Abstract
Purpose
Male infertility is emerging as a major, escalating global health problem that imposes the need to investigate research trends in male infertility. The purpose of this study is to analyze male infertility research trends in the past 20 years using the bibliometric database from Scopus.
Materials and Methods
In order to perform an in-depth bibliometric analysis, we propose a ‘Funnel Model’, which includes several layers representing different sub-areas of male infertility research. Adopting this Funnel Model, using Scopus, we retrieved relevant bibliometric data (articles per year, authors, affiliations, journals, and countries) for various areas of male infertility research and performed descriptive statistics.
Results
The bibliometric analysis showed an exponential increase in male infertility research in the last 20 years. USA dominated in research output, with Agarwal, A. as the most prolific researcher. Testicular cancer, obesity and metabolic syndrome, and azoospermia were found to dominate male infertility research, whereas erectile dysfunction and unexplained male infertility had lesser attention. Interestingly, prognostic/diagnostic and mechanistic studies have significantly increased in parallel over the last 20 years. Furthermore, our bibliometric analysis revealed fewer publications in proteomics, transcriptomics and metabolomics when compared to genomics. Also, an increasing trend in publication was seen in assisted reproductive technology (ART) research.
Conclusions
An integrated and steep escalation in the field of omics and ART research appears to be a prerequisite for further development of future diagnostic and therapeutic strategies for male infertility.
Keywords: Bibliometric analysis; Diagnosis; Infertility, male; Prognosis; Publications
INTRODUCTION
Substantial evidence signifies infertility as a global problem affecting around 15% of couples in which male factor contributes to more than half of the cases [1]. Around 30 million men in the world are infertile, with the highest rates reported in Africa and Eastern Europe [2]. Apart from an increasing incidence of male infertility, reports on declining semen quality among healthy men around the world has significantly accelerated male infertility research in recent years [3,4]. The extensive research on male infertility is emulated with an increased number of publications in the past decades.
Bibliometrics, a quantitative analysis of literature, has recently emerged as a convenient tool to evaluate the growth of various research fields [5,6]. Until now, only a few bibliometric analyses on male infertility have been published. These analyses have reported one or more of the following: publication trends, top countries, institutions, and authors contributing scientific articles, major journals, frequently used keywords, coword analysis, hot topics, co-authorship network, and collaboration patterns [7,8,9,10]. Though this kind of data provides a broader view on research trends, it lacks an in-depth analysis of several major elements within male infertility research.
Male infertility research is a broad spectrum involving various elements, such as influencing factors, molecular mechanisms underlying the pathogenesis, prognosis and diagnosis of various infertility scenarios, and advancements in assisted reproductive technology (ART). In recent years, development in research techniques have paved way for new generation ‘omics’ technologies that validate genes (genomics), mRNAs (transcriptomics), proteins (proteomics), and metabolites (metabolomics) as potential diagnostic and therapeutic biomarker for male infertility [11]. Bibliometric analyses reported so far have not shed light on these crucial and emerging technologies, which necessitates the need for an in-depth analysis of male infertility research.
A detailed analysis of research trends will enable us to understand the extent of publications on (a) defining the magnitude of male infertility, (b) understanding the molecular basis of male infertility, and (c) aiding the provision of solutions to male infertility. Information on these will provide a clear picture about where we currently stand in male infertility research, recent developments in new generation technologies and how far we have truly progressed in finding solutions. In order to perform an in-depth bibliometric analysis, we have proposed a “Funnel Model”, which includes several layers representing different areas of male infertility research. This model facilitates the analysis of male infertility as a broader topic and then progressively narrows down to sub-areas and key aspects of male infertility research.
MATERIALS AND METHODS
1. Ethics statement
The present study did not involve any human subject participation, and it was entirely performed using the bibliometric data retrieved from Scopus and hence, it is deemed to be exempted from the Institutional Review Board approval.
2. Data source
Bibliographic databases such as Scopus, Web of Science, Google Scholar, PubMed, etc. are used to retrieve data for bibliometric analysis [9,10,12]. In the present study, we retrieved relevant data exclusively from Scopus, since it is the most comprehensive bibliographic database. Scopus covers more than 22,800 titles (Health Sciences and Life Sciences with 7,133 and 4,106 titles, respectively) and the titles can be listed in more than one subject area. Currently, Scopus has over 71 million core records from nearly 5,000 publishers with 1.4 billion cited references. Each year, about 3 million new items (~5,500 each day) are added to the database. Notably, the Scopus database can be searched with Boolean operators, such as ‘AND’, ‘OR’, and ‘NOT’ with specific keywords to generate a more defined query for obtaining relevant data. Besides, Scopus has a variety of operating functions that simplify bibliometric analysis, such as author, year of publication, type of document, journal name, affiliations, country, subject area, the number of citations, and Hirsch-index metrics [13,14].
3. Data retrieval strategies
The selection of keywords is pivotal in bibliometric analysis since keywords directly influence the amount of data retrieved, results and findings. In the present study, the online search in Scopus was performed on October 26, 2018. The search criteria in Scopus was based on ‘All Fields’ using specific keywords with certain limitation imposed by the Boolean operators to nullify false-positive results (Table 1). Furthermore, the search criteria was limited to scientific articles published in the English-language from 1998 to 2017 by using the keywords listed in Table 1. Since the 2018 data in Scopus does not represent the entire year, it was not included in the analysis.
