Abstract
Prostate cancer has become the second leading cancer in men worldwide. Androgen plays an important role in normal functioning, development, and differentiation of the prostate, and thus is considered to be the most powerful candidate that mediates reactive oxygen species (ROS) balance in the prostate. The elevation of ROS has been associated with the progression and development of this disease. Conventional therapy has shown a high cure rate in patients with localized prostate cancer. Despite the patients respond favorably initially, this therapy fails to response in the advanced stage of the diseases even in the absence of androgens. Indeed, the onset and progression of prostate cancer could be prevented by changing dietary habits. Much information indicates that oxidative stress and prostate cancer can be modulated by dietary components rich in antioxidants. While there is substantial evidence to suggest an association between prostate cancer risk and ROS-mediated oxidative stress; therefore, the interactions and mechanisms of this phenomenon are worth to discuss further. This review aimed to discuss the mechanisms of action of oxidative stress involved in the progression of prostate cancer. We also highlighted how some of the vital dietary components dampen or exacerbate inflammation, oxidative stress, and prostate cancer. Overall, the reported information would provide a useful approach to the prevention of prostate cancer.
Keywords: Inflammation, Oxidative stress, Phytochemicals, Prostate, Reactive oxygen species
INTRODUCTION
Prostate cancer has become the second leading cancer in men globally [1], accounting for 1.3 million new cases in 2018 [2]. Prostate cancer was intimately linked to androgen and androgen receptor [3]. Suppression of testosterone is considered one of the most effective approaches to treat metastatic prostate cancer. When serum prostate-specific antigen (PSA) was used for screening in asymptomatic men, the age-adjusted incidence rates of prostate cancer have increased dramatically [4]. Patients with advanced prostate cancer are often treated with endocrine therapy including maximal androgen blockade (anti-androgens combined with castration) and classical androgen deprivation (orchiectomy or luteinizing hormone-releasing hormone agonists) [5]. Despite nearly 70% to 80% of patients respond favorably for several months or years, progression to castration-resistant disease is nearly universal [6]. Of importance, androgen ablation is the mainstay of therapy for progressive prostate cancer. Nonetheless, majority of the patients fail to respond to this therapy and lastly die due to the recurrent androgen-independent prostate cancer [7].
Elevation of cellular reactive oxygen species (ROS) and impaired protective mechanisms have been associated with increased prostate cancer risk [8]. ROS are generated continuously in the body through immune function, oxidative metabolism, and mitochondrial bioenergetics. ROS are usually present in the form of superoxide anion, hyphochlorous acid, hydrogen peroxide, singlet oxygen, hypochlorite, hydroxyl radical, and lipid peroxides, which are produced during cells progression, growth, death, and differentiation [9]. They can bind to the protein, membrane lipids, nucleic acid, enzymes, and other small molecules. Increased oxidative stress has been found as a predominant risk factor in the initiation and progression of prostate cancer [10]. Animal models and cell culture experiments have reported the mechanisms that implicate prostate cancer are complex and involve many cell signaling pathways [11]. Oxidative free radicals are caused by several factors including regulating androgens, delaying in the recruitment of p53, and inflammation. Specifically, it has been suggested that serum androgens increase ROS accumulation and production in prostate cancer cells [12].
Furthermore, compelling evidence shows the adverse outcomes of excessive consumption of saturated fat and refined carbohydrates [13]. The effect of oxidative stress has been associated with the absolute quantity and the type of macronutrients consumed [14]. Both of these aspects favor to oxidative stress and may contribute the development of prostate cancer [15]. Indeed, the mechanisms of action and interactions underlying prostate cancer risk and ROS-mediated oxidative stress are complex and worth to discuss further. Hence, this review aimed to discuss the biological mechanism of oxidative stress involved in the progression of prostate cancer. We also highlighted how some of the vital dietary components dampen or exacerbate inflammation, oxidative stress, and prostate cancer. Overall, the reported information would provide a useful approach to the prevention of prostate cancer.
MAIN BODY
1. Pathophysiology of oxidative stress
According to the oxidative stress hypothesis, oxidative damage can be induced by unrestricted production of ROS as well as other oxidants, for instance, reactive lipid species and reactive nitrogen species (RNS) [16]. In general, all aerobic cells produced reactive oxygen and nitrogen species (RONS); however, increased ROS is associated with the progression and onset of aging [17]. Despite ROS production may not play a crucial role in aging, it is more likely to provoke aging via oxidative damage and interaction with mitochondria [18].
In general, there are two RONS sources, namely endogenous and exogenous. The redox imbalance is more likely induced by the net effect of low antioxidative defense systems and thus constantly produces endogenous RONS, such as angiotensin II, lipoxygenase, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, and myeloperoxidase [19]. Among all these sources, NADPH oxidase is the common source of radical superoxide anion (O2˙) that is generated by reducing one-electron of molecular oxygen. Subsequently, O2˙ is dismutated by superoxide dismutase (SOD) into hydrogen peroxide (H2O2). Although H2O2 is not a free radical, it is able to produce reactive ROS hydroxyl ion (OH˙) via Haber–Weiss or Fenton reaction. Nitric oxide (NO) is produced from L-arginine by three predominant isoforms of nitric oxide synthase (NOS), namely inducible nitric oxide synthase (iNOS), neuronal NOS, and epithelial NOS. The O2 may interact with NO to form peroxynitrite (ONOO−) [19].
Exogenous and endogenous RONS may cause oxidative modifications of several cellular macromolecules, including DNA, proteins, lipids, and carbohydrates [19]. A study reported by Barreiro [20] showed that protein carbonyl is produced by Fenton reaction of oxidants with threonine, proline, arginine, and lysine residues of the protein side chains. The carbonyl groups may produce when aldehydic lipid oxidation products interacting with histidine, cysteine, and lysine residues known as Michael-addition reactions [21]. While, some of the RNS interacts with tyrosine residues may trigger the formation of nitrotyrosine [21]. In addition, the amino groups of arginine and lysine bind with carbonyl groups of carbohydrate can also produce advanced glycation end products, such as glucosepane, pentosidine, and hydroimidazolone [22].
2. Oxidative stress and prostate cancer
Changes in the ratios of androgenic hormones and androgens as well as paracrine/autocrine growth stimulatory factors including insulin growth factor (IGF) binding proteins and growth inhibitory factors, for instance, IGF, nerve growth factor, epidermal growth factor, and transforming growth factor β are implicated in abnormal prostatic growth. Intriguingly, physiological activation of the androgen receptor has been demonstrated to promote ROS production [23]. Because aging is linked to reduced free radical scavenging enzymes and intracellular antioxidant levels, and androgen stimulation in prostate cancer cells; thereby, disrupting the balance of antioxidant-prooxidant levels. Such finding implies the androgen activation existing in prostate cancer cells could be attributed to the mitochondrial DNA mutation and aging. Intracellular redox balance is primarily due to cyclic oxidation and reduction of glutathione both in the mitochondria and cytoplasm of the cells. Glutathione is synthesized in the cytosol, and plays a critical role to prevent the mitochondria from the detrimental effects of ROS produced by electron transport [24]. The previous study has revealed that glutathione peroxidase enzymes catalyze the neutralization of peroxide through the glutathione redox system [25]. In support of this, circulating expression of glutathione peroxidase in the prostate tissue and plasma are markedly reduced in patients with prostate cancer. In this regard, increased loss of glutathione may change the intracellular environment to a prooxidant state and thereby caused prominent changes in gene expression, which is ultimately evolving into a malignant state [26].
