Abstract
Liposarcoma was mainly occurring in the lower extremities and deep retroperitoneal soft tissues, but rarely occurred in the thoracic cavity. Most cases were reported in the literature, and most of them were middle-aged and elderly people. It was even more rare in adolescents with tumors occupying the entire thoracic cavity. Recently, one case of myxomatous liposarcoma was admitted and treated in our hospital. This paper reports this case and discusses the diagnostic method, pathological type and treatment of giant liposarcoma in the chest, in order to provide a reference for the clinical diagnosis and treatment of this rare tumor.
Keywords: Thoracic cavity, liposarcoma, case reports
Introduction
Liposarcoma is a soft-tissue malignancy that usually occurs in the extremities and retroperitoneum and is composed of four histological subtypes: myxoid, highly differentiated, dedifferentiated, and pleomorphic [1]. Rarely, liposarcoma occurs in the pleural cavity and is usually a well-differentiated tumor. More rarely, a pleural liposarcoma presents as an abnormally large and rapidly growing intrathoracic mass, with symptoms such as chest pain, cough, and shortness of breath or difficulty breathing due to pressure on surrounding tissue. These particular tumors are called giant intrathoracic liposarcomas. Therefore, we describe the typical manifestations, imaging findings, and treatment principles of a giant intrathoracic liposarcoma in the following typical cases.
Case data
The patient was a male, 14 years old. He was admitted to hospital due to chest pain and shortness of breath for 2 weeks and aggravation for 5 days. Physical examination showed shortness of breath and fullness of left thoracic cage. Reduced respiratory motility. Percussion of the left lung is solid and auscultation of breath sounds is absent. No special abnormality was found in blood biochemistry. Our chest CT examination: on the left side of a huge mediastinal - visible on the left side of the chest cavity irregular mixed mass in shape, density and size of about 195 mm * 140 mm * 120 mm, and local owe edge is clear, uniform density owe, scan CT value about - 84-24 Hu, show inhomogeneity enhancement adjacent local compression of the left lung tissue atelectatic, mediastinum, migration of the trachea to the right, the left lung door structure is not clear; A few patchy fuzzy shadows with increased density can be seen locally in the left lung. CT diagnosis: left mediastinal - left thoracic massive fatty neoplastic lesions (accompanied by adjacent left lung local compression collapse and mild left lung local inflammation), the nature is to be determined, mainly considering the differentiation of teratoma and liposarcoma, the possibility of the former is high. After admission, double-lumen endotracheal intubation combined with intravenous anesthesia was performed under left thoracotomy and massive thoracic tumor resection (Figure 1A-C). Intraoperative exploration of the tumor almost occupied the thoracic cavity, with a complete capsule tightly adhering to the chest wall and mediastinum, and originated from the left posterior chest wall. Complete excision was performed to remove the tumor, showing that the tumor was round, with a complete capsule, about 20 cm × 15 cm × 11 cm in size, and weighed about 3.7 kg (Figures 2, 3). Adipose tissue was found after incision. Postoperative pathology: the tumor was composed of spindle or oval cells, adipoid cells, and adipocyte. Spindle or oval cells showed slight atypia, and mucoid changes were observed in the stroma (Figure 4A). Immunohistochemical results: S-100 fat cells and fat cell (+) CD34 (+) vessels, SOX-10 (-), HMB45 (-), MeleanA (-), CK (-), EMA (-), Actin (-), Desmin (-), a small amount of (+), P53, CD68 (-), CD3 (-), CD5 (-), CD20 (-), CD79a (-), the TdT (-), STAT6 (-), CD117 (-), DOG-1 (-), Ki-67 hot area about 10% (+); Genetic tests: MDM2 (-), CHOP (-). Combined with HE morphology, immunohistochemical results and gene detection, the lesions were consistent with (malignant) myxoid liposarcoma. The patient had a good postoperative left lung expansion.
Figure 1.

As shown in (A-C), there is a large irregular mass in the left thoracic cavity. The mediastinum and trachea are deviated to the right, and after enhancement, the mass presents an uneven enhancement.
Figure 2.
