Abstract
The global emergency caused by the novel coronavirus (COVID‐19) pandemic has impacted access to goods and services such as health care and social supports, but the impact on infant feeding remains unclear. Thus, the objective of this study was to explore how caregivers of infants under 6 months of age perceived changes to infant feeding and other food and health‐related matters during the COVID‐19 State of Emergency in Nova Scotia, Canada. Four weeks after the State of Emergency began, between 17 April and 15 May 2020, caregivers completed this online survey, including the Perceived Stress Scale. Participants (n = 335) were 99% female and mostly White (87%). Over half (60%) were breastfeeding, and 71% had a household income over CAD$60,000. Most participants (77%) received governmental parental benefits before the emergency, and 59% experienced no COVID‐19‐related economic changes. Over three quarters of participants (77%) scored moderate levels of perceived stress. Common themes of concern included social isolation, COVID‐19 infection (both caregiver and infant), and a lack of access to goods, namely, human milk substitutes (‘infant formula’), and services, including health care, lactation support, and social supports. Most COVID‐19‐related information was sought from the internet and social media, so for broad reach, future evidence‐based information should be shared via online platforms. Although participants were experiencing moderate self‐perceived stress and shared numerous concerns, very few COVID‐19‐related changes to infant feeding were reported, and there were few differences by socio‐economic status, likely due to a strong economic safety net in this Canadian setting.
Keywords: bottle feeding, breastfeeding, COVID‐19, emergency, pandemic, Perceived Stress Scale, public health, SARS‐CoV‐2
Key messages.
Despite the COVID‐19 State of Emergency, Nova Scotian participants reported minimal changes in feeding practices, regardless of income and educational attainment, population density, parity, age, and ethnicity.
Many participants felt unsupported and socially isolated due to the cancellation of routine post‐partum appointments, lactation support services, public health home visits, and organized support or play groups.
Some breastfeeding participants reported delayed growth monitoring and subsequent introduction of infant formula to more closely control their infant's intake.
Formula‐feeding participants were concerned about access to, and retail stock‐outs of, infant formula, particularly specialized forms (e.g., lactose free and hydrolysed).
1. INTRODUCTION
The World Health Organization's global infant and young child feeding recommendations include guidance to breastfeed exclusively until the introduction of safe and nutritionally adequate complementary foods at 6 months (World Health Organization, 2020a). Appropriate infant feeding plays a particularly important role in the prevention of infection during times of increased pathogen exposure, as human milk provides immunoprotective compounds, and appropriate first complementary foods contain iron and zinc which can reduce risk of infection (Eneroth, Persson, El Arifeen, & Ekström, 2011; Hassiotou et al., 2013; Yakoob et al., 2011).
Emergencies are similarly important times for infant feeding, as infants are often more vulnerable to health risks than older age groups, in part due to a more urgent need for appropriate nutrition and food security (American Academy of Pediatrics, 2015; Carothers & Gribble, 2014; Gribble, 2014; IFE Core Group, 2017). For instance, emergencies such as natural disasters and infectious disease outbreaks pose a unique set of barriers to optimal infant feeding (Carothers & Gribble, 2014; IFE Core Group, 2017) that can result in cessation of breastfeeding or the introduction of suboptimal food or feeding practices (Ververs et al., 2019). Barriers to optimal infant feeding and resulting dangerous feeding practices have been documented during past emergencies (Callaghan et al., 2007; DeYoung, Chase, Branco, & Park, 2018; Ishii et al., 2016); however, much of the literature documenting the impact of emergencies on infant feeding takes place in low‐ and middle‐income countries, and those in high‐income countries predominantly report on responses specific to natural disasters (DeYoung et al., 2018; Ishii et al., 2016). Often, these reports describe emergency responses where infants and caregivers have been displaced or evacuated from their homes, are staying in precarious and often overcrowded emergency shelters and/or are without access to clean water (DeYoung et al., 2018; Hirani, Richter, Salami, & Vallianatos, 2019; Ishii et al., 2016).
In contrast, the global COVID‐19 pandemic has posed a unique emergency, layering a high risk of communicable disease exposure, and isolation rather than overcrowding, on infant feeding challenges. The novel coronavirus disease COVID‐19, caused by SARS‐CoV‐2 infection, is transmitted via respiratory droplets and aerosols, prompting public health guidelines of physical distancing (Lackey et al., 2020; Tang et al., 2020). In Nova Scotia, Canada, a provincial State of Emergency was declared on 22 March 2020, triggering subsequent orders to limit direct social contact, leading to closures of schools and day cares, limitations to public transportation and restricted opening hours for businesses, in turn limiting access to goods and services (Government of Nova Scotia, 2020a). Importantly, many Nova Scotians lost income or were put at higher risk of contracting COVID‐19 by continuing to work (Government of Canada, 2020a).
In Nova Scotia, breastfeeding women tend to be older, more highly educated, partnered and have higher incomes (Brown et al., 2013). Here, breastfeeding rates are among the lowest in Canada, with only 22% of infants breastfed exclusively to 6 months (vs. 33% nationally) despite an initiation rate of 86%, and the issue of infant food insecurity is a growing concern (Frank, 2020; Statistics Canada, 2018). This State of Emergency had the potential to present unique challenges to the caregivers of young infants, thus exacerbating these existing issues, increasing the vulnerability of infants. Given the novelty of COVID‐19, there is a gap in understanding of how caregivers could experience this State of Emergency, how it could impact young infants, and how to best support caregivers during a potential second wave of virus transmission and emergency‐related social restrictions and/or future pandemics. Therefore, the purpose of this study was to explore COVID‐19 State of Emergency‐related changes in feeding practices among caregivers of young infants in Nova Scotia.
2. METHODS
2.1. Study objective
This was a cross‐sectional study designed to explore how caregivers of infants under 6 months of age perceived changes to infant feeding and other food and health‐related matters during the COVID‐19 State of Emergency in Nova Scotia, Canada.
2.2. Research context
Data collection took place between 17 April and 15 May 2020, 4 weeks after a State of Emergency was declared in Nova Scotia on 22 March 2020. During this time period (22 March to 15 May 2020), there were cumulatively 1034 confirmed positive cases of COVID‐19 in the province (Government of Nova Scotia, 2020b). Nova Scotians were instructed to limit social gatherings to five people (including household members) and to only leave home for essential items, maintaining social distancing when doing so (Government of Nova Scotia, 2020a). Licensed childcare providers, schools and most public spaces were closed during this time, public transportation services were limited and some health care services were suspended, such as lactation support and postnatal visits and check‐ups, at the discretion of the physician (Reproductive Care Program of Nova Scotia, 2020). On 1 May 2020, some provincial and municipal parks, trails, community gardens, campgrounds, sport fishing and outdoor businesses were reopened (Government of Nova Scotia, 2020a).
The Canada Emergency Response Benefit (CERB) was implemented by the Government of Canada starting on 15 March 2020 to provide temporary financial support and offset any COVID‐19‐related loss of employment for eligible individuals. The CERB provided CAD$500 per week of unemployment for those not already receiving other forms of employment insurance (EI) (Government of Canada, 2020b). While other members of the household may have been receiving CERB or regular EI, caregivers who were receiving Canadian universal parental EI were not eligible for CERB or regular EI. The Canadian universal parental EI remained unchanged, providing a maximum of 55% of an individual's earnings (to a maximum of $573 per week), which may be ‘topped up’ by some employers (Government of Canada, 2020c). The only other financial support available to Nova Scotian families during the COVID‐19 pandemic was a one‐time CAD$300 ‘top‐up’ per child (in addition to their normal Canada Child Benefit which provides a maximum of $564/child per month, based on household income) (Government of Canada, 2020d).
2.3. Recruitment and data collection
To participate in this online questionnaire, individuals had to be at least 19 years of age and must have resided full time in Nova Scotia for at least 1 month before the State of Emergency was declared. Participants must have been the primary caregiver of an infant born between 22 October 2019 and 22 March 2020 and, thus, were born before the State of Emergency was declared but were less than 6 months old. Only infants less than 6 months old were included to capture the period of exclusive milk feeding. Participants were recruited via a poster shared on various social media platforms and our research lab website over a 4‐week period of rolling recruitment. This poster contained a URL linking directly to the study questionnaire (SimpleSurvey, OutsideSoft Solutions Inc, Montreal, Canada) titled ‘Infant Feeding in Nova Scotia during COVID‐19’. Participants were asked to answer eligibility screening questions and provide implied consent. The survey was anonymous, and participants were provided the opportunity to be entered into a draw for one of three $50 gift cards to a store of their choice. This study was approved by the Mount Saint Vincent University Research Ethics Board (MSVU UREB 2019‐189).
Over the data collection period, 1425 individuals accessed the questionnaire URL and 604 completed the eligibility questions, of which 532 were eligible and provided implied consent by clicking to the first page of study questions. After removing entries with insufficient data (n = 196 responded to <20% of study questions), and one entry removed for a complex medical condition that could not be controlled for in analyses, 335 participants were included in final analysis.
2.4. Questionnaire design
Sociodemographic information about the participant and their household were collected. The remainder of the questionnaire included three sections of both open‐ and close‐ended questions: (1) infant feeding changes, (2) caregiver's general knowledge, information seeking and behaviours with regard to COVID‐19; and (3) caregiver concerns and perceived stress during the State of Emergency. Depending on the caregiver's responses about feeding modality, they received questions about breastfeeding, feeding infant formula, or both. The Perceived Stress Scale, a widely used measure of stress which has been previously validated among breastfeeding and bottle‐feeding mothers (Cohen, Kamarck, & Mermelstein, 1983; Mezzacappa, 2004), was also employed.