Table 1. Key words used for each layer in the Funnel Model.
| Layer | Content (1998–2017) | Keywords |
|---|---|---|
| Layer 1 | Male Infertility | (A) |
| Layer 2a | Varicocele | (A) AND (Varicocele OR Varicocoele) |
| Layer 2b | Azoospermia | (A) AND (Azoospermia) |
| Layer 2c | Oligozoospermia | (A) AND (Oligozoospermia) |
| Layer 2d | Testicular cancer | (A) AND (Testicular Cancer OR carcinoma) |
| Layer 2e | Erectile Dysfunction | (A) AND (Erectile Dysfunction) |
| Layer 2f | Male Genital Tract infection | (A) AND (Reproductive Tract Infection) |
| Layer 2g | UMI | (A) AND (Unexplained Male Infertility OR Unexplained infertile men OR UMI) |
| Layer 2h | Hypogonadism | (A) AND (Hypogonadism) |
| Layer 2i | Obesity and Metabolic Syndrome | (A) AND (Obesity OR Overweight OR BMI OR Metabolic Syndrome) |
| Layer 2j | Lifestyle | (A) AND (Lifestyle OR Smoking OR Alcohol) |
| Layer 2k | Occupational Exposure | (A) AND (Occupational Exposure) |
| Layer 3 | Mechanistic Studies | (A) AND (Mechanism) |
| Prognostic /Diagnostic Studies | (A) AND (Prognosis OR Diagnosis OR prognostic OR Diagnostic) | |
| Layer 4 | Genomics | (A) AND (Genomics OR Genome) |
| Transcriptomics | (A) AND (Transcriptomics OR Transcriptome) | |
| Proteomics | (A) AND (Proteomics OR Proteome) | |
| Metabolomics | (A) AND (Metabolomics OR Metabolome) | |
| Layer 5 | ART | (A) AND (Assisted Reproductive Technology OR ART OR IVF OR ICSI) |
(A): ALL (Male AND Infertility OR Subfertility OR Sterility) AND (Human OR Man), UMI: unexplained male infertility, BMI: body mass index, ART: assisted reproductive technology, IVF: in vitro fertilization, ICSI: intracytoplasmic sperm injection.
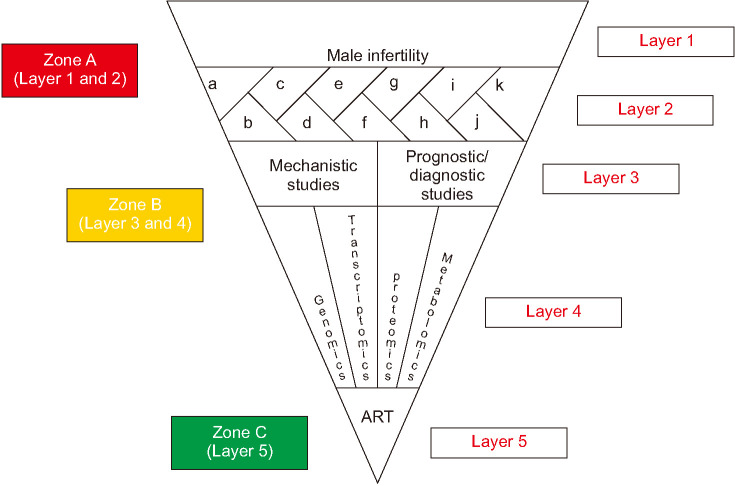
We have adopted a Funnel Model (Fig. 1) to retrieve relevant bibliometric data in the area of male infertility from Scopus. This Funnel Model was broadly divided into three zones (A, B, and C) and five layers. Indications of each layer and zone are summarized in Table 2. Zone A comprised of Layers 1 and 2. In Layer 1, all the bibliometric data available from 1998 to 2017 in male infertility was retrieved using the search option ‘ALL (Male AND Infertility OR subfertility OR Sterility) AND (Human OR Man)’. The selection of keywords for Layer 1 was similar to a recent publication on bibliometric analysis of male infertility [9]. The Layer 2 has been classified into sub-sections (a to k) in which the search option for Layer 1 was used along with additional specific keywords for azoospermia, erectile dysfunction (ED), hypogonadism, lifestyle, male genital tract infection, obesity and metabolic syndrome (MetS), occupational exposure, oligozoospermia, testicular cancer, unexplained male infertility (UMI), and varicocele to retrieve the bibliometric data (Table 1). Zone B comprised of Layers 3 and 4. In Layer 3, the bibliometric data were obtained using the search option used for Layer 1 along with the keywords for mechanistic studies and prognostic or diagnostic studies. In Layer 4, the bibliometric data were derived by using the search option used for Layer 1 along with the keywords for genomics, transcriptomics, proteomics and metabolomics. Zone C comprised of Layer 5 in which the bibliometric data were obtained using the search option for Layer 1 with an additional keyword for ART.
Fig. 1. Schematic representation of the Funnel Model. Layer 1 represents overall trend in male infertility research; Layer 2 is a sub-classification of Layer 1 having a (azoospermia), b (erectile dysfunction, ED), c (hypogonadism), d (lifestyle), e (male genital tract infection), f (obesity and Metabolic Syndrome, MetS), g (occupational exposure), h (oligozoospermia), i (testicular cancer), j (unexplained male infertility, UMI), and k (varicocele); Layer 3 represents mechanistic and prognostic/diagnostic studies of male infertility; Layer 4 represents omics (genomics, transcriptomics, proteomics, and metabolomics)-based publications in male infertility; Layer 5 represents assisted reproductive technology (ART)-based publications on male infertility. Zone A is comprised of Layer 1 and 2. Publications in zone A defines the problem; Zone B is comprised of Layer 3 and Layer 4. Publications in zone B helps in understanding the basis of the problem. Zone C comprised of Layer 5 and publications in this zone provide possible solution(s) to the problem.
