Abstract
Respiratory sinus arrhythmia (RSA) is a biomarker of mental health, but RSA-symptom relations in parents of young children are understudied. We examined how anxiety symptoms, depressive symptoms, resting RSA, and RSA reactivity during challenging parent-child interactions clustered in a community sample of mothers (N=126) and fathers (N=87) of 3-year-olds and whether profiles predicted child emotional and behavioral dysregulation at age 4. Mothers fit four profiles (Typical, Mild Risk, Moderate Risk/Withdrawal, Moderate Risk/Augmentation), suggesting that RSA reactivity was distinct by predominant symptom type at higher levels of risk: specifically, heightened RSA withdrawal was associated with a higher probability of anxiety symptoms and RSA augmentation was associated with a higher probability of depressive symptoms. Fathers fit three profiles (Typical, Mild Risk, Moderate Risk) where Moderate Risk was characterized by RSA augmentation and a higher probability of both anxiety and depressive symptoms. Mild risk profiles showed heightened resting RSA for mothers and fathers but no differences in RSA reactivity. Both mild and moderate risk profiles predicted higher child dysregulation one year later compared to typical profiles. Findings offer preliminary evidence that parasympathetic physiology covaries with symptoms differently for mothers and fathers and that parental profiles of physiology and symptoms inform children’s developmental psychopathology.
Keywords: respiratory sinus arrhythmia, anxiety, depression, fathers, behavior problems
Anxiety and depressive symptoms are the most commonly experienced mental health symptoms by adults in the United States (APA, 2013). They include symptoms such as depressed mood, loss of interest in activities, sleep and eating disturbances, nervousness, increased heart rate, and concentration problems (APA, 2013). Approximately 68% of symptomatic women are mothers and 57% of symptomatic men are fathers (Royal College of Psychiatrists, 2016). Both mothers and fathers are at risk for developing anxiety and depressive symptoms after childbirth (Paulson & Bazemore, 2010), likely due to the additional stressors presented by parenthood (Crnic & Low, 2002). Understanding parent symptomology is particularly important because parents’ anxiety and depressive symptoms may negatively impact children’s outcomes through their effects on parenting practices, parent self-regulation, parent-child interaction patterns, and/or the modeling of anxious and depressive styles (Tronick & Beeghly, 2011).
Symptoms of anxiety and depression are thought to have a biological basis in dysregulated physiology, including in the functioning of the parasympathetic nervous system on the heart, typically measured using respiratory sinus arrythmia (RSA; Berntson, Cacioppo, & Quigley, 1993). Beginning early in development, RSA contributes to the physiological regulation of arousal and stress (Porges, 2007), which in turn provides support for emotion regulation (ER) skills (i.e., the ability to monitor, evaluate, and modify emotional responses in accordance with one’s goals; Thompson, 1994). Conversely, when RSA is dysregulated, it is thought to reflect poorer ER skills, which in turn underlie mental health symptoms (Beauchaine, 2015).
Dysregulated RSA is well documented as a biomarker of both anxiety and depressive symptoms in clinical studies of adults (Gouin, Deschenes, & Dugas, 2014). However, relatively little research has focused on how RSA relates to subclinical levels of symptoms in community samples, posing a significant gap in our understanding of whether and how RSA functions as a biomarker of psychopathology risk at lower symptom levels. In addition, understanding whether the physiological correlates of anxiety and depressive symptoms are unique versus shared could inform our precision in diagnosing and treating underlying mental health issues before they reach clinical levels. Further, understanding parent RSA-symptom relations in the context of parent-child interactions may help inform how risk for psychopathology is transmitted from parent to child. Accordingly, we examined person-centered profiles of resting RSA, RSA reactivity, and anxiety and depressive symptoms in a community sample of parents and whether these profiles predicted child outcomes commonly associated with parental symptoms, namely emotional and behavioral dysregulation, to understand their role in children’s developmental psychopathology.
Respiratory Sinus Arrhythmia
RSA is a measure of cardiac vagal activity, reflecting engagement of the parasympathetic nervous system on the heart (Berntson et al., 1993). At rest, RSA is typically higher, which acts as a “brake” that slows heart rate during times of rest (Porges, 1991). When an individual experiences stress or challenge, the “brake” is withdrawn (i.e., RSA decreases), allowing the fight-or-flight response to engage and heart rate to speed up to respond to environmental demands (Porges, 1991). Thus, in better-regulated individuals, it is typically expected that RSA is higher during rest and lower during instances of stress or challenge.
The withdrawal of RSA may be one of the fastest and most flexible physiological markers of stress, reflecting quick adaptation to varying demands in social environments (Porges, 2007). Theories regarding the importance of RSA (e.g., Polyvagal Theory, Porges, 2007; Neurovisceral Integration Model, Thayer & Lane, 2000) have placed it at the heart of processes of emotional expression, social engagement, and self-regulation. RSA is considered part of a greater neurovisceral network enabling the spontaneous expressions of emotion that are universally recognized in humans (Porges, 2007). Connections with the prefrontal cortex have also been proposed, suggesting that RSA may serve as a periphery measure of executive self-regulatory processes (Holzman & Bridgett, 2017; Thayer & Lane, 2000).
Accordingly, RSA is relevant to everyday interactions in which social engagement and effort are required, including parents’ interactions with their children. Parental emotion and self-regulation during challenging interactions with young children, who need support and structure during goal-oriented tasks, correspond with RSA change on the order of seconds wherein greater parenting effort is associated with parent RSA withdrawal (Lunkenheimer, Busuito, Brown, Panlilio, & Skowron, 2019; Shih, Quiñones-Camacho, Karan, & Davis, 2019). In laboratory studies, parents show RSA withdrawal when moving from baseline tasks to more effortful tasks (Bornstein & Suess, 2000); parents also show lower RSA concordance with children when that effort is absent, i.e., when they are disengaged (Skoranski, Lunkenheimer, & Lucas-Thompson, 2017). Given that parent-child interactions serve as critical socialization contexts for child development, they are important contexts for the examination of parents’ RSA reactivity.
The roles of RSA in social engagement, self-regulation, and inhibition of the fight-or-flight response make it a candidate biomarker for psychopathology, as mental health symptoms often reflect deficiencies in these areas (Beauchaine, 2015; Porges, 2007). For example, the inability to inhibit sympathetic arousal during times of safety (i.e., when the context does not call for such responses) is a key feature of anxiety disorders (Porges, 2007). Depressive disorders also include behavioral symptoms that align with how dysregulated RSA manifests in the context of social interactions, such as unresponsive social behavior and less shared gaze (Rottenberg, Clift, Boden, & Salomon, 2007). Thus, a better understanding of how RSA and symptomology covary is needed to delineate the utility of RSA in research on psychopathology risk.
Distinguishing Biomarkers of Anxiety and Depressive Symptoms
Accounts differ as to whether dysregulated RSA represents a general biomarker for all psychopathology or differs in relation to anxiety versus depressive symptoms (Beauchaine & Thayer, 2015). According to the Tripartite Model (Clark & Watson, 1991), anxiety and depression share a general distress factor that accounts for their overlap in symptoms and comorbid diagnoses. However, each disorder also has unique characteristics: in particular, depression is uniquely characterized by low positive affect (i.e., anhedonia), whereas anxiety is characterized by heightened autonomic arousal. The Tripartite Model has been supported by factor analytic studies (Anderson & Hope, 2008; Watson et al., 1995), suggesting support for both shared and unique characteristics across these syndromes, at least at the behavioral level.
In applying the Tripartite Model to the role of RSA in anxiety and depressive symptoms, one possibility is that dysregulated resting RSA reflects a general distress factor that is observed in both depressive and anxious individuals. Supporting this idea, resting RSA tends to be lower in individuals who display greater symptoms of either depression or anxiety (Beauchaine & Thayer, 2015; Rottenberg et al., 2007; Watkins, Grossman, Krishnan, & Sherwood, 1998). On the other hand, differentiation in RSA functioning between anxious and depressed individuals has also been demonstrated, particularly in terms of RSA reactivity. For example, depressive symptoms (e.g., rumination) are associated with no change or RSA augmentation in response to challenge (Rottenberg et al., 2007), considered a “hyporeactive” response, whereas anxiety symptoms (e.g., worry) are related to “excessive” RSA withdrawal (i.e., extreme relative to the situation; Gouin et al., 2014; Kircanski, Waugh, Camacho, & Gotlib, 2016), considered a “hyperreactive” response. Thus, whereas resting RSA may be similarly affected by symptoms of anxiety or depression, dysregulated RSA reactivity may be distinct by symptom type.
However, findings do not always support the Tripartite Model (Licht, de Geus, van Dyck, & Pennix, 2009). For example, some researchers have observed excessive RSA withdrawal to a stressful interview among patients with both anxiety and depression (Hu, Lamers, de Geus, & Pennix, 2016), suggesting comorbidity may relate to RSA reactivity. Others have found that depressed individuals who showed higher, not lower, resting RSA reported greater sadness and less recovery from a depressive episode (Rottenberg, Wilhelm, Gross, & Gotlib, 2002), suggesting that higher resting RSA may also be a risk factor. Inconsistencies in findings across studies may stem from differences in stressors used to elicit RSA reactivity (e.g., psychosocial stressors, worry induction, or cognitive challenge), or from differences in patient samples (e.g., individuals with GAD versus comorbid anxiety and depressive disorders). Thus, while this model offers strong theoretical guidance on RSA-symptom relations, more empirical evidence is needed.