2.5. Data analysis
Descriptive statistics were computed and presented as n (%) or mean (95% CI). Chi‐square tests were used to assess for differences in the following sociodemographic characteristics by feeding modality: infant age, sex and ethnicity; caregiver age, gender, relationship to infant, parity, ethnicity, marital status and education level; household income, parental benefits, geographic area and population density, number of adults and children in the household, changes in income and changes in childcare; and pumping, usual pumping frequency, type of infant formula and form of infant formula. When applicable (findings differed from expected values; P < 0.05), a Bonferroni post hoc correction was employed to determine where differences existed (Beasley & Schumacker, 1995). The same statistical tests were used for comparisons for COVID‐19‐related information‐seeking behaviours and household income (categorized above and below CAD$60,000, the median Nova Scotian household income; Government of Nova Scotia: Finance and Treasury Board, 2017) and age (categorized above and below 35 years, the cut‐off for advanced maternal age; Benzies, 2008; Bushnik & Garner, 2008). Participants' cumulative score for the Perceived Stress Scale was used to categorize participants as experiencing self‐perceived low, moderate or high stress (Cohen et al., 1983). Data analyses were performed using IBM SPSS v. 26.0 for Mac OS (IBM Corp, 2018) with a significance level of P < 0.05. Open‐ended responses among participants' indicating infant food‐related changes since the initiation of the State of Emergency were analysed thematically and categorized as COVID‐19 related (e.g., stress, food availability and income), related to another factor (e.g., infant age) or reason unknown (e.g., no reason given) (Attride‐Stirling, 2001). Illustrative participant quotes that either demonstrated common themes or minority responses are presented.
3. RESULTS
3.1. Participant characteristics
Nearly all participants were White (87%), female (99%) and most (60%) participants breastfed their infants (Table 1). Participants were, on average, 31 years old, and their infants (50% female) averaged 16 weeks of age (range: 4–24 weeks). Most (77%) of the participants were receiving parental EI benefits at the time of participation, and 59% of participants experienced no change in source of income due to the COVID‐19 State of Emergency. Approximately one third of participants were impacted by loss of childcare or school cancellation. Significantly more of the breastfeeding caregivers, as compared with formula and mixed feeders, were married or in common‐law relationships (n = 187, 94%), had completed a graduate or professional degree (n = 48, 24%) and had household income over CAD$60,000 per year (n = 161, 82%) (P < 0.05).
TABLE 1.
Sociodemographic characteristics of study participants
| Characteristic | N a | All | Breastfeeders | Formula feeders | Mixed feeders |
|---|---|---|---|---|---|
| N = 335 | n = 200 | n = 70 | n = 65 | ||
| Infant | |||||
| Age, weeks | 334 | 16.1 (6.6) | 15.5 (6.5) | 17.0 (7.1) | 16.6 (6.4) |
| Infant sex, female | 335 | 168 (50%) | 101 (51%) | 35 (50%) | 32 (49%) |
| Infant ethnicity | 335 | ||||
| White | 283 (85%) | 179 (90%)* | 56 (80%) | 48 (74%) | |
| Mixed ethnicity | 34 (10%) | 15 (8%) | 12 (17%) | 7 (11%) | |
| Acadian | 5 (2%) | 4 (2%) | 0 (0%) | 1 (2%) | |
| Indigenous Canadian | 4 (1%) | 0 (0%) | 1 (1%) | 3 (5%) | |
| Other b | 9 (3%) | 2 (1%) | 1 (1%) | 6 (9%) | |
| Caregiver | |||||
| Age, years | 331 | 31.0 (4.6) | 31.3 (4.0) | 29.7 (5.6) | 31.5 (5.1) |
| Gender, woman | 335 | 332 (99%) | 198 (99%) | 69 (99%) | 65 (100%) |
| Relationship to infant, mother | 335 | 332 (99%) | 199 (100%) | 68 (97%) | 65 (100%) |
| Parity, primiparous | 332 | 200 (60%) | 116 (58%) | 42 (62%) | 42 (65%) |
| Ethnicity | 334 | ||||
| White | 292 (87%) | 181 (91%) | 60 (86%) | 51 (79%) | |
| Mixed ethnicity | 22 (7%) | 10 (5%) | 7 (10%) | 5 (8%) | |
| Indigenous Canadian | 6 (2%) | 0 (0%)* | 2 (3%) | 4 (6%)* | |
| Other c | 14 (4%) | 8 (4%) | 1 (1%) | 5 (8%) | |
| Marital status, married or common‐law | 335 | 287 (86%) | 187 (94%)* | 49 (70%)* | 51 (79%) |
| Education attained | 335 | ||||
| Some or completed high school | 59 (18%) | 25 (13%)* | 21 (30%)* | 13 (20%) | |
| College diploma | 95 (28%) | 46 (23%) | 29 (41%) | 20 (31%) | |
| Undergraduate degree | 118 (35%) | 81 (41%) | 12 (17%)* | 25 (39%) | |
| Graduate/professional degree | 63 (19%) | 48 (24%)* | 8 (11%) | 7 (11%) | |
| Annual household income | 332 | ||||
| <CAD$60,000 | 94 (28%) | 36 (18%)* | 33 (57%)* | 25 (39%) | |
| ≥CAD$60,000 | 238 (71%) | 161 (82%)* | 37 (53%)* | 40 (62%) | |
| Recipient of monetary parental benefits d | 335 | 259 (77%) | 158 (79%) | 49 (70%) | 52 (80%) |
| Resides in Greater Halifax area | 335 | 194 (58%) | 115 (58%) | 35 (50%) | 44 (68%) |
| Population density, urban | 335 | 185 (55%) | 116 (58%) | 30 (43%) | 39 (60%) |
| Number of adults in the household | 333 | 2.0 (0.6) | 1.9 (0.4) | 2.0 (0.9) | 2.1 (0.8) |
| Number of children in the household | 300 | 1.76 (1.1) | 1.69 (0.9) | 1.93 (1.2) | 1.83 (1.5) |
| ≤6 months | 335 | 335 (100%) | 200 (100%) | 70 (100%) | 65 (100%) |
| 7–23 months | 289 | 21 (7%) | 8 (5%) | 10 (17%)* | 3 (5%) |
| ≥24 months | 293 | 131 (45%) | 85 (48%) | 26 (45%) | 20 (35%) |
| Changes in income due to COVID‐19 | 335 | ||||
| No change | 199 (59%) | 121 (61%) | 37 (53%) | 41 (63%) | |
| Started receiving EI/CERB e | 75 (22%) | 37 (19%) | 23 (33%) | 15 (23%) | |
| Loss of income and no EI/CERB | 40 (12%) | 26 (13%) | 6 (9%) | 8 (12%) | |
| Other f | 21 (6%) | 16 (8%) | 4 (6%) | 1 (1%) | |
| Change in childcare due to COVID‐19 | 332 | ||||
| No change | 212 (63%) | 128 (65%) | 40 (58%) | 44 (68%) | |
| Impacted by loss of childcare | 77 (23%) | 48 (24%) | 19 (28%) | 10 (15%) | |
| Impacted by school cancellation | 43 (13%) | 22 (11%) | 10 (14%) | 11 (17%) | |
| Infant feeding characteristics before COVID‐19 | |||||
| Breastfeeding | |||||
| Expressed (‘pumped’) human milk | 264 | 174 (66%) | 133 (67%) | ‐ | 41 (64%) |
| Usual pumping frequency | |||||
| Occasionally | 9 (5%) | 8 (6%) | ‐ | 1 (3%) | |
| 1–2 times daily | 122 (72%) | 97 (75%) | ‐ | 25 (64%) | |
| >2 times daily | 38 (23%) | 25 (19%) | ‐ | 13 (33%) | |
| Infant formula feeding | |||||
| Type of infant formula | |||||
| Regular (Cow's milk‐based) | 115 (87%) | ‐ | 58 (83%) | 57 (92%) | |
| Hydrolysed | 11 (8%) | ‐ | 7 (10%) | 4 (6%) | |
| Lactose free | 4 (3%) | ‐ | 4 (6%) | 0 (0%) | |
| Soy based | 2 (2%) | ‐ | 1 (1%) | 1 (2%) | |
| Form of infant formula | |||||
| Ready‐to‐feed | 50 (39%) | ‐ | 20 (29%) | 30 (52%) | |
| Powder | 43 (34%) | ‐ | 25 (36%) | 18 (31%) | |
| Liquid concentrate | 34 (27%) | ‐ | 24 (35%) | 10 (17%) | |
Note: Data presented as n (%) or mean (SD). Percentages may not add to 100% due to rounding. Within each comparison category (gender, age, household income, parental status and education), values labelled with ‘*’ within a row differ from expected values, P < 0.05 (χ 2 test with Bonferroni post hoc test); absence of ‘*’ indicates no significant difference.
Abbreviations: CAD, Canadian dollars; CERB, Canadian Emergency Response Benefit; EI, employment insurance.
N differs due to participants skipping some questions.
Other baby's ethnicities included Filipino (n = 3), Black (n = 2), South Asian (n = 2), Arab (n = 1) and Mexican (n = 1).
Other ethnicities included Filipino (n = 3), South Asian (n = 3), Acadian (n = 2), Black (n = 2), Arab (n = 2) and Latin American (n = 2).
‘Monetary parental benefits’ refers to governmental parental EI in Canada which provides up to 55% of a caregiver's preleave earnings to a maximum of CAD$573 per week for 50 weeks and/or any voluntary ‘top‐ups’ from employers.
In Canada, EI and CERB benefits during the pandemic were available to any adult 15 years or older who lost their job through no fault of their own, including because of COVID‐19 and provided up to CAD$500 per week starting on 15 March 2020 throughout the entire data collection period.
Other changes to income due to COVID‐19 included increase in income (i.e., ‘hero pay’, new job; n = 12), top‐up from employer ended (n = 4), increase in hours worked without an increase in income (n = 2), self‐employed: decrease in business (n = 2) and loss of overtime hours (n = 1).