Table 2. Indications for each layer and zone in the Funnel Model.
| Layer/Zone | Content (1998–2017) |
|---|---|
| Layer 1 | Total number of publications on “male infertility” in the past 20 years. |
| Layer 2 | Number of publications in specified areas of male infertility research, such as Azoospermia, Erectile Dysfunction, Hypogonadism, Lifestyle, Male Genital Tract Infection, Obesity and Metabolic Syndrome, Occupational Exposure, Oligozoospermia, Testicular cancer, Unexplained Male Infertility, and Varicocele. |
| This layer indicates the area(s) that have received greater/lesser attention in the past 20 years. | |
| Layer 3 | Indicates the percentage of article that contributes to understand the mechanism/basis of male infertility as well as articles with prognostic or diagnostic values. |
| Layer 4 | Indicates the number of articles on new generation omics technologies (genomics, transcriptomics, proteomics, and metabolomics). |
| Layer 5 | Indicates the publications on assisted reproductive technology. |
| Zone A (Layer 1&2) | Articles in this zone represent the current trends in male infertility and defines the problem. |
| Zone B (Layer 3&4) | Articles in this zone help in understanding the basis of the problem. |
| Zone C (Layer 5) | Articles in this zone provide solution to the problem. |
4. Bibliometric data analysis
In the present study, the bibliometric data were obtained for author, affiliation, country, journal, and number of articles per year from Scopus as commaseparated value files and converted to Microsoft Excel files for descriptive statistical analysis. The bibliometric data retrieved from Scopus has a default threshold value of 15 for each operating function. Significant contributors in each sub-areas of male infertility research based on the number of publications in the past 20 years were reported.
RESULTS
1. Research trends in male infertility over the past 20 years (Layer 1)
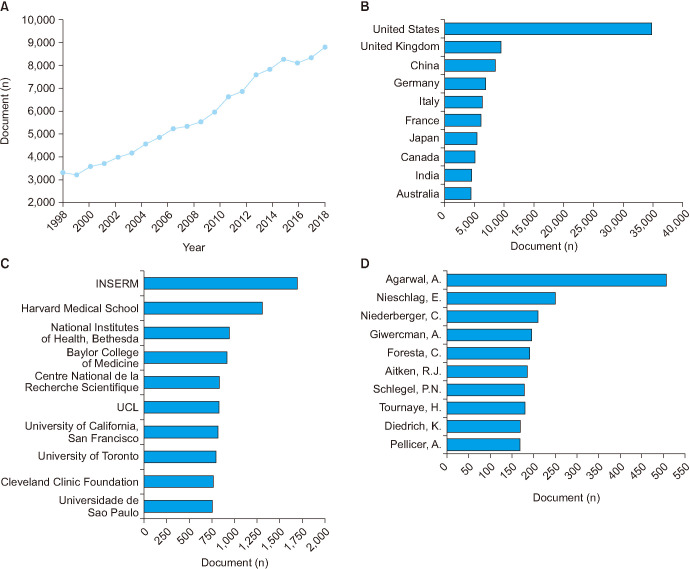
Analysis of male infertility research with respect to year revealed that 3,311 articles were published in 1998, whereas the number of published articles increased to 8,772 in 2017 (Fig. 2A). This phenomenal 265% increase in research articles over the past 20 years indicates that male infertility research has gained utmost importance in the scientific community. Further analysis of publications revealed that Fertility and Sterility (n=4,909), Human Reproduction (n=3,533), PloS One (n=1,576), Biology of Reproduction (n=1,539), and Reproductive Biomedicine Online (n=1,226) were the major journals publishing maximum number of articles in this field (data not shown). The analysis of origin of articles revealed that 30% of male infertility research articles were from the United States (n=34,748; 29.9%), followed by the United Kingdom (n=9,474; 8.2%) (Fig. 2B). INSERM (n=1,700), Harvard Medical School (n=1,310), National Institute of Health, Bethesda (n=945), Baylor College of Medicine (n=919), and Centre National de la Recherche Scientifique (n=833) were the top 5 institutions with maximum number of publications (Fig. 2C). Analysis of author contribution revealed Agarwal, A. (n=509) as the top scientist in the field of male infertility research followed by Nieschlag, E. (n=250), Niederberger, C. (n=211), Giwercman, A. (n=197), and Foresta, C. (n=191) (Fig. 2D).
Fig. 2. Publication trend in male infertility research by year (A), country (B), affiliation (C), and author (D) over the past 20 years (1998–2017). CNRS: Centre National de la Recherche Scientifique, UCL: University College London.
2. Publications in various areas of male infertility research over the past 20 years (Layer 2)
Upon analyzing the overall male infertility research trends, we further narrowed down the specific areas within male infertility research. Our results indicated that in the past 20 years, testicular cancer (n=15,110), obesity & MetS (n=14,383), and azoospermia (n=11,194) were the top three sub-areas, while the less focused areas were UMI (n=2,134) and ED (n=3,941) (Fig. 3). The other significant sub-areas of male infertility research included, but were not limited to, hypogonadism (n=7,414), lifestyle (n=6,715), and varicocele (n=5,400). The total number of articles published in various areas of male infertility research have been shown in Table 3. Our results also identified the top eminent researchers in each sub-category (Table 4).
Fig. 3. Publication trend in specific areas of male infertility research over the past 20 years. (A) Publication trend of varicocele, azoospermia, oligozoospermia, testicular cancer, erectile dysfunction, and male genital tract infection by year from 1998–2017. (B) Publication trends of unexplained male infertility (UMI), hypogonadism, obesity and metabolic syndrome, lifestyle, and occupational exposure by year from 1998–2017.
