
Risk of bias analysis was performed for only RCTs using the criteria recommended by the Cochrane Collaboration.23 These criteria cover selection bias, performance bias, attrition bias, detection bias, and selective outcome reporting bias. Two authors independently scored these criteria as: low risk of bias, high risk of bias, or unclear. Disagreements were resolved by consensus and if necessary, by evaluation of a third author.
Bias Across Studies
Conflict of interest was determined for all included studies based upon the information provided by the authors in their publication. Publication bias was assessed using a funnel plot and based upon symmetry.
Data Analyses
Measures of Treatment Effect
Only data from RCTs were considered for the meta-analysis, as the observational studies may be of limited value due to the risk of selection bias. Primary continuous outcomes (leg pain and functional status) were expressed as a standardized mean difference (SMD), including 95% confidence intervals (CI). A negative effect size indicates that PTED is more beneficial than OM, meaning subjects have less pain or better functional status. The primary outcomes were defined as short-term (1 day), intermediate (3–6 months), and long-term (12–16 months) and data were analyzed according to the closest time interval. When multiple outcomes were available from a single study, the value was used which was thought to be best correlated to that time interval. A random-effects model was used for all analyses based upon the DerSimonian and Laird approach.24 RevMan 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration, Denmark) was used to perform the meta-analysis. Data from prospective studies and data of the secondary outcomes were described.
Statistical Heterogeneity
Statistical heterogeneity was examined by inspecting the Forest plot and formally tested by the Q-test (chi-square) and I2. There was insufficient data to explore cases of considerable heterogeneity.
Data Synthesis and Quality of the Evidence
We evaluated the overall quality of the evidence for the primary outcomes, back pain, and the following complications: durotomies, (transient) neurological deficits, and wound infections. The GRADE-method was applied, which ranges from high to very low quality and is based upon the following five domains: limitations of design, inconsistency of results, indirectness, imprecision, and other factors (e.g., publication bias).25
RESULTS
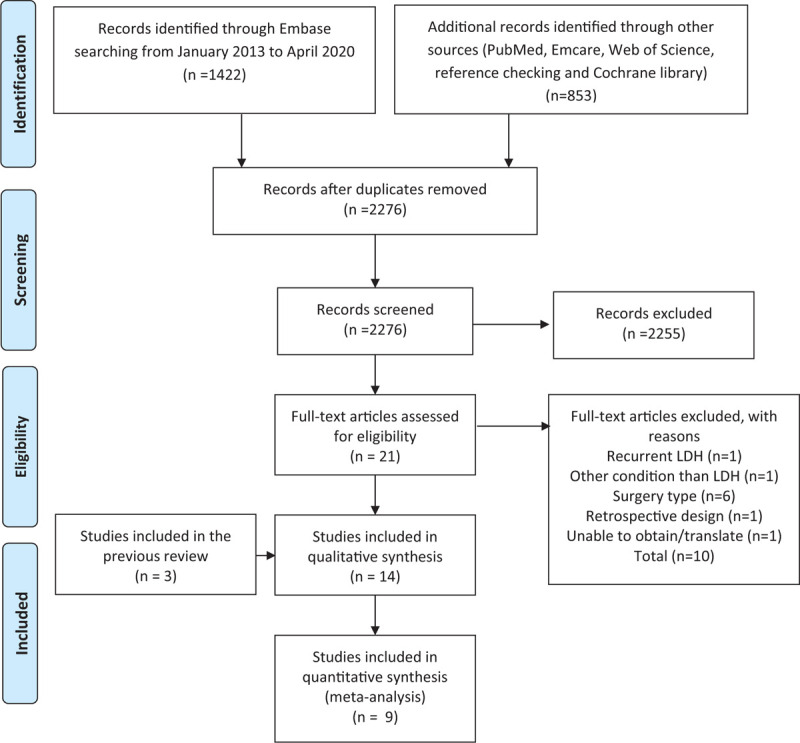
Search Results
The initial search retrieved 2276 studies. Of these, 2255 were excluded based on title and/or abstract checking, while an additional 10 studies were excluded based on assessing the full-text articles (see supplementary Table 2). With the addition of the three studies identified by Kamper et al,17 14 studies were included for this systematic review and meta-analysis comprising a total of 1465 patients26–39 (Figure 1). Of the 14 studies, nine were (quasi)randomized studies and the remaining were observational studies (Table 1).
Figure 1.
Flow-chart of the study selection process.
TABLE 1.