3.2. COVID‐19‐related information‐seeking behaviours
The majority of caregivers (87%) actively sought out COVID‐19‐related information, with 73% searching for this information once or more per day (Table 2). There were very few differences in information‐seeking behaviours by household income, educational attainment or caregiver age. Most caregivers ranked the internet and social media sites as their key information sources for COVID‐19‐related information. In open‐ended responses regarding infant feeding during the COVID‐19 State of Emergency, 33% (data not shown) of participants looked to specific social media pages (e.g., breastfeeding support groups, La Leche League Facebook page and The Leaky Boob), whereas the internet (e.g., KellyMom.com and a human milk substitute company website) was the second top ranked information source (23%). Other sources listed most to least common were health care professionals, television or radio, the World Health Organization, government sources and word of mouth. When asked about their knowledge of infant feeding and COVID‐19, more than half of participants noted that they should continue breastfeeding, whereas much smaller proportions of participants wrote about precautions related to bottle feeding (e.g., sanitizing bottles and cleaning formula packages; 6%) and general COVID‐19‐related recommendations (e.g., hand washing and self‐isolation; 4%). Over one quarter (29%) of participants reported not knowing anything about infant feeding during COVID‐19.
TABLE 2.
COVID‐19‐related information‐seeking behaviours of participating Nova Scotian caregivers to infants < 6 months
| All | Household income | Completed education level | Age | ||||||
|---|---|---|---|---|---|---|---|---|---|
| <CAD$60,000 | ≥CAD$60,000 | High school or less | College | Undergraduate | Graduate/professional | <35 years | ≥35 years | ||
| Sought out information about COVID‐19 | n = 282 | n = 70 | n = 209 | n = 48 | n = 77 | n = 99 | n = 58 | n = 222 | n = 53 |
| Yes | 245 (87%) | 55 (79%)* | 188 (90%)* | 35 (73%)* | 60 (78%) | 94 (95%)* | 56 (97%) | 190 (86%) | 48 (91%) |
| Frequency of COVID‐19 information seeking a | n = 228 | n = 60 | n = 166 | n = 38 | n = 58 | n = 80 | n = 52 | n = 184 | n = 38 |
| Multiple times per day | 82 (36%) | 18 (30%) | 64 (39%) | 13 (34%) | 14 (24%) | 36 (45%) | 19 (37%) | 59 (32%) | 21 (55%) |
| Daily | 85 (37%) | 20 (33%) | 64 (39%) | 11 (29%) | 25 (43%) | 31 (39%) | 18 (35%) | 74 (40%) | 9 (24%) |
| 1+ times per week | 36 (16%) | 13 (22%) | 23 (14%) | 9 (24%) | 13 (22%) | 7 (9%) | 7 (14%) | 30 (16%) | 5 (13%) |
| Never | 10 (4%) | 7 (12%)* | 3 (2%)* | 4 (11%) | 2 (3%) | 3 (4%) | 1 (2%) | 10 (5%) | 0 (0%) |
| Other b | 15 (5%) | 3 (5%) | 12 (7%) | 1 (3%) | 4 (7%) | 3 (4%) | 7 (13%) | 12 (7%) | 3 (8%) |
| Top ranked sources of COVID‐19 information a | n = 229 | n = 51 | n = 177 | n = 30 | n = 55 | n = 91 | n = 53 | n = 179 | n = 45 |
| Internet | 136 (59%) | 26 (51%) | 109 (62%) | 14 (47%) | 36 (66%) | 53 (58%) | 33 (63%) | 105 (59%) | 28 (62%) |
| Social media | 53 (23%) | 17 (33%) | 36 (20%) | 13 (43%) | 8 (15%) | 25 (28%) | 7 (13%) | 45 (25%) | 7 (16%) |
| Television | 31 (14%) | 7 (14%) | 24 (14%) | 3 (10%) | 9 (16%) | 10 (11%) | 9 (17%) | 22 (12%) | 8 (18%) |
| Other | 9 (4%) | 1 (2%) | 8 (5%) | 0 (0%) | 2 (4%) | 3 (3%) | 4 (8%) | 7 (4%) | 2 (4%) |
| Sought out information about infant feeding and COVID‐19 | n = 280 | n = 69 | n = 208 | n = 46 | n = 77 | n = 99 | n = 58 | n = 220 | n = 53 |
| Yes | 88 (31%) | 48 (70%) | 141 (68%) | 9 (20%) | 24 (31%) | 34 (34%) | 21 (36%) | 67 (31%) | 18 (34%) |
| Top ranked sources of information about infant feeding and COVID‐19 a | n = 106 | n = 28 | n = 78 | n = 15 | n = 32 | n = 38 | n = 21 | n = 80 | n = 22 |
| Internet | 81 (76%) | 17 (61%) | 64 (82%) | 6 (40%)* | 26 (81%) | 33 (87%) | 16 (76%) | 60 (75%) | 18 (82%) |
| Social media | 17 (16%) | 7 (25%) | 10 (13%) | 6 (40%) | 5 (16%) | 4 (11%) | 2 (10%) | 14 (18%) | 3 (14%) |
| Other | 8 (8%) | 4 (14%) | 4 (5%) | 3 (20%) | 1 (3%) | 1 (3%) | 3 (14%) | 6 (8%) | 1 (5%) |
Note: Data presented as n (%). Percentages may not add to 100% due to rounding. Within each comparison category (household income, completed education level and age), values labelled with ‘*’ within a row differ from expected values, P < 0.05 (χ 2 test with Bonferroni post hoc test); absence of ‘*’ indicates no significant difference.
n differs due to participants skipping some questions.
Other frequencies of information seeking included looking monthly (n = 3), looking more often at the beginning of the State of Emergency but less or not at all now (n = 4), only see information passively (n = 2), looked once or twice (n = 4), only checked to see if breastfeeding was possible if infected (n = 1) and every couple weeks to see if information has changed (n = 1).
3.3. Changes to infant feeding due to COVID‐19
Changes to infant feeding experienced during the State of Emergency, with illustrative quotes from participants contextualizing changes, are shown in Table 3. In general, the participating Nova Scotian caregivers experienced minimal COVID‐19‐related changes to their infant's diet, with very few dietary or feeding changes beyond expected age‐related adjustments. Over a quarter (27%) of the caregivers experienced lactation challenges, and of those, 66% described challenges accessing lactation support (e.g., lactation consultants or public health nurses) due to COVID‐19 State of Emergency restrictions.
TABLE 3.
Infant feeding‐related changes experienced by participating caregivers of infants aged < 6 months due to COVID‐19 State of Emergency in Nova Scotia
| N a | Changed since State of Emergency | Change caused by … | Illustrative quote(s): examples of usual (• illustrative of the majority of respondents) and unusual (▪ illustrates ‘cases’ or minority viewpoints) responses | |||
|---|---|---|---|---|---|---|
| COVID‐19 (e.g., food availability and income) | Other factor (e.g., infant age) | Reason unknown | ||||
| Food provided to infant | ||||||
| Breast milk from breast | 333 | 50 (15%) | 3 (6%) | 18 (36%) | 29 (58%) |
• ‘I could not keep my milk supply up with my baby's needs’ • ‘Baby needed more than I produced, so we changed to formula’ • ‘Breast couldn't produce enough milk’ ▪ ‘We spend most of our days topless and skin to skin so she has fed a lot more unrestricted than if we were permitted to go places or have visitors’. ▪ ‘Less bottle feeding since I am apart from baby less’ ▪ ‘Had to breast feed more to try to make up for lack of calories due to running out of formula’ |
| Breast milk from a bottle | 319 | 63 (20%) | 10 (16%) | 26 (41%) | 27 (43%) | |
| Infant formula | 326 | 62 (19%) | 8 (13%) | 24 (39%) | 30 (48%) | |
| Water | 320 | 16 (5%) | 0 (0%) | 12 (75%) | 4 (25%) | • ‘Baby turned 6 months’ |
| Introduced solid foods during COVID‐19 | 335 | 48 (14%) | 4 (8%) | 12 (25%) | 32 (67%) |
• ‘Started showing signs he was ready [for complementary foods]’ • ‘Was going to wait until 6 months but he was very interested so I started a few purees around 5.5 months’ ▪ ‘More time at home has led to increased meals at the table for our family; baby showed interest in food. Also was “something different” to stimulate my baby in the absence of community programs, baby groups, scenery changes, etc.’ ▪ ‘Started one week early for baby to have more things to do to pass the time in the day’ |
| Introduced solids earlier than expected | 16 (33%) | 4 (25%) | 12 (75%) | ‐ | ||
| Feeding habits | ||||||
| Frequency | 335 | 11 (3%) | 5 (45%) | 6 (55%) | ‐ |
• ‘Baby is bored from being home more so I found that my baby would feed a lot more’ ▪ ‘We went with more of a schedule now doing around 7 bottles a day’ |
| Amount | 335 | 7 (2%) | 1 (14%) | 6 (86%) | ‐ |
• ‘We decreased my babies food intake an ounce or 2 due to him spitting up a lot’. ▪ ‘Ran out of formula at one point and store didn't have any in stock …’ |
| Food safety | 327 | 20 (6%) | 20 (6%) | 0 (0%) | ‐ |
• ‘I'm more careful about regular sanitizing as opposed to just thorough cleaning’. ▪ ‘Use dishwasher, don't have time to handwash and sanitize as much’ |
| Feeding style altered to limit potential spread of COVID‐19 | 333 | 40 (12%) | 40 (100%) | 0 (0%) | ‐ |
• ‘More hand washing’ ▪ ‘I pumped before COVID‐19, stopped because of all of the sanitizing’. |
| Primary caregiver no longer shops in‐store or does not shop in‐store as frequently | 282 | 242 (86%) | ‐ | ‐ | ‐ | ▪ ‘I still shop in‐store but I don't bring my kids unless my mother is absolutely unavailable and I have no other option and it cannot wait’ |
| Breastfeeding | ||||||
| Challenges | 264 | 71 (27%) | 6 (8%) | 62 (87%) | 3 (4%) |
• ‘Engorgement, nipple blanching, decreased milk supply’ ▪ ‘… with my other children being home from school and trying to enforce homeschooling while breastfeeding a newborn. I prefer to feed on demand, and let baby nurse until they are done even if it's purely for comfort. That had been affected as there is more demand for my time and attention now’. |
| Different access to breastfeeding support | 71 | 47 (66%) | 42 (59%) | 5 (7%) | ‐ |
• ‘We had to give up on breastfeeding directly because the public health nurse who was trying to help us wasn't allowed to do home visits and it's impossible to trouble shoot breastfeeding over the phone when the child isn't latching or feeding from the breast no matter how perfect the technique. Now I have to pump 100%’ ▪ ‘I would have reached out to other mothers online’ |
| Positive experiences | 264 | 50 (19%) | 33 (66%) | 16 (32%) | 1 (2%) |
• ‘Breastfeeding was hard for us. We had to get lactation consultant and tongue tie fix in month 2‐3. We were just settling into feeding when pandemic started. Because I have nowhere to go now I spend a lot more time relaxing with baby and doing comfort nursing. I would have felt pressure to be on the go with baby but pandemic has allowed me to relax with baby and focus on breastfeeding’ ▪ ‘Gradually getting the hang of things with less pain’ |
| Now pump milk more often | 174 | 42 (24%) | 26 (62%) | 14 (33%) | 1 (2%) |
• ‘Wanted to ensure I have milk stored in case I was to get sick my partner would have EBM to use’ ▪ ‘Baby's preference to bottle has increased’ |
| Now pump milk less often | 174 | 51 (29%) | 36 (71%) | 12 (24%) | 3 (6%) |
• ‘… I won't be away from him because of the pandemic. So, I don't feel a need to store breastmilk in the freezer for bottles since I won't be going out’ ▪ ‘Prescribed Domperidone’ |
| Formula feeding | ||||||
| Formula form | 133 | 28 (21%) | 15 (54%) | 12 (43%) | 1(3%) |
• ‘Needed to use both stage 1 and stage 2 formula because there wasn't enough stage one available at stores’. ▪ ‘We ran out of the ready‐made and were naturally ready to switch to powder’. |
Data presented as n (%). Percentages may not add to 100% due to rounding.