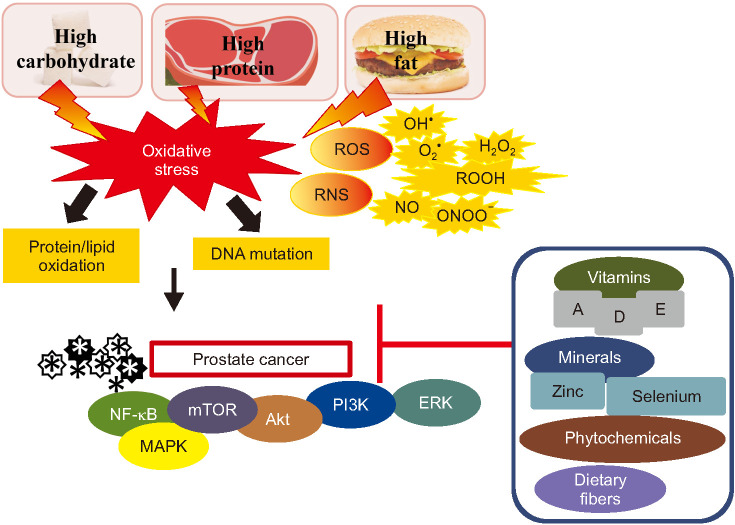
Chronic administration of dihydrotestosterone (DHT) and estradiol promotes proinflammatory cytokines within the prostate in rats. DHT is synthesized by 5α-reductase in the prostate, was shown a potent effect due to its high affinity to the androgen receptor [3]. The androgen receptor interacts with androgen receptor elements in the promoter regions and thus regulates cellular proliferation [3]. In this regard, inappropriate activation of estrogen receptor alpha signaling concomitantly with the elevation of testosterone has been demonstrated to trigger prostate cancer and prostate hyperplasia in mice [27]. Fig. 1. shows the effect of oxidative stress on prostate cancer.
Fig. 1. The effect of oxidative stress on prostate cancer. Consumption of high carbohydrate, high protein, and high-fat diets may induce oxidative stress. Oxidative damage is not only induced by the unrestricted reactive oxygen species (ROS) production but also due to other oxidants, such as reactive nitrogen species (RNS). Overproduction of reactive species, including hydroxyl radical (·OH), superoxide anion (O2˙), hydrogen peroxide (H2O2), hydroperoxides (ROOH), nitric oxide (NO), and peroxynitrite (ONOO−) may lead to protein/lipid oxidation and DNA mutation. Elevation of ROS can result in the progression and development of prostate cancer. The onset and progression of prostate cancer could be prevented by changing dietary habits by modulating nuclear factor-kappa B (NF-κB), mammalian target of rapamycin (mTOR), mitogen-activated protein kinase (MAPK), Akt, extracellular signal-regulated kinase (ERK), and phosphoinositide 3-kinases (PI3K) signaling pathways. Consumption of diet high in vitamins A, D, and E, minerals (selenium and zinc), phytochemicals, and dietary fibers may reduce the risk of prostate cancer.
3. Macronutrients-mediated oxidative stress
1) High carbohydrates
Emerging evidence revealed that high consumption of macronutrients can increase oxidative stress and thus trigger inflammation [9]. Dietary carbohydrate is crucial to discuss here because it may lead to the long-term consequences of nutritionally mediated oxidative stress [28]. Intakes of carbohydrates have drawn a great deal of interest among researchers due to an association between high glycemic load (GL) or glycemic index diet with prostate cancer [29]. High GL diet has been characterized as a common characteristic of Western culture, in which they are high in refined carbohydrates and added sugars [30]. Data from an earlier study have revealed that insulin is a proliferation factor for prostate cancer; conversely, decreased carbohydrates intake may slow down prostate cancer proliferation and reduce serum insulin [31]. Despite study has found a positive relationship between carbohydrate and prostate cancer, not all data showed such a link. A recent meta-analysis study did not identify an association between prostate cancer risk and carbohydrate intake [29].
Intake of carbohydrates can disturb the insulin secretion and glycemic response of an individual, in which the effect of blood glucose response depends on the amount of carbohydrates ingested [32]. Hyperinsulinemia is linked to various cancers, including prostate cancer. Insulin resistance leads to reduced insulin sensitivity in peripheral tissues, and thereby caused in hyperinsulinemia. Insulin is a potent growth factor linked to an increase of prostate tumor proliferation [33]. Higher grade of prostate tumors was shown to have high expression of insulin receptor-A (IR-A) isoform and increased number of IR both in vivo and in vitro studies [34,35]. Stimulation of IR upregulates both mitogen-activated protein (MAP)/extracellular signal-regulated kinase and phosphoinositide 3-kinases/Akt/mammalian target of rapamycin (PI3K/Akt/mTOR) signaling pathways and subsequently leading to inhibiting of apoptosis and promoting cell migration and proliferation [33].
2) High animal-based protein
Animal meat is a source of protein in the Western diet, composes of 20% of daily fat, 40% of daily protein, and 15% of daily energy intake [36]. Excessive protein intake could increase ROS production in the digestive gland, impair oxidation of amino acids in the digestive system, and promote instability of antioxidants. Several metabolites are produced such as hydrogen sulfide (H2S) and ammonia (NH3), compounds are known to induce toxicity of the mucosa during fermentation of excessive proteins in the gut. Although meats are rich in dietary protein, it can be a source of mutagens due to the presence of heterocyclic amines (HCA) and polycyclic aromatic hydrocarbons (PAH) during high-temperature grilling and cooking and N-nitroso compounds in processed meats [37]. Evidence from the case-control study demonstrated the consumption of cooked red meat potentially leads to advanced prostate cancer risk [38]. This finding indicates the metabolic changes induced by red meat are more likely initiated by the formation of carcinogenic PAH and HCA.
During cooking, free Fe2+ is markedly increased in uncured meat [39]. However, nitrite curing inhibits the phosphorylation of heme-Fe via modulation of the porphyrin ring [39]. Indeed, heat treatment can lead to a reduction of the antioxidant enzyme, for instance, glutathione peroxidase, and produces oxygen from oxymyoglobin, which subsequently leads to the production of H2O2. When the oxidative processes are initiated, free Fe2+ catalyzes the Fenton reaction [40]. Taken together, nitrite curing of meat in the colonic was vitally important because it was related to a low amount of malondialdehyde but doubled heptanal levels and proportionally increased of hydroxy-2-nonenal levels in the cooked and overcooked meats [39].
3) High fat consumption
When caloric intake surpasses energy expenses, the substrate promotes in citric acid cycle which increases the production of ROS. Administration of high-fat diet promotes the production of ROS, along with the elevation of tumor necrosis factor-alpha (TNF-α) and adipokine secretion, thereby resulting in chronic inflammation [41]. Animal feeding with a high-fat diet increased metastasis rates and local invasion of prostate cancer in transgenic adenocarcinoma of mouse prostate mice, suggesting the circulating cytokine and adipokine alterations in response to excess adipose tissue deposition induced by a high-fat diet may enhance prostate cancer progression [42]. Data from in vivo study also revealed that a high-fat diet accelerates the proliferation of prostate tumors and increased M2/M1 macrophage ratio and myeloid-derived suppressor cells fraction via interleukin (IL)-6/phospho-signal transducer and activator of transcription 3 (pSTAT3) signaling [43].
Mitochondrial β-oxidation of free fatty acids are related to the conversion of oxidized cofactors (FAD and NAD+) into reduced cofactors, namely FADH2 and NADH. Subsequently, it was reoxidized and restored back into FAD and NAD+ by the mitochondrial respiratory chain. Through the process of reoxidation, FADH2 and NADH transfer the electrons to the first complexes of the respiratory chain. This electron shift to cytochrome c oxidase and interact with protons and oxygen to form water. The intermediates may bind with oxygen to generate superoxide anion and produce ROS. In this regard, sustained chronic fat consumption induces mitochondrial β-oxidation of free fatty acids and resulted to excess electron flow using cytochrome c oxidase, which promotes ROS levels. High-fat diet-induced ROS may promote proinflammatory signaling and stimulate nuclear factor-kappa B (NF-κB) transcriptional factor, and hence inducing NF-κB-dependent proinflammatory molecules, for instance, TNF-α, interferon-γ, and iNOS [44].
