Summary
Background
Measures during the COVID‐19 pandemic, including the closure of schools and sports facilities, may have lasting impact on the physical activity (PA) of children that persists for a long time.
Objective
To investigate the effect of COVID‐19 measures on screen time and PA in Dutch children pre‐, during‐ and post‐school closures.
Methods
In cohort A (n = 102, 10.5 ± 3.6 years, 42.4% boys), data on PA and screen time during the lockdown were collected using a questionnaire. In cohort B (n = 131, 10.2 ± 0.9 years, 43.5% boys), data on PA and screen time were collected using a questionnaire and accelerometry 1 year before and after school closure.
Results
In cohort A, 62% reported less total PA. Self‐reported screen time on week days increased 34 ± 105 min/d during the lockdown. In cohort B, sedentary time as measured by accelerometry, increased by 45 ± 67 min/d and only 20% reached PA levels of 60 min/d compared to 64% in May 2019. Self‐reported screen time increased by 59 ± 112 min/d and 62 ± 130 min/d during week and weekend days, respectively.
Conclusions
Children were less physically active, and screen time was higher during and after the school closures due to the COVID‐19 lockdown. This is alarming as an active lifestyle in children is crucial in preventing chronic diseases such as obesity.
Keywords: accelerometry, BAECKE, children, COVID‐19 pandemic, physical activity, screen time
1. INTRODUCTION
The COVID‐19 pandemic is a serious health crisis, and it is a global priority to limit the spread of the virus. The COVID‐19 pandemic is not only a direct threat to human health; the controlled lockdown may also impact health indirectly. In the Netherlands, the government announced a controlled lockdown on 15 March 2020, by ordering a nationwide shutdown of schools, sport clubs, bars and restaurants aimed at minimizing the spread of SARS‐CoV‐2. Even though children seem to be at a lower risk for severe infection, their lifestyle may be severely impacted by these measures. Particularly, physical activity (PA) levels among children may have been affected by the controlled lockdown. Since opportunities where children normally engage in PA, such as physical education, after‐school activities, active transport to school and organized sports, were restricted, being physically active became more challenging. It is well‐known that PA has been associated with numerous health benefits in children including the prevention of cardiovascular disease and obesity and a better health‐related quality of life. 1 , 2 , 3 , 4 The COVID‐19 pandemic may have exacerbated risk factors for weight gain and might contribute to the epidemic of childhood obesity and increase disparities in obesity risk. Therefore, a shift in PA patterns as a result of the lockdown is of great concern. Following the 2003 SARS‐CoV epidemic and the 2012 MERS‐CoV epidemic, the COVID‐19 pandemic is the third time in 20 years that a coronavirus has crossed species and infected the human population. 5 This indicates that a similar pandemic or second COVID‐19 lockdown may occur in the near future. A better understanding of the impact of the current pandemic on PA, and screen time among children is therefore highly important to provide more effective care and public health policies for children in the future.
The importance of regular PA is reinforced by initiatives from organizations such as the WHO to increase or maintain engagement in PA and reduce sedentary time during the pandemic. 6 , 7 Despite these recommendations, preliminary evidence indicates that PA is negatively affected by lockdown measures. A study among 2426 Chinese children and adolescents showed that during the current COVID‐19 pandemic, PA levels decreased on average by 7.25 h/wk and screen time increased by 30 h/wk. 8 A study among Italian children with obesity showed a reduction of 2.5 h/wk spent on sports activities and an increase of screen time by 4 h/d during the lockdown. 9 Canadian children showed a significant decline in self‐reported PA, especially outdoor PA and sport. 10 In addition, 87% of Canadian children reported increased screen time during the pandemic. 11 Also Spanish children reported a reduction of PA of 103 minutes per day during the lockdown and increased their screen time by 2.9 hours per day. 12 In the Netherlands, 42% of parents estimated that their child was less physically active during the spring of 2020 compared to this period in previous years, 13 though to date PA levels were not established during the pandemic. In addition, 36% of US parents and 94% of South Korean parents estimated that their child was less physically active. 14 , 15 Remarkably, although German children reported a decrease in sport‐related PA, they reported an increase in total PA. 16 All studies used questionnaires to evaluate PA levels, though objectively measured PA confirming these findings is lacking. Further, more insight into the reversibility of effects on PA after measures have been lifted is necessary to be able to estimate long‐term effects.
