Abstract
Background:
Community Health Workers (CHWs) have been identified as effective members of healthcare teams in improving health outcomes and reducing health disparities, especially among racial and ethnic minorities. There is a growing interest in integrating CHWs into clinical settings using health informatics based strategies to help provide coordinated patient care and foster health promoting behaviors.
Objective:
In this scoping review, we outline health informatics based strategies for CHW-provider communication that aim to improve integration of CHWs into clinical settings.
Design:
A scoping review was conducted.
Eligibility Criteria:
US-based sources between 2013–2018 were eligible.
Study Selection:
Literature was identified through PubMed and Google queries and hand searching key reference lists. Articles were screened by title, abstract, then full text.
Main Outcome Measures:
Health informatics based strategies for CHW-provider communication and their impacts on patient care were documented and analyzed.
Results:
31 articles discussed health informatics based strategies for CHW-provider communication and/or integration of CHWs into clinical settings. These strategies include direct CHW documentation of patient encounters in electronic health records (EHRs), and other web-based applications. The technologies were used to document patient encounters and patient barriers to healthcare providers, but were additionally used for secure messaging and referral systems. These strategies were found to meet the needs of providers and CHWs while facilitating CHW-provider communication, CHW integration, and coordinated care.
Conclusions:
Health informatics based strategies for CHW-provider communication are important for facilitating CHW integration and potentially improving patient outcomes and improving disparities among minority populations. This integration can support the development of future disease prevention programs and healthcare policies, in which CHWs are an established part of the public health workforce. However, further investigation must be done on overcoming implementation challenges (e.g., lack of time or funding), especially in smaller resource-challenged community-based clinics that serve minority patients.
Keywords: community health workers, electronic health records, health disparities
Introduction
Racial and ethnic health disparities have been shown to consistently exist across various diseases in the United States,1,2 contributing to earlier disease onset, greater severity of disease, and increased mortality rates.3 These disparities can stem from barriers posed by the organization of health systems, such as complex reimbursement procedures for health education and counseling efforts, limited access to culturally and linguistically appropriate services, and lack of referral sources for social services.3 Facilitating public health models that enhance linkages between community and clinical settings is one approach to reducing these barriers. Such approaches allow for the integration of culturally and linguistically tailored patient education programs into healthcare settings through multi-disciplinary, team-based care that leverages community strengths and resources.4,5 Community-clinical linkage models provide opportunities to enhance patients’ awareness and self-efficacy related to disease prevention and management, and have the potential to improve quality of care and patient outcomes, resulting in decreased health disparities among minority populations, especially in the context of chronic disease.4–7 However, the majority of prior research on reduction of health disparities has focused on targeting patients, rather than healthcare institutions and communities. Thus, the most effective way to facilitate community-clinical linkage programs across various healthcare contexts remains poorly understood and organizational structures for the development of such programs remain limited.7
There has been growing interest in the integration of community health workers (CHWs) into healthcare settings as a community-clinical linkage model with special promise to reduce health disparities through coordinated care and disease prevention8,9. CHWs are public health professionals who are members of the community and share the same culture, language, socioeconomic status, and/or racial and ethnic backgrounds.10 CHWs provide culturally and linguistically tailored health education/outreach; offer social, emotional, and mental support; connect patients to community resources; and offer medical screening services with the intent of helping individual community members manage their health.11–13 Due to their unique role, CHWs have been shown to have positive impacts on health outcomes, lifestyle modifications, and disease prevention,14 and the Community Preventive Services Taskforce has recommended that CHWs be integrated into services for cardiovascular disease prevention and diabetes prevention, and management.8 Moreover, CHW programs have been shown to be cost effective by reducing unnecessary healthcare utilization and increasing net savings for institutions.15,16
There has been a recent call for the integration of CHWs into primary care teams to improve health disparities in minority populations, which has been supported by specific policy efforts. The Patient Protection and Affordable Care Act, for example, indicates that programs utilizing CHWs will be supported through grant funding and reimbursement opportunities.12 The best practices for such integration, which involves the maximization of CHWs’ roles in healthcare teams while maintaining their unique function, have been identified as: well-defined CHW roles, training team members on the value of CHWs, organized workflows, and improved communication between CHWs and clinical teams.6,7,9,11 Notably, improved communication allows for a stronger mutual understanding between CHWs and other healthcare providers, which maximizes CHWs’ impacts within care teams, including the public health workforce. Through regular interactions and better communication with CHWs, providers can have access to a broader scope of information on patients, allowing for a more patient-centered approach to coordination of care, and improved patient disease management and prevention.11,13,17
While the benefits of CHW integration into care teams through improved CHW-team communication methods have been well documented, there has been limited data on specific mechanisms and tools to most effectively accomplish such integration.4,18–20 Specifically, there has been recent interest in exploring health informatics to enhance integration and communication through CHW access to technologies that allow for inclusion of CHW collected data into workflows and care plans.12,19–21 These technologies include electronic health records (EHRs), cloud-based services, medical devices, mobile apps, and other non-EHR web-based technologies that transmit information without acting as official patient health records.22 Health informatics can help organize and integrate patient social determinants of health (SDOH) data (e.g., income level and employment status) into clinical workflows to support actions such as referrals to community resources or appropriate patient education, potentially making them a useful tool for CHW documentation and communication23. Under this framework, health informatics strategies can support integration and optimization of CHWs’ public health efforts by acting as an organizational platform where CHWs can document their work, which can then be interpreted by healthcare teams to better address SDOH needs and reinforce health promoting behaviors.23
Accordingly, we conducted a scoping review on health informatics based strategies for CHW-provider communication that aim to improve integration of CHWs into clinical settings. We also discuss the advantages, limitations, and future directions to maximize these strategies in the context of clinical care.