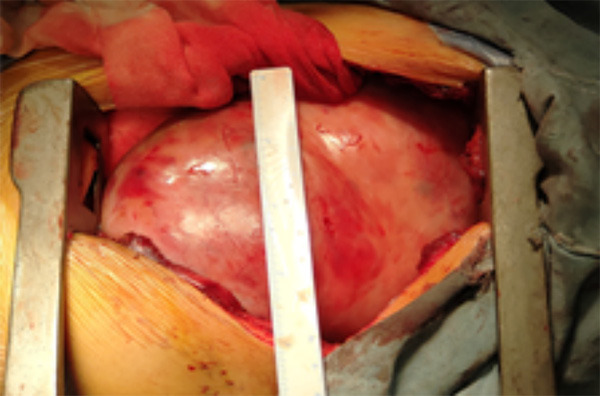
Intraoperative exploration showed that the tumor filled the left thoracic cavity.
Figure 3.

After the tumor was cut open, the tumor tissue showed a fish-like appearance.
Figure 4.

A-C. Frozen pathological section: The sample was adipose tissue with prominent nuclear atypia and liposarcoma cells, which was diagnosed as liposarcoma.
Discussion
Liposarcoma is a soft tissue malignancy arising from mesenchymal tissues. It can occur in all parts of the body, especially retroperitoneum and limb trunk soft tissue. Primary intrathoracic liposarcoma is rare, accounting for only 0.1-0.75% of all mediastinal tumors [2]. Of the reported cases, 85% were symptomatic and 15% were incidental [3]. The median age of diagnosis was 43~49 years old, without gender difference [4]. In the early stage, there were no obvious clinical symptoms. With the increase of the mass, the tumor size, location and the pressure or invasion of the surrounding tissues showed pain, edema and other symptoms. Typical symptoms are compression of intrathoracic structures resulting in abdominal clinical manifestations, including dyspnea, shortness of breath, chest pain, wheezing, hoarseness, compression of the superior vena cava and arrhythmias, and heart failure. By looking at similar literature, 19 cases of mediastinal liposarcoma have been published in English literature (Table 1). The mean age of the patients was 63.3±13.2 years, and there was no difference in sex ratio. The report details the symptoms of 13 patients: 7 complained of some symptoms, 6 did not, and the tumor was discovered by chance. The most common symptom is difficulty breathing, followed by difficulty swallowing and hoarseness. More than half of the cases were located in the posterior mediastinum, followed by the anterior, middle and upper mediastinum. In this case, the left thoracic cavity was almost full of tumor, and the patient was admitted to hospital with chest pain and discomfort symptoms. The patient was an adolescent, which was a rare case.
Table 1.
Summary of similar literature previously reported
| Authors | No. Of patients | Age | Gender | Location | Symptom | Tumor size (cm) | Initial treatment | Recurrence | RFS (months) | OS |
|---|---|---|---|---|---|---|---|---|---|---|
| Boland et al. [5] | 5 | 68 | M | Posterior | Unknown | Unknown | Surgery | Yes | 48 | 72 |
| 63 | F | Anterior | Unknown | Unknown | Surgery | Yes | 24 | 34 | ||
| 47 | F | Middle | Unknown | Unknown | Surgery | No | 60 | 60 | ||
| 71 | F | Posterior | Unknown | Unknown | Surgery (incomplete) | Residual | 12 | 12 | ||
| 76 | F | Anterior | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | ||
| Ortega et al. [7] | 3 | 75 | M | Posterior | Weightloss, dyspnea | 14 | Surgery | Yes | Unknown | 6 |
| 66 | M | Posterior | Chestpain, dysphagia, malaise | 9 | Surgery | No | Unknown | 24 | ||
| 53 | F | Posterior | Dysphagia | 23 | Surgery | Unknown | Unknown | Unknown | ||
| Chen et al. [4] | 1 | 64 | M | Anterior | Unknown | 6 | Surgery | No | 12 | 12 |
| Fukai et al. [8] | 1 | 56 | M | Anterior | None | 16.5 | Surgery | No | 36 | 36 |
| Hamanaka et al. [9] | 1 | 74 | M | Posterior | Drycough | 11 | Surgery | No | 8 | 8 |
| Coulibaly et al. [10] | 1 | 34 | F | Posterior | Dyspnoea | 20 | Surgery | Yes | 15 | 114 |
| Narasimman et al. [11] | 1 | 48 | M | Posterior | None | 15 | Surgery | No | 12 | 12 |
| Hirai et al. [12] | 1 | 64 | M | Unknown | Hoarseness | 6.5 | Surgery | No | 14 | 14 |
| Miura et al. [13] | 5 | 45 | F | Middle | None | 12.7 | Surgery | Yes | 51 | 60 |
| 62 | F | Superior | None | 12 | Surgery | Yes | 28 | 48 | ||
| 84 | M | Anterior | None | 6.6 | Surgery | Yes | 27 | 40 | ||
| 75 | M | Posterior | None | 20 | Surgery | No | 3 | 3 | ||
| 78 | M | Superior | Dyspnea, Hoarseness | 11 | Chemo (Doxorubicin) | - | - | 0.5 |
Chemo, chemotherapy; OS, overall survival; FRS, recurrence-free survival.