Therefore, the aim of this longitudinal study was to investigate the effect of the COVID‐19 pandemic on PA behaviour and screen time among children in the Netherlands, using both objective (accelerometry) and subjective (BAECKE questionnaire) measures of PA and screen‐time questionnaires pre‐, during‐ and post‐school closures.
2. METHODS
2.1. Setting and participants
PA and screen‐time data were collected from two different cohorts. Cohort A consists of children participating in the Children, Obesity and Lifestyle during COVID‐19 (COLC) study. The COLC study is an ongoing prospective study examining how the COVID‐19 pandemic affects the lifestyle of children and their families. Children were eligible for inclusion if they were living in the Netherlands and were 4 to 18 years old. A webpage including all information about the study for parents and children was provided. Recruitment of children took place via social media and traditional media. To enhance recruitment and include a representative sample, primary and secondary schools in the Netherlands were contacted via email and were asked to share the study information with all children and their parents. Subsequently, both parents of each child gave written informed consent. Informed consent was also obtained from children aged ≥12 years. This study used self‐administered online questionnaires to assess children's PA and screen time prior to and during the COVID‐19 pandemic. A retrospective baseline questionnaire was completed in May 2020 including questions about the child's demographics, PA (measured with the validated BAECKE questionnaire 17 ) and screen time prior to the lockdown period (February 2020). Three weeks later (late May/early June) children and parents completed a follow‐up questionnaire regarding the previous period during which COVID‐19 safety measures applied. Children were instructed to fill out the questionnaire by themselves in case of >12 years. If the child was <12 years old, the parent and child were instructed to complete the questionnaire together.
Cohort B was derived from an on‐going study (clinicaltrial.gov; NCT03440580) that consists of primary school children (7‐12 years old). Children were provided with the ActiGraph GT3X accelerometer for objective PA measures and with the BAECKE questionnaire for subjective PA measures in May‐June 2019. After the controlled lockdown, when the schools reopened fulltime (June 2020), a subgroup of children from the cohort filled out the follow‐up BAECKE questionnaire and screen‐time questionnaires, and accelerometry data were collected.
2.2. Study measurements
2.2.1. Demographics
Parents of children who participated in the COLC study (cohort A) were asked to provide characteristics of the child, such as gender, age, height and bodyweight. Height and bodyweight of the children in cohort B were measured by study staff in the period of May‐June 2019. Body weight was measured using an electric scale (Seca© 877, Seca, Hamburg, Germany) to the nearest 0.1 kg. Standing height was measured using a portable stadiometer (Seca© 213 stadiometer, Seca, Hamburg). Measurements were done twice, and the average was reported. For both cohorts, body mass index (BMI) (weight [kg]/height [m]2) was calculated and age‐ and sex‐specific BMI z‐scores were established (TNO Growth Calculator, TNO, The Hague, the Netherlands). 18 In addition, weight status was classified using the IOTF classification. 19
2.2.2. Physical activity
PA at school, during leisure time and during organized sports, were investigated using the BAECKE questionnaire and analysed according to the scoring system provided by Baecke et al. 17 PA indices for school, leisure time, and sports are derived from a five‐point Likert scare, ranging from 1 to 5 (lowest to highest activity). Total PA is calculated as the sum of all three indices.
Objective accelerometry data in cohort B were collected using the ActiGraph GT3X (ProCare, the Netherlands), which is a triaxial accelerometer that is commonly used for the measurement of PA behaviour in children. Children were instructed to wear the accelerometer on their right hip using a waistband for seven consecutive days during waking hours, except during water activities (eg, showering, swimming) and contact sports (eg, judo). Accelerometry data were downloaded (10 s epochs) using the ActiLife software, and mean counts per minute (CPM) was calculated. Valid wear time was defined as a minimum of 4 days, consisting of at least 480 minutes per day of recording. Cut‐off points by Evenson et al 20 were applied in order to determine sedentary time, light PA (LPA), and moderate‐to‐vigorous PA (MVPA).