Table 3. Total number of articles published in different areas of male infertility research.
| Layer | Content | Total number of documents (1998–2017) |
|---|---|---|
| Layer 1 | Male Infertility | 116,233 |
| Layer 2a | Varicocele | 5,400 |
| Layer 2b | Azoospermia | 11,194 |
| Layer 2c | Oligozoospermia | 4,263 |
| Layer 2d | Testicular cancer | 15,110 |
| Layer 2e | Erectile Dysfunction | 3,941 |
| Layer 2f | Male Genital Tract infection | 4,498 |
| Layer 2g | UMI | 2,134 |
| Layer 2h | Hypogonadism | 7,414 |
| Layer 2i | Obesity and Metabolic Syndrome | 14, 383 |
| Layer 2j | Lifestyle | 6,715 |
| Layer 2k | Occupational Exposure | 5,293 |
| Layer 3 | Mechanistic Studies | 49,998 |
| Prognostic/Diagnostic Studies | 42,945 | |
| Layer 4 | Genomics | 26,190 |
| Transcriptomics | 4,088 | |
| Proteomics | 6,122 | |
| Metabolomics | 976 | |
| Layer 5 | ART | 20,703 |
UMI: unexplained male infertility, ART: assisted reproductive technology.
Table 4. Top scientists in various subcategories of male infertility research.
| Layer | Content | Total number of documents (1998–2017) |
|---|---|---|
| Varicocele | Agarwal, A. | 203 |
| Esteves, S.C. | 83 | |
| Sharma, R. | 56 | |
| Goldstein, M. | 53 | |
| Mostafa, T. | 50 | |
| Azoospermia | Schlegel, P.N. | 135 |
| Nieschlag, E. | 112 | |
| Agarwal, A. | 98 | |
| Foresta, C. | 83 | |
| Lipshultz, L.I. | 78 | |
| Oligozoospermia | Nieschlag, E. | 72 |
| Foresta, C. | 63 | |
| Agarwal, A. | 60 | |
| Ferlin, A. | 53 | |
| Krausz, C. | 48 | |
| Testicular cancer | Skakkebæk, N.E. | 154 |
| Agarwal, A. | 117 | |
| Giwercman, A. | 98 | |
| Toppari, J. | 80 | |
| Huhtaniemi, I. | 76 | |
| Erectile dysfunction | Maggi, M. | 77 |
| Corona, G. | 53 | |
| Hellstrom, W.J.G. | 51 | |
| Jannini, E.A. | 35 | |
| Lenzi, A. | 35 | |
| Male genital tract infection | Agarwal, A. | 68 |
| La Vignera, S. | 36 | |
| Calogero, A.E. | 34 | |
| Weidner, W. | 34 | |
| Vicari, E. | 32 | |
| Unexplained male infertility | Agarwal, A. | 79 |
| Esteves, S.C. | 38 | |
| Carrell, D.T. | 28 | |
| Majzoub, A. | 17 | |
| Garrido, N. | 16 | |
| McElreavey, K. | ||
| Hypogonadism | Nieschlag, E. | 122 |
| Maggi, M. | 79 | |
| Huhtaniemi, I. | 74 | |
| Simoni, M. | 53 | |
| Corona, G. | 51 | |
| Obesity and metabolic syndrome | Maggi, M. | 72 |
| Legro, R.S. | 48 | |
| Corona, G. | 47 | |
| Nieschlag, E. | 41 | |
| Azziz, R. | 40 | |
| Lifestyle | Skakkebæk, N.E. | 37 |
| Buck Louis, G.M. | 32 | |
| Bonde, J.P. | 30 | |
| Agarwal, A. | 29 | |
| Jensen, T.K. | 25 | |
| Occupational exposure | Bonde, J.P. | 139 |
| Giwercman, A. | 73 | |
| Olsen, J. | 61 | |
| Hauser, R. | 59 | |
| Toft, G. | 56 |
3. Publication trends in mechanistic and prognostic or diagnostic studies of male infertility (Layer 3)
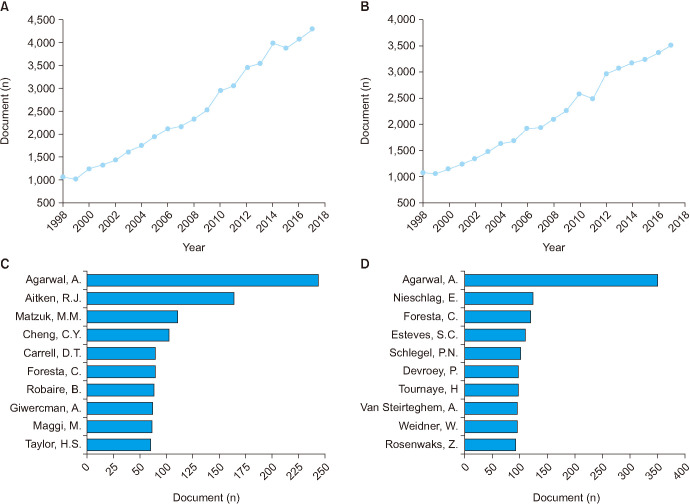
The articles published in male infertility research were further analyzed by sub-categorizing them into mechanistic and prognostic or diagnostic studies. This analysis indicates the percentage of article that contributes to understanding the basis of male infertility as well as articles with prognostic or diagnostic values. Out of 116,233 articles published on male infertility during the reporting period, 49,998 (43.02%) and 42,945 (36.95%) articles fell under the category of mechanistic studies, and prognostic or diagnostic studies respectively (Fig. 4A, 4B). Our bibliometric analysis reveals that finding the root cause as well as diagnosis have gained equal attention in male infertility research.
Fig. 4. Publication trends in mechanistic and prognostic/diagnostic studies over the past 20 years. (A) Trends in the number of articles on mechanistic studies of male infertility by year. (B) Top scientists in the research area of mechanistic studies of male infertility during the period 1998–2017. (C) Trends in the number of articles on prognostic or diagnostic studies of male infertility by year. (D) Top scientists involved in prognostic or diagnostic studies of male infertility during the period 1998–2017.
We also analyzed the results at the contributor level. Fig. 4C, 4D shows the top scientists working in mechanistic and prognostic/diagnostic studies of male infertility respectively. Agarwal, A. dominated the publications in both categories, which is in line with the Layer 1 results. Other authors dominating mechanistic studies further include Aitken, R.J., Matzuk, M.M., Cheng, C.Y., and Carrell, D.T. However, a different set of authors dominate prognostic and diagnostic studies, specifically Nieschlag, E., Foresta, C., Esteves, S.C., and Schlegel, P.N. in the top five.