Methods
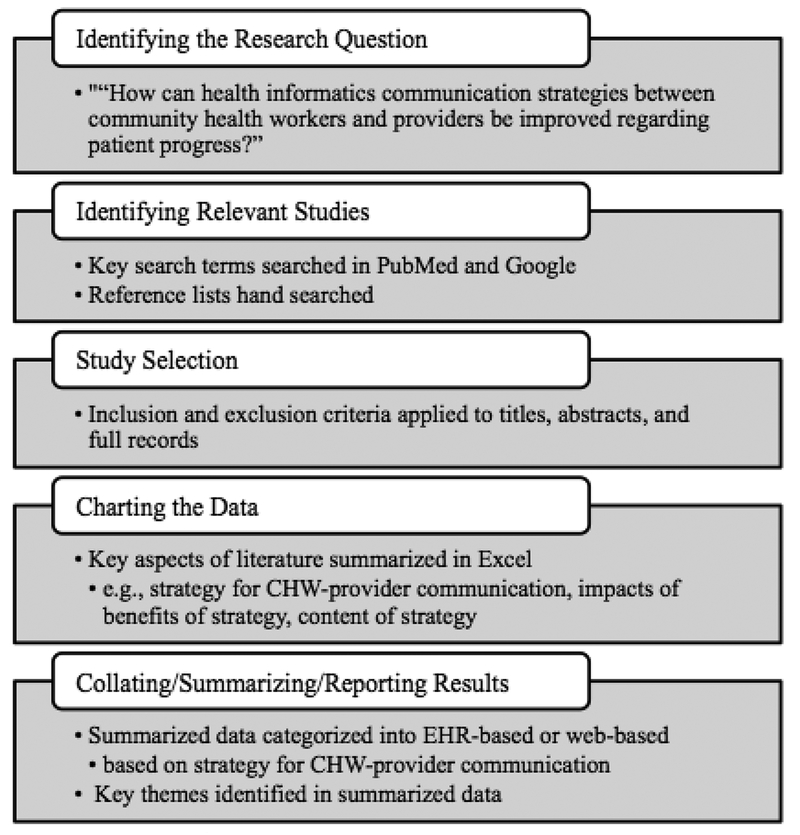
A scoping review was conducted in order to identify and summarize strategies for communication between CHWs and medical providers in the context of improving CHW integration into clinical settings. A scoping review aims to examine literature using a broader framework with the intent of providing an overview of existing evidence and/or identifying gaps in literature rather than answering a specific question.24 We utilized common procedures outlined by Levac et al’s recommendations on Arskey and O’Malley’s methodological framework for conducting scoping reviews (detailed in Figure 1).25
Figure 1:
Overview of Methodology
Identifying the research question
The initial research question to guide the scoping review was “How can community health workers be integrated into the clinical setting?” Due to the wide breadth of strategies for integration, this question was narrowed down to focus on health informatics based strategies for communication between CHWs and clinic staff to allow for a more depth in exploration. The revised and final questions were “What are the various types of health informatics strategies that are currently being utilized to improve communication between CHWs and providers?” and “What is the impact of CHW use of health informatics on patient care?”
Identifying relevant studies
The searches were conducted in July 2018. Relevant literature was identified through PubMed queries and hand searching of reference lists for peer reviewed articles. Google searches were also conducted to identify grey literature, which includes materials produced by institutions outside of commercial publishing, such as government agency reports, research institute working papers, or organization technical guides.26 A broad set of search terms were utilized to encompass healthcare persons similar to CHWs (detailed in Table 1).
Table 1.
Key Search Terms
| Concept or intervention | Context |
|---|---|
| Community health worker(s) | Integration |
| CHW(s) | Strategy |
| Patient navigator(s)/navigation | Communication |
| Promotore(s) |
Study selection
Identified literature was screened first by title, then abstract, then full text. Inclusion criteria for the study were: 1) the primary focus was CHW programs; 2) the CHW programs were implemented in clinical settings; 3) the CHWs did not have previous training in other healthcare careers (e.g., nursing, social work, etc.); and 4) specific health informatics based methods for how CHWs in the program communicated and/or interacted with medical providers were discussed. Manuscripts focusing on CHW programs based in countries outside the United States were excluded. Manuscripts published more than 5 years ago (before 2013) were excluded, unless they discussed strategies for CHW-provider communication not found in more recent literature. If multiple papers were discussing the same method for CHW-provider communication in the context of the same CHW program, only the most recent paper was included. One reviewer (AK) screened all the titles and abstracts; the methodology for study selection was reviewed and overseen by SL.