2.2.3. Screen time
Screen‐time questionnaires for cohort A included three sub‐categories: screen‐time used for schoolwork, leisure time on a weekday and leisure time on a weekend day (h/d). Children from cohort B reported their screen time separately for weekdays and weekend days using the following questions: ‘How many hours a day during the last 4 weeks did you watch TV on a normal weekday/weekend day?’ and ‘How many hours a day during the last 4 weeks have you played console games or used a computer for your free time activities on a normal weekday/weekend day?’ Possible responses were: ‘not at all’, ‘0.5 hours per day’, ‘one hour per day’, ‘2 hours per day’, ‘2.5 hours per day’, ‘3 hours per day’, ‘3.5 hours per day’ and ‘4 hours or more per day’. Total screen time was derived from the sum of time spent on watching TV and computer/video games.
2.3. Statistical analyses
Data were checked for normality using P‐P plots and histograms, scatter plots for linearity and residual plots for homoscedasticity, where Cook's distance >1 was used to define influential outliers. A paired sample t‐test was used to evaluate significant changes in PA levels and screen time. Multivariable linear regression analyses were used to evaluate the associations between the differences in objectively measured PA prior the lockdown (May 2019) vs after the school closure (May/June 2020), gender and age. A P‐value ≤.05 was considered statistically significant. All analyses were performed using IBM SPSS Statistics for Windows version 25.0 (IBM Corp., Armonk, New York).
2.4. Ethical approval
Both studies were reviewed and approved by the Medical Ethics Committee of the Maastricht University Medical Centre+ (METC2020‐1330‐A‐1 and METC172043/NL64324.068.17) and registered at Clinicaltrials.gov (NCT04411511 and NCT03440580), for cohort A and B, respectively.
3. RESULTS
3.1. Subject characteristics
Online BAECKE and screen‐time questionnaires were completed by 102 children in cohort A and 131 children in Cohort B. Anthropometric data were available for 77 children in cohort A (self‐reported) and 131 children in cohort B (measured by study staff). Table 1 shows the baseline characteristics of children from the two cohorts.
TABLE 1.
Age, sex and weight distribution of participating children in the present study
| Cohort A (n = 102) | Cohort B (n = 131) | |
|---|---|---|
| Age, years | 10.5 ± 3.6 | 10.2 ± 0.9 |
| Gender, M/F % | 42.2/57.8 | 43.5/56.5 |
| BMI z‐score a | −0.27 ± 1.14 (n = 49) | 0.24 ± 1.11 |
| Normal weight, % a | 81.2 (n = 49) | 80.8 |
| Overweight, % a | 18.9 (n = 49) | 19.2 |
BMI z‐score and IOTF criteria were determined for 49 children in cohort A (other participants did not report bodyweight and/or height).
3.2. Self‐reported PA
In cohort A, 62% of the children reported less total PA during the COVID‐19 lockdown period compared to the period right before. PA levels decreased significantly for school, leisure time and sports subdomains (Table 2). Total PA was 0.54 ± 0.92 points (P = <.01) lower for boys and 0.22 ± 0.65 points (P = <.01) lower for girls.
TABLE 2.
Subjectively measured physical activity and screen‐time in children before and during the COVID‐19 pandemic
| Before COVID‐19 pandemic Cohort A | During COVID‐19 pandemic Cohort A | P‐value | Before COVID‐19 pandemic Cohort B | During COVID‐19 pandemic Cohort B | P‐value | |
|---|---|---|---|---|---|---|
| PA BAECKE | (n = 102) | (n = 102) | (n = 131) | (n = 131) | ||
| School index | 2.76 ± 0.32 | 2.68 ± 0.35 | <.01* | 2.78 ± 0.35 | 2.74 ± 0.34 | .18 |
| Sport index | 3.28 ± 78 | 3.14 ± 0.80 | <.01* | 3.11 ± 0.63 | 2.92 ± 0.62 | <.01* |
| Leisure time | 3.25 ± 0.48 | 3.12 ± 0.49 | <.01* | 3.13 ± 0.67 | 3.23 ± 0.71 | .07 |
| Total score | 9.29 ± 1.03 | 8.94 ± 1.07 | <.01* | 9.03 ± 1.22 | 8.89 ± 1.30 | .16 |
| Screen‐time a | ||||||
| Screen‐time school (min/d) | 82 ± 152 | 125 ± 120 | .04* | |||
| Screen‐time weekday (min/d) | 132 ± 109 | 164 ± 123 | <.01* | 181 ± 118 | 240 ± 118 | <.01* |
| Screen‐time weekend day (min/d) | 215 ± 141 | 232 ± 150 | .55 | 197 ± 131 | 260 ± 126 | <.01* |
Abbreviation: PA, physical activity.