Overview of the Included Studies
| Study | Study Period | Study Location | Study Type | Sample Size (PTED/OM) | Average age | Inclusion Criteria | Outcomes |
| Mayer et al, 1993 | 1987 | Germany | RCT | 40 (20/20) | 41 | Radiculopathy caused by small non-contained LDH, confirmed on imaging, failed cons. Rx | Surgical outcomes, patient satisfaction, RTW, clinical scoring system modified from Suezawa and Schreiber. |
| Hermantin et al, 1999 | - | USA | RCT | 60 (30/30) | 40 | Radiculopathy, positive tension signs, imaging confirming single small intracanalicular LDH at L2-S1, failed cons. Rx, absence of central or lateral stenosis, absence of litigation claim due to LDH. | Surgical outcomes, pain, improvement, RTW, patient satisfaction, narcotic usage. |
| Krappel et al, 2001 | 1996–1997 | Germany | RCT | 40 (20/20) | 40 | Persistent radiculopathy of 4 to 6 weeks, failed cons. Rx, MRI confirmed LDH at L4–5 or L5–S1, no motor or only limited sensory neurological deficit. | Surgical outcomes, patient satisfaction, RTW, complications, radiological outcomes, costs. |
| Akcakaya et al, 2016 | - | Turkey | RCT | 30 (15/15) | 44 | Indication for LDH surgery | Surgical outcomes, sciatica VAS, functional outcomes, serology. |
| Gibson et al, 2017 | - | UK | RCT | 140 (70/70) | 41 | Age 25–70, single level LDH, failure of cons.Rx. | Surgical outcomes, leg pain, back pain, QoL, patient satisfaction. |
| Tao et al, 2018 | 2011–2016∗ | China | RCT | 462 (231/231) | 45 | LDH >1 year, VAS pain >6, confirmed by imaging, failed cons.Rx for 4 to 8 weeks. | Surgical outcomes, pain, functional outcomes, patient satisfaction, serology. |
| Tacconi et al, 2019 | 2014–2018 | Italy | RCT | 38 (18/20) | 45 | Age >18 years, clinical diagnosis of extraforaminal LDH, confirmed on MRI, symptoms lasting >6 weeks, failed cons. Rx, at least 14 months clinical follow-up. | Surgical outcomes, leg pain, functional outcomes. |
| Tacconi et al, 2020 | 2017–2019 | Italy | RCT | 50 (25/25)† | 44 | Confirmed single-level LDH, protrusion preferentially localized at disk level, invalidating radicular pain lasting >6 weeks and adequate imaging studies. | Surgical outcomes, back pain, leg pain, radiological outcomes. |
| Dai et al, 2020 | 2017–2018 | China | RCT | 94 (47/47) | 43 | LDH | Surgical outcomes, pain, QoL, serology. |
| Pan et al, 2016 | 2009–2012 | China | Pros. | 106 (48/58) | 41 | LDH confirmed by imaging. | Surgical outcomes, leg pain, back pain, functional outcomes, patient satisfaction, serology, radiological outcomes. |
| Wang et al, 2017 | 2015–2016 | China | Pros. | 110 (60/50) | 54 | Single segment LDH, confirmed by imaging and conforming diagnostic criteria, failed cons.Rx after three months, no contraindication for surgery. | Surgical outcomes, pain, functional outcomes, serology. |
| Choi et al, 2018 | - | Korea | Pros. | 40 (20/20) | 43 | Sciatica and back pain >6 weeks, failed cons.Rx, clinical LDH confirmed by imaging. | Surgical outcomes, leg pain, back pain, functional outcomes, serology, radiological outcomes. |
| Chang et al, 2018 | 2015–2016 | China | Pros. | 110 (60/50) | 45 | Meeting diagnostic criteria of LDH, single segment LDH confirmed by imaging, failed cons. Rx, no surgical contraindications. | Surgical outcomes, pain, functional outcomes, serology. |
| Xu et al, 2020 | 2017–2018 | China | Pros. | 145 (58/87) | 37 | LDH meeting diagnostic criteria, failed cons.Rx, without spondylolisthesis and spinal stenosis | Surgical outcomes, patient satisfaction functional outcomes, serology, pain. |
The abstract of Tao et al describes June 2012 to May 2016, while the methods section June 2011 to May 2014 as enrollment period.
Tacconi et al 2019 performed OM through Wilkes approach.
cons.Rx indicates conservative therapy; LDH, lumbar disc herniation; QoL, quality of life; RTW, return to work; VAS, visual analogue scale. Surgical outcomes: duration of surgery, length of hospital stay, reoperations, complications and/or blood loss.
Serological outcomes: CRP, CK, TNF-a, IL-4, IL-6, CD3+ T-cells, CD4+ T-cells, CD8+ T-cells, malondialdehyde, myeloperoxidase, superoxide dismutase, total antioxidant capacity.
Patient satisfaction: modified McNab-score, Odom‘s criteria.
Functional outcomes: Oswestry disability index.
Risk of Bias Analysis
The results of the risk of bias analysis are shown in Figure 2. Three studies reported a random sequence generation, of which two had an adequate allocation concealment.27,31 All studies had a high risk of performance bias due to the fundamental differences of PTED and OM. As all studies measured patient-reported outcome measures, all had a high risk of detection bias.
Figure 2.
Risk of bias assessment for all included RCTs.
Bias Across Studies
Eight out of nine RCTs reported on the conflict of interest.26–33 Of these studies, only one had authors that would receive benefits from a commercial party.33 The remaining studies declared no conflict of interest.26–32 Publication bias was not formally assessed given too few data.