Parent Physiology and Symptom Profiles in Community Populations
It is not yet clear whether the ways in which RSA and symptoms cluster in clinical populations are applicable to community populations with lower symptoms. A better understanding of RSA-symptom relations in community populations could inform the degree to which RSA acts as a biomarker of risk at lower levels of symptomology. Additionally, how symptoms interact with parental RSA in the context of typical parent-child interactions may inform the everyday mechanisms by which psychopathology risk is transmitted to children. Existing work shows mothers with greater depressive symptoms display lower average RSA during unstructured free play tasks with children (Lunkenheimer et al., 2018), and that higher average maternal RSA is a buffer from the effects of mothers’ depressive symptoms on adaptive parent-child interaction processes (Connell, Hughes-Scalise, Klostermann, & Azem, 2011). These findings are informative but more work is needed. Accordingly, we examined resting RSA and RSA reactivity during challenging parent-child interactions in a community sample of parents and whether they aligned with anxiety and depressive symptoms in ways previously demonstrated in the literature.
To explore these relations, latent profile analysis was employed to examine the clustering of parasympathetic physiology and anxiety and depressive symptoms in parents. Person-centered approaches have been used previously to examine multiple predictors within person as a cluster rather than as separate predictors (Hernandez, Smith, Day, Neal, & Dunsmore, 2018), including the conjoint assessment of physiological and emotional factors (Turpyn, Chaplin, Cook, & Martelli, 2015). However, no known studies have utilized such an approach to examine how parasympathetic physiology and mental health symptoms covary in parents of young children.
One potential pitfall of person-centered approaches is that because they are data-driven, they may capture clusters within a sample but may not always generalize to other samples. Thus, they can be supplemented with tests of validity that allow greater confidence that profiles relate in expected ways to other variables. We were interested in parents due to the potential for their symptoms to have direct or indirect negative effects on child outcomes. Thus, to help validate parent physiology and symptom profiles, we examined their relation to child outcomes known to be associated with parents’ anxiety and depressive symptoms, specifically internalizing problems, externalizing problems, and emotion regulation and dysregulation.
Parent Symptoms and Child Adjustment
When parents experience symptoms of depression or anxiety, children are at greater risk for developing mental health problems themselves (Joormann, Eugene, & Gotlib, 2008), showing greater internalizing (e.g., withdrawal, shyness) and externalizing (e.g., hyperactivity, aggression) problems in early childhood (Goodman et al., 2011). Parental depressive symptoms are linked to lower attention towards children and greater withdrawal from interactions, but also inconsistent parenting, as depressed parents may oscillate between more withdrawn and intrusive behaviors (Connell et al., 2011; Joormann et al., 2008). Parental anxiety symptoms are linked to more hypervigilant attention and intrusion (Root, Hastings, & Rubin, 2016). These parenting behaviors have been shown to thwart children’s developing ER abilities (Zahn-Waxler, Iannotti, Cummings, & Denham, 1990). Parents with greater depressive or anxiety symptoms may also have difficulty regulating their own emotions, presenting poor models of ER for children, which in turn could lead to emotion dysregulation in children (Han, Lei, Qian, Li, & Wang, 2016; Kerns, Pincus, McLaughlin, & Comer, 2017). Thus, we were interested in whether parent profiles of RSA and symptoms predicted child emotional and behavioral dysregulation.
Current Study
The current study aimed to fill several gaps in the extant literature. First, we sought to examine how resting RSA, RSA reactivity, and symptoms of anxiety and depression clustered within individuals in a community sample of parents of young children using a person-centered approach, in order to improve our understanding of whether and how RSA functions as a biomarker of mental health in non-clinical populations. Although the nature of model fitting in person-centered analysis is inherently exploratory, we had some expectations about the number and type of profiles that could emerge, which are described below. We expected overall symptom levels to be in the none to moderate range on average given that it was a community sample. One possibility was that three profiles would emerge along the lines of no, mild, and moderate risk based on a single general distress factor underlying anxiety and depressive symptoms (Beauchaine & Thayer, 2015). In this case, we might expect to observe: a) a “typical” profile with no or very low symptoms, higher resting RSA, and RSA withdrawal to challenge; b) a mild risk profile with low symptoms and modest differences in resting RSA and RSA reactivity compared to the typical profile; and c) a moderate risk profile with higher symptom levels and dysregulated RSA patterns shown in prior research (e.g., low resting RSA, RSA augmentation to challenge, or excessive RSA withdrawal; Kircanski et al., 2016; Rottenberg et al., 2007).
Another possibility was that we would observe four profiles in line with the notion that when individuals are at higher risk for psychopathology, RSA patterns associated with anxiety and depressive symptoms are distinct (Greaves-Lord et al., 2007). In this case, we could observe: a) a “typical” profile as noted above; b) a mild risk profile as noted above; c) a moderate risk profile with heightened anxiety symptoms, lower resting RSA, and heightened RSA reactivity (RSA withdrawal) relative to other profiles; and d) a moderate risk profile with heightened depressive symptoms, lower resting RSA, and blunted RSA reactivity (RSA augmentation) relative to other profiles. These varying hypotheses were explored by comparing LPA model solutions using established fit indices.
Second, assuming parent profiles were found, we sought to test the utility of such parental biobehavioral profiles for understanding the potential developmental transmission of mental health risk. Thus, we examined whether parent profiles predicted differences in children’s internalizing problems, externalizing problems, and emotion regulation and dysregulation one year later to evaluate their effects on child adjustment. Although the profile solution was yet unknown, we predicted that if we did indeed find either a 3- or 4-profile solution as outlined above, the parent profiles with mild or moderate risk would be associated with greater deficit in socioemotional competence among young children one year later compared to those with no risk (“typical”). Finally, we sought to test whether mental health profile solutions differed by parent gender (in this sample, all couples were heterosexual and likely most were cisgender; gender identity information was unavailable). Mother and father models were analyzed separately in consideration of the novelty of the research questions and the novelty of examining RSA and symptoms in fathers; given this novelty, we were interested in exploring whether there were differences in profiles or their relations to child adjustment by parent. Some research indicates that men and women experience the physiological aspects of mental health in different ways (e.g., men experience fewer somatic symptoms of anxiety, Dekker et al., 2008), which may lead to different clustering of profiles in mothers and fathers.
Method
Participants
Families (N = 126, 53% boys) were recruited to participate in a longitudinal study of parent-child biobehavioral dynamics and familial risk. All mothers and 87 fathers agreed to participate. To capture familial risk, families were oversampled for low income (200% or less of the federal poverty level), risk for child maltreatment based on potential Child Protective Services (CPS) involvement, or higher life stress based on the Social Readjustment Rating Scale (e.g., job loss, divorce; Holmes & Rahe, 1967). Families were recruited via flyers and word-of-mouth at preschools, community events, service agencies, and CPS. Exclusion criteria were the inability to read and write in English, child diagnosis of developmental disabilities, or if parents or children had a cardiac condition that interfered with cardiac data collection or interpretation.
Mothers’ race/ethnicity was reported as 75% White, 14% Latina, 3% Multiethnic, 2% Black, 2% Native American, 1% Asian, and 3% “other” or unknown. Fathers were 29% White, 53% Latino, 8% Multiethnic, 2% Black, 2% Native American, 1% Asian, and 4% “other” or unknown. Children were 64% White, 22% Latinx, 7% Multiethnic, 3% Black, 1% Native American, and 3% “other” or unknown. Parents were married (66.7%), 12.7% living together (12.7%), single (11.3%), or separated or divorced (8.7%). Annual household income ranged from < $5,000 to >$90,000, with a median range of $30,000 to $39,000. Average parental educational level was some college for both mothers and fathers. Retention was 83% for mothers and 78% for fathers across assessments. There were no significant differences in primary study variables or sociodemographic variables between families with and without participating fathers, with the exception of income being higher in father-participating families (t = −5.27, p < .001).
Procedure
Families participated at child ages 2 ½ (Time 1), 3 (Time 2; M = 3.04, SD = 0.11), and 4 (Time 3; M = 4.00, SD = 0.12 years) years; only the latter two waves involved physiological data and were involved in the present analysis. Two-hour laboratory sessions at Time 2 began with electrode and respiratory belt application and a resting baseline in which parents and children watched a 3-min video of dolphins in the ocean. Next, parents and children participated in three dyadic tasks: Free Play (7 minutes), Clean-up (4 minutes), and the Parent-Child Challenge Task (10 minutes), described below. Children also participated in individual tasks and parents filled out surveys about mental health, parenting, and child behavior. Mother-child and father-child sessions were scheduled on different days. Toys and puzzles for dyadic tasks were counterbalanced across parents so that children encountered novel stimuli each time. Families earned $135 when one parent participated and $210 when two parents participated.
Parent-Child Challenge Task (PCCT).