A subgroup of 77 participants of cohort A completed the screen‐time questionnaire at both before and during the COVID‐19 pandemic. Data are presented as mean ± SD.
Significant difference between before COVID‐19 pandemic and during COVID‐19 pandemic.
Children in cohort B significantly decreased PA in sports (−0.19 ± 0.64 points, P = <.01) but reported no difference for school and leisure time PA compared to before the COVID‐19 pandemic. Fifty‐four percent of the children in cohort B reported a decrease in total PA compared to the same period 1 year before. In this cohort, total PA decreased by −0.34 ± 0.98 (P = <.01) points in girls, though boys did not report a significant decrease.
3.3. Objectively measured PA
In cohort B, 64 children (10.1 ± 0.7 years, 33.3% boys) provided accelerometry data with valid wear time. Sedentary time was 45 ± 67 min/d higher during the COVID‐19 pandemic (P = <.001), and total PA was 51 ± 52 min/d lower compared to May 2019. Time spent in LPA was 34 ± 42 min/d (P = <.01) lower, and time spent in MVPA deceased by 17 ± 19 min/d (P = <.01; Table 3). In May 2020, 84.4% of the children spent less time in MVPA compared to May 2019. Figure 1 shows that children with higher MVPA levels at baseline showed a larger decrease in time spent in MVPA compared to children with lower levels of PA at baseline. Children who met the PA guidelines of 60 min/d MVPA in May 2019 spent 23 ± 20 min/d (30.5%) less in MVPA during COVID‐19, whereas children who did not meet the guidelines spent 7 ± 9 min/d (14.9%) less in MVPA (P = <.01). The difference in LPA for girls was larger (−44 ± 41 min/d) than in boys (−18 ± 38 min/d, P = .02) (Table 4). However, additional linear regression analyses showed that the decrease in PA was independent of age and sex.
TABLE 3.
Objectively measured physical activity in children before and during the COVID‐19 pandemic
| Before COVID‐19 pandemic (May/June 2019); n = 64 | During Covid‐19 pandemic (June 2020); n = 64 | P‐value | |
|---|---|---|---|
| PA accelerometry | |||
| Sedentary time (min/d) | 420 ± 60 | 465 ± 70 | <.01* |
| LPA (min/d) | 252 ± 34 | 218 ± 39 | <.01* |
| MVPA (min/d) | 65 ± 18 | 48 ± 18 | <.01* |
| CPM | 1236 ± 274 | 1003 ± 266 | <.01* |
| Adhering to MVPA guideline of 60 min/d; (n[%]) | 41 (64) | 13 (20) | <.01* |
Note: Values are presented as mean ± SD.
Abbreviations: CPM, counts per minute; LPA, light physical activity; MVPA, moderate‐to‐vigorous physical activity; PA, physical activity.
Significant difference between before COVID‐19 pandemic and during COVID‐19 pandemic.
FIGURE 1.