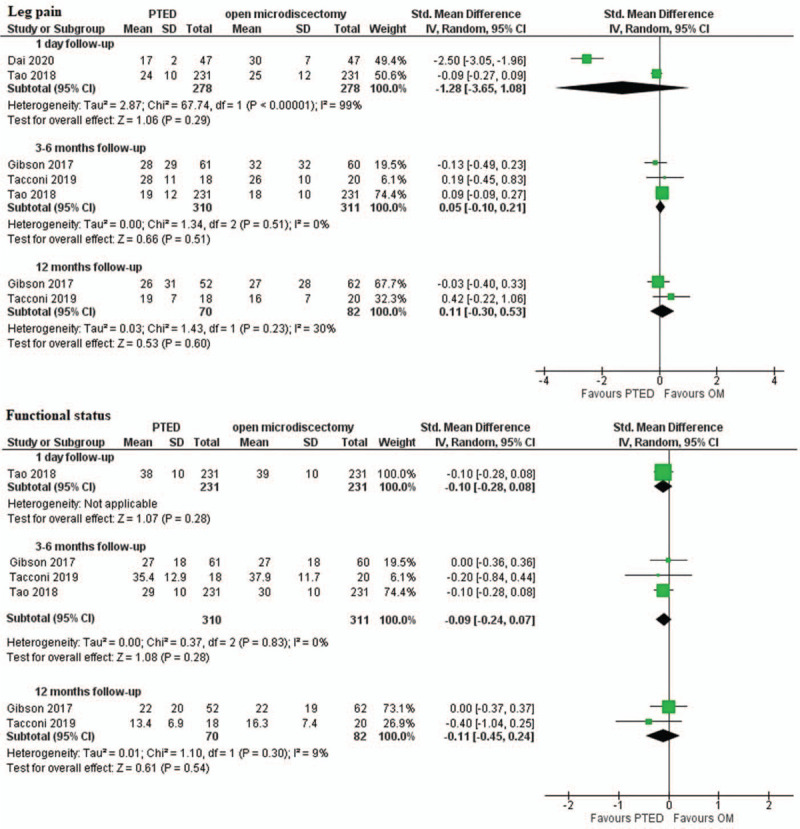
Primary Outcomes
Leg Pain
Twelve studies reported VAS scores, of which seven were RCTs (Table 2). Four of these RCTs did not specifically describe that the VAS-score referred to leg pain.26,28,30,33 Only two provided data which could be used for meta-analysis.28,30 Short-term leg pain did not differ between groups (SMD –1.28, 95% CI –3.65–1.08; two studies, N = 556) but there was high heterogeneity (I2 = 99%) (Figure 3). At intermediate and long-term, there was moderate quality evidence of no difference in leg pain between groups (SMD 0.05, 95% CI –0.10–0.21; three studies, N = 621 and SMD 0.11, 95% CI –0.30–0.53, two studies, N = 152, respectively) (see Table 3). Omitting the RCT that did not specifically mention VAS for leg pain did not affect the results.28,30 Of the studies that were not included in the meta-analysis, Akçakaya et al26 showed that patients who underwent PTED had less leg pain at short-term and Tacconi et al27 showed no difference in leg pain at intermediate-term. In the study of Hermantin et al33 the average pain score was 1.9 in the OM-group versus 1.2 in the PTED group on a scale of 0 to 10. At 2 years of follow-up, Gibson et al31 showed that patients who underwent PTED had less leg pain than patients who underwent OM (35 vs. 19, N = 123).
TABLE 2.
Outcomes of RCTs and of Observational Studies
| Study (PTED/OM) | Leg Pain | Functional Outcome | Back Pain | Patient Satisfaction | Serology | Radiology | Blood Loss | Length of Hospital Stay | Reoperation for LDH | Return to Work | Costs |
| Mayer et al, 1993N = 40 (20/20) | 70% vs. 55% | 3 vs. 1 | 95% vs. 72% | ||||||||
| Hermantin et al, 1999N = 60 (30/30) | 12 vs. 19 | 73% vs. 67% | 0∗vs. 2 | +27 vs. 49 days | |||||||
| Krappel et al, 2001N = 40 (20/20) | +/−84% vs. 75% | + | 1 vs. 0 | +/−100% vs. 100% | - | ||||||
| Akcakaya et al, 2016N = 30 (15/15) | +18 vs. 28 | +/−12 vs. 14 | + | +/−1 vs. 1.2 | |||||||
| Gibson et al, 2017N = 140 (70/70) | +19 ± 26 vs. 35 ± 31 | +/−22 ± 20 vs. 18 ± 17 | +/−25 ± 25 vs. 30 ± 28 | +1.40 ± 0.1 vs. 1.80 ± 0.1 | +0.7 ± 0.7 vs. 1.4 ± 1.3 | +/−5 vs. 2 | +/−78% vs. 82% | ||||
| Tao et al, 2018N = 462 (231/231) | +/−19 ± 10 vs. 18 ± 10 | +/−22 ± 5 vs. 23 ± 5 | +/−85% vs. 88% | + | + | +3 ± 1.5 vs. 14 ± 1.8 | |||||
| Tacconi et al, 2019N = 38 (18/20) | +/−19 ± 7 vs. 16 ± 7 | +/−13 ± 7 vs. 16 ± 7 | + | NR vs. 1 | |||||||
| Tacconi et al, 2020N = 50 (25/25) | +/−20 vs. 20 | +20 vs. 40 | +/+/−† | 1 vs. 0 | |||||||
| Dai et al, 2020N = 94 (47/47) | +17 ± 2 vs. 30 ± 7 | + | +5.1 ± 1.0 vs. 8 ± 1.2 | ||||||||
| Pan et al, 2016N = 106 (48/58) | +/− | +/− | +/− | +/− | + | +‡/ +/− | + | + | + | ||
| Wang et al, 2017N = 110 (60/50) | + | + | + | +/− | |||||||
| Choi et al, 2018N = 40 (20/20) | +/− | +/− | +/− | + | + | + | |||||
| Chang et al. 2018N = 110 (60/50) | + | + | + | ||||||||
| Xu et al, 2020N = 145 (58/87) | + | + | +/− | + | + |
One additional procedure in PTED group due to lumbar spinal stenosis.