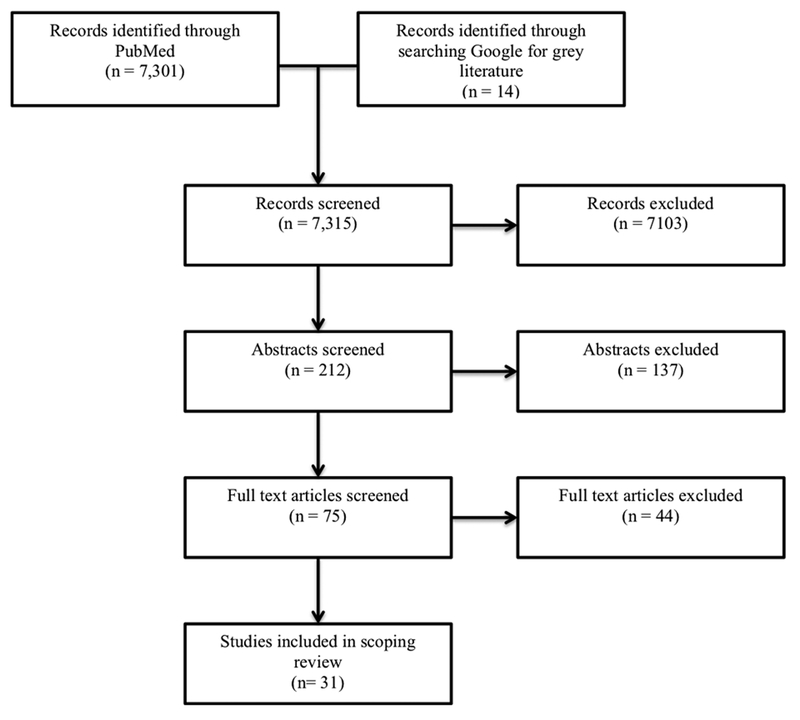
The initial search generated 7,315 records, of which 7,103 records were excluded due to not being within the past 5 years, not being based in the United States, and/or the titles not being relevant to the research question (Figure 2). The abstracts of the remaining 212 records were screened, of which 137 were excluded. The full text articles of the remaining 75 records were screened; 44 were excluded, resulting in 31 articles included in the scoping review.
Figure 2:
Study Selection Process
Charting the data
Information from the selected literature was documented in Microsoft Excel by recording key aspects of the CHW programs discussed, including name of the program, affiliated institutions, location, target population, target disease, CHW roles, strategies for and content of CHW-provider communication, and evaluation of strategies.
Collating, summarizing, and reporting results
The data from each article was first deductively coded with the research questions in mind to provide a basic analysis of the characteristics and context of the literature. Second, the data was inductively coded using descriptive thematic analysis and narrative synthesis. Thematic analysis involves sorting of data, searching for themes by identifying patterns through tables or maps, and defining the themes.27 Narrative synthesis includes exploring relationships in the data and assessing the validity of the data.28 The data was coded by AK; the coding scheme and final themes were reviewed by SL.
Results
31 papers were included in the review and are summarized in Tables 2 and 3. Seven of the strategies utilized web-based or mobile applications while twenty-four used EHRs. Thirteen of the papers were evaluations/descriptions of CHW programs, eleven were analyses (including randomized controlled trials) of CHW program outcomes, three were grey literature guides to implementation of CHW programs, two were perspective pieces, one was a case study, and one was a review. CHW programs were based in a variety of settings, including: academic hospitals or health systems (11); community clinics (8), two of which were closely affiliated with academic institutions; federally qualified health centers (3); and patient-centered medical homes (2), both of which were affiliated with academic institutions.
Table 2.
Characteristics of Included Studies Utilizing Health Informatics Strategies
| Type of Health Informatics Technology | Primary Role of Health Informatics in Communication | First Author | Study Type | Setting | Comments on Strategy |
|---|---|---|---|---|---|
| EHR – Direct Access | Direct CHW Communication with Providers | Allen et al, 201518 | Evaluation of CHW perspectives | CHWs recruited from American Public Health Association | CHWs used EHRs to communicate directly and indirectly with providers, make appointments, and track patients |
| Valaitis et al29 | Scoping review | Patient navigator programs across US | Navigators used EHRs to share information with providers | ||
| Documentation of CHW Encounters | Gunn et al, 201430 | Exploratory study | Patient navigation programs across US | Navigators used EMRs, charts, or other systems to document patient care | |
| Gunn et al, 201731 | Mixed-methods analysis | Patient Navigation Research Program | Navigators documented/communicated patient progress with providers via EMR/IT systems | ||
| Horny et al32 | Retrospective cohort study | Boston Medical Center | Navigators recorded information, including patient barriers, in detailed navigator template forms in EMRs | ||
| Johnson et al21 | Perspective on CHWs | Children’s Hospital of Wisconsin | CHWs used EHRs to receive providers’ referrals and document patient progress | ||
| Jolly et al33 | Description of program | Cleveland Clinic | Navigators used EHR templates to document/communicate patient data | ||
| King et al34 | Evaluation of programs | Navajo clinics in Southwest US | CHWs documented patient encounters in EHR | ||
| Ngo et al35 | Guide | Sinai Urban Health Institute | CHWs documented case notes in EHRs | ||
| Ramachandran et al36 | Secondary analysis | Boston Patient Navigation Research Program | Navigators documented patient encounters, barriers to care, care plans, and progress in a template in EHR | ||
| Reinschmidt et al13 | Evaluation of programs | Federally Qualified Health Centers in Arizona | CHWs documented patient encounters into EHRs (directly during visits or copy from paper | ||
| Rohan et al37 | Randomized trial | Boston Medical Center | Navigators documented patient notes in medical records system form | ||
| Spiro et al38 | Description of CHW model | Massachusetts General Hospital Chelsea Community Health | CHWs entered patient progress into EMRs | ||
| Vora et al39 | Report on program | Charles B Wang Community Health Center | Navigators updated patient flow sheet in EMR; navigators reviewed patient history and patients’ barriers in EMR | ||
| EHR – Indirect Access | Documentation of CHW Encounters | Wennerstrom et al40 | Description and evaluation of program | Patient Centered Medical Home in Louisiana | CHWs tracked patient information in electronic spreadsheets; medical office assistants attached spreadsheets to EHR |
| Other | Lopez et al19 | Protocol for randomized controlled trial | Community clinics in New York City | EHR intervention (routine patient registry reports, medical alerts, culturally tailored order sets) combined with CHW program | |
| Mobile Applications | Direct CHW Communication with Providers AND Documentation of CHW Encounters | Cherrington et al41 | Description of web application | Congregations for Public Health and Cooper Green Mercy Health System | CHWs used web based mobile application to document progress reports, track patients, and communicate with healthcare team |
| Cloud Based Systems | Direct CHW Communication with Providers AND Documentation of CHW Encounters | Kangovi et al, 201442 Kangovi et al, 201743 |
Randomized clinical trial | University of Pennsylvania IMPaCT Model | CHWs utilized cloud based software that integrates with EHRs to track workflow, analyze patient progress, create reports, and can be used to message providers |
| Web-Based Systems | Documentation of CHW Encounters | DeGroff et al44 | Randomized control trial | Boston Medical Center | Navigators documented participant barriers in navigator database |
| Justvig et al45 | Prospective description | Stony Brook University Hospital | CHWs documented patient visits in Research Electronic Data Capture | ||
| Kane et al46 Walton et al47 |
Analysis of CHW program outcomes | Baylor Health Care System/Baylor Scott and White Health community clinics | CHWs and providers utilized a HIPAA compliant web-based system to record patient progress and create reports that were added to patient’s medical records | ||
| Percac-Lima et al48 | Randomized clinical trial | Massachusetts General Primary Care Practice Research Network | Navigators used IT application to track/contact patients and document interventions |
Table 3.