4. Modulation of prostate cancer by dietary components
1) Vitamins
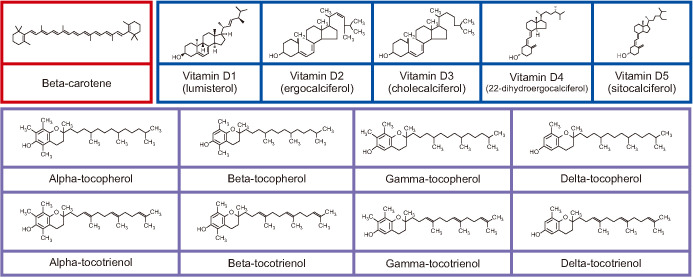
Vitamins are essential for normal metabolism. Most of the vitamins cannot be synthesized by humans, except vitamin D; therefore, they need to be consumed from the diet to prevent metabolism disorders [45]. The protective effect of vitamins in prostate cancer has been widely demonstrated in clinical trials and laboratory experiments [46,47], in which most of the data exists for vitamins D, A or provitamin A carotenoids, and E. Vitamin E (four tocotrienols and four tocopherols) (Fig. 2) is a fat-soluble vitamin found naturally in food. Both tocotrienols and tocopherols are divided into α-, β-, γ-, and δ-based on the hydroxyl and methyl substitution in their phenolic rings [48]. The predominant biological roles of vitamin E in response to prostate cancer have been reported and the positive impact of oxidative damage has been evaluated. The proposed aspects of vitamin E including inhibiting cell proliferation, cell adhesion, and protein kinase C activity, improving immunity, and modulating anti-angiogenic and antioxidation properties [49]. Data from a cohort study (18,541 controls and 11,239 cases) revealed that α-tocopherol reduces the risk of prostate cancer [50]. These findings are in line with an earlier study reported by Antwi et al [51], who found that high α-tocopherol levels are negatively linked to serum PSA concentrations in patients with recurrent prostate cancer. Kyriakopoulos et al [52] further revealed that APC-100, an antioxidant moiety of α-tocopherol, has shown the median progression-free survival of 2.8 months in patients with castrate-resistant prostate cancer. Intriguingly, several studies have demonstrated that vitamin E increased prostate cancer. Evidence from National Institutes of Health (NIH)-AARP Diet and Health Study revealed that a high frequency of vitamin E (>7 times/wk) increased the risk of prostate cancer [53]. The study further showed that supplementation of vitamin E (800 IU/d) was linked to the prostate cancer risk, regardless of frequency. High levels of α-tocopherol in plasma have also been related to high-grade prostate cancer [54]. Although the data show a positive relationship between vitamin E and prostate cancer, several large population studies showed null findings in relation to prostate cancer and benign prostatic hyperplasia (BPH) [55,56].
Fig. 2. Molecule structures of beta-carotene, vitamin D including lumisterol (D1), ergocalciferol (D2), cholecalciferol (D3), 22-dihydroergocalciferol (D4), and sitocalciferol (D5), and vitamin E congeners including tocopherols (α-tocopherol, β-tocopherol, γ-tocopherol, and δ-tocopherol) and tocotrienols (α-tocotrienol, β-tocotrienol, γ-tocotrienol, and δ-tocotrienol).
Vitamin A or provitamin A carotenoids play a critical role in maintaining healthy vision [57]. Carotenoids (Fig. 2) are naturally organic pigments produced in the fungi, bacteria, and plastids of algae and plants. In general, carotenoids absorb wavelengths 400–550 nm, thereby the compounds appear in red, orange, or yellow color. Carotenoids are not only served as an efficient radical scavenger but also exerted anticancer properties by regulating cell signaling pathways, improving immune system, and modulating cell differentiation, apoptosis, and cell cycle [58]. Vitamin A such as retinol exerts antineoplastic properties including suppression of cellular growth and induction of apoptosis [59]. Nonetheless, Peehl and Feldman [59] revealed that retinoids enhanced tumor proliferation, possibly via sex steroids or insulin-like growth factor I receptor [50]. Data from Alpha-Tocopherol, Beta-Carotene Cancer Prevention (ATBC) study further demonstrated that supplementation of 20 mg β-carotene per day [60] increased the incidence of prostate cancer in men. Intriguingly, some research has emerged to suggest that carotenoids (β-cryptoxanthin, α-carotene, and β-carotene) were not linked to prostate cancer [50]. Cook et al [61] and Omenn et al [62] also demonstrated that supplementation with 30 and 50 mg β-carotene was not related to prostate cancer.
Vitamin D is a fat-soluble vitamin, consists of five isoforms including ergocalciferol with lumisterol (D1), sitocalciferol (D5), 22-dihydroergocalciferol (D4), cholecalciferol (D3), ergocalciferol (D2) (Fig. 2), and usually found in fortified food products, flour, and dairy. Vitamin D not only can be obtained from foods, it can also be synthesized by skin in response to sunlight [63]. Vitamin D is predominantly circulated as 25-hydroxyvitamin D (25(OH)D) and thus converted by 1α-hydroxylase into its active form, 1,25-dihydroxyvitamin D [1,25(OH)2D]. Adequate consumption of vitamin D is essential to regulate bone mineralization and maintain calcium homeostasis [64]. Vitamin D deficiency is linked to the development of prostate cancer. Low vitamin D intake (<20 ng/mL) was demonstrated to be a significant risk factor for the progression of prostate cancer in certain subpopulations [65]. Data from two large nested case-control studies showed that vitamin D reduced the aggressive prostate cancer [66]. In support of this, high vitamin D serum levels were also decreased the risk of prostate cancer in men [67].
High levels of 25(OH)D decrease the inflammatory markers, for instance, IL-8 and serum C-reactive protein in patients with prostate cancer [68]. Evidence from an in vitro study has suggested that 1α,25-dihydroxyvitamin D3 upregulated the expression of tumor suppressor candidate 3 (TUSC-3) in prostate cancer cells. In fact, a low level of TUSC-3 was demonstrated to correspond with poor prostate cancer prognosis in patients, and TUSC-3 silencing promotes cell proliferation and migration [69]. Intriguingly, data from ATBC study has demonstrated that high circulating 25(OH)D increased the risk of prostate cancer [70]. Such finding highlights the association of high dosages of vitamin D-binding protein in the elevation of prostate cancer among men [71]. Collectively, there are inconsistent findings supporting the clinical use of vitamins E, A, and D in delaying or preventing the progression or onset of prostate cancer, and most of the studies are limited in their duration of exposure and sample size. In particular, how vitamins may detrimental to the development of prostate cancer and whether low concentrations of vitamins can be preventive measures are warranted in a long-term study. Table 1 [50,51,52,53,54,55,56,60,61,62,65,66,67,68,70,72,73,74,75,76,77,78,79,80,81,82] shows the clinical studies of dietary components in relation to prostate cancer.
