Letter to the editor
There are currently two global pandemics: COVID-19 and physical inactivity [1]. Since the World Health Organization states nearly 2 million deaths per year to sedentary lifestyle [2], exercise medicine becomes even more relevant since sports medicine research (SMR) generates the theoretical framework for prescription and evidence-based approaches, which allows the population - from athletes to the elderly - to exercise in an optimized and safe manner. We herein outline the foreseeable impact of COVID-19 on SMR and point to tips to minimize the pandemic’s influence on exercise intervention studies.
In general, exercise programs demand that the practitioner move to the research facilities (e.g., laboratories, hospitals, and physical therapy centers) for several weeks or months, raising social interaction. Due to distancing policies, the pandemic has already impacted SMR and has forced a temporary but potentially ongoing cessation in human studies, including investigations from basic sciences to population clinical studies, as noted in the U.S. National Library of Medicine (Suppl Table 1). Regular exercise can be beneficial for the host’s immune defense, especially in people with chronic diseases and older adults [3], in whom moderate-intensity exercise is associated with a lower prevalence of COVID-19-related hospitalization [4]; thus, planning to reduce the impact of COVID-19 on the SMR sector is even more crucial.
Strategies of knowledge diffusion include the development of review papers, systematic reports, and meta-analysis; strategies and partnerships for remote interventions, creating data management plans on virtual platforms (e.g., DPMtool), and sharing information on academic networks (e.g., ResearchGate and Academia.edu) and in clinical exercise forums (e.g., Clinical Exercise Physiology Association forum).
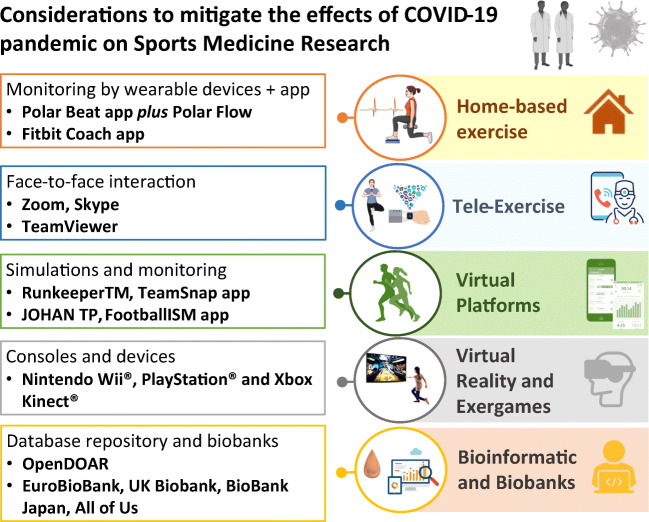
New technologies can allow the training condition of volunteers in social isolation. Figure 1 indicates suggestions and practical examples with the following strategies: (i) home-based exercise intervention delivered and monitored remotely by wearable devices or personalized apps as an accessible route for healthcare professionals in real-time rehabilitation; (ii) “tele-exercise” by video conferencing software and remote-control software to promote a face-to-face interaction and reduce the physical and mental consequences of social isolation; (iii) virtual platforms to maintain the fitness levels and virtual simulations organized by Internet resources, where athletes can participate in different locations at the same moment or the same location in different moments; (iv) virtual reality and exergames to simulate a wide variety of sports [5]; and (v) the use of bioinformatics for handling repository data and biobanks. Monitoring technologies, besides being useful in this pandemic moment, can also contribute to a more flexible sports science practice in the future, where hybrid formats (laboratory and home-based) can result in greater ecological validity when compared to exercise protocols developed exclusively in laboratories.
Fig. 1.
Research strategies and key considerations to mitigate the effects of the COVID-19 pandemic on sports medicine research. Illustration created by the authors to exemplify new possibilities for intervention and exercise monitoring that renew the perspectives of studies compared to traditional models
Despite the opportunity for the development of SMR, we have no specific peer-reviewed guidelines indicating the amount and type of home-training exercise suggested during this pandemic, and there are still open questions regarding COVID-19 and physical activity. Besides the fact that exercise intensity depends on an individual’s age, health status, and fitness level, the effect of a single bout of exercise and the exercise-associated hormesis curve on human immune function remain controversial, which may conduct to health benefits or increased infection risk [6]. With this perspective, we aim to advise caution in developing exercise training protocols and we recommend involving the entire multidisciplinary health team in the decisions (e.g., physiologists, medical staff, head of performance, coaches, and players).
In these uncertain times, with a second wave of the epidemic ongoing or approaching, research on remote monitoring of physical activity by widely technological tools could advance our knowledge in the field, allowing sports scientists to overcome the challenges of social distance.
Supplementary Information
(DOCX 43 kb)
Funding
This work was supported by the CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) [grant number 88882.314890/2013–01 and 88887.321687/2019–00, Finance Code 001]; FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo); and CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico) [grant number 308700/2017–1] and PROANTAR [442645/2018–0].
Data availability
Not applicable.
Code availability
Not applicable.
Declarations
Competing interests
All authors report no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Mobile; Wireless Health
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Leandro Borges and Michele M. Moraes contributed equally to this work.
References
- 1.Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R (2020). A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization (2020). Sedentary lifestyle: a global public health problem. https://www.who.int/docstore/world-health-day/2002/fact_sheets4.en.pdf (accessed January 5, 2021).
- 3.Borges L, Passos MEP, Silva MBB, et al. Dance Training Improves Cytokine Secretion and Viability of Neutrophils in Diabetic Patients. Mediators Inflamm. 2019;2019:2924818. doi: 10.1155/2019/2924818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Souza FR, Motta-Santos D, Santos Soares D dos, et al (2020). Physical Activity Decreases the Prevalence of COVID-19-associated Hospitalization: Brazil EXTRA Study. MedRxiv:2020.10.14.20212704. 10.1101/2020.10.14.20212704.
- 5.Amorim MGS, de Oliveira MD, Soares DS, et al. Effects of exergaming on cardiovascular risk factors and adipokine levels in women. J Physiol Sci. 2018;68:671–8. doi: 10.1007/s12576-017-0581-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radak Z, Chung HY, Koltai E, Taylor AW, Goto S. Exercise, oxidative stress and hormesis. Ageing Res Rev. 2008;7:34–42. doi: 10.1016/j.arr.2007.04.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 43 kb)
Data Availability Statement
Not applicable.
Not applicable.