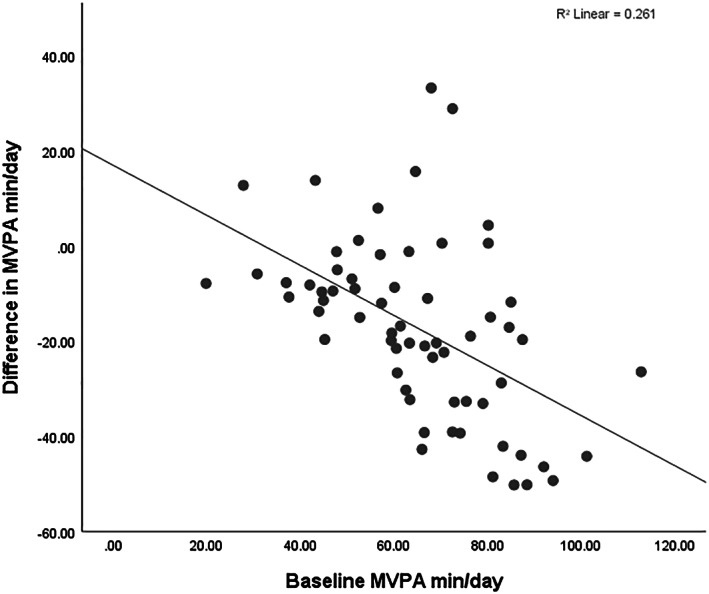
Baseline MVPA (min/d) compared to change in MVPA (min/d) of children during lockdown. Differences in MVPA were calculated as followed: during the COVID‐19 pandemic (June 2020) – before the COVID‐19 pandemic (May/June 2019)
TABLE 4.
Sex differences for objectively measured physical activity changes during the COVID‐19 pandemic compared to the same period 1 year before
| Boys | Girls | P‐value | |
|---|---|---|---|
| PA accelerometry | |||
| Sedentary time (min/d) | +52 ± 71 | +43 ± 66 | .63 |
| LPA (min/d) | −18 ± 38 | −44 ± 41 | .02* |
| MVPA (min/d) | −15 ± 16 | −18 ± 20 | .51 |
| CPM | −201 ± 203 | −252 ± 254 | .43 |
Note: Values are presented as mean ± SD.
Abbreviations: CPM, counts per minute; LPA, light physical activity; MVPA, moderate‐to‐vigorous physical activity; PA, physical activity.
Significant difference between boys and girls.
3.4. Screen time
Seventy‐seven children in cohort A completed the screen‐time questionnaire at both time points. Forty‐three percent spent more time on screens on weekdays (34 ± 105 min/d, P = <.01) during the COVID‐19 pandemic (Table 2). Elevated school‐related screen time was reported by 50% of the children. On average, school‐related screen time increased by 43 ± 175 min/d (P = .04). Screen time on weekend days did not change significantly. Similar results were found in cohort B (n = 131), as the majority reported increased screen time during both week (66%) and weekend days (63%), resulting in an average increase of 59 ± 112 min/d (P = <.01) and 62 ± 130 min/d (P = <.01), respectively.
4. DISCUSSION
This study is the first to include both self‐reported and objectively measured PA, and screen time in children, in order to evaluate the impact of the COVID‐19 pandemic on PA behaviour at a young age. This study indicates that the majority of Dutch children (cohort A: 62%, cohort B: 54%) reported lower levels of total PA during the COVID‐19 pandemic compared to before the pandemic, which was confirmed by accelerometry data in a subgroup. The number of children meeting PA guidelines of ≥60 min/d of MVPA decreased from 64% to 20% during the pandemic, even after reopening of schools and sport clubs. Furthermore, during the first stages of the pandemic, subjective data showed that screen time increased by 1 hour per day and, concordantly, sedentary time by 45 min/d.
The present data are in line with previous studies, showing a negative effect of the COVID‐19 pandemic on self‐reported PA during lockdown. 8 , 9 , 10 , 12 , 13 , 14 , 15 , 21 Thirty‐six percent of US parents, 94% of South Korean parents and 42% of Dutch parents estimated that their child was less physically active during the COVID‐19 pandemic compared to prior to the pandemic. 13 , 14 , 15 The present study confirmed decreased levels of total PA during the COVID‐19 pandemic among children in the Netherlands, compared to before the pandemic. In addition, PA was reported to be lower during the COVID‐19 pandemic, regardless of residence 8 , 12 , 13 , 14 , 15 or weight category (normal weight category vs children with obesity 9 ). In contrast with these studies, German children reported an increase in total PA. 16 Differences in COVID‐19‐related measures among countries might explain these differences in PA in children during the pandemic. For example, China had a strict lockdown 8 compared to Germany where non‐organized sports and outdoor play were allowed 16 during the COVID‐19 pandemic.