Characteristics of Included Studies Recommending Health Informatics Strategies
| Type of Health Informatics Technology | Primary Role of Health Informatics in Communication | First Author | Study Type | Setting | Comments on Strategy |
|---|---|---|---|---|---|
| EHR – Direct Access | Documentation of CHW Encounters | Allen et al, 201420 | Guide | CHW programs in US | Recommend giving supervisor access to EHR or CHW access to EHR templates |
| Brown et al49 | Evaluation of provider views | Bellevue and VA NY Harbor Hospitals | Suggest CHWs enter patient updates into EHRs | ||
| Collinsworth et al50 | Evaluation of programs | Community clinics in Dallas | Suggest giving CHWs access to EHRs | ||
| Ingram et al51 | Qualitative analysis | Federally qualified health centers | Suggest CHWs use EHRs to collect data | ||
| Matiz et al52 | Case study | Patient Centered Medical Homes in New York City | Suggest CHW data collection via EHRs rather than paper forms | ||
| Whiteman et al53 | Perspective on programs | N/A | Suggest CHWs should record patient progress summaries in EMRs | ||
| Mobile Applications | Documentation of CHW Encounters | Broderick et al54 | Guide | CHW programs in California | Recommend partnering with mobile health technology organizations to utilize CHW mobile data collection strategies |
Type of CHW access to health informatics
A majority of strategies for CHW-provider communication leveraged EHRs in the context of a variety of settings including community clinics and academic health systems. Nine papers reported CHWs having access to EHRs or EMRs, and five papers suggested this access should occur, but none of the paper specified in what format information would be captured.13,18,21,29–31,34,35,38,49–53 Six papers discussed CHWs having access to specific forms, structured questionnaires, or templates in EHRs.20,32,33,36,37,39 In one study, some of the CHWs input patient information directly into the EHR during the patient visit, while others took notes on paper and later input them into the EHR.13 One paper suggested giving only CHW supervisors access to EHRs20 while another had medical office assistants attach CHW documentation to the EHRs.40 Two papers reported utilizing or suggested utilizing mobile applications for CHWs to collect patient information.41,54 One program had CHWs document patient updates into an online research database,45 while three utilized other web-based or cloud-based systems.42,43,46–48 Of the programs using non-EHR web-based applications, all were associated with academic health systems; in one of these programs, reports generated from the system were faxed to the patient’s provider to be added to the patient’s medical record.47
Role of health informatics for CHW documentation
A majority of papers reported utilizing health informatics to document patient notes/progress from CHW encounters. Because a majority of papers indicate that the purpose of documentation is to share this information with providers, degree of documentation may allow for increased potential amount of communication. In one program, this included documenting patients’ health concerns and referrals made to social services.40 The patient notes also included clinical indicators and sociodemographic characteristics (e.g., literacy, blood pressure) as well as patients’ knowledge of their disease, physical activity, and quality of life.47 In another program, screening test results alerting the provider to follow up with the patient were documented.39 CHWs also documented specific SDOH barriers in health information systems,32,36,37,44 such as transportation, housing, and childcare32 as well as actions taken to these address barriers.37 All of the papers that described documentation of patient barriers were associated with multiple studies conducted within one academic institution in an urban setting. In three papers, it was explicitly discussed that CHWs documented and/or shared the patient’s care plan or intervention.36,43,48 Of note, less than half of the papers described the variables that were documented by CHWs.