4. Publication trend of omics studies in male infertility (Layer 4)
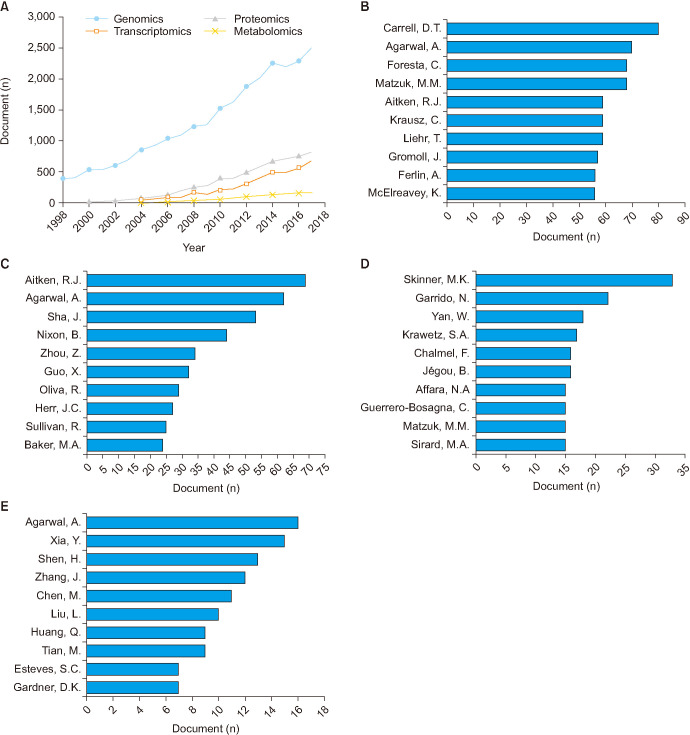
Bibliometric analysis revealed an increased number of publications in genomics from 398 (1998) to 2,545 (2017) (Fig. 5A). In the field of proteomics, a significant increase in the number of publication from 3 (1999) to 833 (2017) was observed (Fig. 5A). However, publication record on transcriptomics and metabolomics indicated the emergence of these specific fields only from year 2001 and 2002, respectively. Since then, the number of articles in transcriptomics and metabolomics have increased from 1 to 688 and 183 (Fig. 5A). Analysis of author contribution revealed the top researchers as Carrell, D.T., Agarwal, A., and Foresta, C., in the field of genomics; Aitken, R.J., Agarwal, A., and Sha, J., in the field of proteomics; Skinner, M.K., Garrido, N., and Yan, W., in the field of transcriptomics; Agarwal, A., Xia, Y., and Shen, H., in the field of metabolomics. Top scientists contributing extensively to these emerging new generation technologies are depicted in Fig. 5B–5E.
Fig. 5. (A) Publication trends in genomics, transcriptomics, proteomics, and metabolomics of male infertility by year from 1998–2017. Top scientists in the field of genomics (B), proteomics (C), transcriptomics (D), and metabolomics of male infertility (E) research during the period 1998–2017.
5. Publication trend in ART over the past 20 years (Layer 5)
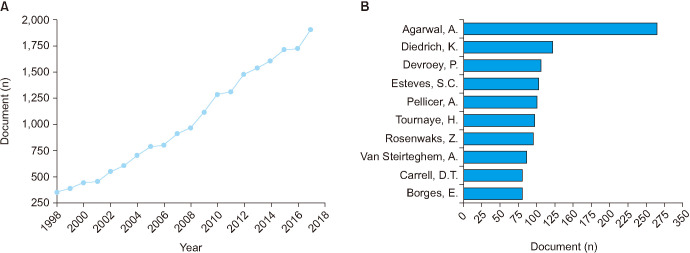
In the past 20 years, the number of articles published on ART have significantly increased from 350 (1998) to 1,912 (2017) (Fig. 6A). The top 5 journals that published articles in ART are Fertility and Sterility (n=2,054), Human Reproduction (n=1,663), Reproductive Biomedicine Online (n=832), Journal of Assisted Reproduction and Genetics (n=799), and Theriogenology (n=296). INSERM, Cleveland Clinic Foundation, and Harvard Medical School were the top 3 institutions actively involved in ART research (data not shown). Analysis of author contribution revealed that Agarwal, A., Diedrich, K., Devroey, P., Esteves, S.C., and Pellicer, A. were the specialists in the field of ART related research (Fig. 6B).
Fig. 6. (A) Publication trend in assisted reproductive technology (ART) by year from 1998–2017. (B) Top scientists in the field of ART related research during the period 1998–2017.
DISCUSSION
Bibliometric analysis provides an idea about the progress of research and contributions of the researcher in a specified field [14]. The Scopus literature database is an ideal platform for bibliometric analysis (https://www.scopus.com/). Recently, Zhang et al [9] reported an overall increasing trend in male infertility research from 1995 to 2014. However, the bibliometric data were retrieved with a single set of keywords using the Web of Science database. Until now, articles on bibliometric analysis of male infertility research have provided only a broader picture, which excludes crucial aspects, such as prognosis/diagnosis and new generation omics technologies. In this context, we propose a novel model (Funnel Model) that enables deeper insight into male infertility research (Fig. 1). The Funnel Model allows the articles retrieved under the broad category of ‘Male Infertility’ to be further sub-categorized using specific keywords to study the distribution of articles into respective sub-topics. The Funnel Model serves as a roadmap for analysis of male infertility research trends, and its applications are detailed in Table 5.