Favors PTED on two different MRI reconstructions, but found no difference on two other MRI reconstructions.
Favors PTED in reduction of the Cobb angle but no differences in intervertebral space height were found.
For clinical outcomes of RCTs values measured at the latest moment of follow-up are shown with their standard deviations, when reported. + indicates the outcome is in favor of PTED, – , the outcome is in favor of OM; +/−, there is no difference between PTED and OM. Favors means a statistically significant difference was shown in individual studies. In case if differences were not tested, no symbol is shown. Scores for leg pain, back pain and functional status are reported from 0 to 100 with 0 indicating no pain or disability. NR, not reported
Figure 3.
Pooled results of PTED versus OM on the primary outcomes. OM indicates open microdiscectomy; PTED, percutaneous transforaminal endoscopic discectomy.
TABLE 3.
GRADE Evidence Summary of Findings for the Effect of PTED Versus Open Microdiscectomy
| Quality Assessment | No. of Patients | ||||||||||
| No. of Studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other | PTED | OM | Effect (95% CI) | Quality of Evidence | |
| Leg pain (intermediate term) | 4 | RCT | Serious limitations∗ | No serious inconsistency | No serious indirectness | No serious imprecision | No serious considerations | 335 | 336 | SMD 0.05 (–0.10 to 0.21) | Moderate |
| Leg pain (long term) | 3 | RCT | No serious limitations | No serious inconsistency | No serious indirectness | Serious imprecision§ | No serious considerations | 100 | 112 | SMD 0.11 (–0.30 to 0.53) | Moderate |
| Functional outcome (intermediate term) | 3 | RCT | Serious limitations∗ | No serious inconsistency | No serious indirectness | No serious imprecision | No serious considerations | 309 | 311 | SMD –0.09 (–0.24 to 0.07) | Moderate |
| Functional outcome (long term) | 2 | RCT | No serious limitations | No serious inconsistency | No serious indirectness | Serious imprecision§ | No serious considerations | 70 | 82 | SMD –0.11 (–0.45 to 0.24) | Moderate |
| Back pain (intermediate term) | 1 | RCT | No serious limitations | Serious inconsistency† | No serious indirectness | Serious imprecision§ | No serious considerations | 61 | 60 | SMD –0.04 (–0.39 to 0.32) | Low |
| Back pain (long term) | 1 | RCT | No serious limitations | Serious inconsistency† | No serious indirectness | Serious imprecision§ | No serious considerations | 52 | 62 | SMD 0 (–0.37 to 0.37) | Low |
| Complications|| | 12 | RCTProsp. | Serious limitations∗ | No serious inconsistency | No serious indirectness | Serious imprecision§ | Serious considerations¶ | 647 | 678 | Not calculated | Very low |
Quality of evidence is downgraded if >50% of the study population origins of studies with a high or unclear risk of bias for allocation concealment.
Quality of evidence is downgraded if the I2 statistic >75% or if only one study reports on the outcome.
3 Quality of evidence is downgraded if study results are not generalizable.
Quality of evidence is downgraded if there are <400 patients in the study sample for continuous outcomes or if there are less than 300 events in the study sample for dichotomous outcomes.
Quality of evidence is downgraded if there are signs of publication bias or conflicts of interest.
Dural tears, (transient) neurological deficits and wound infections were taken into this analysis.
Functional Outcomes
Functional outcomes were measured with the ODI in nine studies.27,29–31 Two studies reported on short term function and did not find a difference between PTED and OM.26,30 At intermediate term there was evidence of moderate quality of no difference between PTED and OM (SMD –0.09, 95% CI –0.24–0.07; three studies, N = 621); the same was found at long term (SMD –0.11, 95% CI –0.45–0.24; two studies, N = 152).
Secondary Outcomes
Back Pain
Two RCTs reported VAS scores for back pain.27,31 Gibson et al31 reported no differences between PTED or OM in back pain at intermediate (30 vs. 31, N = 121) and long term (31 vs. 31, N = 114). Tacconi et al27 reported lower postoperative back pain at short term in favor of PTED (20 vs. 40; N = 50, see Table 2). Overall, there is low quality evidence suggesting no difference in back pain between techniques at intermediate and long term (see Table 3).