RSA data was collected during the PCCT (Lunkenheimer, Kemp, Lucas-Thompson, Cole, & Albrecht, 2016), a dyadic task designed to be both collaborative and challenging. Parents and 3-year-olds were asked to complete three puzzles above the child’s ability level that increased in difficulty in order to win a prize; parents were asked to use only their words and not physically assist their children. The task consisted of three phases. Baseline was the first 4 minutes of assembly, after which the experimenter entered to say dyads had only two minutes left to finish, initiating the Challenge condition (3 minutes). Then, the experimenter re-entered the room and gave the prize regardless of completion status, asking parents and children to play with the prize (art materials) as the Recovery condition (3 minutes).
Measures
RSA.
Respiration and electrocardiograph (ECG) data were transmitted to a computer through wireless devices worn in backpacks. Interbeat interval data was processed and cleaned offline by graduate research assistants using Mindware Heart Rate Variability 3.0 software. RSA was calculated for each 30s segment as the natural logarithm of the variance of heart period within the frequency related to respiration (0.24–1.04 Hz for children and 0.12–0.40 Hz for adults; Fracasso, Porges, Lamb & Rosenberg, 1994). Segments with 10% or greater noise or artifact were excluded from analysis. Parent resting RSA was measured as mean RSA across the 3-min resting period that preceded the dyadic interaction tasks. Parent RSA reactivity was calculated as the difference score between the mean RSA during the 4-minute baseline period of the PCCT and the mean RSA during the 3-min challenge period of the PCCT, with negative values reflecting RSA withdrawal and positive values reflecting RSA augmentation.
Anxiety and depressive symptoms.
Parents completed the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983) at Time 2, involving 53 items, 9 psychopathology constructs, and a general distress measure. Respondents indicate on a scale of 0 – 4 how much they experience each symptom, with 0 = not at all and 4 = extremely. The depressive subscale (6 items) reflects dysphoric mood, lack of interest in activities, and feelings of hopelessness. The anxiety subscale (6 items) reflects symptoms of restlessness, nervousness, tension, and feelings of panic. We found each subscale was internally consistent among our sample (depressive α = 0.85; anxiety α = 0.81) and each has been found to be reliable across time in prior investigations (depressive r = 0.84; anxiety r = 0.79; Derogatis & Melisaratos, 1983). The anxiety and depressive subscales of the BSI have been shown to emerge as distinct factors in prior analyses of construct validity (e.g., Hayes, 1997, Urbán et al., 2014), and provide similar insight as more in-depth self-report measures of depression and anxiety (e.g., Morlan & Tan, 1998).
Symptoms were positively skewed for mothers (anxiety skew = 1.06, SE = 0.22; depressive skew = 2.35, SE = 0.22) and fathers (anxiety skew = 2.11, SE = 0.27; depressive skew = 2.41, SE = 0.27). Given skew and our expectation that symptoms would fall into roughly three levels, symptoms were categorized into three levels that reflected the number and severity of symptoms endorsed on the 6-item depressive and anxiety subscales: no symptoms (0 symptoms endorsed), mild symptoms (less than 75th percentile of sample), and moderate symptoms (75th percentile of sample or greater). The upper 75th percentile was used as the cut-off to indicate elevated risk based on similar methods used in measures of cumulative risk (e.g., MacKenzie, Kotch, & Lee, 2011). Using this criterion, the sample was fairly evenly divided into three levels for mothers (anxiety: 36% no, 32% mild, and 32% moderate risk; depressive: 46% no, 28% mild, and 26% moderate risk) and fathers (anxiety: 46% no, 32% mild, and 22% moderate risk; depressive: 55% no, 21% mild, and 24% moderate risk). Endorsed symptom means for mothers were 1.26 (mild) and 4.18 (moderate) for anxiety and were 1.56 (mild) and 5.32 (moderate) for depressive symptoms. Symptom means for fathers were 1.46 (mild) and 5.17 (moderate) for anxiety and were 1.35 (mild) and 5.65 (moderate) for depressive symptoms. Scores for anxiety and depressive symptoms for both mothers and fathers in the “moderate risk” group were elevated relative to norms delineated for non-clinical community samples (Derogatis, 1992) as well as relative to prior studies conducted with parents of young children (e.g., Tzoumakis, Lussier, & Corrado, 2014), however, they were lower than those of clinical outpatient groups (Derogatis, 1992).
Child internalizing and externalizing.
Mothers reported internalizing and externalizing problems on the Child Behavior Checklist (Achenbach & Rescorla, 2001) at Time 3 (4 years old). Mothers responded to 100 items about their children’s behavior on a three-point scale, where 0 = not true of my child, 1 = somewhat or sometimes true, 2 = very true. Internalizing subscale items reflected anxiety, depression, and withdrawal (e.g., ‘Too fearful or anxious,’ ‘Unhappy, sad, or depressed’). Externalizing subscale items reflected attention problems, hyperactivity, and aggressive behavior (e.g., ‘Temper tantrums or hot temper,’ ‘Can’t sit still, restless, or hyperactive). Cronbach’s alpha was 0.89 for internalizing and 0.92 for externalizing.
Child emotion regulation.
Also at Time 3, mothers completed the Emotion Regulation Checklist (ERC; Shields & Cicchetti, 1997), a 24-item checklist that includes two subscales: emotion regulation (i.e., the ability to modulate emotion to facilitate engagement with the environment) and emotional negativity//lability (i.e., lability of emotions and dysregulated negative emotions). Parents rated children on each item using a 4-point scale where 1 = never, 2 = sometimes, 3 = often, and 4 = almost always. Sample items include, “Can recover from stress” (emotion regulation scale), and “Is prone to angry outbursts” (negativity/lability scale). Cronbach’s alpha was 0.81 for emotional negativity/lability and 0.73 for emotion regulation.
Data Analytic Plan
Person-centered profiles of parent physiology and symptoms were examined using latent profile analysis (LPA; Lazarsfeld & Henry, 1968) using data from Time 2 assessments. LPA allows individuals to be divided into subgroups based on an unobservable construct based on patterns of responses on measured variables. The optimal number of profiles was determined by examining model fit indices of multi-solution models fit in MPlus 8 (Muthen & Muthen, 1998–2017) with the goal of obtaining the most parsimonious solution that explained the greatest amount of individual variability. To evaluate the best fitting model, the Akaike information criterion (AIC), Bayesian information criterion (BIC), sample size adjusted BIC (SSBIC), chi-square value (G2), and the Bootstrapped Log-Ratio Test (BLRT; Tein, Coxe, & Cham, 2013) were used. A model was selected once the AIC, BIC, and G2 reached their smallest levels and began to increase with the addition of more profiles, and once the BLRT became non-significant, indicating that the addition of another profile was not necessary. Four variables were included in profiles: resting RSA, RSA reactivity, anxiety symptoms, and depressive symptoms. Full information maximum likelihood estimation was used to address missing data.
Resting RSA and RSA reactivity were continuous variables whereas parents’ anxiety and depressive symptoms were categorical, making this a mixed indicator LPA model. Values for resting RSA and RSA reactivity were standardized before entering into latent class models so that class means could be compared statistically to the sample mean of 0 for interpretation purposes. Symptom variables were interpreted based on item-response probabilities, which provide information on the likelihood of a response on a categorical indicator given membership in a particular class. Since symptom variables had three levels, observed probabilities were interpreted by comparing against the “chance” probability of 0.33. As an example, for individuals who belong to a hypothetical moderate risk profile, we might expect the class-specific mean of resting RSA to be lower than the sample mean (i.e., negative), paired with higher probabilities of reporting moderate levels of anxiety and/or depressive symptoms.
Next, sociodemographic covariates were explored in relation to profiles. Child age, sex, ethnicity, maternal education, and paternal education were not related to class membership and thus were not considered further. Family income was higher in mothers’ Typical profile than the Mild Risk profile, χ2 = 6.016, p < .05. No other income differences among groups were found for mothers, and no differences by income were found for fathers. Because this was not a robust nor comparable factor across mothers and fathers, it was not included as a covariate.
Next, LPA class membership at Time 2 was used to predict children’s internalizing, externalizing, emotion regulation, and emotional negativity/lability at Time 3 (one year later) using the BCH method (Bakk & Vermunt, 2016). BCH is an alternative to the traditional classify-analyze approach where posterior probabilities are used to assign individuals to a class and class membership is then treated as a known variable in other models. This traditional approach flattens the variability associated with posterior probabilities across individuals, attenuating effects and increasing the chance of type II errors. Conversely, BCH applies weights to class membership values, which helps to account for individual differences in posterior probabilities within a given class (Bakk & Vermunt, 2016).
Results
Preliminary Analyses
See Table 1 for descriptive data. Bivariate correlations indicated mothers’ greater RSA reactivity (i.e., more withdrawal) was related to higher anxiety symptoms. Mothers’ and fathers’ resting RSA were positively intercorrelated. Mothers’ depressive symptoms were positively related to child internalizing, externalizing, and emotional negativity/lability, and mothers’ greater RSA reactivity (i.e., more withdrawal) was related to higher child emotion regulation at age 4. Fathers’ anxiety symptoms were negatively related to child emotion regulation, and fathers’ lesser RSA reactivity (i.e., more augmentation) was related to higher child externalizing problems at age 4. Little’s MCAR test showed data was missing completely at random for all primary study variables. We did not find any significant differences between families who did and did not complete the Time 3 assessment in sociodemographic variables (mothers’, fathers’, and children’s race or ethnicity, mothers’ or fathers’ education level, or family income) or key study variables (mother’s and fathers’ resting RSA, anxiety symptoms, or depressive symptoms). Models were run using full information maximum likelihood (FIML) estimation in Mplus, which accounts for missingness in the data without dropping full cases. The valid N was 126 for the mother LPA models and 87 for the father LPA models (Table 1).