Role of health informatics for direct CHW-patient and CHW-provider communication
Of the studies utilizing health informatics for CHW-provider communication, many had uses beyond documentation of encounters. CHWs used EHRs to generate reminders for patient follow-up,18 to make appointments with patients,18,21 or to view patients’ histories before patient visits.13,39 Three papers utilized web-based/cloud-based applications to generate reports on data from CHW encounters, such as frequency of contact with patients and achievement of patient goals.42,43,46,47 CHWs also used health informatics to communicate with providers through secure direct messaging systems18,41 or referral systems.21 Additionally, in one program, EHRs were used to augment the work of CHWs by implementing culturally tailored ordered sets;19 order sets consist of a “bundle” of evidence-based guidelines and/or educational materials that help providers order the appropriate prescriptions/labs, and counsel patients in a standardized manner.19,55 In a different program, clinical pathways were embedded into web-based applications to prompt CHWs to contact providers immediately when urgent concerns, such as critically abnormal blood pressures or glucose measurements, arose.46 In another study, CHWs used an IT application to directly contact patients and provide them with educational resources.48 Of the papers that recommended health informatics strategies, none mentioned uses beyond documentation of patient encounters.
Impact of health informatics on CHW-provider communication
Several studies found that CHW utilization of EHRs and other health information technologies improved communication between CHWs and providers.18,33,38,50 Two papers found that it allowed for CHWs to maintain continuous communication with providers with real-time patient updates.37,53 CHW use of EHRs also increased the ability of CHWs to contact providers regarding patient concerns, augmenting the overall amount of communication.34 In two papers, the improved CHW-provider communication resulting from utilization of EHRs was shown to be key in enhancing the role of CHWs in clinical teams.21,30 In focus groups conducted among CHWs, it was found that CHWs were more likely to be recognized and valued by providers due to the improved communication. This was found to be a necessary step in helping providers consider CHWs a part of their care teams.34
Furthermore, improved communication with CHWs was found to fulfill the needs of providers and CHWs in enriching their abilities to provide care in academic and community health systems. Providers indicated that they wanted CHWs to enter patient progress updates in EHRs49 and that this documentation facilitated their communication with CHWs.49,50 Specifically, EHR notes from CHWs allowed providers to view patients’ clinical data at the same time as contextual information on sociocultural backgrounds to enhance their understanding of the patients’ motivations to seek care.50,51 This system allows for data collected by CHWs to be imparted onto providers, thus increasing the level of communication. In one paper, it was found that sharing information about patient visits with providers through reports generated from a web-based application were useful in highlighting issues that may need to be addressed at subsequent visits with the provider.47 Similarly, using EHRs allowed CHWs to tailor their patient education by allowing them to view patients’ histories and gain insight on the barriers the patient may be facing.39
Impact of health informatics on patient care
Health informatics based communication between CHWs and providers was also found to impact patient care and outcomes. It was found that CHW utilization of EHRs and web-based applications facilitated better-coordinated care and improved patient outcomes in the context of community clinics, such as a 7% increase in colon cancer screening rates and decrease in mean hemoglobin A1C from 8.7% to 7.4% in diabetes patients after intervention.39,47 Another paper found that a CHW based health informatics intervention was associated with improvement in smoking cessation (5.6 vs 1.3 mean decrease in cigarettes smoked daily in CHW-health informatics group compared to control group).43
Barriers presented by health informatics
In a few papers, CHW use of health informatics was found to present certain challenges. For example, in a provider focus group, not all of the information documented by CHWs was found to be useful in clinical decision-making and was considered excessive by providers40,49. On the other hand, certain information that is relevant to clinical care, such as social determinants of health, were found to be difficult to track via EHRs because these technologies have not been designed to document this information51. Additionally, in one CHW program, some providers were unaware that they were able to view CHWs’ notes in EHRs, which would limit the benefits of this form of communication. Furthermore, the providers who were aware of the CHW notes felt it was too complicated and time consuming to view the notes13.
Discussion
A majority of the health informatics based strategies for CHW-provider communication identified through the 31 papers in the scoping review suggested giving CHWs access to EHRs, templates within EHRs, or web-based/cloud-based applications in order to provide a tool for CHW documentation of patient progress as well as communication of patient sociodemographic characteristics, clinical indicators, barriers, and action plans with providers. They also support CHW-provider and CHW-patient communication through additional features such as secure messaging systems and generated reports. The papers found that these strategies may allow for increased communication between CHWs and providers, deeper provider understanding of the patient with more tailored care, though most evaluations for provider-CHW communication were qualitative in nature. Some of the papers also found these strategies to be associated with better coordination of care, with the potential to support improved patient outcomes through promotion of positive health behaviors and delay in disease progression. Given the wide distribution of cities and populations targeted in the reviewed literature, these findings suggest that using health informatics for communication between CHWs and providers may be a promising approach to increasing CHW engagement and integration into clinics accommodating diverse urban populations, racial and ethnic communities, and diseases. However, while the studies in this review suggest a potentially significant impact of use of health informatics tools to improve communication between CHWs, providers, and patients, none of the papers in this review included rigorous randomized control or pragmatic trial designs comparing health informatics with other methods of communication, presenting a clear opportunity to advance the science of CHW integration in the setting of community-centered interventions aimed at reducing racial and ethnic disparities.
Moreover, given the barriers to using health informatics in the context of smaller, community clinics, such as providers finding it too complicated or time consuming to view CHW notes in EHRs, there is also a need for additional studies that examine the use of health informatics strategies to facilitate CHW integration in such settings.13,56 Limitations faced by these practices including time, staff, and funding leading to diminished administrative support for utilizing EHRs and accessing trainings, have been well documented and may further impact the use of health informatics to support CHW integration in such.57 For example, in community clinics, CHWs may play an especially important supportive role to an already small team and have decreased capacity and time for accessing/entering data into EHRs. Further, many community clinics have limited opportunities to develop alternate web-based applications to facilitate CHW-provider communication. Small, community-based practices serve disproportionate numbers of minority patients;58 thus, effectively implementing community-centered, culturally tailored, public health interventions and integrating CHWs into these clinics is especially critical and warrants further attention.