Table 5. Applications of the Funnel Model.
| Applications of the Funnel Model |
|---|
| • Projects the overall trends in male infertility research |
| • Identifies the relative distribution of publications in various subareas of male infertility research |
| • Identifies the areas that have gained more/less attention over a given period of time |
| • Identifies the prolific authors in different areas of male infertility research |
| • Identifies the top institutions in each subcategory of male infertility research |
| • Identifies the research groups on the basis of their research approaches (e.g., mechanistic, prognostic, or diagnostic) |
| • Can be applied to an individual author/research group as a self-evaluation tool |
| • To identify collaborative partners for research and inter-disciplinary opportunities |
| • To compare different time periods and reveal the relative growth in male infertility research |
There has been an exponential increase in male infertility research over the last 20 years. An increased incidence of male infertility accompanied by a significant decline in semen quality over the past decades [2,15,16] clearly explains the accelerated demand-driven research on male infertility in order to identify the causes and development of effective treatment options. Male infertility arises from a variety of health problems, including genetic causes, organic pathology, and lifestyle or environmental factors that can negatively influence the male reproductive functions [17,18]. It is estimated that 20% to 50% of male infertility are idiopathic with no known underlying causes (UMI) [19]. However, well defined acquired etiologies include varicoceles, urogenital infections, ED, testicular cancer, and hypogonadism [18,19,20]. Further risk factors include obesity and MetS, poor lifestyle choice and occupational exposures. These well-defined etiologies laid the platform for the keywords used in the secondary analysis (Layer 2). Our analysis revealed that in the past 20 years, testicular cancer, obesity and MetS, and azoospermia received greater research interest, whereas ED and UMI received lesser attention in male infertility research.
Further, we analyzed the reason(s) why some specific areas have gained greater attention over the others in the past 20 years. Testicular cancer is the most common malignancy in young male of reproductive age (15–34 years), and its incidence has doubled in the last 30 years in industrialized regions [21]. Furthermore, this increased incidence has been negatively correlated with a reduction in semen quality and fertility [21]. Aligned with the overall results, the major globalized nations USA, UK, and China were found to be the top three countries in testicular cancer publications (data not shown). Our analysis reflects a dramatic increase in publications per year in the last 20-year period (413%), indicating the increased incidence and clinical importance of testicular cancer. Obesity and MetS are of significant public health concerns, and their prevalence has increased exponentially in recent decades [22], which was reflected in the dramatic increase of articles (707%) published in this field. Significant number of research articles on obesity and MetS is indeed relevant, as their negative impact on male reproduction has been established with poorly understood mechanisms and therapeutic options [23,24,25,26]. Azoospermia, the absence of spermatozoa in the ejaculate, is a relatively common infertility finding, identified in 15% of infertile males [27]. As a common feature of male infertility, the relatively high attention on this affliction is understandable.
Conversely, ED and UMI have received lesser attention over the 20 years as reflected by the relatively low number of articles published in these fields. ED, the inability to maintain sufficient penile erection for sexual intercourse, is a multifactorial concern involving ageing, microvasculature disease, neuropathy, metabolic, immune and endocrine dysregulation, prostate pathology and a major psychogenic component in many cases [28,29]. Hence, ED is a subject of broader multidisciplinary concern, and it is not clear why there are relatively fewer publications. It is possible that publications on ED might be more related to sexual dysfunction rather than a sub-area of male infertility. However, this field was recorded to have the most significant increase in the number of articles in 2017 compared to 1998 (765%), reflecting the recent understanding and importance of ED in male infertility. In light of the relative common occurrence of UMI, our bibliometric results showed a relatively weak interest in this topic, even though there is a significant need for understanding the co-morbidities, mechanisms and management options for UMI. As found for ED, though the number of publications is fewer, the significant increase in percentage (429%) in the last 20 years suggests that UMI is gaining importance in male infertility research.
Mechanistic and prognostic/diagnostic studies are both broad and critical areas of biomedical research. Mechanistic studies aim to investigate and understand the physiological and pathophysiological processes associated with normal function and disease pathways [30]. As discussed above, there are numerous poorly understood clinical concerns including testicular cancer, obesity & MetS, and UMI. Prognostic studies aim to understand the predictive and risk factors in outcomes of disease process for the general or specific population, in which clinical decision making and the selection of appropriate management options can be guided by evidence [31]. Similarly, studies investigating diagnostic tools and protocols in clinically defined diseases are critical for the assessment of patients. Diagnostic studies examine the efficacy of a protocol to diagnose or rule out disease, with a focus specifically on false positives and false negative rates [32]. The prognostic and diagnostic considerations in more complex pathologies require further focus, such as UMI, obesity and MetS, and many cases of oligozoospermia. Our results indicate that prognostic and mechanistic studies have significantly increased in parallel over the last 20 years, with approximately equal focus in the literature. This emphasizes the fact that researchers in male infertility are equally interested in finding the reason(s) associated with male infertility as well as the prognosis and diagnosis of male infertility.
Omics technologies are an innovative and promising approach to identify new biomarkers of male infertility [33]. Integration of omics data with computational bioinformatic analysis helps in the understanding of the molecular mechanisms at the subcellular level [34]. Genomics was the first omics tool used to detect and screen genetic abnormalities. Later, introduction of transcriptomics was able to identify the defects at the level of transcription and generation of transcript mRNAs. Emergence of other omics tools such as proteomics and metabolomics have revolutionized the male infertility research using advanced and sophisticated instruments [35]. The field of genomics has significantly expanded over the past 20 years, and it is reflected in an increased number of publications in this field. Conversely, the publication trends suggest that proteomics research is currently in a growing phase while transcriptomics and metabolomics are still in an emerging phase. In spite of advancements in technology, fewer publications in omics (transcriptomics, metabolomics, and proteomics) indicate the dearth use of advanced techniques by the researchers. This may be due to the limited accessibility of sophisticated instruments and knowledge about the high throughput tools. Also, without computational analysis, omics data are valueless. Since all the omics data undergo bioinformatics analysis using critical softwares, expertise with bioinformatics skills and knowledge of reproductive biology limits this type of research across the world. However, increased collaborations between the institutes and consortiums may enhance research by using newer generation platforms that would help in identifying non-invasive bio-markers and improvising treatment strategies for male infertility.