Table 1.
Means, standard deviations, and bivariate correlations among key study variables
| Mean | Min | Max | N | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother Anxiety Symptoms | 1.74 | 0 | 7.98 | 121 | -- | ||||||||||
| 2. Father Anxiety Symptoms | 1.60 | 0 | 10.08 | 82 | .16 | -- | |||||||||
| 3. Mother Depressive Symptoms | 1.80 | 0 | 16.02 | 121 | .54** | .09 | -- | ||||||||
| 4. Father Depressive Symptoms | 1.65 | 0 | 12 | 82 | .30** | .81** | .31** | -- | |||||||
| 5. Mother Resting RSA | 6.10 | 1.91 | 9.75 | 103 | −.02 | .21^ | −.04 | .12 | -- | ||||||
| 6. Father Resting RSA | 6.13 | 1.68 | 9.29 | 76 | .15 | .04 | .08 | −.11 | .26* | -- | |||||
| 7. Mother RSA Reactivity | −1.30 | −2.14 | 1.57 | 105 | −.27** | −.12 | −.04 | −.17 | .04 | .07 | -- | ||||
| 8. Father RSA Reactivity | 0.02 | −0.95 | 1.76 | 76 | .00 | .16 | −.05 | .26* | .02 | −.17 | −.00 | -- | |||
| 9. Child Internalizing | 7.12 | 0 | 32 | 118 | .05 | .05 | .19** | .11 | .04 | −.17 | −.07 | .05 | -- | ||
| 10. Child Externalizing | 11.81 | 0 | 36 | 118 | .14 | .07 | .29** | .20 | .03 | −.12 | −.16 | .24* | .66** | -- | |
| 11. Child Negativity/Lability | 26.56 | 17 | 43 | 117 | .07 | −.04 | .25* | .07 | .03 | −.16 | −.09 | .16 | .57** | .78** | -- |
| 12. Child Emotion Regulation | 27.44 | 16 | 32 | 117 | −.07 | −.12 | −.06 | −.11 | .05 | −.05 | .05 | −.23^ | −.40** | −.34** | −.32** |
Note: Significant or trending correlations are noted in bold text.
p < .10,
p < .05,
p < .01
Primary Analyses
LPA model selection.
LPAs with two to five classes were run and fit indices were compared to determine the optimal number of classes. For mothers, a 4-class solution was chosen (Table 2). The BIC and G2 decreased between the 2- and 3-class models and between the 3- and 4-class models but increased between the 4- and 5-class models. Thus, indices were lowest for the 4-class model indicating best model fit. Also, the BLRT was significant for the 2- and 3-class models but was not for the 4-class model, indicating the addition of a fifth class was not necessary. The AIC and SSBIC continued to decrease indefinitely, which may be expected when continuous indicators are used (Collins & Lanza, 2010).
Table 2.
Model fit statistics for mother and father LPA models
| Classes | AIC | BIC | SSBIC | BLRT | G2 |
|---|---|---|---|---|---|
| Mothers | |||||
| 2 | 1107.50 | 1150.04 | 1102.61 | 0 | 8.33 |
| 3 | 1103.26 | 1165.66 | 1096.08 | 0 | 2.85 |
| 4 | 1101.35 | 1183.60 | 1091.89 | 0.2 | 0.40 |
| 5 | 1098.38 | 1200.48 | 1086.64 | 0.1 | 0.43 |
| Fathers | |||||
| 2 | 748.871 | 785.860 | 738.350 | 0 | 0.908 |
| 3 | 749.736 | 803.986 | 734.569 | 0.2 | 0.110 |
| 4 | 755.595 | 827.106 | 735.602 | 0.667 | 0.015 |
| 5 | 757.824 | 846.597 | 733.005 | 0.0 | 0.157 |
Note: Statistics used to inform model selection are noted in bold text.
For fathers, a 3-class solution was chosen (Table 2), but indices were less cut-and-dried. The BLRT was significant for the 2-class but not the 3-class model, indicating a fourth class may not be necessary. But the AIC, BIC, and SSBIC continued to increase indefinitely, which may indicate that model fit did not improve from 2 to 3 classes or with the continued addition of classes. Also, the G2 continued to increase between the 2- and 4-class solutions but decreased between 4- and 5-class solutions, indicating model fit improved between 4- and 5-class models. Accordingly, a 3-class model was chosen for fathers for a few reasons. First, the 5-class model included two classes that only consisted of 2 individuals each. Second, prior work suggests when continuous indicators are used, there are limitations to the interpretability of the AIC, BIC, SSBIC, and G2 (Lanza & Collins, 2010), but BLRT is more robust to these limitations. Finally, the 3-class solution aligned with one of the two hypothesized profile solutions based on prior research, which can inform model selection (Bray, Foti, Thompson, & Wills, 2014).
Mother LPA profiles.
Means and item-response probabilities are shown in Table 3. The first profile, labeled Typical, encompassed the majority of the sample (79 mothers, 62.7%) and were characterized by resting RSA and RSA reactivity close to the standardized sample mean of zero and no depressive or anxiety symptoms. The second class, labeled Mild Risk (12 mothers, 9.5%), had resting RSA approximately 1½ SD higher than the sample mean, RSA reactivity about equal to the sample mean, and mild levels of depressive and anxiety symptoms (versus no or moderate symptoms). The third class, Moderate Risk/Withdrawal (16 mothers, 12.7%), had resting RSA about equal to the sample mean and RSA reactivity roughly 1½ SD below the sample mean, indicating RSA withdrawal to challenge that was more pronounced than the other three classes. These mothers showed higher probabilities of moderate levels of anxiety (0.91) and depressive (0.68) symptoms versus mild or no symptoms, where the probability of anxiety symptoms was higher/predominant. Finally, the fourth class, Moderate Risk/Augmentation (19 mothers, 15.1%), had average resting RSA and RSA reactivity roughly ¾ SD above the sample mean, suggesting augmentation of RSA to challenge on average. This profile also had higher probabilities of moderate levels of anxiety and depressive symptoms versus mild or no symptoms, but in this case the depressive symptoms were higher/predominant. Thus, whereas both classes exhibited moderate risk, heightened anxiety symptoms were more characteristic of the Withdrawal profile, and heightened depressive symptoms were more characteristic of the Augmentation profile.
Table 3.
Item-response probabilities for latent profile analyses of physiology and symptoms in mothers and fathers
| Mother Profiles | Father Profiles | ||||||
|---|---|---|---|---|---|---|---|
| “Typical” (62.7%) |
“Mild Risk” (9.5%) |
“Moderate Risk/ Withdrawal” (12.7%) |
“Moderate Risk/ Augmentation” (15.1%) |
“Typical” (47.1%) |
“Mild Risk” (36.8%) |
“Moderate Risk” (16.1%) |
|
| Depressive Symptoms | |||||||
| No symptoms | 0.74 | 0 | 0 | 0 | 0.79 | 0.47 | 0.00 |
| Lower severity | 0.23 | 0.84 | 0.32 | 0.20 | 0.21 | 0.29 | 0.03 |
| Higher severity | 0.04 | 0.16 | 0.68 | 0.80 | 0.00 | 0.24 | 0.97 |
| Anxiety Symptoms | |||||||
| No symptoms | 0.59 | 0 | 0.09 | 0 | 0.97 | 0.00 | 0.00 |
| Lower severity | 0.29 | 1.00 | 0 | 0.33 | 0.03 | 0.84 | 0.00 |
| Higher severity | 0.15 | 0 | 0.91 | 0.67 | 0.00 | 0.16 | 1.00 |
| Resting RSA | |||||||
| Class Mean | −0.10 | 1.56 | −0.16 | −0.24 | −0.26 | 0.45 | −0.27 |
| RSA Reactivity | |||||||
| Class Mean | 0.13 | −0.20 | −1.37 | 0.73 | −0.04 | −0.22 | 0.74 |
Note: Significant item response probabilities are noted in bold text.
Mothers’ profile membership and child outcomes.
Figure 1a displays means of child internalizing, externalizing, emotional negativity/lability, and emotion regulation at age 4 as a function of mothers’ profile membership one year prior. Mothers’ profile membership significantly predicted child internalizing (Overall G2=14.50, p=.002), externalizing (Overall G =12.68, p=.005), and negativity/lability (Overall G2=8.15, p=.04). Across all outcomes, children of mothers in the three risk classes at age 3 had higher levels of emotional and behavioral dysregulation at age 4 than children of mothers in the Typical class. For internalizing, these differences were between the Typical class and the Mild Risk (G2=8.31, p=.004), Moderate Risk/Withdrawal (G2=4.42, p=.04), and Moderate Risk/Augmentation classes (G2=6.91, p=.009). For externalizing, differences were observed between the Typical class and the Mild Risk (G2=6.98, p=.008) and Moderate Risk/Augmentation classes (G2=5.84, p=.02), but not the Moderate Risk/Withdrawal class (G2=1.67, p=.20). For emotional negativity/lability, only the difference between the Typical and Mild Risk classes was significant (G2=6.52, p=.01). No significant differences were found for child emotion regulation (Overall G2=0.44, p=.80). In addition, no significant differences in outcomes were observed among the three risk classes.