Finally, regarding future directions of health informatics for CHW documentation, some papers in this review suggested amending EHRs for more detailed and easier documentation of SDOH data.13,51 Interestingly, a majority of papers in this review did not mention the format in which SDOH data was documented, perhaps because the appropriate manner for capturing this information is still being established. One possible format includes EHR based flowsheets filled out by CHWs on factors such as patients’ financial limitations, social support, and education level.59 By capturing this SDOH data, CHWs maximize their role in the public health workforce by enhancing providers’ capacity to address upstream factors that impact well-being. The SDOH data in EHRs can be interpreted by providers to enhance their contextual understanding of patients’ barriers to care in order to appropriately tailor patient outreach. This framework of EHR as a tool for communication and integration of data collected by CHWs amplifies CHWs’ efforts to foster patient disease self-management, medication adherence, lifestyle modifications, and other behaviors that prevent disease progression.
To optimize this integration, EHRs should be complemented by regular healthcare team trainings on how to most effectively understand and utilize the social context data entered by CHWs in clinical decision-making.13 This is important because CHWs are advocates for their patients and experts on their communities; effectively acknowledging their perspectives and integrating their work into clinic workflows creates a unique opportunity to provide enhanced, patient-centered, culturally tailored, and coordinated care in which cultural/linguistic barriers are reduced and patients are connected to appropriate community resources.9 This elevated care in minority communities is a crucial component of reducing disease severity and working towards health equity. Moreover, as CHWs continue to become more integrated into clinical settings, they are at risk of becoming medicalized and their identities and impacts are being lost. CHWs utilizing EHRs and becoming habituated to the clinical algorithms and medical pathways embedded into such systems may propagate this process. Guidance from both community members and healthcare leaders in order to clearly define CHW identities, expectations, and roles as well as tailoring EHRs and relevant trainings will help minimize medicalization while highlighting the perspectives of CHWs.60
There are several limitations to this review. First, this review did not address the cost of different health informatics platforms as it was beyond the scope of the review, though it is an important area of research. The search, study selection, and study extraction were conducted by one reviewer, which could have allowed for selection bias. While the search was expanded to include terms alternately used for CHWs, papers using other terms for this role could have been missed. In addition, because papers were excluded based on titles and abstracts, it is possible that relevant papers were missed. However, this methodology allowed for us to identify a broader range of literature. Finally, because a scoping review, rather than a systematic review, was conducted, the quality of papers was not assessed using a standardized criteria.
Implications for Policy and Practice.
Given current policies, such as the Patient Protection and Affordable Care Act, continue to support CHWs through grant funding, it is important to evaluate their impact in clinical settings and improve their efficiency and efficacy to optimize health outcomes, especially for racial and ethnic minority communities.
To improve CHW integration into clinics and communication with providers, encouraging direct CHW utilization of EHRs may be a best practice, particularly for capturing SDOH data and other contextual factors faced by patients that CHWs are uniquely suited to discover and document. However, careful attention must be placed on setting clear expectations, maintaining community identities, defining a unique scope of work, and integrating workflows for CHWs through balanced health-community partnerships.60
To optimize CHW utilization of technology, further research should be done on conducting regular trainings for CHWs and healthcare providers regarding documentation and interpretation of SDOH data and other CHW-collected data on patient needs and experiences.
To overcome implementation barriers in smaller community clinics, further research should be done on sustainability and efficacy of CHW use of health informatics in these settings to help guide local policies and municipal agencies in providing appropriate resources to support technologies that can be utilized by CHWs.
Acknowledgements:
We would like to thank the community health workers that are a part of NYU Department of Population Health’s Section for Health Equity for their efforts and ongoing feedback on program enhancement.
Funding: This publication was supported by the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (NIMHD) grant U54MD000538; Centers for Disease Control and Prevention (CDC) Grant U48DP001904; NIH National Institute of Diabetes and Digestive Kidney Diseases (NIDDK) grants R01DK110048 and R18DK110740; and NIH National Center for the Advancement of Translational Science (NCATS) Grant UL1TR001445. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH NIMHD, CDC, NIH NIDDK, or NIH NCATS.
Footnotes
Funding Disclosure:
The authors declare that they have no funding disclosures.
Conflicts of Interest:
The authors declare that they have no conflicts of interest.