ART is the most effective treatment option available for various male infertility issues. A total of five million births all over the world and around 2% to 4% of births in developed countries are the results of ART [36,37]. In this regard, an exponential increase in ART research over the past 20 years is well-understood. Our analysis revealed that the relative contribution from ART (17.81%) is less than that of publications on mechanistic (43.02%) and prognostic/diagnostic studies (36.95%), which emphasizes the need for more research directed towards ART. It is a very potent research area that needs to expand its horizon as ART is primarily directed towards solving infertility related issues irrespective of etiology.
Overall, our study proposes a model that could serve as a roadmap for bibliometric analysis of male infertility research trends. However, the search results retrieved using this model were based on the keywords rather than the findings in the published articles, which is one the limitations of this study. Furthermore, extensive analysis on each sub-areas of male infertility research as well as inter-layer and inter-zone analysis could be conducted in future.
CONCLUSIONS
The bibliometric analysis using the Funnel Model revealed an exponential increase in male infertility research over the past 20 years, in which testicular cancer, obesity and MetS, and azoospermia were the predominant research areas, while lesser focused areas were ED and UMI. Prognostic/diagnostic and mechanistic studies on male infertility research have significantly increased in parallel over the last 20 years, with almost equal focus in the literature. Balanced growth of these sub-categories suggests that male infertility research is on a reliable and progressive direction. However, an integrated and steep escalation in the field of omics and ART research appears to be a pre-requisite for the development of future diagnostic and therapeutic strategies for male infertility.
ACKNOWLEDGEMENTS
The authors thank Ahmad Majzoub, MD (Qatar), Chak-Lak Cho, MD (Hong Kong), Damayanthi Durairajanayagam, PhD (Malaysia), and Trevor G Cooper, PhD (Hong Kong) for review of our manuscript and offering helpful comments. The authors also thank Ms. Bernastine Buchanan, Center for Medical Art & Photography, Cleveland Clinic, for her assistance in preparing the figures for this study.
Footnotes
Conflict of Interest: The authors have nothing to disclose.
- Conceptualization: AA, SB, RH.
- Data curation: Pushparaj PNP, SB.
- Formal analysis: all authors.
- Supervision: AA.
- Writing-original draft: SB, MKPS, PNP, KL, RH.
- Writing-review & editing: all authors.
- Approval of the final manuscript: all authors.
Data Sharing Statement: The data analyzed for this study have been deposited in HARVARD Dataverse and are available at https://doi.org/10.7910/DVN/CQZTXH.
References
- 1.Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21:411–426. doi: 10.1093/humupd/dmv016. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015;13:37. doi: 10.1186/s12958-015-0032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swan SH, Elkin EP. Declining semen quality: can the past inform the present? Bioessays. 1999;21:614–621. doi: 10.1002/(SICI)1521-1878(199907)21:7<614::AID-BIES10>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 4.Sengupta P, Nwagha U, Dutta S, Krajewska-Kulak E, Izuka E. Evidence for decreasing sperm count in African population from 1965 to 2015. Afr Health Sci. 2017;17:418–427. doi: 10.4314/ahs.v17i2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rondanelli M, Perna S, Peroni G, Guido D. A bibliometric study of scientific literature in Scopus on botanicals for treatment of androgenetic alopecia. J Cosmet Dermatol. 2016;15:120–130. doi: 10.1111/jocd.12198. [DOI] [PubMed] [Google Scholar]
- 6.Maula AW, Fuad A, Utarini A. Ten-years trend of dengue research in Indonesia and South-east Asian countries: a bibliometric analysis. Glob Health Action. 2018;11:1504398. doi: 10.1080/16549716.2018.1504398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.González-Alcaide G, Aleixandre-Benavent R, Navarro-Molina C, Valderrama-Zurián JC. Coauthorship networks and institutional collaboration patterns in reproductive biology. Fertil Steril. 2008;90:941–956. doi: 10.1016/j.fertnstert.2007.07.1378. [DOI] [PubMed] [Google Scholar]
- 8.Aleixandre-Benavent R, Simon C, Fauser BC. Trends in clinical reproductive medicine research: 10 years of growth. Fertil Steril. 2015;104:131–137.e5. doi: 10.1016/j.fertnstert.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Xiao F, Lu S, Song J, Zhang C, Li J, et al. Research trends and perspectives of male infertility: a bibliometric analysis of 20 years of scientific literature. Andrology. 2016;4:990–1001. doi: 10.1111/andr.12204. [DOI] [PubMed] [Google Scholar]
- 10.Makkizadeh F, Sa'adat F. Bibliometric and thematic analysis of articles in the field of infertility (2011–2015) Int J Reprod Biomed (Yazd) 2017;15:719–728. [PMC free article] [PubMed] [Google Scholar]