In this study, the decrease in PA was confirmed by objective PA data as measured using accelerometry. Of note, subjects received accelerometers when the schools and sport clubs reopened (May/June, 2020). This demonstrates that although children were able to engage in PA, which was more difficult during the controlled lockdown (eg, after‐school activities, transportation to school and organized sports were cancelled), total PA decreased by 51 min/d and sedentary time increased by 45 min/d, when compared to the same period a year before (May 2019). The percentage of children that reported to be less physically active than 1 year before was 54%, even though lockdown measures were already downscaled at the moment of completing the questionnaires. This indicates that reopening schools and organized sports did not result in restored PA levels in children. Potential factors that might have an effect on PA are amount of sleep, parental support, lack of time and lack of energy. 10 , 13 Several authors suggested that parental support was a key correlate to promote PA during the COVID‐19 pandemic and thereby potentially stimulate children's health. 10 , 21 , 22 Therefore, it is suggested that improving parental support might be a target for promoting PA, especially during the COVID‐19 pandemic or future pandemics.
Previous studies showed that boys are generally more physically active than girls and PA declines with increasing age. 23 , 24 This has also been found in a study regarding COVID‐19 restrictions in the United States, showing a larger impact on the self‐reported decrease of PA and increase of sedentary time in girls compared to boys and among older children (9‐13 years vs 5‐8 years). 14 The present study found a difference in objectively measured light intensity PA between boys and girls. However, when age and sex were added in the linear regression model as covariates, no effect of sex and age on PA (total PA as well on MVPA and LPA) was found.
Our data indicated that compared to the pre‐COVID period, screen time increased by 1 hour per day and sedentary time by with 45 min/d, during the lockdown of spring 2020. A study in Italy showed that children with obesity showed an average increase in screen time of 4.85 h/d. 9 Carroll et al 11 showed that 87% of Canadian children reported increased recreational screen time during the COVID‐19 lockdown. Chinese children reported an average increase of 30 h/wk; however, only 30.9% of these children reported more than 2 hours of leisure screen time per day. 8 Although previous studies did not differentiate between school‐related screen time and leisure‐related screen time, the children in the present study reported a smaller increase in screen time compared to children from other countries. 8 , 9 An explanation for this difference might be that children from those countries were restricted to home quarantine, and therefore outside activities were extremely limited, while in the Netherlands, the controlled lockdown still provided opportunities for outdoor play. Although Dutch parents have set rules for playing outside (ie, keeping distance from other children and playing close to home), 91% of the parents reported that their child was allowed to play outside during the controlled lockdown. 13 Though the current study differentiated between weekdays and weekend days, only small differences in increased screen time between week and weekend days were reported, which is remarkable as school‐related screen time during week days increased.
A methodological strength of this study is the unique inclusion of objectively measured PA using accelerometry in addition to self‐reported PA at different time points. This is a novelty in COVID‐19 studies, as previous studies only described self‐reported PA. 8 , 9 , 10 , 13 , 14 These objectively measured results confirm and extend the findings of previous studies. Another strength of this study is that the self‐reported PA was collected in the situation prior, during and after the lockdown, while the objectively measured data were collected prior to the COVID‐19 pandemic and after reopening the schools and sportclubs. The results of the different time points that PA and screen time were measured indicate that the COVID‐19 pandemic may have a lasting impact on PA and screen time and that these unhealthy behavioural adaptations in children may become their new normal.