REFERENCES
- 1.Johnson-Askew WL, Gordon L, Sockalingam S. Practice paper of the American Dietetic Association: addressing racial and ethnic health disparities. J Am Diet Assoc. 2011;111(3):446–456. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine Committee on U, Eliminating R, Ethnic Disparities in Health C. In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US) [PubMed] [Google Scholar]
- 3.Institute of M The National Academies Collection: Reports funded by National Institutes of Health. In: Smedley BD, Stith AY, Nelson AR, eds. How Far Have We Come in Reducing Health Disparities? Progress Since 2000: Workshop Summary. Washington (DC): National Academies Press (US) National Academy of Sciences.; 2012. [PubMed] [Google Scholar]
- 4.Fisher TL, Burnet DL, Huang ES, Chin MH, Cagney KA. Cultural leverage: interventions using culture to narrow racial disparities in health care. Medical care research and review : MCRR. 2007;64(5 Suppl):243s–282s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Islam NS, Kwon SC, Wyatt LC, et al. Disparities in diabetes management in Asian Americans in New York City compared with other racial/ethnic minority groups. American journal of public health. 2015;105 Suppl 3:S443–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chin MH, Clarke AR, Nocon RS, et al. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med. 2012;27(8):992–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clarke AR, Goddu AP, Nocon RS, et al. Thirty years of disparities intervention research: what are we doing to close racial and ethnic gaps in health care? Med Care. 2013;51(11):1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Force CPST. Guide to Community Preventitive Services. Community Health Workers. The Community Guide. 2017. [Google Scholar]
- 9.Islam N, Nadkarni SK, Peretz PJ, et al. Integration of Community Health Workers into Primary Care Health Systems: The Time for New York is Now! NYU-CUNY Prevention Research Center. 2016. [Google Scholar]
- 10.Love MB, Gardner K, Legion V. Community health workers: who they are and what they do. Health education & behavior : the official publication of the Society for Public Health Education. 1997;24(4):510–522. [DOI] [PubMed] [Google Scholar]
- 11.Association APH. Support for Community Health Workers to Increase Health Access and to Reduce Health Inequities. 2009. [Google Scholar]
- 12.Islam N, Nadkarni SK, Zahn D, Skillman M, Kwon SC, Trinh-Shevrin C. Integrating community health workers within Patient Protection and Affordable Care Act implementation. Journal of public health management and practice : JPHMP. 2015;21(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reinschmidt KM, Ingram M, Morales S, et al. Documenting Community Health Worker Roles in Primary Care: Contributions to Evidence-Based Integration Into Health Care Teams, 2015. The Journal of ambulatory care management. 2017;40(4):305–315. [DOI] [PubMed] [Google Scholar]
- 14.Roland KB, Milliken EL, Rohan EA, et al. Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes Among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review. Health equity. 2017;1(1):61–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. American journal of public health. 2005;95(4):652–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of west Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethnicity & disease. 2003;13(1):22–27. [PubMed] [Google Scholar]
- 17.Findley S, Matos S, Hicks A, Chang J, Reich D. Community health worker integration into the health care team accomplishes the triple aim in a patient-centered medical home: a Bronx tale. J Ambul Care Manage. 2014;37(1):82–91. [DOI] [PubMed] [Google Scholar]
- 18.Allen CG, Escoffery C, Satsangi A, Brownstein JN. Strategies to Improve the Integration of Community Health Workers Into Health Care Teams: “A Little Fish in a Big Pond”. Preventing chronic disease. 2015;12:E154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez PM, Zanowiak J, Goldfeld K, et al. Protocol for project IMPACT (improving millions hearts for provider and community transformation): a quasi-experimental evaluation of an integrated electronic health record and community health worker intervention study to improve hypertension management amongSouth Asian patients. BMC health services research. 2017;17(1):810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Allen C, Brownstein JN, Mirambeau A, Jayapaul-Philip B. Technical Assistance Guide for States Implementing Community Health Worker Strategies. CDC 2014. [Google Scholar]
- 21.Johnson SL, Gunn VL. Community Health Workers as a Component of the Health Care Team. Pediatric clinics of North America. 2015;62(5):1313–1328. [DOI] [PubMed] [Google Scholar]
- 22.Hemmat M, Ayatollahi H, Maleki M, Saghafi F. Future Research in Health Information Technology: A Review. Perspectives in health information management. 2017;14(1b). [PMC free article] [PubMed] [Google Scholar]
- 23.Cottrell EK, Gold R, Likumahuwa S, et al. Using Health Information Technology to Bring Social Determinants of Health into Primary Care: A Conceptual Framework to Guide Research. Journal of health care for the poor and underserved. 2018;29(3):949–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bassi J, Lau F. Measuring value for money: a scoping review on economic evaluation of health information systems. Journal of the American Medical Informatics Association : JAMIA. 2013;20(4):792–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levac D, Colquhoun H, O’Brien KKJIS. Scoping studies: advancing the methodology. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Systemic Reviews: the process: Grey Literature. Duke University. Published 2019. Accessed2019. [Google Scholar]
- 27.Nowell LS, Norris JM, White DE, Moules NJ. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. International Journal of Qualitative Methods. 2017;16(1):1609406917733847. [Google Scholar]
- 28.Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice AU - Snilstveit, Birte. Journal of Development Effectiveness. 2012;4(3):409–429. [Google Scholar]
- 29.Valaitis RK, Carter N, Lam A, Nicholl J, Feather J, Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC health services research. 2017;17(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gunn CM, Clark JA, Battaglia TA, Freund KM, Parker VA. An assessment of patient navigator activities in breast cancer patient navigation programs using a nine-principle framework. Health services research. 2014;49(5):1555–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gunn C, Battaglia TA, Parker VA, et al. What Makes Patient Navigation Most Effective: Defining Useful Tasks and Networks. Journal of health care for the poor and underserved. 2017;28(2):663–676. [DOI] [PubMed] [Google Scholar]