Figure 1.
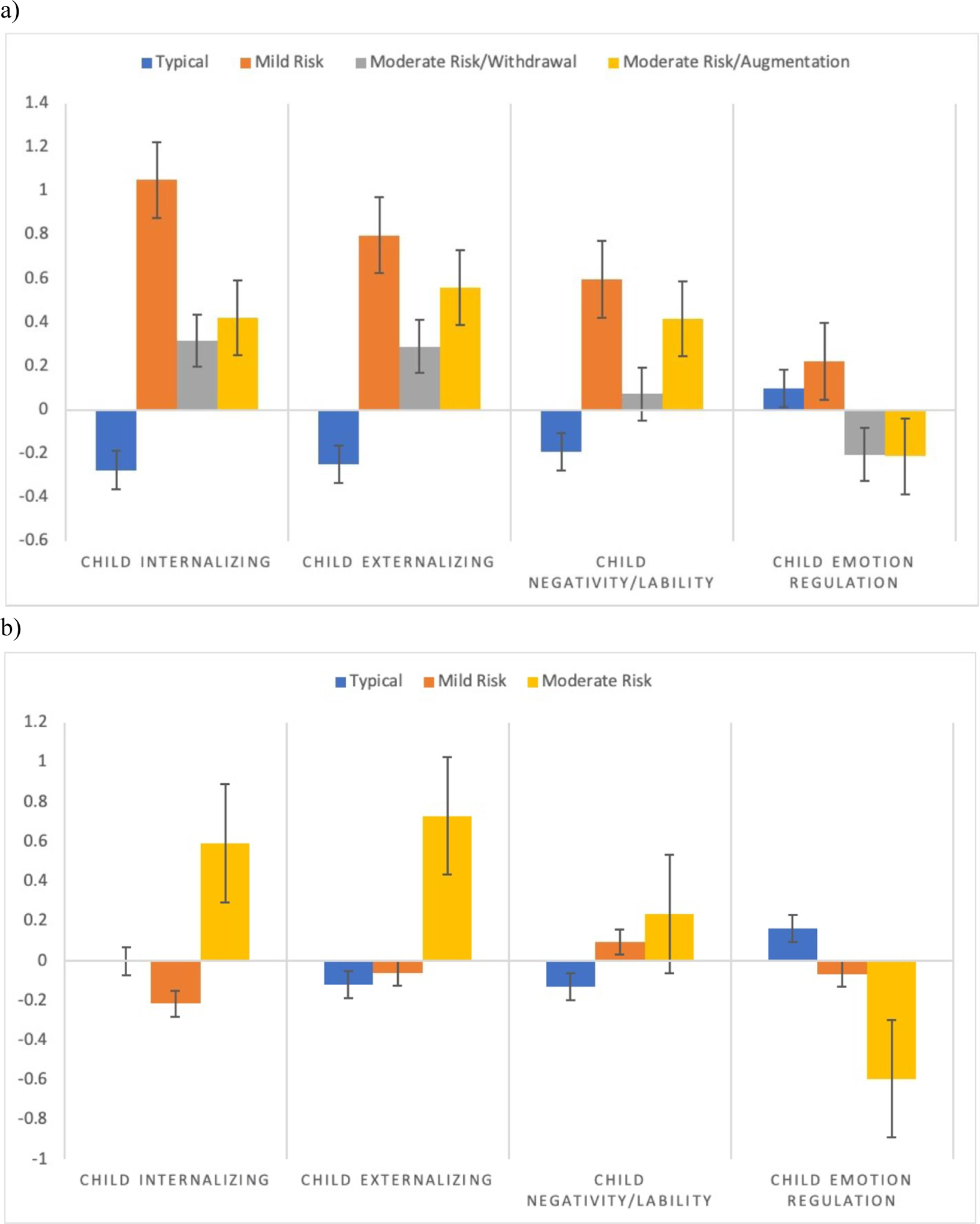
Children’s internalizing, externalizing, negativity/lability, and emotion regulation at age 4 as a function of (a) mothers’ profile membership and (b) fathers’ profile membership one year prior.
Father LPA profiles.
Means and item-response probabilities for fathers are in Table 3. The Typical profile (41 fathers, 47.1%) showed RSA reactivity close to the sample mean, slightly lower-than-average resting RSA (roughly ¼ SD below the sample mean), and no anxiety or depressive symptoms. The second class, labeled Mild Risk (32 fathers, 36.8%), displayed higher resting RSA, roughly ½ SD above the sample mean, and RSA reactivity roughly ¼ SD below the sample mean, indicating some RSA withdrawal to challenge on average. This profile had no difference in probabilities of depressive symptoms compared to the sample mean, but a higher likelihood of mild levels of anxiety symptoms (versus no or moderate symptoms). Finally, the third profile was labeled Moderate Risk (14 fathers, 16.1%) and had RSA reactivity ¾ SD above the mean, indicating RSA augmentation to challenge on average. Resting RSA was roughly ¼ SD below the sample mean but did not differ significantly from the Typical class. This profile also had a higher probability of higher symptoms of both depression and anxiety versus mild or no symptoms.
Fathers’ profile membership and child outcomes.
Figure 1b displays the means of child internalizing, externalizing, negativity/lability, and emotion regulation at age 4 as a function of fathers’ profile membership one year prior. None of the overall models reached significance, however, the overall model for externalizing was trending significant (Overall G2=5.80, p=.055) and there were significant and marginal effects at the parameter level. Trends across all outcomes were such that children of fathers in the Moderate Risk class had higher emotional and behavioral dysregulation compared to children of fathers in the Typical or Mild Risk classes. Specifically, there was marginally higher internalizing in the Moderate Risk than the Mild Risk class (G2=3.82, p=.051); significantly higher externalizing in the Moderate Risk than the Typical class (G2=5.74, p=.02) and marginally higher externalizing in the Moderate Risk than the Mild Risk class (G2=3.62, p=.057); and marginally lower emotion regulation in the Moderate Risk class versus the Typical class (G2=3.59, p=.058). No differences between fathers’ classes were observed for children’s emotional negativity/lability.
Discussion
This study is the first to our knowledge to examine how parasympathetic physiology and anxiety and depressive symptoms cluster within parents of young children using a person-centered approach, and whether they cluster in ways that support theoretical models about how dysregulated RSA acts as a biomarker of psychopathology risk. Our findings suggest there may be distinct risk profiles of parents that differ from a more “typical” profile by nature of their elevated anxiety and/or depression symptoms as well as differences in resting levels of RSA and/or RSA reactivity. The profiles discovered generally supported the theoretical assumptions of the Tripartite Model (Clark & Watson, 1991) in that both shared and distinct physiological features were present across symptom types.
However, a few particularly notable findings emerged. First, lower resting RSA did not characterize the risk profiles as hypothesized. Rather, higher resting RSA was characteristic of both mothers and fathers at mild risk for psychopathology in a community sample. Second, only mothers showed distinct RSA reactivity patterns by predominant symptom type at moderate risk levels in ways expected based on prior research (Rottenberg et al., 2007; Kircanski et al., 2016). Specifically, mothers characterized by excessive RSA withdrawal had the greatest likelihood of elevated anxiety symptoms, while mothers characterized by RSA augmentation had the greatest likelihood of elevated depressive symptoms. Third, fathers at moderate risk had a higher probability of both anxious and depressive symptoms combined with RSA augmentation, suggesting they respond differently than mothers and may be more likely to show a hyporeactive physiological response to challenge. Fourth, physiology and symptom profiles showed relevance for developmental psychopathology in that child emotional and behavioral dysregulation one year later was greater when mothers or fathers belonged to a mild or moderate risk profile as compared to the typical profile. However, outcomes were robust for mothers and trending for fathers, likely due to the smaller sample size of fathers. Findings will need to be replicated with larger samples, but this study takes a first step forward in understanding how parasympathetic physiology and internalizing symptoms covary in mothers and fathers in community populations.
Parasympathetic Physiology and Low Symptoms in Community Samples
We hypothesized that lower resting RSA could reflect the general distress factor observed in depressed and anxious individuals according to the Tripartite model (Clark & Watson, 1991), but lower resting RSA did not characterize risk profiles. This relation may be less robust in community than clinical samples if the greater symptom severity characteristic of clinical disorders prompts or is underscored by greater physiological regulatory dysfunction, making statistical relations more robust. To our knowledge, no other studies have examined clustering of RSA and symptoms in a community sample, however, other studies have found no relation between heart rate variability and depressive symptom severity in non-clinical samples (Koenig, Kemp, Beauchaine, Thayer, & Kaess, 2019). We also found that moderate risk groups showed elevated levels of both depressive and anxiety symptoms, reflecting the comorbidity of these symptoms established in prior clinical work (Kircanski et al., 2016). It is intriguing that an overlap of symptoms was present and yet differentiation in RSA reactivity patterns by the most predominant symptom type was still apparent in mothers, perhaps as a function of the greater time spent experiencing that symptom type and its associated emotional and behavioral regulatory correlates. The fact that we observed stronger relations between symptoms of anxiety and depression and patterns of hyper- and hyporeactivity, respectively, provides some support for the Tripartite Model, at least among mothers. This suggests that in community populations, a person-centered approach may be useful for understanding RSA as a biomarker of psychopathology risk, even in individuals showing lower symptom levels and multiple symptom types.