Table 1. Clinical studies conducted in some dietary components in prostate cancer.
| Dietary component | Finding | Reference |
|---|---|---|
| Vitamin E | ↓Risk of prostate cancer and aggressive disease | [50] |
| ↓PSA serum levels in recurrent prostate cancer patients | [51] | |
| Maintain stable disease and median progression-free survival of 2.8 months in patients with castrate-resistant prostate cancer | [52] | |
| ↑Risk of prostate cancer (>7 times/wk) | [53] | |
| ↑High-grade of prostate cancer | [54] | |
| No effect on prostate cancer and BPH | [55,56] | |
| Carotenoids | ↑Incidence of prostate cancer (20 mg/d) | [60] |
| Not associated with prostate cancer (30 mg or 50 mg) | [61,62] | |
| Not associated with prostate cancer | [50] | |
| Vitamin D | ↑Prostate cancer in certain subpopula-tions (<20 ng/mL) | [65] |
| ↓Aggressive prostate cancer | [66] | |
| ↓Risk of prostate cancer | [67] | |
| ↓IL-8 and CRP in patients with prostate cancer | ||
| ↓CRP in prostate cancer patients | [68] | |
| ↑Risk of prostate cancer | [70] | |
| Zinc | ↑4.36-fold of developing fatal prostate cancer | [53] |
| Selenium | ↓Prostate cancer susceptibility | [72] |
| ↓Risk of aggressive prostate cancer | [73] | |
| No effect | [74,75] | |
| Flavonoids | ↓Prostate cancer | [76] |
| Dietary fiber | ↓Total and advanced prostate cancer | [77,78,79,80] |
| No effect | [81,82] |
PSA: prostate-specific antigen, BPH: benign prostatic hyperplasis, IL: interleukin, CRP: C-reactive protein.
2) Minerals
Minerals are chemical elements required by all organisms. It facilitates the modulation of heartbeat, hormones synthesis, and bone formation. In humans, minerals can be obtained from drinking water and food. However, mineral supplements are essential for those who did not meet the daily intake of mineral [83]. Dietary minerals can be classified into two groups, namely trace minerals and macrominerals. Macrominerals such as chloride, potassium, magnesium, sodium, calcium, and phosphorus are required in large amounts by the body. Conversely, trace elements are dietary minerals that are needed in minimal levels to maintain regular cellular function, including iron, fluoride, iodine, zinc, selenium, and copper. Among all minerals stated above, zinc and selenium have been extensively studied in relation to prostate cancer. Indeed, both zinc and selenium exert antioxidant properties. Zinc serves as a cofactor for SOD enzyme, modulation of metallothionein expression, suppression of NADPH oxidase, and regulation of glutathione metabolism in the body [84]. Dietary zinc showed a protective effect in patients with advanced prostate cancer susceptibility. Dietary administration of zinc inhibits the proangiogenic and invasive capabilities of metastatic prostate cancer cells. Inhibition of Krebs cycle in normal prostate cells leading to accumulation and secretion of citrate, which is predominantly obtained via the suppression of m-aconitase, due to an accumulation of zinc in normal prostate cells [85]. High levels of zinc in the mitochondria truncate the Krebs cycle by suppressing m-aconitase and determining the peculiar metabolism of normal prostate cells [85]. It has been demonstrated that zinc concentrations are markedly decreased in prostate cancer cells [86], as well as inducing the reactivation of m-aconitase of the Kreb cycle. Besides inhibiting maconitase, zinc also induces apoptosis in prostate cancer cells via inhibition of NF-κB, stimulation of caspases cascade, and induction of the cytochrome c from the mitochondria [87]. However, several studies have demonstrated either null or/and detrimental effects of dietary zinc and prostate cancer [55,88]. Data from NIH-AARP Diet and Health Study revealed that excessive consumption of zinc was linked to a 4.36-fold increase of developing fatal prostate cancer in men (1,476 advanced and 8,765 localized cases) [53].
In addition to the effects observed in zinc, the previous study has revealed the role of selenium in relation to prostate cancer. The activity of selenium is modulated by antioxidant enzymes leading to a reduction of ROS. Changes in the physiological levels of selenium may affect the metabolic and biochemical processes in prostate cancer. Compared to BPH specimens, malignant prostate tissue has relatively low levels of selenium [89]. A meta-analysis of 17 western population-based studies demonstrated that selenium in serum levels was inversely associated with prostate cancer susceptibility [72]. Likewise, data from a meta-analysis involving 15 prospective studies (6,021 controls and 4,527 cases) found that high selenium plasma levels were linked to the reduced risk of aggressive prostate cancer [73]. Conversely, in the Italian cohort for the Procomb trial, dietary selenium for two years did not lead to any significant changes in PSA levels or prostate cancer susceptibility [74]. Data from the Phase III clinical trial showed that supplementation selenium in a concentration of 200–400 µg for 3–5 years did not lead to any adverse outcomes such as prostate cancer mortality or PSA velocity in patients with a high risk of prostate cancer [75]. Taken together, several, but not all, observational studies show that zinc and selenium may possess anti-prostate cancer properties. The preventive role of zinc and selenium against cancer is more likely due to its antioxidant activity. In this regard, there has been a tremendous interest in the study of zinc and selenium in this disease. The crucial role played by selenium and zinc is nonetheless worth study in-depth in prostate cancer.
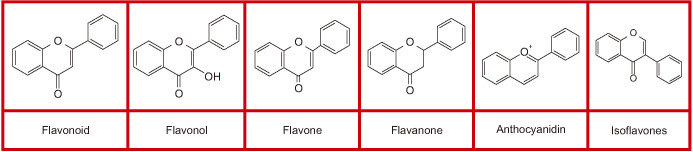
3) Phytochemicals
Phytochemicals are plant-derived non-nutritive compounds found in herbs and crops. In addition to the vitamins and minerals stated above, plants contain large amounts of phytochemicals. Polyphenols are secondary metabolites that are extensively present in vegetables, grains, traditional medicinal herbs, and fruits. Among all polyphenolic compounds, the flavonoids are the most common classes of polyphenol. Flavonoids are divided into different subgroups, namely chalcones, anthocyanins, catechins, flavanones, flavanonols, flavones, and flavonols, based on the degree of unsaturation and the carbon (Fig. 3).
Fig. 3. Molecule structures of polyphenols (flavonoid, flavonol, flavone, flavanone, anthocyanidin, and isoflavones).
Flavonoids have beneficial antioxidants and biochemical effects against cancer including prostate cancer [90]. Dietary administration of flavonoid tangeretin suppresses the growth of prostate cancer cells via downregulation of PI3K/Akt/mTOR pathways [90]. Tangeretin is found abundantly in peel of citrus fruits. Praud et al [91] found that a high intake of proanthocyanidin is inversely linked to prostate cancer. Importantly, the favorable effect could be attributed to the capacity of some oligomeric forms to influence the proliferation of androgen-resistant and androgen-sensitive human prostate cancer cell lines [92]. Study by Neuwirt et al [93] has shown an ability of proanthocyanidins extracted from grape seeds to suppress the growth of androgen-sensitive prostate cancer cell lines via a few mechanisms including regulating the expression of MAP kinase and activator protein 1. Furthermore, the consumption of red wine, a vital source of proanthocyanidins, was negatively linked to prostate cancer, demonstrated in a United States case-control study [94]. In vitro study showed that resveratrol sensitizes the prostate cancer cell lines to chemotherapeutic drugs such as methotrexate, taxol, actinomycin D, cytarabine, and doxorubicin by inducing apoptosis and downregulating survivin levels [95]. These findings are in parallel with an earlier study reported in the preclinical study for resveratrol, largely present in red wine, in which it has chemopreventive effects against prostate cancer [96]. The recent study suggests that resveratrol upregulates DUSP1 expression in androgen-independent prostate cancer cells through suppression of cyclooxygenase-2 and NF-κB activity [97]. Based on the evidence, it was evident that the administration of naturally-occurring phytochemicals may have a protective role in the development of prostate cancer. Nonetheless, there are several limitations such as the concentration of phytochemicals and bioavailability in relation to prostate cancer. Further studies are required to elucidate the role of these phytochemicals or in combination with other agents in prostate cancer prevention and treatment.