The World Health Organization histopathological classification of liposarcoma is divided into four subtypes: highly differentiated, dedifferentiated, mucoid, and pleomorphic, and histopathology have been found to be associated with clinical recurrence and survival. Boland et al. reported 24 patients with mediastinal liposarcoma spanning 60 years, and found that 5 of 7 patients with polyoma died and 2 of 2 patients with myxoid liposarcoma died. In contrast, only 1 of 6 patients with highly differentiated tumors died, and only 1 of 4 patients with dedifferentiated liposarcoma died [5]. Similarly, Chen Ming et al. reported 23 patients with mediastinal liposarcoma spanning 10 years, and found that patients with myxoid, pleomorphic or dedifferentiated liposarcoma had poorer disease survival and overall survival than those with highly differentiated liposarcoma [4]. Consistent with these results, Brenner et al. demonstrated in PET-CT that the tissue type of mediastinal liposarcoma was positively correlated with FDG, and the SUVmax of highly differentiated liposarcoma was significantly higher than that of myxoid and pleomorphic subtypes. In addition, the disease-free survival of SUVMax 3.6 patients was significantly prolonged [6]. Among the four subtypes, highly differentiated liposarcomas had a higher survival rate, while dedifferentiated and pleomorphic liposarcomas had the worst prognosis.
The diagnosis of liposarcoma mainly depends on imaging examination and histopathological examination. The radiographic appearance of liposarcoma on CT depends on the degree of differentiation of these subtypes. On CT scanning, liposarcoma performance from the main pathological changes into a solid mass of fat, such as different performance, the CT value in Hu - 100-80, characterized by mass of uneven density, with irregular flake inside fat density and a high density of irregular lamellar soft tissue density shadow, liposarcoma of the heterogeneity and necrosis, calcification, blood vessels, capsule and the extent of the soft tissue component. However, preoperative radiological diagnosis of liposarcoma and lipoma is very difficult, so histopathological diagnosis and typing are necessary. Fine needle biopsy and postoperative pathological biopsy can confirm the diagnosis.
Mainly with good hair in the differential diagnosis of this disease before, mediastinal teratoma in phase identification, teratoma mainly happens on the front and in the mediastinum, teratoma typical CT images show the uneven density of round or lobulated cystic mass, calcification lesions, uneven thickness of capsule wall, edge smooth, neat, bag piece containing fat density shadow and hypoplasia of bones and teeth, if the bag piece inside the liquid containing fat and at the same time, the liquid - liquid under visible to fat fat interface, also can be seen from the capsule wall is raised within the bag piece of substantive nodular shadows. Intrathoracic liposarcoma is easily misdiagnosed as teratoma. This patient was considered as teratoma in preoperative CT examination.
Complete surgical resection is still the primary treatment for liposarcomas. Small mediastinal liposarcomas can be removed with a minimally invasive procedure including a video-assisted or machine-assisted thoracoscope, while larger tumors often require open surgery. The use of radiotherapy or chemotherapy did not result in a satisfactory improvement in prognosis. The prognosis of liposarcoma is not affected by tumor size, gender, age and other factors, and histopathological type may be the most important factor determining survival of liposarcoma patients. In this case, because the patient had no manifestations of extrathoracic and mediastinal metastasis, only surgical treatment was performed, and postoperative chemoradiotherapy was not performed. The patient was followed up for one year and no tumor recurrence was found so far.