Interestingly, both mothers’ and fathers’ mild risk profiles were characterized by higher resting RSA. This finding was the most novel relative to prior research. Resting RSA is thought to reflect readiness to respond to stimuli, including challenge, and greater flexibility in adapting to the environment (Porges, 2007). But greater sensitivity to the environment, while adaptive in some situations (e.g., attending to child needs), may also increase susceptibility to environmental stressors (Belsky & Pluess, 2009). Thus, those with higher resting RSA may also show greater sensitivity to challenges, which could be associated with a greater tendency to experience mild mental health symptoms. Notably, both mothers and fathers demonstrated this heightened resting RSA associated with mild symptoms. Some clinical research has also indicated higher resting RSA may act as a risk factor for depressive symptoms (Rottenberg et al., 2002). Future research will be needed to better understand higher resting RSA levels and the degree to which they represent risk or protective factors in relation to symptoms of psychopathology.
Differential RSA Patterns Underlying Heightened Risk for Anxiety and Depression
Mothers showed differences in RSA reactivity aligned with heightened anxiety and depressive symptoms in line with the Tripartite Model (Clark & Watson, 1991). In the Moderate Risk/Withdrawal profile, RSA change was significantly lower than the sample mean, reflecting withdrawal that was more pronounced than expected. This finding echoes prior research showing that individuals with clinical or subclinical anxiety demonstrate “excessive” RSA withdrawal to challenge, which could be associated with an overactive fight-or-flight response via increased activation of the sympathetic nervous system (Beauchaine, 2015). In contrast, the Moderate Risk/Augmentation profile showed mean RSA change significantly above the sample mean, indicating RSA augmentation to challenge was the norm within this class. This may reflect the blunted parasympathetic response observed in depressed individuals across physiological and neuroendocrine systems (Grisson & Bhatnagar, 2009). Hyporeactivity can reflect self-protection from the damaging effects of an overactivated autonomic response to chronic stress (McEwen, 2000). Our findings suggest these RSA patterns may be present in community samples of mothers, which could inform the identification of risk for anxiety versus depressive disorders.
Mothers’ and Fathers’ Similarities and Differences
This study also explored differences in mothers’ and fathers’ physiology and symptoms. Given our subsample of fathers was smaller, direct comparisons are challenging, but we can interpret findings as preliminary evidence of potential similarities and differences. Both mothers and fathers had a typical class that did not report symptoms and showed minimal RSA change across tasks. Also, mild risk groups for mothers and fathers were similar, both showing elevated resting RSA and higher likelihood of anxiety symptoms (though mothers in the mild profile also showed elevated depressive symptoms). Further, moderate risk groups for both mothers and fathers evidenced “comorbidity” such that there were higher probabilities of moderate levels of both anxiety and depressive symptoms relative to mild or no symptoms.
A major difference between mothers and fathers was that Moderate Risk fathers showed no distinction in RSA reactivity: the single moderate risk profile showed RSA augmentation to challenge rather than withdrawal. This may be explained by differences in the way that men and women experience mental health symptoms (McClean et al., 2011). Men typically display fewer somatic symptoms such as increased heart palpitations (Dekker et al., 2008), which may mean fathers are less prone to physiological hyperreactivity than mothers. Fathers at higher risk for psychopathology may be more likely to show hyporeactive than hyperreactive parasympathetic patterns. The implications of these findings for research on parenting are interesting: parenting deficits among fathers may be more likely to fall into a disengaged or unresponsive than an intrusive and hypervigilant category. It may also be the case that parenting tasks are not as stressful for fathers as they are for mothers, in which case, risk may be more likely reflected in RSA augmentation than withdrawal in the context of our stressful parenting challenge. Prior work regarding gender differences in perceived stress has been mixed, with some studies finding lower levels among fathers than mothers (e.g., Frank et al., 1991; Holden et al., 1989) but others finding similar reports (e.g., Deater-Deckard & Scarr, 1996; Davis & Carter, 2008). It will be important for future research to employ larger and more comparable samples of mothers and fathers to determine if these profiles are replicated, perhaps incorporating different types of challenges to probe for RSA change.
Effects of Parents’ Profile Membership on Child Adjustment
Regarding child adjustment, mothers’ membership in any risk class predicted greater emotional and behavioral problems for children than membership in the typical class. This finding is consistent with prior work associating mothers’ depressive and anxiety symptoms with children’s internalizing and externalizing problems (Graziano & Derefinko, 2013), such that any level other than ‘no symptoms’ was associated with increased child dysregulation. This pattern may reflect that children are sensitive to any level of maternal symptoms; it is also possible that we did not have a large enough range of maternal symptoms needed to detect differences in child outcomes between mild and moderate symptom levels. Parents with elevated levels of symptoms may also be more likely to rate children higher on emotional and behavioral dysregulation (Goodman et al., 2011).
Some distinct relations were also observed between mothers’ risk profiles and child outcomes. For instance, membership in the Moderate Risk/Withdrawal group predicted greater child internalizing relative to the Typical group, but membership in the Moderate Risk/Augmentation group did not. Thus, mothers’ membership in the Moderate Risk/Withdrawal profile (indicating RSA hyperreactivity to challenge) may imbue a specific risk for children’s internalizing behaviors. It is also a possibility that links between the Moderate risk/Augmentation profile and children’s internalizing behaviors were not detected at such an early stage, as depressive symptoms increase over mid-to-late adolescence (Hankin et al., 2015) and the blunting of physiological responses (i.e., hyporeactivity) may be associated with greater chronicity of depressive symptoms (e.g., Booij et al., 2013). Such differences in RSA patterns between risk groups could translate into different pathways from profile membership to child behavior problems (i.e., different means to the same ends; Cicchetti & Rogosch, 1996), but more research will be needed to replicate these findings and to test additional mechanisms of this transmission, such as differences in parenting behavior or genetic contributions.
Importantly, significant differences were demonstrated not only between the typical and moderate risk classes, but also between the typical and mild risk class, suggesting that even mild risk in mothers (i.e., low symptom levels and heightened resting RSA) had an effect on child dysregulation. This result underscores the need to consider the implications of parental RSA differences for child psychopathology risk even when reported parental symptoms appear low. The fact that maternal profiles were distinguished based on patterns of resting RSA and RSA regulation in addition to symptoms, combined with the impact such profiles appear to have on child functioning, suggests that there could be some utility in screening individuals for parenting programs and/or treatment for coping with stress by using physiological measurement. It will be interesting to replicate these findings in future work with larger samples to test whether greater analytic power can help to distinguish differences between lower and higher risk profiles, and/or between anxiety and depressive-centered profiles.
For fathers, there were trending differences between risk classes such that children of fathers in moderate risk classes showed marginally higher emotional and behavior problems than those in mild risk and typical classes. Thus, whereas the mild and moderate risk profiles for mothers each had direct implications for children’s adjustment outcomes, only the moderate risk profile for fathers was associated with children’s emotional and behavioral problems. This may reflect that parent-child relations may be less susceptible to fathers’ lower-level symptoms as compared to those of mothers. However, the marginal significance of the overall model for fathers means that these findings can only be offered as preliminary evidence of these possible relations, and that future research is needed to replicate these tests on larger samples of fathers.
Limitations
The present findings are only generalizable to a community sample in which a lower incidence of anxiety and depressive disorders is the norm. We utilized a measurement tool, the BSI, that is more commonly used to measure general distress rather than differentiate between anxiety and depression (although certain BSI subscales including anxiety and depressive symptoms have been shown to be meaningful; Hayes, 1997). Future research could lend support to our findings by examining profiles using one or more instruments that measure anxiety and depressive symptoms more specifically. Another limitation of the current study was the use of self-report questionnaires to assess anxiety and depressive symptoms and mothers’ report to assess behavioral and emotional problems in children. As noted above, this may have led to an inflation of relations between mothers’ symptoms and children’s outcomes, however, this likely did not affect the father models given that fathers’ ratings of outcomes were not used. Although relations between parent profiles and parent-reported child outcomes are informative, future research could examine potential mediating factors, such as observed or self-reported parenting behavior, to better understand how parent physiology and symptoms influence children’s regulation and dysregulation. Sample size differences between mother and father models may have contributed to their differential effects and made it more difficult to interpret differences between them. Although larger sample sizes would have aided analytic power, confidence in our LPA results is strengthened by a few factors. These include a low number of indicators, a fairly large degree of separation between profiles (differences in RSA means were on the order of 0.75 to 2 SD), and clear differentiation between symptom severity categories (with probabilities between .8 and 1 for most classes) (Tein et al., 2013). Nonetheless, the smaller sample size may have impeded our ability to identify and interpret additional profiles and may have impacted the strength of effects of profile membership on child adjustment. As such, replication with larger samples (particularly fathers) will be needed to validate these findings. Most participants were White or Latinx, thus replication will also be important to establish generalizability to other racial and ethnic groups.