4) Dietary fibers
Dietary fibers are dietary components that are not degraded enzymatically to absorbable fractions in the stomach and small intestine. Many studies support the roles of dietary fiber in preventing the progression and development of prostate cancer. The previous study showed that insoluble fiber was inversely correlated to total and advanced prostate cancer [77]. This study further demonstrated that very low fiber intake was positively linked to prostate cancer in Japanese men [77]. In line with the study reported by Sawada et al [77], fiber intake has also been reported to have antiproliferative activity against prostate cancer [78]. Compared to those who consume fiber (less than 15 g/d), men who consume fiber (more than 15 g/d) can reduce the risk of prostate cancer by 40% [79]. Likewise, data from a prospective study in the United States showed the intake of dietary fiber reduced aggressive prostate cancer among European Americans and African Americans [80]. However, some prospective studies from Western countries have found that consumption of fiber was not related to prostate cancer [81,82].
Indeed, the anticancer ability of dietary fiber is mediated via a few mechanisms including (1) affecting steroid hormone level by reducing circulating androgens and estrogens; (2) increasing sex hormone-binding globulin levels; (3) reducing IGF bioactivity and enhancing insulin sensitivity [98]. Dietary fibers, particularly from legume and insoluble fiber, were inversely linked to prostate cancer risk [99]. Importantly, dietary fiber in vegetables and fruits will undergo fermentation by gut microbiota, and thereby lead to the production of short-chain fatty acids including propionic, butyrate, and acetate acids [100]. Overall, the intake of food rich in dietary fiber regularly may decrease the risk of prostate cancer.
CONCLUSIONS
Evidence from clinical and preclinical studies showed that ROS signaling plays a crucial role in the progression and development of prostate cancer. Several environmental factors, for example, inflammation, diet, and changes in cellular functions like mitochondrial DNA mutations, androgen signaling, and redox imbalance are all contributed to the elevation of ROS. Increased ROS may enhance genetic instability, promote cell proliferation, and alter somatic DNA mutations. Research evidence suggests that a diet high in animal proteins and carbohydrates and excessive fat consumption can generate ROS and thereby results in oxidative stress. The previous study suggests that a diet rich in vitamins (A, D, and E) and minerals, dietary fibers, and phytochemicals are likely to alleviate or prevent prostate cancer. Despite the beneficial effects of these components for reducing the risk of prostate cancer have been reported in both preclinical studies and clinical trials, not all studies supported an association between these dietary patterns and risk of prostate cancer. Therefore, future research is warranted to evaluate the molecular link to better elucidate the possible role of these dietary patterns on prostate cancer prevention and treatment. Indeed, the best dietary advice for prostate cancer management or prevention seems to include: reducing carbohydrate intakes, consuming moderate amounts of calories, decreasing overcooked meats intakes, reducing saturated and total fats, substituting refined carbohydrates with whole grains, and increasing vegetables and fruits.
ACKNOWLEDGEMENTS
This research was supported by Putra Grant (UPM/700-2/1/GPB/2017/9549900).
Footnotes
Conflict of Interest: The authors have nothing to disclose.
- Conceptualization: BLT.
- Writing—original draft: BLT.
- Writing—review & editing: BLT, MEN.
References
- 1.World Health Organization. Cancer [Internet] Geneva: World Health Organization; c2019. [cited 2019 Sep 9]. Available from: https://www.who.int/health-topics/cancer#tab=tab_1. [Google Scholar]
- 2.International Agency for Research on Cancer. Prostate (source: Globocan 2018) [Internet] Geneva: World Health Organization; c2018. [cited 2019 Sep 9]. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/27-Prostate-fact-sheet.pdf. [Google Scholar]
- 3.Fujita K, Nonomura N. Role of androgen receptor in prostate cancer: a review. World J Mens Health. 2019;37:288–295. doi: 10.5534/wjmh.180040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Cancer Research Fund International. Prostate cancer statistics: prostate cancer is the second most common cancer in men worldwide [Internet] London: World Cancer Research Fund International; c2019. [cited 2019 Sep 9]. Available from: https://www.wcrf.org/dietandcancer/cancer-trends/prostate-cancer-statistics. [Google Scholar]
- 5.Elder K, Dixon JM, Blackmur JP, Laurie J. Endocrine therapy for cancer. Surgery. 2018;36:128–133. [Google Scholar]
- 6.Taplin ME, Antonarakis ES, Ferrante KJ, Horgan K, Blumenstein B, Saad F, et al. Androgen receptor modulation optimized for response-splice variant: a phase 3, randomized trial of galeterone versus enzalutamide in androgen receptor splice variant-7-expressing metastatic castration-resistant prostate cancer. Eur Urol. 2019;76:843–851. doi: 10.1016/j.eururo.2019.08.034. [DOI] [PubMed] [Google Scholar]
- 7.Tang J, Xiao L, Cui R, Li D, Zheng X, Zhu L, et al. CX3CL1 increases invasiveness and metastasis by promoting epithelial-to-mesenchymal transition through the TACE/TGF-α/EGFR pathway in hypoxic androgen-independent prostate cancer cells. Oncol Rep. 2016;35:1153–1162. doi: 10.3892/or.2015.4470. [DOI] [PubMed] [Google Scholar]
- 8.Miller DR. The role of ROS in the progression and treatment of castration-resistant prostate cancer [thesis] Omaha: University of Nebraska Medical Center; 2019. [Google Scholar]
- 9.Tan BL, Norhaizan ME, Liew WP. Nutrients and oxidative stress: friend or foe? Oxid Med Cell Longev. 2018;2018:9719584. doi: 10.1155/2018/9719584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed Amar SA, Eryilmaz R, Demir H, Aykan S, Demir C. Determination of oxidative stress levels and some antioxidant enzyme activities in prostate cancer. Aging Male. 2019;22:198–206. doi: 10.1080/13685538.2018.1488955. [DOI] [PubMed] [Google Scholar]
- 11.Long MD, Singh PK, Russell JR, Llimos G, Rosario S, Rizvi A, et al. The miR-96 and RARγ signaling axis governs androgen signaling and prostate cancer progression. Oncogene. 2019;38:421–444. doi: 10.1038/s41388-018-0450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi Y, Han JJ, Tennakoon JB, Mehta FF, Merchant FA, Burns AR, et al. Androgens promote prostate cancer cell growth through induction of autophagy. Mol Endocrinol. 2013;27:280–295. doi: 10.1210/me.2012-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiNicolantonio JJ, Lucan SC, O'Keefe JH. The evidence for saturated fat and for sugar related to coronary heart disease. Prog Cardiovasc Dis. 2016;58:464–472. doi: 10.1016/j.pcad.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biobaku F, Ghanim H, Batra M, Dandona P. Macronutrient-mediated inflammation and oxidative stress: relevance to insulin resistance, obesity, and atherogenesis. J Clin Endocrinol Metab. 2019;104:6118–6128. doi: 10.1210/jc.2018-01833. [DOI] [PubMed] [Google Scholar]