Patient Satisfaction
Seven studies reported on patient satisfaction following surgery; five of which were RCTs.30–35,38 Gibson et al31 used the Odom‘s criteria to assess patient satisfaction and found a higher rate of satisfaction in the PTED group 2 years after surgery, but no difference at 3 and 12 months. Hermantin et al used an unclear instrument to measure patient satisfaction while the other RCTs used the modified McNab score. Two of these reported no differences in patient satisfaction using the McNab score.30,32
Surgical Outcomes: Blood Loss, Stay in Hospital, Complications, Reoperation for Recurrent LDH, Return to Work
Blood loss was reported in seven studies and all showed results in favor of PTED (Table 2).28–30,35,37–39 Of the studies that measured postoperative length of hospital stay all but one RCT found shorter hospitalization duration in the PTED group.26,28,30,31,35,36,38
Complications among patients who underwent PTED and OM were reported in 12 studies (Table 4).27–38 Overall, there was very low quality of evidence that complication rates (of dural tears, neurological deficits, and wound infections) between PTED and OM were comparable.
TABLE 4.
Complications Mentioned in All Included Studies
| Study | Sample Size (PTED/OM) | Total Complications N (%) | Complications PTED N (%) | Description | Complications OM N (%) | Description |
| Mayer et al, 1993 | 40 (20/20) | 0 | 0 | – | 0∗ | – |
| Hermantin et al, 1999 | 60 (30/30) | 1 (1.7%) | 0 | – | 1 (3.3%) | 1 (3.3%) incidental durotomy |
| Krappel et al, 2001 | 40 (20/20) | 0 | 0 | – | 0 | – |
| Gibson et al, 2017 | 140 (70/70) | 7 (5%) | 6 (8.6%) | 2 (2.9%) possibly dural tears4 (5.7%) mild dysesthesia | 1 (1.4%) | 1 (1.4%) persistent foot drop |
| Tao et al, 2018 | 462 (231/231) | 77 (16.6%) | 14 (6.1%) | 14 (6.1%) transient leg paresthesia | 63 (27.3%) | 7 (3.0%) incidental durotomy56 (24.2%) chronic low back pain |
| Tacconi et al, 2019 | 38 (18/20) | 3 | 1 (5.5%) | 1 (5.5%) reversible hypothermia | 2 (10%) | 1 (5%) superficial wound infection1 (5%) transient leg paresthesia |
| Tacconi et al, 2020 | 50 (25/25) | 0 | 0 | – | 0 | - |
| Dai et al, 2020 | 94 (47/47) | 5 (5.3%) | 1 (2.1%) | 1 (2.1%) dystasia | 4 (8.5%) | 1 (2.1%) lumbar deformation1 (2.1%) aggravated pain2 (4.3%) dystasia |
| Pan et al, 2016 | 106 (48/58) | 16 (15.1%) | 3 (6.3%) | 3 (6.3%) transient leg paresthesia | 13 (22.4%) | 3 (5.2%) transient leg paresthesia2 (3.4%) dural lacerations4 (6.7%) transient leg weakness4 (6.7%) urinary retention |
| Wang et al, 2017 | 110 (60/50) | 0 | – | 0 | – | – |
| Choi et al, 2018 | 40 (20/20) | 0 | 0 | – | 0 | – |
| Xu et al, 2020 | 145 (58/87) | 29 (20%) | 5 (8.6%) | 3 (5.2%) wound infections2 (3.4%) transient nerve paralysis | 24 (27.6%) | 7 (8.0%) wound infections10 (11.5%) transient nerve paralysis7 (8.0%) spinal instability |
| Overall | 1325 (647/678) | 138 (10.4%) | 30 (4.6%) | 108 (15.9%) |
One patient in the OM group underwent a revision procedure due to scar tissue. This revision procedure was complicated due to the development of spondylodiscitis.
Six RCTs reported reoperation rates for recurrent disc herniation.27,29,31–34 Reoperation rates were low (2%–10%) and none of the studies showed significant differences between groups. Return to work was reported in four studies.31–34 Hermantin et al reported that patients who underwent PTED returned earlier to work than patients who underwent OM (27 vs. 49 days). Mayer et al34 reported that 95% of the patients in the PTED group returned to work after 12 months compared with 72% in the OM group. Krappel et al32 and Gibson et al31 found no differences in return to work rates.
Biochemical Outcomes
Five studies reported on CRP and were all in favor of PTED at one or more postoperative time points (ranging from 1 hour to 7 days after surgery).30,36–39 Four studies reported on the CK values26,30,36,38; all studies showed significantly higher CK rates in the OM group at one or more time points.