A limitation of this study is the use of a convenience sample from an ongoing study (cohort B). Although this population might not be fully representative for the general Dutch population, based on the distribution of sex, age and school environment (SES‐distribution), it is expected that the findings provide a reliable estimation of the PA patterns of children. Furthermore, the baseline questionnaires in cohort A might have been subject to recall‐bias as PA and screen‐time behaviour were questioned retrospectively regarding the period prior to the lockdown. Moreover, especially in young children (<10 years), questions on PA and screen time might be difficult to interpret or answer, and they may not fully understand the concept of PA. 25 However, to prevent bias, parents were instructed to complete the questionnaire together with their child (<16 years). Secondly, only 49% of all children that used the accelerometer had valid wear time to include data in the current analysis. Although more girls than boys had worn the accelerometer according to the instructions (65.6%), the average age of this subgroup was similar to the entire cohort. In combination with the data derived from the BAECKE questionnaire, we believe that this subgroup is representative for the entire cohort. Furthermore, seasonal influences may have affected the results, as children from cohort A filled out the baseline BAECKE questionnaire about the situation in February 2020, while the follow‐up questionnaire was filled out in May 2020. Previous research showed that seasonal influences such as winter and the amount of daylight per day may affect PA levels in children. 26 , 27 Based on this knowledge, the negative effect of the COVID‐19 regulations on PA becomes even more explicit, as spring time usually affects PA in a positive manner. Moreover, objectively measured data confirm the findings in this study, while possible seasonal effects were excluded as these data were collected during similar periods (May 2019 vs May‐June 2020).
To summarize, after the Dutch governmental regulations were introduced in order to prevent spread of the disease, PA levels decreased and sedentary time and screen time increased in 4‐ to 18‐year‐old children. The findings suggest that abrogation of the COVID‐19 measures alone might not be sufficient to restore PA levels in children after months of changed behaviours. These side effects of the regulations may have a negative impact on the long‐term health of children. 28 The controlled lockdown in the Netherlands still provided opportunities for children to play outside. Therefore, it is possible that the effects on the decrease in PA and increase in ST, including screen time, is even more pronounced in countries were the measures are more restricted (ie, home quarantine) and/or the duration of the lockdown was longer. In view of the growing prevalence of overweight and obesity at a young age and the negative consequences later in life, strategies to stimulate PA during the current and potential future pandemics, are warranted to prevent unhealthy weight development in children.
5. CONCLUSION
PA levels in school‐aged children decreased during the COVID‐19 pandemic, while screen time increased and children were more sedentary. Importantly, even after the controlled lockdown (ie, reopening of schools and sport clubs), objectively measured PA levels were still decreased, while screen time and ST were increased. These findings highlight the need for strategies to promote PA and reduce sedentary time, including screen‐time, in children during the current and potential future pandemics to prevent long‐term health risks.
CONFLICT OF INTEREST
We declare no competing interest.
AUTHOR CONTRIBUTIONS
Anita Vreugdenhil, Gabrielle ten Velde, Judith Lubrecht, Lisanne Arayess, Christiana van Loo and Marijn Hesselink designed the study. Gabrielle ten Velde, Judith Lubrecht, Lisanne Arayess and Christiana van Loo contributed to data acquisition. Gabrielle ten Velde and Judith Lubrecht cleaned the data. Gabrielle ten Velde performed the statistical analyses. Gabrielle ten Velde wrote the first draft of this manuscript. Anita Vreugdenhil, Dorien Reijnders and Christiana van Loo have contributed to the writing of the final version of this manuscript. Anita Vreugdenhil had the primary responsibility for the final content. All authors revised the manuscript and approved the manuscript for publication.
ACKNOWLEDGEMENTS
The authors acknowledge all children and families that have participated in this study. Data from children from cohort B were collected from an ongoing study which received funding from Province Limburg (SAS‐2015‐04956).
ten Velde G, Lubrecht J, Arayess L, et al. Physical activity behaviour and screen time in Dutch children during the COVID‐19 pandemic: Pre‐, during‐ and post‐school closures. Pediatric Obesity. 2021;16:e12779. 10.1111/ijpo.12779
Funding information Province Limburg, Grant/Award Number: SAS‐2015‐04956
REFERENCES
- 1. Mendis S, Puska P, Norrving B, Organization WH . Global Atlas on Cardiovascular Disease Prevention and Control. Geneva: World Health Organization; 2011. [Google Scholar]
- 2. Steinbeck KS. The importance of physical activity in the prevention of overweight and obesity in childhood: a review and an opinion. Obes Rev. 2001;2(2):117‐130. [DOI] [PubMed] [Google Scholar]
- 3. Wu XY, Han LH, Zhang JH, Luo S, Hu JW, Sun K. The influence of physical activity, sedentary behavior on health‐related quality of life among the general population of children and adolescents: a systematic review. PLoS One. 2017;12(11):e0187668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school‐aged children and youth. Int J Behav Nutr Phys Act. 2010;7(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang Y, Xu J, Li H, Cao B. A novel coronavirus (COVID‐19) outbreak: a call for action. Chest. 2020;157(4):e99‐e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Organization WH . Coronavirus disease (COVID‐19): staying active. 2020. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/question‐and‐answers‐hub/q‐a‐detail/be‐active‐during‐covid‐19
- 7. UNICEF . Indoor play ideas to stimulate young children at home. 2020.