- 15.Laurent V, Toulet A, Attané C, Milhas D, Dauvillier S, Zaidi F, et al. Periprostatic adipose tissue favors prostate cancer cell invasion in an obesity-dependent manner: role of oxidative stress. Mol Cancer Res. 2019;17:821–835. doi: 10.1158/1541-7786.MCR-18-0748. [DOI] [PubMed] [Google Scholar]
- 16.Csiszar A, Podlutsky A, Podlutskaya N, Sonntag WE, Merlin SZ, Philipp EE, et al. Testing the oxidative stress hypothesis of aging in primate fibroblasts: Is there a correlation between species longevity and cellular ROS production? J Gerontol A Biol Sci Med Sci. 2012;67:841–852. doi: 10.1093/gerona/glr216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ham HJ, Park JW, Bae YS. Defect of SIRT1-FoxO3a axis is associated with the production of reactive oxygen species during protein kinase CK2 downregulation-mediated cellular senescence and nematode aging. BMB Rep. 2019;52:265–270. doi: 10.5483/BMBRep.2019.52.4.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dias V, Junn E, Mouradian MM. The role of oxidative stress in Parkinson's disease. J Parkinsons Dis. 2013;3:461–491. doi: 10.3233/JPD-130230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salisbury D, Bronas U. Reactive oxygen and nitrogen species: impact on endothelial dysfunction. Nurs Res. 2015;64:53–66. doi: 10.1097/NNR.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 20.Barreiro E. Role of protein carbonylation in skeletal muscle mass loss associated with chronic conditions. Proteomes. 2016;4:E18. doi: 10.3390/proteomes4020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frijhoff J, Winyard PG, Zarkovic N, Davies SS, Stocker R, Cheng D, et al. Clinical relevance of biomarkers of oxidative stress. Antioxid Redox Signal. 2015;23:1144–1170. doi: 10.1089/ars.2015.6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynaert NL, Gopal P, Rutten EPA, Wouters EFM, Schalkwijk CG. Advanced glycation end products and their receptor in age-related, non-communicable chronic inflammatory diseases; overview of clinical evidence and potential contributions to disease. Int J Biochem Cell Biol. 2016;81(Pt B):403–418. doi: 10.1016/j.biocel.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 23.Gonthier K, Poluri RTK, Audet-Walsh É. Functional genomic studies reveal the androgen receptor as a master regulator of cellular energy metabolism in prostate cancer. J Steroid Biochem Mol Biol. 2019;191:105367. doi: 10.1016/j.jsbmb.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 24.Kowluru RA, Mishra M. Oxidative stress, mitochondrial damage and diabetic retinopathy. Biochim Biophys Acta. 2015;1852:2474–2483. doi: 10.1016/j.bbadis.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Pradedova EV, Nimaeva OD, Salyaev RK. Redox processes in biological systems. Russ J Plant Physiol. 2017;64:822–832. [Google Scholar]
- 26.Bansal A, Simon MC. Glutathione metabolism in cancer progression and treatment resistance. J Cell Biol. 2018;217:2291–2298. doi: 10.1083/jcb.201804161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonkhoff H. Estrogen receptor signaling in prostate cancer: implications for carcinogenesis and tumor progression. Prostate. 2018;78:2–10. doi: 10.1002/pros.23446. [DOI] [PubMed] [Google Scholar]
- 28.Zhao T, Wu K, Hogstrand C, Xu YH, Chen GH, Wei CC, et al. Lipophagy mediated carbohydrate-induced changes of lipid metabolism via oxidative stress, endoplasmic reticulum (ER) stress and ChREBP/PPARγ pathways. Cell Mol Life Sci. 2019 doi: 10.1007/s00018-019-03263-6. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fan LL, Su HX, Gu XJ, Chen YH, Nan CJ. Carbohydrate intake and the risk of prostate cancer. Clin Chim Acta. 2018;484:60–71. doi: 10.1016/j.cca.2018.05.032. [DOI] [PubMed] [Google Scholar]
- 30.Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10:e0117959. doi: 10.1371/journal.pone.0117959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lubik AA, Gunter JH, Hendy SC, Locke JA, Adomat HH, Thompson V, et al. Insulin increases de novo steroidogenesis in prostate cancer cells. Cancer Res. 2011;71:5754–5764. doi: 10.1158/0008-5472.CAN-10-2470. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez JT, Betts JA. Dietary sugars, exercise and hepatic carbohydrate metabolism. Proc Nutr Soc. 2019;78:246–256. doi: 10.1017/S0029665118002604. [DOI] [PubMed] [Google Scholar]
- 33.Arcidiacono B, Iiritano S, Nocera A, Possidente K, Nevolo MT, Ventura V, et al. Insulin resistance and cancer risk: an overview of the pathogenetic mechanisms. Exp Diabetes Res. 2012;2012:789174. doi: 10.1155/2012/789174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox ME, Gleave ME, Zakikhani M, Bell RH, Piura E, Vickers E, et al. Insulin receptor expression by human prostate cancers. Prostate. 2009;69:33–40. doi: 10.1002/pros.20852. [DOI] [PubMed] [Google Scholar]
- 35.Perks CM, Zielinska HA, Wang J, Jarrett C, Frankow A, Ladomery MR, et al. Insulin receptor isoform variations in prostate cancer cells. Front Endocrinol (Lausanne) 2016;7:132. doi: 10.3389/fendo.2016.00132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Food and Agriculture Organization of the United Nations. Food balance sheets: a handbook [Internet] Rome: Food and Agriculture Organization of the United Nations; c2001. [cited 2019 Sep 9]. Available from: http://www.fao.org/3/X9892E/X9892E00.htm. [Google Scholar]
- 37.Ledesma E, Rendueles M, Díaz M. Contamination of meat products during smoking by polycyclic aromatic hydrocarbons: Processes and prevention. Food Control. 2016;60:64–87. [Google Scholar]
- 38.Joshi AD, Corral R, Catsburg C, Lewinger JP, Koo J, John EM, et al. Red meat and poultry, cooking practices, genetic susceptibility and risk of prostate cancer: results from a multiethnic case-control study. Carcinogenesis. 2012;33:2108–2118. doi: 10.1093/carcin/bgs242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Hecke T, Vossen E, Hemeryck LY, Vanden Bussche J, Vanhaecke L, De Smet S. Increased oxidative and nitrosative reactions during digestion could contribute to the association between well-done red meat consumption and colorectal cancer. Food Chem. 2015;187:29–36. doi: 10.1016/j.foodchem.2015.04.029. [DOI] [PubMed] [Google Scholar]
- 40.Bokare AD, Choi W. Review of iron-free Fenton-like systems for activating H2O2 in advanced oxidation processes. J Hazard Mater. 2014;275:121–135. doi: 10.1016/j.jhazmat.2014.04.054. [DOI] [PubMed] [Google Scholar]
- 41.Maurizi G, Della Guardia L, Maurizi A, Poloni A. Adipocytes properties and crosstalk with immune system in obesity-related inflammation. J Cell Physiol. 2018;233:88–97. doi: 10.1002/jcp.25855. [DOI] [PubMed] [Google Scholar]
- 42.Hu MB, Xu H, Zhu WH, Bai PD, Hu JM, Yang T, et al. High-fat diet-induced adipokine and cytokine alterations promote the progression of prostate cancer in vivo and in vitro. Oncol Lett. 2018;15:1607–1615. doi: 10.3892/ol.2017.7454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hayashi T, Fujita K, Nojima S, Hayashi Y, Nakano K, Ishizuya Y, et al. High-fat diet-induced inflammation accelerates prostate cancer growth via IL6 signaling. Clin Cancer Res. 2018;24:4309–4318. doi: 10.1158/1078-0432.CCR-18-0106. [DOI] [PubMed] [Google Scholar]
- 44.Dalvi PS, Chalmers JA, Luo V, Han DY, Wellhauser L, Liu Y, et al. High fat induces acute and chronic inflammation in the hypothalamus: effect of high-fat diet, palmitate and TNF-α on appetite-regulating NPY neurons. Int J Obes (Lond) 2017;41:149–158. doi: 10.1038/ijo.2016.183. [DOI] [PubMed] [Google Scholar]