Abbreviation: EBM, expressed breast milk.
N differs due to participants skipping some questions.
A number of concerning challenges were reported by individual participants which were not common across the whole sample. For instance, one participant reported adding more water to formula in order to conserve it, whereas two reported feeding other foods in lieu of formula because of financial constraints caused by COVID‐19. Similarly, four participants reported introducing solids earlier than expected due to perceived infant boredom brought on by COVID‐19 isolation restrictions.
3.4. Perceived impacts of the COVID‐19 State of Emergency
Quotes selected to illustrate prominent themes regarding the impact of the COVID‐19 State of Emergency on the participating caregiver–infant dyads and infant feeding are presented in Box 1. Common concerns emerged around the impact of isolation on both infants and caregivers, access to health care and related potential health consequences and mixed feelings of relief and concern around infant feeding. Open‐ended responses also demonstrated difficulties accessing infant formula, particularly specialized formulas, causing concern about running out.
3.5. Perceived stress and concerns of caregivers
The majority of participants were categorized as experiencing moderate perceived stress (n = 252, 77%) based on their responses to the Perceived Stress Scale, with only 19 (6%) experiencing high perceived stress (see Figure 1). Of investigator‐generated potential concerns, 144 (51%) participants reported often or always being concerned about going outside, and 120 (43%) were often or always concerned about their infant missing check‐ups.
FIGURE 1.
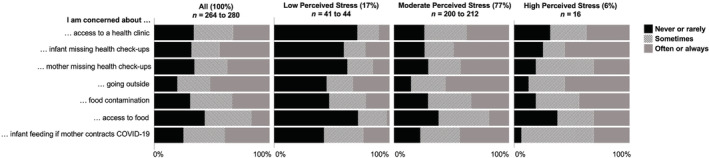
Self‐rated caregiver concerns about various activities and issues with potential to be impacted by the COVID‐19 State of Emergency, displayed by participants' Perceived Stress Scale score
When asked about their top concern in an open‐ended question, participants most commonly cited the risk of COVID‐19 infection and the safety of their infant (n = 153, 63%). One quarter (25 of 98 responses) of participants reported issues with formula access, such as the affordability of formula, and shortages in general, but particularly specialized formulas (e.g., lactose free and hydrolysed). Some caregivers reported feelings of stress and fear associated with the COVID‐19 pandemic (n = 25, 26%). Nine breastfeeding caregivers who reported experiencing a perceived low milk supply cited stress as the cause (27%) in open‐ended responses; nine others expressed a fear of developing low milk supply due to COVID‐19‐related stress. Some caregivers made positive comments regarding breastfeeding (n = 18, 18%) such as being thankful for being able to breastfeed through the State of Emergency, spending more time with their infant or referring to breastfeeding as protective because they had not perceived many lifestyle or caregiving changes due to the COVID‐19 State of Emergency.
Box 1
Participant quotes illustrative of prominent themes related to caregiver experiences during the COVID‐19 State of Emergency in Nova Scotia
Impact of the COVID‐19 pandemic on the infant
‘I am concerned about socialization as he was a very anxious baby … I'm concerned about taking him to the doctor's office for vaccines. I'm scared if he's allergic to food that he might not get the necessary treatment right away for long‐term impact. I'm scared of him needing to go to the [local children's hospital] if it's overwhelmed with COVID‐19 cases. It is basically illegal to have the village raise the child with you so parents are all alone and shamed if they are having trouble’. Primiparous formula‐feeding mother, 31 years old
‘Infection of my baby—insufficient data to truly conclude [that COVID‐19] is benign for babies, though I'd be more concerned about elderly relatives’. Primiparous breastfeeding mother, 32 years old
‘Lack of socialization with other babies, grandparents and extended families. Lack of activities like going to the park, or swim lessons, I'll have less time to share these activities when I return to work, so I feel we've missed out on these special moments. And of course, [I'm concerned about] him getting sick’. Primiparous breastfeeding mother, 30 years old.
Impact of COVID‐19 on mothers
‘It has been isolating. Being separated from family and friends and not being able to engage in Public Health drop‐ins or breastfeeding/baby groups has been challenging. I have also felt my health, postpartum, is/was more neglected by myself due to the inconvenience of medical appointments and the closure of clinics. I feel very frustrated and anxious most of the time’. Primiparous breastfeeding mother, 36 years old
‘Of course the worry is always there that your kids could get sick. I also worry about my own mental health during isolation and how that may affect my baby. Being isolated from our extended family and his exposure being limited to our house and yard. As he gets older I hope we are able to have more socializing with friends and family’. Multiparous breastfeeding mother, 36 years old
Breastfeeding during COVID‐19 pandemic
‘This emergency has caused me to reconsider switching to formula after 6 months of breastfeeding, which was my original plan. I now intend to continue nursing until approximately 12 months for several reasons—health benefits for baby, not worrying about availability of formula, etc.’. Primiparous breastfeeding mother, 31 years old
‘I definitely feel more pressure when it comes to breastfeeding. I feel like I need to do it with this whole [COVID‐19] thing going on … I constantly worry about losing my supply and what I would do. I do have a stash built up in the freezer for if he had to slowly switch to formula!’ Primiparous breastfeeding mother, 23 years old
Formula feeding during COVID‐19 pandemic
‘I went from breastfeeding to formula feeding after a month of my son being born. I feel like the stress of being isolated and him not getting the proper attention from public health visits to doctors visits (since they have all been over the phone) made me unable to produce enough milk for him. Also, me not knowing his weight weekly (public health and doctors) scared me into switching to formula since it guaranteed him gaining weight. It was scary trying to find a good formula for him and making sure he was able to have access to it at these times since a lot of people stockpiled the first couple weeks and I was behind’. Multiparous formula‐feeding mother, 28 years old
‘I find it especially stressful and guilt inducing to be formula feeding. I already felt guilty because of all of the “breast is best” encouragement; and I tried so hard to breastfeed. I felt like a failure for not succeeding with it and have been ashamed. Now formula is hard to acquire and I'm worried about the supply chain’. Primiparous formula‐feeding mother, 32 years old
‘Not being able to find my daughter's formula. I've spent hours crying over this. She has an intolerance to lactose and is on [Brand] formula … Now with people stock piling and hoarding formula I worry I won't find this for her. I keep one case ahead if possible in case of a temporary shortage’. Multiparous formula‐feeding mother, 30 years old
‘[The baby] growing properly because I switched to a lesser known, cheaper brand of formula’. Primiparous formula‐feeding mother, 26 years old
‘Try to break [feeding] up to conserve formula, give water in between’. Multiparous formula‐feeding mother, 24 years old
Access to health care
‘Concerned that [the baby] is not getting the follow up care that was provided prior to COVID‐19 pandemic. This is the reason that his weight gain issues were only caught at 4 weeks’. Primiparous breastfeeding mother, 36 years old
‘Our biggest issue was losing our lactation consultants due to COVID‐19. We dealt with a tongue tie, thrush, and hard letdown within a few weeks of the COVID measures being put in place, and essentially had to deal with these on our own. We were able to get the tongue tie clipped right as measures were being introduced, but all follow up visits were cancelled and we felt overwhelmed trying to figure out feeding and healing without any professional help’. Primiparous breastfeeding mother, 31 years old
‘I would of like to meet with my doctor. My 6‐week appointment got cancelled and a doctor never followed up with me since I gave birth. No one has checked in about my healing or offered me birth control’. Primiparous breastfeeding mother, 28 years old
Isolation and family supports
‘If I got sick, who would look after my children? What would happen to my baby to be fed if I ended up in hospital?’ Multiparous breastfeeding mother, 35 years old
‘… I am worried to have to be hospitalized and not be able to care for my baby … With the social distancing and isolation we have already completely lost our support system for early baby care. We would be in real trouble if I get sick. We have some breastmilk frozen in case but only about 4 days worth so if I am seriously ill my husband would have to start using formula’. Primiparous breastfeeding mother, 35 years old
4. DISCUSSION
The global COVID‐19 pandemic and related State of Emergency measures have created a novel emergency with prolonged impacts on multiple aspects of daily life (World Health Organization, 2020b). This exploratory study was designed to gain insights into how the COVID‐19 pandemic and associated State of Emergency in Nova Scotia impacted caregivers and young infants. We found that participating caregivers perceived stress and held many concerns, but few changed infant feeding behaviours. Of note, the changes in attitudes and behaviours as a result of the State of Emergency did not appear to impact any one sociodemographic group differently; in fact, our results were similar across income and educational attainment levels, population density, parity, age and ethnicity. Despite 99% of participants self‐identifying as White, our sample was not vastly different from the Nova Scotian population, where only 6.5% of people self‐identify as a visible minority (The Government of Canada, 2017). Likewise, only 21.4% of women have no certificate diploma or degree in Nova Scotia, as compared with 18% in our sample. However, there were a large number of caregivers with high household incomes and levels of education in our sample, and therefore, results may not represent the experiences of caregivers with lower household incomes or education levels who may be the most vulnerable.