Conclusions
Intrathoracic liposarcoma is rare. Through this case, we can make accurate diagnosis and treatment of the huge tumor in the chest of teenagers. Through the surgical treatment, the prognosis of this case can be improved, and life-threatening complications such as the systemic spread of the tumor can be avoided. Through this case, the future patients can be through the diagnosis of the disease and treatment means to provide clinical data.
Acknowledgements
Thanks to Naturel Science Foundation of Guangdong Province, People’s Republic of China for its support. Grant Number: 2017A030313856.
Disclosure of conflict of interest
None.
References
- 1.Fletcher C, Unni K, Mertens F. Pathology & genetics of tumours of soft tissue and bone, vol. 4. Lyon: Iarc.; 2002. pp. 316–317. [Google Scholar]
- 2.McLean TR, Almassi GH, Hackbarth DA, Janjan NA, Potish RA. Mediastinal involvement by myxoid liposarcoma. Ann Thorac Surg. 1989;47:920–921. doi: 10.1016/0003-4975(89)90038-6. [DOI] [PubMed] [Google Scholar]
- 3.Schweitzer DL, Aguam AS. Primary liposarcoma of the mediastinum: report of a case and review of the literature. J Thorac Cardiovasc Surg. 1977;74:83–97. [PubMed] [Google Scholar]
- 4.Chen M, Yang J, Zhu L, Zhou C, Zhao H. Primary intrathoracic liposarcoma: a clinicopathologic study and prognostic analysis of 23 cases. J Cardiothorac Surg. 2014;9:119. doi: 10.1186/1749-8090-9-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boland JM, Colby TV, Folpe AL. Liposarcomas of the mediastinum and thorax: a clinicopathologic and molecular cytogenetic study of 24 cases, emphasizing unusual and diverse histologic features. Am J Surg Pathol. 2012;36:1395–1403. doi: 10.1097/PAS.0b013e3182562bc1. [DOI] [PubMed] [Google Scholar]
- 6.Brenner W, Eary JF, Hwang W, Vernon C, Conrad EU. Risk assessment in liposarcoma patients based on FDG PET imaging. Eur J Nucl Med Mol Imaging. 2006;33:1290–1295. doi: 10.1007/s00259-006-0170-y. [DOI] [PubMed] [Google Scholar]
- 7.Ortega P, Suster D, Falconieri G, Zambrano E, Moran CA, Morrison C, Suster S. Liposarcomas of the posterior mediastinum: clinicopathologic study of 18 cases. Mod Pathol. 2015;28:721–731. doi: 10.1038/modpathol.2014.152. [DOI] [PubMed] [Google Scholar]
- 8.Fukai R, Fukumura Y, Suzuki K. A dedifferentiated liposarcoma of the anterior mediastinum. Int J Clin Oncol. 2009;14:174–177. doi: 10.1007/s10147-008-0819-6. [DOI] [PubMed] [Google Scholar]
- 9.Hamanaka K, Ohashi M, Nakamura T. Primary mediastinal dedifferentiated liposarcoma resected by lateral thoracotomy with video-assisted thoracoscopic surgery. J Surg Case Rep. 2016;2016:rjv163. doi: 10.1093/jscr/rjv163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coulibaly B, Bouvier C, Jose Payan M, Thomas P. Recurrent dedifferentiated liposarcoma of mediastinum involving lung and pleura. Interact Cardiovasc Thorac Surg. 2009;9:741–742. doi: 10.1510/icvts.2009.209494. [DOI] [PubMed] [Google Scholar]
- 11.Narasimman S, Jasjit S, Navarasi S, Premnath N. A dedifferentiated large posterior mediastinal liposarcoma-an incidental finding successfully resected. Med J Malaysia. 2016;71:201–202. [PubMed] [Google Scholar]
- 12.Hirai S, Hamanaka Y, Mitsui N, Uegami S, Matsuura Y. Surgical resection of primary liposarcoma of the anterior mediastinum. Ann Thorac Cardiovasc Surg. 2008;14:38. [PubMed] [Google Scholar]
- 13.Miura K, Hamanaka K, Matsuoka S, Takeda T, Agatsuma H, Hyogotani A, Ito Ki, Nishimaki F, Koizumi T, Uehara T. Primary mediastinal dedifferentiated liposarcoma: five case reports and a review. Thorac Cancer. 2018;9:1733–1740. doi: 10.1111/1759-7714.12888. [DOI] [PMC free article] [PubMed] [Google Scholar]