- 45.Thomas-Valdés S, Tostes MDGV, Anunciação PC, da Silva BP, Sant'Ana HMP. Association between vitamin deficiency and metabolic disorders related to obesity. Crit Rev Food Sci Nutr. 2017;57:3332–3343. doi: 10.1080/10408398.2015.1117413. [DOI] [PubMed] [Google Scholar]
- 46.Hernáandez J, Syed S, Weiss G, Fernandes G, von Merveldt D, Troyer DA, et al. The modulation of prostate cancer risk with alpha-tocopherol: a pilot randomized, controlled clinical trial. J Urol. 2005;174:519–522. doi: 10.1097/01.ju.0000165151.08560.6a. [DOI] [PubMed] [Google Scholar]
- 47.Huang H, He Y, Cui XX, Goodin S, Wang H, Du ZY, et al. Potent inhibitory effect of δ-tocopherol on prostate cancer cells cultured in vitro and grown as xenograft tumors in vivo. J Agric Food Chem. 2014;62:10752–10758. doi: 10.1021/jf504058f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Joshi YB, Praticò D. Vitamin E in aging, dementia, and Alzheimer's disease. Biofactors. 2012;38:90–97. doi: 10.1002/biof.195. [DOI] [PubMed] [Google Scholar]
- 49.Lee GY, Han SN. The role of vitamin E in immunity. Nutrients. 2018;10:E1614. doi: 10.3390/nu10111614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Key TJ, Appleby PN, Travis RC, Albanes D, Alberg AJ, Barricarte A, et al. Endogenous Hormones Nutritional Biomarkers Prostate Cancer Collaborative Group. Carotenoids, retinol, tocopherols, and prostate cancer risk: pooled analysis of 15 studies. Am J Clin Nutr. 2015;102:1142–1157. doi: 10.3945/ajcn.115.114306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Antwi SO, Steck SE, Zhang H, Stumm L, Zhang J, Hurley TG, et al. Plasma carotenoids and tocopherols in relation to prostate-specific antigen (PSA) levels among men with biochemical recurrence of prostate cancer. Cancer Epidemiol. 2015;39:752–762. doi: 10.1016/j.canep.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kyriakopoulos CE, Heath EI, Eickhoff JC, Kolesar J, Yayehyirad M, Moll T, et al. A multicenter phase 1/2a dose-escalation study of the antioxidant moiety of vitamin E 2,2,5,7,8-pentamethyl-6-chromanol (APC-100) in men with advanced prostate cancer. Invest New Drugs. 2016;34:225–230. doi: 10.1007/s10637-016-0334-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lawson KA, Wright ME, Subar A, Mouw T, Hollenbeck A, Schatzkin A, et al. Multivitamin use and risk of prostate cancer in the National Institutes of Health-AARP Diet and Health Study. J Natl Cancer Inst. 2007;99:754–764. doi: 10.1093/jnci/djk177. [DOI] [PubMed] [Google Scholar]
- 54.Albanes D, Till C, Klein EA, Goodman PJ, Mondul AM, Weinstein SJ, et al. Plasma tocopherols and risk of prostate cancer in the Selenium and Vitamin E Cancer Prevention Trial (SELECT) Cancer Prev Res (Phila) 2014;7:886–895. doi: 10.1158/1940-6207.CAPR-14-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lane JA, Oliver SE, Appleby PN, Lentjes MA, Emmett P, Kuh D, et al. Prostate cancer risk related to foods, food groups, macronutrients and micronutrients derived from the UK Dietary Cohort Consortium food diaries. Eur J Clin Nutr. 2017;71:274–283. doi: 10.1038/ejcn.2016.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sarre S, Määttänen L, Tammela TL, Auvinen A, Murtola TJ. Postscreening follow-up of the Finnish Prostate Cancer Screening Trial on putative prostate cancer risk factors: vitamin and mineral use, male pattern baldness, pubertal development and non-steroidal anti-inflammatory drug use. Scand J Urol. 2016;50:267–273. doi: 10.3109/21681805.2016.1145734. [DOI] [PubMed] [Google Scholar]
- 57.Gilbert C. The eye signs of vitamin A deficiency. Community Eye Health. 2013;26:66–67. [PMC free article] [PubMed] [Google Scholar]
- 58.Karadas F, Erdogan S, Kor D, Oto G, Uluman M. The effects of different types of antioxidants (Se, vitamin E and carotenoids) in broiler diets on the growth performance, skin pigmentation and liver and plasma antioxidant concentrations. Rev Bras Cienc Avic. 2016;18:101–116. [Google Scholar]
- 59.Peehl DM, Feldman D. The role of vitamin D and retinoids in controlling prostate cancer progression. Endocr Relat Cancer. 2003;10:131–140. doi: 10.1677/erc.0.0100131. [DOI] [PubMed] [Google Scholar]
- 60.Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994;330:1029–1035. doi: 10.1056/NEJM199404143301501. [DOI] [PubMed] [Google Scholar]
- 61.Cook NR, Le IM, Manson JE, Buring JE, Hennekens CH. Effects of beta-carotene supplementation on cancer incidence by baseline characteristics in the Physicians' Health Study (United States) Cancer Causes Control. 2000;11:617–626. doi: 10.1023/a:1008995430664. [DOI] [PubMed] [Google Scholar]
- 62.Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Risk factors for lung cancer and for intervention effects in CARET, the Beta-Carotene and Retinol Efficacy Trial. J Natl Cancer Inst. 1996;88:1550–1559. doi: 10.1093/jnci/88.21.1550. [DOI] [PubMed] [Google Scholar]
- 63.Abboud M, Rybchyn MS, Rizk R, Fraser DR, Mason RS. Sunlight exposure is just one of the factors which influence vitamin D status. Photochem Photobiol Sci. 2017;16:302–313. doi: 10.1039/c6pp00329j. [DOI] [PubMed] [Google Scholar]
- 64.Goltzman D. Functions of vitamin D in bone. Histochem Cell Biol. 2018;149:305–312. doi: 10.1007/s00418-018-1648-y. [DOI] [PubMed] [Google Scholar]
- 65.Nelson SM, Batai K, Ahaghotu C, Agurs-Collins T, Kittles RA. Association between serum 25-hydroxy-vitamin D and aggressive prostate cancer in African American men. Nutrients. 2016;9:E12. doi: 10.3390/nu9010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Batai K, Murphy AB, Ruden M, Newsome J, Shah E, Dixon MA, et al. Race and BMI modify associations of calcium and vitamin D intake with prostate cancer. BMC Cancer. 2017;17:64. doi: 10.1186/s12885-017-3060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mondul AM, Weinstein SJ, Layne TM, Albanes D. Vitamin D and cancer risk and mortality: state of the science, gaps, and challenges. Epidemiol Rev. 2017;39:28–48. doi: 10.1093/epirev/mxx005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xie DD, Chen YH, Xu S, Zhang C, Wang DM, Wang H, et al. Low vitamin D status is associated with inflammation in patients with prostate cancer. Oncotarget. 2017;8:22076–22085. doi: 10.18632/oncotarget.16195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lin VC, Huang SP, Ting HJ, Ma WL, Yu CC, Huang CY, et al. Vitamin D receptor-binding site variants affect prostate cancer progression. Oncotarget. 2017;8:74119–74128. doi: 10.18632/oncotarget.18271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Albanes D, Mondul AM, Yu K, Parisi D, Horst RL, Virtamo J, et al. Serum 25-hydroxy vitamin D and prostate cancer risk in a large nested case-control study. Cancer Epidemiol Biomarkers Prev. 2011;20:1850–1860. doi: 10.1158/1055-9965.EPI-11-0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weinstein SJ, Mondul AM, Kopp W, Rager H, Virtamo J, Albanes D. Circulating 25-hydroxyvitamin D, vitamin D-binding protein and risk of prostate cancer. Int J Cancer. 