4.1. Socio‐economic impacts
In the United States, where financial supports included a one‐time stimulus check for those with a low income, and up to US$300 a week (in 35 states) for those unemployed due to COVID‐19 (United States Government, 2020), disproportionate effects of the COVID‐19 pandemic have been reported among those earning a low income (Kim & Bostwick, 2020; Niles et al., 2020; Wolfson & Leung, 2020), minority race or ethnic groups (Kim & Bostwick, 2020; Webb Hooper, Nápoles, & Pérez‐Stable, 2020) and families with children (Lauren Bauer, 2020). This does not align with our study, where infant feeding did not differ in type or frequency across socio‐economic characteristics, likely because 77% of participants were receiving parental EI benefits before COVID‐19, and only 12% experienced a loss of household income without EI or CERB. These findings suggest that for those who are eligible, governmental economic supports may mitigate some of the expected household impacts of income loss associated with the pandemic (Pérez‐Escamilla, Cunningham, & Moran, 2020). This further supports the importance of paid parental leave on optimal infant feeding practices, such as longer duration of exclusive breastfeeding, as demonstrated by Baker and Milligan (2008).
4.2. COVID‐19‐related information‐seeking behaviour
Caregivers' top ranked sources for information about COVID‐19 were the internet and social media, particularly parent support groups and specific organizations/institutions (e.g., the WHO) or social media pages (e.g., the Leaky Boob). This aligns with the findings of a recent survey in Taiwan (n = 1904), where 81% of participants found COVID‐19 information online (Ko et al., 2020). As demonstrated by participants in the current study, social media is also an important source of information and support, despite high levels of problematic misinformation known to be circulating on social media (Asiodu, Waters, Dailey, Lee, & Lyndon, 2015; Holtz, Smock, & Reyes‐Gastelum, 2015), especially regarding COVID‐19 (Bastani & Bahrami, 2020). When asked to self‐report knowledge, a small proportion of participants (4%) cited incorrect feeding recommendations, such as the need to isolate a mother from her infant and to cease feeding at the breast. Similarly concerning, many (29%) reported not knowing anything regarding infant feeding during the COVID‐19 pandemic. However, 42% of our participant group correctly identified that breastfeeding should continue as usual regardless of mother's COVID‐19 infection status (World Health Organization, 2020c). Although some participants specifically referenced looking for information from credible government and/or health organizations such as the WHO, most information was sought from social media pages that were likely more familiar to caregivers before the pandemic, such as parent support groups. As such, credible sources should investigate paying for ads or partnering with social media influencers or popular parenting sites to ensure accurate, up‐to‐date, evidence‐based information is shared where caregivers are most likely to see it.
4.3. Changes to infant feeding due to COVID‐19
Caregivers who fed their infants infant formula reported stockpiling or buying the product more often during the State of Emergency. This is not surprising, as stockpiling has also become common practice during the COVID‐19 pandemic in China, especially among women of higher education and income (Wang, An, Gao, Kiprop, & Geng, 2020), similar to the sociodemographic profile of our study. This behaviour has also been observed in other types of emergencies such as Hurricane Sandy (New York City, 2012), the Tōhoku earthquake and tsunami‐induced nuclear power plant disaster (Japan, 2011) and the Fort McMurray wildfires (Alberta, Canada, 2016) (Bloomberg, 2012; DeYoung et al., 2018; Wang, An, Gao, Kiprop, & Geng, 2020). Unfortunately, stockpiling results in retail stock‐outs and can pose a serious risk to the food system (E. Wang, An, et al., 2020). Participants in this study reported driving further, or to multiple stores, to find their preferred or required infant formula type or brand, whereas others reported switching to a more commonly available or cheaper brand or form. Due to the risks of stockpiling and the vulnerability of formula‐fed infants (access, watering down, switching to inappropriate alternatives), the development of an online registry of products should be considered, so caregivers can assess availability of their infant's formula online, across multiple stores. Such a resource could prevent placing excess financial strain on those who are already at high risk of infant food insecurity and reduce the risk of pathogen exposure for caregivers who would otherwise have to visit multiple stores.
Human milk expression (‘pumping’) has become a common practice for caregivers in high‐income countries (Johns et al., 2013). Before the COVID‐19 State of Emergency, this practice was typically related to medical lactation issues such as mastitis or nipple pain, oversupply or undersupply of milk, to avoid breastfeeding in public, to allow other people to feed the infant, or to return to work or other work‐related constraints (Johns, Forster, Amir, & McLachlan, 2013). As circumstances have changed due to COVID‐19, so have caregivers' pumping behaviours. Participants who indicated pumping less frequently referenced ‘stay at home’ orders, explaining that they did not have to breastfeed in public or in the presence of other people, and having expressed human milk ready to be fed by another person, such as a babysitter, was no longer necessary. This may be one of various unanticipated positive effect of the pandemic, as increased breastfeeding at the breast can improve responsiveness during feeding, which has been shown to have long‐lasting health benefits for the infant (Bartok & Ventura, 2009; Ventura, 2017).
Though there were many reported negative impacts of the COVID‐19 pandemic, participants also reported unanticipated positive experiences, including less pressure and more time with their baby, which has been reported by others. Like those in our study, Nova Scotian caregivers who responded to an open‐ended survey on post‐partum experiences during the COVID‐19 pandemic also described a complex time, reporting not only negative themes, such as isolation, but also ‘blessings’, such as freedom from social expectations and more family bonding time (Joy et al., 2020). Unanticipated positive impacts of the COVID‐19 pandemic have also been reported by breastfeeding women surveyed in the United Kingdom, who experienced more privacy, fewer visitors and increased responsive feeding (Brown & Shenker, 2021).
Many participants who reported an increase in pumping referenced the common practice of increasing milk supply (World Health Organization, 2009; Johns et al., 2013) or building a ‘stash’ of human milk to ensure their infant had food if caregivers were to be separated due to COVID‐19 infection, even though separation is not recommended. Although freezing and thawing expressed milk may result in some nutrient and bioactive losses, and an increased risk of contamination due to handling (Johns et al., 2013), mother's own expressed milk remains the best option before supplementing with donor human milk or infant formula under normal circumstances. However, there is a lack of evidence for pumping and feeding mother's own expressed human milk during emergencies, likely due to inconsistencies in inclusion of feeding expressed human milk in the definition of ‘breastfeeding’ (American Academy of Pediatrics, 2015; Calil, Krebs, & Brunow De Carvalho, 2020; Carothers & Gribble, 2014; Johns et al., 2013). Future guidelines on infant feeding during COVID‐19 and other emergencies should specifically include consideration of mother's own expressed milk, if available and safe, as the optimal second choice in case of separation.
4.4. Lack of access to post‐partum support and services
The COVID‐19 State of Emergency and associated restrictions on in‐person services resulted in the cancellation of post‐partum appointments, lactation services and programmes offered by public health such as home visits and family‐drop‐in services (Reproductive Care Program of Nova Scotia, 2020), which left participants in our study feeling unsupported. Many were impacted specifically by a lack of access to public health nurses, who were highlighted in a 2014 study as strong enablers to continued breastfeeding, reducing stress and building confidence among Nova Scotian mothers (Aston et al., 2014). Participants in the current study cited the lack of public health programmes as detrimental in various aspects of infant health. For instance, participants reported reduced opportunities for infant growth tracking, leading to delayed observation of growth faltering or the introduction of infant formula to more closely control their infant's food intake. Similarly, breastfeeding caregivers discussed having to tackle lactation problems on their own due to a lack of access to certified lactation consultants, which are being increasingly recognized as playing an important role in improving breastfeeding outcomes (Haase, Brennan, & Wagner, 2019). Given the need identified through the current study, future programmes should attempt to closely replicate face‐to‐face health services. For instance, during the 7.1 magnitude earthquake in Mexico in 2017, International Board Certified Lactation Consultants (IBCLC) from the Asociacion de Consultores Certificados en Lactancia Materna de Mexico rapidly responded by promoting free lactation support through the popular mobile social media application WhatsApp, allowing mothers to easily access personal, professional, evidence‐based support wherever they were in the emergency (Buccini, Harding, Hromi‐Fiedler, & Pérez‐Escamilla, 2019). If appropriate personal protective equipment is not available for face‐to‐face interactions, adequate public health supports for caregivers, including specialized services such as relactation, may be delivered through a similar private social media platform that allows voice or text chats with photograph or video exchange staffed by health care professionals.