Conclusions
A better understanding of how parents with mental health symptoms respond physiologically to challenging interactions with children may have important implications for their potential to transmit risk for psychopathology to their children. It is important to know whether heterogeneity exists within parents at risk for mental health problems that subsequently impacts their children’s well-being. Results of this study encourage future research to form more holistic profiles of risk that inform risk transmission, potentially improving the fit of intervention efforts catered towards unique groups of individuals. Understanding the role of parasympathetic physiology in psychopathology risk in community samples of parents and children may help refine our understanding of RSA as a biomarker of mental health, as well as informing the etiology and prevention of dysregulated emotional and behavioral problems in children.
Acknowledgements
This research was supported by funding from the National Institute of Child Health and Human Development, K01HD068170.
Footnotes
The authors have no conflict of interest to declare. Research data are not shared or publicly available.
References
- Achenbach TM & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VA: University of Vermont. [Google Scholar]
- American Psychological Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychological Association [Google Scholar]
- Anderson ER & Hope DA (2008). A review of the tripartite model for understanding the link between anxiety and depression in youth. Clinical Psychology Review, 28, 275–287. doi: 10.1016/j.cpr.2007.05.004 [DOI] [PubMed] [Google Scholar]
- Bakk Z, & Vermunt J (2016). Robustness of stepwise latent class modeling with continuous distal outcomes. Structural Equation Modeling: A Multidisciplinary Journal, 23(1), 20–31. [Google Scholar]
- Beauchaine TP (2015). Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child & Adolescent Psychology, 44(5), 875–896. doi: 10.1080/15374416.2015.1038827 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, & Thayer JF (2015). Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology, 98, 338–350. doi: 10.1016/j.ijpsycho.2015.08.004 [DOI] [PubMed] [Google Scholar]
- Belsky J, & Pluess M (2009). Beyond diathesis stress: Differential susceptibility to environmental influences. Psychological Bulletin, 135(6), 885–908. doi: 10.1037/a0017376 [DOI] [PubMed] [Google Scholar]
- Booij SH, Bouma EMC, de Jonge P, Ormel J, & Oldehinkel AJ (2013). Chronicity of depressive problems and the cortisol response to psychosocial stress in adolescents: The TRAILS study. Psychoneuroendocrinology, 38(5), 659–666. https://doi-org.libproxy.uoregon.edu/10.1016/j.psyneuen.2012.08.004 [DOI] [PubMed] [Google Scholar]
- Berntson GG, Cacioppo JT, & Quigley KS (1993). Respiratory sinus arrhythmia: Autonomic origins, physiological mechanisms, and psychophysiological implications. Psychophysiology, 30(2), 183–196. doi: 10.1111/j.1469-8986.1993.tb01731.x [DOI] [PubMed] [Google Scholar]
- Bornstein MH, & Suess PE (2000). Child and mother cardiac vagal tone: Continuity, stability, and concordance across the first 5 years. Developmental Psychology, 36(1), 54–65. 10.1037/0012-1649.36.1.54 [DOI] [PubMed] [Google Scholar]
- Bray BC, Foti RJ, Thompson NJ, & Wills SF (2014). Disentangling the effects of self leader perceptions and ideal leader prototypes on leader judgments using loglinear modeling with latent variables. Human Performance, 27(5), 393–415. doi: 10.1080/08959285.2014.956176 [DOI] [Google Scholar]
- Cicchetti D, & Rogosch FA (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology, 8(4), 597–600. [Google Scholar]
- Cicchetti D, & Schneider-Rosen K (1986). An organizational approach to childhood depression. In Rutter M, Izard C, & Read P (Eds.), Depression in Young People: Clinical and Developmental Perspectives (pp. 71–134). New York: Guilford. [Google Scholar]
- Clark LA & Watson D (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100(3), 316–336. [DOI] [PubMed] [Google Scholar]
- Connell AM, Hughes-Scalise A, Klostermann S, & Azem T (2011). Maternal depression and the heart of parenting: Respiratory sinus arrhythmia and affective dynamics during parent–adolescent interactions. Journal of Family Psychology, 25(5), 653–662. 10.1037/a0025225 [DOI] [PubMed] [Google Scholar]
- Crnic K, & Low C (2002). Everyday stresses and parenting. In Bornstein MH (Ed.) Handbook of parenting: Practical issues in parenting, 2nd ed (pp. 243–267). Mahwah, NJ: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Davis NO, & Carter AS (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders, 38(7), 1278–1291. doi: 10.1007/s10803-007-0512-z [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, & Scarr S (1996). Parenting stress among dual-earner mothers and fathers: Are there gender differences? Journal of Family Psychology, 10(1), 45–59. doi: 10.1037/0893-3200.10.1.45 [DOI] [Google Scholar]
- Dekker J, Koelen JA, Peen J, Schoevers RA, & Gijsbers-Van Wijk C (2008). Gender differences in clinical features of depressed outpatients: Preliminary evidence for subtyping of depression? Women & Health, 46(4), 19–38. doi:10.1300/J013v46n04_02 [DOI] [PubMed] [Google Scholar]
- Derogatis LR (1992). BSI: Administration, scoring, and procedures manual – II. Clinical Psychometric Research, Towson, MD. [Google Scholar]
- Derogatis LR & Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. [PubMed] [Google Scholar]
- Ellis BJ, Boyce WT, Belsky J, Bakermans-Kranenburg M, & Van Ijzendoorn MH (2011). Differential susceptibility to the environment: An evolutionary–neurodevelopmental theory. Development and Psychopathology, 23(1), 7–28. doi:http://dx.doi.org.ezaccess.libraries.psu.edu/10.1017/S0954579410000611 [DOI] [PubMed] [Google Scholar]
- Fracasso MP, Porges SW, Lamb ME, & Rosenberg AA (1994). Cardiac activity in infancy: Reliability and stability of individual differences. Infant Behavior & Development, 17(3), 277–284. doi: 10.1016/0163-6383(94)90006-X [DOI] [Google Scholar]
- Frank SJ, Olmstead CL, Wagner AE, Laub CC, Freeark K, Breitzer GM, & Peters JM (1991). Child illness, the parenting alliance, and parenting stress. Journal of Pediatric Psychology, 16, 361–371. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Robbins Broth M, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14, 1–27. doi: 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Gouin JP, Deschenes SS, & Dugas MJ (2014). Respiratory sinus arrhythmia during worry forecasts stress-related increases in psychological distress. Stress, 17(5), 416–422. doi: 10.3109/10253890.2014.949666 [DOI] [PubMed] [Google Scholar]
- Graziano PA, & Derefinko K (2013). Cardiac vagal control and children’s adaptive functioning: A meta-analysis. Biological Psychology, 94(1), 22–37. doi: 10.1016/j.biopsycho.2013.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaves-Lord K, Ferdinand RF, Sondeijker F, Dietrich A Oldehinkel AJ … & Verhulst FC (2007). Testing the tripartite model in young adolescents: Is hyperarousal specific for anxiety and not depression? Journal of Affective Disorders, 102, 55–63. doi: 10.1016/j.jad.12.009 [DOI] [PubMed] [Google Scholar]
- Grissom N, & Bhatnagar S (2009). Habituation to repeated stress: Get used to it. Neurobiology of Learning and Memory, 92(2), 215–224. doi: 10.1016/j.nlm.2008.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han ZR, Lei X, Qian J, Li P, Wang H, & Zhang X (2016). Parent and child psychopathological symptoms: The mediating role of parental emotion dysregulation. Child and Adolescent Mental Health, 21(3), 161–168. doi: 10.1111/camh.12169 [DOI] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley LD, … & Oppenheimer CW (2015). Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology, 124(4), 803–816. doi: 10.1037/abn0000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes JA (1997). What does the Brief Symptom Inventory measure in college and university counseling center clients? Journal of Counseling Psychology, 44(4), 360–367. 10.1037/0022-0167.44.4.360 [DOI] [Google Scholar]
- Hernandez E, Smith CL, Day KL, Neal A, & Dunsmore JC (2018). Patterns of parental emotion-related discourse and links with children’s problem behaviors: A person-centered approach. Developmental Psychology, 54(11), 2077–2089. doi: 10.1037/dev0000602 [DOI] [PubMed] [Google Scholar]
- Holden EW, Willis DJ, & Foltz L (1989). Child abuse potential and parenting stress: Relationships in maltreating parents. Psychological Assessment, 1, 64–67. [Google Scholar]
- Holmes TH, & Rahe RH (1967). The Social Readjustment Rating Scale. Journal of Psychosomatic Research, 11(2), 213–218. doi: 10.1016/0022-3999(67)90010-4 [DOI] [PubMed] [Google Scholar]
- Holzman JB, & Bridgett DJ (2017). Heart rate variability indices as bio-markers of top-down self-regulatory mechanisms: A meta-analytic review. Neuroscience & biobehavioral reviews, 74, 233–255. 10.1016/j.neubiorev.2016.12.032 [DOI] [PubMed] [Google Scholar]