2013;132:2940–2947. doi: 10.1002/ijc.27969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cui Z, Liu D, Liu C, Liu G. Serum selenium levels and prostate cancer risk: a MOOSE-compliant meta-analysis. Medicine (Baltimore) 2017;96:e5944. doi: 10.1097/MD.0000000000005944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Allen NE, Travis RC, Appleby PN, Albanes D, Barnett MJ, Black A, et al. Selenium and prostate cancer: analysis of individual participant data from fifteen prospective studies. J Natl Cancer Inst. 2016;108:djw153. doi: 10.1093/jnci/djw153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Morgia G, Voce S, Palmieri F, Gentile M, Iapicca G, Giannantoni A, et al. Association between selenium and lycopene supplementation and incidence of prostate cancer: results from the post-hoc analysis of the procomb trial. Phytomedicine. 2017;34:1–5. doi: 10.1016/j.phymed.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 75.Lü J, Zhang J, Jiang C, Deng Y, Özten N, Bosland MC. Cancer chemoprevention research with selenium in the post-SELECT era: promises and challenges. Nutr Cancer. 2016;68:1–17. doi: 10.1080/01635581.2016.1105267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Reale G, Russo GI, Di Mauro M, Regis F, Campisi D, Giudice AL, et al. Association between dietary flavonoids intake and prostate cancer risk: a case-control study in Sicily. Complement Ther Med. 2018;39:14–18. doi: 10.1016/j.ctim.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 77.Sawada N, Iwasaki M, Yamaji T, Shimazu T, Sasazuki S, Inoue M, et al. Fiber intake and risk of subsequent prostate cancer in Japanese men. Am J Clin Nutr. 2015;101:118–125. doi: 10.3945/ajcn.114.089581. [DOI] [PubMed] [Google Scholar]
- 78.Lewis JE, Soler-Vilá H, Clark PE, Kresty LA, Allen GO, Hu JJ. Intake of plant foods and associated nutrients in prostate cancer risk. Nutr Cancer. 2009;61:216–224. doi: 10.1080/01635580802419756. [DOI] [PubMed] [Google Scholar]
- 79.Walker AR, Walker BF, Tsotetsi NG, Sebitso C, Siwedi D, Walker AJ. Case-control study of prostate cancer in black patients in Soweto, South Africa. Br J Cancer. 1992;65:438–441. doi: 10.1038/bjc.1992.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tabung F, Steck SE, Su LJ, Mohler JL, Fontham ET, Bensen JT, et al. Intake of grains and dietary fiber and prostate cancer aggressiveness by race. Prostate Cancer. 2012;2012:323296. doi: 10.1155/2012/323296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bradbury KE, Appleby PN, Key TJ. Fruit, vegetable, and fiber intake in relation to cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC) Am J Clin Nutr. 2014;100 Suppl 1:394S–398S. doi: 10.3945/ajcn.113.071357. [DOI] [PubMed] [Google Scholar]
- 82.Sheng T, Shen RL, Shao H, Ma TH. No association between fiber intake and prostate cancer risk: a meta-analysis of epidemiological studies. World J Surg Oncol. 2015;13:264. doi: 10.1186/s12957-015-0681-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Schwalfenberg GK, Genuis SJ. Vitamin D, essential minerals, and toxic elements: exploring interactions between nutrients and toxicants in clinical medicine. ScientificWorldJournal. 2015;2015:318595. doi: 10.1155/2015/318595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Marreiro DD, Cruz KJ, Morais JB, Beserra JB, Severo JS, de Oliveira AR. Zinc and oxidative stress: current mechanisms. Antioxidants (Basel) 2017;6:E24. doi: 10.3390/antiox6020024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Costello LC, Franklin RB. The clinical relevance of the metabolism of prostate cancer; zinc and tumor suppression: connecting the dots. Mol Cancer. 2006;5:17. doi: 10.1186/1476-4598-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tsui KH, Chang PL, Juang HH. Zinc blocks gene expression of mitochondrial aconitase in human prostatic carcinoma cells. Int J Cancer. 2006;118:609–615. doi: 10.1002/ijc.21411. [DOI] [PubMed] [Google Scholar]
- 87.Feng P, Liang JY, Li TL, Guan ZX, Zou J, Franklin R, et al. Zinc induces mitochondria apoptogenesis in prostate cells. Mol Urol. 2000;4:31–36. [PubMed] [Google Scholar]
- 88.Eriksen KT, Halkjær J, Meliker JR, McElroy JA, Sørensen M, Tjønneland A, et al. Dietary cadmium intake and risk of prostate cancer: a Danish prospective cohort study. BMC Cancer. 2015;15:177. doi: 10.1186/s12885-015-1153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Singh BP, Dwivedi S, Dhakad U, Murthy RC, Choubey VK, Goel A, et al. Status and interrelationship of zinc, copper, iron, calcium and selenium in prostate cancer. Indian J Clin Biochem. 2016;31:50–56. doi: 10.1007/s12291-015-0497-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu WB, Xiao N, Liu XJ. Dietary flavonoid tangeretin induces reprogramming of epithelial to mesenchymal transition in prostate cancer cells by targeting the PI3K/Akt/mTOR signaling pathway. Oncol Lett. 2018;15:433–440. doi: 10.3892/ol.2017.7307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Praud D, Parpinel M, Guercio V, Bosetti C, Serraino D, Facchini G, et al. Proanthocyanidins and the risk of prostate cancer in Italy. Cancer Causes Control. 2018;29:261–268. doi: 10.1007/s10552-018-1002-7. [DOI] [PubMed] [Google Scholar]
- 92.Kampa M, Theodoropoulou K, Mavromati F, Pelekanou V, Notas G, Lagoudaki ED, et al. Novel oligomeric proanthocyanidin derivatives interact with membrane androgen sites and induce regression of hormone-independent prostate cancer. J Pharmacol Exp Ther. 2011;337:24–32. doi: 10.1124/jpet.110.177246. [DOI] [PubMed] [Google Scholar]
- 93.Neuwirt H, Arias MC, Puhr M, Hobisch A, Culig Z. Oligomeric proanthocyanidin complexes (OPC) exert anti-proliferative and pro-apoptotic effects on prostate cancer cells. Prostate. 2008;68:1647–1654. doi: 10.1002/pros.20829. [DOI] [PubMed] [Google Scholar]
- 94.Schoonen WM, Salinas CA, Kiemeney LA, Stanford JL. Alcohol consumption and risk of prostate cancer in middle-aged men. Int J Cancer. 2005;113:133–140. doi: 10.1002/ijc.20528. [DOI] [PubMed] [Google Scholar]
- 95.Gupta SC, Kannappan R, Reuter S, Kim JH, Aggarwal BB. Chemosensitization of tumors by resveratrol. Ann N Y Acad Sci. 2011;1215:150–160. doi: 10.1111/j.1749-6632.2010.05852.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kumar A, Dhar S, Rimando AM, Lage JM, Lewin JR, Zhang X, et al. Epigenetic potential of resveratrol and analogs in preclinical models of prostate cancer. Ann N Y Acad Sci. 2015;1348:1–9. doi: 10.1111/nyas.12817. [DOI] [PubMed] [Google Scholar]
- 97.Martínez-Martínez D, Soto A, Gil-Araujo B, Gallego B, Chiloeches A, Lasa M. Resveratrol promotes apoptosis through the induction of dual specificity phosphatase 1 and sensitizes prostate cancer cells to cisplatin. Food Chem Toxicol. 2019;124:273–279. doi: 10.1016/j.fct.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 98.Johnston KL, Thomas EL, Bell JD, Frost GS, Robertson MD. Resistant starch improves insulin sensitivity in metabolic syndrome. Diabet Med. 2010;27:391–397. doi: 10.1111/j.1464-5491.2010.02923.x. [DOI] [PubMed] [Google Scholar]
- 99.Deschasaux M, Pouchieu C, His M, Hercberg S, Latino-Martel P, Touvier M. Dietary total and insoluble fiber intakes are inversely associated with prostate cancer risk. J Nutr. 2014;144:504–510. doi: 10.3945/jn.113.189670. [DOI] [PubMed] [Google Scholar]
- 100.Yang Y, Nirmagustina DE, Kumrungsee T, Okazaki Y, Tomotake H, Kato N. Feeding of the water extract from Ganoderma lingzhi to rats modulates secondary bile acids, intestinal microflora, mucins, and propionate important to colon cancer. Biosci Biotechnol Biochem. 2017;81:1796–1804. doi: 10.1080/09168451.2017.1343117. [DOI] [PubMed] [Google Scholar]