Radiological Outcomes
Four studies reported radiological outcomes of PTED versus OM.27,33,36,38 One study compared scarring measured on postoperative MRIs and found less scarring in the PTED group, but no correlation to clinical outcomes.33 Another study assessed lumbar stability by measuring the Cobb angle and the height of the intervertebral space as measured on x-rays and found a significant reduction in the Cobb angle in the PTED group postoperatively.38 No differences were found in the postoperative Cobb angle in the OM group or in the measured intervertebral space height in either group. Choi et al36 measured the cross-sectional area of high-intensity lesions in the paraspinal muscles on MRIs postoperatively, which were larger in patients that underwent OM compared with PTED. Finally, in a randomized study that analyzed paraspinal muscle signal intensity changes on postoperative MRI, higher mean volume of paravertebral muscle alterations were found in the OM group on two specific MRI reconstructions.27
Costs and Cost-Effectiveness
Two studies reported on some of the costs of the interventions. Krappel et al calculated the costs by computing the costs of the operating room, hospitalization, endoscopes, and sterilization of the equipment. Total costs of PTED were higher than for OM (U.S.$ 7707 vs. U.S.$ 1417, respectively).32,40 Of the total costs of PTED, 66.2% were attributable to the costs of the endoscope. Pan et al38 only reported the costs of hospitalization which were lower in the PTED group (U.S.$ 1279 for PTED vs. U.S.$ 1622 for OM).40 None of the identified studies performed economic evaluations.
DISCUSSION
The update of our systematic review which examined the effect of PTED versus OM for the treatment of LDH suggests that there is moderate quality evidence of no difference in leg pain and functional status at the intermediate and long-term follow-up. Data on short-term leg pain showed substantial heterogeneity, and only one study provided data on short-term functional status. These data on leg pain and functional status didn’t show any differences between PTED and OM. Our review could not affirm a lower rate of back pain which could be expected from full-endoscopic spine surgery. Back pain was only assessed by one RCT and there was low quality evidence of no difference in back pain between patients who underwent PTED versus OM. Overall, complications were more frequently reported in patients who underwent OM, although the incidence of complications after lumbar discectomy is low.
Comparison With Other Studies
In recent years, other reviews with different methodology have been published.11,13,41,42 The current review differs in that we only compared full endoscopic transforaminal discectomy with OM which is considered to be the standard procedure. Furthermore, our review included four RCTs published after completion of the previous reviews.27–30 Nevertheless the results of the present review are in concordance with prior reviews; clinical outcomes such as leg pain, back pain, functional status, and rate of recurrent disc herniation, are comparable or differed minimally between PTED and OM, but PTED is associated with shorter hospitalization duration and blood loss.11,13,42
In our previous review, we identified three RCTs comparing PTED with OM.17 Of these RCTs, only one evaluated pain and none assessed specifically back pain or functional status as is customary in lumbar spine surgery nowadays.32–34 Furthermore, cautious interpretation of these trials was also warranted because of the unclear or high risk of selection bias. The current search added six RCTs to the results of which two had a low risk of selection bias.27,31 Of these two studies only the trial by Gibson et al31 with moderate sample size (N = 140) provided relevant clinical outcomes on short and long term.
Strengths and Limitations
Despite the inclusion of 11 new studies to this update, there remains a paucity of high-quality studies with a low risk of bias reporting on patient-centered outcomes relevant to lumbar disc surgery.17 For instance, postoperative leg pain was only reported in three and two studies at intermediate and long term respectively, and postoperative back pain was only measured by one study at intermediate and long term. The paucity of studies also led to the inability to formally assess publication bias. Another limitation is inherent to cultural and time differences between the studies. For example, cultural differences may explain the difference in postoperative length of hospital stay following discectomy between studies conducted in European countries in comparison to studies conducted in other countries. An example of timely differences is the trend that the duration of hospitalization for lumbar disc surgery is decreasing over the years.9,43 Nevertheless, because these cultural and time differences are applied on both patient categories, we expect the influence of these differences on the outcomes to be limited but they may explain heterogeneity between the studies on these other outcomes. The inability of blinding patients is a limitation which may also warrant cautious interpretation of some outcomes. For instance, some expected short-term benefits such as patient satisfaction, and return-to-work and length-of-hospital stay rates, may be influenced by the patient's own expectation of undergoing endoscopic surgery, also frequently named as minimally invasive surgery.
The findings of the current review warrant further studies of high methodological quality and sufficient sample size to further explore clinical merits of PTED in comparison to OM on core clinical outcomes as leg pain, functional status, and back pain. As we would expect no differences in clinical outcomes or small difference of limited clinical relevance based on the results of this meta-analysis, prospective economic evaluations are essential, especially since PTED is expected to be more expensive as procedure but to have lower hospitalization costs. Results of a RCT comparing the effectiveness and cost-effectiveness of PTED to OM are expected.44
An important concern for the use of PTED for sciatica is the surgical learning curve, which is considered to be relatively long and difficult.45–47 Two studies that focused on the learning curve of full-endoscopic surgery show a steep learning curve of full-endoscopic surgery and suggest that the procedure may be more difficult to master as compared with OM.45,46 Despite this learning curve, however, clinical outcomes such as functional status and pain appear to be comparable to those after OM. A recent systematic review attempted to estimate a cutoff number of cases needed to perform to master PTED. A case load of 20 was commonly used, but insufficient evidence was found to support any number of procedures.47
CONCLUSION
There is moderate level evidence of no difference in leg pain or functional status at intermediate and long term between PTED and OM in the treatment of LDH. High quality and robust studies reporting on clinical outcomes on the long-term and performing economic evaluations are lacking.
Key Points
PTED is an alternative surgical technique to treat lumbar disk herniation. It is unclear if PTED has comparable outcomes compared to open microdiscectomy.