4.5. Perceived stress and concerns of caregivers
Stress was a key theme throughout the survey. Three quarters of study participants were categorized as experiencing moderate perceived stress on the Perceived Stress Scale, and many reported feelings of stress and fear in their open‐ended responses related to COVID‐19, parenting without in‐person public health supports and the potential long‐term consequences of the State of Emergency on themselves and their infants' health (Table 3 and Box 1). Caregivers often report elevated psychological stress levels, especially in the first year post‐partum, which despite being common, can negatively impact feeding interactions, responsiveness, bonding, sleep and infant health overall (Field, 2018; Hurley, Black, Papas, & Caufield, 2008; Perren, Von Wyl, Bürgin, Simoni, & Von Klitzing, 2005). Increased stress levels have been observed during past infectious outbreak emergencies (Hirani et al., 2019), where people experience increased fears associated with morbidity and mortality (Hall, Hall, & Chapman, 2008) compounded by the closure of schools and businesses (Van Bortel et al., 2016). Higher than normal levels of stress were also observed in China during the current COVID‐19 pandemic, particularly among women (C. Wang, Pan, et al., 2020). Similar to previous research (Maehara et al., 2017), we did not find significant differences in stress levels between breastfeeding and infant formula‐feeding caregivers; however, the observed challenges and emotions experienced by each were very different.
There is a common misconception that mothers cannot breastfeed during emergencies because the stress will limit the quality and/or quantity of milk produced (Hirani et al., 2019). Although there is a physiologically plausible pathway by which stress could impair lactation (Lau, 2001), to date, there is limited evidence that maternal stress can adversely impact milk supply. However, breastfeeding relaxation interventions have been shown to improve breastfeeding outcomes, and a recent meta‐analysis has shown improved milk production with musical therapy for relaxation (Düzgün & Özer, 2020; Shukri, Husna, Wells, & Fewtrell, 2018). Regardless, several participants in the current study cited stress as the cause of their self‐perceived low milk supply. This is in line with previous research reporting perceptions of stress‐induced low milk supply among mothers after the Fort McMurray wildfires in Alberta, Canada, in 2016, who, like the participants of the current study, specifically described stress associated with a lack of in‐person lactation supports (DeYoung et al., 2018). Caregivers in our study also expressed concern over losing their milk supply if they were to be infected with COVID‐19, despite the recommendation to continue to breastfeed or pump and to consider relactation after recovery if milk supply were affected (IFE Core Group, 2017; World Health Organization, 2020a).
Stress among infant formula‐feeding caregivers centred more around concerns of access and infant food security. Approximately 90% of Nova Scotian infants under 6 months of age are formula fed (Brown et al., 2013). Infant formula is expensive: in Nova Scotia, regular, powdered infant formula costs CADC$73.61 per month (Frank et al., 2020), with other powdered formulas (e.g., thickened, soy protein and partially hydrolysed) costing upwards of CAD$150 per month, and ready‐to‐feed infant formula, which is recommended for the first 2 months, costing CAD$380 per month (Parent Health Education Resource Working Group, 2015). Job loss, or even just a decrease in wages, could substantially impact a family's ability to purchase infant formula, potentially driving caregivers to seek infant formula from food banks, or to introduce potentially risky alternatives such as cow's milk or solids, as mentioned by our study participants.
Social supports for mothers, especially organized groups (McLeish & Redshaw, 2017; Strange, Fisher, Howat, & Wood, 2014), are known to have positive impacts on mothers' levels of parenting stress (Telleen, Herzog, & Kilbane, 1989), as well as feelings of isolation (Strange et al., 2014), emotional well‐being (McLeish & Redshaw, 2017) and exclusive breastfeeding duration (Laugen, Islam, & Janssen, 2016). Unfortunately, in‐person play groups, public health home visits and events and programmes for families were cancelled at least for the duration of the study due to restrictions on social gatherings (Government of Nova Scotia, 2020a). Despite some programmes continuing or restarting virtually, many participants reported feeling socially isolated, concerned about infant socialization and lacking support from friends and family. Inconsistent or lack of social support is a known contributor to post‐partum depression (Cutrona & Troutman, 1986; Howell, Mora, & Leventhal, 2006), so being unable to have family physically close for instrumental support, or to socialize and seek peer support, could have detrimental impacts on both mothers and infants, as well as infant feeding outcomes (Dennis & McQueen, 2009).
4.6. Caregivers' feelings
Over the last decade, researchers have argued that Canadian mothers feel pressure to breastfeed due to the prevailing societal view that breastfeeding is an integral aspect of ‘good motherhood’ (Andrews & Knaak, 2013; Knaak, 2010), with formula‐feeding caregivers often expressing feelings of guilt, remorse and shame due to their perceived failure to achieve this standard (Lee, 2008; Taylor & Wallace, 2019; Thomson, Ebisch‐Burton, & Flacking, 2015). Similarly, during the COVID‐19 State of Emergency, related issues with access to formula have were described by some participants as the cause for feelings of guilt and shame for ‘choosing’ a less reliable feeding method. In contrast, some breastfeeding participants described feelings of gratitude and perceived being ‘lucky’ or ‘blessed’ for being able to continue breastfeeding (Box 1). Mental health was a similarly important theme in the New Mum Study in the United Kingdom, where the majority of participants reported symptoms of low mood, anxiety and loneliness during the COVID‐19 pandemic (Dib, Rougeaux, Vázquez‐Vázquez, Wells, & Fewtrell, 2020). These results emphasize the importance of caregiver mental health care during and after the COVID‐19 State of Emergency, especially for caregivers who have experienced difficulty feeding their infants. The results of the current study particularly highlight the importance to support not only breastfeeders but also formula feeders, who are more vulnerable to supply chain issues, and potentially, to mental health issues, during emergencies.
4.7. Strengths and limitations
This study was the first to explore caregivers' perceptions of infant feeding and health in Atlantic Canada. Researchers recently identified low knowledge of infant and young child feeding recommendations in the general population of Nova Scotia (Chan & Whitfield, 2020), which has one of the lowest breastfeeding rates in the country (Statistics Canada, 2018). A strength of this study is the use of both closed‐ and open‐ended questions, which were used complementarily to gain a holistic view of caregivers' experiences. A limitation of this study is the study population, which, through convenience sampling, was made up primarily of White, breastfeeding women with high socio‐economic status, despite efforts to recruit participants from different populations by promoting the study across numerous social media platforms and groups. This may be because we sought caregivers with infants less than 6 months of age, so responses were almost entirely from caregivers who were at home with their infants and earning parental benefits rather than those in low‐paying, and often essential, jobs that would yield lower government parental benefits. Likewise, our focus on web‐based advertising may have excluded those with poorer English literacy or without access to internet. Therefore, these results may not reflect the experiences of those in more challenging circumstances who may be more vulnerable to the impacts of the pandemic.
5. CONCLUSIONS
The COVID‐19 State of Emergency has impacted the Nova Scotian caregivers who participated in this study, resulting in stress, feelings of isolation and lack of support (family, friends and health care), and some limited adverse feeding practices such as early cessation of breastfeeding or introduction of solid foods. These issues have potential to result in life‐long impacts on the health of the infant. As infants are a highly vulnerable group, every effort should be made on the level of the government, community and individual, to support caregivers in feeding their infants, especially during emergencies. Therefore, interventions to increase access to health care services in the post‐partum period, allow for personal lactation and infant feeding supports, and implementing systems to ease access to infant foods (e.g., online inventory system) could reduce barriers currently experienced by caregivers in Nova Scotia. Lessons from this unique emergency may inform future public health programmes, in future COVID‐19 outbreaks or other prolonged emergencies.
CONFLICTS OF INTEREST
Authors declare no conflicts of interest. The funder had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
CONTRIBUTIONS
HLF and KCW conceived the study, and KCW obtained funding. HLF, OL, KK, JLB, JG and KC designed the study tools and assisted with data collection. HLF, OL, KK, JLB, JG and KC analysed the data, overseen by KCW. HLF and KCW drafted the manuscript. All authors have contributed to the intellectual content of and have read and approved the manuscript; KCW is responsible for the final version of the manuscript.
ACKNOWLEDGMENTS
We thank all the participants of this study. This study was funded by a Nova Scotia COVID‐19 Health Research Coalition grant (HRC‐2020‐082). HLF, KC and KK are supported by Research Nova Scotia, Scotia Scholars Awards. JLB and OL are supported by Nova Scotia Research and Innovation Graduate Scholarships. JG is supported by a Canadian Institute of Health Research Canada Graduate Scholarship—Masters Award.