- 32.Horny M, Glover W, Gupte G, Saraswat A, Vimalananda V, Rosenzweig J. Patient navigation to improve diabetes outpatient care at a safety-net hospital: a retrospective cohort study. BMC health services research. 2017;17(1):759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jolly SE, Navaneethan SD, Schold JD, et al. Development of a chronic kidney disease patient navigator program. BMC nephrology. 2015;16:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King C, Goldman A, Gampa V, et al. Strengthening the role of Community Health Representatives in the Navajo Nation. BMC public health. 2017;17(1):348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ngo V, Hammer H, Bodenheimer T. Health coaching in the teamlet model: a case study. Journal of general internal medicine. 2010;25(12):1375–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramachandran A, Freund KM, Bak SM, Heeren TC, Chen CA, Battaglia TA. Multiple barriers delay care among women with abnormal cancer screening despite patient navigation. Journal of women’s health (2002). 2015;24(1):30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rohan EA, Slotman B, DeGroff A, Morrissey KG, Murillo J, Schroy P. Refining the Patient Navigation Role in a Colorectal Cancer Screening Program: Results From an Intervention Study. Journal of the National Comprehensive Cancer Network : JNCCN. 2016;14(11):1371–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spiro A, Oo SA, Marable D, Collins JP. A unique model of the community health worker: the MGH Chelsea Community Health Improvement team. Family & community health. 2012;35(2):147–160. [DOI] [PubMed] [Google Scholar]
- 39.Vora S, Lau JD, Kim E, Sim SC, Oster A, Pong P. Patient Navigation Program for Colorectal Cancer Screening in Chinese Americans at an Urban Community Health Center: Lessons Learned. Journal of health care for the poor and underserved. 2017;28(3):887–895. [DOI] [PubMed] [Google Scholar]
- 40.Wennerstrom A, Bui T, Harden-Barrios J, Price-Haywood EG. Integrating community health workers into a patient-centered medical home to support disease self-management among Vietnamese Americans: lessons learned. Health promotion practice. 2015;16(1):72–83. [DOI] [PubMed] [Google Scholar]
- 41.Cherrington AL, Agne AA, Lampkin Y, et al. Diabetes Connect: Developing a Mobile Health Intervention to Link Diabetes Community Health Workers With Primary Care. The Journal of ambulatory care management. 2015;38(4):333–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA internal medicine. 2014;174(4):535–543. [DOI] [PubMed] [Google Scholar]
- 43.Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community Health Worker Support for Disadvantaged Patients With Multiple Chronic Diseases: A Randomized Clinical Trial. American journal of public health. 2017;107(10):1660–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DeGroff A, Schroy PC 3rd, Morrissey KG, et al. Patient Navigation for Colonoscopy Completion: Results of an RCT. American journal of preventive medicine. 2017;53(3):363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Justvig SP, Li J, Caravella G, et al. Improving Adherence to Care Recommendations Using a Community Health Worker (CHW) Intervention with the Pediatric Medical Home. Journal of community health. 2017;42(3):444–452. [DOI] [PubMed] [Google Scholar]
- 46.Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes with community health workers. Family practice. 2016;33(5):523–528. [DOI] [PubMed] [Google Scholar]
- 47.Walton JW, Snead CA, Collinsworth AW, Schmidt KL. Reducing diabetes disparities through the implementation of a community health worker-led diabetes self-management education program. Family & community health. 2012;35(2):161–171. [DOI] [PubMed] [Google Scholar]
- 48.Percac-Lima S, Ashburner JM, Zai AH, et al. Patient Navigation for Comprehensive Cancer Screening in High-Risk Patients Using a Population-Based Health Information Technology System: A Randomized Clinical Trial. JAMA internal medicine. 2016;176(7):930–937. [DOI] [PubMed] [Google Scholar]
- 49.Brown A, Wong G, Gore R, Schwartz M. Baseline Assessment of Providers’ Perspectives on Integrating Community Health Workers into Primary Care Teams to Improve Diabetes Prevention (google search). [Google Scholar]
- 50.Collinsworth A, Vulimiri M, Snead C, Walton J. Community health workers in primary care practice: redesigning health care delivery systems to extend and improve diabetes care in underserved populations. Health promotion practice. 2014;15(2 Suppl):51s–61s. [DOI] [PubMed] [Google Scholar]
- 51.Ingram M, Doubleday K, Bell ML, et al. Community Health Worker Impact on Chronic Disease Outcomes Within Primary Care Examined Using Electronic Health Records. American journal of public health. 2017;107(10):1668–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matiz LA, Peretz PJ, Jacotin PG, Cruz C, Ramirez-Diaz E, Nieto AR. The impact of integrating community health workers into the patient-centered medical home (similar to Integratig Community Health Workers). Journal of primary care & community health. 2014;5(4):271–274. [DOI] [PubMed] [Google Scholar]
- 53.Whiteman LN, Gibbons MC, Smith WR, Stewart RW. Top 10 Things You Need to Know to Run Community Health Worker Programs: Lessons Learned in the Field. Southern medical journal. 2016;109(9):579–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Broderick A, Barnett K. Community Health Workers in California: Sharpening Our Focus on Strategies to Expand Engagement. California Health Workfroce Alliance. 2015. [Google Scholar]
- 55.Clinical Decision Support: More than just ‘Alerts’ Tipsheet. Centers for Medicare & Medicaid Services. [Google Scholar]
- 56.Schlotthauer AE, Badler A, Cook SC, Perez DJ, Chin MH. Evaluating interventions to reduce health care disparities: an RWJF program. Health affairs (Project Hope). 2008;27(2):568–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Divney AA, Lopez PM, Huang TT, Thorpe LE, Trinh-Shevrin C, Islam NS. Research-grade data in the real world: challenges and opportunities in data quality from a pragmatic trial in community-based practices. Journal of the American Medical Informatics Association. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Archives of internal medicine. 2007;167(12):1233–1239. [DOI] [PubMed] [Google Scholar]
- 59.Gold R, Bunce A, Cowburn S, et al. Adoption of Social Determinants of Health EHR Tools by Community Health Centers. Annals of family medicine. 2018;16(5):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Garfield C, Kangovi S. Integrating Community Health Workers Into Health Care Teams Without Coopting Them. In. Health Affairs Blog: Health Affairs; 2019. [Google Scholar]