Multiple online databases were systematically searched up to April 2020 for randomized controlled trials and prospective studies measuring clinical outcomes.
Fourteen studies were included of which nine trials.
There is moderate quality evidence suggesting no difference in leg pain or functional status at intermediate and long-term follow-up between PTED and OM in the treatment of LDH.
High quality, robust studies reporting on clinical outcomes and cost-effectiveness on the long term are lacking.
Supplementary Material
Acknowledgments
The authors would like to thank Jan W. Schoones from the Waleus Library, Leiden University Medical Center for performing the systematic search.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
ZonMw, The Netherlands Organization for Health Research and Development (project number 837004013) funds were received in support of this work.
Relevant financial activities outside the submitted work: grants, payment for lecture.
Supplemental digital content is available for this article.
References
- 1.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976) 2008; 33:2464–2472. [DOI] [PubMed] [Google Scholar]
- 2.Ropper AH, Zafonte RD. Sciatica. N Engl J Med 2015; 372:1240–1248. [DOI] [PubMed] [Google Scholar]
- 3.Weber H, Holme I, Amlie E. The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine (Phila Pa 1976) 1993; 18:1433–1438. [PubMed] [Google Scholar]
- 4.Gadjradj PS, Arts MP, van Tulder MW, et al. Management of symptomatic lumbar disk herniation: an international perspective. Spine (Phila Pa 1976) 2017; 42:1826–1834. [DOI] [PubMed] [Google Scholar]
- 5.Telfeian AE, Veeravagu A, Oyelese AA, et al. A brief history of endoscopic spine surgery. Neurosurg Focus 2016; 40:E2. [DOI] [PubMed] [Google Scholar]
- 6.Kambin P, Brager MD. Percutaneous posterolateral discectomy - anatomy and mechanism. Clin Orthop Relat Res 1987; 145–154. [PubMed] [Google Scholar]
- 7.Kambin P, Gellman H. Percutaneous lateral discectomy of the lumbar spine - a preliminary-report. Clin Orthop Relat Res 1983; 174:127–132. [Google Scholar]
- 8.Ruetten S, Komp M, Merk H, et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique - a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008; 33:931–939. [DOI] [PubMed] [Google Scholar]
- 9.Gadjradj PS, van Tulder MW, Dirven CM, et al. Clinical outcomes after percutaneous transforaminal endoscopic discectomy for lumbar disc herniation: a prospective case series. Neurosurg Focus 2016; 40:E3. [DOI] [PubMed] [Google Scholar]
- 10.Nellensteijn J, Ostelo R, Bartels R, et al. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J 2010; 19:181–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qin R, Liu B, Hao J, et al. Percutaneous endoscopic lumbar discectomy versus posterior open lumbar microdiscectomy for the treatment of symptomatic lumbar disc herniation: a systemic review and meta-analysis. World Neurosurg 2018; 120:352–362. [DOI] [PubMed] [Google Scholar]
- 12.Cong L, Zhu Y, Tu G. A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur Spine J 2016; 25:134–143. [DOI] [PubMed] [Google Scholar]
- 13.Barber SM, Nakhla J, Konakondla S, et al. Outcomes of endoscopic discectomy compared with open microdiscectomy and tubular microdiscectomy for lumbar disc herniations: a meta-analysis. J Neurosurg Spine 2019; 1–14. [DOI] [PubMed] [Google Scholar]
- 14.Chen X, Chamoli U, Vargas Castillo J, et al. Complication rates of different discectomy techniques for symptomatic lumbar disc herniation: a systematic review and meta-analysis. Eur Spine J 2020; 29:1752–1770. [DOI] [PubMed] [Google Scholar]
- 15.Ding W, Yin J, Yan T, et al. Meta-analysis of percutaneous transforaminal endoscopic discectomy vs. fenestration discectomy in the treatment of lumbar disc herniation (Metaanalyse der perkutanen transforaminalen endoskopischen Diskektomie im Vergleich zur Fensterungsdiskektomie in der Behandlung des lumbalen Bandscheibenvorfalls). Orthopade 2018; 47:574–584. [DOI] [PubMed] [Google Scholar]
- 16.Li X, Han Y, Di Z, et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation. J Clin Neurosci 2016; 33:19–27. [DOI] [PubMed] [Google Scholar]
- 17.Kamper SJ, Ostelo RW, Rubinstein SM, et al. Minimally invasive surgery for lumbar disc herniation: a systematic review and meta-analysis. Eur Spine J 2014; 23:1021–1043. [DOI] [PubMed] [Google Scholar]
- 18.Garner P, Hopewell S, Chandler J, et al. When and how to update systematic reviews: consensus and checklist. BMJ 2016; 354:i3507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muka T, Glisic M, Milic J, et al. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur J Epidemiol 2020; 35:49–60. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gadjradj PS, Harhangi BS. Percutaneous transforaminal endoscopic discectomy for lumbar disk herniation. Clin Spine Surg 2016; 29:368–371. [DOI] [PubMed] [Google Scholar]
- 22.Caspar W. New operative procedure of lumbar-disk herniation using a microscopic approach thereby causing less tissue injury. Acta Neurochir 1977; 36:273–274. [Google Scholar]