- 11.Egea RR, Puchalt NG, Escrivá MM, Varghese AC. OMICS: current and future perspectives in reproductive medicine and technology. J Hum Reprod Sci. 2014;7:73–92. doi: 10.4103/0974-1208.138857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sweileh WM. Research trends on human trafficking: a bibliometric analysis using Scopus database. Global Health. 2018;14:106. doi: 10.1186/s12992-018-0427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hirsch JE. An index to quantify an individual's scientific research output. Proc Natl Acad Sci U S A. 2005;102:16569–16572. doi: 10.1073/pnas.0507655102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal A, Durairajanayagam D, Tatagari S, Esteves SC, Harlev A, Henkel R, et al. Bibliometrics: tracking research impact by selecting the appropriate metrics. Asian J Androl. 2016;18:296–309. doi: 10.4103/1008-682X.171582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992;305:609–613. doi: 10.1136/bmj.305.6854.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharlip ID, Jarow JP, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. Best practice policies for male infertility. Fertil Steril. 2002;77:873–882. doi: 10.1016/s0015-0282(02)03105-9. [DOI] [PubMed] [Google Scholar]
- 17.Dada R, Thilagavathi J, Venkatesh S, Esteves SC, Agarwal A. Genetic testing in male infertility. Open Reprod Sci J. 2011;3:42–56. [Google Scholar]
- 18.Esteves SC, Hamada A, Kondray V, Pitchika A, Agarwal A. What every gynecologist should know about male infertility: an update. Arch Gynecol Obstet. 2012;286:217–229. doi: 10.1007/s00404-012-2274-x. [DOI] [PubMed] [Google Scholar]
- 19.Hamada A, Esteves SC, Nizza M, Agarwal A. Unexplained male infertility: diagnosis and management. Int Braz J Urol. 2012;38:576–594. doi: 10.1590/s1677-55382012000500002. [DOI] [PubMed] [Google Scholar]
- 20.Hamada A, Esteves SC, Agarwal A. The role of contemporary andrology in unraveling the mystery of unexplained male infertility. Open Reprod Sci J. 2011;4:27–41. [Google Scholar]
- 21.Walsh TJ, Croughan MS, Schembri M, Chan JM, Turek PJ. Increased risk of testicular germ cell cancer among infertile men. Arch Intern Med. 2009;169:351–356. doi: 10.1001/archinternmed.2008.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Potenza MV, Mechanick JI. The metabolic syndrome: definition, global impact, and pathophysiology. Nutr Clin Pract. 2009;24:560–577. doi: 10.1177/0884533609342436. [DOI] [PubMed] [Google Scholar]
- 23.Hammoud AO, Gibson M, Peterson CM, Meikle AW, Carrell DT. Impact of male obesity on infertility: a critical review of the current literature. Fertil Steril. 2008;90:897–904. doi: 10.1016/j.fertnstert.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 24.Du Plessis SS, Cabler S, McAlister DA, Sabanegh E, Agarwal A. The effect of obesity on sperm disorders and male infertility. Nat Rev Urol. 2010;7:153–161. doi: 10.1038/nrurol.2010.6. [DOI] [PubMed] [Google Scholar]
- 25.Leisegang K, Bouic PJ, Menkveld R, Henkel RR. Obesity is associated with increased seminal insulin and leptin alongside reduced fertility parameters in a controlled male cohort. Reprod Biol Endocrinol. 2014;12:34. doi: 10.1186/1477-7827-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lotti F, Corona G, Vignozzi L, Rossi M, Maseroli E, Cipriani S, et al. Metabolic syndrome and prostate abnormalities in male subjects of infertile couples. Asian J Androl. 2014;16:295–304. doi: 10.4103/1008-682X.122341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bieniek JM, Kashanian JA, Deibert CM, Grober ED, Lo KC, Brannigan RE, et al. Influence of increasing body mass index on semen and reproductive hormonal parameters in a multi-institutional cohort of subfertile men. Fertil Steril. 2016;106:1070–1075. doi: 10.1016/j.fertnstert.2016.06.041. [DOI] [PubMed] [Google Scholar]
- 28.Yafi FA, Jenkins L, Albersen M, Corona G, Isidori AM, Goldfarb S, et al. Erectile dysfunction. Nat Rev Dis Primers. 2016;2:16003. doi: 10.1038/nrdp.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collica S, Pederzoli F, Bivalacqua T. The epidemiology and pathophysiology of erectile dysfunction and the role of environment. In: Sikka SC, Hellstrom WJG, editors. Bioenvironmental issues affecting men's reproductive and sexual health. London: Elsevier/Academic Press; 2018. pp. 439–455. [Google Scholar]
- 30.Aickin M. Conceptualization and analysis of mechanistic studies. J Altern Complement Med. 2007;13:151–158. doi: 10.1089/acm.2006.6341. [DOI] [PubMed] [Google Scholar]
- 31.Mak K, Kum CK. How to appraise a prognostic study. World J Surg. 2005;29:567–569. doi: 10.1007/s00268-005-7914-x. [DOI] [PubMed] [Google Scholar]
- 32.Mallett S, Halligan S, Thompson M, Collins GS, Altman DG. Interpreting diagnostic accuracy studies for patient care. BMJ. 2012;345:e3999. doi: 10.1136/bmj.e3999. [DOI] [PubMed] [Google Scholar]
- 33.Kovac JR, Pastuszak AW, Lamb DJ. The use of genomics, proteomics, and metabolomics in identifying biomarkers of male infertility. Fertil Steril. 2013;99:998–1007. doi: 10.1016/j.fertnstert.2013.01.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sinha A, Singh V, Yadav S. Multi-omics and male infertility: status, integration and future prospects. Front Biosci (Schol Ed) 2017;9:375–394. doi: 10.2741/s493. [DOI] [PubMed] [Google Scholar]
- 35.Panner Selvam MK, Agarwal A. Update on the proteomics of male infertility: a systematic review. Arab J Urol. 2017;16:103–112. doi: 10.1016/j.aju.2017.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poenicke K, Grunewald S, Glander H, Paasch U. Sperm selection in assisted reproductive techniques. In: Rao KA, Agarwal A, Srinivas MS, editors. Andrology laboratory manual. Bengaluru: Jaypee Brothers Medical Pub.; 2010. pp. 173–187. [Google Scholar]
- 37.Centers for Disease Control and Prevention; American Society for Reproductive Medicine; Society for Assisted Reproductive Technology. 2012 Assisted reproductive technology: fertility clinic success rates report. Atlanta: US Department of Health and Human Services; 2014. [Google Scholar]