Fry HL, Levin O, Kholina K, et al. Infant feeding experiences and concerns among caregivers early in the COVID‐19 State of Emergency in Nova Scotia, Canada. Matern Child Nutr. 2021;17:e13154. 10.1111/mcn.13154
Funding information Nova Scotia COVID‐19 Health Research Coalition , Grant/Award Number: HRC‐2020‐082; Research Nova Scotia, Scotia Scholars Awards; Nova Scotia Research and Innovation Graduate Scholarships; Canadian Institute of Health Research Canada Graduate Scholarship—Masters Award
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- American Academy of Pediatrics . (2015). Infant feeding in disasters and emergencies: Breastfeeding and other options. AAP Policy and Publications. [Google Scholar]
- Andrews, T. , & Knaak, S. (2013). Medicalized mothering: Experiences with breastfeeding in Canada and Norway. The Sociological Review, 61(1), 88–110. 10.1111/1467-954X.12006 [DOI] [Google Scholar]
- Asiodu, I. V. , Waters, C. M. , Dailey, D. E. , Lee, K. A. , & Lyndon, A. (2015). Breastfeeding and use of social media among first‐time African American mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(2), 268–278. 10.1111/1552-6909.12552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aston, M. , Price, S. , Etowa, J. , Vukic, A. , Young, L. , Hart, C. , … Randel, P. (2014). Listening to the voices of mothers and public health nurses: Personal, social, and institutional aspects of early home visits. Retrieved from https://cdn.dal.ca/content/dam/dalhousie/pdf/healthprofessions/SchoolofNursing/faculty_docs/Listening_to_the_Voices_of_Mothers_and_Public_Health_Nurses_Personal_Social_and_Institutional_Aspects_of_Early_Home_Visits.pdf
- Attride‐Stirling, J. (2001). Thematic networks: an analytical tool for qualitative research. Qualitative Research, 1(3), 385–405. 10.1177/146879410100100307 [DOI] [Google Scholar]
- Baker, M. , & Milligan, K. (2008). Maternal employment, breastfeeding, and health: Evidence from maternity leave mandates. Journal of Health Economics, 27, 871–887. [DOI] [PubMed] [Google Scholar]
- Bartok, C. J. , & Ventura, A. K. (2009). Mechanisms underlying the association between breastfeeding and obesity. International Journal of Pediatric Obesity, 4(4), 196–204. 10.3109/17477160902763309 [DOI] [PubMed] [Google Scholar]
- Bastani, P. , & Bahrami, M. A. (2020). COVID‐19 related misinformation on social media: A qualitative study from Iran. Journal of Medical Internet Research. 10.2196/18932 [DOI] [PubMed] [Google Scholar]
- Beasley, T. M. , & Schumacker, R. E. (1995). Multiple regression approach to analyzing contingency tables: Post hoc and planned comparison procedures. The Journal of Experimental Education, 64(1), 79–93. 10.1080/00220973.1995.9943797 [DOI] [Google Scholar]
- Benzies, K. M. (2008). Advanced maternal age: Are decisions about the timing of child‐bearing a failure to understand the risks? Canadian Medical Association Journal, 178(2), 183–184. 10.1503/cmaj.071577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloomberg, M. R. (2012). Mayor Bloomberg updates New Yorkers on city response to Hurricane Sandy. Retrieved from https://www1.nyc.gov/office-of-the-mayor/news/385‐12/mayor‐bloomberg‐new‐yorkers‐city‐response‐hurricane‐sandy
- Brown, A. , & Shenker, N. (2021). Experiences of breastfeeding during COVID‐19: Lessons for future practical and emotional support. Maternal & Child Nutrition, 17(1), e13088. 10.1111/mcn.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, C. R. L. , Dodds, L. , Attenborough, R. , Bryanton, J. , Rose, A. E. , Flowerdew, G. , … Semenic, S. (2013). Rates and determinants of exclusive breastfeeding in first 6 months among women in Nova Scotia: A population‐based cohort study. CMAJ Open, 1(1), E9–E17. 10.9778/CMAJO.20120011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buccini, G. , Harding, K. L. , Hromi‐Fiedler, A. , & Pérez‐Escamilla, R. (2019). How does “Becoming Breastfeeding Friendly” work? A programme impact pathways analysis. Maternal & Child Nutrition, 15(3), e12766. 10.1111/mcn.12766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bushnik, T. , & Garner, R. (2008). The children of older first‐time mothers in Canada: Their health and development. Statistics Canada. [Google Scholar]
- Calil, V. M. L. T. , Krebs, V. L. J. , & Brunow De Carvalho, W. (2020). Guidance on breastfeeding during the Covid‐19 pandemic. Revista da Associação Médica Brasileira, 66(4), 541–546. 10.1590/1806-9282.66.4.541 [DOI] [PubMed] [Google Scholar]
- Callaghan, W. M. , Rasmussen, S. A. , Jamieson, D. J. , Ventura, S. J. , Farr, S. L. , Sutton, P. D. , … Posner, S. F. (2007). Health concerns of women and infants in times of natural disasters: Lessons learned from Hurricane Katrina. Maternal and Child Health Journal, 11(4), 307–311. 10.1007/s10995-007-0177-4 [DOI] [PubMed] [Google Scholar]
- Carothers, C. , & Gribble, K. (2014). Infant and young child feeding in emergencies. Journal of Human Lactation, 30(3), 272–275. 10.1177/0890334414537118 [DOI] [PubMed] [Google Scholar]
- Chan, K. , & Whitfield, K. C. (2020). High confidence, yet poor knowledge of infant feeding recommendations among adults in Nova Scotia, Canada. Maternal & Child Nutrition, 16(2), e12903. 10.1111/mcn.12903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cutrona, C. E. , & Troutman, B. R. (1986). Social support, infant temperament, and parenting self‐efficacy: A mediational model of postpartum depression. Child Development, 57(6), 1507–1518. 10.2307/1130428 [DOI] [PubMed] [Google Scholar]
- Dennis, C. L. , & McQueen, K. (2009). The relationship between infant‐feeding outcomes and postpartum depression: A qualitative systematic review. Pediatrics, 123(4), e736–e751. 10.1542/peds.2008-1629 [DOI] [PubMed] [Google Scholar]
- DeYoung, S. E. , Chase, J. , Branco, M. P. , & Park, B. (2018). The effect of mass evacuation on infant feeding: The case of the 2016 Fort McMurray Wildfire. Maternal and Child Health Journal, 22(12), 1826–1833. 10.1007/s10995-018-2585-z [DOI] [PubMed] [Google Scholar]
- Dib, S. , Rougeaux, E. , Vázquez‐Vázquez, A. , Wells, J. C. K. , & Fewtrell, M. (2020). Maternal mental health and coping during the COVID‐19 lockdown in the UK: Data from the COVID‐19 New Mum Study. International Journal of Gynecology & Obstetrics, 151(3), 407–414. 10.1002/ijgo.13397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Düzgün, M. V. , & Özer, Z. (2020). The effects of music ıntervention on breast milk production in breastfeeding mothers: A systematic review and meta‐analysis of randomized controlled trials. Journal of Advanced Nursing, 76(12), 3307–3316. 10.1111/jan.14589 [DOI] [PubMed] [Google Scholar]
- Eneroth, H. , Persson, L. , El Arifeen, S. , & Ekström, E. (2011). Infant anaemia is associated with infection, low birthweight and iron deficiency in rural Bangladesh. Acta Paediatrica, 100(2), 220–225. 10.1111/J.1651-2227.2010.02011.X [DOI] [PubMed] [Google Scholar]
- Field, T. (2018). Postnatal anxiety prevalence, predictors and effects on development: A narrative review. Infant Behavior and Development, 51, 24–32. 10.1016/J.INFBEH.2018.02.005 [DOI] [PubMed] [Google Scholar]
- Frank, L. (2020). Out of milk: Infant food insecurity in a rich nation. UBC Press. [Google Scholar]
- Frank, L. , Waddington, M. , Sim, M. , Rossiter, M. , Grant, S. , & Williams, P. L. (2020). The cost and affordability of growing and feeding a baby in Nova Scotia. Canadian Journal of Public Health, 111(4), 531–542. 10.17269/s41997-020-00306-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada . (2020a). Canada child benefit (CCB). Retrieved December 14, 2020, from https://www.canada.ca/en/revenue‐agency/campaigns/covid‐19‐update/covid‐19‐ccb‐payment‐increase.html
- Government of Canada . (2020b). Canada Emergency Response Benefit (CERB). Retrieved September 4, 2020, from https://www.canada.ca/en/services/benefits/ei/cerb‐application.html
- Government of Canada . (2020c). EI maternity and parental benefits: What these benefits offer. Retrieved July 6, 2020, from https://www.canada.ca/en/services/benefits/ei/ei‐maternity‐parental.html
- Government of Canada . (2020d). Labour Force Survey. Retrieved from https://www150.statcan.gc.ca/n1/daily‐quotidien/200710/dq200710a‐eng.pdf
- Government of Nova Scotia . (2020a). Coronavirus (COVID‐19): Case data. Retrieved September 27, 2020, from https://novascotia.ca/coronavirus/data/
- Government of Nova Scotia . (2020b). Coronavirus (COVID‐19): Restriction updates. Retrieved August 31, 2020, from https://novascotia.ca/coronavirus/restriction‐updates/
- Government of Nova Scotia: Finance and Treasury Board . (2017). Nova Scotia Department of Finance—Statistics. Retrieved September 4, 2020, from https://www.novascotia.ca/finance/statistics/archive_news.asp?id=13155
- Gribble, K. D. (2014). Formula feeding in emergencies. In Preedy V. R., Watson R. R., & Zibadi S. (Eds.), Handbook of dietary and nutritional aspects of bottle feeding. Wageningen Academic Publishers. 10.3920/978-90-8686-777-6 [DOI] [Google Scholar]
- Haase, B. , Brennan, E. , & Wagner, C. L. (2019). Effectiveness of the IBCLC: Have we made an impact on the care of breastfeeding families over the past decade? Journal of Human Lactation, 35(3), 441–452. 10.1177/0890334419851805 [DOI] [PubMed] [Google Scholar]
- Hall, R. C. W. , Hall, R. C. W. , & Chapman, M. J. (2008). The 1995 Kikwit Ebola outbreak: Lessons hospitals and physicians can apply to future viral epidemics. General Hospital Psychiatry, 30(5), 446–452. 10.1016/J.GENHOSPPSYCH.2008.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassiotou, F. , Hepworth, A. R. , Metzger, P. , Tat Lai, C. , Trengove, N. , Hartmann, P. E. , & Filgueira, L. (2013). Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clinical & Translational Immunology, 2(4), e3. 10.1038/cti.2013.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirani, S. A. A. , Richter, S. , Salami, B. O. , & Vallianatos, H. (2019). Breastfeeding in disaster relief camps. Advances in Nursing Science, 42(2), E1–E12. 10.1097/ANS.0000000000000231 [DOI] [PubMed] [Google Scholar]