- 23.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventionsed. 2011. [Google Scholar]
- 24.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177–188. [DOI] [PubMed] [Google Scholar]
- 25.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ 2004; 328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akcakaya MO, Yorukoglu AG, Aydoseli A, et al. Serum creatine phosphokinase levels as an indicator of muscle injury following lumbar disc surgery: comparison of fully endoscopic discectomy and microdiscectomy. Clin Neurol Neurosurg 2016; 145:74–78. [DOI] [PubMed] [Google Scholar]
- 27.Tacconi L, Signorelli F, Giordan E. Is full endoscopic lumbar discectomy less invasive than conventional surgery? A randomized MRI study. World Neurosurg 2020; 138:e867–e875. [DOI] [PubMed] [Google Scholar]
- 28.Dai HJ, Zhang X, Wang LT, et al. The effect of percutaneous transforaminal endoscopic discectomy (PTED) on serum inflammatory factors and pain in patients with lumbar disc herniation after surgery. Int J Clin Exp Med 2020; 13:597–603. [Google Scholar]
- 29.Tacconi L, Giordan E. Endoscopic transforaminal discectomy vs. far lateral discectomy for extraforaminal disc protrusions: our experience. NeuroQuantology 2019; 17:18–22. [Google Scholar]
- 30.Tao XZ, Jing L, Li H. Therapeutic effect of transforaminal endoscopic spine system in the treatment of prolapse of lumbar intervertebral disc. Eur Rev Med Pharmaco 2018; 22:103–110. [DOI] [PubMed] [Google Scholar]
- 31.Gibson JNA, Subramanian AS, Scott CEH. A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur Spine J 2017; 26:847–856. [DOI] [PubMed] [Google Scholar]
- 32.Krappel FA, Schmitz R, Bauer E, et al. Open or endoscopic nucleotomy? Orthopadische Praxis 2001; 37:164–169. [Google Scholar]
- 33.Hermantin FU, Peters T, Quartararo L, et al. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am 1999; 81:958–965. [DOI] [PubMed] [Google Scholar]
- 34.Mayer HM, Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg 1993; 78:216–225. [DOI] [PubMed] [Google Scholar]
- 35.Xu G, Zhang C, Zhu K, et al. Endoscopic removal of nucleus pulposus of intervertebral disc on lumbar intervertebral disc protrusion and the influence on inflammatory factors and immune function. Exp Ther Med 2020; 19:301–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi KC, Shim HK, Hwang JS, et al. Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg 2018; 116:e750–e758. [DOI] [PubMed] [Google Scholar]
- 37.Wang H, Song Y, Cai L. Effect of percutaneous transforaminal lumbar spine endoscopic discectomy on lumbar disc herniation and its influence on indexes of oxidative stress. Biomed Res 2017; 28: [Google Scholar]
- 38.Pan Z, Ha Y, Yi S, et al. Efficacy of Transforaminal Endoscopic Spine System (TESSYS) technique in treating lumbar disc herniation. Med Sci Monit 2016; 22:530–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chang F, Zhang T, Gao G, et al. Therapeutic effect of percutaneous endoscopic lumbar discectomy on lumbar disc herniation and its effect on oxidative stress in patients with lumbar disc herniation. Exp Ther Med 2018; 15:295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.FxtopCompany. Historical converter], 2018. Available at: https://fxtop.com/. Accessed 23-05-2020. For Krappel et. al, exchange rates of 2001 were used. For Pan et al., exchange rates of 2010 were used. [Google Scholar]
- 41.Gadjradj PS, van Tulder MW, Vleggeert-Lankamp C, et al. Letter to the editor regarding “Percutaneous Endoscopic Lumbar Discectomy Versus Posterior Open Lumbar Microdiscectomy for the Treatment of Symptomatic Lumbar Disc Herniation: A Systemic Review and Meta-Analysis”: a critical appraisal. World Neurosurg 2019; 122:715–717. [DOI] [PubMed] [Google Scholar]
- 42.Zhang B, Liu S, Liu J, et al. Transforaminal endoscopic discectomy versus conventional microdiscectomy for lumbar discherniation: a systematic review and meta-analysis. J Orthop Surg Res 2018; 13:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arts MP, Brand R, van den Akker ME, et al. Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA 2009; 302:149–158. [DOI] [PubMed] [Google Scholar]
- 44.Seiger A, Gadjradj PS, Harhangi BS, et al. PTED study: design of a non-inferiority, randomised controlled trial to compare the effectiveness and cost-effectiveness of percutaneous transforaminal endoscopic discectomy (PTED) versus open microdiscectomy for patients with a symptomatic lumbar disc herniation. BMJ Open 2017; 7:e018230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Son S, Ahn Y, Lee SG, et al. Learning curve of percutaneous endoscopic interlaminar lumbar discectomy versus open lumbar microdiscectomy at the L5-S1 level. PLoS One 2020; 15:e0236296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hsu HT, Chang SJ, Yang SS, et al. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J 2013; 22:727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ahn Y, Lee S, Son S, et al. Learning curve for transforaminal percutaneous endoscopic lumbar discectomy: a systematic review. World Neurosurg 2020; 143:471–479. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