- Hu MX, Larners F, de Geus EJC, & Penninx BWJH (2016). Differential autonomic nervous system reactivity in depression and anxiety during stress depending on type of stressor. Psychosomatic Medicine, 78, 562–572. doi: 10.1097/PSY.0000000000000313 [DOI] [PubMed] [Google Scholar]
- Joormann J, Eugène F, & Gotlib IH (2008). Parental depression: Impact on offspring and mechanisms underlying transmission of risk. In Nolen-Hoeksema S (Ed.), Handbook of adolescent depression (pp. 441–471). New York, NY: Guilford Press. [Google Scholar]
- Kerns CE, Pincus DB, McLaughlin KA, & Comer JS (2017). Maternal emotion regulation during child distress, child anxiety accommodation, and links between maternal and child anxiety. Journal of Anxiety Disorders, 50, 52–59. doi: 10.1016/j.janxdis.2017.05.002 [DOI] [PubMed] [Google Scholar]
- Kircanski K, Waugh CE, Camacho MC, & Gotlib IH (2016). Aberrant parasympathetic stress responsivity in pure and co-occurring major depressive disorder and generalized anxiety disorder. Journal of Psychopathology and Behavioral Assessment, 38(1), 5–19. doi: 10.1007/s10862-015-9493-y [DOI] [Google Scholar]
- Koenig J, Kemp AH, Beauchaine TP, Thayer JF, & Kaess M (2016). Depression and resting state heart rate variability in children and adolescents—A systematic review and meta-analysis. Clinical Psychology Review, 46, 136–150. doi: 10.1016/j.cpr.2016.04.013 [DOI] [PubMed] [Google Scholar]
- Lamers F, van Oppen P, Comijs HC, Smit JH, Spinhoven P, … & Penninx BWJH (2011). Comorbidity patterns of anxiety and depressive disorders in a large cohort study: The Netherlands Study of Depression and Anxiety (NESDA). The Journal of Clinical Psychiatry, 72(3), 341–348. doi: 10.4088/JCP.10m06176blu [DOI] [PubMed] [Google Scholar]
- Lanza S, & Collins LM (2009). Latent class and latent transition analysis for application in the social, behavioral, and health sciences. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Lazarsfeld PF, & Henry NW (1968). Latent structure analysis. Boston, MA: Houghton Mifflin. [Google Scholar]
- Licht CMM, de Geus EJC, van Dyck R, & Penninx BWJH (2009). Association between anxiety disorders and heart rate variability in the Netherlands Study of Depression and Anxiety (NESDA). Psychosomatic Medicine, 71, 508–518. doi: 10.1097/PSY.0b013e3181a292a6 [DOI] [PubMed] [Google Scholar]
- Lunkenheimer E, Busuito A, Brown K, Panlilio C, & Skowron EA (2019). The interpersonal neurobiology of child maltreatment: Parasympathetic substrates of interactive repair in maltreating and non-maltreating mother-child dyads. Child Maltreatment, 24(4), 353–363. doi: 10.1177/1077559518824058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunkenheimer ES, Kemp CJ, Lucas-Thompson RG, Cole PM, & Albrecht EC (2016). Assessing biobehavioural self-regulation and coregulation in early childhood: The Parent-Child Challenge Task. Infant and Child Development, 26(1). doi: 10.1002/icd.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunkenheimer E, Tiberio SS, Skoranski AM, Buss KA, & Cole PM (2018). Parent-child coregulation of parasympathetic processes varies by social context and risk for psychopathology. Psychophysiology, 55(2). doi: 10.1111/psyp.12985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKenzie MJ, Kotch JB, & Lee LC (2011). Toward a cumulative ecological risk model for the etiology of child maltreatment. Children and Youth Services Review, 33(9), 1638–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS (2000). Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology, 22(2), 108–124. doi: 10.1016/S0893-133X(99)00129-3 [DOI] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, & Hofmann SG (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035. doi: 10.1016/j.jpsychires.2011.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, & Clark LA (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology,49, 377–412. doi: 10.1146/annurev.psych.49.1.377 [DOI] [PubMed] [Google Scholar]
- Morlan KK, & Tan SY (1998). Comparison of the Brief Psychiatric Rating Scale and the Brief Symptom Inventory. Journal of Clinical Psychology, 54(7), 885–894. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus user’s guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Paulson JF, & Bazemore SD (2010). Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA: Journal of the American Medical Association, 303(19), 1961–1969. doi: 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- Porges SW (1991). Vagal tone: An autonomic mediator of affect. In Garber J, Dodge KA, Garber J & Dodge KA (Eds.), The development of emotion regulation and dysregulation. (pp. 111–128). New York, NY, US: Cambridge University Press. [Google Scholar]
- Porges SW (2007). The polyvagal perspective. Biological Psychology, 74(2), 116–143. doi: 10.1016/j.biopsycho.2006.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Root AE, Hastings PD, & Rubin KH (2016). The parenting behaviors of shy–anxious mothers: The moderating role of vagal tone. Journal of Child and Family Studies, 25(4), 1325–1333. doi: 10.1007/s10826-015-0296-2 [DOI] [Google Scholar]
- Rottenberg J, Clift A, Boden S, & Salomon K (2007). RSA fluctuation in major depressive disorder. Psychophysiology, 44, 450–458. doi: 10.1111/j.1469-8986.2007.00509.x [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Wilhelm FH, Gross JJ, & Gotlib IH (2002). Respiratory sinus arrhythmia as a predictor of outcome in major depressive disorder. Journal of Affective Disorders, 71, 265–272. [DOI] [PubMed] [Google Scholar]
- Royal College of Psychiatrists. (2016). Parental mental illness: The impact on children and adolescents. Information for parents, carers and anyone who works with young people. rcpsych.ac.uk/healthadvice/parentsandyouthinfo/parentscarers/parentalmentalillness.aspx
- Shields A, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33(6), 906–916 [DOI] [PubMed] [Google Scholar]
- Shih EW, Quiñones‐Camacho LE, Karan A, & Davis EL (2019). Physiological contagion in parent–child dyads during an emotional challenge. Social Development, 28(3), 620–636. doi: 10.1111/sode.12359 [DOI] [Google Scholar]
- Skoranski AM, Lunkenheimer E, & Lucas-Thompson RG (2017). The effects of maternal respiratory sinus arrhythmia and behavioral engagement on mother-child physiological coregulation. Developmental Psychobiology, 59(7), 888–898. doi: 10.1002/dev.21543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stifter CA, & Fox NA (1990). Infant reactivity: Physiological correlates of newborn and 5-month temperament. Developmental Psychology, 26(4), 582–588. doi: 10.1037/0012-1649.26.4.582 [DOI] [Google Scholar]
- Tein J, Coxe S, & Cham H (2013). Statistical power to detect the correct number of classes in latent profile analysis. Structural Equation Modeling, 20(4), 640–657. doi: 10.1080/10705511.2013.82478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer JF, Friedman BH, & Borkovec TD (1995). Autonomic characteristics of generalized anxiety disorder. Biological Psychiatry, 39, 255–266. [DOI] [PubMed] [Google Scholar]
- Thayer JF & Lane RD (2000). A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders, 61, 201–216. [DOI] [PubMed] [Google Scholar]
- Thompson RA (1994). Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development, 59(2–3), 25–52, 250–283. doi: 10.2307/1166137 [DOI] [PubMed] [Google Scholar]
- Tronick EZ (1989). Emotions and emotional communication in infants. American Psychologist, 44(2), 112–119. doi: 10.1037/0003-066X.44.2.112 [DOI] [PubMed] [Google Scholar]
- Tronick E & Beeghly M (2011). Infants’ meaning-making and the development of mental health problems. American Psychologist, 66(2), 107–119. doi: 10.1037/a0021631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turpyn CC, Chaplin TM, Cook EC, & Martelli AM (2015). A person-centered approach to adolescent emotion regulation: Associations with psychopathology and parenting. Journal of Experimental Child Psychology, 136, 1–16. doi: 10.1016/j.jecp.2015.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzoumakis S, Lussier P, & Corrado RR (2014). The persistence of early childhood physical aggression: Examining maternal delinquency and offending, mental health, and cultural differences. Journal of Criminal Justice, 42(5), 408–420. [Google Scholar]
- Urbán R, Kun B, Farkas J, Paksi B, Kökönyei G, Unoka Z, … & Demetrovics Z (2014). Bifactor structural model of symptom checklists: SCL-90-R and Brief Symptom Inventory (BSI) in a non-clinical community sample. Psychiatry Research, 216(1), 146–154. doi: 10.1016/j.psychres.2014.01.027 [DOI] [PubMed] [Google Scholar]
- Watkins LL, Grossman P, Krishnan R, & Sherwood A (1998). Anxiety and vagal control of heart rate. Psychosomatic Medicine, 60, 498–502. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, & McCormick RA (1995). Testing a tripartite model: Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology, 104(1), 3–14. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Iannotti RJ, Cummings EM, & Denham S (1990). Antecedents of problem behaviors in children of depressed mothers. Development and Psychopathology, 2(3), 271–291. 10.1017/S0954579400000778 [DOI] [Google Scholar]