- 8. Xiang M, Zhang Z, Kuwahara K. Impact of COVID‐19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63:531‐532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28:1382‐1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID‐19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carroll N, Sadowski A, Laila A, et al. The impact of COVID‐19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12(8):2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. López‐Bueno R, López‐Sánchez GF, Casajús J, et al. Health‐related behaviors among school‐aged children and adolescents during the Spanish Covid‐19 confinement. Front Pediatr. 2020;8:573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Slot‐Heijs JdJM, Lucassen J, Singh A. Beweeggedrag van kinderen in tijden van corona. 2020.
- 14. Dunton GF, Do B, Wang SD. Early effects of the COVID‐19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health. 2020;20(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guan H, Okely AD, Aguilar‐Farias N, et al. Promoting healthy movement behaviours among children during the COVID‐19 pandemic. Lancet Child Adolesc Health. 2020;4(6):416‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schmidt SCE, Anedda B, Burchartz A, et al. Physical activity and screen time of children and adolescents before and during the COVID‐19 lockdown in Germany: a natural experiment. Sci Rep. 2020;10(1):21780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936‐942. [DOI] [PubMed] [Google Scholar]
- 18. De Onis M, Lobstein T. Defining Obesity Risk Status in the General Childhood Population: Which Cut‐Offs Should We Use? Oxfordshire: Taylor & Francis; 2010. [DOI] [PubMed] [Google Scholar]
- 19. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284‐294. [DOI] [PubMed] [Google Scholar]
- 20. Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557‐1565. [DOI] [PubMed] [Google Scholar]
- 21. López‐Bueno R, López‐Sánchez GF, Casajús JA, Calatayud J, Tully MA, Smith L. Potential health‐related behaviors for pre‐school and school‐aged children during COVID‐19 lockdown: a narrative review. Prev Med. 2020;143:106349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guerrero MD, Vanderloo LM, Rhodes RE, Faulkner G, Moore SA, Tremblay MS. Canadian children's and youth's adherence to the 24‐h movement guidelines during the COVID‐19 pandemic: a decision tree analysis. J Sport Health Sci. 2020;9:313‐321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Andersen LB, Harro M, Sardinha LB, et al. Physical activity and clustered cardiovascular risk in children: a cross‐sectional study (The European Youth Heart Study). Lancet. 2006;368(9532):299‐304. [DOI] [PubMed] [Google Scholar]
- 24. Whitt‐Glover MC, Taylor WC, Floyd MF, Yore MM, Yancey AK, Matthews CE. Disparities in physical activity and sedentary behaviors among US children and adolescents: prevalence, correlates, and intervention implications. J Public Health Policy. 2009;30(1):S309‐S334. [DOI] [PubMed] [Google Scholar]
- 25. Trost SG. State of the art reviews: measurement of physical activity in children and adolescents. Am J Lifestyle Med. 2007;1(4):299‐314. [Google Scholar]
- 26. Goodman A, Page AS, Cooper AR. Daylight saving time as a potential public health intervention: an observational study of evening daylight and objectively‐measured physical activity among 23,000 children from 9 countries. Int J Behav Nutr Phys Act. 2014;11(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Atkin AJ, Sharp SJ, Harrison F, Brage S, Van Sluijs EM. Seasonal variation in children's physical activity and sedentary time. Med Sci Sports Exerc. 2016;48(3):449‐456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Saunders TJ, Gray CE, Poitras VJ, et al. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school‐aged children and youth. App Physiol Nutr Metab. 2016;41(6):S283‐S293. [DOI] [PubMed] [Google Scholar]