- Holtz, B. , Smock, A. , & Reyes‐Gastelum, D. (2015). Connected motherhood: Social support for moms and moms‐to‐be on Facebook. Telemedicine and E‐Health, 21(5), 415–421. 10.1089/tmj.2014.0118 [DOI] [PubMed] [Google Scholar]
- Howell, E. A. , Mora, P. , & Leventhal, H. (2006). Correlates of early postpartum depressive symptoms. Maternal and Child Health Journal, 10(2), 149–157. 10.1007/s10995-005-0048-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley, K. M. , Black, M. M. , Papas, M. A. , & Caufield, L. E. (2008). Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. The Journal of Nutrition, 138(4), 799–805. 10.1093/jn/138.4.799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp . (2018). IBM SPSS Statistics for Mac OS. IBM Corp. [Google Scholar]
- IFE Core Group . (2017). Infant and young child feeding in emergencies (Vol. 3). [Google Scholar]
- Ishii, K. , Goto, A. , Ota, M. , Yasumura, S. , Abe, M. , & Fujimori, K. (2016). Factors associated with infant feeding methods after the nuclear power plant accident in Fukushima: Data from the pregnancy and birth survey for the fiscal year 2011 Fukushima Health Management Survey. Maternal and Child Health Journal, 20(8), 1704–1712. 10.1007/s10995-016-1973-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns, H. M. , Forster, D. A. , Amir, L. H. , & McLachlan, H. L. (2013). Prevalence and outcomes of breast milk expressing in women with healthy term infants: A systematic review. BMC Pregnancy and Childbirth, 13(1), 212. 10.1186/1471-2393-13-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joy, P. , Aston, M. , Price, S. , Sim, M. , Ollivier, R. , Benoit, B. , … Iduye, D. (2020). Blessings and curses: Exploring the experiences of new mothers during the COVID‐19 pandemic. Nursing Reports, 10(2), 207–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. J. , & Bostwick, W. (2020). Social vulnerability and racial inequality in COVID‐19 deaths in Chicago. Health Education & Behavior, 47(4), 509–513. 10.1177/1090198120929677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knaak, S. J. (2010). Contextualising risk, constructing choice: Breastfeeding and good mothering in risk society. Health, Risk and Society, 12(4), 345–355. 10.1080/13698571003789666 [DOI] [Google Scholar]
- Ko, N.‐Y. , Lu, W.‐H. , Chen, Y.‐L. , Li, D.‐J. , Wang, P.‐W. , Hsu, S.‐T. , … Yen, C.‐F. (2020). COVID‐19‐related information sources and psychological well‐being: An online survey in Taiwan. Brain, Behavior, and Immunity, 87, 153–154. 10.1016/j.bbi.2020.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackey, K. A. , Pace, R. M. , Williams, J. E. , Bode, L. , Donovan, S. M. , Järvinen, K. M. , … McGuire, M. K. (2020). SARS‐CoV‐2 and human milk: What is the evidence? Maternal and Child Nutrition, (May), 16, 1, e13032–12. 10.1111/mcn.13032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau, C. (2001). Effects of stress on lactation. Pediatric Clinics of North America, 48(1), 221–234. 10.1016/S0031-3955(05)70296-0 [DOI] [PubMed] [Google Scholar]
- Laugen, C. M. , Islam, N. , & Janssen, P. A. (2016). Social support and exclusive breast feeding among Canadian Women. Paediatric and Perinatal Epidemiology, 30(5), 430–438. 10.1111/ppe.12303 [DOI] [PubMed] [Google Scholar]
- Lauren Bauer . (2020). The COVID‐19 crisis has already left too many children hungry in America. Retrieved September 28, 2020, from The Hamilton Project website: https://www.hamiltonproject.org/blog/the_covid_19_crisis_has_already_left_too_many_children_hungry_in_america#_ftn1
- Lee, E. (2008). Living with risk in the age of “intensive motherhood”: Maternal identity and infant feeding. Health, Risk and Society, 10(5), 467–477. 10.1080/13698570802383432 [DOI] [Google Scholar]
- Maehara, K. , Mori, E. , Iwata, H. , Sakajo, A. , Aoki, K. , & Morita, A. (2017). Postpartum maternal function and parenting stress: Comparison by feeding methods. International Journal of Nursing Practice, 23, 1–8. 10.1111/ijn.12549 [DOI] [PubMed] [Google Scholar]
- McLeish, J. , & Redshaw, M. (2017). Mothers' accounts of the impact on emotional wellbeing of organised peer support in pregnancy and early parenthood: A qualitative study. BMC Pregnancy and Childbirth, 17(1), 1–14. 10.1186/s12884-017-1220-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezzacappa, E. S. (2004). Breastfeeding and maternal stress response and health. Nutrition Reviews, 62(7), 261–268. 10.1301/nr.2004.jul.261-268 [DOI] [PubMed] [Google Scholar]
- Niles, M. T. , Bertmann, F. , Belarmino, E. H. , Wentworth, T. , Biehl, E. , & Neff, R. (2020). The early food insecurity impacts of COVID‐19. Nutrients, 12(7). 10.3390/nu12072096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parent Health Education Resource Working Group . (2015). How to feed your baby with infant formula. Retrieved from https://novascotia.ca/dhw/healthy-development/documents/05115-How-to-Feed‐Your‐Baby‐with‐Infant‐Formula‐Linked‐Index‐En.pdf
- Pérez‐Escamilla, R. , Cunningham, K. , & Moran, V. H. (2020). COVID‐19 and maternal and child food and nutrition insecurity: A complex syndemic. Maternal & Child Nutrition, 16(3), e13036. 10.1111/mcn.13036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perren, S. , Von Wyl, A. , Bürgin, D. , Simoni, H. , & Von Klitzing, K. (2005). Depressive symptoms and psychosocial stress across the transition to parenthood: Associations with parental psychopathology and child difficulty. Journal of Psychosomatic Obstetrics and Gynecology, 26(3), 173–183. 10.1080/01674820400028407 [DOI] [PubMed] [Google Scholar]
- Reproductive Care Program of Nova Scotia . (2020). COVID‐19 and Pregnancy, Maternal and Newborn Care Maternal Child Bulletin #1‐April 16, 2020. Retrieved from https://when‐to‐call‐about‐covid19.novascotia.ca/en
- Shukri, M. , Husna, N. , Wells, J. C. K. , & Fewtrell, M. (2018). The effectiveness of interventions using relaxation therapy to improve breastfeeding outcomes: A systematic review. Maternal & Child Nutrition, 14(2). 10.1111/mcn.12563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada . (2018). Exclusive breastfeeding, at least 6 months, by age group. Retrieved from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009622
- Strange, C. , Fisher, C. , Howat, P. , & Wood, L. (2014). Fostering supportive community connections through mothers' groups and playgroups. Journal of Advanced Nursing, 70(12), 2835–2846. 10.1111/jan.12435 [DOI] [PubMed] [Google Scholar]
- Tang, S. , Mao, Y. , Jones, R. M. , Tan, Q. , Ji, J. S. , Li, N. , … Shi, X. (2020). Aerosol transmission of SARS‐CoV‐2? Evidence, prevention and control. Environment International, 144, 106039. 10.1016/j.envint.2020.106039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, E. N. , & Wallace, L. E. (2019). For shame: Feminism, breastfeeding advocacy, and maternal guilt. Hypatia, 27(1), 76–98. [Google Scholar]
- Telleen, S. , Herzog, A. , & Kilbane, T. L. (1989). Impact of a family support program on mothers' social support and parenting stress. American Journal of Orthopsychiatry, 59(3), 410–419. 10.1111/j.1939-0025.1989.tb01676.x [DOI] [PubMed] [Google Scholar]
- The Government of Canada . (2017). Nova Scotia Census Profile, 2016.
- Thomson, G. , Ebisch‐Burton, K. , & Flacking, R. (2015). Shame if you do—Shame if you don't: Women's experiences of infant feeding. Maternal & Child Nutrition, 11(1), 33–46. 10.1111/mcn.12148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Government . (2020). Disaster financial assistance with food, housing, and bills. Retrieved September 28, 2020, from https://www.usa.gov/disaster‐help‐food‐housing‐bills
- Van Bortel, T. , Basnayake, A. , Wurie, F. , Jambai, M. , Koroma, A. S. , Muana, A. T. , … Nellums, L. B. (2016). Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bulletin of the World Health Organization, 94, 210–214. 10.2471/BLT.15.158543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura, A. K. (2017). Associations between breastfeeding and maternal responsiveness: A systematic review of the literature. Advances in Nutrition: An International Review Journal, 8(3), 495–510. 10.3945/an.116.014753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ververs, B. M. , Hwang, C. , Fernandes, C. , Branco, M. , Aarts, M. , Modigell, I. , … Emary, C. (2019). Barriers to infant feeding in emergencies programming in middle and high‐income countries. (61), 24–26.
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, E. , An, N. , Gao, Z. , Kiprop, E. , & Geng, X. (2020). Consumer food stockpiling behavior and willingness to pay for food reserves in COVID‐19. Food Security, 12(4), 739–747. 10.1007/s12571-020-01092-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper, M. , Nápoles, A. M. , & Pérez‐Stable, E. J. (2020). COVID‐19 and racial/ethnic disparities. JAMA, 323(24), 2466–2467. 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson, J. A. , & Leung, C. W. (2020). Food insecurity and COVID‐19: Disparities in early effects for US adults. Nutrients, 12(6). 10.3390/nu12061648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2009). Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. [PubMed]
- World Health Organization . (2020a). Breastfeeding and COVID‐19. Retrieved from https://www.who.int/news‐room/commentaries/detail/breastfeeding‐and‐covid‐19
- World Health Organization . (2020b). How is WHO responding to COVID‐19? Retrieved September 27, 2020, from https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/who‐response‐in‐countries
- World Health Organization . (2020c). Infant and young child feeding. Retrieved from https://www.who.int/en/news‐room/fact‐sheets/detail/infant‐and‐young‐child‐feeding
- Yakoob, M. Y. , Theodoratou, E. , Jabeen, A. , Imdad, A. , Eisele, T. P. , Ferguson, J. , … Bhutta, Z. A. (2011). Preventive zinc supplementation in developing countries: Impact on mortality and morbidity due to diarrhea, pneumonia and malaria. BMC Public Health, 11(Suppl 3), S23. 10.1186/1471-2458-11-S3-S23 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


